| Revision as of 18:47, 20 July 2009 editWebHamster (talk | contribs)18,133 edits Undid revision 303178497 by Edison (talk) FM isn't officially a MUPS diagnosis regardless of what the refs say. The refs are right the prose is incorrect and POV← Previous edit | Latest revision as of 06:23, 3 December 2024 edit undo2601:642:c303:f370:95a7:1d7d:444c:ec64 (talk) ce | ||
| Line 1: | Line 1: | ||
| {{Short description|Chronic pain of unknown cause}} | |||
| {{pp-full}} | |||
| {{cs1 config|name-list-style=vanc}} | |||
| {{Infobox disease | |||
| {{Distinguish|text=] nor with ]}} | |||
| | Name = Fibromyalgia | |||
| <!--CFS/ME is often misremembered in conflation with FM because both involve themes of "chronic fatigue + hard to DDx + nosologic contentiousness", and MF is sometimes misremembered in conflation with FM because of the -my- and -fibr- syllables of the names plus symptom overlap (e.g., pain, fatigue).--> | |||
| | Image = | |||
| {{Use dmy dates|date=April 2021}} | |||
| | Caption = | |||
| {{Infobox medical condition (new) | |||
| | DiseasesDB = <!-- no entry --> | |||
| | name = Fibromyalgia | |||
| | image = Fibromyalgia pain sites APS 2019.svg | |||
| | caption = The nine possible pain sites of fibromyalgia according to the ]. | |||
| | ICDO = | |||
| | field =], ]<ref>{{Cite web |date=October 2009 |title=Neurology Now: Fibromyalgia: Is Fibromyalgia Real? {{!}} American Academy of Neurology |url=http://tools.aan.com/elibrary/neurologynow/?event=home.showArticle&id=ovid.com:/bib/ovftdb/01222928-200905050-00024 |access-date=1 June 2018 |website=tools.aan.com}}{{Dead link|date=December 2019 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> | |||
| | OMIM = | |||
| | pronounce = {{IPAc-en|ˌ|f|aɪ|b|r|oʊ|m|aɪ|ˈ|æ|l|dʒ|ə}}<ref>{{Cite web |title=fibromyalgia |url=http://www.collinsdictionary.com/dictionary/american/fibromyalgia |url-status=live |archive-url=https://web.archive.org/web/20151004020527/http://www.collinsdictionary.com/dictionary/american/fibromyalgia |archive-date=4 October 2015 |access-date=16 March 2016 |website=Collins Dictionaries}}</ref> | |||
| | MedlinePlus = 000427 | |||
| | synonyms = Fibromyalgia syndrome | |||
| | eMedicineSubj = med | |||
| | symptoms = Widespread pain, feeling tired, sleep problems<ref name="pmid21303476"/><ref name=JAMA2014/> | |||
| | eMedicineTopic = 790 | |||
| | complications = | |||
| | eMedicine_mult = {{eMedicine2|med|2934}} {{eMedicine2|ped|777}} {{eMedicine2|pmr|47}} | |||
| | onset = Early-Middle age<ref name=NIH2014Tx/> | |||
| | duration = Long term<ref name="pmid21303476"/> | |||
| | causes = Unknown<ref name=JAMA2014/><ref name=NIH2014Tx/> | |||
| | risks = | |||
| | diagnosis = Based on symptoms after ruling out other potential causes<ref name=JAMA2014/><ref name=NIH2014Tx/> | |||
| | differential = ], ] (such as ], ], ], ], or ]), ], ], ]<ref>{{Cite book |title=Ferri's differential diagnosis: a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders |vauthors=Ferri FF |date=2010 |publisher=Elsevier/Mosby |isbn=978-0-323-07699-9 |edition=2nd |location=Philadelphia, PA |chapter=Chapter F}}</ref><ref>{{Cite journal |vauthors=Schneider MJ, Brady DM, Perle SM |date=2006 |title=Commentary: differential diagnosis of fibromyalgia syndrome: proposal of a model and algorithm for patients presenting with the primary symptom of chronic widespread pain |journal=Journal of Manipulative and Physiological Therapeutics |volume=29 |issue=6 |pages=493–501 |doi=10.1016/j.jmpt.2006.06.010 |pmid=16904498}}</ref> | |||
| | prevention = | |||
| | treatment = Sufficient sleep and exercise<ref name=NIH2014Tx/> | |||
| | medication = ], ], ], ]<ref name=NIH2014Tx/><ref name=Coch2017Gab/> | |||
| | prognosis = Normal life expectancy<ref name=NIH2014Tx/> | |||
| | frequency = 2%<ref name=JAMA2014/> | |||
| | deaths = | |||
| }} | }} | ||
| <!-- Definition and symptoms --> | |||
| '''Fibromyalgia''' (new lat., ''fibro-'', fibrous tissue, Gk. ''myo-'', muscle, Gk. ''algos-'', pain), meaning ] and ] pain (also referred to as FM or FMS), is a disorder classified by the presence of chronic widespread ] and a heightened and painful response to pressure (]).<ref name=Wolfe>{{cite journal |author=Wolfe F, Smythe HA, Yunus MB ''et al.'' |title=The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee |journal=Arthritis Rheum. |volume=33 |issue=2 |pages=160–72 |month=February |year=1990 |pmid=2306288 |doi=10.1002/art.1780330203 }}</ref> Other core symptoms are debilitating fatigue, sleep disturbance, and joint stiffness. Other symptoms include ],<ref name=p15361320>{{cite journal |author=Wallace DJ, Hallegua DS. |title=Fibromyalgia: the gastrointestinal link. |journal=Curr Pain Headache Rep. |volume=8 |issue=5 |pages=364–8 |month=October |year=2002 |pmid=15361320 }}</ref> bowel and bladder abnormalities,<ref name=p9201654>{{cite journal |author=Clauw DJ, Schmidt M, Radulovic D, Singer A, Katz P, Bresette J. |title=The relationship between fibromyalgia and interstitial cystitis. |journal=J Psychiatr Res. |volume=31 |issue=1 |pages=125–31 |month=Jan-February |year=1997 |pmid=9201654 }}</ref> numbness and tingling (]),<ref name=p3184073 >{{cite journal |author=Simms RW, Goldenberg DL.|title=Symptoms mimicking neurologic disorders in fibromyalgia syndrome. |journal=J Rheumatol.|volume=15 |issue=8 |pages=1271–3 |month=August |year=1988 |pmid=3184073 }}</ref> and cognitive dysfunction.<ref name=p17092441>{{cite journal |author=Glass JM.|title=Cognitive dysfunction in fibromyalgia and chronic fatigue syndrome: new trends and future directions. |journal=Curr Rheumatol Rep. |volume=8 |issue=6 |pages=425–9 |month=December |year=2006 |pmid=17092441 }}</ref> An increased prevalence of affective- and anxiety-disorders is also well known.<ref name=p17894922 >{{cite journal |author=Buskila D, Cohen H.|title=Comorbidity of fibromyalgia and psychiatric disorders. |journal=Curr Pain Headache Rep.|volume=11 |issue=5 |pages=333–8 |month=October |year=2007 |pmid=17894922 }}</ref> Because fibromyalgia involves more than just pain, the term "'''fibromyalgia syndrome'''" is often used. However, not all affected persons experience all associated symptoms.<ref name=p6582267 >{{cite journal |author=Yunus MB.|title=Fibromyalgia syndrome: a need for uniform classification. |journal=J Rheumatol. |volume=10 |issue=6 |pages=841 |month=December |year=1983 |pmid=6582267 }}</ref> | |||
| '''Fibromyalgia''' is a ] that causes chronic widespread ], accompanied by ], awakening unrefreshed, and ]. Other symptoms can include ], ] or ]s, and ].<ref name="Wolfe2016">{{Cite journal |display-authors=6 |vauthors=Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, Mease PJ, Russell AS, Russell IJ, Walitt B |date=December 2016 |title=2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria |journal=Seminars in Arthritis and Rheumatism |volume=46 |issue=3 |pages=319–329 |doi=10.1016/j.semarthrit.2016.08.012 |pmid=27916278}}</ref> People with fibromyalgia can also experience ]<ref name="Wu-2017" /> and general ].<ref name="Hauser2019" /><ref name="Arnold-2019" /> <!--Cause, mechanism, and diagnosis --> The cause of fibromyalgia is unknown, but is believed to involve a combination of genetic and environmental factors.<ref name=JAMA2014/> Environmental factors may include ], ], and some ]s.<ref name=JAMA2014/> Since the pain appears to result from processes in the ], the condition is referred to as a "central sensitization syndrome".<ref name=JAMA2014/><ref name="Central sensitivity and fibromyalgi" /> Although a protocol using an algometer (algesiometer) for determining central sensitization has been proposed as an objective diagnostic test, fibromyalgia continues to be primarily ] despite the high possibility of misdiagnosis.<ref name=":6" /> | |||
| <!--Epidemiology, history, and culture --> | |||
| <br /> | |||
| Fibromyalgia was first defined in 1990, with updated criteria in 2011,<ref name="JAMA2014">{{Cite journal |vauthors=Clauw DJ |date=April 2014 |title=Fibromyalgia: a clinical review |journal=JAMA |volume=311 |issue=15 |pages=1547–1555 |doi=10.1001/jama.2014.3266 |pmid=24737367 |s2cid=43693607}}</ref> 2016,<ref name=Wolfe2016/> and 2019.<ref name="Arnold-2019" /> The term 'fibromyalgia' is from ] ''fibro-'', meaning 'fibrous tissues'; ] μυο- ''myo-'', 'muscle'; and Greek άλγος ''algos'', 'pain'; thus, the term literally means "'] and ] pain'.<ref>{{Cite book |url=https://books.google.com/books?id=JxEiRjNm8nMC&pg=PA165 |title=Neurobiological foundations for EMDR practice |vauthors=Bergmann U |date=2012 |publisher=Springer Pub. Co. |isbn=978-0-8261-0938-5 |location=New York |page=165}}</ref> Fibromyalgia is estimated to affect 2 to 4% of the population.<ref name="Fitz2021">{{Cite journal |vauthors=Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W |date=May 2021 |title=Nociplastic pain: towards an understanding of prevalent pain conditions |journal=Lancet |volume=397 |issue=10289 |pages=2098–2110 |doi=10.1016/s0140-6736(21)00392-5 |pmid=34062144 |s2cid=235245552}}</ref> Women are affected about twice as often as men.<ref name=JAMA2014/><ref name=Fitz2021/> Rates appear similar across areas of the world and among varied cultures.<ref name=JAMA2014/> | |||
| <!-- Prevention, treatment, and prognosis --> | |||
| The treatment of fibromyalgia is ]<ref name="Prab2019" /> and ].<ref name="Macfarlane-2017" /> The ] strongly recommends ] and ].<ref name="Macfarlane-2017" /> Weak recommendations are given for ], ], ], ], and meditative exercise such as ], ], and ].<ref name="Macfarlane-2017" /> The use of medication in the treatment of fibromyalgia is debated,<ref name="Macfarlane-2017" /><ref name="Hauser2018" /> although ]s can improve ].<ref name="Mascarenhas-2021" /> Other medications commonly considered helpful in managing fibromyalgia include ], ]s, and ]s.<ref>{{Cite journal |vauthors=Kia S, Choy E |date=May 2017 |title=Update on Treatment Guideline in Fibromyalgia Syndrome with Focus on Pharmacology |journal=Biomedicines |language=English |volume=5 |issue=2 |pages=20 |doi=10.3390/biomedicines5020020 |pmc=5489806 |pmid=28536363 |doi-access=free}}</ref> ] and ] supplements may ] and improve quality of life.<ref name="Ibáñez-Vera-2018" /> While symptoms of fibromyalgia are persistent in nearly all patients, they are not caused by ] or any ].<ref name="Hauser2018" /> | |||
| {{TOC limit|3}} | |||
| ==History== | |||
| Chronic widespread pain had been described in the literature in the 19th century, but the term ''fibromyalgia'' was not first used until 1976, when ] used it to describe these symptoms.<ref name="pmid19623319"/> Many names, including '''muscular rheumatism''', ''fibrositis'', ''psychogenic rheumatism'', and '']'' were applied historically to symptoms resembling those of fibromyalgia.<ref>{{Cite web |last=Health Information Team |date=February 2004 |title=Fibromyalgia |url=http://hcd2.bupa.co.uk/fact_sheets/mosby_factsheets/fibromyalgia.html |url-status=dead |archive-url=https://web.archive.org/web/20060622064234/http://hcd2.bupa.co.uk/fact_sheets/mosby_factsheets/fibromyalgia.html |archive-date=22 June 2006 |access-date=24 August 2006 |publisher=BUPA insurance}}</ref> The term ''fibromyalgia'' was coined by researcher Mohammed Yunus as a synonym for fibrositis. and was first used in a scientific publication in 1981.<ref>{{Cite journal |vauthors=Yunus M, Masi AT, Calabro JJ, Miller KA, Feigenbaum SL |date=August 1981 |title=Primary fibromyalgia (fibrositis): clinical study of 50 patients with matched normal controls |journal=Seminars in Arthritis and Rheumatism |volume=11 |issue=1 |pages=151–171 |doi=10.1016/0049-0172(81)90096-2 |pmid=6944796}}</ref> Fibromyalgia is from the ] ''fibra'' (fiber)<ref>{{Cite web |title=Fibro- |url=http://dictionary.reference.com/browse/fibro- |url-status=live |archive-url=https://web.archive.org/web/20091213070938/http://dictionary.reference.com/browse/fibro- |archive-date=13 December 2009 |access-date=21 May 2008 |publisher=Dictionary.com}}</ref> and the ] words ''myo'' (muscle)<ref>{{Cite web |date=12 April 2009 |title=Meaning of myo |url=http://www.bartleby.com/61/94/M0509400.html |archive-url=https://web.archive.org/web/20090412005428/http://www.bartleby.com/61/94/M0509400.html |archive-date=12 April 2009 |access-date=26 August 2012}}</ref> and ''algos'' (pain).<ref>{{Cite web |date=12 April 2009 |title=Meaning of algos |url=http://www.bartleby.com/61/59/A0195900.html |archive-url=https://web.archive.org/web/20090412005958/http://www.bartleby.com/61/59/A0195900.html |archive-date=12 April 2009 |access-date=26 August 2012}}</ref> | |||
| Historical perspectives on the development of the fibromyalgia concept note the "central importance" of a 1977 paper on fibrositis by Smythe and Moldofsky.<ref name=FMWars/><ref>{{Cite journal |vauthors=Smythe HA, Moldofsky H |year=1977 |title=Two contributions to understanding of the "fibrositis" syndrome |journal=Bulletin on the Rheumatic Diseases |volume=28 |issue=1 |pages=928–931 |pmid=199304}}</ref> The first ], controlled study of the characteristics of fibromyalgia syndrome was published in 1981,<ref name="Winfield">{{Cite journal |vauthors=Winfield JB |date=June 2007 |title=Fibromyalgia and related central sensitivity syndromes: twenty-five years of progress |journal=Seminars in Arthritis and Rheumatism |volume=36 |issue=6 |pages=335–338 |doi=10.1016/j.semarthrit.2006.12.001 |pmid=17303220}}</ref> providing support for symptom associations. In 1984, an interconnection between fibromyalgia syndrome and other similar conditions was proposed,<ref name="Inanici">{{Cite journal |vauthors=Inanici F, Yunus MB |date=October 2004 |title=History of fibromyalgia: past to present |journal=Current Pain and Headache Reports |volume=8 |issue=5 |pages=369–378 |doi=10.1007/s11916-996-0010-6 |pmid=15361321 |s2cid=42573740}}</ref> and in 1986, trials of the first proposed medications for fibromyalgia were published.<ref name=Inanici/> | |||
| While historically considered either a musculoskeletal disease or neuropsychiatric condition, evidence from research conducted in the last three decades has demonstrated abnormalities within the ] affecting brain regions that may be linked both to clinical symptoms and research phenomena. Despite these abnormalities, fibromyalgia might be the result of childhood stress or prolonged or severe stress rather than a primary disorder of the brain. <ref name=p18270311 >{{cite journal |author=Schweinhardt P, Sauro KM, Bushnell MC. |title=Fibromyalgia: a disorder of the brain? |journal=Neuroscientist. |volume=14 |issue=5 |pages=415–21 |month=October |year=2008 |pmid=18270311 }}</ref> There is no recognized cure for fibromyalgia, but some treatments have been demonstrated by controlled clinical trials to be effective in reducing symptoms, including medications, patient education, exercise, and behavioral interventions.<ref name=Goldenberg2008/> | |||
| A 1987 article in the '']'' used the term 'fibromyalgia syndrome', while saying it was a "controversial condition".<ref name="Goldenberg1987">{{Cite journal |vauthors=Goldenberg DL |date=May 1987 |title=Fibromyalgia syndrome. An emerging but controversial condition |journal=JAMA |volume=257 |issue=20 |pages=2782–2787 |doi=10.1001/jama.257.20.2782 |pmid=3553636}}</ref> The ] (ACR) published its first classification criteria for fibromyalgia in 1990.<ref name="Wolfe">{{Cite journal |display-authors=6 |vauthors=Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P |date=February 1990 |title=The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee |journal=Arthritis and Rheumatism |volume=33 |issue=2 |pages=160–172 |doi=10.1002/art.1780330203 |pmid=2306288}}</ref> Later revisions were made in 2010,<ref name="Wolfe2010" /> 2016,<ref name="Wolfe2016" /> and 2019.<ref name="Arnold-2019" /> | |||
| ==Classification== | |||
| Fibromyalgia is a controversial diagnosis. Many members of the medical community consider fibromyalgia a ‘non-disease’ because of a lack of abnormalities on physical examination, the absence of objective diagnostic tests,<ref name=FMWars>{{cite journal |author=Wolfe F |title=Fibromyalgia wars |journal=J Rheumatol. |volume=36 |issue=4 |pages=679-83 |month=April |year=2009 |pmid=19342721 }}</ref><ref name<ref name=p7880118>{{cite journal |author=Goldenberg DL |title=Fibromyalgia: why such controversy? |journal=Ann. Rheum. Dis. |volume=54 |issue=1 |pages=3–5 |year=1995 |month=January |pmid=7880118 |pmc=1005499 |doi= |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1005499}}</ref> and extensive overlap with other proposed conditions like ] and ].<ref name="Deary"/><ref name=Buchwald>{{cite journal |author=Buchwald D, Garrity D |title=Comparison of patients with chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities |journal=Arch Intern Med |volume=154 |issue=18 |pages=2049-53 |year=1995 |month=September |pmid=8092909 }}</ref> Although several brain imaging studies have show evidence for possible neurological differences in fibromyalgia and healthy controls, these studies may show only correlation, not causation,<ref name=FMWars/> and fibromyalgia might be the result of childhood stress or prolonged or severe stress rather than a primary disorder of the brain.<ref name=p18270311 >{{cite journal |author=Schweinhardt P, Sauro KM, Bushnell MC. |title=Fibromyalgia: a disorder of the brain? |journal=Neuroscientist. |volume=14 |issue=5 |pages=415–21 |month=October |year=2008 |pmid=18270311 }}</ref> | |||
| Fibromyalgia is classified as a disorder of ] processing due to abnormalities in how pain signals are processed in the ].<ref name="Clauw-2011">{{Cite journal |vauthors=Clauw DJ, Arnold LM, McCarberg BH |date=September 2011 |title=The science of fibromyalgia |journal=Mayo Clinic Proceedings |volume=86 |issue=9 |pages=907–911 |doi=10.4065/mcp.2011.0206 |pmc=3258006 |pmid=21878603}}</ref> The ] (]) includes fibromyalgia in the category of "Chronic widespread pain," code MG30.01.<ref>{{Cite web |title=ICD-11 for Mortality and Morbidity Statistics |url=https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/849253504 |url-status=live |archive-url=https://archive.today/20180801205234/https://icd.who.int/browse11/l-m/en%23/http://id.who.int/icd/entity/294762853#/http://id.who.int/icd/entity/849253504 |archive-date=1 August 2018 |access-date=2022-04-09 |website=icd.who.int}}</ref> People with fibromyalgia differ in several dimensions: severity, adjustment, symptom profile, psychological profile, and response to treatment.<ref>{{Cite journal |last=Gianlorenço |first=Anna Carolyna |last2=Costa |first2=Valton |last3=Fabris-Moraes |first3=Walter |last4=Menacho |first4=Maryela |last5=Alves |first5=Luana Gola |last6=Martinez-Magallanes |first6=Daniela |last7=Fregni |first7=Felipe |date=2024-05-15 |title=Cluster analysis in fibromyalgia: a systematic review |url=https://link.springer.com/10.1007/s00296-024-05616-2 |journal=Rheumatology International |language=en |doi=10.1007/s00296-024-05616-2 |issn=1437-160X |pmid=38748219}}</ref> | |||
| ==Signs and symptoms== | ==Signs and symptoms== | ||
| The defining symptoms of fibromyalgia are chronic widespread ], ], and ].<ref name="Arnold-2019" /> Other symptoms may include heightened pain in response to tactile pressure (]),<ref name="Arnold-2019" /> cognitive problems,<ref name="Arnold-2019" /> ] stiffness,<ref name="Arnold-2019" /> ],<ref name="Arnold-2019" /> ],<ref name="Arnold-2019" /> ],<ref>{{Cite journal |vauthors=Besiroglu MD, Dursun MD |date=July 2019 |title=The association between fibromyalgia and female sexual dysfunction: a systematic review and meta-analysis of observational studies |journal=International Journal of Impotence Research |volume=31 |issue=4 |pages=288–297 |doi=10.1038/s41443-018-0098-3 |pmid=30467351 |s2cid=53717513}}</ref> and visual symptoms.<ref>{{Cite journal |vauthors=Zdebik N, Zdebik A, Bogusławska J, Przeździecka-Dołyk J, Turno-Kręcicka A |date=January 2021 |title=Fibromyalgia syndrome and the eye – A review |journal=Survey of Ophthalmology |volume=66 |issue=1 |pages=132–137 |doi=10.1016/j.survophthal.2020.05.006 |pmid=32512032 |s2cid=219548664}}</ref> Some people with fibromyalgia experience ], in which symptoms flare up a day or longer after physical exercise.<ref>{{Cite web |title=Archived copy |url=https://academic.oup.com/painmedicine/article/23/6/1144/6404604 |url-status=live |archive-url=https://web.archive.org/web/20230521195848/https://academic.oup.com/painmedicine/article/23/6/1144/6404604 |archive-date=21 May 2023 |access-date=2024-02-11 |website=academic.oup.com}}</ref> | |||
| === Pain === | |||
| The defining symptoms of fibromyalgia are chronic, widespread pain, fatigue, and heightened pain in response to pressure (]). Other symptoms may include tingling of the skin, prolonged ], ] in the limbs, ], functional bowel disturbances,<ref name=p15361320/> and chronic ].<ref name=pmid169541>{{cite journal |author=Moldofsky H, Scarisbrick P, England R, Smythe H |title=Musculosketal symptoms and non-REM sleep disturbance in patients with "fibrositis syndrome" and healthy subjects |journal=Psychosom Med |volume=37 |issue=4 |pages=341–51 |year=1975 |pmid=169541 |doi= |url=http://www.psychosomaticmedicine.org/cgi/pmidlookup?view=long&pmid=169541 |accessdate=2008-05-21}}</ref> | |||
| Fibromyalgia is predominantly a chronic ] disorder.<ref name="Arnold-2019" /> According to the ], widespread pain is one major symptom, which could feel like an ache, a burning sensation, or a sharp, stabbing pain.<ref>{{Cite web |date=2017-10-20 |title=Fibromyalgia – Symptoms |url=https://www.nhs.uk/conditions/fibromyalgia/symptoms/ |url-status=live |archive-url=https://web.archive.org/web/20180323080320/https://www.nhs.uk/conditions/fibromyalgia/symptoms/ |archive-date=23 March 2018 |access-date=2020-10-21 |website=nhs.uk |language=en}}</ref> Patients are also highly sensitive to pain, and the slightest touch can cause pain. Pain also tends to linger for longer when a patient experiences pain.<ref>{{Cite web |date=2017-10-20 |title=Fibromyalgia - Symptoms |url=https://www.nhs.uk/conditions/fibromyalgia/symptoms/ |access-date=2024-04-11 |website=nhs.uk |language=en}}</ref> | |||
| === Fatigue === | |||
| Many patients experience cognitive dysfunction<ref name=p17092441/> (known as "brain fog" or "fibrofog"), which may be characterized by impaired concentration,<ref name=pmid17041327>{{cite journal |author=Leavitt F, Katz RS, Mills M, Heard AR |title=Cognitive and Dissociative Manifestations in Fibromyalgia |journal=J Clin Rheumatol. |volume=8 |issue=2 |pages=77–84 |year=2002 |pmid=17041327|doi=10.1097/00124743-200204000-00003}}</ref> problems with ]<ref name=pmid17041327/><ref name=pmid17894922>{{cite journal |author=Buskila D, Cohen H |title=Comorbidity of fibromyalgia and psychiatric disorders |journal=Curr Pain Headache Rep |volume=11 |issue=5 |pages=333–8 |year=2007 |month=October |pmid=17894922 |doi= 10.1007/s11916-007-0214-4|url= |accessdate=2008-05-21}}</ref> and ], short-term memory consolidation,<ref name=pmid17894922/> impaired speed of performance,<ref name=pmid17041327/><ref name=pmid17894922/> inability to multi-task, cognitive overload,<ref name=pmid17041327/><ref name=pmid17894922/> diminished ], ], and ] symptoms.<ref name=pmid17894922/> | |||
| ] is one of the defining symptoms of fibromyalgia.<ref name="Arnold-2019" /> Patients may experience physical or mental fatigue. Physical fatigue can present as a feeling of exhaustion after ] or limitation in daily activities.<ref name="Arnold-2019" /> | |||
| === Sleep problems === | |||
| Other symptoms often attributed to fibromyalgia that may possibly be due to a ] disorder include ] also referred to as Chronic Myofascial Pain, diffuse non-dermatomal ]s, functional bowel disturbances and ] (possibly linked to lower levels of ],<ref name=pmid17689128>{{cite journal |author=Tander B, Atmaca A, Aliyazicioglu Y, Canturk F |title=Serum ghrelin levels but not GH, IGF-1 and IGFBP-3 levels are altered in patients with fibromyalgia syndrome |journal=Joint Bone Spine |volume=74 |issue=5 |pages=477–81 |year=2007 |month=October |pmid=17689128 |doi=10.1016/j.jbspin.2007.01.024 |url=http://linkinghub.elsevier.com/retrieve/pii/S1297-319X(07)00183-2 |accessdate=2008-05-21}}</ref> ] symptoms and ], ] disorders, ]s, ], and symptomatic ]. Although fibromyalgia is classified based on the presence of chronic widespread pain, pain may also be localized in areas such as the ]s, ], low ], ]s, or other areas. Many sufferers also experience varying degrees of facial pain and have high rates of comorbid ]. | |||
| Sleep problems are a core symptom of fibromyalgia.<ref name="Arnold-2019" /> These include ], awakening while sleeping, and waking up feeling unrefreshed.<ref name="Arnold-2019" /> A ] compared ] and ] sleep metrics in people with fibromyalgia and healthy people. Individuals with fibromyalgia indicated lower sleep quality and efficiency, longer wake time after sleep start, shorter sleep duration, lighter sleep, and greater trouble initiating sleep when quantitatively assessed; and more difficulty initiating sleep when qualitatively assessed.<ref name="Wu-2017">{{Cite journal |vauthors=Wu YL, Chang LY, Lee HC, Fang SC, Tsai PS |date=May 2017 |title=Sleep disturbances in fibromyalgia: A meta-analysis of case-control studies |journal=Journal of Psychosomatic Research |volume=96 |pages=89–97 |doi=10.1016/j.jpsychores.2017.03.011 |pmid=28545798}}</ref> Sleep problems may contribute to pain by decreased release of ] and ], leading to decreased ].<ref>{{Cite journal |vauthors=Kimura S, Toyoura M, Toyota Y, Takaoka Y |date=December 2020 |title=Serum concentrations of insulin-like growth factor-1 as a biomarker of improved circadian rhythm sleep-wake disorder in school-aged children |journal=Journal of Clinical Sleep Medicine |volume=16 |issue=12 |pages=2073–2078 |doi=10.5664/jcsm.8778 |pmc=7848940 |pmid=32876042}}</ref> Improving sleep quality can help people with fibromyalgia manage pain.<ref>{{Cite journal |vauthors=Spaeth M, Rizzi M, Sarzi-Puttini P |date=April 2011 |title=Fibromyalgia and sleep |journal=Best Practice & Research. Clinical Rheumatology |volume=25 |issue=2 |pages=227–239 |doi=10.1016/j.berh.2011.03.004 |pmid=22094198}}</ref><ref name="bradley">{{Cite journal |vauthors=Bradley LA |date=December 2009 |title=Pathophysiology of fibromyalgia |journal=The American Journal of Medicine |volume=122 |issue=12 Suppl |pages=S22–S30 |doi=10.1016/j.amjmed.2009.09.008 |pmc=2821819 |pmid=19962493}}</ref> | |||
| === Cognitive problems === | |||
| An epidemiology study consisting of an internet-based survey of 2,596 people with fibromyalgia<ref name=p17349056 >{{cite journal |author=Bennett RM, Jones J, Turk DC, Russell IJ, Matallana L.|title=An internet survey of 2,596 people with fibromyalgia.|journal=BMC Musculoskelet Disord. 9;8:27. |volume=9 |issue=6 |pages=27 |year=2007 |month=March |pmid=17349056 }}</ref> reported that the most frequently cited factors perceived to worsen fibromyalgia symptoms were emotional distress (83%), weather changes (80%), sleeping problems (79%), strenuous activity (70%), mental stress (68%), worrying (60%), car travel (57%), family conflicts (52%), physical injuries (50%) and physical inactivity (50%). Other factors included infections, allergies, lack of emotional support, perfectionism, side effects of medications, and chemical exposures. | |||
| Many people with fibromyalgia experience ] (known as ''fibrofog'' or ]). One study found that approximately 50% of fibromyalgia patients experienced subjective cognitive dysfunction and that it was associated with higher levels of pain and other fibromyalgia symptoms.<ref>{{Cite journal |vauthors=Wolfe F, Rasker JJ, Ten Klooster P, Häuser W |date=December 2021 |title=Subjective Cognitive Dysfunction in Patients With and Without Fibromyalgia: Prevalence, Predictors, Correlates, and Consequences |journal=Cureus |volume=13 |issue=12 |pages=e20351 |doi=10.7759/cureus.20351 |pmc=8752385 |pmid=35036191 |doi-access=free}}</ref> The ] recognizes these problems as a major feature of fibromyalgia, characterized by trouble ], ], and ].<ref name="Arnold-2019" /> About 75% of people with fibromyalgia report significant problems with concentration, memory, and multitasking.<ref name="Bell2018">{{Cite journal |vauthors=Bell T, Trost Z, Buelow MT, Clay O, Younger J, Moore D, Crowe M |date=September 2018 |title=Meta-analysis of cognitive performance in fibromyalgia |journal=Journal of Clinical and Experimental Neuropsychology |volume=40 |issue=7 |pages=698–714 |doi=10.1080/13803395.2017.1422699 |pmc=6151134 |pmid=29388512}}</ref> A 2018 meta-analysis found that the largest differences between people with fibromyalgia and healthy subjects were in ], memory, and ].<ref name=Bell2018/> It is hypothesized that the chronic pain in fibromyalgia compromises attention systems, resulting in cognitive problems.<ref name=Bell2018/> | |||
| == |
=== Hypersensitivity === | ||
| In addition to ], patients with fibromyalgia experience hypersensitivity to other stimuli,<ref name="Hauser2019" /> such as bright lights, loud noises, perfumes, and ].<ref name="Arnold-2019" /> A ] found that they have a lower cold ].<ref>{{Cite journal |vauthors=Berwick RJ, Siew S, Andersson DA, Marshall A, Goebel A |date=May 2021 |title=A Systematic Review Into the Influence of Temperature on Fibromyalgia Pain: Meteorological Studies and Quantitative Sensory Testing |journal=The Journal of Pain |volume=22 |issue=5 |pages=473–486 |doi=10.1016/j.jpain.2020.12.005 |pmid=33421589 |s2cid=231437516 |doi-access=free}}</ref> Other studies documented an acoustic hypersensitivity.<ref>{{Cite journal |vauthors=Staud R, Godfrey MM, Robinson ME |date=August 2021 |title=Fibromyalgia Patients Are Not Only Hypersensitive to Painful Stimuli But Also to Acoustic Stimuli |journal=The Journal of Pain |volume=22 |issue=8 |pages=914–925 |doi=10.1016/j.jpain.2021.02.009 |pmid=33636370 |s2cid=232066286 |doi-access=free}}</ref> | |||
| The cause of fibromyalgia is currently unknown. However, several hypotheses have been developed. | |||
| == Comorbidity == | |||
| === Genetic predisposition === | |||
| Fibromyalgia as a stand-alone diagnosis is uncommon, as most fibromyalgia patients often have other chronic overlapping pain problems or ]s.<ref name=Hauser2019/> Fibromyalgia is associated with ] issues like ],<ref name="Kleykamp-2021">{{cite journal | vauthors = Kleykamp BA, Ferguson MC, McNicol E, Bixho I, Arnold LM, Edwards RR, Fillingim R, Grol-Prokopczyk H, Turk DC, Dworkin RH | display-authors = 6 | title = The Prevalence of Psychiatric and Chronic Pain Comorbidities in Fibromyalgia: an ACTTION systematic review | journal = Seminars in Arthritis and Rheumatism | volume = 51 | issue = 1 | pages = 166–174 | date = February 2021 | pmid = 33383293 | doi = 10.1016/j.semarthrit.2020.10.006 | s2cid = 229948862 }}</ref> ],<ref name="JAMA2014" /><ref name="Kleykamp-2021" /> ],<ref name="Kleykamp-2021" /> ],<ref>{{cite journal | vauthors = Habibi Asgarabad M, Salehi Yegaei P, Jafari F, Azami-Aghdash S, Lumley MA | title = The relationship of alexithymia to pain and other symptoms in fibromyalgia: A systematic review and meta-analysis | journal = European Journal of Pain | volume = 27 | issue = 3 | pages = 321–337 | date = March 2023 | pmid = 36471652 | doi = 10.1002/ejp.2064 | s2cid = 254273680 }}</ref> and depression.<ref name="Kleykamp-2021" /><ref name="Fitz2018">{{cite journal | vauthors = Fitzcharles MA, Perrot S, Häuser W | title = Comorbid fibromyalgia: A qualitative review of prevalence and importance | journal = European Journal of Pain | volume = 22 | issue = 9 | pages = 1565–1576 | date = October 2018 | pmid = 29802812 | doi = 10.1002/ejp.1252 | s2cid = 44068037 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Yepez D, Grandes XA, Talanki Manjunatha R, Habib S, Sangaraju SL | title = Fibromyalgia and Depression: A Literature Review of Their Shared Aspects | journal = Cureus | volume = 14 | issue = 5 | pages = e24909 | date = May 2022 | pmid = 35698706 | pmc = 9187156 | doi = 10.7759/cureus.24909 | doi-access = free }}</ref> Patients with fibromyalgia are five times more likely to have major depression than the general population.<ref>{{cite journal | vauthors = Løge-Hagen JS, Sæle A, Juhl C, Bech P, Stenager E, Mellentin AI | title = Prevalence of depressive disorder among patients with fibromyalgia: Systematic review and meta-analysis | journal = Journal of Affective Disorders | volume = 245 | pages = 1098–1105 | date = February 2019 | pmid = 30699852 | doi = 10.1016/j.jad.2018.12.001 | s2cid = 73411416 }}</ref> Experiencing pain and limited energy from having fibromyalgia leads to less activity, leading to ] and increased stress levels, which tends to cause anxiety and depression.<ref>{{Cite web |last1=Bruce |first1=Debra Fulghum |last2=PhD |title=Fibromyalgia and Depression |url=https://www.webmd.com/fibromyalgia/fibromyalgia-and-depression |access-date=2024-04-01 |website=WebMD |language=en}}</ref> | |||
| There is evidence that genetic factors may play a role in the development of fibromyalgia. For example, there is a high aggregation of fibromyalgia in families.<ref>{{cite journal |author=Stormorken H |coauthors=Brosstad F |authorlink=Helge Stormorken |title=Fibromyalgia: family clustering and sensory urgency with early onset indicate genetic predisposition and thus a "true" disease |journal=Scand J Rheumatol. |volume=21 |issue=4 |pages=207 |year=1992 |pmid=1529291 |doi=10.3109/03009749209099225}}</ref><ref>{{cite journal |author=Arnold LM, Hudson JI, Hess EV, ''et al.'' |title=Family study of fibromyalgia |journal=Arthritis Rheum. |volume=50 |issue=3 |pages=944–52 |year=2004 |month=March |pmid=15022338 |doi=10.1002/art.20042}}</ref> The mode of inheritance is currently unknown, but it is most probably ].<ref>{{cite journal |author=Buskila D, Sarzi-Puttini P |title=Biology and therapy of fibromyalgia. Genetic aspects of fibromyalgia syndrome |journal=Arthritis Res Ther. |volume=8 |issue=5 |pages=218 |year=2006 |pmid=16887010 |pmc=1779444 |doi=10.1186/ar2005}}</ref> Research has demonstrated that fibromyalgia is associated with polymorphisms of genes in the serotoninergic,<ref>{{cite journal |author=Cohen H, Buskila D, Neumann L, Ebstein RP |title=Confirmation of an association between fibromyalgia and serotonin transporter promoter region (5- HTTLPR) polymorphism, and relationship to anxiety-related personality traits |journal=Arthritis Rheum. |volume=46 |issue=3 |pages=845–7 |year=2002 |month=March |pmid=11920428 |doi=10.1002/art.10103 }}</ref> dopaminergic<ref>{{cite journal |author=Buskila D, Dan B, Cohen H, ''et al.'' |title=An association between fibromyalgia and the dopamine D4 receptor exon III repeat polymorphism and relationship to novelty seeking personality traits |journal=Mol. Psychiatry |volume=9 |issue=8 |pages=730–1 |year=2004 |month=August |pmid=15052273 |doi=10.1038/sj.mp.4001506 }}</ref> and catecholaminergic systems.<ref>{{cite journal |author=Zubieta JK, Heitzeg MM, Smith YR, ''et al.'' |title=COMT val158met genotype affects mu-opioid neurotransmitter responses to a pain stressor |journal=Science (journal) |volume=299 |issue=5610 |pages=1240–3 |year=2003 |month=February |pmid=12595695 |doi=10.1126/science.1078546 }}</ref> However, these polymorphisms are not specific for fibromyalgia and are associated with a variety of allied disorders (e.g. chronic fatigue syndrome,<ref>{{cite journal |author=Narita M, Nishigami N, Narita N, ''et al.'' |title=Association between serotonin transporter gene polymorphism and chronic fatigue syndrome |journal=Biochem Biophys Res Commun. |volume=311 |issue=2 |pages=264–6 |year=2003 |month=November |pmid=14592408 |doi=10.1016/j.bbrc.2003.09.207 |url=http://linkinghub.elsevier.com/retrieve/pii/S0006291X03020497}} | |||
| </ref> irritable bowel syndrome<ref>{{cite journal |author=Camilleri M, Atanasova E, Carlson PJ, ''et al.'' |title=Serotonin-transporter polymorphism pharmacogenetics in diarrhea-predominant irritable bowel syndrome |journal=Gastroenterology |volume=123 |issue=2 |pages=425–32 |year=2002 |month=August |pmid=12145795 |doi=10.1053/gast.2002.34780 |url=http://linkinghub.elsevier.com/retrieve/pii/S0016508502001208}}</ref>) and with depression.<ref> Hudson JI, Mangweth B, Pope HG JR, De COL C, Hausmann A, Gutweniger S, Laird NM, Biebl W, Tsuang MT. Family study of affective spectrum disorder. Arch Gene Psychiatry. 2003;60:170–177. doi: 10.1001/archpsyc.60.2.170.</ref> | |||
| Numerous ] conditions are often comorbid with fibromyalgia.<ref name="Fitz2018" /> These include chronic ]s,<ref name="Kleykamp-2021" /> ],<ref name="Kleykamp-2021" /> and ].<ref name="Kleykamp-2021" /> ], ], ], and ] are four ]s that have been linked to pain or fibromyalgia.<ref name=Fitz2018/> | |||
| === Stress === | |||
| <!-- Stress hypothesis is very big in FMS and this section should have better source, there is alot of MEDRS better then two studies w correlation --> | |||
| ] may be an important precipitating factor in the development of fibromyalgia.<ref>{{cite journal |author = Anderberg UM, Marteinsdottir I, Theorell T, von Knorring L |title=The impact of life events in female patients with fibromyalgia and in female healthy controls |journal=Eur Psychiatry |month=August |year=2000 |pages=33–41 |volume=15 |issue=5 |pmid=10954873 |doi=10.1016/S0924-9338(00)00397-7}}</ref> Fibromyalgia is frequently comorbid with stress-related disorders such as ], ], ] and ]<ref name="p18270311"/>. Two studies that employed single-voxel ] (1H-MRS) reported metabolic abnormalities within the hippocampal complex in patients with fibromyalgia, with significant correlations between hippocampal metabolic abnormalities and severity of clinical symptoms.<ref name=p18484688 >{{cite journal |author=Emad Y, Ragab Y, Zeinhom F, El-Khouly G, Abou-Zeid A, Rasker JJ.|title=Hippocampus dysfunction may explain symptoms of fibromyalgia syndrome. A study with single-voxel magnetic resonance spectroscopy. |journal=J Rheumatol. |volume=35 |issue=7 |pages=1371–7 |year=2008|month=July|pmid=18484688}}</ref><ref name=p18771960 >{{cite journal |author=Wood PB, Ledbetter CR, Glabus MF, Broadwell LK, Patterson JC 2nd|title=Hippocampal Metabolite Abnormalities in Fibromyalgia: Correlation With Clinical Features.|journal=J Pain. |doi=10.1016/j.jpain.2008.07.003|pmid=18771960}}</ref> | |||
| Fibromyalgia largely overlaps with several syndromes that may share the same pathogenetic mechanisms.<ref name="Ramírez-Morales-2022" /><ref name=":3">{{Cite journal |last=Goldenberg |first=Don L |date=2024 |title=How to understand the overlap of long COVID, chronic fatigue syndrome/myalgic encephalomyelitis, fibromyalgia and irritable bowel syndromes |url=https://linkinghub.elsevier.com/retrieve/pii/S0049017224000957 |journal=Seminars in Arthritis and Rheumatism |language=en |volume=67 |pages=152455 |doi=10.1016/j.semarthrit.2024.152455|pmid=38761526 }}</ref> These include ]<ref name="Anderson_2020">{{cite journal | vauthors = Anderson G, Maes M | title = Mitochondria and immunity in chronic fatigue syndrome | journal = Progress in Neuro-Psychopharmacology & Biological Psychiatry | volume = 103 | issue = | pages = 109976 | date = December 2020 | pmid = 32470498 | doi = 10.1016/j.pnpbp.2020.109976 | s2cid = 219104988 }}</ref><ref name="Ramírez-Morales-2022">{{cite journal | vauthors = Ramírez-Morales R, Bermúdez-Benítez E, Martínez-Martínez LA, Martínez-Lavín M | title = Clinical overlap between fibromyalgia and myalgic encephalomyelitis. A systematic review and meta-analysis | journal = Autoimmunity Reviews | volume = 21 | issue = 8 | pages = 103129 | date = August 2022 | pmid = 35690247 | doi = 10.1016/j.autrev.2022.103129 | doi-access = free }}</ref> and ].<ref name=":3" /> | |||
| Other authors have proposed that, because exposure to stressful conditions can alter the function of the ], the development of fibromyalgia may stem from stress-induced disruption of the HPA axis.<ref> {{cite journal|author=McBeth J, Chiu YH, Silman AJ, Ray D, Morriss R, Dickens C, Gupta A, Macfarlane GJ.|title=Hypothalamic-pituitary-adrenal stress axis function and the relationship with chronic widespread pain and its antecedents|journal=Arthritis Res Ther. |year=2005| volume=7|issue=5|pages=R992–R1000|pmid=16207340}}</ref> This proposition is supported in part by a prospective epidemiology study which found that variations in HPA function characterized by high levels of circulating ] following ]ing, low levels of morning salivary cortisol and high levels of evening salivary cortisol are all associated with the development of chronic widespread pain.<ref> {{cite journal|author=McBeth J, Silman AJ, Gupta A, Chiu YH, Ray D, Morriss R, Dickens C, King Y, Macfarlane GJ. | title=Moderation of psychosocial risk factors through dysfunction of the hypothalamic-pituitary-adrenal stress axis in the onset of chronic widespread musculoskeletal pain: findings of a population-based prospective cohort study.|journal=Arthritis Rheum. 2007 Jan;56(1):360–71.. |year=2007| volume=56|issue=1|pages=360–71|pmid=17195240 }}</ref> | |||
| ] fibromyalgia has been reported to occur in 20–30% of individuals with ].<ref name="Fitz2018" /> It has been reported in people with noninflammatory ].<ref name="Fitz2018" /> | |||
| ===Central dopamine dysfunction (hypodopaminergia)=== | |||
| The '] hypothesis of fibromyalgia’ proposes that the central abnormality responsible for symptoms associated with fibromyalgia is a disruption of normal dopamine-related neurotransmission. Dopamine is a ] ] with roles in pain perception and natural analgesia. There is also strong evidence for a role of dopamine in ],<ref name=pmid16816393>{{cite journal |author=Cervenka S, Pålhagen SE, Comley RA, ''et al.'' |title=Support for dopaminergic hypoactivity in restless legs syndrome: a PET study on D2-receptor binding |journal=Brain |volume=129 |issue=Pt 8 |pages=2017–28 |year=2006 |month=August |pmid=16816393 |doi=10.1093/brain/awl163 |url=http://brain.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16816393 |accessdate=2008-05-21}}</ref> which is a condition found frequently in patients with fibromyalgia.<ref name=pmid8646049>{{cite journal |author=Yunus MB, Aldag JC |title=Restless legs syndrome and leg cramps in fibromyalgia syndrome: a controlled study |journal=BMJ |volume=312 |issue=7042 |pages=1339 |year=1996 |month=May |pmid=8646049 |doi= |url=http://bmj.com/cgi/pmidlookup?view=long&pmid=8646049 |accessdate=2008-05-21}}</ref> Some fibromyalgia patients responded in controlled trials to ], a ] that selectively stimulates dopamine D2/D3 receptors and is used to treat both Parkinson's disease and restless leg syndrome.<ref name=pmid16052595>{{cite journal |author=Holman AJ, Myers RR |title=A randomized, double-blind, placebo-controlled trial of pramipexole, a dopamine agonist, in patients with fibromyalgia receiving concomitant medications |journal=Arthritis Rheum. |volume=52 |issue=8 |pages=2495–505 |year=2005 |month=August |pmid=16052595 |doi=10.1002/art.21191 |accessdate=2008-05-21}}</ref> | |||
| The prevalence of fibromyalgia in ] has been described mostly for ]<ref name="Fitz2018" /> and ] (IBS).<ref name="Fitz2018" /><ref name="Kleykamp-2021" /> IBS and fibromyalgia share similar pathogenic mechanisms, involving immune system ]s, inflammatory biomarkers, ]s, and ]s such as ]. ] alter serotonin levels, leading to ] hyperstimulation.<ref>{{cite journal | vauthors = Valencia C, Fatima H, Nwankwo I, Anam M, Maharjan S, Amjad Z, Abaza A, Vasavada AM, Sadhu A, Khan S | display-authors = 6 | title = A Correlation Between the Pathogenic Processes of Fibromyalgia and Irritable Bowel Syndrome in the Middle-Aged Population: A Systematic Review | journal = Cureus | volume = 14 | issue = 10 | pages = e29923 | date = October 2022 | pmid = 36381861 | pmc = 9635936 | doi = 10.7759/cureus.29923 | doi-access = free }}</ref> | |||
| ===Abnormal serotonin metabolism=== | |||
| In 1975, researchers hypothesized that ], a ] that regulates sleep patterns, mood, concentration and pain, could be involved in the ] of fibromyalgia-associated symptoms.<ref name=p169541/> In 1992, decreased serotonin metabolites in patient ]<ref>{{cite journal |author=Russell IJ, Michalek JE, Vipraio GA, Fletcher EM, Javors MA, Bowden CA |title=Platelet 3H-imipramine uptake receptor density and serum serotonin levels in patients with fibromyalgia/fibrositis syndrome |journal=J Rheumatol. |volume=19 |issue=1 |pages=104–9 |year=1992 |month=January |pmid=1313504 }}</ref> and ] were reported.<ref name="Russell IJ, Vaeroy H, Javors M, Nyberg F 1992 550–6">{{cite journal |author=Russell IJ, Vaeroy H, Javors M, Nyberg F |title=Cerebrospinal fluid biogenic amine metabolites in fibromyalgia/fibrositis syndrome and rheumatoid arthritis |journal=Arthritis Rheum. |volume=35 |issue=5 |pages=550–6 |year=1992 |month=May |pmid=1374252 |doi=10.1002/art.1780350509 }}</ref> However, ] (SSRIs) have met with limited success in alleviating the symptoms of the disorder, while drugs with activity as mixed ]s (SNRIs) have been more successful.<ref>{{cite journal |author=Arnold LM |title=Biology and therapy of fibromyalgia. New therapies in fibromyalgia |journal=Arthritis Res Ther. |volume=8 |issue=4 |pages=212 |year=2006 |pmid=16762044 |pmc=1779399 |doi=10.1186/ar1971 }}</ref> ] (]), a SNRI originally used to treat depression and painful ], has been demonstrated by controlled trials{{Citation needed|date=July 2009}} to relieve symptoms of some patients. However, the relevance of dysregulated serotonin metabolism to pathophysiology is a matter of debate.<ref>{{cite journal |author=Jaschko G, Hepp U, Berkhoff M, ''et al.'' |title=Serum serotonin levels are not useful in diagnosing fibromyalgia |journal=Ann Rheum Dis. |volume=66 |issue=9 |pages=1267–8 |year=2007 |month=September |pmid=17693607 |doi=10.1136/ard.2006.058842 }}</ref> Complicating the analysis, one of the more effective types of medication for the treatment of the disorder (i.e. serotonin ]s) actually blocks some of the effects of serotonin.<ref>{{cite journal |author=Späth M |title=Current experience with 5-HT3 receptor antagonists in fibromyalgia |journal=Rheum Dis Clin North Am. |volume=28 |issue=2 |pages=319–28 |year=2002 |month=May |pmid=12122920 |doi=10.1016/S0889-857X(01)00014-X }}</ref> | |||
| Fibromyalgia has also been linked with obesity.<ref>{{cite journal | vauthors = D'Onghia M, Ciaffi J, Lisi L, Mancarella L, Ricci S, Stefanelli N, Meliconi R, Ursini F | display-authors = 6 | title = Fibromyalgia and obesity: A comprehensive systematic review and meta-analysis | journal = Seminars in Arthritis and Rheumatism | volume = 51 | issue = 2 | pages = 409–424 | date = April 2021 | pmid = 33676126 | doi = 10.1016/j.semarthrit.2021.02.007 | s2cid = 232136088 }}</ref> Other conditions that are associated with fibromyalgia include ],<ref>{{cite journal | vauthors = Alsiri N, Alhadhoud M, Alkatefi T, Palmer S | title = The concomitant diagnosis of fibromyalgia and connective tissue disorders: A systematic review | journal = Seminars in Arthritis and Rheumatism | volume = 58 | pages = 152127 | date = February 2023 | pmid = 36462303 | doi = 10.1016/j.semarthrit.2022.152127 | s2cid = 253650110 | url = https://orca.cardiff.ac.uk/id/eprint/158035/1/Alsiri%20and%20Palmer%202023%20ACCEPTED.pdf | access-date = 7 January 2024 | archive-date = 7 January 2024 | archive-url = https://web.archive.org/web/20240107080034/https://orca.cardiff.ac.uk/id/eprint/158035/1/Alsiri%20and%20Palmer%202023%20ACCEPTED.pdf | url-status = live }}</ref> cardiovascular autonomic abnormalities,<ref>{{cite journal | vauthors = Kocyigit BF, Akyol A | title = Coexistence of fibromyalgia syndrome and inflammatory rheumatic diseases, and autonomic cardiovascular system involvement in fibromyalgia syndrome | journal = Clinical Rheumatology | volume = 42 | issue = 3 | pages = 645–652 | date = March 2023 | pmid = 36151442 | doi = 10.1007/s10067-022-06385-8 | s2cid = 252496799 }}</ref> ]-hypopnea syndrome,<ref>{{Cite journal |last=He |first=Jie |date=2024 |title=Fibromyalgia in Obstructive Sleep Apnea-hypopnea Syndrome: A Systematic Review and Meta-analysis |journal= Frontiers in Physiology|volume=15|doi=10.3389/fphys.2024.1394865 |doi-access=free |pmid=38831795 |pmc=11144865 }}</ref> ]<ref>{{Cite journal |last1=Padhan |first1=Prasanta |last2=Maikap |first2=Debashis |last3=Pathak |first3=Mona |date=2023 |title=Restless leg syndrome in rheumatic conditions: Its prevalence and risk factors, a meta-analysis |url=https://onlinelibrary.wiley.com/doi/10.1111/1756-185X.14710 |journal=International Journal of Rheumatic Diseases |language=en |volume=26 |issue=6 |pages=1111–1119 |doi=10.1111/1756-185X.14710 |pmid=37137528 |s2cid=258484602 |issn=1756-1841 |access-date=28 July 2023 |archive-date=28 July 2023 |archive-url=https://web.archive.org/web/20230728152815/https://onlinelibrary.wiley.com/doi/10.1111/1756-185X.14710 |url-status=live }}</ref> and an ].<ref>{{cite journal | vauthors = Goldberg N, Tamam S, Weintraub AY | title = The association between overactive bladder and fibromyalgia: A systematic review and meta-analysis | journal = International Journal of Gynaecology and Obstetrics | volume = 159 | issue = 3 | pages = 630–641 | date = December 2022 | pmid = 35641437 | doi = 10.1002/ijgo.14290 | s2cid = 249236213 }}</ref> | |||
| ===Deficient human growth hormone (HGH) secretion=== | |||
| Levels of hormones under the direct or indirect control of human growth hormone (HGH), including ], ], ] and ] may be abnormal in people with fibromyalgia,<ref>{{cite journal |author=Anderberg UM, Liu Z, Berglund L, Nyberg F |pmid=10700334 |title=Elevated plasma levels of neuropeptide Y in female fibromyalgia patients |journal=Eur J Pain |volume=3 |issue=1 |year=1999 |pages=19–30 |doi=10.1016/S1090-3801(99)90185-4}}</ref> but supplementing growth hormone in patients does not have large effects, and a 2007 literature review reported a need for "further study before any solid recommendations can be made."<ref> {{ cite journal |author=Jones KD, Deodhar P, Lorentzen A, Bennett RM, Deodhar AA |title=Growth hormone perturbations in fibromyalgia: a review |journal=Seminars in Arthritis and Rheumatism |year=2007 |volume=36 |issue=6 |pages=357–79 |pmid=17224178 |doi=10.1016/j.semarthrit.2006.09.006 }}</ref> There is disagreement about the role of HGH in fibromyalgia.<ref>{{cite journal |last=Shuer |first=ML |title=Fibromyalgia: symptom constellation and potential therapeutic options |journal=Endocrine |volume=22 |issue=1 |pages=67–76 |pmid=14610300 |doi=10.1385/ENDO:22:1:67 |year=2003}}</ref><ref>{{cite journal |last=Yuen |first=KC |coauthors=Bennett RM, Hryciw CA, Cook MB, Rhoads SA, Cook DM |journal=Growth hormone & IGF research |title=Is further evaluation for growth hormone (GH) deficiency necessary in fibromyalgia patients with low serum insulin-like growth factor (IGF)-I levels? |volume=17 |issue=1 |year=2007 |pages=82–8 |pmid=17289417 |doi=10.1016/j.ghir.2006.12.006 }}</ref><ref>{{cite journal | last = Bennett | first = RM | coauthors = Cook DM, Clark SR, Burckhardt CS, Campbell SM. | pmid = 9228141 | title = Hypothalamic-pituitary-insulin-like growth factor-I axis dysfunction in patients with fibromyalgia | volume = 24 | issue = 7 | pages = 1384–9 | journal =J Rheumatology }}</ref><ref>{{cite journal | last = McCall-Hosenfeld | first = JS | coauthors = Goldenberg DL, Hurwitz S, Adler GK. | title = Growth hormone and insulin-like growth factor-1 concentrations in women with fibromyalgia | journal = Journal of Rheumatology | volume = 30 | issues = 4 | pages = 809–14 | pmid = 12672204 }}</ref> | |||
| == |
==Risk factors== | ||
| The cause of fibromyalgia is unknown.<ref>{{Cite journal |last=Sarzi-Puttini |first=Piercarlo |last2=Atzeni |first2=Fabiola |last3=Mease |first3=Philip J. |date=April 2011 |title=Chronic widespread pain: from peripheral to central evolution |url=https://pubmed.ncbi.nlm.nih.gov/22094190/ |journal=Best Practice & Research. Clinical Rheumatology |volume=25 |issue=2 |pages=133–139 |doi=10.1016/j.berh.2011.04.001 |issn=1532-1770 |pmid=22094190}}</ref><ref>{{Cite journal |last=Schmidt-Wilcke |first=Tobias |last2=Clauw |first2=Daniel J. |date=2011-07-19 |title=Fibromyalgia: from pathophysiology to therapy |url=https://pubmed.ncbi.nlm.nih.gov/21769128/ |journal=Nature Reviews. Rheumatology |volume=7 |issue=9 |pages=518–527 |doi=10.1038/nrrheum.2011.98 |issn=1759-4804 |pmid=21769128}}</ref> However, several risk factors, genetic and environmental, have been identified. | |||
| There is strong evidence that major depression is associated with fibromyalgia, although the nature of the association is controversial. A comprehensive review into the relationship between fibromyalgia and ] (MDD) found substantial similarities in neuroendocrine abnormalities, psychological characteristics, physical symptoms and treatments between fibromyalgia and MDD, but currently available findings do not support the assumption that MDD and fibromyalgia refer to the same underlying construct or can be seen as subsidiaries of one disease concept.<ref name=Pae>{{cite journal |title=The relationship between fibromyalgia and major depressive disorder: a comprehensive review. |journal=Curr Med Res Opin |volume=24 |issue=8 |pages=2359–71 |month=August |year=2008 |pmid=18606054 |author=Pae CU, Luyten P, Marks DM, Han C, Park SH, Patkar AA, Masand PS, Van Houdenhove B |doi=10.1185/03007990802288338}}</ref> Indeed, the sensation of pain has at least two dimensions: a sensory dimension which processes the magnitude of the pain, and an affective-motivational dimension which processes the unpleasantness. Accordingly, a study that employed ] to evaluate brain responses to experimental pain among fibromyalgia patients found that depressive symptoms were associated with the magnitude of clinically-induced pain response specifically in areas of the brain that participate in affective pain processing, but not in areas involved in sensory processing which indicate that the amplification of the sensory dimension of pain in fibromyalgia occurs independently of mood or emotional processes.<ref name=Giesecke>{{cite journal |title=The relationship between depression, clinical pain, and experimental pain in a chronic pain cohort. |journal=Arthritis Rheum. |volume=52 |issue=5 |pages=1577–84 |month=May |year=2005 |pmid=15880832 |author=Giesecke T, Gracely RH, Williams DA, Geisser ME, Petzke FW, Clauw DJ |doi=10.1002/art.21008 }}</ref> | |||
| ===Genetics=== | |||
| An alternative hypothesis regarding the development of fibromyalgia in relationship to psychological conflict proposes that the disorder may be a ] as described by ]'s writing related to "]," in which ] is proposed to be a psychic ] of the mind's ] strategy of distracting painful or dangerous emotions. Education, attitude change, and in some cases, psychotherapy are proposed as treatments.<ref>{{cite book |last=Sarno |first=Dr. John E. et al.|title=The Divided Mind: The Epidemic of Mindbody Disorders |year=2006 |isbn=0-06-085178-3 |pages=21–2, 235–7, 294–8 |publisher=HC |location=New York}}</ref> | |||
| Genetics plays a major role in fibromyalgia and may explain up to 50% of the disease's susceptibility.<ref name="D'Agnelli-2019">{{cite journal | vauthors = D'Agnelli S, Arendt-Nielsen L, Gerra MC, Zatorri K, Boggiani L, Baciarello M, Bignami E | title = Fibromyalgia: Genetics and epigenetics insights may provide the basis for the development of diagnostic biomarkers | journal = Molecular Pain | volume = 15 | pages = 1744806918819944 | date = January 2019 | pmid = 30486733 | pmc = 6322092 | doi = 10.1177/1744806918819944 }}</ref> Fibromyalgia is potentially associated with ] of genes in the ],<ref name="Ablin-2015">{{cite journal | vauthors = Ablin JN, Buskila D | title = Update on the genetics of the fibromyalgia syndrome | journal = Best Practice & Research. Clinical Rheumatology | volume = 29 | issue = 1 | pages = 20–28 | date = February 2015 | pmid = 26266996 | doi = 10.1016/j.berh.2015.04.018 }}</ref> ]<ref name="Ablin-2015" /> and ] systems.<ref name="Ablin-2015" /> Several genes have been suggested as candidates for susceptibility to fibromyalgia. These include ],<ref name="D'Agnelli-2019" /> ],<ref name="D'Agnelli-2019" /> ],<ref name="D'Agnelli-2019" /> ],<ref name="D'Agnelli-2019" /> and the ] 102T/C polymorphism.<ref name="pmid21120487">{{cite journal | vauthors = Lee YH, Choi SJ, Ji JD, Song GG | title = Candidate gene studies of fibromyalgia: a systematic review and meta-analysis | journal = Rheumatology International | volume = 32 | issue = 2 | pages = 417–426 | date = February 2012 | pmid = 21120487 | doi = 10.1007/s00296-010-1678-9 | s2cid = 6239018 }}</ref> The ] of fibromyalgia is estimated to be higher in patients younger than 50.<ref>{{cite journal | vauthors = Dutta D, Brummett CM, Moser SE, Fritsche LG, Tsodikov A, Lee S, Clauw DJ, Scott LJ | display-authors = 6 | title = Heritability of the Fibromyalgia Phenotype Varies by Age | journal = Arthritis & Rheumatology | volume = 72 | issue = 5 | pages = 815–823 | date = May 2020 | pmid = 31736264 | pmc = 8372844 | doi = 10.1002/art.41171 }}</ref> | |||
| Nearly all the genes suggested as potential risk factors for fibromyalgia are associated with neurotransmitters and their receptors.<ref name=":1" /> ] and ] often co-occur with fibromyalgia — the reason for this ] appears to be due to shared ] abnormalities, which leads to impairments in ], ], ], ] and ] signaling. In these vulnerable individuals, ] or illness can cause abnormalities in inflammatory and stress pathways that regulate mood and pain. Eventually, a sensitization and kindling effect occurs in certain ]s leading to the establishment of fibromyalgia and sometimes a ].<ref name="Maletic-2009">{{cite journal | vauthors = Maletic V, Raison CL | title = Neurobiology of depression, fibromyalgia and neuropathic pain | journal = Frontiers in Bioscience | volume = 14 | issue = 14 | pages = 5291–5338 | date = June 2009 | pmid = 19482616 | doi = 10.2741/3598 | doi-access = free }}</ref> | |||
| ===Other hypotheses=== | |||
| Other hypotheses have been proposed. One of these is an aberrant immune response to ].<ref name="AnnRheumDis2004-PimentalM">{{cite journal | author=Pimental M, Wallace D, Hallegua D et al. | title=A link between irritable bowel syndrome and fibromyalgia may be related to findings on lactulose breath testing | journal=J Rheumatol Suppl | month=November | year=1989 | pages=23–7 | volume=19 |pmid=2691680 }}</ref> | |||
| === Stress === | |||
| ] may be an important precipitating factor in the development of fibromyalgia.<ref name="Martins-2021">{{cite journal | vauthors = Martins DF, Viseux FJ, Salm DC, Ribeiro AC, da Silva HK, Seim LA, Bittencourt EB, Bianco G, Moré AO, Reed WR, Mazzardo-Martins L | display-authors = 6 | title = The role of the vagus nerve in fibromyalgia syndrome | journal = Neuroscience and Biobehavioral Reviews | volume = 131 | pages = 1136–1149 | date = December 2021 | pmid = 34710514 | doi = 10.1016/j.neubiorev.2021.10.021 | s2cid = 239772451 }}</ref> A 2021 ] found ] to be strongly associated with fibromyalgia.<ref name="Kaleycheva-2021">{{cite journal | vauthors = Kaleycheva N, Cullen AE, Evans R, Harris T, Nicholson T, Chalder T | title = The role of lifetime stressors in adult fibromyalgia: systematic review and meta-analysis of case-control studies | journal = Psychological Medicine | volume = 51 | issue = 2 | pages = 177–193 | date = January 2021 | pmid = 33602373 | doi = 10.1017/S0033291720004547 | s2cid = 231955641 | doi-access = free }}</ref><ref name="Jung-2021">{{cite journal | vauthors = Jung YH, Kim H, Lee D, Lee JY, Moon JY, Choi SH, Kang DH | title = Dysfunctional energy metabolisms in fibromyalgia compared with healthy subjects | journal = Molecular Pain | volume = 17 | pages = 17448069211012833 | date = January 2021 | pmid = 33940974 | pmc = 8113919 | doi = 10.1177/17448069211012833 }}</ref> People who suffered abuse in their lifetime were three times more likely to have fibromyalgia; people who suffered medical trauma or other stressors in their lifetime were about twice as likely.<ref name="Kaleycheva-2021" /> | |||
| Some authors have proposed that, because exposure to stressful conditions can alter the function of the ], the development of fibromyalgia may stem from stress-induced disruption of the HPA axis.<ref>{{cite journal | vauthors = Schmidt-Wilcke T, Clauw DJ | title = Fibromyalgia: from pathophysiology to therapy | journal = Nature Reviews. Rheumatology | volume = 7 | issue = 9 | pages = 518–527 | date = July 2011 | pmid = 21769128 | doi = 10.1038/nrrheum.2011.98 | s2cid = 20678671 }}</ref><ref>{{cite journal | vauthors = Casale R, Sarzi-Puttini P, Botto R, Alciati A, Batticciotto A, Marotto D, Torta R | title = Fibromyalgia and the concept of resilience | journal = Clinical and Experimental Rheumatology | volume = 37 | issue = 1 | pages = 105–113 | date = January 2019 | pmid = 30747098 | url = https://pubmed.ncbi.nlm.nih.gov/30747098 | access-date = 9 April 2022 | archive-date = 9 April 2022 | archive-url = https://web.archive.org/web/20220409072659/https://pubmed.ncbi.nlm.nih.gov/30747098/ | url-status = live }}</ref> | |||
| === Personality=== | |||
| Studies on personality and fibromyalgia have shown inconsistent results.<ref name=":7" /> Although some have suggested that fibromyalgia patients are more likely to have specific personality traits, it appears that in comparison to other diseases – when anxiety and depression are ] for{{Snd}}personality has far less relevance.<ref name=":7">{{cite journal |vauthors=Conversano C, Marchi L, Rebecca C, Carmassi C, Contena B, Bazzichi LM, Gemignani A |date=2018-09-28 |title=Personality Traits in Fibromyalgia (FM): Does FM Personality Exists? A Systematic Review |journal=Clinical Practice and Epidemiology in Mental Health |volume=14 |issue=1 |pages=223–232 |doi=10.2174/1745017901814010223 |pmc=6166394 |pmid=30294356 |quote=Personality traits are often studied in patients with rheumatic diseases and, most of all, in those with fibromyalgia. However, the literature on this topic presents inconsistent results...Although in many studies FM patients are compared with healthy controls and personality differences are found, when comparison is made with other disorders with controlled depression, personality traits appear to be less relevant than before.}}</ref> | |||
| === Other risk markers === | |||
| Other risk markers for fibromyalgia include ], ], childhood cognitive and psychosocial problems, primary pain disorders, multiregional pain, infectious illness, ], ], and ].<ref name="Tan-2019">{{cite journal | vauthors = Tan AC, Jaaniste T, Champion D | title = Chronic Widespread Pain and Fibromyalgia Syndrome: Life-Course Risk Markers in Young People | journal = Pain Research & Management | volume = 2019 | pages = 6584753 | date = 2019-05-05 | pmid = 31191788 | pmc = 6525804 | doi = 10.1155/2019/6584753 | doi-access = free }}</ref> ] has also been linked with fibromyalgia, especially in response to ] but also inorganic ], ], and ].<ref>{{cite journal | vauthors = Roach K, Roberts J | title = A comprehensive summary of disease variants implicated in metal allergy | journal = Journal of Toxicology and Environmental Health Part B: Critical Reviews | volume = 25 | issue = 6 | pages = 279–341 | date = August 2022 | pmid = 35975293 | doi = 10.1080/10937404.2022.2104981 | pmc = 9968405 | bibcode = 2022JTEHB..25..279R | s2cid = 251623384 }}</ref> Following the ], some have suggested that the ] virus may trigger fibromyalgia.<ref>{{Cite journal |last1=Fialho |first1=Maria Fernanda Pessano |last2=Brum |first2=Evelyne Silva |last3=Oliveira |first3=Sara Marchesan |date=2023 |title=Could the fibromyalgia syndrome be triggered or enhanced by COVID-19? |journal=Inflammopharmacology |language=en |volume=31 |issue=2 |pages=633–651 |doi=10.1007/s10787-023-01160-w |issn=0925-4692 |pmc=9970139 |pmid=36849853}}</ref> | |||
| ==Pathophysiology== | ==Pathophysiology== | ||
| As of 2022, the pathophysiology of fibromyalgia has not yet been elucidated<ref>{{cite journal | vauthors = de Tommaso M, Vecchio E, Nolano M | title = The puzzle of fibromyalgia between central sensitization syndrome and small fiber neuropathy: a narrative review on neurophysiological and morphological evidence | journal = Neurological Sciences | volume = 43 | issue = 3 | pages = 1667–1684 | date = March 2022 | pmid = 35028777 | doi = 10.1007/s10072-021-05806-x | s2cid = 245909381 }}</ref> and several theories have been suggested. The prevailing view is that fibromyalgia is a condition resulting from an amplification of pain by the central nervous system.<ref name=":1">{{Cite journal |last1=Pinto |first1=Ana Margarida |last2=Luís |first2=Mariana |last3=Geenen |first3=Rinie |last4=Palavra |first4=Filipe |last5=Lumley |first5=Mark A. |last6=Ablin |first6=Jacob N. |last7=Amris |first7=Kirstine |last8=Branco |first8=Jaime |last9=Buskila |first9=Dan |last10=Castelhano |first10=João |last11=Castelo-Branco |first11=Miguel |last12=Crofford |first12=Leslie J. |last13=Fitzcharles |first13=Mary-Ann |last14=Häuser |first14=Winfried |last15=Kosek |first15=Eva |date=2023 |title=Neurophysiological and psychosocial mechanisms of fibromyalgia: A comprehensive review and call for an integrative model |url=http://dx.doi.org/10.1016/j.neubiorev.2023.105235 |journal=Neuroscience & Biobehavioral Reviews |volume=151 |pages=105235 |doi=10.1016/j.neubiorev.2023.105235 |pmid=37207842 |hdl=1874/429361 |s2cid=258745974 |issn=0149-7634|hdl-access=free }}</ref> Substantial biological findings have backed up this notion, leading to development and adoption of the concept of ].<ref name=":1" /> | |||
| ===Sleep disturbances=== | |||
| Fibromyalgia is associated with the deregulation of ] related to ] and ] cascades, as well as to ].<ref name=":4">{{Cite journal |last1=Gkouvi |first1=Arriana |last2=Tsiogkas |first2=Sotirios G. |last3=Bogdanos |first3=Dimitrios P. |last4=Gika |first4=Helen |last5=Goulis |first5=Dimitrios G. |last6=Grammatikopoulou |first6=Maria G. |date=2024-04-23 |title=Proteomics in Patients with Fibromyalgia Syndrome: A Systematic Review of Observational Studies |journal=Current Pain and Headache Reports |language=en |doi=10.1007/s11916-024-01244-4 |issn=1531-3433|doi-access=free |pmid=38652420 |pmc=11271354 }}</ref> An excessive ] response may cause dysregulation of many proteins.<ref name=":4" /> | |||
| The first objective findings associated with the disorder were reported in 1975 by Moldofsky and colleagues, who reported the presence of anomalous alpha wave activity (typically associated with arousal states) on sleep ] (EEG) during non-rapid-eye-movement sleep.<ref name=p169541>{{cite journal |author=Moldofsky H, Scarisbrick P, England R, Smythe H |title=Musculosketal symptoms and non-REM sleep disturbance in patients with "fibrositis syndrome" and healthy subjects |journal=Psychosom Med |volume=37 |issue=4 |pages=341–51 |month=Jul-August |year=1975 |pmid=169541 |url=http://www.psychosomaticmedicine.org/cgi/pmidlookup?view=long&pmid=169541 |day=01}}</ref> By disrupting stage IV sleep consistently in young, healthy subjects, the researchers reproduced a significant increase in muscle tenderness similar to that experienced in fibromyalgia but which resolved when the subjects were able to resume their normal sleep patterns.<ref>{{cite journal |author=Moldofsky H, Scarisbrick P |title=Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation |journal=Psychosom Med |volume=38 |issue=1 |pages=35–44 |month=Jan-February |year=1976 |pmid=176677 |url=http://www.psychosomaticmedicine.org/cgi/pmidlookup?view=long&pmid=176677 |day=01}}</ref> In 1995, additional EEG sleep abnormalities were reported in fibromyalgia patients.<ref>{{cite journal |author=Drewes AM, Gade K, Nielsen KD, Bjerregård K, Taagholt SJ, Svendsen L |title=Clustering of sleep electroencephalographic patterns in patients with the fibromyalgia syndrome |journal=Br J Rheumatol. |volume=34 |issue=12 |pages=1151–6 |year=1995 |month=December |pmid=8608357 |url=http://rheumatology.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=8608357 |doi=10.1093/rheumatology/34.12.1151}}</ref> | |||
| === |
=== Nervous system === | ||
| ==== Pain processing abnormalities ==== | |||
| Results from studies examining responses to experimental stimulation have shown that fibromyalgia patients display sensitivity to pressure, heat, cold, electrical and chemical stimulation.<ref>{{cite journal |author=Desmeules JA, Cedraschi C, Rapiti E, ''et al.'' |title=Neurophysiologic evidence for a central sensitization in patients with fibromyalgia |journal=Arthritis Rheum. |volume=48 |issue=5 |pages=1420–9 |year=2003 |month=May |pmid=12746916 |doi=10.1002/art.10893 }}</ref> Experiments examining pain regulatory systems have shown that fibromyalgia patients also display a dysregulation of diffuse noxious inhibitory control,<ref>{{cite journal |author=Kosek E, Hansson P |title=Modulatory influence on somatosensory perception from vibration and heterotopic noxious conditioning stimulation (HNCS) in fibromyalgia patients and healthy subjects |journal=Pain |volume=70 |issue=1 |pages=41–51 |year=1997 |month=March |pmid=9106808 |url=http://linkinghub.elsevier.com/retrieve/pii/S0304395996032952 |doi=10.1016/S0304-3959(96)03295-2}}</ref> an exaggerated wind-up in response to repetitive stimulation,<ref>{{cite journal |author=Staud R, Vierck CJ, Cannon RL, Mauderli AP, Price DD |title=Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome |journal=Pain |volume=91 |issue=1-2 |pages=165–75 |year=2001 |month=March |pmid=11240089 |url=http://linkinghub.elsevier.com/retrieve/pii/S0304-3959(00)00432-2 |doi=10.1016/S0304-3959(00)00432-2}}</ref> and an absence of exercise-induced analgesic response.<ref>{{cite journal |author=Staud R, Robinson ME, Price DD |title=Isometric exercise has opposite effects on central pain mechanisms in fibromyalgia patients compared to normal controls |journal=Pain |volume=118 |issue=1-2 |pages=176–84 |year=2005 |month=November |pmid=16154700 |doi=10.1016/j.pain.2005.08.007 }} | |||
| ] can be divided into three categories. ] is pain caused by ] or damage to tissues. ] is pain caused by ] damage. ] (or central sensitization) is less understood and is the common explanation of the pain experienced in fibromyalgia.<ref name="Central sensitivity and fibromyalgi">{{cite journal | vauthors = Mezhov V, Guymer E, Littlejohn G | title = Central sensitivity and fibromyalgia | journal = Internal Medicine Journal | volume = 51 | issue = 12 | pages = 1990–1998 | date = December 2021 | pmid = 34139045 | doi = 10.1111/imj.15430 | s2cid = 235471910 | doi-access = free }}</ref><ref name=Fitz2021/><ref>{{cite journal | vauthors = den Boer C, Dries L, Terluin B, van der Wouden JC, Blankenstein AH, van Wilgen CP, Lucassen P, van der Horst HE | display-authors = 6 | title = Central sensitization in chronic pain and medically unexplained symptom research: A systematic review of definitions, operationalizations and measurement instruments | journal = Journal of Psychosomatic Research | volume = 117 | pages = 32–40 | date = February 2019 | pmid = 30665594 | doi = 10.1016/j.jpsychores.2018.12.010 | s2cid = 58565532 }}</ref> Because the three forms of pain can overlap, fibromyalgia patients may experience ] (e.g., ] illnesses) and ] (e.g., ]) pain, in addition to nociplastic pain.<ref name=Fitz2021/> | |||
| </ref> Together these results point to dysregulation of the nociceptive system at the central level. | |||
| ==== Nociplastic pain (central sensitization) ==== | |||
| ===Neuroendocrine disruption=== | |||
| {{Main|Nociplastic pain}} | |||
| Fibromyalgia can be viewed as a condition of nociplastic pain.<ref>{{cite journal | vauthors = Bidari A, Ghavidel-Parsa B | title = Nociplastic pain concept, a mechanistic basis for pragmatic approach to fibromyalgia | journal = Clinical Rheumatology | volume = 41 | issue = 10 | pages = 2939–2947 | date = October 2022 | pmid = 35701625 | doi = 10.1007/s10067-022-06229-5 | s2cid = 249650477 }}</ref> Nociplastic pain is caused by an altered function of pain-related sensory pathways in the ] and the ], resulting in hypersensitivity.<ref>{{cite journal | vauthors = Nijs J, Lahousse A, Kapreli E, Bilika P, Saraçoğlu İ, Malfliet A, Coppieters I, De Baets L, Leysen L, Roose E, Clark J, Voogt L, Huysmans E | display-authors = 6 | title = Nociplastic Pain Criteria or Recognition of Central Sensitization? Pain Phenotyping in the Past, Present and Future | journal = Journal of Clinical Medicine | volume = 10 | issue = 15 | pages = 3203 | date = July 2021 | pmid = 34361986 | pmc = 8347369 | doi = 10.3390/jcm10153203 | doi-access = free }}</ref> | |||
| Nociplastic pain is commonly referred to as "Nociplastic pain syndrome" because it is coupled with other symptoms.<ref name=Fitz2021/> These include ], ], ], ] to environmental stimuli, anxiety, and depression.<ref name=Fitz2021/> Nociplastic pain is caused by either (1) increased processing of ] or (2) decreased suppression of pain stimuli at several levels in the ], or both.<ref name=Fitz2021/> | |||
| Patients with fibromyalgia have been demonstrated to have a disruption of normal neuroendocrine function, characterized by mild hypocortisolemia,<ref>{{cite journal |author=Gur A, Cevik R, Sarac AJ, Colpan L, Em S |title=Hypothalamic-pituitary-gonadal axis and cortisol in young women with primary fibromyalgia: the potential roles of depression, fatigue, and sleep disturbance in the occurrence of hypocortisolism |journal=Ann. Rheum. Dis. |volume=63 |issue=11 |pages=1504–6 |year=2004 |month=November |pmid=15479904 |pmc=1754816 |doi=10.1136/ard.2003.014969 }} | |||
| </ref> hyperreactivity of pituitary adrenocorticotropin hormone release in response to challenge, and glucocorticoid feedback resistance.<ref>{{cite journal |author=Griep EN, Boersma JW, Lentjes EG, Prins AP, van der Korst JK, de Kloet ER |title=Function of the hypothalamic-pituitary-adrenal axis in patients with fibromyalgia and low back pain |journal=J. Rheumatol. |volume=25 |issue=7 |pages=1374–81 |year=1998 |month=July |pmid=9676772 }}</ref> A progressive reduction of serum growth hormone levels has also been documented—at baseline in a minority of patients, while most demonstrate reduced secretion in response to exercise or pharmacological challenge.<ref>{{cite journal |author=Bennett RM |title=Adult growth hormone deficiency in patients with fibromyalgia |journal=Curr Rheumatol Rep |volume=4 |issue=4 |pages=306–12 |year=2002 |month=August |pmid=12126582 |doi=10.1007/s11926-002-0039-4 }} | |||
| </ref> Other abnormalities include reduced responsivity of thyrotropin and thyroid hormones to thyroid-releasing hormone,<ref>{{cite journal |author=Neeck G, Riedel W |title=Thyroid function in patients with fibromyalgia syndrome |journal=J. Rheumatol. |volume=19 |issue=7 |pages=1120–2 |year=1992 |month=July |pmid=1512769 }} | |||
| </ref> a mild elevation of prolactin levels with disinhibition of prolactin release in response to challenge<ref> {{cite journal |author=Riedel W, Layka H, Neeck G |title=Secretory pattern of GH, TSH, thyroid hormones, ACTH, cortisol, FSH, and LH in patients with fibromyalgia syndrome following systemic injection of the relevant hypothalamic-releasing hormones |journal=Z Rheumatol |volume=57 Suppl 2 |issue= |pages=81–7 |year=1998 |pmid=10025090 |url=http://link.springer.de/link/service/journals/00393/bibs/857%20Suppl%202000/857%20Suppl%2020081.htm |doi=10.1007/s003930050242}}</ref> and hyposecretion of adrenal androgens.<ref>{{cite journal |author=Dessein PH, Shipton EA, Joffe BI, Hadebe DP, Stanwix AE, Van der Merwe BA |title=Hyposecretion of adrenal androgens and the relation of serum adrenal steroids, serotonin and insulin-like growth factor-1 to clinical features in women with fibromyalgia |journal=Pain |volume=83 |issue=2 |pages=313–9 |year=1999 |month=November |pmid=10534604 |url=http://linkinghub.elsevier.com/retrieve/pii/S030439599900113X |doi=10.1016/S0304-3959(99)00113-X}} | |||
| </ref> These changes might be attributed to the effects of chronic stress, which, after being perceived and processed by the central nervous system, activates hypothalamic corticotrophin-releasing hormone neurons. Thus, the multiple neuroendocrine changes evident in fibromyalgia have been proposed to stem from chronic overactivity of corticotropin-releasing hormone releasing neurons, resulting in a disruption of normal function of the pituitary-adrenal axis and an increased stimulation of hypothalamic somatostatin secretion, which, in turn, inhibits the secretion of a multiplicity of other hormones.<ref>{{cite journal |author=Neeck G, Crofford LJ |title=Neuroendocrine perturbations in fibromyalgia and chronic fatigue syndrome |journal=Rheum. Dis. Clin. North Am. |volume=26 |issue=4 |pages=989–1002 |year=2000 |month=November |pmid=11084955 |doi=10.1016/S0889-857X(05)70180-0 }}</ref> | |||
| ==== Neuropathic pain ==== | |||
| ===Sympathetic hyperactivity=== | |||
| An alternative hypothesis to ] views fibromyalgia as a ]-related ] with neuropathic pain features.<ref name=Martinez2018>{{cite journal | vauthors = Martínez-Lavín M | title = Fibromyalgia and small fiber neuropathy: the plot thickens! | journal = Clinical Rheumatology | volume = 37 | issue = 12 | pages = 3167–3171 | date = December 2018 | pmid = 30238382 | doi = 10.1007/s10067-018-4300-2 | s2cid = 52306843 }}</ref> This view highlights the role of ] and ] ] nervous systems in the generation of widespread pain, ], and ].<ref>{{cite journal | vauthors = Martínez-Lavín M | title = Dorsal root ganglia: fibromyalgia pain factory? | journal = Clinical Rheumatology | volume = 40 | issue = 2 | pages = 783–787 | date = February 2021 | pmid = 33409721 | pmc = 7787228 | doi = 10.1007/s10067-020-05528-z }}</ref> The description of ] in a subgroup of fibromyalgia patients supports the disease ]-] underpinning.<ref name=Martinez2018/> However, others claim that ] occurs only in small groups of those with fibromyalgia.<ref name=Hauser2018>{{cite journal | vauthors = Häuser W, Fitzcharles MA | title = Facts and myths pertaining to fibromyalgia | journal = Dialogues in Clinical Neuroscience | volume = 20 | issue = 1 | pages = 53–62 | date = March 2018 | pmid = 29946212 | pmc = 6016048 | doi = 10.31887/dcns.2018.20.1/whauser }}</ref> | |||
| ==== Autonomic nervous system ==== | |||
| Functional analysis of the autonomic system in patients with fibromyalgia has demonstrated disturbed activity characterized by hyperactivity of the sympathetic nervous system at baseline<ref> Martinez-Lavin M. Biology and therapy of fibromyalgia. Stress, the stress response system, and fibromyalgia. Arthritis Res Ther. 2007;9(4):216.</ref> with reduced sympathoadrenal reactivity in response to a variety of stressors including physical exertion and mental stress.<ref>{{cite journal |author=Giske L, Vøllestad NK, Mengshoel AM, Jensen J, Knardahl S, Røe C |title=Attenuated adrenergic responses to exercise in women with fibromyalgia--a controlled study |journal=Eur J Pain |volume=12 |issue=3 |pages=351–60 |year=2008 |month=April |pmid=17827042 |doi=10.1016/j.ejpain.2007.07.007 }} | |||
| Some suggest that fibromyalgia is caused or maintained by a decreased vagal tone, which is indicated by low levels of heart rate variability,<ref name="Martins-2021" /> signaling a heightened ] response.<ref name="Martinez-Lavin-2021">{{cite journal | vauthors = Martinez-Lavin M, Holman AJ | title = Heart rate variability analysis in rheumatology: past, present… and future? | journal = Clinical and Experimental Rheumatology | volume = 39 | issue = 5 | pages = 927–930 | date = 2021 | pmid = 34464245 | doi = 10.55563/clinexprheumatol/nmvth1 | s2cid = 237375381 | doi-access = free }}</ref> Accordingly, several studies show that clinical improvement is associated with an increase in heart rate variability.<ref>{{cite journal | vauthors = Figueroa A, Kingsley JD, McMillan V, Panton LB | title = Resistance exercise training improves heart rate variability in women with fibromyalgia | journal = Clinical Physiology and Functional Imaging | volume = 28 | issue = 1 | pages = 49–54 | date = January 2008 | pmid = 18005081 | doi = 10.1111/j.1475-097X.2007.00776.x | s2cid = 40592827 | doi-access = free }}</ref><ref name="Martinez-Lavin-2021" /><ref>{{cite journal | vauthors = Park HY, Jung WS, Kim J, Hwang H, Lim K | title = Twelve Weeks of Aerobic Exercise at the Lactate Threshold Improves Autonomic Nervous System Function, Body Composition, and Aerobic Performance in Women with Obesity | journal = Journal of Obesity & Metabolic Syndrome | volume = 29 | issue = 1 | pages = 67–75 | date = March 2020 | pmid = 32045515 | pmc = 7118007 | doi = 10.7570/jomes19063 }}</ref> Some examples of interventions that increase the heart rate variability and vagal tone are meditation, yoga, mindfulness, and exercise.<ref name="Martins-2021" /> In 2023 the Fibromyalgia: Imbalance of Threat and Soothing Systems (FITSS) model was suggested as a working hypothesis.<ref name="Pinto-2023">{{cite journal | vauthors = Pinto AM, Geenen R, Wager TD, Lumley MA, Häuser W, Kosek E, Ablin JN, Amris K, Branco J, Buskila D, Castelhano J, Castelo-Branco M, Crofford LJ, Fitzcharles MA, López-Solà M, Luís M, Marques TR, Mease PJ, Palavra F, Rhudy JL, Uddin LQ, Castilho P, Jacobs JW, da Silva JA | display-authors = 6 | title = Emotion regulation and the salience network: a hypothetical integrative model of fibromyalgia | journal = Nature Reviews. Rheumatology | volume = 19 | issue = 1 | pages = 44–60 | date = January 2023 | pmid = 36471023 | doi = 10.1038/s41584-022-00873-6 | hdl = 1874/426650 | s2cid = 254273384 | hdl-access = free }}</ref> According to the FITSS model, the ] (also known as the midcingulo-insular network) may remain continuously hyperactive due to an imbalance in ], which is reflected by an overactive "threat" system and an underactive "soothing" system. This hyperactivation, along with other mechanisms, may contribute to fibromyalgia.<ref name="Pinto-2023" /> | |||
| </ref><ref> Nilsen KB, Sand T, Westgaard RH, Stovner LJ, White LR, Bang Leistad R, Helde G, Rø M. Autonomic activation and pain in response to low-grade mental stress in fibromyalgia and shoulder/neck pain patients. Eur J Pain. 2007 Oct;11(7):743-55. </ref> Fibromyalgia patients demonstrate lower heart rate variability, an index of sympathetic/parasympathetic balance, indicating sustained sympathetic hyperactivity, especially at night.<ref> {{cite journal |author=Martínez-Lavín M, Hermosillo AG, Mendoza C, ''et al.'' |title=Orthostatic sympathetic derangement in subjects with fibromyalgia |journal=J. Rheumatol. |volume=24 |issue=4 |pages=714–8 |year=1997 |month=April |pmid=9101507 }} | |||
| </ref> In addition, plasma levels of neuropeptide Y, which is co-localized with norepinephrine in the sympathetic nervous system, have been reported as low in patients with fibromyalgia,<ref>{{cite journal |author=Anderberg UM, Liu Z, Berglund L, Nyberg F |title=Elevated plasma levels of neuropeptide Y in female fibromyalgia patients |journal=Eur J Pain |volume=3 |issue=1 |pages=19–30 |year=1999 |month=March |pmid=10700334 |doi=10.1016/S1090-3801(99)90185-4 }}</ref> while circulating levels of epinephrine and norepinephrine have been variously reported as low, normal and high.<ref>{{cite journal |author=van Denderen JC, Boersma JW, Zeinstra P, Hollander AP, van Neerbos BR |title=Physiological effects of exhaustive physical exercise in primary fibromyalgia syndrome (PFS): is PFS a disorder of neuroendocrine reactivity? |journal=Scand. J. Rheumatol. |volume=21 |issue=1 |pages=35–7 |year=1992 |pmid=1570485 |doi=10.3109/03009749209095060 }}</ref><ref>{{cite journal |author=Adler GK, Kinsley BT, Hurwitz S, Mossey CJ, Goldenberg DL |title=Reduced hypothalamic-pituitary and sympathoadrenal responses to hypoglycemia in women with fibromyalgia syndrome |journal=Am J Med. |volume=106 |issue=5 |pages=534–43 |year=1999 |month=May |pmid=10335725 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002934399000741 |doi=10.1016/S0002-9343(99)00074-1}}</ref> Administration of interleukin-6, a cytokine capable of stimulating the release of hypothalamic corticotropin-releasing hormone which in turn stimulates activity within the sympathetic nervous system, results in a dramatic increase in circulating norepinephrine levels and a significantly greater increase in heart rate over baseline in fibromyalgia patients as compared to healthy controls.<ref>{{cite journal |author=Torpy DJ, Papanicolaou DA, Lotsikas AJ, Wilder RL, Chrousos GP, Pillemer SR |title=Responses of the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis to interleukin-6: a pilot study in fibromyalgia |journal=Arthritis Rheum. |volume=43 |issue=4 |pages=872–80 |year=2000 |month=April |pmid=10765933 |doi=10.1002/1529-0131(200004)43:4<872::AID-ANR19>3.0.CO;2-T }}</ref> | |||
| ==== Neurotransmitters ==== | |||
| ===Cerebrospinal fluid abnormalities=== | |||
| Some neurochemical abnormalities that occur in fibromyalgia also regulate mood, ], and energy, thus explaining why mood, sleep, and ] problems are commonly ] with fibromyalgia.<ref name="Clauw-2011" /> Serotonin is the most widely studied neurotransmitter in fibromyalgia. It is hypothesized that an imbalance in the serotoninergic system may lead to the development of fibromyalgia.<ref name="Singh-2019">{{cite journal | vauthors = Singh L, Kaur A, Bhatti MS, Bhatti R | title = Possible Molecular Mediators Involved and Mechanistic Insight into Fibromyalgia and Associated Co-morbidities | journal = Neurochemical Research | volume = 44 | issue = 7 | pages = 1517–1532 | date = July 2019 | pmid = 31004261 | doi = 10.1007/s11064-019-02805-5 | s2cid = 123945497 }}</ref> There is also some data that suggests altered dopaminergic and noradrenergic signaling in fibromyalgia.<ref name="bellato">{{cite journal | vauthors = Bellato E, Marini E, Castoldi F, Barbasetti N, Mattei L, Bonasia DE, Blonna D | title = Fibromyalgia syndrome: etiology, pathogenesis, diagnosis, and treatment | journal = Pain Research and Treatment | volume = 2012 | pages = 426130 | date = 1 January 2012 | pmid = 23213512 | pmc = 3503476 | doi = 10.1155/2012/426130 | doi-access = free }}</ref> Supporting the monoamine related theories is the efficacy of monoaminergic ]s in fibromyalgia.<ref name="Mascarenhas-2021" /> Glutamate/creatine ratios within the bilateral ventrolateral prefrontal cortex were found to be significantly higher in fibromyalgia patients than in controls and may disrupt glutamate neurotransmission.<ref name="Jung-2021" /><ref name="Feraco-2011">{{cite journal | vauthors = Feraco P, Bacci A, Pedrabissi F, Passamonti L, Zampogna G, Pedrabissi F, Malavolta N, Leonardi M | display-authors = 6 | title = Metabolic abnormalities in pain-processing regions of patients with fibromyalgia: a 3T MR spectroscopy study | journal = AJNR. American Journal of Neuroradiology | volume = 32 | issue = 9 | pages = 1585–1590 | date = October 2011 | pmid = 21799042 | pmc = 7965402 | doi = 10.3174/ajnr.A2550 }}</ref> | |||
| ==== Neurophysiology ==== | |||
| The most reproduced laboratory finding in patients with fibromyalgia is an elevation in cerebrospinal fluid levels of substance P, a putative nociceptive neurotransmitter.<ref>{{cite journal |author=Russell IJ, Orr MD, Littman B, ''et al.'' |title=Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome |journal=Arthritis Rheum. |volume=37 |issue=11 |pages=1593–601 |year=1994 |month=November |pmid=7526868 |doi=10.1002/art.1780371106 }}</ref><ref> {{cite journal |author=Vaerøy H, Helle R, Førre O, Kåss E, Terenius L |title=Elevated CSF levels of substance P and high incidence of Raynaud phenomenon in patients with fibromyalgia: new features for diagnosis |journal=Pain |volume=32 |issue=1 |pages=21–6 |year=1988 |month=January |pmid=2448729 |url=http://linkinghub.elsevier.com/retrieve/pii/0304-3959(88)90019-X |doi=10.1016/0304-3959(88)90019-X}}</ref><ref>{{cite journal |author=Evengard B, Nilsson CG, Lindh G, ''et al.'' |title=Chronic fatigue syndrome differs from fibromyalgia. No evidence for elevated substance P levels in cerebrospinal fluid of patients with chronic fatigue syndrome |journal=Pain |volume=78 |issue=2 |pages=153–5 |year=1998 |month=November |pmid=9839828 |url=http://linkinghub.elsevier.com/retrieve/pii/S0304-3959(98)00134-1 |doi=10.1016/S0304-3959(98)00134-1}} | |||
| Neuroimaging studies have observed that fibromyalgia patients have increased ] in the right ] and left ], and decreased grey matter in the right ], right paracingulate gyrus, left ], and left ].<ref name=":0">{{Cite journal |last1=Xin |first1=Ming |last2=Qu |first2=Yuzhu |last3=Peng |first3=Xingfu |last4=Zhu |first4=Deliang |last5=Cheng |first5=Shirui |date=2023-05-09 |title=A systematic review and meta-analysis of voxel-based morphometric studies of fibromyalgia |journal=Frontiers in Neuroscience |volume=17 |doi=10.3389/fnins.2023.1164145 |issn=1662-453X |pmc=10203234 |pmid=37229427 |doi-access=free }}</ref> These regions are associated with affective and cognitive functions and with motor adaptations to pain processing.<ref name=":0" /> Other studies have documented decreased grey matter of the ] in people with fibromyalgia.<ref name="Lin-2016">{{cite journal | vauthors = Lin C, Lee SH, Weng HH | title = Gray Matter Atrophy within the Default Mode Network of Fibromyalgia: A Meta-Analysis of Voxel-Based Morphometry Studies | journal = BioMed Research International | volume = 2016 | pages = 7296125 | date = 1 January 2016 | pmid = 28105430 | pmc = 5220433 | doi = 10.1155/2016/7296125 | doi-access = free }}</ref> These deficits are associated with pain processing.<ref name="Lin-2016" /> | |||
| </ref> Metabolites for the monoamine neurotransmitters serotonin, norepinephrine, and dopamine—all of which play a role in natural analgesia—have been shown to be lower,<ref name="Russell IJ, Vaeroy H, Javors M, Nyberg F 1992 550–6"/> while concentrations of endogenous opioids (i.e., endorphins and enkephalins) appear to be higher.<ref> {{cite journal |author=Vaerøy H, Nyberg F, Terenius L |title=No evidence for endorphin deficiency in fibromyalgia following investigation of cerebrospinal fluid (CSF) dynorphin A and Met-enkephalin-Arg6-Phe7 |journal=Pain |volume=46 |issue=2 |pages=139–43 |year=1991 |month=August |pmid=1684241 |url=http://linkinghub.elsevier.com/retrieve/pii/0304-3959(91)90068-9 |doi=10.1016/0304-3959(91)90068-9}}</ref> The mean concentration of nerve growth factor, a substance known to participate in structural and functional plasticity of nociceptive pathways within the dorsal root ganglia and spinal cord, is elevated.<ref>{{cite journal |author=Giovengo SL, Russell IJ, Larson AA |title=Increased concentrations of nerve growth factor in cerebrospinal fluid of patients with fibromyalgia |journal=J Rheumatol. |volume=26 |issue=7 |pages=1564–9 |year=1999 |month=July |pmid=10405946 }}</ref> There is also evidence for increased excitatory amino acid release within cerebrospinal fluid, with a correlation demonstrated between levels for metabolites of glutamate and nitric oxide and clinical indices of pain.<ref>{{cite journal |author=Larson AA, Giovengo SL, Russell IJ, Michalek JE |title=Changes in the concentrations of amino acids in the cerebrospinal fluid that correlate with pain in patients with fibromyalgia: implications for nitric oxide pathways |journal=Pain |volume=87 |issue=2 |pages=201–11 |year=2000 |month=August |pmid=10924813 |url=http://linkinghub.elsevier.com/retrieve/pii/S0304-3959(00)00284-0 |doi=10.1016/S0304-3959(00)00284-0}}</ref> | |||
| === |
==== Neuroendocrine system ==== | ||
| Studies on the neuroendocrine system and ] in fibromyalgia have been inconsistent. The depressed function of the HPA axis results in ] and potentially chronic fatigue.<ref name="pmid362464011">{{cite journal | vauthors= Assavarittirong C, Samborski W, Grygiel-Górniak B | title=Oxidative Stress in Fibromyalgia: From Pathology to Treatment| journal=] | volume=2022 | pages=1582432 | year=2022 | doi = 10.1155/2022/1582432 | pmc=9556195 | pmid=36246401| doi-access=free}}</ref> | |||
| One study found fibromyalgia patients exhibited higher plasma ], more extreme peaks and troughs, and higher rates of ] non-suppression. However, other studies have only found correlations between a higher ] and pain, and not any other abnormalities in cortisol.<ref name="bradley" /> Increased baseline ] and increase in response to ] have been observed, and hypothesized to be a result of decreased negative feedback.<ref name="bellato" /> | |||
| Evidence of abnormal brain involvement in fibromyalgia has been provided via functional neuroimaging. The first findings reported were decreased blood flow within the ] and elements of the ] and mid-brain (i.e., ]).<ref>{{cite journal |author=Mountz JM, Bradley LA, Modell JG, ''et al.'' |title=Fibromyalgia in women. Abnormalities of regional cerebral blood flow in the thalamus and the caudate nucleus are associated with low pain threshold levels |journal=Arthritis Rheum. |volume=38 |issue=7 |pages=926–38 |year=1995 |month=July |pmid=7612042 |doi=10.1002/art.1780380708 }}</ref><ref>{{cite journal |author=Kwiatek R, Barnden L, Tedman R, ''et al.'' |title=Regional cerebral blood flow in fibromyalgia: single-photon-emission computed tomography evidence of reduction in the pontine tegmentum and thalami |journal=Arthritis Rheum. |volume=43 |issue=12 |pages=2823–33 |year=2000 |month=December |pmid=11145042 |doi=10.1002/1529-0131(200012)43:12<2823::AID-ANR24>3.0.CO;2-E }}</ref> Differential activation in response to painful stimulation has also been demonstrated.<ref name=p12115241>{{cite journal |author=Gracely RH, Petzke F, Wolf JM, Clauw DJ |title=Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia |journal=Arthritis Rheum. |volume=46 |issue=5 |pages=1333–43 |year=2002 |month=May |pmid=12115241 |doi=10.1002/art.10225 }}</ref><ref name=p14760810 >{{cite journal |author=Cook DB, Lange G, Ciccone DS, Liu WC, Steffener J, Natelson BH |title=Functional imaging of pain in patients with primary fibromyalgia |journal=J Rheumatol. |volume=31 |issue=2 |pages=364–78 |year=2004 |month=February |pmid=14760810 |url=http://www.jrheum.com/subscribers/04/02/364.html |doi=10.1093/rheumatology/31.6.364}}</ref> Brain centers showing hyperactivation in response to noxious stimulation include such pain-related brain centers as the primary and secondary somatosensory cortex, anterior cingulate cortex and insular cortex, while relative hypoactivation at subjectively equal pain levels appears to occur within the thalamus and basal ganglia. Patients also exhibit neural activation in brain regions associated with pain perception in response to nonpainful stimuli in such areas as the prefrontal, supplemental motor, insular, and cingulate cortices. Evidence of hippocampal disruption indicated by reduced brain metabolite ratios has been demonstrated by studies using single-voxel ] (1H-MRS).<ref name=p18484688>{{cite journal |author=Emad Y, Ragab Y, Zeinhom F, El-Khouly G, Abou-Zeid A, Rasker JJ |title=Hippocampus dysfunction may explain symptoms of fibromyalgia syndrome. A study with single-voxel magnetic resonance spectroscopy |journal=J Rheumatol. |volume=35 |issue=7 |pages=1371–7 |year=2008 |month=July |pmid=18484688 |url=http://www.jrheum.com/subscribers/08/07/1371.html}}</ref><ref name=p18771960 /> A significant negative correlation was demonstrated between abnormal metabolite ratios and a validated index of the clinical severity (i.e. the Fibromyalgia Impact Questionnaire).<ref name=p1865419 >{{cite journal |author=Burckhardt CS, Clark SR, Bennett RM.|title=The fibromyalgia impact questionnaire: development and validation. |journal=J Rheumatol. |volume=18 |issue=5 |pages=728–33 |year=1991 |month=May |pmid=1865419}}</ref> Correlations between clinical pain severity and concentrations of the excitatory amino acid neurotransmitter ] within the insular cortex have also been demonstrated using 1H-MRS.<ref name=p18311814 >{{cite journal |author=Harris RE, Sundgren PC, Pang Y, Hsu M, Petrou M, Kim SH, McLean SA, Gracely RH, Clauw DJ.|title=Dynamic levels of glutamate within the insula are associated with improvements in multiple pain domains in fibromyalgia. |journal=Arthritis Rheum.|volume=58|issue=3 |pages=903–7 |year=2008|month=March|pmid=18311814 }}</ref> An acceleration of normal age-related brain atrophy has been demonstrated using ] (VBM) with areas of reduced gray matter located in the cingulate cortex, insula and parahippocampal gyrus.<ref>{{cite journal |author=Kuchinad A, Schweinhardt P, Seminowicz DA, Wood PB, Chizh BA, Bushnell MC |title=Accelerated brain gray matter loss in fibromyalgia patients: premature aging of the brain? |journal=J Neurosci. |volume=27 |issue=15 |pages=4004–7 |year=2007 |month=April |pmid=17428976 |doi=10.1523/JNEUROSCI.0098-07.2007 }}</ref> Studies utilizing ] have demonstrated reduced dopamine synthesis in the brainstem and elements of the limbic cortex.<ref name=p17023218 >{{cite journal |author=Wood PB, Patterson JC, Sunderland JJ, Tainter KH, Glabus MF, Lilien DL |title=Reduced presynaptic dopamine activity in fibromyalgia syndrome demonstrated with positron emission tomography: a pilot study |journal=J Pain |volume=8 |issue=1 |pages=51–8 |year=2007 |month=January |pmid=17023218 |doi=10.1016/j.jpain.2006.05.014 }}</ref> A significant negative correlation between pain severity and dopamine synthesis was demonstrated within the insular cortex. A subsequent study demonstrated gross disruption of dopaminergic reactivity in response to a tonic pain stimulus within the ] with a significant positive correlation between the defining feature of the disorder (i.e. tender point index) and dopamine D2 receptor binding potential specifically in the right ].<ref name=p17610577>{{cite journal |author=Wood PB, Schweinhardt P, Jaeger E, ''et al.'' |title=Fibromyalgia patients show an abnormal dopamine response to pain |journal=Eur J Neurosci. |volume=25 |issue=12 |pages=3576–82 |year=2007 |month=June |pmid=17610577 |doi=10.1111/j.1460-9568.2007.05623.x }}</ref> Finally, reduced availability of mu-opioid receptors in the ]/] and cingulate cortex has been demonstrated, with a significant negative correlation between affective pain levels and receptor availability in the nucleus accumbens.<ref name=p17855614>{{cite journal |author=Harris RE, Clauw DJ, Scott DJ, McLean SA, Gracely RH, Zubieta JK |title=Decreased central mu-opioid receptor availability in fibromyalgia |journal=J Neurosci. |volume=27 |issue=37 |pages=10000–6 |year=2007 |month=September |pmid=17855614 |doi=10.1523/JNEUROSCI.2849-07.2007 }}</ref> | |||
| ==== Oxidative stress ==== | |||
| ==Diagnosis== | |||
| Pro-oxidative processes correlate with pain in fibromyalgia patients.<ref name="pmid362464011"/> Decreased ], increased ] activity, and increased ] production are observed.<ref name="pmid362464011"/> The high proportion of lipids in the central nervous system (CNS) makes the CNS especially vulnerable to ] damage. Levels of lipid peroxidation products correlate with fibromyalgia symptoms.<ref name="pmid362464011"/> | |||
| ] criteria for fibromyalgia.]] | |||
| There is still debate over what should be considered essential diagnostic criteria. The difficulty with diagnosing fibromyalgia is that, in most cases, laboratory testing appears normal and that many of the symptoms mimic those of other rheumatic conditions such as arthritis or osteoporosis. In general, most doctors diagnose patients with a process called differential diagnosis, which means that doctors consider all of the possible things that might be wrong with the patient based on the patient's symptoms, gender, age, geographic location, medical history and other factors. They then narrow down the diagnosis to the most likely one. The most widely accepted set of classification criteria for research purposes was elaborated in 1990 by the Multicenter Criteria Committee of the . These criteria, which are known informally as "the ACR 1990," define fibromyalgia according to the presence of the following criteria: | |||
| === Immune system === | |||
| *A history of widespread pain lasting more than three months—affecting all four quadrants of the body, i.e., both sides, and above and below the waist. | |||
| ] has been suggested to have a role in the pathogenesis of fibromyalgia.<ref>{{cite journal | vauthors = Coskun Benlidayi I | title = Role of inflammation in the pathogenesis and treatment of fibromyalgia | journal = Rheumatology International | volume = 39 | issue = 5 | pages = 781–791 | date = May 2019 | pmid = 30756137 | doi = 10.1007/s00296-019-04251-6 | s2cid = 131775636 }}</ref> People with fibromyalgia tend to have higher levels of inflammatory ]s ],<ref name="Singh-2019" /><ref name="Uçeyler-2011" /><ref name="cytokines" /> and ].<ref name="Singh-2019" /><ref name="Uçeyler-2011">{{cite journal | vauthors = Uçeyler N, Häuser W, Sommer C | title = Systematic review with meta-analysis: cytokines in fibromyalgia syndrome | journal = BMC Musculoskeletal Disorders | volume = 12 | pages = 245 | date = October 2011 | pmid = 22034969 | pmc = 3234198 | doi = 10.1186/1471-2474-12-245 | doi-access = free }}</ref><ref name="cytokines">{{cite journal | vauthors = Rodriguez-Pintó I, Agmon-Levin N, Howard A, Shoenfeld Y | title = Fibromyalgia and cytokines | journal = Immunology Letters | volume = 161 | issue = 2 | pages = 200–203 | date = October 2014 | pmid = 24462815 | doi = 10.1016/j.imlet.2014.01.009 }}</ref> There are also increased levels of the pro-inflammatory cytokines ].<ref name="Uçeyler-2011" /><ref name="cytokines" /> Increased levels of pro-inflammatory cytokines may increase sensitivity to pain, and contribute to mood problems.<ref name="sickness behavior">{{cite journal | vauthors = Dell'Osso L, Bazzichi L, Baroni S, Falaschi V, Conversano C, Carmassi C, Marazziti D | title = The inflammatory hypothesis of mood spectrum broadened to fibromyalgia and chronic fatigue syndrome | journal = Clinical and Experimental Rheumatology | volume = 33 | issue = 1 Suppl 88 | pages = S109–S116 | date = 1 January 2015 | pmid = 25786052 }}</ref> Anti-inflammatory interleukins such as ] have also been associated with fibromyalgia.<ref name="Singh-2019" /> | |||
| *Tender points—there are 18 designated possible tender or trigger points (although a person with the disorder may feel pain in other areas as well). During diagnosis, four ] (39 ]s) of ] is exerted at each of the 18 points; the patient must feel pain at 11 or more of these points for fibromyalgia to be considered.<ref>{{cite web |author=National Institute of Arthritis and Musculoskeletal and Skin Diseases |title=Questions and Answers About Fibromyalgia – How Is Fibromyalgia Diagnosed? |url=http://www.niams.nih.gov/hi/topics/fibromyalgia/fibrofs.htm#fib_d |month=June | year=2004 |publisher=National Institutes for Health}}</ref> Four kilograms of force is about the amount of pressure required to blanch the thumbnail when applying pressure. | |||
| A repeated observation shows that ] triggers such as traumas and ]s are among the most frequent events preceding the onset of fibromyalgia.<ref name=Bazzichi2020>{{cite journal | vauthors = Bazzichi L, Giacomelli C, Consensi A, Giorgi V, Batticciotto A, Di Franco M, Sarzi-Puttini P | title = One year in review 2020: fibromyalgia | journal = Clinical and Experimental Rheumatology | volume = 38 | issue = 1 | pages = 3–8 | date = 2020 | pmid = 32116216 }}</ref> Neurogenic inflammation has been proposed as a contributing factor to fibromyalgia.<ref>{{cite journal | vauthors = Littlejohn G | title = Neurogenic neuroinflammation in fibromyalgia and complex regional pain syndrome | journal = Nature Reviews. Rheumatology | volume = 11 | issue = 11 | pages = 639–648 | date = November 2015 | pmid = 26241184 | doi = 10.1038/nrrheum.2015.100 | s2cid = 4368913 }}</ref> | |||
| This set of criteria was developed by the American College of Rheumatology as a means of classifying an individual as having fibromyalgia for both clinical and research purposes. While these criteria for classification of patients were originally established as inclusion criteria for research purposes and were not intended for clinical diagnosis, they have become the ''de facto'' diagnostic criteria in the clinical setting. It should be noted that the number of tender points that may be active at any one time may vary with time and circumstance. | |||
| === Digestive system === | |||
| ==Treatment== | |||
| As with many other ], there is no known cure or universally accepted treatment for fibromyalgia, and treatment is typically aimed at symptom management. Developments in the understanding of the pathophysiology of the disorder have led to improvements in treatment, which include prescription medication, behavioral intervention, exercise, and ] and ]. Indeed, integrated treatment plans that incorporate medication, patient education, aerobic exercise and cognitive-behavioral therapy have been shown to be effective in alleviating pain and other fibromyalgia-related symptoms.<ref name=Goldenberg2008>{{cite journal |author=Goldenberg DL |title=Multidisciplinary modalities in the treatment of fibromyalgia |journal=J Clin Psychiatry |volume=69 |suppl=2 |pages=30–4 |year=2008 |pmid=18537461 }}</ref> In 2005, the ] produced the first comprehensive guidelines for patient evaluation and management.<ref name=APS_2005>{{cite journal |author=Burkhardt C, Goldenberg DL, Crofford LJ, et al. |title=Guideline for the Management of Fibromyalgia Syndrome Pain in Adults and Children |journal= APS Clinical Practice Guidelines Series, No. 4, 2005 }}</ref> | |||
| More recently, the ] (EULAR) issued updated treatment guidelines.<ref name=p17644548 >{{cite journal |author=Carville SF, Arendt-Nielsen S, Bliddal H, et al. |title=EULAR evidence-based recommendations for the management of fibromyalgia syndrome.|journal=Ann Rheum Dis. |volume=67 |pages=536–41 |year=2008 |pmid=17644548 }}</ref> | |||
| === |
==== Gut microbiome ==== | ||
| Though there is a lack of evidence in this area, it is hypothesized that ] may play a role in fibromyalgia.<ref>{{cite journal | vauthors = Erdrich S, Hawrelak JA, Myers SP, Harnett JE | title = Determining the association between fibromyalgia, the gut microbiome and its biomarkers: A systematic review | journal = BMC Musculoskeletal Disorders | volume = 21 | issue = 1 | pages = 181 | date = March 2020 | pmid = 32192466 | pmc = 7083062 | doi = 10.1186/s12891-020-03201-9 | doi-access = free }}</ref> People with fibromyalgia are more likely to show ], a decrease in microbiota diversity.<ref>{{cite journal | vauthors = Wang Y, Wei J, Zhang W, Doherty M, Zhang Y, Xie H, Li W, Wang N, Lei G, Zeng C | display-authors = 6 | title = Gut dysbiosis in rheumatic diseases: A systematic review and meta-analysis of 92 observational studies | journal = eBioMedicine | volume = 80 | pages = 104055 | date = June 2022 | pmid = 35594658 | pmc = 9120231 | doi = 10.1016/j.ebiom.2022.104055 }}</ref> There is a bidirectional interplay between the gut and the nervous system. Therefore, the gut can affect the nervous system, but the nervous system can also affect the gut. Neurological effects mediated via the ] as well as the ] are directed to intestinal functional ]s, which in turn are under the influence of the gut microbiota.<ref>{{cite journal | vauthors = Minerbi A, Fitzcharles MA | title = Gut microbiome: pertinence in fibromyalgia | journal = Clinical and Experimental Rheumatology | volume = 38 | issue = 1 | pages = 99–104 | date = January 2020 | pmid = 32116215 }}</ref> | |||
| Some medications have reduced symptoms in some patients, but the results of pharmacological interventions must be weighed against side effects. In review in the 2009 Journal of Rheumatology, fibromyalgia researcher H.A. Smythe writes, “patients receive some benefit, but when side effects make the patient dull, lethargic, or fat, neither their goals nor those of society are satisfactorily met.”<ref name=SmytheMUS>Smythe HA, Explaining medically unexplained symptoms: widespread pain. J Rheumatol. 2009 Apr;36(4):679-83.</ref> | |||
| ==== |
==== Gut-brain axis ==== | ||
| The ], which connects the ] to the ] via the ], is another area of research. Fibromyalgia patients have less varied ] and altered ] levels of ] and ],<ref>{{cite journal | vauthors = Clos-Garcia M, Andrés-Marin N, Fernández-Eulate G, Abecia L, Lavín JL, van Liempd S, Cabrera D, Royo F, Valero A, Errazquin N, Vega MC, Govillard L, Tackett MR, Tejada G, Gónzalez E, Anguita J, Bujanda L, Orcasitas AM, Aransay AM, Maíz O, López de Munain A, Falcón-Pérez JM | display-authors = 6 | title = Gut microbiome and serum metabolome analyses identify molecular biomarkers and altered glutamate metabolism in fibromyalgia | journal = eBioMedicine | volume = 46 | pages = 499–511 | date = August 2019 | pmid = 31327695 | pmc = 6710987 | doi = 10.1016/j.ebiom.2019.07.031 }}</ref> implying abnormalities in ] ].<ref name=Bazzichi2020/> | |||
| A 2009 meta analysis in the ] reported that some antidepressants were effective, but with small ]es, against pain, fatigue, sleep disturbance, and depression in fibromyalgia. The analysis found “strong evidence against a favorable effect of antidepressants on fatigue.”<ref name="Treatment of fibromyalgia syndrome with antidepressants: a meta-analysis.">{{cite web |url=http://www.ncbi.nlm.nih.gov/pubmed/19141768?dopt=Abstract |title=Treatment of fibromyalgia syndrome with antidepressants: a meta-analysis. Häuser W, Bernardy K, Uçeyler N, Sommer C. |work= |accessdate=2009-01-24}}</ref> The authors conclude that the goal of antidepressants in fibromyalgia should be, at most, a “possible symptom reduction,” and the results must be balanced against side effects. Tricyclic antidepressants were the most effective against pain, fatigue, and sleep problems, but have many side effects due to interaction with adrenergic, cholinergic or histaminergic receptors, and sodium channels. ]s (SSRIs) and ]s (SNRIs) had lower effects. | |||
| === Energy metabolism === | |||
| ==== Low ATP in skeletal muscle ==== | |||
| Patients with fibromyalgia experience ]. Primary fibromyalgia is ] (cause unknown), whereas secondary fibromyalgia is in association with a known underlying disorder (such as ]).<ref>{{cite journal | vauthors = Borenstein D | title = Prevalence and treatment outcome of primary and secondary fibromyalgia in patients with spinal pain | journal = Spine | volume = 20 | issue = 7 | pages = 796–800 | date = April 1995 | pmid = 7701393 | doi = 10.1097/00007632-199504000-00011 | s2cid = 30837539 }}</ref>{{Primary source inline|date=July 2023}} In patients with primary fibromyalgia, studies have found disruptions in energy metabolism within skeletal muscle, including: decreased levels of ATP, ADP, and phosphocreatine, and increased levels of AMP and creatine (use of creatine kinase and myokinase in the ] system due to low ]);<ref>{{cite journal | vauthors = Bengtsson A, Henriksson KG, Larsson J | title = Reduced high-energy phosphate levels in the painful muscles of patients with primary fibromyalgia | journal = Arthritis and Rheumatism | volume = 29 | issue = 7 | pages = 817–821 | date = July 1986 | pmid = 3741498 | doi = 10.1002/art.1780290701 }}</ref>{{Primary source inline|date=July 2023}} increased ];<ref>{{cite journal | vauthors = Gerdle B, Ghafouri B, Lund E, Bengtsson A, Lundberg P, Ettinger-Veenstra HV, Leinhard OD, Forsgren MF | display-authors = 6 | title = Evidence of Mitochondrial Dysfunction in Fibromyalgia: Deviating Muscle Energy Metabolism Detected Using Microdialysis and Magnetic Resonance | journal = Journal of Clinical Medicine | volume = 9 | issue = 11 | pages = 3527 | date = October 2020 | pmid = 33142767 | doi = 10.3390/jcm9113527 | pmc = 7693920 | doi-access = free }}</ref>{{Primary source inline|date=July 2023}} as well as reduced capillary density impairing oxygen delivery to the muscle cells for ].<ref>{{cite journal | vauthors = Srikuea R, Symons TB, Long DE, Lee JD, Shang Y, Chomentowski PJ, Yu G, Crofford LJ, Peterson CA | display-authors = 6 | title = Association of fibromyalgia with altered skeletal muscle characteristics which may contribute to postexertional fatigue in postmenopausal women | journal = Arthritis and Rheumatism | volume = 65 | issue = 2 | pages = 519–528 | date = February 2013 | pmid = 23124535 | pmc = 3558634 | doi = 10.1002/art.37763 }}</ref><ref>{{cite journal | vauthors = Shang Y, Gurley K, Symons B, Long D, Srikuea R, Crofford LJ, Peterson CA, Yu G | display-authors = 6 | title = Noninvasive optical characterization of muscle blood flow, oxygenation, and metabolism in women with fibromyalgia | journal = Arthritis Research & Therapy | volume = 14 | issue = 6 | pages = R236 | date = November 2012 | pmid = 23116302 | pmc = 3674608 | doi = 10.1186/ar4079 | doi-access = free }}</ref>{{Primary source inline|date=July 2023}} | |||
| ==== Low ATP in brain ==== | |||
| Despite being a small percentage of the body's total mass, the brain consumes approximately 20% of the energy produced by the body.<ref name="Jung-2021" />{{Primary source inline|date=July 2023}} Parts of the brain—the anterior cingulate cortex (ACC), thalamus, and insula—were studied using ] (MRS) in patients with fibromyalgia and compared to healthy ]. The fibromyalgia patients were found to have lower phosphocreatine (PCr) and lower creatine (Cr) than the control group. Phosphocreatine is used in the ] system to produce ]. The study found that low creatine and low phosphocreatine were associated with high pain, and that high stress, including PTSD, may contribute to these low levels.<ref name="Jung-2021" />{{Primary source inline|date=July 2023}} | |||
| Low phosphocreatine levels may disrupt glutamate neurotransmission within the brains of those with fibromyalgia. Glutamate/creatine ratios within the bilateral ventrolateral prefrontal cortex were found to be significantly higher than in controls.<ref name="Jung-2021" /><ref name="Feraco-2011" />{{Primary source inline|date=July 2023}} | |||
| == Diagnosis == | |||
| ] criteria for fibromyalgia]] | |||
| There is no single pathological feature, laboratory finding, or biomarker that can diagnose fibromyalgia, and there is debate over what should be considered diagnostic criteria and whether a ] is possible, to begin with.<ref name="Tan-2019" /> In most cases, people with fibromyalgia symptoms may have laboratory test results that appear normal and many of their symptoms may mimic those of other rheumatic conditions such as arthritis or osteoporosis. The specific diagnostic criteria for fibromyalgia have evolved.<ref>{{cite journal | vauthors = Häuser W, Fitzcharles MA | title = Facts and myths pertaining to fibromyalgia | journal = Dialogues in Clinical Neuroscience | volume = 20 | issue = 1 | pages = 53–62 | date = March 2018 | pmid = 29946212 | pmc = 6016048 | doi = 10.31887/DCNS.2018.20.1/whauser }}</ref> | |||
| === American College of Rheumatology=== | |||
| The first widely accepted set of classification criteria for research purposes was elaborated in 1990 by the Multicenter Criteria Committee of the ]. These criteria, which are known informally as "the ACR 1990", defined fibromyalgia according to the presence of the following criteria: | |||
| * A history of widespread pain lasting more than three months – affecting all four quadrants of the body, i.e., both sides and above and below the waist. | |||
| * Tender points – there are 18 designated possible tender points (although a person with the disorder may feel pain in other areas as well). | |||
| The ACR criteria for the classification of patients were originally established as inclusion criteria for research purposes and were not intended for clinical diagnosis but have later become the ''de facto'' diagnostic criteria in the clinical setting. A controversial study was done by a legal team looking to prove their client's disability based primarily on tender points and their widespread presence in non-litigious communities prompted the lead author of the ACR criteria to question now the useful validity of tender points in diagnosis.<ref>{{cite journal | vauthors = Wolfe F | title = Stop using the American College of Rheumatology criteria in the clinic | journal = The Journal of Rheumatology | volume = 30 | issue = 8 | pages = 1671–1672 | date = August 2003 | pmid = 12913920 | url = http://www.jrheum.com/subscribers/03/08/1671.html | url-status = live | archive-url = https://web.archive.org/web/20111014114743/http://jrheum.com/subscribers/03/08/1671.html | archive-date = 14 October 2011 }}</ref> Use of control points has been used to cast doubt on whether a person has fibromyalgia, and to claim the person is malingering.<ref name="pmid19623319">{{cite journal | vauthors = Häuser W, Eich W, Herrmann M, Nutzinger DO, Schiltenwolf M, Henningsen P | title = Fibromyalgia syndrome: classification, diagnosis, and treatment | journal = Deutsches Ärzteblatt International | volume = 106 | issue = 23 | pages = 383–391 | date = June 2009 | pmid = 19623319 | pmc = 2712241 | doi = 10.3238/arztebl.2009.0383 }}</ref> | |||
| ] | |||
| In 2010, the American College of Rheumatology approved provisional revised diagnostic criteria for fibromyalgia that eliminated the 1990 criteria's reliance on tender point testing.<ref name=Wolfe2010>{{cite journal | vauthors = Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB | display-authors = 6 | title = The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity | journal = Arthritis Care & Research | volume = 62 | issue = 5 | pages = 600–610 | date = May 2010 | pmid = 20461783 | doi = 10.1002/acr.20140 | hdl-access = free | s2cid = 17154205 | hdl = 2027.42/75772 }}</ref> The revised criteria used a widespread pain index (WPI) and symptom severity scale (SSS) in place of tender point testing under the 1990 criteria. The WPI counts up to 19 general body areas{{efn|Shoulder girdle (left & right), upper arm (left & right), lower arm (left & right), hip/buttock/trochanter (left & right), upper leg (left & right), lower leg (left & right), jaw (left & right), chest, abdomen, back (upper & lower), and neck.<ref name=Wolfe2010 />{{rp|607}}}} in which the person has experienced pain in the preceding week.<ref name=Wolfe2016/> The SSS rates the severity of the person's fatigue, unrefreshed waking, cognitive symptoms, and general somatic symptoms,{{efn|Somatic symptoms include, but are not limited to muscle pain, irritable bowel syndrome, fatigue or tiredness, problems thinking or remembering, muscle weakness, headache, pain or cramps in the abdomen, numbness or tingling, dizziness, insomnia, depression, constipation, pain in the upper abdomen, nausea, nervousness, chest pain, blurred vision, fever, diarrhea, dry mouth, itching, wheezing, Raynaud's phenomenon, hives or welts, ringing in the ears, vomiting, heartburn, oral ulcers, loss of or changes in taste, seizures, dry eyes, shortness of breath, loss of appetite, rash, sun sensitivity, hearing difficulties, easy bruising, hair loss, frequent or painful urination, and bladder spasms.<ref name=Wolfe2010 />{{rp|607}}}} each on a scale from 0 to 3, for a composite score ranging from 0 to 12.<ref name=Wolfe2016/> The revised criteria for diagnosis were: | |||
| * WPI ≥ 7 and SSS ≥ 5 ''OR'' WPI 3–6 and SSS ≥ 9, | |||
| * Symptoms have been present at a similar level for at least three months, ''and'' | |||
| * No other diagnosable disorder otherwise explains the pain.<ref name=Wolfe2010 />{{rp|607}} | |||
| In 2016, the provisional criteria of the American College of Rheumatology from 2010 were revised.<ref name=Wolfe2016/> The new diagnosis required all of the following criteria: | |||
| # "Generalized pain, defined as pain in at least 4 of 5 regions, is present." | |||
| # "Symptoms have been present at a similar level for at least 3 months." | |||
| # "Widespread pain index (WPI) ≥ 7 and symptom severity scale (SSS) score ≥ 5 OR WPI of 4–6 and SSS score ≥ 9." | |||
| # "A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses."<ref name="Wolfe2016" /> | |||
| === American Pain Society 2019 === | |||
| ] | |||
| In 2019, the ] in collaboration with the U.S. ] developed a new diagnostic system using two dimensions.<ref name="Arnold-2019">{{cite journal | vauthors = Arnold LM, Bennett RM, Crofford LJ, Dean LE, Clauw DJ, Goldenberg DL, Fitzcharles MA, Paiva ES, Staud R, Sarzi-Puttini P, Buskila D, Macfarlane GJ | display-authors = 6 | title = AAPT Diagnostic Criteria for Fibromyalgia | journal = The Journal of Pain | volume = 20 | issue = 6 | pages = 611–628 | date = June 2019 | pmid = 30453109 | doi = 10.1016/j.jpain.2018.10.008 | s2cid = 53872511 | doi-access = free | hdl = 2434/632765 | hdl-access = free }}</ref> The first dimension included core diagnostic criteria and the second included common features. In accordance to the 2016 diagnosis guidelines, the presence of another medical condition or pain disorder does not rule out the diagnosis of fibromyalgia. Nonetheless, other conditions should be ruled out as the main explaining reason for the patient's symptoms. The core diagnostic criteria are:<ref name=":6">{{cite journal |vauthors=Galvez-Sánchez CM, Reyes Del Paso GA |date=April 2020 |title=Diagnostic Criteria for Fibromyalgia: Critical Review and Future Perspectives |journal=Journal of Clinical Medicine |volume=9 |issue=4 |pages=1219 |doi=10.3390/jcm9041219 |pmc=7230253 |pmid=32340369 |quote=Furthermore, in many cases the FMS diagnosis is fundamentally based on the exclusion of other similar diseases; in spite of that practice not being recommended because of its lack of precision and the high possibility of misdiagnosis. |doi-access=free}}</ref> | |||
| # Multisite pain defined as six or more pain sites from a total of nine possible sites (head, arms, chest, abdomen, upper back, lower back, and legs), for at least three months | |||
| # Moderate to severe ] or ], for at least three months | |||
| Common features found in fibromyalgia patients can assist the diagnosis process. These are tenderness (sensitivity to light pressure), ] (difficulty to think), ] stiffness, and ] or ].<ref name="Arnold-2019" /> | |||
| === Self-report questionnaires === | |||
| Some research has suggested using a multidimensional approach taking into consideration somatic symptoms, psychological factors, psychosocial stressors and subjective belief regarding fibromyalgia.<ref name=Wang2015>{{cite journal | vauthors = Wang SM, Han C, Lee SJ, Patkar AA, Masand PS, Pae CU | title = Fibromyalgia diagnosis: a review of the past, present and future | journal = Expert Review of Neurotherapeutics | volume = 15 | issue = 6 | pages = 667–679 | date = June 2015 | pmid = 26035624 | doi = 10.1586/14737175.2015.1046841 | s2cid = 2412984 }}</ref> These symptoms can be assessed by several self-report questionnaires.<ref name="Wolfe2016" /> | |||
| ==== Widespread Pain Index (WPI) ==== | |||
| The Widespread Pain Index (WPI) was introduced by the American College of Rheumatology in 2010. It measures the number of painful body regions.<ref name="Wolfe2010" /> The revised criteria count up to 19 general body areas: ], upper arm, lower arm, hip/buttock/], upper leg, lower leg, jaw, all left & right; plus the chest, abdomen, neck and upper and lower back.<ref name=Wolfe2010 /> The 2016 ACR criteria required a Widespread pain index (WPI) ≥ 7 or WPI of 4–6 for higher severity pain. | |||
| ==== Symptom Severity Scale (SSS) ==== | |||
| The Symptom Severity Scale (SSS) assesses the severity of the fibromyalgia symptoms. | |||
| ==== Fibromyalgia Impact Questionnaire (FIQ) ==== | |||
| The Fibromyalgia Impact Questionnaire (FIQ)<ref>{{cite journal | vauthors = Burckhardt CS, Clark SR, Bennett RM | title = The fibromyalgia impact questionnaire: development and validation | journal = The Journal of Rheumatology | volume = 18 | issue = 5 | pages = 728–733 | date = May 1991 | pmid = 1865419 | url = https://pubmed.ncbi.nlm.nih.gov/1865419 | access-date = 18 June 2022 | archive-date = 16 May 2022 | archive-url = https://web.archive.org/web/20220516122017/https://pubmed.ncbi.nlm.nih.gov/1865419/ | url-status = live }}</ref> and the Revised Fibromyalgia Impact Questionnaire (FIQR)<ref name="Bennett-2009">{{cite journal | vauthors = Bennett RM, Friend R, Jones KD, Ward R, Han BK, Ross RL | title = The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties | journal = Arthritis Research & Therapy | volume = 11 | issue = 4 | pages = R120 | date = 2009-01-01 | pmid = 19664287 | pmc = 2745803 | doi = 10.1186/ar2783 | doi-access = free }}</ref> assess three domains: function, overall impact and symptoms.<ref name="Bennett-2009" /> It is considered a useful measure of disease impact.<ref>{{Cite web |title=Fibromyalgia Impact Questionnaire (FIQ) |url=https://www.rheumatology.org/I-Am-A/Rheumatologist/Research/Clinician-Researchers/Fibromyalgia-Impact-Questionnaire-FIQ |website=American College of Rheumatology |access-date=18 June 2022 |archive-date=1 July 2022 |archive-url=https://web.archive.org/web/20220701012320/https://www.rheumatology.org/I-Am-A/Rheumatologist/Research/Clinician-Researchers/Fibromyalgia-Impact-Questionnaire-FIQ |url-status=live }}</ref> | |||
| ==== Other questionnaires ==== | |||
| Other measures include the ''],'' ''Multiple Ability Self-Report Questionnaire'',<ref>{{cite journal | vauthors = Seidenberg M, Haltiner A, Taylor MA, Hermann BB, Wyler A | title = Development and validation of a Multiple Ability Self-Report Questionnaire | journal = Journal of Clinical and Experimental Neuropsychology | volume = 16 | issue = 1 | pages = 93–104 | date = February 1994 | pmid = 8150893 | doi = 10.1080/01688639408402620 }}</ref> ''Multidimensional Fatigue Inventory, and'' ''Medical Outcomes Study Sleep Scale.'' | |||
| ===Differential diagnosis=== | |||
| As of 2009, as many as two out of every three people who are told that they have fibromyalgia by a ] may have some other medical condition instead.<ref name="Goldenberg2009" /> Fibromyalgia could be misdiagnosed in cases of early undiagnosed ] such as preclinical ], early stages of inflammatory ], ], ]s and ].<ref name=Hauser2019>{{cite journal | vauthors = Häuser W, Sarzi-Puttini P, Fitzcharles MA | title = Fibromyalgia syndrome: under-, over- and misdiagnosis | journal = Clinical and Experimental Rheumatology | volume = 37 | issue = 1 Suppl 116 | pages = 90–97 | date = 2019 | pmid = 30747096 }}</ref><ref name=Hauser2017>{{cite journal | vauthors = Häuser W, Perrot S, Sommer C, Shir Y, Fitzcharles MA | title = Diagnostic confounders of chronic widespread pain: not always fibromyalgia | journal = Pain Reports | volume = 2 | issue = 3 | pages = e598 | date = May 2017 | pmid = 29392213 | pmc = 5741304 | doi = 10.1097/PR9.0000000000000598 }}</ref> ] with an important pain component include ], ] and ].<ref name=Hauser2019/><ref name=Hauser2017/> Other medical illnesses that should be ruled out are ] or ] (], ], ], ]), ] (] and ]), ] (], ] and ]) and the early stages of a ] such as ], ] and ]/].<ref name=Hauser2019/><ref name=Hauser2017/> Other systemic, inflammatory, endocrine, rheumatic, infectious, and neurologic disorders may cause fibromyalgia-like symptoms, such as ], ], ], ], psoriatic-related polyenthesitis, a ] (such as ]), and ].<ref name="RossiDiLollo">{{cite journal | vauthors = Rossi A, Di Lollo AC, Guzzo MP, Giacomelli C, Atzeni F, Bazzichi L, Di Franco M | title = Fibromyalgia and nutrition: what news? | journal = Clinical and Experimental Rheumatology | volume = 33 | issue = 1 Suppl 88 | pages = S117–S125 | date = 2015 | pmid = 25786053 }}</ref><ref name="Goldenberg2009" /><ref name="MarchesoniDeMarco2018" /><ref name="PalazziDAmico2016" /> In addition, several medications can also evoke pain (]s, ], ], and ]s).<ref name="Arnold-2019" /> | |||
| The differential diagnosis is made during the evaluation based on the person's ], physical examination, and laboratory investigations.<ref name="RossiDiLollo" /><ref name="Goldenberg2009">{{cite journal | vauthors = Goldenberg DL | title = Diagnosis and differential diagnosis of fibromyalgia | journal = The American Journal of Medicine | volume = 122 | issue = 12 Suppl | pages = S14–S21 | date = December 2009 | pmid = 19962492 | doi = 10.1016/j.amjmed.2009.09.007 | type = Review }}</ref><ref name="MarchesoniDeMarco2018">{{cite journal | vauthors = Marchesoni A, De Marco G, Merashli M, McKenna F, Tinazzi I, Marzo-Ortega H, McGonagle DG | title = The problem in differentiation between psoriatic-related polyenthesitis and fibromyalgia | journal = Rheumatology | volume = 57 | issue = 1 | pages = 32–40 | date = January 2018 | pmid = 28387854 | doi = 10.1093/rheumatology/kex079 | type = Review | s2cid = 205309871 }}</ref><ref name="PalazziDAmico2016">{{cite journal | vauthors = Palazzi C, D'Amico E, D'Angelo S, Gilio M, Olivieri I | title = Rheumatic manifestations of hepatitis C virus chronic infection: Indications for a correct diagnosis | journal = World Journal of Gastroenterology | volume = 22 | issue = 4 | pages = 1405–1410 | date = January 2016 | pmid = 26819509 | pmc = 4721975 | doi = 10.3748/wjg.v22.i4.1405 | type = Review | doi-access = free }}</ref> The patient's history can provide some hints to a fibromyalgia diagnosis. A ] of early ], a childhood history of pain, an emergence of broad pain following physical and/or psychosocial ], a general hypersensitivity to ], ], ], ], ], and various ] (], ], ], ]), are all examples of these signals.<ref name=Hauser2019/> | |||
| Extensive laboratory tests are usually unnecessary in the differential diagnosis of fibromyalgia.<ref name="Arnold-2019" /> Common tests that are conducted include ], ], ], ], and ].<ref name="Arnold-2019" /> | |||
| ==Management== | |||
| Universally accepted treatments typically consist of symptom management and improving patient quality of life.<ref name=Prab2019>{{cite journal | vauthors = Prabhakar A, Kaiser JM, Novitch MB, Cornett EM, Urman RD, Kaye AD | title = The Role of Complementary and Alternative Medicine Treatments in Fibromyalgia: a Comprehensive Review | journal = Current Rheumatology Reports | volume = 21 | issue = 5 | pages = 14 | date = March 2019 | pmid = 30830504 | doi = 10.1007/s11926-019-0814-0 | s2cid = 73482737 }}</ref> A personalized, multidisciplinary approach to treatment that includes pharmacologic considerations and begins with effective patient education is most beneficial.<ref name=Prab2019/> Developments in the understanding of the pathophysiology of the disorder have led to improvements in treatment, which include prescription medication, behavioral intervention, and exercise. | |||
| Several associations have published guidelines for the diagnosis and management of fibromyalgia. The ] (EULAR; 2017)<ref name="Macfarlane-2017">{{cite journal | vauthors = Macfarlane GJ, Kronisch C, Atzeni F, Häuser W, Choy EH, Amris K, Branco J, Dincer F, Leino-Arjas P, Longley K, McCarthy G, Makri S, Perrot S, Sarzi Puttini P, Taylor A, Jones GT | display-authors = 6 | title = EULAR recommendations for management of fibromyalgia | journal = Annals of the Rheumatic Diseases | volume = 76 | issue = 12 | pages = e54 | date = December 2017 | pmid = 28476880 | doi = 10.1136/annrheumdis-2017-211587 | s2cid = 26251476 | url = https://orca.cardiff.ac.uk/id/eprint/123698/1/EULAR%20recommendations%20for%20management%20of%20fibromyalgia%20%20ECHOY%20%20ANN%20RHEUM%20DIS.pdf | access-date = 4 March 2023 | archive-date = 8 February 2023 | archive-url = https://web.archive.org/web/20230208040018/https://orca.cardiff.ac.uk/id/eprint/123698/1/EULAR%20recommendations%20for%20management%20of%20fibromyalgia%20%20ECHOY%20%20ANN%20RHEUM%20DIS.pdf | url-status = live }}</ref> recommends a multidisciplinary approach, allowing a quick diagnosis and patient education. The recommended initial management should be non-pharmacological, later pharmacological treatment can be added. The ] gave the strongest recommendation for ] and ]. Weak recommendations were given to some treatments, based on their outcomes. ], ], and ] were weakly recommended for improving ] and ]. ] was weakly recommended for improving pain and ]. ] and ] were weakly recommended for improving pain. A weak recommendation was also given to ]. It was more suitable for patients with ]s or unhelpful ]. ] was strongly recommended against, due to ] concerns. Some medications were weakly recommended for severe pain (], ], ]) or ] (], ], ]). Others were not recommended due to a lack of efficacy (]s, ]s and ]s). ], ], ]s, and ]s were strongly recommended against due to lack of efficacy and ]s. | |||
| The guidelines published by the ]<ref name="German">{{cite journal | vauthors = Sommer C, Häuser W, Alten R, Petzke F, Späth M, Tölle T, Uçeyler N, Winkelmann A, Winter E, Bär KJ | display-authors = 6 | title = | journal = Schmerz | volume = 26 | issue = 3 | pages = 297–310 | date = June 2012 | pmid = 22760463 | doi = 10.1007/s00482-012-1172-2 | s2cid = 1348989 | url = http://www.awmf.org/fileadmin/user_upload/Leitlinien/041_D_Interdisziplinaere_V_fuer_Schmerztherapie/041-004le_S3_Fibromyalgiesyndrom_2012-04.pdf#page=43 | url-status = dead | archive-url = https://web.archive.org/web/20130216060923/http://www.awmf.org/fileadmin/user_upload/Leitlinien/041_D_Interdisziplinaere_V_fuer_Schmerztherapie/041-004le_S3_Fibromyalgiesyndrom_2012-04.pdf#page=43 | archive-date = 16 February 2013 }}</ref> inform patients that self-management strategies are an important component in managing the disease.<ref name=Fitz2013/> The ]<ref name="Canadian">{{Cite web|url=http://fmguidelines.ca/?page_id=21|archive-url=https://web.archive.org/web/20130611010115/http://fmguidelines.ca/?page_id=21|url-status=dead|title=Management | Canadian Guidelines for the Diagnosis and Management of Fibromyalgia|archive-date=11 June 2013}}</ref> also published guidelines for the diagnosis and management of fibromyalgia. | |||
| === Exercise === | |||
| Exercise is the only fibromyalgia treatment that has been given a strong recommendation by the European Alliance of Associations for Rheumatology (]). There is strong evidence indicating that exercise improves fitness, sleep and quality of life and may reduce pain and fatigue for people with fibromyalgia.<ref name="Busch2007">{{cite journal | vauthors = Busch AJ, Barber KA, Overend TJ, Peloso PM, Schachter CL | title = Exercise for treating fibromyalgia syndrome | journal = The Cochrane Database of Systematic Reviews | issue = 4 | pages = CD003786 | date = October 2007 | pmid = 17943797 | doi = 10.1002/14651858.CD003786.pub2 }}</ref><ref name="Ibáñez-Vera-2018" /><ref name="Andrade-2020">{{cite journal | vauthors = Andrade A, Dominski FH, Sieczkowska SM | title = What we already know about the effects of exercise in patients with fibromyalgia: An umbrella review | journal = Seminars in Arthritis and Rheumatism | volume = 50 | issue = 6 | pages = 1465–1480 | date = December 2020 | pmid = 32147091 | doi = 10.1016/j.semarthrit.2020.02.003 | s2cid = 212638860 }}</ref> Exercise has an added benefit in that it does not cause any serious adverse effects.<ref name="Andrade-2020" /> There are a number of hypothesized biological mechanisms.<ref name="Masquelier-2021">{{MEDRS|date=March 2022}} {{cite journal | vauthors = Masquelier E, D'haeyere J | title = Physical activity in the treatment of fibromyalgia | journal = Joint Bone Spine | volume = 88 | issue = 5 | pages = 105202 | date = October 2021 | pmid = 33962033 | doi = 10.1016/j.jbspin.2021.105202 }}</ref> Exercise may improve pain modulation<ref>{{cite journal | vauthors = McLoughlin MJ, Stegner AJ, Cook DB | title = The relationship between physical activity and brain responses to pain in fibromyalgia | journal = The Journal of Pain | volume = 12 | issue = 6 | pages = 640–651 | date = June 2011 | pmid = 21330218 | pmc = 3111901 | doi = 10.1016/j.jpain.2010.12.004 }}</ref><ref name="Valim-2013">{{cite journal | vauthors = Valim V, Natour J, Xiao Y, Pereira AF, Lopes BB, Pollak DF, Zandonade E, Russell IJ | display-authors = 6 | title = Effects of physical exercise on serum levels of serotonin and its metabolite in fibromyalgia: a randomized pilot study | language = es | journal = Revista Brasileira de Reumatologia | volume = 53 | issue = 6 | pages = 538–541 | date = November 2013 | pmid = 24477734 | doi = 10.1016/j.rbr.2013.02.001 | doi-access = free }}</ref> through serotoninergic pathways.<ref name="Valim-2013" /> It may reduce pain by altering the hypothalamic-pituitary-adrenal axis and reducing cortisol levels.<ref>{{cite journal | vauthors = Genc A, Tur BS, Aytur YK, Oztuna D, Erdogan MF | title = Does aerobic exercise affect the hypothalamic-pituitary-adrenal hormonal response in patients with fibromyalgia syndrome? | journal = Journal of Physical Therapy Science | volume = 27 | issue = 7 | pages = 2225–2231 | date = July 2015 | pmid = 26311959 | pmc = 4540854 | doi = 10.1589/jpts.27.2225 }}</ref> It also has anti-inflammatory effects that may improve fibromyalgia symptoms.<ref name="El-Shewy-2019" /><ref>{{cite journal | vauthors = Andrade A, Vilarino GT, Sieczkowska SM, Coimbra DR, Steffens RA, Vietta GG | title = Acute effects of physical exercises on the inflammatory markers of patients with fibromyalgia syndrome: A systematic review | journal = Journal of Neuroimmunology | volume = 316 | pages = 40–49 | date = March 2018 | pmid = 29254627 | doi = 10.1016/j.jneuroim.2017.12.007 | s2cid = 46879701 }}</ref> Aerobic exercise can improve muscle metabolism and pain through mitochondrial pathways.<ref name="El-Shewy-2019" /> | |||
| When different exercise programs are compared, aerobic exercise is capable of modulating the autonomic nervous function of fibromyalgia patients, whereas resistance exercise does not show such effects.<ref name="Andrade-2019" /> A 2022 meta-analysis found that aerobic training showed a high effect size while strength interventions showed moderate effects.<ref name="Albuquerque-2022" /> Meditative exercise seems preferable for improving sleep,<ref name="Estevez2021" /><ref>{{Cite journal |last1=Cuenca-Martínez |first1=Ferran |last2=Suso-Martí |first2=Luis |last3=Fernández-Carnero |first3=Josué |last4=Muñoz-Alarcos |first4=Vicente |last5=Sempere-Rubio |first5=Núria |date=2023 |title=Exercise-based interventions on sleep quality in patients with fibromyalgia syndrome: An umbrella and mapping review with meta-analysis |journal=Seminars in Arthritis and Rheumatism |language=en |volume=61 |pages=152216 |doi=10.1016/j.semarthrit.2023.152216|pmid=37229847 |s2cid=258597720 |doi-access=free }}</ref> with no differences between resistance, flexibility, and aquatic exercise in their favorable effects on fatigue.<ref name=Estevez2021>{{cite journal | vauthors = Estévez-López F, Maestre-Cascales C, Russell D, Álvarez-Gallardo IC, Rodriguez-Ayllon M, Hughes CM, Davison GW, Sañudo B, McVeigh JG | display-authors = 6 | title = Effectiveness of Exercise on Fatigue and Sleep Quality in Fibromyalgia: A Systematic Review and Meta-analysis of Randomized Trials | journal = Archives of Physical Medicine and Rehabilitation | volume = 102 | issue = 4 | pages = 752–761 | date = April 2021 | pmid = 32721388 | doi = 10.1016/j.apmr.2020.06.019 | s2cid = 220847961 | doi-access = free | hdl = 10481/68683 | hdl-access = free }}</ref> | |||
| Despite its benefits, exercise is a challenge for patients with fibromyalgia, due to the chronic fatigue and pain they experience.<ref>{{cite journal | vauthors = McVeigh JG, Lucas A, Hurley DA, Basford JR, Baxter GD | title = Patients' perceptions of exercise therapy in the treatment of fibromyalgia syndrome: a survey | journal = Musculoskeletal Care | volume = 1 | issue = 2 | pages = 98–107 | date = September 2003 | pmid = 20217670 | doi = 10.1002/msc.45 }}</ref> They may also feel that those who recommend or deliver exercise interventions do not fully understand the possible negative impact of exercise on fatigue and pain.<ref name="Russell-2018" /> This is especially true for non-personalized exercise programs.<ref name="Russell-2018" /> Adherence is higher when the exercise program is recommended by doctors or supervised by nurses.<ref>{{cite journal | vauthors = Sanz-Baños Y, Pastor-Mira MÁ, Lledó A, López-Roig S, Peñacoba C, Sánchez-Meca J | title = Do women with fibromyalgia adhere to walking for exercise programs to improve their health? Systematic review and meta-analysis | journal = Disability and Rehabilitation | volume = 40 | issue = 21 | pages = 2475–2487 | date = October 2018 | pmid = 28687050 | doi = 10.1080/09638288.2017.1347722 | s2cid = 9032840 }}</ref> | |||
| Sufferers perceive exercise as more effortful than healthy adults.<ref>{{cite journal | vauthors = Barhorst EE, Andrae WE, Rayne TJ, Falvo MJ, Cook DB, Lindheimer JB | title = Elevated Perceived Exertion in People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Fibromyalgia: A Meta-analysis | journal = Medicine and Science in Sports and Exercise | volume = 52 | issue = 12 | pages = 2615–2627 | date = December 2020 | pmid = 32555018 | doi = 10.1249/MSS.0000000000002421 | pmc = 10200687 | s2cid = 219918068 }}</ref> Depression and higher pain intensity serve as barriers to physical activity.<ref>{{cite journal | vauthors = Vancampfort D, McGrath RL, Hemmings L, Gillis V, Bernar K, Van Damme T | title = Physical activity correlates in people with fibromyalgia: a systematic review | journal = Disability and Rehabilitation | pages = 4165–4174 | date = November 2022 | volume = 45 | issue = 25 | pmid = 36398698 | doi = 10.1080/09638288.2022.2146911 | s2cid = 253627372 | url = https://lirias.kuleuven.be/handle/20.500.12942/710200 }}</ref> Exercise may intimidate them, in fear that they will be asked to do more than they are capable of.<ref name="Russell-2018">{{cite journal | vauthors = Russell D, Álvarez Gallardo IC, Wilson I, Hughes CM, Davison GW, Sañudo B, McVeigh JG | title = 'Exercise to me is a scary word': perceptions of fatigue, sleep dysfunction, and exercise in people with fibromyalgia syndrome-a focus group study | journal = Rheumatology International | volume = 38 | issue = 3 | pages = 507–515 | date = March 2018 | pmid = 29340774 | doi = 10.1007/s00296-018-3932-5 | s2cid = 3395036 }}</ref> | |||
| A recommended approach to a graded exercise program begins with small, frequent exercise periods and builds up from there.<ref name="Albuquerque-2022" /><ref name="Ryan2013">{{cite journal | vauthors = Ryan S | title = Care of patients with fibromyalgia: assessment and management | journal = Nursing Standard | volume = 28 | issue = 13 | pages = 37–43 | year = 2013 | pmid = 24279570 | doi = 10.7748/ns2013.11.28.13.37.e7722 }}</ref> In order to reduce pain the use of an exercise program of 13 to 24 weeks is recommended, with each session lasting 30 to 60 minutes.<ref name="Albuquerque-2022">{{cite journal | vauthors = Albuquerque ML, Monteiro D, Marinho DA, Vilarino GT, Andrade A, Neiva HP | title = Effects of different protocols of physical exercise on fibromyalgia syndrome treatment: systematic review and meta-analysis of randomized controlled trials | journal = Rheumatology International | volume = 42 | issue = 11 | pages = 1893–1908 | date = November 2022 | pmid = 35604435 | doi = 10.1007/s00296-022-05140-1 | hdl-access = free | s2cid = 248970279 | hdl = 10400.8/7188 }}</ref> | |||
| ==== Aerobic ==== | |||
| Aerobic exercise for fibromyalgia patients is the most investigated type of exercise.<ref name="Andrade-2020" /> It includes activities such as walking, jogging, spinning, cycling, dancing and exercising in water,<ref name="El-Shewy-2019" /><ref name="Andrade-2019" /> with walking being named as one of the best methods.<ref>{{cite journal | vauthors = Majdoub F, Ben Nessib D, Ferjani HL, Kaffel D, Triki W, Maatallah K, Hamdi W | title = Non-pharmacological therapies in Fibromyalgia: New horizons for physicians, new hopes for patients | journal = Musculoskeletal Care | pages = 603–610 | date = February 2023 | volume = 21 | issue = 3 | pmid = 36757930 | doi = 10.1002/msc.1741 | s2cid = 256696861 }}</ref> A 2017 Cochrane summary concluded that aerobic exercise probably improves quality of life, slightly decreases pain and improves physical function and makes no difference in fatigue and stiffness.<ref name="Bid2017">{{cite journal | vauthors = Bidonde J, Busch AJ, Schachter CL, Overend TJ, Kim SY, Góes SM, Boden C, Foulds HJ | display-authors = 6 | title = Aerobic exercise training for adults with fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 2017 | issue = 6 | pages = CD012700 | date = June 2017 | pmid = 28636204 | pmc = 6481524 | doi = 10.1002/14651858.cd012700 }}</ref> A 2019 meta-analysis showed that exercising aerobically can reduce autonomic dysfunction and increase heart rate variability.<ref name="Andrade-2019">{{cite journal | vauthors = Andrade A, Vilarino GT, Serafim TT, Pereira Júnior AA, de Souza CA, Sieczkowska SM | title = Modulation of Autonomic Function by Physical Exercise in Patients with Fibromyalgia Syndrome: A Systematic Review | journal = PM&R | volume = 11 | issue = 10 | pages = 1121–1131 | date = October 2019 | pmid = 30900831 | doi = 10.1002/pmrj.12158 | s2cid = 85448644 }}</ref> This happens when patients exercise at least twice a week, for 45–60 minutes at about 60%-80% of the maximum heart rate.<ref name="Andrade-2019" /> Aerobic exercise also decreases anxiety and depression and improves the quality of life.<ref name="Andrade-2019" /> | |||
| ==== Flexibility ==== | |||
| Combinations of different exercises such as flexibility and aerobic training may improve stiffness.<ref name=Bidonde2019>{{cite journal | vauthors = Bidonde J, Busch AJ, Schachter CL, Webber SC, Musselman KE, Overend TJ, Góes SM, Dal Bello-Haas V, Boden C | display-authors = 6 | title = Mixed exercise training for adults with fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 2019 | issue = 5 | pages = CD013340 | date = May 2019 | pmid = 31124142 | pmc = 6931522 | doi = 10.1002/14651858.cd013340 }}</ref> However, the evidence is of low-quality.<ref name=Bidonde2019/> It is not clear if flexibility training alone compared to aerobic training is effective at reducing symptoms or has any adverse effects.<ref>{{cite journal | vauthors = Kim SY, Busch AJ, Overend TJ, Schachter CL, van der Spuy I, Boden C, Góes SM, Foulds HJ, Bidonde J | display-authors = 6 | title = Flexibility exercise training for adults with fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 2019 | issue = 9 | pages = CD013419 | date = September 2019 | pmid = 31476271 | pmc = 6718217 | doi = 10.1002/14651858.CD013419 }}</ref> | |||
| ==== Resistance ==== | |||
| In ], participants apply a load to their body using weights, elastic bands, body weight, or other measures. | |||
| Two meta-analyses on fibromyalgia have shown that resistance training can reduce anxiety and depression,<ref name="Andrade-2019" /><ref>{{cite journal | vauthors = Vilarino GT, Andreato LV, de Souza LC, Branco JH, Andrade A | title = Effects of resistance training on the mental health of patients with fibromyalgia: a systematic review | journal = Clinical Rheumatology | volume = 40 | issue = 11 | pages = 4417–4425 | date = November 2021 | pmid = 33987785 | doi = 10.1007/s10067-021-05738-z | s2cid = 234489153 }}</ref> one found that it decreases pain and disease severity<ref>{{Cite journal |last1=Rodríguez-Domínguez |first1=Álvaro-José |last2=Rebollo-Salas |first2=Manuel |last3=Chillón-Martínez |first3=Raquel |last4=Rosales-Tristancho |first4=Abel |last5=Jiménez-Rejano |first5=José-Jesús |date=2023-07-17 |title=Clinical relevance of resistance training in women with fibromyalgia: A systematic review and meta-analysis |journal=European Journal of Pain |volume=28 |issue=1 |pages=21–36 |language=en |doi=10.1002/ejp.2161 |pmid=37458315 |s2cid=259949000 |issn=1090-3801|doi-access=free }}</ref> and one found that it improves quality of life.<ref name="Andrade-2019" /> Resistance training may also improve sleep, with a greater effect than that of flexibility training and a similar effect to that of aerobic exercise.<ref>{{Cite journal |last1=Bastos |first1=Ana Cecilia Rosatelli de Freitas |last2=Vilarino |first2=Guilherme Torres |last3=de Souza |first3=Loiane Cristina |last4=Dominski |first4=Fabio Hech |last5=Branco |first5=Joaquim Henrique Lorenzetti |last6=Andrade |first6=Alexandro |date=2023-05-15 |title=Effects of resistance training on sleep of patients with fibromyalgia: A systematic review |url=http://journals.sagepub.com/doi/10.1177/13591053231172288 |journal=Journal of Health Psychology |volume=28 |issue=11 |language=en |pages=1072–1084 |doi=10.1177/13591053231172288 |pmid=37183814 |s2cid=258687258 |issn=1359-1053 |access-date=28 July 2023 |archive-date=28 July 2023 |archive-url=https://web.archive.org/web/20230728151121/https://journals.sagepub.com/doi/10.1177/13591053231172288 |url-status=live }}</ref> | |||
| The dosage of ] for women with fibromyalgia was studied in a 2022 ].<ref name="daSilva2022">{{cite journal | vauthors = da Silva JM, de Barros BS, Almeida GJ, O'Neil J, Imoto AM | title = Dosage of resistance exercises in fibromyalgia: evidence synthesis for a systematic literature review up-date and meta-analysis | journal = Rheumatology International | volume = 42 | issue = 3 | pages = 413–429 | date = March 2022 | pmid = 34652480 | doi = 10.1007/s00296-021-05025-9 | s2cid = 238991065 }}</ref> Effective dosages were found when exercising twice a week, for at least eight weeks. Symptom improvement was found for even low dosages such as 1–2 sets of 4–20 repetitions.<ref name="daSilva2022" /> Most studies use moderate ] of 40% to 85% ]. This intensity was effective in reducing pain.<ref name="daSilva2022" /> Some treatment regimes increase the intensity over time (from 40% to 80%), whereas others increase it when the participant can perform 12 repetitions.<ref name="daSilva2022" /> High-intensity exercises may cause lower ]. | |||
| ==== Meditative ==== | |||
| A 2021 ] found that ] exercise programs (], ], ]) were superior to other forms of exercise (], ], ]) in improving ] quality.<ref name=Estevez2021/> Other meta-analyses also found positive effects of tai chi for sleep,<ref>{{cite journal | vauthors = Li H, Chen J, Xu G, Duan Y, Huang D, Tang C, Liu J | title = The Effect of Tai Chi for Improving Sleep Quality: A Systematic Review and Meta-analysis | journal = Journal of Affective Disorders | volume = 274 | pages = 1102–1112 | date = September 2020 | pmid = 32663938 | doi = 10.1016/j.jad.2020.05.076 | s2cid = 219743962 }}</ref> fibromyalgia symptoms,<ref>{{cite journal | vauthors = Vasileios P, Styliani P, Nifon G, Pavlos S, Aris F, Ioannis P | title = Managing fibromyalgia with complementary and alternative medical exercise: a systematic review and meta-analysis of clinical trials | journal = Rheumatology International | volume = 42 | issue = 11 | pages = 1909–1923 | date = November 2022 | pmid = 35796820 | doi = 10.1007/s00296-022-05151-y | s2cid = 250317143 }}</ref> and pain, fatigue, depression and quality of life.<ref>{{cite journal | vauthors = Cheng CA, Chiu YW, Wu D, Kuan YC, Chen SN, Tam KW | title = Effectiveness of Tai Chi on fibromyalgia patients: A meta-analysis of randomized controlled trials | journal = Complementary Therapies in Medicine | volume = 46 | pages = 1–8 | date = October 2019 | pmid = 31519264 | doi = 10.1016/j.ctim.2019.07.007 | s2cid = 199039433 }}</ref> These tai chi interventions frequently included 1-hour sessions practiced 1-3 times a week for 12 weeks. Meditative exercises, as a whole, may achieve desired outcomes through biological mechanisms such as ], ], reduction in ] activity and modulation of ] sensitivity.<ref name="El-Shewy-2019" /> | |||
| ==== Aquatic ==== | |||
| Several reviews and meta-analyses suggest that aquatic training can improve symptoms and wellness in people with fibromyalgia.<ref>{{cite journal | vauthors = Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, Richards RS, Rader T | display-authors = 6 | title = Aquatic exercise training for fibromyalgia | journal = The Cochrane Database of Systematic Reviews | issue = 10 | pages = CD011336 | date = October 2014 | volume = 2014 | pmid = 25350761 | doi = 10.1002/14651858.cd011336 | pmc = 10638613 }}</ref><ref>{{cite journal | vauthors = Lima TB, Dias JM, Mazuquin BF, da Silva CT, Nogueira RM, Marques AP, Lavado EL, Cardoso JR | display-authors = 6 | title = The effectiveness of aquatic physical therapy in the treatment of fibromyalgia: a systematic review with meta-analysis | journal = Clinical Rehabilitation | volume = 27 | issue = 10 | pages = 892–908 | date = October 2013 | pmid = 23818412 | doi = 10.1177/0269215513484772 | s2cid = 25701866 }}</ref><ref>{{cite journal | vauthors = Perraton L, Machotka Z, Kumar S | title = Components of effective randomized controlled trials of hydrotherapy programs for fibromyalgia syndrome: A systematic review | journal = Journal of Pain Research | volume = 2 | pages = 165–173 | date = November 2009 | pmid = 21197303 | pmc = 3004626 | doi = 10.2147/JPR.S8052 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Galvão-Moreira LV, de Castro LO, Moura EC, de Oliveira CM, Nogueira Neto J, Gomes LM, Leal PD | title = Pool-based exercise for amelioration of pain in adults with fibromyalgia syndrome: A systematic review and meta-analysis | journal = Modern Rheumatology | volume = 31 | issue = 4 | pages = 904–911 | date = July 2021 | pmid = 32990113 | doi = 10.1080/14397595.2020.1829339 | s2cid = 222167851 }}</ref><ref name="Calles Plata-2023">{{cite journal | vauthors = Calles Plata I, Ortiz-Rubio A, Torres Sánchez I, Cabrera Martos I, Calvache Mateo A, Heredia-Ciuró A, Valenza MC | title = Effectiveness of aquatic therapy on sleep in persons with fibromyalgia. A meta-analysis | journal = Sleep Medicine | volume = 102 | pages = 76–83 | date = February 2023 | pmid = 36603514 | doi = 10.1016/j.sleep.2022.12.016 | s2cid = 255217819 }}</ref><ref>{{cite journal | vauthors = Ma J, Zhang T, Li X, Chen X, Zhao Q | title = Effects of aquatic physical therapy on clinical symptoms, physical function, and quality of life in patients with fibromyalgia: A systematic review and meta-analysis | journal = Physiotherapy Theory and Practice | pages = 205–223 | date = September 2022 | volume = 40 | issue = 2 | pmid = 36062580 | doi = 10.1080/09593985.2022.2119906 | s2cid = 252079586 }}</ref> It is recommended to practice aquatic therapy at least twice a week using a low to moderate intensity.<ref name="Calles Plata-2023" /> However, ] does not appear to be superior to other types of exercise.<ref>{{Cite journal |last1=Correyero-León |first1=Marta |last2=Medrano-de-la-Fuente |first2=Ricardo |last3=Hernando-Garijo |first3=Ignacio |last4=Jiménez-Del-Barrio |first4=Sandra |last5=Hernández-Lázaro |first5=Héctor |last6=Ceballos-Laita |first6=Luis |last7=Mingo-Gómez |first7=María Teresa |date=July 2023 |title=Effectiveness of aquatic training based on aerobic and strengthening exercises in patients with fibromyalgia: systematic review with meta-analysis |url=https://linkinghub.elsevier.com/retrieve/pii/S1550830723001623 |journal=Explore |volume=20 |issue=1 |pages=27–38 |language=en |doi=10.1016/j.explore.2023.07.003|pmid=37460329 |s2cid=259580881 }}</ref> | |||
| ==== Other ==== | |||
| Limited evidence suggests ] in combination with exercise may improve pain, fatigue, and stiffness.<ref>{{cite journal | vauthors = Bidonde J, Busch AJ, van der Spuy I, Tupper S, Kim SY, Boden C | title = Whole body vibration exercise training for fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 2017 | issue = 9 | pages = CD011755 | date = September 2017 | pmid = 28950401 | pmc = 6483692 | doi = 10.1002/14651858.cd011755.pub2 }}</ref> | |||
| === Medications === | |||
| A few countries have published guidelines for the management and treatment of fibromyalgia. As of 2018, all of them emphasize that medications are not required. However, medications, though imperfect, continue to be a component of treatment strategy for fibromyalgia patients. The ] guidelines outlined parameters for drug therapy termination and recommended considering ]s after six months.<ref name=Hauser2018/> | |||
| ] and the US ] (FDA) have approved ]<ref name="FDAFibro">{{cite press release |url=https://www.fda.gov/bbs/topics/NEWS/2007/NEW01656.html |title=FDA Approves First Drug for Treating Fibromyalgia |publisher=U.S. ] |date=21 June 2007 |access-date=14 January 2008 |url-status=live |archive-url=https://web.archive.org/web/20080221172848/https://www.fda.gov/bbs/topics/NEWS/2007/NEW01656.html |archive-date=21 February 2008 }}</ref> (an ]) and ] (a ]) for the management of fibromyalgia. The FDA also approved ] (another ]), but the ] refused marketing authority.<ref name="Doc. Ref.: EMA/814249/2009">{{cite web |last=European Medicines Agency |title=Questions and answers on the recommendation for the refusal of the marketing authorisation for Milnacipran Pierre Fabre Médicament/Impulsor |url=http://www.ema.europa.eu/docs/en_GB/document_library/Summary_of_opinion_-_Initial_authorisation/human/001034/WC500089875.pdf |publisher=European Medicines Agency |access-date=30 May 2013 |url-status=live |archive-url=https://web.archive.org/web/20140222154105/http://www.ema.europa.eu/docs/en_GB/document_library/Summary_of_opinion_-_Initial_authorisation/human/001034/WC500089875.pdf |archive-date=22 February 2014 }}</ref> | |||
| The medications ], ], or ] have been approved by the US ] (FDA) for the management of fibromyalgia.<ref name="pmid38355316">{{cite journal |vauthors=Martinez JE, Guimarães I |title="Fibromyalgia - are there any new approaches?" |journal=Best Pract Res Clin Rheumatol |volume= |issue= |pages=101933 |date=February 2024 |pmid=38355316 |doi=10.1016/j.berh.2024.101933 }}</ref> | |||
| ====Antidepressants==== | |||
| ]s are one of the common drugs for fibromyalgia. A 2021 meta-analysis concluded that antidepressants can improve the quality of life for fibromyalgia patients in the medium term.<ref name="Mascarenhas-2021">{{cite journal | vauthors = Mascarenhas RO, Souza MB, Oliveira MX, Lacerda AC, Mendonça VA, Henschke N, Oliveira VC | title = Association of Therapies With Reduced Pain and Improved Quality of Life in Patients With Fibromyalgia: A Systematic Review and Meta-analysis | journal = JAMA Internal Medicine | volume = 181 | issue = 1 | pages = 104–112 | date = January 2021 | pmid = 33104162 | pmc = 7589080 | doi = 10.1001/jamainternmed.2020.5651 }}</ref> For most people with fibromyalgia, the potential benefits of treatment with the serotonin and norepinephrine reuptake inhibitors duloxetine and milnacipran and the tricyclic antidepressants, such as amitriptyline, are outweighed by significant adverse effects (more adverse effects than benefits), however, a small number of people may experience relief from symptoms with these medications.<ref name="Häuser-2012">{{cite journal |vauthors=Häuser W, Wolfe F, Tölle T, Uçeyler N, Sommer C |date=April 2012 |title=The role of antidepressants in the management of fibromyalgia syndrome: a systematic review and meta-analysis |journal=CNS Drugs |volume=26 |issue=4 |pages=297–307 |doi=10.2165/11598970-000000000-00000 |pmid=22452526 |s2cid=207301478}}</ref><ref>{{cite journal |vauthors=Cording M, Derry S, Phillips T, Moore RA, Wiffen PJ |date=October 2015 |title=Milnacipran for pain in fibromyalgia in adults |journal=The Cochrane Database of Systematic Reviews |volume=2015 |issue=10 |pages=CD008244 |doi=10.1002/14651858.CD008244.pub3 |pmc=6481368 |pmid=26482422}}</ref><ref name="Welsch2018">{{cite journal |vauthors=Welsch P, Üçeyler N, Klose P, Walitt B, Häuser W |date=February 2018 |title=Serotonin and noradrenaline reuptake inhibitors (SNRIs) for fibromyalgia |journal=The Cochrane Database of Systematic Reviews |volume=2 |issue=2 |pages=CD010292 |doi=10.1002/14651858.CD010292.pub2 |pmc=5846183 |pmid=29489029}}</ref> | |||
| The length of time that antidepressant medications take to be effective at reducing symptoms can vary. Any potential benefits from the antidepressant amitriptyline may take up to three months to take effect and it may take between three and six months for duloxetine, milnacipran, and pregabalin to be effective at improving symptoms.<ref>{{cite journal |vauthors=Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ |date=May 2019 |title=Amitriptyline for fibromyalgia in adults |journal=The Cochrane Database of Systematic Reviews |volume=5 |issue=7 |pages=CD011824 |doi=10.1002/14651858.CD011824 |pmc=6485478 |pmid=35658166}}</ref> Some medications have the potential to cause withdrawal symptoms when stopping so gradual discontinuation may be warranted particularly for antidepressants and pregabalin.<ref name="pmid19623319" /> | |||
| ===== Serotonin and norepinephrine reuptake inhibitors ===== | |||
| A 2023 meta-analysis found that duloxetine improved fibromyalgia symptoms, regardless of the dosage.<ref>{{Cite journal |last1=Migliorini |first1=Filippo |last2=Maffulli |first2=Nicola |last3=Eschweiler |first3=Jörg |last4=Baroncini |first4=Alice |last5=Bell |first5=Andreas |last6=Colarossi |first6=Giorgia |date=2023-07-17 |title=Duloxetine for fibromyalgia syndrome: a systematic review and meta-analysis |journal=Journal of Orthopaedic Surgery and Research |language=en |volume=18 |issue=1 |page=504 |doi=10.1186/s13018-023-03995-z |issn=1749-799X |pmc=10351165 |pmid=37461044 |doi-access=free }}</ref> SSRIs may be also be used to treat depression in people diagnosed with fibromyalgia.<ref>{{cite journal | vauthors = Walitt B, Urrútia G, Nishishinya MB, Cantrell SE, Häuser W | title = Selective serotonin reuptake inhibitors for fibromyalgia syndrome | journal = The Cochrane Database of Systematic Reviews | volume = 2015 | issue = 6 | pages = CD011735 | date = June 2015 | pmid = 26046493 | pmc = 4755337 | doi = 10.1002/14651858.cd011735 }}</ref> | |||
| ===== Tricyclic antidepressants ===== | |||
| While amitriptyline has been used as a first-line treatment, the quality of evidence to support this use and comparison between different medications is poor.<ref name="Moore2015">{{cite journal |vauthors=Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ |date=July 2015 |title=Amitriptyline for neuropathic pain in adults |journal=The Cochrane Database of Systematic Reviews |volume=2015 |issue=7 |pages=CD008242 |doi=10.1002/14651858.CD011824 |pmc=6485478 |pmid=26146793}}</ref><ref name="Welsch2018" /> Very weak evidence indicates that a very small number of people may benefit from treatment with the ] ], however, for most, the potential benefits are not great and the risk of adverse effects and potential harm outweighs any potential for benefit.<ref>{{cite journal |vauthors=Welsch P, Bernardy K, Derry S, Moore RA, Häuser W |date=August 2018 |title=Mirtazapine for fibromyalgia in adults |journal=The Cochrane Database of Systematic Reviews |volume=8 |issue=8 |pages=CD012708 |doi=10.1002/14651858.CD012708.pub2 |pmc=6513659 |pmid=30080242}}</ref> As of 2018, the only ] that has sufficient evidence is ].<ref name="Hauser2018" /><ref name="Moore2015" /> | |||
| ===== Monoamine oxidase inhibitors ===== | |||
| Tentative evidence suggests that ]s (MAOIs) such as ] and ] are moderately effective for reducing pain.<ref name=Tort2012>{{cite journal | vauthors = Tort S, Urrútia G, Nishishinya MB, Walitt B | title = Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome | journal = The Cochrane Database of Systematic Reviews | issue = 4 | pages = CD009807 | date = April 2012 | pmid = 22513976 | doi = 10.1002/14651858.cd009807 }}</ref> Very low-quality evidence suggests pirlindole as more effective at treating pain than moclobemide.<ref name=Tort2012/> Side effects of MAOIs may include nausea and vomiting.<ref name=Tort2012/> | |||
| ====Central nervous system depressants==== | |||
| Central nervous system depressants include drug categories such as sedatives, tranquilizers, and hypnotics. A 2021 meta-analysis concluded that such drugs can improve the quality of life for fibromyalgia patients in the medium term.<ref name="Mascarenhas-2021"/> | |||
| ====Anti-seizure medication==== | ====Anti-seizure medication==== | ||
| The anti-convulsant medications ] and ] may be used to reduce pain.<ref name=Coch2017Gab>{{cite journal | vauthors = Cooper TE, Derry S, Wiffen PJ, Moore RA | title = Gabapentin for fibromyalgia pain in adults | journal = The Cochrane Database of Systematic Reviews | volume = 1 | issue = 1 | pages = CD012188 | date = January 2017 | pmid = 28045473 | pmc = 6465053 | doi = 10.1002/14651858.CD012188.pub2 }}</ref> There is tentative evidence that gabapentin may be of benefit for pain in about 18% of people with fibromyalgia.<ref name=Coch2017Gab/> It is not possible to predict who will benefit, and a short trial may be recommended to test the effectiveness of this type of medication. Approximately 6/10 people who take gabapentin to treat pain related to fibromyalgia experience unpleasant side effects such as dizziness, abnormal walking, or swelling from fluid accumulation.<ref>{{cite journal | vauthors = Wiffen PJ, Derry S, Bell RF, Rice AS, Tölle TR, Phillips T, Moore RA | title = Gabapentin for chronic neuropathic pain in adults | journal = The Cochrane Database of Systematic Reviews | volume = 6 | issue = 6 | pages = CD007938 | date = June 2017 | pmid = 28597471 | pmc = 6452908 | doi = 10.1002/14651858.CD007938.pub4 }}</ref> Pregabalin demonstrates a benefit in about 9% of people.<ref>{{cite journal | vauthors = Derry S, Cording M, Wiffen PJ, Law S, Phillips T, Moore RA | title = Pregabalin for pain in fibromyalgia in adults | journal = The Cochrane Database of Systematic Reviews | volume = 9 | issue = 9 | pages = CD011790 | date = September 2016 | pmid = 27684492 | pmc = 6457745 | doi = 10.1002/14651858.CD011790.pub2 }}</ref> Pregabalin reduced time off work by 0.2 days per week.<ref name="Straube2011">{{cite journal | vauthors = Straube S, Moore RA, Paine J, Derry S, Phillips CJ, Hallier E, McQuay HJ | title = Interference with work in fibromyalgia: effect of treatment with pregabalin and relation to pain response | journal = BMC Musculoskeletal Disorders | volume = 12 | pages = 125 | date = June 2011 | pmid = 21639874 | pmc = 3118156 | doi = 10.1186/1471-2474-12-125 | doi-access = free }}</ref> | |||
| The anti-seizure drugs ] (Neurontin)<ref name=pmid17393438>{{cite journal |author=Arnold LM, Goldenberg DL, Stanford SB, ''et al.'' |title=Gabapentin in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled, multicenter trial |journal=Arthritis Rheum. |volume=56 |issue=4 |pages=1336–44 |year=2007 |month=April |pmid=17393438 |doi=10.1002/art.22457 |accessdate=2008-05-21}}</ref> and ] (Lyrica) have been tested. Gabapentin is approved for use in treatment of neuropathic pain but not fibromyalgia. Pregabalin, originally labeled for the treatment of nerve pain suffered by diabetics, has been cleared by the US ] for treatment of fibromyalgia.<ref name="FDAFibro">{{cite press release | url = http://www.fda.gov/bbs/topics/NEWS/2007/NEW01656.html | title = FDA Approves First Drug for Treating Fibromyalgia | publisher = U.S. ] | date = ] ] | accessdate = 2008-01-14}}</ref> A ] of ] 450 mg/day found that 6 patients is the ] for one patient to have a 50% reduction in pain.<ref name=pmid15818684>{{cite journal |author=Crofford LJ, Rowbotham MC, Mease PJ, ''et al.'' |title=Pregabalin for the treatment of fibromyalgia syndrome: results of a randomized, double-blind, placebo-controlled trial |journal=Arthritis Rheum. |volume=52 |issue=4 |pages=1264–73 |year=2005 |pmid=15818684 |doi=10.1002/art.20983}}</ref> A Cochrane Database analysis of pregabalin use in chronic pain concluded that “A minority of patients will have substantial benefit with pregabalin, and more will have moderate benefit. Many will have no or trivial benefit, or will discontinue because of adverse events.”<ref> Moore RA, Straube S, Wiffen PJ, Derry S, McQuay HJ. Pregabalin for acute and chronic pain in adults. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No.: CD007076. DOI: 10.1002/14651858.CD007076.pub2</ref> | |||
| ==== |
==== Cannabinoids ==== | ||
| ]s may have some benefits for people with fibromyalgia. However, as of 2022, the data on the topic is still limited.<ref>{{cite journal | vauthors = Nowell WB, Gavigan K, L Silverman S | title = Cannabis for Rheumatic Disease Pain: a Review of Current Literature | journal = Current Rheumatology Reports | volume = 24 | issue = 5 | pages = 119–131 | date = May 2022 | pmid = 35486218 | doi = 10.1007/s11926-022-01065-7 | s2cid = 248423563 }}</ref><ref>{{cite journal | vauthors = Boehnke KF, Häuser W, Fitzcharles MA | title = Cannabidiol (CBD) in Rheumatic Diseases (Musculoskeletal Pain) | journal = Current Rheumatology Reports | volume = 24 | issue = 7 | pages = 238–246 | date = July 2022 | pmid = 35503198 | pmc = 9062628 | doi = 10.1007/s11926-022-01077-3 }}</ref><ref>{{cite journal | vauthors = Bourke SL, Schlag AK, O'Sullivan SE, Nutt DJ, Finn DP | title = Cannabinoids and the endocannabinoid system in fibromyalgia: A review of preclinical and clinical research | journal = Pharmacology & Therapeutics | volume = 240 | pages = 108216 | date = December 2022 | pmid = 35609718 | doi = 10.1016/j.pharmthera.2022.108216 | s2cid = 248973512 | doi-access = free }}</ref> Cannabinoids may also have adverse effects and may negatively interact with common rheumatological drugs.<ref>{{cite journal | vauthors = Jain N, Moorthy A | title = Cannabinoids in rheumatology: Friend, foe or a bystander? | journal = Musculoskeletal Care | volume = 20 | issue = 2 | pages = 416–428 | date = June 2022 | pmid = 35476898 | pmc = 9322323 | doi = 10.1002/msc.1636 }}</ref> | |||
| ] (e.g. ] (Mirapex) and ] (ReQuip) resulted in some improvement in a minority of patients,<ref name=pmid16052595/> but numerous side effects, including the onset of impulse control disorders like compulsive gambling and shopping, have led to concern about this approach.<ref>J Gambl Stud. 2009 Feb 25. Impulse Control Disorder Behaviors Associated with Pramipexole Used to Treat Fibromyalgia. Holman AJ</ref> A trial of transdermal ] is currently ongoing.<ref></ref> | |||
| ====Opioids==== | |||
| ===Investigational medications=== | |||
| The use of opioids is controversial. As of 2015, no opioid is approved for use in this condition by the FDA.<ref name="Mac2015" /> A 2016 ] concluded that there is no good evidence to support or refute the suggestion that ], alone or in combination with ], reduces pain in fibromyalgia.<ref>{{cite journal | vauthors = Gaskell H, Moore RA, Derry S, Stannard C | title = Oxycodone for pain in fibromyalgia in adults | journal = The Cochrane Database of Systematic Reviews | volume = 2016 | issue = 9 | pages = CD012329 | date = September 2016 | pmid = 27582266 | pmc = 6457853 | doi = 10.1002/14651858.CD012329 | collaboration = Cochrane Pain, Palliative and Supportive Care Group }}</ref> The ] (NIAMS) in 2014 stated that there was a lack of evidence for opioids for most people.<ref name="NIH2014Tx">{{cite web |date=July 2014 |title=Questions and Answers about Fibromyalgia |url=http://www.niams.nih.gov/health_info/fibromyalgia/ |url-status=dead |archive-url=https://web.archive.org/web/20160315112712/http://www.niams.nih.gov/health_info/fibromyalgia/ |archive-date=15 March 2016 |access-date=15 March 2016 |website=NIAMS}}</ref> The ] in 2012 made no recommendation either for or against the use of weak ]s because of the limited amount of scientific research addressing their use in the treatment of fibromyalgia. They strongly advise against using strong opioids.<ref name="German" /> The ] in 2012 said that opioids, starting with a weak opioid like tramadol, can be tried but only for people with moderate to severe pain that is not well-controlled by non-opioid painkillers. They discourage the use of strong opioids and only recommend using them while they continue to provide improved pain and functioning. Healthcare providers should monitor people on opioids for ongoing effectiveness, side effects, and possible unwanted drug behaviors.<ref name="Canadian" /> | |||
| A 2015 review found fair evidence to support tramadol use if other medications do not work.<ref name="Mac2015">{{cite journal | vauthors = MacLean AJ, Schwartz TL | title = Tramadol for the treatment of fibromyalgia | journal = Expert Review of Neurotherapeutics | volume = 15 | issue = 5 | pages = 469–475 | date = May 2015 | pmid = 25896486 | doi = 10.1586/14737175.2015.1034693 | s2cid = 26613022 }}</ref> A 2018 review found little evidence to support the combination of ] (acetaminophen) and tramadol over a single medication.<ref>{{cite journal | vauthors = Thorpe J, Shum B, Moore RA, Wiffen PJ, Gilron I | title = Combination pharmacotherapy for the treatment of fibromyalgia in adults | journal = The Cochrane Database of Systematic Reviews | volume = 2 | issue = 2 | pages = CD010585 | date = February 2018 | pmid = 29457627 | pmc = 6491103 | doi = 10.1002/14651858.CD010585.pub2 }}</ref> Goldenberg ''et al'' suggest that tramadol works via its serotonin and norepinephrine reuptake inhibition, rather than via its action as a weak opioid receptor agonist.<ref name="Don2016">{{cite journal | vauthors = Goldenberg DL, Clauw DJ, Palmer RE, Clair AG | title = Opioid Use in Fibromyalgia: A Cautionary Tale | journal = Mayo Clinic Proceedings | volume = 91 | issue = 5 | pages = 640–648 | date = May 2016 | pmid = 26975749 | doi = 10.1016/j.mayocp.2016.02.002 | s2cid = 20228209 | doi-access = free | type = Review }}</ref> | |||
| Investigational medications include cannabinoids and the 5-HT3 receptor antagonist ].<ref>Wood PB, Holman AJ, Jones KD, "Novel pharmacotherapy for fibromyalgia." Expert Opin Investig Drugs. 2007 Jun;16(6):829-41.</ref> A controlled study of ] failed to demonstrate any benefits from this controversial treatment.<ref name=Bennett>{{cite journal |author=Bennett RM, De Garmo P, Clark SR |title=A Randomized, Prospective, 12 Month Study To Compare The Efficacy Of Guaifenesin Versus Placebo In The Management Of Fibromyalgia |journal=Arthritis and Rheumatism |volume=39 |pages=S212 |year=1996 |url=http://www.myalgia.com/guaif2.htm |format=reprint |doi=10.1002/art.1780391004}}<br/>Lay summary and report: | |||
| * {{cite web |author=Kristin Thorson |work=Fibromyalgia Network |title=Is One Placebo Better Than Another? – The Guaifenesin Story | |||
| |url=http://www.fmnetnews.com/resources-alert-product6.php |year=1997 |publisher=Fibromyalgia Network}}</ref> | |||
| A large study of US people with fibromyalgia found that between 2005 and 2007 37.4% were prescribed short-acting opioids and 8.3% were prescribed long-acting opioids,<ref name="pmid21303476">{{cite journal | vauthors = Ngian GS, Guymer EK, Littlejohn GO | title = The use of opioids in fibromyalgia | journal = International Journal of Rheumatic Diseases | volume = 14 | issue = 1 | pages = 6–11 | date = February 2011 | pmid = 21303476 | doi = 10.1111/j.1756-185X.2010.01567.x | s2cid = 29000267 }}</ref> with around 10% of those prescribed short-acting opioids using tramadol;<ref name="Berger">Berger A. In: EULAR; 2009:SAT0461</ref> and a 2011 Canadian study of 457 people with fibromyalgia found 32% used opioids and two-thirds of those used strong opioids.<ref name="Canadian" /> | |||
| ===Physical treatments=== | |||
| Studies have found exercise improves fitness and sleep and may reduce pain and fatigue in some people with fibromyalgia.<ref name=pmid12137713>{{cite journal |author=Busch A, Schachter CL, Peloso PM, Bombardier C |title=Exercise for treating fibromyalgia syndrome |journal=Cochrane database of systematic reviews (Online) |volume= |issue=3 |pages=CD003786 |year=2002 |pmid=12137713|doi=10.1002/14651858.CD003786}}</ref> Many patients find temporary relief by applying heat to painful areas. Those with access to ], ], or acupuncture may find them beneficial.<ref name=pmid10086765>{{cite journal |author=Berman BM, Ezzo J, Hadhazy V, Swyers JP |title=Is acupuncture effective in the treatment of fibromyalgia? |journal=The Journal of family practice |volume=48 |issue=3 |pages=213–8 |year=1999 |pmid=10086765 |doi=}}</ref> Most patients find exercise, even low intensity exercise to be extremely helpful.<ref name=pmid14770100>{{cite journal |author=Gowans SE, deHueck A |title=Effectiveness of exercise in management of fibromyalgia |journal=Current opinion in rheumatology |volume=16 |issue=2 |pages=138–42 |year=2004 |pmid=14770100|doi=10.1097/00002281-200403000-00012}}</ref> ] can also temporarily relieve pain due to fibromyalgia.<ref name=pmid12090649>{{cite journal |author=Gamber RG, Shores JH, Russo DP, Jimenez C, Rubin BR |title=Osteopathic manipulative treatment in conjunction with medication relieves pain associated with fibromyalgia syndrome: results of a randomized clinical pilot project |journal=The Journal of the American Osteopathic Association |volume=102 |issue=6 |pages=321–5 |year=2002 |pmid=12090649 |doi= |url=http://www.jaoa.org/cgi/reprint/102/6/321.pdf |format=PDF}}</ref> | |||
| ==== Topical treatment ==== | |||
| ===Psychological/behavioural therapies=== | |||
| Capsaicin has been suggested as a topical pain reliever. Preliminary results suggest that it may improve sleep quality and fatigue, but there are not enough studies to support this claim.<ref>{{cite journal | vauthors = Elijah J, Powell K, Smith MA | title = The Efficacy of Capsaicin on Sleep Quality and Fatigue in Fibromyalgia | journal = Journal of Pain & Palliative Care Pharmacotherapy | volume = 36 | issue = 2 | pages = 112–116 | date = June 2022 | pmid = 35471125 | doi = 10.1080/15360288.2022.2063468 | s2cid = 248389141 }}</ref> | |||
| ====Unapproved or unfounded==== | |||
| ] has been shown to alleviate fibromyalgic symptoms, although it is not curative. The greatest benefit occurs when CBT is used along with exercise.<ref name=Goldenberg2008/><ref name=Williams>{{cite journal | last=Williams| first=DA | title=Psychological and behavioural therapies in fibromyalgia and related syndromes. | journal= Best Pract Res Clin Rheumatol. | volume=17 | issue=4 | pages=649–65 |month=August| year=2003 | pmid=12849717 }}</ref> Self-management techniques such as pacing and stress management may also be helpful for some patients. {{Citation needed|date=June 2008}} Because the nature of fibromyalgia is not well understood, some physicians believe that it may be ] or ].<ref>{{cite book |last=Sarno|first=Dr. John E, et al.|authorlink=John E. Sarno| title=The Divided Mind: The Epidemic of Mindbody Disorders|publisher=ReganBooks|year=2006 |isbn=0-06-085178-3 |pages=21–2, 235–7, 264–5, 294–8, 315, 319–20, 363}}</ref> Accordingly, some doctors have claimed to have successfully treated fibromyalgia when a psychological cause is accepted.<ref>{{cite book |last=Leonard-Segal|first=Dr. Andrea| title=The Divided Mind: The Epidemic of Mindbody Disorders|chapter=A Rheumatologist's Experience With Psychosomatic Disorders|publisher=ReganBooks|year=2006 |isbn=0-06-085178-3 |pages=264–5 }}</ref> | |||
| ] increases growth hormone production levels through increased slow-wave sleep patterns. However, this medication was not approved by the FDA for the indication for use in people with fibromyalgia due to the concern for ].<ref>{{cite journal | vauthors = Staud R | title = Sodium oxybate for the treatment of fibromyalgia | journal = Expert Opinion on Pharmacotherapy | volume = 12 | issue = 11 | pages = 1789–1798 | date = August 2011 | pmid = 21679091 | doi = 10.1517/14656566.2011.589836 | s2cid = 33026097 }}</ref> | |||
| The muscle relaxants ], ] with acetaminophen and caffeine, and ] are sometimes used to treat fibromyalgia; however, as of 2015 they are not approved for this use in the United States.<ref>{{cite journal | vauthors = See S, Ginzburg R | title = Choosing a skeletal muscle relaxant | journal = American Family Physician | volume = 78 | issue = 3 | pages = 365–370 | date = August 2008 | pmid = 18711953 | url = http://www.aafp.org/afp/2008/0801/p365.html | url-status = live | archive-url = https://web.archive.org/web/20160401190043/http://www.aafp.org/afp/2008/0801/p365.html | archive-date = 1 April 2016 }}</ref><ref>{{cite book |title=Endotext |vauthors=Kaltsas G, Tsiveriotis K |publisher=MDText.com, Inc. |year=2000 |chapter=Fibromyalgia |pmid=25905317 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK279092/ |access-date=20 February 2017 |archive-date=6 August 2020 |archive-url=https://web.archive.org/web/20200806021142/https://www.ncbi.nlm.nih.gov/books/NBK279092/ |url-status=live }}</ref> The use of nonsteroidal anti-inflammatory drugs is not recommended as first-line therapy.<ref name="Heymann-">{{cite journal | vauthors = Heymann RE, Paiva ED, Helfenstein M, Pollak DF, Martinez JE, Provenza JR, Paula AP, Althoff AC, Souza EJ, Neubarth F, Lage LV, Rezende MC, de Assis MR, Lopes ML, Jennings F, Araújo RL, Cristo VV, Costa ED, Kaziyama HH, Yeng LT, Iamamura M, Saron TR, Nascimento OJ, Kimura LK, Leite VM, Oliveira J, de Araújo GT, Fonseca MC | display-authors = 6 | title = Brazilian consensus on the treatment of fibromyalgia | journal = Revista Brasileira de Reumatologia | volume = 50 | issue = 1 | pages = 56–66 | year = 2010 | pmid = 21125141 | doi = 10.1590/S0482-50042010000100006 | doi-access = free }}</ref> Moreover, nonsteroidal anti-inflammatory drugs cannot be considered as useful in the management of fibromyalgia.<ref>{{cite journal | vauthors = Derry S, Wiffen PJ, Häuser W, Mücke M, Tölle TR, Bell RF, Moore RA | title = Oral nonsteroidal anti-inflammatory drugs for fibromyalgia in adults | journal = The Cochrane Database of Systematic Reviews | volume = 3 | issue = 3 | pages = CD012332 | date = March 2017 | pmid = 28349517 | pmc = 6464559 | doi = 10.1002/14651858.CD012332.pub2 }}</ref> | |||
| Very low-quality evidence suggests ] may be effective in fibromyalgia.<ref>{{cite journal | vauthors = Walitt B, Klose P, Üçeyler N, Phillips T, Häuser W | title = Antipsychotics for fibromyalgia in adults | journal = The Cochrane Database of Systematic Reviews | volume = 2016 | issue = 6 | pages = CD011804 | date = June 2016 | pmid = 27251337 | pmc = 6457603 | doi = 10.1002/14651858.cd011804.pub2 }}</ref> | |||
| No high-quality evidence exists that suggests synthetic ] (]) helps with fibromyalgia.<ref>{{cite journal | vauthors = Walitt B, Klose P, Fitzcharles MA, Phillips T, Häuser W | title = Cannabinoids for fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 7 | issue = 7 | pages = CD011694 | date = July 2016 | pmid = 27428009 | pmc = 6457965 | doi = 10.1002/14651858.cd011694.pub2 }}</ref> | |||
| ===Nutrition and dietary supplements=== | |||
| Nutrition is related to fibromyalgia in several ways. Some nutritional risk factors for fibromyalgia complications are obesity, nutritional deficiencies, food allergies, and consuming food additives.<ref name="Kadayifci-2022">{{cite journal | vauthors = Kadayifci FZ, Bradley MJ, Onat AM, Shi HN, Zheng S | title = Review of nutritional approaches to fibromyalgia | journal = Nutrition Reviews | volume = 80 | issue = 12 | pages = 2260–2274 | date = November 2022 | pmid = 35674686 | doi = 10.1093/nutrit/nuac036 }}</ref> The consumption of fruits and vegetables, low-processed foods, high-quality proteins, and healthy fats may have some benefits.<ref name="Kadayifci-2022" /> Low-quality evidence found some benefits of a vegetarian or ] diet.<ref>{{cite journal | vauthors = Nadal-Nicolás Y, Miralles-Amorós L, Martínez-Olcina M, Sánchez-Ortega M, Mora J, Martínez-Rodríguez A | title = Vegetarian and Vegan Diet in Fibromyalgia: A Systematic Review | journal = International Journal of Environmental Research and Public Health | volume = 18 | issue = 9 | pages = 4955 | date = May 2021 | pmid = 34066603 | pmc = 8125538 | doi = 10.3390/ijerph18094955 | doi-access = free }}</ref> | |||
| Although ]s have been widely investigated concerning fibromyalgia, most of the evidence, as of 2021, is of poor quality. It is therefore difficult to reach conclusive recommendations.<ref>{{cite journal | vauthors = Haddad HW, Mallepalli NR, Scheinuk JE, Bhargava P, Cornett EM, Urits I, Kaye AD | title = The Role of Nutrient Supplementation in the Management of Chronic Pain in Fibromyalgia: A Narrative Review | journal = Pain and Therapy | volume = 10 | issue = 2 | pages = 827–848 | date = December 2021 | pmid = 33909266 | pmc = 8586285 | doi = 10.1007/s40122-021-00266-9 }}</ref> It appears that ] and ] supplements can reduce pain and improve quality of life for fibromyalgia patients.<ref name="Ibáñez-Vera-2018">{{Cite journal| vauthors = Ibáñez-Vera AJ, Alvero-Cruz JR, García-Romero JC |date=2018|title=Therapeutic physical exercise and supplements to treat fibromyalgia |journal=Apunts. Medicina de l'Esport|volume=53|issue=197|pages=33–41|doi=10.1016/j.apunts.2017.07.001}}</ref><ref name="The efficacy of vitamin D in treatm">{{cite journal | vauthors = Qu K, Li MX, Zhou YL, Yu P, Dong M | title = The efficacy of vitamin D in treatment of fibromyalgia: a meta-analysis of randomized controlled studies and systematic review | journal = Expert Review of Clinical Pharmacology | volume = 15 | issue = 4 | pages = 433–442 | date = April 2022 | pmid = 35596576 | doi = 10.1080/17512433.2022.2081151 | s2cid = 248948241 }}</ref> Q10 coenzyme has beneficial effects on ] in fibromyalgia patients, with most studies using doses of 300 mg per day for three months.<ref>{{cite journal | vauthors = Mehrabani S, Askari G, Miraghajani M, Tavakoly R, Arab A | title = Effect of coenzyme Q10 supplementation on fatigue: A systematic review of interventional studies | journal = Complementary Therapies in Medicine | volume = 43 | pages = 181–187 | date = April 2019 | pmid = 30935528 | doi = 10.1016/j.ctim.2019.01.022 | s2cid = 86467031 }}</ref> Q10 coenzyme is hypothesized to improve mitochondrial activity and decrease inflammation.<ref>{{cite book | vauthors = Hargreaves IP, Mantle D | title = Reviews on New Drug Targets in Age-Related Disorders | chapter = Targeted Treatment of Age-Related Fibromyalgia with Supplemental Coenzyme Q10 | series = Advances in Experimental Medicine and Biology | volume = 1286 | pages = 77–85 | date = 2021 | pmid = 33725346 | doi = 10.1007/978-3-030-55035-6_5 | publisher = Springer International Publishing | isbn = 978-3-030-55034-9 | veditors = Guest PC | s2cid = 232261388 | chapter-url = https://researchonline.ljmu.ac.uk/id/eprint/14740/2/Targeted%20treatment%20of%20age-related%20fibromyalgia%20with%20supplemental%20coenzyme%20Q10.pdf | place = Cham | access-date = 17 May 2023 | archive-date = 30 May 2023 | archive-url = https://web.archive.org/web/20230530112702/https://researchonline.ljmu.ac.uk/id/eprint/14740/2/Targeted%20treatment%20of%20age-related%20fibromyalgia%20with%20supplemental%20coenzyme%20Q10.pdf | url-status = live }}</ref> Vitamin D has been shown to improve some fibromyalgia measures, but not others.<ref name="The efficacy of vitamin D in treatm"/><ref>{{cite journal | vauthors = Erkilic B, Dalgic GS | title = The preventive role of vitamin D in the prevention and management of Fibromyalgia syndrome | journal = Nutrition and Health | pages = 223–229 | date = January 2023 | volume = 29 | issue = 2 | pmid = 36591895 | doi = 10.1177/02601060221144801 | s2cid = 255471623 }}</ref> | |||
| Two ]s found that ] treatment has several positive effects on fibromyalgia patients, including the improvement of ], pain, and disease impact.<ref name=":2" /><ref>{{Cite journal |last1=de Carvalho |first1=Jozélio Freire |last2=Skare |first2=Thelma L. |date=2023 |title=Melatonin supplementation improves rheumatological disease activity: A systematic review |url=https://linkinghub.elsevier.com/retrieve/pii/S2405457723001043 |journal=Clinical Nutrition ESPEN |language=en |volume=55 |pages=414–419 |doi=10.1016/j.clnesp.2023.04.011 |pmid=37202076 |s2cid=258273314 |access-date=28 July 2023 |archive-date=5 January 2024 |archive-url=https://web.archive.org/web/20240105080412/https://linkinghub.elsevier.com/retrieve/pii/S2405457723001043 |url-status=live }}</ref> No major ] events were reported.<ref name=":2">{{cite journal | vauthors = Hemati K, Amini Kadijani A, Sayehmiri F, Mehrzadi S, Zabihiyeganeh M, Hosseinzadeh A, Mirzaei A | title = Melatonin in the treatment of fibromyalgia symptoms: A systematic review | journal = Complementary Therapies in Clinical Practice | volume = 38 | pages = 101072 | date = February 2020 | pmid = 31783341 | doi = 10.1016/j.ctcp.2019.101072 | s2cid = 208497324 }}</ref> | |||
| ===Psychotherapy=== | |||
| Due to the uncertainty about the pathogenesis of fibromyalgia, current treatment approaches focus on management of symptoms to improve quality of life,<ref>{{cite journal | vauthors = Arnold LM, Gebke KB, Choy EH | title = Fibromyalgia: management strategies for primary care providers | journal = International Journal of Clinical Practice | volume = 70 | issue = 2 | pages = 99–112 | date = February 2016 | pmid = 26817567 | pmc = 6093261 | doi = 10.1111/ijcp.12757 }}</ref> using integrated pharmacological and non-pharmacological approaches.<ref name="JAMA2014" /> There is no single intervention shown to be effective for all patients.<ref name="Management of fibromyalgia syndrome">{{cite journal | vauthors = Okifuji A, Hare BD | title = Management of fibromyalgia syndrome: review of evidence | journal = Pain and Therapy | volume = 2 | issue = 2 | pages = 87–104 | date = December 2013 | pmid = 25135147 | pmc = 4107911 | doi = 10.1007/s40122-013-0016-9 }}</ref> In a 2020 Cochrane review, ] was found to have a small but beneficial effect for reducing pain and distress but adverse events were not well evaluated.<ref>{{cite journal | vauthors = Williams AC, Fisher E, Hearn L, Eccleston C | title = Psychological therapies for the management of chronic pain (excluding headache) in adults | journal = The Cochrane Database of Systematic Reviews | volume = 8 | issue = 8 | pages = CD007407 | date = August 2020 | pmid = 32794606 | pmc = 7437545 | doi = 10.1002/14651858.CD007407.pub4 }}</ref> Cognitive behavioral therapy and related psychological and behavioural therapies have a small to moderate effect in reducing symptoms of fibromyalgia.<ref>{{cite journal | vauthors = Bernardy K, Klose P, Busch AJ, Choy EH, Häuser W | title = Cognitive behavioural therapies for fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 2013 | issue = 9 | pages = CD009796 | date = September 2013 | pmid = 24018611 | pmc = 6481397 | doi = 10.1002/14651858.CD009796.pub2 }}</ref><ref name="Glo2010">{{cite journal | vauthors = Glombiewski JA, Sawyer AT, Gutermann J, Koenig K, Rief W, Hofmann SG | title = Psychological treatments for fibromyalgia: a meta-analysis | journal = Pain | volume = 151 | issue = 2 | pages = 280–295 | date = November 2010 | pmid = 20727679 | doi = 10.1016/j.pain.2010.06.011 | s2cid = 10513179 }}</ref> Effect sizes tend to be small when cognitive behavioral therapy is used as a stand-alone treatment for patients with fibromyalgia, but these improve significantly when it is part of a wider multidisciplinary treatment program.<ref name="Glo2010" /> | |||
| A 2010 systematic review of 14 studies reported that cognitive behavioral therapy improves self-efficacy or coping with pain and reduces the number of physician visits at post-treatment, but has no significant effect on pain, fatigue, sleep, or health-related quality of life at post-treatment or follow-up. Depressed mood was also improved but this could not be distinguished from some risks of bias.<ref>{{cite journal | vauthors = Bernardy K, Füber N, Köllner V, Häuser W | title = Efficacy of cognitive-behavioral therapies in fibromyalgia syndrome - a systematic review and metaanalysis of randomized controlled trials | journal = The Journal of Rheumatology | volume = 37 | issue = 10 | pages = 1991–2005 | date = October 2010 | pmid = 20682676 | doi = 10.3899/jrheum.100104 | s2cid = 11357808 | doi-access = free }}</ref> A 2022 meta-analysis found that cognitive behavioral therapy reduces insomnia in people with chronic pain, including people with fibromyalgia.<ref name="Whale-2022">{{cite journal | vauthors = Whale K, Dennis J, Wylde V, Beswick A, Gooberman-Hill R | title = The effectiveness of non-pharmacological sleep interventions for people with chronic pain: a systematic review and meta-analysis | journal = BMC Musculoskeletal Disorders | volume = 23 | issue = 1 | pages = 440 | date = May 2022 | pmid = 35546397 | pmc = 9092772 | doi = 10.1186/s12891-022-05318-5 | doi-access = free }}</ref> ], a type of cognitive behavioral therapy, has also proven effective.<ref>{{Cite journal |last1=Eastwood |first1=Florence |last2=Godfrey |first2=Emma |date=2023-12-12 |title=The efficacy, acceptability and safety of acceptance and commitment therapy for fibromyalgia – a systematic review and meta-analysis |journal=British Journal of Pain |volume=18 |issue=3 |pages=243–256 |language=en |doi=10.1177/20494637231221451 |issn=2049-4637|doi-access=free |pmid=38751564 |pmc=11092929 }}</ref> | |||
| === Patient education === | |||
| Patient education is recommended by the ] (EULAR) as an important treatment component.<ref name="Macfarlane-2017" /> As of 2022, there is only low-quality evidence showing that patient education can decrease pain and fibromyalgia impact.<ref>{{cite journal | vauthors = Suso-Martí L, Cuenca-Martínez F, Alba-Quesada P, Muñoz-Alarcos V, Herranz-Gómez A, Varangot-Reille C, Domínguez-Navarro F, Casaña J | display-authors = 6 | title = Effectiveness of Pain Neuroscience Education in Patients with Fibromyalgia: A Systematic Review and Meta-Analysis | journal = Pain Medicine | volume = 23 | issue = 11 | pages = 1837–1850 | date = October 2022 | pmid = 35587171 | doi = 10.1093/pm/pnac077 }}</ref><ref>{{Cite journal |last1=Duhn |first1=Ph |last2=Wæhrens |first2=Ee |last3=Pedersen |first3=Mb |last4=Nielsen |first4=Sm |last5=Locht |first5=H |last6=Bliddal |first6=H |last7=Christensen |first7=R |last8=Amris |first8=K |date=2023-05-10 |title=Effectiveness of patient education as a stand-alone intervention for patients with chronic widespread pain and fibromyalgia: a systematic review and meta-analysis of randomized trials |url=https://www.tandfonline.com/doi/full/10.1080/03009742.2023.2192450 |journal=Scandinavian Journal of Rheumatology |volume=52 |issue=6 |language=en |pages=654–663 |doi=10.1080/03009742.2023.2192450 |pmid=37162478 |s2cid=258588927 |issn=0300-9742 |access-date=28 July 2023 |archive-date=28 July 2023 |archive-url=https://web.archive.org/web/20230728152030/https://www.tandfonline.com/doi/full/10.1080/03009742.2023.2192450 |url-status=live }}</ref> | |||
| ] interventions show low effectiveness in improving insomnia in people with chronic pain.<ref name="Whale-2022" /> | |||
| === Physical therapy === | |||
| Patients with chronic pain, including those with fibromyalgia, can benefit from techniques such as ], ], and ].<ref name=":5">{{Cite journal |last1=Navarro-Ledesma |first1=Santiago |last2=Hamed-Hamed |first2=Dina |last3=Gonzalez-Muñoz |first3=Ana |last4=Pruimboom |first4=Leo |date=2024 |title=Impact of physical therapy techniques and common interventions on sleep quality in patients with chronic pain: A systematic review |journal=Sleep Medicine Reviews |language=en |volume=76 |pages=101937 |doi=10.1016/j.smrv.2024.101937|doi-access=free |pmid=38669729 |hdl=10481/92720 |hdl-access=free }}</ref> These can lessen the experience of chronic pain and increase both the amount and quality of sleep. Patients' ] is also improved by decreasing pain mechanisms and increasing sleep quality, particularly during the ] phase, sleep efficiency, and alertness.<ref name=":5" /> | |||
| ==== Manual therapy ==== | |||
| A 2021 meta-analysis concluded that ] and ] diminish pain in the medium term.<ref name="Mascarenhas-2021" /> As of 2015, there was no good evidence for the benefit of other mind-body therapies.<ref name="coch-mb">{{cite journal | vauthors = Theadom A, Cropley M, Smith HE, Feigin VL, McPherson K | title = Mind and body therapy for fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 2015 | issue = 4 | pages = CD001980 | date = April 2015 | pmid = 25856658 | pmc = 8409283 | doi = 10.1002/14651858.CD001980.pub3 }}</ref> | |||
| ====Acupuncture==== | |||
| A 2013 review found moderate-level evidence on the usage of acupuncture with electrical stimulation for improvement of overall well-being. Acupuncture alone will not have the same effects, but will enhance the influence of exercise and medication in pain and stiffness.<ref>{{cite journal | vauthors = Deare JC, Zheng Z, Xue CC, Liu JP, Shang J, Scott SW, Littlejohn G | title = Acupuncture for treating fibromyalgia | journal = The Cochrane Database of Systematic Reviews | volume = 2013 | issue = 5 | pages = CD007070 | date = May 2013 | pmid = 23728665 | pmc = 4105202 | doi = 10.1002/14651858.CD007070.pub2 }}</ref> | |||
| === Electrical neuromodulation === | |||
| Several forms of electrical neuromodulation, including ] (TENS) and ] (tDCS), have been used to treat fibromyalgia. In general, they help reduce pain and depression and improve functioning.<ref>{{cite journal | vauthors = Cheng YC, Hsiao CY, Su MI, Chiu CC, Huang YC, Huang WL | title = Treating fibromyalgia with electrical neuromodulation: A systematic review and meta-analysis | journal = Clinical Neurophysiology | volume = 148 | pages = 17–28 | date = February 2023 | pmid = 36774784 | doi = 10.1016/j.clinph.2023.01.011 | s2cid = 256461558 }}</ref><ref>{{Cite journal |last1=Gikaro |first1=John Marwa |last2=Bigambo |first2=Francis Manyori |last3=Minde |first3=Victor Mark |last4=Swai |first4=Elia Asanterabi |date=2023-04-20 |title=Efficacy of electrophysical agents in fibromyalgia: A systematic review and network meta-analysis |url=http://journals.sagepub.com/doi/10.1177/02692155231170450 |journal=Clinical Rehabilitation |volume=37 |issue=10 |language=en |pages=1295–1310 |doi=10.1177/02692155231170450 |pmid=37082791 |s2cid=258258250 |issn=0269-2155 |access-date=28 July 2023 |archive-date=28 July 2023 |archive-url=https://web.archive.org/web/20230728153457/https://journals.sagepub.com/doi/10.1177/02692155231170450 |url-status=live }}</ref> | |||
| ==== Transcutaneous electrical nerve stimulation (TENS) ==== | |||
| Transcutaneous electrical nerve stimulation (TENS) is the delivery of pulsed electrical currents to the ] to stimulate ]. TENS is widely used to treat pain and is considered to be a low-cost, safe, and self-administered treatment.<ref>{{cite journal | vauthors = Johnson MI, Claydon LS, Herbison GP, Jones G, Paley CA | title = Transcutaneous electrical nerve stimulation (TENS) for fibromyalgia in adults | journal = The Cochrane Database of Systematic Reviews | volume = 2017 | issue = 10 | pages = CD012172 | date = October 2017 | pmid = 28990665 | pmc = 6485914 | doi = 10.1002/14651858.CD012172.pub2 | collaboration = Cochrane Pain, Palliative and Supportive Care Group }}</ref> As such, it is commonly recommended by clinicians to people suffering from pain.<ref name="Gibson-2019">{{cite journal | vauthors = Gibson W, Wand BM, Meads C, Catley MJ, O'Connell NE | title = Transcutaneous electrical nerve stimulation (TENS) for chronic pain - an overview of Cochrane Reviews | journal = The Cochrane Database of Systematic Reviews | volume = 4 | issue = 4 | pages = CD011890 | date = April 2019 | pmid = 30941745 | pmc = 6446021 | doi = 10.1002/14651858.CD011890.pub3 }}</ref> On 2019, an overview of eight ] was conducted, covering 51 TENS-related ]s.<ref name="Gibson-2019" /> The review concluded that the quality of the available evidence was insufficient to make any recommendations.<ref name="Gibson-2019" /> A later review concluded that transcutaneous electrical nerve stimulation may diminish pain in the short term, but there was uncertainty about the relevance of the results.<ref name="Mascarenhas-2021" /> | |||
| Preliminary findings suggest that electrically stimulating the ] through an implanted device can potentially reduce fibromyalgia symptoms.<ref name="Lange-2011">{{cite journal | vauthors = Lange G, Janal MN, Maniker A, Fitzgibbons J, Fobler M, Cook D, Natelson BH | title = Safety and efficacy of vagus nerve stimulation in fibromyalgia: a phase I/II proof of concept trial | journal = Pain Medicine | volume = 12 | issue = 9 | pages = 1406–1413 | date = September 2011 | pmid = 21812908 | pmc = 3173600 | doi = 10.1111/j.1526-4637.2011.01203.x }}</ref> However, there may be adverse reactions to the procedure.<ref name="Lange-2011" /> | |||
| ==== Noninvasive brain stimulation ==== | |||
| Noninvasive brain stimulation includes methods such as transcranial direct current stimulation and high-frequency repetitive ] (TMS). Both methods have been found to improve pain scores in ] and fibromyalgia.<ref>{{cite journal | vauthors = Gao C, Zhu Q, Gao Z, Zhao J, Jia M, Li T | title = Can noninvasive Brain Stimulation Improve Pain and Depressive Symptoms in Patients With Neuropathic Pain? A Systematic Review and Meta-Analysis | journal = Journal of Pain and Symptom Management | volume = 64 | issue = 4 | pages = e203–e215 | date = October 2022 | pmid = 35550165 | doi = 10.1016/j.jpainsymman.2022.05.002 | s2cid = 248715312 }}</ref> | |||
| A 2023 meta-analysis of 16 RCTs found that ] (tDCS) of over 4 weeks can decrease pain in patients with fibromyalgia.<ref>{{cite journal | vauthors = Teixeira PE, Pacheco-Barrios K, Branco LC, de Melo PS, Marduy A, Caumo W, Papatheodorou S, Keysor J, Fregni F | display-authors = 6 | title = The Analgesic Effect of Transcranial Direct Current Stimulation in Fibromyalgia: A Systematic Review, Meta-Analysis, and Meta-Regression of Potential Influencers of Clinical Effect | journal = Neuromodulation | pages = 715–727 | date = November 2022 | volume = 26 | issue = 4 | pmid = 36435660 | doi = 10.1016/j.neurom.2022.10.044 | pmc = 10203058 | s2cid = 253933442 }}</ref> | |||
| A 2021 meta-analysis of multiple intervention types concluded that magnetic field therapy and transcranial magnetic stimulation may diminish pain in the short-term, but conveyed an uncertainty about the relevance of the result.<ref name="Mascarenhas-2021" /> Several 2022 meta-analyses focusing on transcranial magnetic stimulation found positive effects on fibromyalgia.<ref>{{cite journal | vauthors = Fernandes AM, Graven-Nielsen T, de Andrade DC | title = New updates on transcranial magnetic stimulation in chronic pain | journal = Current Opinion in Supportive and Palliative Care | volume = 16 | issue = 2 | pages = 65–70 | date = June 2022 | pmid = 35639571 | doi = 10.1097/SPC.0000000000000591 | s2cid = 249208885 | url = https://vbn.aau.dk/da/publications/ff6d7a58-1cad-42a8-b36e-1a46384a7382 }}</ref><ref name="Choo-2022" /><ref name="Sun-2022" /> Repetitive transcranial magnetic stimulation improved pain in the short-term<ref name="Choo-2022" /><ref name="Sun-2022">{{cite journal | vauthors = Sun P, Fang L, Zhang J, Liu Y, Wang G, Qi R | title = Repetitive Transcranial Magnetic Stimulation for Patients with Fibromyalgia: A Systematic Review with Meta-Analysis | journal = Pain Medicine | volume = 23 | issue = 3 | pages = 499–514 | date = March 2022 | pmid = 34542624 | doi = 10.1093/pm/pnab276 }}</ref> and quality of life after 5–12 weeks.<ref name="Choo-2022" /><ref name="Sun-2022" /> Repetitive transcranial magnetic stimulation did not improve anxiety, depression, and fatigue.<ref name="Sun-2022" /> Transcranial magnetic stimulation to the left dorsolateral prefrontal cortex was also ineffective.<ref name="Choo-2022">{{cite journal | vauthors = Choo YJ, Kwak SG, Chang MC | title = Effectiveness of Repetitive Transcranial Magnetic Stimulation on Managing Fibromyalgia: A Systematic Meta-Analysis | journal = Pain Medicine | volume = 23 | issue = 7 | pages = 1272–1282 | date = July 2022 | pmid = 34983056 | doi = 10.1093/pm/pnab354 }}</ref> | |||
| ==== EEG neurofeedback ==== | |||
| A systematic review of ] for the treatment of fibromyalgia found most treatments showed significant improvements of the main symptoms of the disease.<ref name="pmid37179502">{{cite journal | vauthors= Torres CB, Barona E, Manso J | title=A systematic review of EEG neurofeedback in fibromyalgia to treat psychological variables, chronic pain and general health | journal=] | year=2023 | volume=274 | issue=4 | pages=981–999 | doi = 10.1007/s00406-023-01612-y | pmid=37179502| doi-access=free | pmc=11127810 }}</ref> However, the protocols were so different, and the lack of ] or randomization impede drawing conclusive results.<ref name="pmid37179502"/> | |||
| === Hyperbaric oxygen therapy === | |||
| ] (HBOT) has shown beneficial effects in treating chronic pain by reducing inflammation and oxidative stress.<ref name="pmid362464011"/> However, treating fibromyalgia with hyperbaric oxygen therapy is still controversial, in light of the scarcity of large-scale ].<ref name="El-Shewy-2019" /> In addition, hyperbaric oxygen therapy raises safety concerns due to the ] that may follow it.<ref name="El-Shewy-2019">{{cite journal | vauthors = El-Shewy KM, Kunbaz A, Gad MM, Al-Husseini MJ, Saad AM, Sammour YM, Abdel-Daim MM | title = Hyperbaric oxygen and aerobic exercise in the long-term treatment of fibromyalgia: A narrative review | journal = Biomedicine & Pharmacotherapy | volume = 109 | pages = 629–638 | date = January 2019 | pmid = 30399600 | doi = 10.1016/j.biopha.2018.10.157 | s2cid = 53240356 | doi-access = free }}</ref> An evaluation of nine trials with 288 patients in total found that HBOT was more effective at relieving fibromyalgia patients' pain than the control intervention. In most of the trials, HBOT improved sleep disturbance, multidimensional function, patient satisfaction, and tender spots. 24% of the patients experienced negative outcomes.<ref>{{cite journal | vauthors = Chen X, You J, Ma H, Zhou M, Huang C | title = Efficacy and safety of hyperbaric oxygen therapy for fibromyalgia: a systematic review and meta-analysis | journal = BMJ Open | volume = 13 | issue = 1 | pages = e062322 | date = January 2023 | pmid = 36690401 | pmc = 9872467 | doi = 10.1136/bmjopen-2022-062322 }}</ref> | |||
| ==Prognosis== | ==Prognosis== | ||
| Although neither degenerative nor fatal, the chronic pain of fibromyalgia is pervasive and persistent. Most |
Although in itself fibromyalgia is neither ] nor fatal, the ] of fibromyalgia is pervasive and persistent. Most people with fibromyalgia report that their symptoms do not improve over time. However, most patients learn to adapt to the symptoms over time. The ] guidelines for patients explain that: | ||
| # The symptoms of fibromyalgia are persistent in nearly all patients. | |||
| ==Epidemiology== | |||
| # Total relief of symptoms is seldom achieved. | |||
| Fibromyalgia is seen in about 2% of the general population<ref name=Chakrabarty>{{cite journal | last=Chakrabarty | first=S | coauthors=Zoorob R | title=Fibromyalgia | journal=American Family Physician | volume=76 | issue=2 | pages=247–254 |month=July | year=2007 | url=http://www.aafp.org/afp/20070715/247.html | pmid=17695569 | accessdate=2008-01-06 }}</ref> and affects more females than males, with a ratio of 9:1 by ACR criteria.<ref>{{eMedicine|med|790|Fibromyalgia}}</ref> It is most commonly diagnosed in individuals between the ages of 20 and 50, though onset can occur in childhood. | |||
| # The symptoms do not lead to ] and do not shorten ].<ref name=Fitz2013>{{cite journal | vauthors = Fitzcharles MA, Shir Y, Ablin JN, Buskila D, Amital H, Henningsen P, Häuser W | title = Classification and clinical diagnosis of fibromyalgia syndrome: recommendations of recent evidence-based interdisciplinary guidelines | journal = Evidence-Based Complementary and Alternative Medicine | volume = 2013 | pages = 528952 | date = 2013 | pmid = 24379886 | pmc = 3860136 | doi = 10.1155/2013/528952 | doi-access = free }}</ref> | |||
| An 11-year ] on 1,555 patients found that most remained with high levels of self-reported symptoms and distress.{{primary-source inline|date=March 2022}}<ref name=Walitt2011>{{MEDRS|date=March 2022}} {{cite journal | vauthors = Walitt B, Fitzcharles MA, Hassett AL, Katz RS, Häuser W, Wolfe F | title = The longitudinal outcome of fibromyalgia: a study of 1555 patients | journal = The Journal of Rheumatology | volume = 38 | issue = 10 | pages = 2238–2246 | date = October 2011 | pmid = 21765102 | doi = 10.3899/jrheum.110026 | s2cid = 207672626 | doi-access = free }}</ref> However, there was a great deal of patient ] accounting for almost half of the ]. At the final observation, 10% of the patients showed substantial improvement with minimal symptoms. An additional 15% had moderate improvement. This state, though, may be transient, given the fluctuations in symptom severity.{{primary-source inline|date=March 2022}}<ref name=Walitt2011/> | |||
| ==History== | |||
| Many names, including “muscular rheumatism,” “fibrositis,” “psychogenic rheumatism,” and “neurasthenia” were applied historically to symptoms resembling those of fibromyalgia.<ref>{{cite web |author=Health Information Team |title=Fibromyalgia |url=http://hcd2.bupa.co.uk/fact_sheets/mosby_factsheets/fibromyalgia.html |month=February | year=2004 |publisher=BUPA insurance}}</ref> The term ''fibromyalgia'' was coined in 1976 from the ] ''fibra'' (fiber)<ref>{{cite web | url = http://dictionary.reference.com/browse/fibro- | title = Fibro- | publisher = Dictionary.com | accessdate = 2008-05-21 }}</ref> and the ] words ''myo'' (muscle)<ref></ref> and ''algos'' (pain).<ref></ref> | |||
| A study of 97 ] diagnosed with fibromyalgia followed them for eight years.{{primary-source inline|date=March 2022}} After eight years, the majority of youth still experienced pain and ] in physical, social, and psychological areas. At the last follow-up, all participants reported experiencing one or more fibromyalgia symptoms such as pain, fatigue, and/or ], with 58% matching the complete ACR 2010 criteria for fibromyalgia. Based on the WPI and SS score cut-points, the remaining 42% exhibited subclinical symptoms. Pain and emotional symptom trajectories, on the other hand, displayed a variety of longitudinal patterns. The study concluded that while most patient's fibromyalgia symptoms endure, the severity of their pain tends to reduce over time.<ref name="KashikarNONRS">{{MEDRS|date=March 2022}} {{cite journal | vauthors = Kashikar-Zuck S, Cunningham N, Peugh J, Black WR, Nelson S, Lynch-Jordan AM, Pfeiffer M, Tran ST, Ting TV, Arnold LM, Carle A, Noll J, Powers SW, Lovell DJ | display-authors = 6 | title = Long-term outcomes of adolescents with juvenile-onset fibromyalgia into adulthood and impact of depressive symptoms on functioning over time | journal = Pain | volume = 160 | issue = 2 | pages = 433–441 | date = February 2019 | pmid = 30335681 | pmc = 6344278 | doi = 10.1097/j.pain.0000000000001415 }}</ref> | |||
| Historical perspectives on the development of the fibromyalgia concept note the “central importance” of a 1977 paper by Smythe and Moldofsky on fibrositis.<ref>Smythe HA, Moldofsky H. Two contributions to understanding of the “fibrositis” syndrome. Bull Rheum Dis 1977;28:928–3</ref><ref name=FMWars/> The first ], controlled study of the characteristics of fibromyalgia syndrome was published in 1981,<ref name=Winfield>{{cite journal |author=Winfield JB |title=Fibromyalgia and related central sensitivity syndromes: twenty-five years of progress |journal=Semin. Arthritis Rheum. |volume=36 |issue=6 |pages=335–8 |year=2007 |month=June |pmid=17303220 |doi=10.1016/j.semarthrit.2006.12.001 |url=http://linkinghub.elsevier.com/retrieve/pii/S0049-0172(06)00180-6 |accessdate=2008-05-21}}</ref> providing support for symptom associations. In 1984, an interconnection between fibromyalgia syndrome and other similar conditions was proposed,<ref name=Inanici>{{cite journal |author=Inanici F, Yunus MB |title=History of fibromyalgia: past to present |journal=Curr Pain Headache Rep |volume=8 |issue=5 |pages=369–78 |year=2004 |month=October |pmid=15361321 |doi= 10.1007/s11916-996-0010-6|url= |accessdate=2008-05-21}}</ref> and in 1986, trials of the first proposed medications for fibromyalgia were published.<ref name=Inanici/> | |||
| Baseline ] symptoms in adolescents appear to predict worse pain at follow-up periods.<ref>{{cite journal | vauthors = Leino-Arjas P, Rajaleid K, Mekuria G, Nummi T, Virtanen P, Hammarström A | title = Trajectories of musculoskeletal pain from adolescence to middle age: the role of early depressive symptoms, a 27-year follow-up of the Northern Swedish Cohort | journal = Pain | volume = 159 | issue = 1 | pages = 67–74 | date = January 2018 | pmid = 28937577 | doi = 10.1097/j.pain.0000000000001065 | s2cid = 22164186 }}</ref><ref>{{cite journal | vauthors = Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S | title = Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology | journal = Pain | volume = 93 | issue = 3 | pages = 247–257 | date = September 2001 | pmid = 11514084 | doi = 10.1016/s0304-3959(01)00324-4 | s2cid = 25457728 }}</ref> | |||
| A 1987 article in the ] used the term "fibromyalgia syndrome" while saying it was a "controversial condition."<ref name=Goldenberg1987>{{cite journal |author=Goldenberg DL |title=Fibromyalgia syndrome. An emerging but controversial condition |journal=JAMA |volume=257 |issue=20 |pages=2782–7 |year=1987|month=May|pmid=3553636 |doi=10.1001/jama.257.20.2782}}</ref> The ] (ACR) published its first classification criteria for fibromyalgia in 1990,<ref name=Wolfe/> although these are not strictly diagnostic criteria.<ref name=p17653720/> | |||
| A meta-analysis based on close to 200,000 fibromyalgia patients found that they were at a higher risk for ]. Specific mortality causes that were suggested were ], ] and ].<ref>{{Cite journal |last1=Treister-Goltzman |first1=Yulia |last2=Peleg |first2=Roni |date=2023 |title=Fibromyalgia and mortality: a systematic review and meta-analysis |journal=RMD Open |volume=9 |issue=3 |pages=e003005 |doi=10.1136/rmdopen-2023-003005|pmid=37429737 |pmc=10335452 |s2cid=259502501 }}</ref> | |||
| ==Controversies== | |||
| ==Epidemiology== | |||
| Fibromyalgia continues to be a disputed diagnosis. Many members of the medical community consider fibromyalgia a ‘non-disease’ because of a lack of abnormalities on physical examination, the absence of objective diagnostic tests,<ref name=FMWars>{{cite journal |author=Wolfe F |title=Fibromyalgia wars |journal=J Rheumatol. |volume=36 |issue=4 |pages=679-83 |month=April |year=2009 |pmid=19342721 }}</ref><ref name<ref name=p7880118>{{cite journal |author=Goldenberg DL |title=Fibromyalgia: why such controversy? |journal=Ann. Rheum. Dis. |volume=54 |issue=1 |pages=3–5 |year=1995 |month=January |pmid=7880118 |pmc=1005499 |doi= |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1005499}}</ref> and extensive overlap with other proposed conditions like ].<ref name="Deary"/><ref name=Buchwald>{{cite journal |author=Buchwald D, Garrity D |title=Comparison of patients with chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities |journal=Arch Intern Med |volume=154 |issue=18 |pages=2049-53 |year=1995 |month=September |pmid=8092909 }}</ref> | |||
| Fibromyalgia is estimated to affect 1.8% of the population.<ref>{{Cite journal |last1=Heidari |first1=Fatemeh |last2=Afshari |first2=Mahdi |last3=Moosazadeh |first3=Mahmood |date=September 2017 |title=Prevalence of fibromyalgia in the general population and patients, a systematic review and meta-analysis |url=http://link.springer.com/10.1007/s00296-017-3725-2 |journal=Rheumatology International |language=en |volume=37 |issue=9 |pages=1527–1539 |doi=10.1007/s00296-017-3725-2 |pmid=28447207 |s2cid=5043754 |issn=0172-8172}}</ref> | |||
| Even though more than 90% of fibromyalgia patients are women, only 60% of people with fibromyalgia symptoms are female in the general population.<ref>{{Cite journal |last1=Wolfe |first1=Frederick |last2=Walitt |first2=Brian |last3=Perrot |first3=Serge |last4=Rasker |first4=Johannes J. |last5=Häuser |first5=Winfried |date=2018-09-13 |editor-last=Sommer |editor-first=Claudia |title=Fibromyalgia diagnosis and biased assessment: Sex, prevalence and bias |journal=PLOS ONE |language=en |volume=13 |issue=9 |pages=e0203755 |doi=10.1371/journal.pone.0203755 |issn=1932-6203 |pmc=6136749 |pmid=30212526 |bibcode=2018PLoSO..1303755W |doi-access=free }}</ref> | |||
| Several controversial issues exist with regard to fibromyalgia that range from questions regarding the validity of the disorder as a clinical entity, to issues regarding primary pathophysiology and the potential existence of fibromyalgia subtypes. | |||
| ==Society and culture== | |||
| According to the article "Fibromyalgia wars", “the large majority of physicians, sociologists, and medical historians” <ref name=FMWars/> are skeptical about the validity of fibromyalgia as a clinical entity.<ref>Wolfe F, Rasker JJ “Fibromyalgia.” In: Firestein GS, Budd RC, Harris ED, Jr, McInnes IB, Ruddy S, Sergent JS, editors. Kelley’s textbook of rheumatology. 8th ed. Amsterdam: Elsevier; 2008</ref> Some call fibromyalgia a “non-disease”<ref name=p7880118/> and “an over-inclusive and ultimately meaningless label.”<ref>Baillieres Best Pract Res Clin Rheumatol. 1999 Sep;13(3):421-5. “Is fibromyalgia a distinct clinical entity? The disapproving rheumatologist's evidence.” Cohen ML</ref> Frederick Wolfe, the most-cited fibromyalgia researcher and lead author of the 1990 paper that first defined the fibromyalgia classification criteria, questions the validity of fibromyalgia as a disease. He considers fibromyalgia a physical response to stress, depression, and economic and social anxiety,<ref name=nytimes>http://www.nytimes.com/2008/01/14/health/14pain.html</ref> and believes the associated symptoms are a normal part of everyday life. In 2009, he wrote, "the tendency to respond with distress to physical and mental stressors is part of the human condition."<ref name=Fibromyalgianess>{{cite journal |author=Wolfe F |title=Fibromyalgianess |journal=Arthritis Rheum |volume=61 |issue=6 |pages=715-6 |year=2009 |month=June |pmid=19479689 }}</ref> Wolfe and other opponents of the fibromyalgia concept say that labeling fibromyalgia as a "disease" simply legitimizes patients’ sickness behavior, slowing their recovery and harming them.<ref name=p7880118/> | |||
| ===Economics=== | |||
| In a study of 100 individuals identified as having fibromyalgia, physical functioning decreased significantly over time, and individuals who had been diagnosed earlier had larger numbers of reported symptoms and greater severity. However, there was also a statistically significant improvement in satisfaction with health following classification.<ref name=p12115155 >{{cite journal |author=White KP et al. |title=Does the label "fibromyalgia" alter health status, function, and health service utilization? A prospective, within-group comparison in a community cohort of adults with chronic widespread pain.|journal=Arthritis Rheum. |volume=47 |issue=3 |pages=260–5 |year=2002|month=June|pmid=12115155}}</ref> The authors of the study concluded that the ‘fibromyalgia label’ does not have a meaningful adverse affect on clinical outcome over the long term. It is however possible that these results can be accounted for by ]. | |||
| People with fibromyalgia generally have higher healthcare costs and utilization rates. A review of 36 studies found that fibromyalgia causes a significant economic burden on healthcare systems.<ref name="D'Onghia-2022">{{cite journal | vauthors = D'Onghia M, Ciaffi J, Ruscitti P, Cipriani P, Giacomelli R, Ablin JN, Ursini F | title = The economic burden of fibromyalgia: A systematic literature review | journal = Seminars in Arthritis and Rheumatism | volume = 56 | pages = 152060 | date = October 2022 | pmid = 35849890 | doi = 10.1016/j.semarthrit.2022.152060 | s2cid = 250271053 }}</ref> Annual costs per patient were estimated to be up to $35,920 in the US and $8,504 in Europe.<ref name="D'Onghia-2022" /> | |||
| ===Controversies=== | |||
| The validity of fibromyalgia as a unique clinical entity is also a matter of contention. There is considerable overlap between fibromyalgia and other ], which are frequently referred to collectively as "functional somatic syndromes" (e.g. ], ]).<ref>{{cite journal |author=Kanaan RA, Lepine JP, Wessely SC |title=The association or otherwise of the functional somatic syndromes |journal=Psychosom Med |volume=69 |issue=9 |pages=855–9 |year=2007 |month=December |pmid=18040094 |pmc=2575798 |doi=10.1097/PSY.0b013e31815b001a }}</ref> | |||
| Fibromyalgia was defined relatively recently. In the past, it was a disputed diagnosis. Rheumatologist Frederick Wolfe, lead author of the 1990 paper that first defined the diagnostic guidelines for fibromyalgia, stated in 2008 that he believed it "clearly" not to be a disease but instead a physical response to depression and stress.<ref name=Berenson>{{cite news| vauthors = Berenson A |title=Drug Approved. Is Disease Real?|url=https://www.nytimes.com/2008/01/14/health/14pain.html|newspaper=The New York Times|access-date=26 March 2014|url-status=live|archive-url=https://web.archive.org/web/20150510060103/http://www.nytimes.com/2008/01/14/health/14pain.html|archive-date=10 May 2015|date=2008-01-14}}</ref> In 2013, Wolfe added that its causes "are controversial in a sense" and "there are many factors that produce these symptoms – some are psychological and some are physical and it does exist on a continuum".<ref name="news-medical.net">{{cite web |url=http://www.news-medical.net/news/20130322/Fibromyalgia-an-interview-with-Dr-Frederick-Wolfe-University-of-Kansas-School-of-Medicine.aspx |title=Fibromyalgia: An interview with Dr Frederick Wolfe, University of Kansas School of Medicine |access-date=2014-05-28 |url-status=live |archive-url=https://web.archive.org/web/20140529065741/http://www.news-medical.net/news/20130322/Fibromyalgia-an-interview-with-Dr-Frederick-Wolfe-University-of-Kansas-School-of-Medicine.aspx |archive-date=29 May 2014 |date=2013-03-22 }}</ref> Some members of the medical community do not consider fibromyalgia a disease because of a lack of abnormalities on physical examination and the absence of objective diagnostic tests.<ref name="FMWars">{{cite journal | vauthors = Wolfe F | title = Fibromyalgia wars | journal = The Journal of Rheumatology | volume = 36 | issue = 4 | pages = 671–678 | date = April 2009 | pmid = 19342721 | doi = 10.3899/jrheum.081180 | s2cid = 2091976 | doi-access = free }}</ref><ref name="p7880118">{{cite journal | vauthors = Goldenberg DL | title = Fibromyalgia: why such controversy? | journal = Annals of the Rheumatic Diseases | volume = 54 | issue = 1 | pages = 3–5 | date = January 1995 | pmid = 7880118 | pmc = 1005499 | doi = 10.1136/ard.54.1.3 }}</ref> | |||
| In the past, some psychiatrists have viewed fibromyalgia as a type of ], or a ]. These controversies do not engage healthcare specialists alone; some patients object to fibromyalgia being described in purely somatic terms.<ref>{{cite journal | vauthors = Hadlandsmyth K, Dailey DL, Rakel BA, Zimmerman MB, Vance CG, Merriwether EN, Chimenti RL, Geasland KM, Crofford LJ, Sluka KA | display-authors = 6 | title = Somatic symptom presentations in women with fibromyalgia are differentially associated with elevated depression and anxiety | journal = Journal of Health Psychology | volume = 25 | issue = 6 | pages = 819–829 | date = May 2020 | pmid = 29076404 | pmc = 6287969 | doi = 10.1177/1359105317736577 }}</ref> | |||
| Some researchers believe that differences in psychological and autonomic nervous system profiles among affected individuals may indicate the existence of fibromyalgia subtypes. A 2007 review divides individuals with fibromyalgia into four groups as well as “mixed types”:<ref name=p17653720>{{cite journal |author=Müller W, Schneider EM, Stratz T |title=The classification of fibromyalgia syndrome |journal=Rheumatol Int. |volume=27 |issue=11 |pages=1005–10 |year=2007 |month=September |pmid=17653720 |doi=10.1007/s00296-007-0403-9 |url=http://www.springerlink.com/content/1271314042w8405g/}}</ref> | |||
| # “extreme sensitivity to pain but no associated psychiatric conditions” (may respond to medications that block the 5-HT3 receptor) | |||
| # “fibromyalgia and comorbid, pain-related depression” (may respond to antidepressants) | |||
| # “depression with concomitant fibromyalgia syndrome” (may respond to antidepressants) | |||
| # “fibromyalgia due to somatization” (may respond to psychotherapy). | |||
| As of 2022, ]s and pain specialists tend to view fibromyalgia as a pathology due to dysfunction of muscles and connective tissue as well as functional abnormalities in the central nervous system. ] define the syndrome in the context of "]" – heightened brain response to normal stimuli in the absence of disorders of the muscles, joints, or connective tissues. Because of this symptomatic overlap, some researchers have proposed that fibromyalgia and other analogous syndromes be classified together as central sensitivity syndromes.<ref>{{cite journal | vauthors = Yunus MB | title = Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes | journal = Seminars in Arthritis and Rheumatism | volume = 36 | issue = 6 | pages = 339–356 | date = June 2007 | pmid = 17350675 | doi = 10.1016/j.semarthrit.2006.12.009 }}</ref><ref name="Central sensitivity and fibromyalgi" /> | |||
| ==See also== | |||
| *'']'', documentary film | |||
| == |
==Notes== | ||
| {{ |
{{notelist}} | ||
| == |
== References == | ||
| {{Reflist}} | |||
| <!-- BEFORE inserting new links here you should first post it to the talk page, otherwise your edit is likely to be reverted--> | |||
| * from the National Fibromyalgia Association | |||
| * from the National Fibromyalgia Association | |||
| * FAME Project, Unihealth Foundation grant | |||
| * | |||
| * at US Food and Drug Administration | |||
| * by the National Institute of Arthritis and Musculoskeletal and Skin Diseases | |||
| *{{dmoz|/Health/Conditions_and_Diseases/Musculoskeletal_Disorders/Connective_Tissue/Fibromyalgia/}} | |||
| * by the CDC | |||
| * Published by | |||
| {{Soft tissue disorders}} | |||
| == External links == | |||
| ] | |||
| * by the CDC | |||
| ] | |||
| * by the ] | |||
| ] | |||
| * by the ] | |||
| ] | |||
| * by the ] | |||
| {{Medical condition classification and resources | |||
| ] | |||
| | DiseasesDB = | |||
| ] | |||
| | ICD10 = {{ICD10|M79.7}} | |||
| ] | |||
| | ICD9 = {{ICD9|729.1}} | |||
| ] | |||
| | ICDO = | |||
| ] | |||
| | OMIM = | |||
| ] | |||
| | MedlinePlus = 000427 | |||
| ] | |||
| | eMedicineSubj = med | |||
| ] | |||
| | eMedicineTopic = 790 | |||
| ] | |||
| | eMedicine_mult = {{eMedicine2|med|2934}} {{eMedicine2|ped|777}} {{eMedicine2|pmr|47}} | |||
| ] | |||
| | MeshID = D005356 | |||
| ] | |||
| |ICD11={{ICD11|MG30.01}}}} | |||
| ] | |||
| {{Myopathy}} | |||
| ] | |||
| {{Neuropathy}} | |||
| ] | |||
| {{Authority control}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 06:23, 3 December 2024
Chronic pain of unknown causeNot to be confused with Myalgic encephalomyelitis/chronic fatigue syndrome nor with Myelofibrosis.
Medical condition
| Fibromyalgia | |
|---|---|
| Other names | Fibromyalgia syndrome |
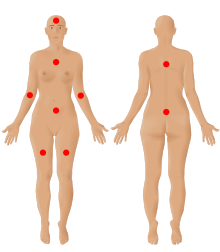 | |
| The nine possible pain sites of fibromyalgia according to the American Pain Society. | |
| Pronunciation | |
| Specialty | Rheumatology, neurology |
| Symptoms | Widespread pain, feeling tired, sleep problems |
| Usual onset | Early-Middle age |
| Duration | Long term |
| Causes | Unknown |
| Diagnostic method | Based on symptoms after ruling out other potential causes |
| Differential diagnosis | Anemia, autoimmune disorders (such as ankylosing spondylitis, polymyalgia rheumatica, rheumatoid arthritis, scleroderma, or multiple sclerosis), Lyme disease, osteoarthritis, thyroid disease |
| Treatment | Sufficient sleep and exercise |
| Medication | Duloxetine, milnacipran, pregabalin, gabapentin |
| Prognosis | Normal life expectancy |
| Frequency | 2% |
Fibromyalgia is a medical syndrome that causes chronic widespread pain, accompanied by fatigue, awakening unrefreshed, and cognitive symptoms. Other symptoms can include headaches, lower abdominal pain or cramps, and depression. People with fibromyalgia can also experience insomnia and general hypersensitivity. The cause of fibromyalgia is unknown, but is believed to involve a combination of genetic and environmental factors. Environmental factors may include psychological stress, trauma, and some infections. Since the pain appears to result from processes in the central nervous system, the condition is referred to as a "central sensitization syndrome". Although a protocol using an algometer (algesiometer) for determining central sensitization has been proposed as an objective diagnostic test, fibromyalgia continues to be primarily diagnosed by exclusion despite the high possibility of misdiagnosis.
Fibromyalgia was first defined in 1990, with updated criteria in 2011, 2016, and 2019. The term 'fibromyalgia' is from Neo-Latin fibro-, meaning 'fibrous tissues'; Greek μυο- myo-, 'muscle'; and Greek άλγος algos, 'pain'; thus, the term literally means "'muscle and fibrous connective tissue pain'. Fibromyalgia is estimated to affect 2 to 4% of the population. Women are affected about twice as often as men. Rates appear similar across areas of the world and among varied cultures.
The treatment of fibromyalgia is symptomatic and multidisciplinary. The European Alliance of Associations for Rheumatology strongly recommends aerobic and strengthening exercise. Weak recommendations are given for mindfulness, psychotherapy, acupuncture, hydrotherapy, and meditative exercise such as qigong, yoga, and tai chi. The use of medication in the treatment of fibromyalgia is debated, although antidepressants can improve quality of life. Other medications commonly considered helpful in managing fibromyalgia include serotonin–norepinephrine reuptake inhibitors, nonsteroidal anti-inflammatory drugs, and muscle relaxants. Q10 coenzyme and vitamin D supplements may reduce pain and improve quality of life. While symptoms of fibromyalgia are persistent in nearly all patients, they are not caused by cell damage or any organic disease.
History
Chronic widespread pain had been described in the literature in the 19th century, but the term fibromyalgia was not first used until 1976, when Phillip Kahler Hench used it to describe these symptoms. Many names, including muscular rheumatism, fibrositis, psychogenic rheumatism, and neurasthenia were applied historically to symptoms resembling those of fibromyalgia. The term fibromyalgia was coined by researcher Mohammed Yunus as a synonym for fibrositis. and was first used in a scientific publication in 1981. Fibromyalgia is from the Latin fibra (fiber) and the Greek words myo (muscle) and algos (pain).
Historical perspectives on the development of the fibromyalgia concept note the "central importance" of a 1977 paper on fibrositis by Smythe and Moldofsky. The first clinical, controlled study of the characteristics of fibromyalgia syndrome was published in 1981, providing support for symptom associations. In 1984, an interconnection between fibromyalgia syndrome and other similar conditions was proposed, and in 1986, trials of the first proposed medications for fibromyalgia were published.
A 1987 article in the Journal of the American Medical Association used the term 'fibromyalgia syndrome', while saying it was a "controversial condition". The American College of Rheumatology (ACR) published its first classification criteria for fibromyalgia in 1990. Later revisions were made in 2010, 2016, and 2019.
Classification
Fibromyalgia is classified as a disorder of pain processing due to abnormalities in how pain signals are processed in the central nervous system. The International Classification of Diseases (ICD-11) includes fibromyalgia in the category of "Chronic widespread pain," code MG30.01. People with fibromyalgia differ in several dimensions: severity, adjustment, symptom profile, psychological profile, and response to treatment.
Signs and symptoms
The defining symptoms of fibromyalgia are chronic widespread pain, fatigue, and sleep disturbance. Other symptoms may include heightened pain in response to tactile pressure (allodynia), cognitive problems, musculoskeletal stiffness, environmental sensitivity, hypervigilance, sexual dysfunction, and visual symptoms. Some people with fibromyalgia experience post-exertional malaise, in which symptoms flare up a day or longer after physical exercise.
Pain
Fibromyalgia is predominantly a chronic pain disorder. According to the NHS, widespread pain is one major symptom, which could feel like an ache, a burning sensation, or a sharp, stabbing pain. Patients are also highly sensitive to pain, and the slightest touch can cause pain. Pain also tends to linger for longer when a patient experiences pain.
Fatigue
Fatigue is one of the defining symptoms of fibromyalgia. Patients may experience physical or mental fatigue. Physical fatigue can present as a feeling of exhaustion after exercise or limitation in daily activities.
Sleep problems
Sleep problems are a core symptom of fibromyalgia. These include difficulty falling or staying asleep, awakening while sleeping, and waking up feeling unrefreshed. A meta-analysis compared quantitative and qualitative sleep metrics in people with fibromyalgia and healthy people. Individuals with fibromyalgia indicated lower sleep quality and efficiency, longer wake time after sleep start, shorter sleep duration, lighter sleep, and greater trouble initiating sleep when quantitatively assessed; and more difficulty initiating sleep when qualitatively assessed. Sleep problems may contribute to pain by decreased release of IGF-1 and human growth hormone, leading to decreased tissue repair. Improving sleep quality can help people with fibromyalgia manage pain.
Cognitive problems
Many people with fibromyalgia experience cognitive problems (known as fibrofog or brain fog). One study found that approximately 50% of fibromyalgia patients experienced subjective cognitive dysfunction and that it was associated with higher levels of pain and other fibromyalgia symptoms. The American Pain Society recognizes these problems as a major feature of fibromyalgia, characterized by trouble concentrating, forgetfulness, and disorganized or slow thinking. About 75% of people with fibromyalgia report significant problems with concentration, memory, and multitasking. A 2018 meta-analysis found that the largest differences between people with fibromyalgia and healthy subjects were in inhibitory control, memory, and processing speed. It is hypothesized that the chronic pain in fibromyalgia compromises attention systems, resulting in cognitive problems.
Hypersensitivity
In addition to hyperalgesia, patients with fibromyalgia experience hypersensitivity to other stimuli, such as bright lights, loud noises, perfumes, and cold. A review article found that they have a lower cold pain threshold. Other studies documented an acoustic hypersensitivity.
Comorbidity
Fibromyalgia as a stand-alone diagnosis is uncommon, as most fibromyalgia patients often have other chronic overlapping pain problems or mental disorders. Fibromyalgia is associated with mental health issues like anxiety, posttraumatic stress disorder, bipolar disorder, alexithymia, and depression. Patients with fibromyalgia are five times more likely to have major depression than the general population. Experiencing pain and limited energy from having fibromyalgia leads to less activity, leading to social isolation and increased stress levels, which tends to cause anxiety and depression.
Numerous chronic pain conditions are often comorbid with fibromyalgia. These include chronic tension headaches, myofascial pain syndrome, and temporomandibular disorders. Multiple sclerosis, post-polio syndrome, neuropathic pain, and Parkinson's disease are four neurological disorders that have been linked to pain or fibromyalgia.
Fibromyalgia largely overlaps with several syndromes that may share the same pathogenetic mechanisms. These include myalgic encephalomyelitis/chronic fatigue syndrome and irritable bowel syndrome.
Comorbid fibromyalgia has been reported to occur in 20–30% of individuals with rheumatic diseases. It has been reported in people with noninflammatory musculoskeletal diseases.
The prevalence of fibromyalgia in gastrointestinal disease has been described mostly for celiac disease and irritable bowel syndrome (IBS). IBS and fibromyalgia share similar pathogenic mechanisms, involving immune system mast cells, inflammatory biomarkers, hormones, and neurotransmitters such as serotonin. Changes in the gut biome alter serotonin levels, leading to autonomic nervous system hyperstimulation.
Fibromyalgia has also been linked with obesity. Other conditions that are associated with fibromyalgia include connective tissue disorders, cardiovascular autonomic abnormalities, obstructive sleep apnea-hypopnea syndrome, restless leg syndrome and an overactive bladder.
Risk factors
The cause of fibromyalgia is unknown. However, several risk factors, genetic and environmental, have been identified.
Genetics
Genetics plays a major role in fibromyalgia and may explain up to 50% of the disease's susceptibility. Fibromyalgia is potentially associated with polymorphisms of genes in the serotoninergic, dopaminergic and catecholaminergic systems. Several genes have been suggested as candidates for susceptibility to fibromyalgia. These include SLC6A4, TRPV2, MYT1L, NRXN3, and the 5-HT2A receptor 102T/C polymorphism. The heritability of fibromyalgia is estimated to be higher in patients younger than 50.
Nearly all the genes suggested as potential risk factors for fibromyalgia are associated with neurotransmitters and their receptors. Neuropathic pain and major depressive disorder often co-occur with fibromyalgia — the reason for this comorbidity appears to be due to shared genetic abnormalities, which leads to impairments in monoaminergic, glutamatergic, neurotrophic, opioid and proinflammatory cytokine signaling. In these vulnerable individuals, psychological stress or illness can cause abnormalities in inflammatory and stress pathways that regulate mood and pain. Eventually, a sensitization and kindling effect occurs in certain neurons leading to the establishment of fibromyalgia and sometimes a mood disorder.
Stress
Stress may be an important precipitating factor in the development of fibromyalgia. A 2021 meta-analysis found psychological trauma to be strongly associated with fibromyalgia. People who suffered abuse in their lifetime were three times more likely to have fibromyalgia; people who suffered medical trauma or other stressors in their lifetime were about twice as likely.
Some authors have proposed that, because exposure to stressful conditions can alter the function of the hypothalamic-pituitary-adrenal (HPA) axis, the development of fibromyalgia may stem from stress-induced disruption of the HPA axis.
Personality
Studies on personality and fibromyalgia have shown inconsistent results. Although some have suggested that fibromyalgia patients are more likely to have specific personality traits, it appears that in comparison to other diseases – when anxiety and depression are statistically controlled for – personality has far less relevance.
Other risk markers
Other risk markers for fibromyalgia include premature birth, female sex, childhood cognitive and psychosocial problems, primary pain disorders, multiregional pain, infectious illness, hypermobility of joints, iron deficiency, and small-fiber polyneuropathy. Metal-induced allergic inflammation has also been linked with fibromyalgia, especially in response to nickel but also inorganic mercury, cadmium, and lead. Following the COVID-19 pandemic, some have suggested that the SARS-CoV-2 virus may trigger fibromyalgia.
Pathophysiology
As of 2022, the pathophysiology of fibromyalgia has not yet been elucidated and several theories have been suggested. The prevailing view is that fibromyalgia is a condition resulting from an amplification of pain by the central nervous system. Substantial biological findings have backed up this notion, leading to development and adoption of the concept of nociplastic pain.
Fibromyalgia is associated with the deregulation of proteins related to complement and coagulation cascades, as well as to iron metabolism. An excessive oxidative stress response may cause dysregulation of many proteins.
Nervous system
Pain processing abnormalities
Chronic pain can be divided into three categories. Nociceptive pain is pain caused by inflammation or damage to tissues. Neuropathic pain is pain caused by nerve damage. Nociplastic pain (or central sensitization) is less understood and is the common explanation of the pain experienced in fibromyalgia. Because the three forms of pain can overlap, fibromyalgia patients may experience nociceptive (e.g., rheumatic illnesses) and neuropathic (e.g., small fiber neuropathy) pain, in addition to nociplastic pain.
Nociplastic pain (central sensitization)
Main article: Nociplastic painFibromyalgia can be viewed as a condition of nociplastic pain. Nociplastic pain is caused by an altered function of pain-related sensory pathways in the periphery and the central nervous system, resulting in hypersensitivity.
Nociplastic pain is commonly referred to as "Nociplastic pain syndrome" because it is coupled with other symptoms. These include fatigue, sleep disturbance, cognitive disturbance, hypersensitivity to environmental stimuli, anxiety, and depression. Nociplastic pain is caused by either (1) increased processing of pain stimuli or (2) decreased suppression of pain stimuli at several levels in the nervous system, or both.
Neuropathic pain
An alternative hypothesis to nociplastic pain views fibromyalgia as a stress-related dysautonomia with neuropathic pain features. This view highlights the role of autonomic and peripheral nociceptive nervous systems in the generation of widespread pain, fatigue, and insomnia. The description of small fiber neuropathy in a subgroup of fibromyalgia patients supports the disease neuropathic-autonomic underpinning. However, others claim that small fiber neuropathy occurs only in small groups of those with fibromyalgia.
Autonomic nervous system
Some suggest that fibromyalgia is caused or maintained by a decreased vagal tone, which is indicated by low levels of heart rate variability, signaling a heightened sympathetic response. Accordingly, several studies show that clinical improvement is associated with an increase in heart rate variability. Some examples of interventions that increase the heart rate variability and vagal tone are meditation, yoga, mindfulness, and exercise. In 2023 the Fibromyalgia: Imbalance of Threat and Soothing Systems (FITSS) model was suggested as a working hypothesis. According to the FITSS model, the salience network (also known as the midcingulo-insular network) may remain continuously hyperactive due to an imbalance in emotion regulation, which is reflected by an overactive "threat" system and an underactive "soothing" system. This hyperactivation, along with other mechanisms, may contribute to fibromyalgia.
Neurotransmitters
Some neurochemical abnormalities that occur in fibromyalgia also regulate mood, sleep, and energy, thus explaining why mood, sleep, and fatigue problems are commonly co-morbid with fibromyalgia. Serotonin is the most widely studied neurotransmitter in fibromyalgia. It is hypothesized that an imbalance in the serotoninergic system may lead to the development of fibromyalgia. There is also some data that suggests altered dopaminergic and noradrenergic signaling in fibromyalgia. Supporting the monoamine related theories is the efficacy of monoaminergic antidepressants in fibromyalgia. Glutamate/creatine ratios within the bilateral ventrolateral prefrontal cortex were found to be significantly higher in fibromyalgia patients than in controls and may disrupt glutamate neurotransmission.
Neurophysiology
Neuroimaging studies have observed that fibromyalgia patients have increased grey matter in the right postcentral gyrus and left angular gyrus, and decreased grey matter in the right cingulate gyrus, right paracingulate gyrus, left cerebellum, and left gyrus rectus. These regions are associated with affective and cognitive functions and with motor adaptations to pain processing. Other studies have documented decreased grey matter of the default mode network in people with fibromyalgia. These deficits are associated with pain processing.
Neuroendocrine system
Studies on the neuroendocrine system and HPA axis in fibromyalgia have been inconsistent. The depressed function of the HPA axis results in adrenal insufficiency and potentially chronic fatigue.
One study found fibromyalgia patients exhibited higher plasma cortisol, more extreme peaks and troughs, and higher rates of dexamethasone non-suppression. However, other studies have only found correlations between a higher cortisol awakening response and pain, and not any other abnormalities in cortisol. Increased baseline ACTH and increase in response to stress have been observed, and hypothesized to be a result of decreased negative feedback.
Oxidative stress
Pro-oxidative processes correlate with pain in fibromyalgia patients. Decreased mitochondrial membrane potential, increased superoxide activity, and increased lipid peroxidation production are observed. The high proportion of lipids in the central nervous system (CNS) makes the CNS especially vulnerable to free radical damage. Levels of lipid peroxidation products correlate with fibromyalgia symptoms.
Immune system
Inflammation has been suggested to have a role in the pathogenesis of fibromyalgia. People with fibromyalgia tend to have higher levels of inflammatory cytokines IL-6, and IL-8. There are also increased levels of the pro-inflammatory cytokines IL-1 receptor antagonist. Increased levels of pro-inflammatory cytokines may increase sensitivity to pain, and contribute to mood problems. Anti-inflammatory interleukins such as IL-10 have also been associated with fibromyalgia.
A repeated observation shows that autoimmunity triggers such as traumas and infections are among the most frequent events preceding the onset of fibromyalgia. Neurogenic inflammation has been proposed as a contributing factor to fibromyalgia.
Digestive system
Gut microbiome
Though there is a lack of evidence in this area, it is hypothesized that gut bacteria may play a role in fibromyalgia. People with fibromyalgia are more likely to show dysbiosis, a decrease in microbiota diversity. There is a bidirectional interplay between the gut and the nervous system. Therefore, the gut can affect the nervous system, but the nervous system can also affect the gut. Neurological effects mediated via the autonomic nervous system as well as the hypothalamic pituitary adrenal axis are directed to intestinal functional effector cells, which in turn are under the influence of the gut microbiota.
Gut-brain axis
The gut-brain axis, which connects the gut microbiome to the brain via the enteric nervous system, is another area of research. Fibromyalgia patients have less varied gut flora and altered serum metabolome levels of glutamate and serine, implying abnormalities in neurotransmitter metabolism.
Energy metabolism
Low ATP in skeletal muscle
Patients with fibromyalgia experience exercise intolerance. Primary fibromyalgia is idiopathic (cause unknown), whereas secondary fibromyalgia is in association with a known underlying disorder (such as Ankylosing spondylitis). In patients with primary fibromyalgia, studies have found disruptions in energy metabolism within skeletal muscle, including: decreased levels of ATP, ADP, and phosphocreatine, and increased levels of AMP and creatine (use of creatine kinase and myokinase in the phosphagen system due to low ATP); increased pyruvate; as well as reduced capillary density impairing oxygen delivery to the muscle cells for oxidative phosphorylation.
Low ATP in brain
Despite being a small percentage of the body's total mass, the brain consumes approximately 20% of the energy produced by the body. Parts of the brain—the anterior cingulate cortex (ACC), thalamus, and insula—were studied using proton magnetic resonance spectroscopy (MRS) in patients with fibromyalgia and compared to healthy controls. The fibromyalgia patients were found to have lower phosphocreatine (PCr) and lower creatine (Cr) than the control group. Phosphocreatine is used in the phosphagen system to produce ATP. The study found that low creatine and low phosphocreatine were associated with high pain, and that high stress, including PTSD, may contribute to these low levels.
Low phosphocreatine levels may disrupt glutamate neurotransmission within the brains of those with fibromyalgia. Glutamate/creatine ratios within the bilateral ventrolateral prefrontal cortex were found to be significantly higher than in controls.
Diagnosis

There is no single pathological feature, laboratory finding, or biomarker that can diagnose fibromyalgia, and there is debate over what should be considered diagnostic criteria and whether a medical diagnosis is possible, to begin with. In most cases, people with fibromyalgia symptoms may have laboratory test results that appear normal and many of their symptoms may mimic those of other rheumatic conditions such as arthritis or osteoporosis. The specific diagnostic criteria for fibromyalgia have evolved.
American College of Rheumatology
The first widely accepted set of classification criteria for research purposes was elaborated in 1990 by the Multicenter Criteria Committee of the American College of Rheumatology. These criteria, which are known informally as "the ACR 1990", defined fibromyalgia according to the presence of the following criteria:
- A history of widespread pain lasting more than three months – affecting all four quadrants of the body, i.e., both sides and above and below the waist.
- Tender points – there are 18 designated possible tender points (although a person with the disorder may feel pain in other areas as well).
The ACR criteria for the classification of patients were originally established as inclusion criteria for research purposes and were not intended for clinical diagnosis but have later become the de facto diagnostic criteria in the clinical setting. A controversial study was done by a legal team looking to prove their client's disability based primarily on tender points and their widespread presence in non-litigious communities prompted the lead author of the ACR criteria to question now the useful validity of tender points in diagnosis. Use of control points has been used to cast doubt on whether a person has fibromyalgia, and to claim the person is malingering.

In 2010, the American College of Rheumatology approved provisional revised diagnostic criteria for fibromyalgia that eliminated the 1990 criteria's reliance on tender point testing. The revised criteria used a widespread pain index (WPI) and symptom severity scale (SSS) in place of tender point testing under the 1990 criteria. The WPI counts up to 19 general body areas in which the person has experienced pain in the preceding week. The SSS rates the severity of the person's fatigue, unrefreshed waking, cognitive symptoms, and general somatic symptoms, each on a scale from 0 to 3, for a composite score ranging from 0 to 12. The revised criteria for diagnosis were:
- WPI ≥ 7 and SSS ≥ 5 OR WPI 3–6 and SSS ≥ 9,
- Symptoms have been present at a similar level for at least three months, and
- No other diagnosable disorder otherwise explains the pain.
In 2016, the provisional criteria of the American College of Rheumatology from 2010 were revised. The new diagnosis required all of the following criteria:
- "Generalized pain, defined as pain in at least 4 of 5 regions, is present."
- "Symptoms have been present at a similar level for at least 3 months."
- "Widespread pain index (WPI) ≥ 7 and symptom severity scale (SSS) score ≥ 5 OR WPI of 4–6 and SSS score ≥ 9."
- "A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses."
American Pain Society 2019
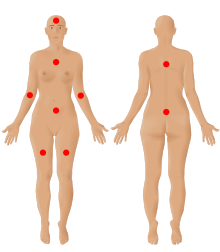
In 2019, the American Pain Society in collaboration with the U.S. Food and Drug Administration developed a new diagnostic system using two dimensions. The first dimension included core diagnostic criteria and the second included common features. In accordance to the 2016 diagnosis guidelines, the presence of another medical condition or pain disorder does not rule out the diagnosis of fibromyalgia. Nonetheless, other conditions should be ruled out as the main explaining reason for the patient's symptoms. The core diagnostic criteria are:
- Multisite pain defined as six or more pain sites from a total of nine possible sites (head, arms, chest, abdomen, upper back, lower back, and legs), for at least three months
- Moderate to severe sleep problems or fatigue, for at least three months
Common features found in fibromyalgia patients can assist the diagnosis process. These are tenderness (sensitivity to light pressure), dyscognition (difficulty to think), musculoskeletal stiffness, and environmental sensitivity or hypervigilance.
Self-report questionnaires
Some research has suggested using a multidimensional approach taking into consideration somatic symptoms, psychological factors, psychosocial stressors and subjective belief regarding fibromyalgia. These symptoms can be assessed by several self-report questionnaires.
Widespread Pain Index (WPI)
The Widespread Pain Index (WPI) was introduced by the American College of Rheumatology in 2010. It measures the number of painful body regions. The revised criteria count up to 19 general body areas: shoulder girdle, upper arm, lower arm, hip/buttock/trochanter, upper leg, lower leg, jaw, all left & right; plus the chest, abdomen, neck and upper and lower back. The 2016 ACR criteria required a Widespread pain index (WPI) ≥ 7 or WPI of 4–6 for higher severity pain.
Symptom Severity Scale (SSS)
The Symptom Severity Scale (SSS) assesses the severity of the fibromyalgia symptoms.
Fibromyalgia Impact Questionnaire (FIQ)
The Fibromyalgia Impact Questionnaire (FIQ) and the Revised Fibromyalgia Impact Questionnaire (FIQR) assess three domains: function, overall impact and symptoms. It is considered a useful measure of disease impact.
Other questionnaires
Other measures include the Hospital Anxiety and Depression Scale, Multiple Ability Self-Report Questionnaire, Multidimensional Fatigue Inventory, and Medical Outcomes Study Sleep Scale.
Differential diagnosis
As of 2009, as many as two out of every three people who are told that they have fibromyalgia by a rheumatologist may have some other medical condition instead. Fibromyalgia could be misdiagnosed in cases of early undiagnosed rheumatic diseases such as preclinical rheumatoid arthritis, early stages of inflammatory spondyloarthritis, polymyalgia rheumatica, myofascial pain syndromes and hypermobility syndrome. Neurological diseases with an important pain component include multiple sclerosis, Parkinson's disease and peripheral neuropathy. Other medical illnesses that should be ruled out are endocrine disease or metabolic disorder (hypothyroidism, hyperparathyroidism, acromegaly, vitamin D deficiency), gastro-intestinal disease (celiac and non-celiac gluten sensitivity), infectious diseases (Lyme disease, hepatitis C and immunodeficiency disease) and the early stages of a malignancy such as multiple myeloma, metastatic cancer and leukemia/lymphoma. Other systemic, inflammatory, endocrine, rheumatic, infectious, and neurologic disorders may cause fibromyalgia-like symptoms, such as systemic lupus erythematosus, Sjögren syndrome, ankylosing spondylitis, Ehlers-Danlos syndromes, psoriatic-related polyenthesitis, a nerve compression syndrome (such as carpal tunnel syndrome), and myasthenia gravis. In addition, several medications can also evoke pain (statins, aromatase inhibitors, bisphosphonates, and opioids).
The differential diagnosis is made during the evaluation based on the person's medical history, physical examination, and laboratory investigations. The patient's history can provide some hints to a fibromyalgia diagnosis. A family history of early chronic pain, a childhood history of pain, an emergence of broad pain following physical and/or psychosocial stress, a general hypersensitivity to touch, smell, noise, taste, hypervigilance, and various somatic symptoms (gastrointestinal, urology, gynecology, neurology), are all examples of these signals.
Extensive laboratory tests are usually unnecessary in the differential diagnosis of fibromyalgia. Common tests that are conducted include complete blood count, comprehensive metabolic panel, erythrocyte sedimentation rate, C-reactive protein, and thyroid function test.
Management
Universally accepted treatments typically consist of symptom management and improving patient quality of life. A personalized, multidisciplinary approach to treatment that includes pharmacologic considerations and begins with effective patient education is most beneficial. Developments in the understanding of the pathophysiology of the disorder have led to improvements in treatment, which include prescription medication, behavioral intervention, and exercise.
Several associations have published guidelines for the diagnosis and management of fibromyalgia. The European League Against Rheumatism (EULAR; 2017) recommends a multidisciplinary approach, allowing a quick diagnosis and patient education. The recommended initial management should be non-pharmacological, later pharmacological treatment can be added. The European League Against Rheumatism gave the strongest recommendation for aerobic and strengthening exercise. Weak recommendations were given to some treatments, based on their outcomes. Qigong, yoga, and tai chi were weakly recommended for improving sleep and quality of life. Mindfulness was weakly recommended for improving pain and quality of life. Acupuncture and hydrotherapy were weakly recommended for improving pain. A weak recommendation was also given to psychotherapy. It was more suitable for patients with mood disorders or unhelpful coping strategies. Chiropractic was strongly recommended against, due to safety concerns. Some medications were weakly recommended for severe pain (duloxetine, pregabalin, tramadol) or sleep disturbance (amitriptyline, cyclobenzaprine, pregabalin). Others were not recommended due to a lack of efficacy (nonsteroidal anti-inflammatory drugs, monoamine oxidase inhibitors and selective serotonin reuptake inhibitors). Growth hormone, sodium oxybate, opioids, and steroids were strongly recommended against due to lack of efficacy and side effects.
The guidelines published by the Association of the Scientific Medical Societies in Germany inform patients that self-management strategies are an important component in managing the disease. The Canadian Pain Society also published guidelines for the diagnosis and management of fibromyalgia.
Exercise
Exercise is the only fibromyalgia treatment that has been given a strong recommendation by the European Alliance of Associations for Rheumatology (EULAR). There is strong evidence indicating that exercise improves fitness, sleep and quality of life and may reduce pain and fatigue for people with fibromyalgia. Exercise has an added benefit in that it does not cause any serious adverse effects. There are a number of hypothesized biological mechanisms. Exercise may improve pain modulation through serotoninergic pathways. It may reduce pain by altering the hypothalamic-pituitary-adrenal axis and reducing cortisol levels. It also has anti-inflammatory effects that may improve fibromyalgia symptoms. Aerobic exercise can improve muscle metabolism and pain through mitochondrial pathways.
When different exercise programs are compared, aerobic exercise is capable of modulating the autonomic nervous function of fibromyalgia patients, whereas resistance exercise does not show such effects. A 2022 meta-analysis found that aerobic training showed a high effect size while strength interventions showed moderate effects. Meditative exercise seems preferable for improving sleep, with no differences between resistance, flexibility, and aquatic exercise in their favorable effects on fatigue.
Despite its benefits, exercise is a challenge for patients with fibromyalgia, due to the chronic fatigue and pain they experience. They may also feel that those who recommend or deliver exercise interventions do not fully understand the possible negative impact of exercise on fatigue and pain. This is especially true for non-personalized exercise programs. Adherence is higher when the exercise program is recommended by doctors or supervised by nurses.
Sufferers perceive exercise as more effortful than healthy adults. Depression and higher pain intensity serve as barriers to physical activity. Exercise may intimidate them, in fear that they will be asked to do more than they are capable of.
A recommended approach to a graded exercise program begins with small, frequent exercise periods and builds up from there. In order to reduce pain the use of an exercise program of 13 to 24 weeks is recommended, with each session lasting 30 to 60 minutes.
Aerobic
Aerobic exercise for fibromyalgia patients is the most investigated type of exercise. It includes activities such as walking, jogging, spinning, cycling, dancing and exercising in water, with walking being named as one of the best methods. A 2017 Cochrane summary concluded that aerobic exercise probably improves quality of life, slightly decreases pain and improves physical function and makes no difference in fatigue and stiffness. A 2019 meta-analysis showed that exercising aerobically can reduce autonomic dysfunction and increase heart rate variability. This happens when patients exercise at least twice a week, for 45–60 minutes at about 60%-80% of the maximum heart rate. Aerobic exercise also decreases anxiety and depression and improves the quality of life.
Flexibility
Combinations of different exercises such as flexibility and aerobic training may improve stiffness. However, the evidence is of low-quality. It is not clear if flexibility training alone compared to aerobic training is effective at reducing symptoms or has any adverse effects.
Resistance
In resistance exercise, participants apply a load to their body using weights, elastic bands, body weight, or other measures.
Two meta-analyses on fibromyalgia have shown that resistance training can reduce anxiety and depression, one found that it decreases pain and disease severity and one found that it improves quality of life. Resistance training may also improve sleep, with a greater effect than that of flexibility training and a similar effect to that of aerobic exercise.
The dosage of resistance exercise for women with fibromyalgia was studied in a 2022 meta-analysis. Effective dosages were found when exercising twice a week, for at least eight weeks. Symptom improvement was found for even low dosages such as 1–2 sets of 4–20 repetitions. Most studies use moderate exercise intensity of 40% to 85% one-repetition maximum. This intensity was effective in reducing pain. Some treatment regimes increase the intensity over time (from 40% to 80%), whereas others increase it when the participant can perform 12 repetitions. High-intensity exercises may cause lower treatment adherence.
Meditative
A 2021 meta-analysis found that meditative exercise programs (tai chi, yoga, qigong) were superior to other forms of exercise (aerobic, flexibility, resistance) in improving sleep quality. Other meta-analyses also found positive effects of tai chi for sleep, fibromyalgia symptoms, and pain, fatigue, depression and quality of life. These tai chi interventions frequently included 1-hour sessions practiced 1-3 times a week for 12 weeks. Meditative exercises, as a whole, may achieve desired outcomes through biological mechanisms such as antioxidation, anti-inflammation, reduction in sympathetic activity and modulation of glucocorticoid receptor sensitivity.
Aquatic
Several reviews and meta-analyses suggest that aquatic training can improve symptoms and wellness in people with fibromyalgia. It is recommended to practice aquatic therapy at least twice a week using a low to moderate intensity. However, aquatic therapy does not appear to be superior to other types of exercise.
Other
Limited evidence suggests vibration training in combination with exercise may improve pain, fatigue, and stiffness.
Medications
A few countries have published guidelines for the management and treatment of fibromyalgia. As of 2018, all of them emphasize that medications are not required. However, medications, though imperfect, continue to be a component of treatment strategy for fibromyalgia patients. The German guidelines outlined parameters for drug therapy termination and recommended considering drug holidays after six months.
Health Canada and the US Food and Drug Administration (FDA) have approved pregabalin (an anticonvulsant) and duloxetine (a serotonin–norepinephrine reuptake inhibitor) for the management of fibromyalgia. The FDA also approved milnacipran (another serotonin–norepinephrine reuptake inhibitor), but the European Medicines Agency refused marketing authority.
The medications duloxetine, milnacipran, or pregabalin have been approved by the US Food and Drug Administration (FDA) for the management of fibromyalgia.
Antidepressants
Antidepressants are one of the common drugs for fibromyalgia. A 2021 meta-analysis concluded that antidepressants can improve the quality of life for fibromyalgia patients in the medium term. For most people with fibromyalgia, the potential benefits of treatment with the serotonin and norepinephrine reuptake inhibitors duloxetine and milnacipran and the tricyclic antidepressants, such as amitriptyline, are outweighed by significant adverse effects (more adverse effects than benefits), however, a small number of people may experience relief from symptoms with these medications.
The length of time that antidepressant medications take to be effective at reducing symptoms can vary. Any potential benefits from the antidepressant amitriptyline may take up to three months to take effect and it may take between three and six months for duloxetine, milnacipran, and pregabalin to be effective at improving symptoms. Some medications have the potential to cause withdrawal symptoms when stopping so gradual discontinuation may be warranted particularly for antidepressants and pregabalin.
Serotonin and norepinephrine reuptake inhibitors
A 2023 meta-analysis found that duloxetine improved fibromyalgia symptoms, regardless of the dosage. SSRIs may be also be used to treat depression in people diagnosed with fibromyalgia.
Tricyclic antidepressants
While amitriptyline has been used as a first-line treatment, the quality of evidence to support this use and comparison between different medications is poor. Very weak evidence indicates that a very small number of people may benefit from treatment with the tetracyclic antidepressant mirtazapine, however, for most, the potential benefits are not great and the risk of adverse effects and potential harm outweighs any potential for benefit. As of 2018, the only tricyclic antidepressant that has sufficient evidence is amitriptyline.
Monoamine oxidase inhibitors
Tentative evidence suggests that monoamine oxidase inhibitors (MAOIs) such as pirlindole and moclobemide are moderately effective for reducing pain. Very low-quality evidence suggests pirlindole as more effective at treating pain than moclobemide. Side effects of MAOIs may include nausea and vomiting.
Central nervous system depressants
Central nervous system depressants include drug categories such as sedatives, tranquilizers, and hypnotics. A 2021 meta-analysis concluded that such drugs can improve the quality of life for fibromyalgia patients in the medium term.
Anti-seizure medication
The anti-convulsant medications gabapentin and pregabalin may be used to reduce pain. There is tentative evidence that gabapentin may be of benefit for pain in about 18% of people with fibromyalgia. It is not possible to predict who will benefit, and a short trial may be recommended to test the effectiveness of this type of medication. Approximately 6/10 people who take gabapentin to treat pain related to fibromyalgia experience unpleasant side effects such as dizziness, abnormal walking, or swelling from fluid accumulation. Pregabalin demonstrates a benefit in about 9% of people. Pregabalin reduced time off work by 0.2 days per week.
Cannabinoids
Cannabinoids may have some benefits for people with fibromyalgia. However, as of 2022, the data on the topic is still limited. Cannabinoids may also have adverse effects and may negatively interact with common rheumatological drugs.
Opioids
The use of opioids is controversial. As of 2015, no opioid is approved for use in this condition by the FDA. A 2016 Cochrane review concluded that there is no good evidence to support or refute the suggestion that oxycodone, alone or in combination with naloxone, reduces pain in fibromyalgia. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) in 2014 stated that there was a lack of evidence for opioids for most people. The Association of the Scientific Medical Societies in Germany in 2012 made no recommendation either for or against the use of weak opioids because of the limited amount of scientific research addressing their use in the treatment of fibromyalgia. They strongly advise against using strong opioids. The Canadian Pain Society in 2012 said that opioids, starting with a weak opioid like tramadol, can be tried but only for people with moderate to severe pain that is not well-controlled by non-opioid painkillers. They discourage the use of strong opioids and only recommend using them while they continue to provide improved pain and functioning. Healthcare providers should monitor people on opioids for ongoing effectiveness, side effects, and possible unwanted drug behaviors.
A 2015 review found fair evidence to support tramadol use if other medications do not work. A 2018 review found little evidence to support the combination of paracetamol (acetaminophen) and tramadol over a single medication. Goldenberg et al suggest that tramadol works via its serotonin and norepinephrine reuptake inhibition, rather than via its action as a weak opioid receptor agonist.
A large study of US people with fibromyalgia found that between 2005 and 2007 37.4% were prescribed short-acting opioids and 8.3% were prescribed long-acting opioids, with around 10% of those prescribed short-acting opioids using tramadol; and a 2011 Canadian study of 457 people with fibromyalgia found 32% used opioids and two-thirds of those used strong opioids.
Topical treatment
Capsaicin has been suggested as a topical pain reliever. Preliminary results suggest that it may improve sleep quality and fatigue, but there are not enough studies to support this claim.
Unapproved or unfounded
Sodium oxybate increases growth hormone production levels through increased slow-wave sleep patterns. However, this medication was not approved by the FDA for the indication for use in people with fibromyalgia due to the concern for abuse.
The muscle relaxants cyclobenzaprine, carisoprodol with acetaminophen and caffeine, and tizanidine are sometimes used to treat fibromyalgia; however, as of 2015 they are not approved for this use in the United States. The use of nonsteroidal anti-inflammatory drugs is not recommended as first-line therapy. Moreover, nonsteroidal anti-inflammatory drugs cannot be considered as useful in the management of fibromyalgia.
Very low-quality evidence suggests quetiapine may be effective in fibromyalgia.
No high-quality evidence exists that suggests synthetic THC (nabilone) helps with fibromyalgia.
Nutrition and dietary supplements
Nutrition is related to fibromyalgia in several ways. Some nutritional risk factors for fibromyalgia complications are obesity, nutritional deficiencies, food allergies, and consuming food additives. The consumption of fruits and vegetables, low-processed foods, high-quality proteins, and healthy fats may have some benefits. Low-quality evidence found some benefits of a vegetarian or vegan diet.
Although dietary supplements have been widely investigated concerning fibromyalgia, most of the evidence, as of 2021, is of poor quality. It is therefore difficult to reach conclusive recommendations. It appears that Q10 coenzyme and vitamin D supplements can reduce pain and improve quality of life for fibromyalgia patients. Q10 coenzyme has beneficial effects on fatigue in fibromyalgia patients, with most studies using doses of 300 mg per day for three months. Q10 coenzyme is hypothesized to improve mitochondrial activity and decrease inflammation. Vitamin D has been shown to improve some fibromyalgia measures, but not others.
Two review articles found that melatonin treatment has several positive effects on fibromyalgia patients, including the improvement of sleep quality, pain, and disease impact. No major adverse events were reported.
Psychotherapy
Due to the uncertainty about the pathogenesis of fibromyalgia, current treatment approaches focus on management of symptoms to improve quality of life, using integrated pharmacological and non-pharmacological approaches. There is no single intervention shown to be effective for all patients. In a 2020 Cochrane review, cognitive behavioral therapy was found to have a small but beneficial effect for reducing pain and distress but adverse events were not well evaluated. Cognitive behavioral therapy and related psychological and behavioural therapies have a small to moderate effect in reducing symptoms of fibromyalgia. Effect sizes tend to be small when cognitive behavioral therapy is used as a stand-alone treatment for patients with fibromyalgia, but these improve significantly when it is part of a wider multidisciplinary treatment program.
A 2010 systematic review of 14 studies reported that cognitive behavioral therapy improves self-efficacy or coping with pain and reduces the number of physician visits at post-treatment, but has no significant effect on pain, fatigue, sleep, or health-related quality of life at post-treatment or follow-up. Depressed mood was also improved but this could not be distinguished from some risks of bias. A 2022 meta-analysis found that cognitive behavioral therapy reduces insomnia in people with chronic pain, including people with fibromyalgia. Acceptance and commitment therapy, a type of cognitive behavioral therapy, has also proven effective.
Patient education
Patient education is recommended by the European League Against Rheumatism (EULAR) as an important treatment component. As of 2022, there is only low-quality evidence showing that patient education can decrease pain and fibromyalgia impact.
Sleep hygiene interventions show low effectiveness in improving insomnia in people with chronic pain.
Physical therapy
Patients with chronic pain, including those with fibromyalgia, can benefit from techniques such as manual therapy, cryotherapy, and balneotherapy. These can lessen the experience of chronic pain and increase both the amount and quality of sleep. Patients' quality of life is also improved by decreasing pain mechanisms and increasing sleep quality, particularly during the REM phase, sleep efficiency, and alertness.
Manual therapy
A 2021 meta-analysis concluded that massage and myofascial release diminish pain in the medium term. As of 2015, there was no good evidence for the benefit of other mind-body therapies.
Acupuncture
A 2013 review found moderate-level evidence on the usage of acupuncture with electrical stimulation for improvement of overall well-being. Acupuncture alone will not have the same effects, but will enhance the influence of exercise and medication in pain and stiffness.
Electrical neuromodulation
Several forms of electrical neuromodulation, including transcutaneous electrical nerve stimulation (TENS) and transcranial direct current stimulation (tDCS), have been used to treat fibromyalgia. In general, they help reduce pain and depression and improve functioning.
Transcutaneous electrical nerve stimulation (TENS)
Transcutaneous electrical nerve stimulation (TENS) is the delivery of pulsed electrical currents to the skin to stimulate peripheral nerves. TENS is widely used to treat pain and is considered to be a low-cost, safe, and self-administered treatment. As such, it is commonly recommended by clinicians to people suffering from pain. On 2019, an overview of eight Cochrane reviews was conducted, covering 51 TENS-related randomized controlled trials. The review concluded that the quality of the available evidence was insufficient to make any recommendations. A later review concluded that transcutaneous electrical nerve stimulation may diminish pain in the short term, but there was uncertainty about the relevance of the results.
Preliminary findings suggest that electrically stimulating the vagus nerve through an implanted device can potentially reduce fibromyalgia symptoms. However, there may be adverse reactions to the procedure.
Noninvasive brain stimulation
Noninvasive brain stimulation includes methods such as transcranial direct current stimulation and high-frequency repetitive transcranial magnetic stimulation (TMS). Both methods have been found to improve pain scores in neuropathic pain and fibromyalgia.
A 2023 meta-analysis of 16 RCTs found that transcranial direct current stimulation (tDCS) of over 4 weeks can decrease pain in patients with fibromyalgia.
A 2021 meta-analysis of multiple intervention types concluded that magnetic field therapy and transcranial magnetic stimulation may diminish pain in the short-term, but conveyed an uncertainty about the relevance of the result. Several 2022 meta-analyses focusing on transcranial magnetic stimulation found positive effects on fibromyalgia. Repetitive transcranial magnetic stimulation improved pain in the short-term and quality of life after 5–12 weeks. Repetitive transcranial magnetic stimulation did not improve anxiety, depression, and fatigue. Transcranial magnetic stimulation to the left dorsolateral prefrontal cortex was also ineffective.
EEG neurofeedback
A systematic review of EEG neurofeedback for the treatment of fibromyalgia found most treatments showed significant improvements of the main symptoms of the disease. However, the protocols were so different, and the lack of controls or randomization impede drawing conclusive results.
Hyperbaric oxygen therapy
Hyperbaric oxygen therapy (HBOT) has shown beneficial effects in treating chronic pain by reducing inflammation and oxidative stress. However, treating fibromyalgia with hyperbaric oxygen therapy is still controversial, in light of the scarcity of large-scale clinical trials. In addition, hyperbaric oxygen therapy raises safety concerns due to the oxidative damage that may follow it. An evaluation of nine trials with 288 patients in total found that HBOT was more effective at relieving fibromyalgia patients' pain than the control intervention. In most of the trials, HBOT improved sleep disturbance, multidimensional function, patient satisfaction, and tender spots. 24% of the patients experienced negative outcomes.
Prognosis
Although in itself fibromyalgia is neither degenerative nor fatal, the chronic pain of fibromyalgia is pervasive and persistent. Most people with fibromyalgia report that their symptoms do not improve over time. However, most patients learn to adapt to the symptoms over time. The German guidelines for patients explain that:
- The symptoms of fibromyalgia are persistent in nearly all patients.
- Total relief of symptoms is seldom achieved.
- The symptoms do not lead to disablement and do not shorten life expectancy.
An 11-year follow-up study on 1,555 patients found that most remained with high levels of self-reported symptoms and distress. However, there was a great deal of patient heterogeneity accounting for almost half of the variance. At the final observation, 10% of the patients showed substantial improvement with minimal symptoms. An additional 15% had moderate improvement. This state, though, may be transient, given the fluctuations in symptom severity.
A study of 97 adolescents diagnosed with fibromyalgia followed them for eight years. After eight years, the majority of youth still experienced pain and disability in physical, social, and psychological areas. At the last follow-up, all participants reported experiencing one or more fibromyalgia symptoms such as pain, fatigue, and/or sleep problems, with 58% matching the complete ACR 2010 criteria for fibromyalgia. Based on the WPI and SS score cut-points, the remaining 42% exhibited subclinical symptoms. Pain and emotional symptom trajectories, on the other hand, displayed a variety of longitudinal patterns. The study concluded that while most patient's fibromyalgia symptoms endure, the severity of their pain tends to reduce over time.
Baseline depressive symptoms in adolescents appear to predict worse pain at follow-up periods.
A meta-analysis based on close to 200,000 fibromyalgia patients found that they were at a higher risk for all-cause mortality. Specific mortality causes that were suggested were accidents, infections and suicide.
Epidemiology
Fibromyalgia is estimated to affect 1.8% of the population.
Even though more than 90% of fibromyalgia patients are women, only 60% of people with fibromyalgia symptoms are female in the general population.
Society and culture
Economics
People with fibromyalgia generally have higher healthcare costs and utilization rates. A review of 36 studies found that fibromyalgia causes a significant economic burden on healthcare systems. Annual costs per patient were estimated to be up to $35,920 in the US and $8,504 in Europe.
Controversies
Fibromyalgia was defined relatively recently. In the past, it was a disputed diagnosis. Rheumatologist Frederick Wolfe, lead author of the 1990 paper that first defined the diagnostic guidelines for fibromyalgia, stated in 2008 that he believed it "clearly" not to be a disease but instead a physical response to depression and stress. In 2013, Wolfe added that its causes "are controversial in a sense" and "there are many factors that produce these symptoms – some are psychological and some are physical and it does exist on a continuum". Some members of the medical community do not consider fibromyalgia a disease because of a lack of abnormalities on physical examination and the absence of objective diagnostic tests.
In the past, some psychiatrists have viewed fibromyalgia as a type of affective disorder, or a somatic symptom disorder. These controversies do not engage healthcare specialists alone; some patients object to fibromyalgia being described in purely somatic terms.
As of 2022, neurologists and pain specialists tend to view fibromyalgia as a pathology due to dysfunction of muscles and connective tissue as well as functional abnormalities in the central nervous system. Rheumatologists define the syndrome in the context of "central sensitization" – heightened brain response to normal stimuli in the absence of disorders of the muscles, joints, or connective tissues. Because of this symptomatic overlap, some researchers have proposed that fibromyalgia and other analogous syndromes be classified together as central sensitivity syndromes.
Notes
- Shoulder girdle (left & right), upper arm (left & right), lower arm (left & right), hip/buttock/trochanter (left & right), upper leg (left & right), lower leg (left & right), jaw (left & right), chest, abdomen, back (upper & lower), and neck.
- Somatic symptoms include, but are not limited to muscle pain, irritable bowel syndrome, fatigue or tiredness, problems thinking or remembering, muscle weakness, headache, pain or cramps in the abdomen, numbness or tingling, dizziness, insomnia, depression, constipation, pain in the upper abdomen, nausea, nervousness, chest pain, blurred vision, fever, diarrhea, dry mouth, itching, wheezing, Raynaud's phenomenon, hives or welts, ringing in the ears, vomiting, heartburn, oral ulcers, loss of or changes in taste, seizures, dry eyes, shortness of breath, loss of appetite, rash, sun sensitivity, hearing difficulties, easy bruising, hair loss, frequent or painful urination, and bladder spasms.
References
- "fibromyalgia". Collins Dictionaries. Archived from the original on 4 October 2015. Retrieved 16 March 2016.
- "Neurology Now: Fibromyalgia: Is Fibromyalgia Real? | American Academy of Neurology". tools.aan.com. October 2009. Retrieved 1 June 2018.
- ^ Ngian GS, Guymer EK, Littlejohn GO (February 2011). "The use of opioids in fibromyalgia". International Journal of Rheumatic Diseases. 14 (1): 6–11. doi:10.1111/j.1756-185X.2010.01567.x. PMID 21303476. S2CID 29000267.
- ^ Clauw DJ (April 2014). "Fibromyalgia: a clinical review". JAMA. 311 (15): 1547–1555. doi:10.1001/jama.2014.3266. PMID 24737367. S2CID 43693607.
- ^ "Questions and Answers about Fibromyalgia". NIAMS. July 2014. Archived from the original on 15 March 2016. Retrieved 15 March 2016.
- Ferri FF (2010). "Chapter F". Ferri's differential diagnosis: a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. ISBN 978-0-323-07699-9.
- Schneider MJ, Brady DM, Perle SM (2006). "Commentary: differential diagnosis of fibromyalgia syndrome: proposal of a model and algorithm for patients presenting with the primary symptom of chronic widespread pain". Journal of Manipulative and Physiological Therapeutics. 29 (6): 493–501. doi:10.1016/j.jmpt.2006.06.010. PMID 16904498.
- ^ Cooper TE, Derry S, Wiffen PJ, Moore RA (January 2017). "Gabapentin for fibromyalgia pain in adults". The Cochrane Database of Systematic Reviews. 1 (1): CD012188. doi:10.1002/14651858.CD012188.pub2. PMC 6465053. PMID 28045473.
- ^ Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, et al. (December 2016). "2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria". Seminars in Arthritis and Rheumatism. 46 (3): 319–329. doi:10.1016/j.semarthrit.2016.08.012. PMID 27916278.
- ^ Wu YL, Chang LY, Lee HC, Fang SC, Tsai PS (May 2017). "Sleep disturbances in fibromyalgia: A meta-analysis of case-control studies". Journal of Psychosomatic Research. 96: 89–97. doi:10.1016/j.jpsychores.2017.03.011. PMID 28545798.
- ^ Häuser W, Sarzi-Puttini P, Fitzcharles MA (2019). "Fibromyalgia syndrome: under-, over- and misdiagnosis". Clinical and Experimental Rheumatology. 37 (1 Suppl 116): 90–97. PMID 30747096.
- ^ Arnold LM, Bennett RM, Crofford LJ, Dean LE, Clauw DJ, Goldenberg DL, et al. (June 2019). "AAPT Diagnostic Criteria for Fibromyalgia". The Journal of Pain. 20 (6): 611–628. doi:10.1016/j.jpain.2018.10.008. hdl:2434/632765. PMID 30453109. S2CID 53872511.
- ^ Mezhov V, Guymer E, Littlejohn G (December 2021). "Central sensitivity and fibromyalgia". Internal Medicine Journal. 51 (12): 1990–1998. doi:10.1111/imj.15430. PMID 34139045. S2CID 235471910.
- ^ Galvez-Sánchez CM, Reyes Del Paso GA (April 2020). "Diagnostic Criteria for Fibromyalgia: Critical Review and Future Perspectives". Journal of Clinical Medicine. 9 (4): 1219. doi:10.3390/jcm9041219. PMC 7230253. PMID 32340369.
Furthermore, in many cases the FMS diagnosis is fundamentally based on the exclusion of other similar diseases; in spite of that practice not being recommended because of its lack of precision and the high possibility of misdiagnosis.
- Bergmann U (2012). Neurobiological foundations for EMDR practice. New York: Springer Pub. Co. p. 165. ISBN 978-0-8261-0938-5.
- ^ Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W (May 2021). "Nociplastic pain: towards an understanding of prevalent pain conditions". Lancet. 397 (10289): 2098–2110. doi:10.1016/s0140-6736(21)00392-5. PMID 34062144. S2CID 235245552.
- ^ Prabhakar A, Kaiser JM, Novitch MB, Cornett EM, Urman RD, Kaye AD (March 2019). "The Role of Complementary and Alternative Medicine Treatments in Fibromyalgia: a Comprehensive Review". Current Rheumatology Reports. 21 (5): 14. doi:10.1007/s11926-019-0814-0. PMID 30830504. S2CID 73482737.
- ^ Macfarlane GJ, Kronisch C, Atzeni F, Häuser W, Choy EH, Amris K, et al. (December 2017). "EULAR recommendations for management of fibromyalgia" (PDF). Annals of the Rheumatic Diseases. 76 (12): e54. doi:10.1136/annrheumdis-2017-211587. PMID 28476880. S2CID 26251476. Archived (PDF) from the original on 8 February 2023. Retrieved 4 March 2023.
- ^ Häuser W, Fitzcharles MA (March 2018). "Facts and myths pertaining to fibromyalgia". Dialogues in Clinical Neuroscience. 20 (1): 53–62. doi:10.31887/dcns.2018.20.1/whauser. PMC 6016048. PMID 29946212.
- ^ Mascarenhas RO, Souza MB, Oliveira MX, Lacerda AC, Mendonça VA, Henschke N, Oliveira VC (January 2021). "Association of Therapies With Reduced Pain and Improved Quality of Life in Patients With Fibromyalgia: A Systematic Review and Meta-analysis". JAMA Internal Medicine. 181 (1): 104–112. doi:10.1001/jamainternmed.2020.5651. PMC 7589080. PMID 33104162.
- Kia S, Choy E (May 2017). "Update on Treatment Guideline in Fibromyalgia Syndrome with Focus on Pharmacology". Biomedicines. 5 (2): 20. doi:10.3390/biomedicines5020020. PMC 5489806. PMID 28536363.
- ^ Ibáñez-Vera AJ, Alvero-Cruz JR, García-Romero JC (2018). "Therapeutic physical exercise and supplements to treat fibromyalgia". Apunts. Medicina de l'Esport. 53 (197): 33–41. doi:10.1016/j.apunts.2017.07.001.
- ^ Häuser W, Eich W, Herrmann M, Nutzinger DO, Schiltenwolf M, Henningsen P (June 2009). "Fibromyalgia syndrome: classification, diagnosis, and treatment". Deutsches Ärzteblatt International. 106 (23): 383–391. doi:10.3238/arztebl.2009.0383. PMC 2712241. PMID 19623319.
- Health Information Team (February 2004). "Fibromyalgia". BUPA insurance. Archived from the original on 22 June 2006. Retrieved 24 August 2006.
- Yunus M, Masi AT, Calabro JJ, Miller KA, Feigenbaum SL (August 1981). "Primary fibromyalgia (fibrositis): clinical study of 50 patients with matched normal controls". Seminars in Arthritis and Rheumatism. 11 (1): 151–171. doi:10.1016/0049-0172(81)90096-2. PMID 6944796.
- "Fibro-". Dictionary.com. Archived from the original on 13 December 2009. Retrieved 21 May 2008.
- "Meaning of myo". 12 April 2009. Archived from the original on 12 April 2009. Retrieved 26 August 2012.
- "Meaning of algos". 12 April 2009. Archived from the original on 12 April 2009. Retrieved 26 August 2012.
- ^ Wolfe F (April 2009). "Fibromyalgia wars". The Journal of Rheumatology. 36 (4): 671–678. doi:10.3899/jrheum.081180. PMID 19342721. S2CID 2091976.
- Smythe HA, Moldofsky H (1977). "Two contributions to understanding of the "fibrositis" syndrome". Bulletin on the Rheumatic Diseases. 28 (1): 928–931. PMID 199304.
- Winfield JB (June 2007). "Fibromyalgia and related central sensitivity syndromes: twenty-five years of progress". Seminars in Arthritis and Rheumatism. 36 (6): 335–338. doi:10.1016/j.semarthrit.2006.12.001. PMID 17303220.
- ^ Inanici F, Yunus MB (October 2004). "History of fibromyalgia: past to present". Current Pain and Headache Reports. 8 (5): 369–378. doi:10.1007/s11916-996-0010-6. PMID 15361321. S2CID 42573740.
- Goldenberg DL (May 1987). "Fibromyalgia syndrome. An emerging but controversial condition". JAMA. 257 (20): 2782–2787. doi:10.1001/jama.257.20.2782. PMID 3553636.
- Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. (February 1990). "The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee". Arthritis and Rheumatism. 33 (2): 160–172. doi:10.1002/art.1780330203. PMID 2306288.
- ^ Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. (May 2010). "The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity". Arthritis Care & Research. 62 (5): 600–610. doi:10.1002/acr.20140. hdl:2027.42/75772. PMID 20461783. S2CID 17154205.
- ^ Clauw DJ, Arnold LM, McCarberg BH (September 2011). "The science of fibromyalgia". Mayo Clinic Proceedings. 86 (9): 907–911. doi:10.4065/mcp.2011.0206. PMC 3258006. PMID 21878603.
- "ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Archived from the original on 1 August 2018. Retrieved 9 April 2022.
- Gianlorenço AC, Costa V, Fabris-Moraes W, Menacho M, Alves LG, Martinez-Magallanes D, Fregni F (15 May 2024). "Cluster analysis in fibromyalgia: a systematic review". Rheumatology International. doi:10.1007/s00296-024-05616-2. ISSN 1437-160X. PMID 38748219.
- Besiroglu MD, Dursun MD (July 2019). "The association between fibromyalgia and female sexual dysfunction: a systematic review and meta-analysis of observational studies". International Journal of Impotence Research. 31 (4): 288–297. doi:10.1038/s41443-018-0098-3. PMID 30467351. S2CID 53717513.
- Zdebik N, Zdebik A, Bogusławska J, Przeździecka-Dołyk J, Turno-Kręcicka A (January 2021). "Fibromyalgia syndrome and the eye – A review". Survey of Ophthalmology. 66 (1): 132–137. doi:10.1016/j.survophthal.2020.05.006. PMID 32512032. S2CID 219548664.
- "Archived copy". academic.oup.com. Archived from the original on 21 May 2023. Retrieved 11 February 2024.
{{cite web}}: CS1 maint: archived copy as title (link) - "Fibromyalgia – Symptoms". nhs.uk. 20 October 2017. Archived from the original on 23 March 2018. Retrieved 21 October 2020.
- "Fibromyalgia - Symptoms". nhs.uk. 20 October 2017. Retrieved 11 April 2024.
- Kimura S, Toyoura M, Toyota Y, Takaoka Y (December 2020). "Serum concentrations of insulin-like growth factor-1 as a biomarker of improved circadian rhythm sleep-wake disorder in school-aged children". Journal of Clinical Sleep Medicine. 16 (12): 2073–2078. doi:10.5664/jcsm.8778. PMC 7848940. PMID 32876042.
- Spaeth M, Rizzi M, Sarzi-Puttini P (April 2011). "Fibromyalgia and sleep". Best Practice & Research. Clinical Rheumatology. 25 (2): 227–239. doi:10.1016/j.berh.2011.03.004. PMID 22094198.
- ^ Bradley LA (December 2009). "Pathophysiology of fibromyalgia". The American Journal of Medicine. 122 (12 Suppl): S22 – S30. doi:10.1016/j.amjmed.2009.09.008. PMC 2821819. PMID 19962493.
- Wolfe F, Rasker JJ, Ten Klooster P, Häuser W (December 2021). "Subjective Cognitive Dysfunction in Patients With and Without Fibromyalgia: Prevalence, Predictors, Correlates, and Consequences". Cureus. 13 (12): e20351. doi:10.7759/cureus.20351. PMC 8752385. PMID 35036191.
- ^ Bell T, Trost Z, Buelow MT, Clay O, Younger J, Moore D, Crowe M (September 2018). "Meta-analysis of cognitive performance in fibromyalgia". Journal of Clinical and Experimental Neuropsychology. 40 (7): 698–714. doi:10.1080/13803395.2017.1422699. PMC 6151134. PMID 29388512.
- Berwick RJ, Siew S, Andersson DA, Marshall A, Goebel A (May 2021). "A Systematic Review Into the Influence of Temperature on Fibromyalgia Pain: Meteorological Studies and Quantitative Sensory Testing". The Journal of Pain. 22 (5): 473–486. doi:10.1016/j.jpain.2020.12.005. PMID 33421589. S2CID 231437516.
- Staud R, Godfrey MM, Robinson ME (August 2021). "Fibromyalgia Patients Are Not Only Hypersensitive to Painful Stimuli But Also to Acoustic Stimuli". The Journal of Pain. 22 (8): 914–925. doi:10.1016/j.jpain.2021.02.009. PMID 33636370. S2CID 232066286.
- ^ Kleykamp BA, Ferguson MC, McNicol E, Bixho I, Arnold LM, Edwards RR, et al. (February 2021). "The Prevalence of Psychiatric and Chronic Pain Comorbidities in Fibromyalgia: an ACTTION systematic review". Seminars in Arthritis and Rheumatism. 51 (1): 166–174. doi:10.1016/j.semarthrit.2020.10.006. PMID 33383293. S2CID 229948862.
- Habibi Asgarabad M, Salehi Yegaei P, Jafari F, Azami-Aghdash S, Lumley MA (March 2023). "The relationship of alexithymia to pain and other symptoms in fibromyalgia: A systematic review and meta-analysis". European Journal of Pain. 27 (3): 321–337. doi:10.1002/ejp.2064. PMID 36471652. S2CID 254273680.
- ^ Fitzcharles MA, Perrot S, Häuser W (October 2018). "Comorbid fibromyalgia: A qualitative review of prevalence and importance". European Journal of Pain. 22 (9): 1565–1576. doi:10.1002/ejp.1252. PMID 29802812. S2CID 44068037.
- Yepez D, Grandes XA, Talanki Manjunatha R, Habib S, Sangaraju SL (May 2022). "Fibromyalgia and Depression: A Literature Review of Their Shared Aspects". Cureus. 14 (5): e24909. doi:10.7759/cureus.24909. PMC 9187156. PMID 35698706.
- Løge-Hagen JS, Sæle A, Juhl C, Bech P, Stenager E, Mellentin AI (February 2019). "Prevalence of depressive disorder among patients with fibromyalgia: Systematic review and meta-analysis". Journal of Affective Disorders. 245: 1098–1105. doi:10.1016/j.jad.2018.12.001. PMID 30699852. S2CID 73411416.
- Bruce DF, PhD. "Fibromyalgia and Depression". WebMD. Retrieved 1 April 2024.
- ^ Ramírez-Morales R, Bermúdez-Benítez E, Martínez-Martínez LA, Martínez-Lavín M (August 2022). "Clinical overlap between fibromyalgia and myalgic encephalomyelitis. A systematic review and meta-analysis". Autoimmunity Reviews. 21 (8): 103129. doi:10.1016/j.autrev.2022.103129. PMID 35690247.
- ^ Goldenberg DL (2024). "How to understand the overlap of long COVID, chronic fatigue syndrome/myalgic encephalomyelitis, fibromyalgia and irritable bowel syndromes". Seminars in Arthritis and Rheumatism. 67: 152455. doi:10.1016/j.semarthrit.2024.152455. PMID 38761526.
- Anderson G, Maes M (December 2020). "Mitochondria and immunity in chronic fatigue syndrome". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 103: 109976. doi:10.1016/j.pnpbp.2020.109976. PMID 32470498. S2CID 219104988.
- Valencia C, Fatima H, Nwankwo I, Anam M, Maharjan S, Amjad Z, et al. (October 2022). "A Correlation Between the Pathogenic Processes of Fibromyalgia and Irritable Bowel Syndrome in the Middle-Aged Population: A Systematic Review". Cureus. 14 (10): e29923. doi:10.7759/cureus.29923. PMC 9635936. PMID 36381861.
- D'Onghia M, Ciaffi J, Lisi L, Mancarella L, Ricci S, Stefanelli N, et al. (April 2021). "Fibromyalgia and obesity: A comprehensive systematic review and meta-analysis". Seminars in Arthritis and Rheumatism. 51 (2): 409–424. doi:10.1016/j.semarthrit.2021.02.007. PMID 33676126. S2CID 232136088.
- Alsiri N, Alhadhoud M, Alkatefi T, Palmer S (February 2023). "The concomitant diagnosis of fibromyalgia and connective tissue disorders: A systematic review" (PDF). Seminars in Arthritis and Rheumatism. 58: 152127. doi:10.1016/j.semarthrit.2022.152127. PMID 36462303. S2CID 253650110. Archived (PDF) from the original on 7 January 2024. Retrieved 7 January 2024.
- Kocyigit BF, Akyol A (March 2023). "Coexistence of fibromyalgia syndrome and inflammatory rheumatic diseases, and autonomic cardiovascular system involvement in fibromyalgia syndrome". Clinical Rheumatology. 42 (3): 645–652. doi:10.1007/s10067-022-06385-8. PMID 36151442. S2CID 252496799.
- He J (2024). "Fibromyalgia in Obstructive Sleep Apnea-hypopnea Syndrome: A Systematic Review and Meta-analysis". Frontiers in Physiology. 15. doi:10.3389/fphys.2024.1394865. PMC 11144865. PMID 38831795.
- Padhan P, Maikap D, Pathak M (2023). "Restless leg syndrome in rheumatic conditions: Its prevalence and risk factors, a meta-analysis". International Journal of Rheumatic Diseases. 26 (6): 1111–1119. doi:10.1111/1756-185X.14710. ISSN 1756-1841. PMID 37137528. S2CID 258484602. Archived from the original on 28 July 2023. Retrieved 28 July 2023.
- Goldberg N, Tamam S, Weintraub AY (December 2022). "The association between overactive bladder and fibromyalgia: A systematic review and meta-analysis". International Journal of Gynaecology and Obstetrics. 159 (3): 630–641. doi:10.1002/ijgo.14290. PMID 35641437. S2CID 249236213.
- Sarzi-Puttini P, Atzeni F, Mease PJ (April 2011). "Chronic widespread pain: from peripheral to central evolution". Best Practice & Research. Clinical Rheumatology. 25 (2): 133–139. doi:10.1016/j.berh.2011.04.001. ISSN 1532-1770. PMID 22094190.
- Schmidt-Wilcke T, Clauw DJ (19 July 2011). "Fibromyalgia: from pathophysiology to therapy". Nature Reviews. Rheumatology. 7 (9): 518–527. doi:10.1038/nrrheum.2011.98. ISSN 1759-4804. PMID 21769128.
- ^ D'Agnelli S, Arendt-Nielsen L, Gerra MC, Zatorri K, Boggiani L, Baciarello M, Bignami E (January 2019). "Fibromyalgia: Genetics and epigenetics insights may provide the basis for the development of diagnostic biomarkers". Molecular Pain. 15: 1744806918819944. doi:10.1177/1744806918819944. PMC 6322092. PMID 30486733.
- ^ Ablin JN, Buskila D (February 2015). "Update on the genetics of the fibromyalgia syndrome". Best Practice & Research. Clinical Rheumatology. 29 (1): 20–28. doi:10.1016/j.berh.2015.04.018. PMID 26266996.
- Lee YH, Choi SJ, Ji JD, Song GG (February 2012). "Candidate gene studies of fibromyalgia: a systematic review and meta-analysis". Rheumatology International. 32 (2): 417–426. doi:10.1007/s00296-010-1678-9. PMID 21120487. S2CID 6239018.
- Dutta D, Brummett CM, Moser SE, Fritsche LG, Tsodikov A, Lee S, et al. (May 2020). "Heritability of the Fibromyalgia Phenotype Varies by Age". Arthritis & Rheumatology. 72 (5): 815–823. doi:10.1002/art.41171. PMC 8372844. PMID 31736264.
- ^ Pinto AM, Luís M, Geenen R, Palavra F, Lumley MA, Ablin JN, Amris K, Branco J, Buskila D, Castelhano J, Castelo-Branco M, Crofford LJ, Fitzcharles MA, Häuser W, Kosek E (2023). "Neurophysiological and psychosocial mechanisms of fibromyalgia: A comprehensive review and call for an integrative model". Neuroscience & Biobehavioral Reviews. 151: 105235. doi:10.1016/j.neubiorev.2023.105235. hdl:1874/429361. ISSN 0149-7634. PMID 37207842. S2CID 258745974.
- Maletic V, Raison CL (June 2009). "Neurobiology of depression, fibromyalgia and neuropathic pain". Frontiers in Bioscience. 14 (14): 5291–5338. doi:10.2741/3598. PMID 19482616.
- ^ Martins DF, Viseux FJ, Salm DC, Ribeiro AC, da Silva HK, Seim LA, et al. (December 2021). "The role of the vagus nerve in fibromyalgia syndrome". Neuroscience and Biobehavioral Reviews. 131: 1136–1149. doi:10.1016/j.neubiorev.2021.10.021. PMID 34710514. S2CID 239772451.
- ^ Kaleycheva N, Cullen AE, Evans R, Harris T, Nicholson T, Chalder T (January 2021). "The role of lifetime stressors in adult fibromyalgia: systematic review and meta-analysis of case-control studies". Psychological Medicine. 51 (2): 177–193. doi:10.1017/S0033291720004547. PMID 33602373. S2CID 231955641.
- ^ Jung YH, Kim H, Lee D, Lee JY, Moon JY, Choi SH, Kang DH (January 2021). "Dysfunctional energy metabolisms in fibromyalgia compared with healthy subjects". Molecular Pain. 17: 17448069211012833. doi:10.1177/17448069211012833. PMC 8113919. PMID 33940974.
- Schmidt-Wilcke T, Clauw DJ (July 2011). "Fibromyalgia: from pathophysiology to therapy". Nature Reviews. Rheumatology. 7 (9): 518–527. doi:10.1038/nrrheum.2011.98. PMID 21769128. S2CID 20678671.
- Casale R, Sarzi-Puttini P, Botto R, Alciati A, Batticciotto A, Marotto D, Torta R (January 2019). "Fibromyalgia and the concept of resilience". Clinical and Experimental Rheumatology. 37 (1): 105–113. PMID 30747098. Archived from the original on 9 April 2022. Retrieved 9 April 2022.
- ^ Conversano C, Marchi L, Rebecca C, Carmassi C, Contena B, Bazzichi LM, Gemignani A (28 September 2018). "Personality Traits in Fibromyalgia (FM): Does FM Personality Exists? A Systematic Review". Clinical Practice and Epidemiology in Mental Health. 14 (1): 223–232. doi:10.2174/1745017901814010223. PMC 6166394. PMID 30294356.
Personality traits are often studied in patients with rheumatic diseases and, most of all, in those with fibromyalgia. However, the literature on this topic presents inconsistent results...Although in many studies FM patients are compared with healthy controls and personality differences are found, when comparison is made with other disorders with controlled depression, personality traits appear to be less relevant than before.
- ^ Tan AC, Jaaniste T, Champion D (5 May 2019). "Chronic Widespread Pain and Fibromyalgia Syndrome: Life-Course Risk Markers in Young People". Pain Research & Management. 2019: 6584753. doi:10.1155/2019/6584753. PMC 6525804. PMID 31191788.
- Roach K, Roberts J (August 2022). "A comprehensive summary of disease variants implicated in metal allergy". Journal of Toxicology and Environmental Health Part B: Critical Reviews. 25 (6): 279–341. Bibcode:2022JTEHB..25..279R. doi:10.1080/10937404.2022.2104981. PMC 9968405. PMID 35975293. S2CID 251623384.
- Fialho MF, Brum ES, Oliveira SM (2023). "Could the fibromyalgia syndrome be triggered or enhanced by COVID-19?". Inflammopharmacology. 31 (2): 633–651. doi:10.1007/s10787-023-01160-w. ISSN 0925-4692. PMC 9970139. PMID 36849853.
- de Tommaso M, Vecchio E, Nolano M (March 2022). "The puzzle of fibromyalgia between central sensitization syndrome and small fiber neuropathy: a narrative review on neurophysiological and morphological evidence". Neurological Sciences. 43 (3): 1667–1684. doi:10.1007/s10072-021-05806-x. PMID 35028777. S2CID 245909381.
- ^ Gkouvi A, Tsiogkas SG, Bogdanos DP, Gika H, Goulis DG, Grammatikopoulou MG (23 April 2024). "Proteomics in Patients with Fibromyalgia Syndrome: A Systematic Review of Observational Studies". Current Pain and Headache Reports. doi:10.1007/s11916-024-01244-4. ISSN 1531-3433. PMC 11271354. PMID 38652420.
- den Boer C, Dries L, Terluin B, van der Wouden JC, Blankenstein AH, van Wilgen CP, et al. (February 2019). "Central sensitization in chronic pain and medically unexplained symptom research: A systematic review of definitions, operationalizations and measurement instruments". Journal of Psychosomatic Research. 117: 32–40. doi:10.1016/j.jpsychores.2018.12.010. PMID 30665594. S2CID 58565532.
- Bidari A, Ghavidel-Parsa B (October 2022). "Nociplastic pain concept, a mechanistic basis for pragmatic approach to fibromyalgia". Clinical Rheumatology. 41 (10): 2939–2947. doi:10.1007/s10067-022-06229-5. PMID 35701625. S2CID 249650477.
- Nijs J, Lahousse A, Kapreli E, Bilika P, Saraçoğlu İ, Malfliet A, et al. (July 2021). "Nociplastic Pain Criteria or Recognition of Central Sensitization? Pain Phenotyping in the Past, Present and Future". Journal of Clinical Medicine. 10 (15): 3203. doi:10.3390/jcm10153203. PMC 8347369. PMID 34361986.
- ^ Martínez-Lavín M (December 2018). "Fibromyalgia and small fiber neuropathy: the plot thickens!". Clinical Rheumatology. 37 (12): 3167–3171. doi:10.1007/s10067-018-4300-2. PMID 30238382. S2CID 52306843.
- Martínez-Lavín M (February 2021). "Dorsal root ganglia: fibromyalgia pain factory?". Clinical Rheumatology. 40 (2): 783–787. doi:10.1007/s10067-020-05528-z. PMC 7787228. PMID 33409721.
- ^ Martinez-Lavin M, Holman AJ (2021). "Heart rate variability analysis in rheumatology: past, present… and future?". Clinical and Experimental Rheumatology. 39 (5): 927–930. doi:10.55563/clinexprheumatol/nmvth1. PMID 34464245. S2CID 237375381.
- Figueroa A, Kingsley JD, McMillan V, Panton LB (January 2008). "Resistance exercise training improves heart rate variability in women with fibromyalgia". Clinical Physiology and Functional Imaging. 28 (1): 49–54. doi:10.1111/j.1475-097X.2007.00776.x. PMID 18005081. S2CID 40592827.
- Park HY, Jung WS, Kim J, Hwang H, Lim K (March 2020). "Twelve Weeks of Aerobic Exercise at the Lactate Threshold Improves Autonomic Nervous System Function, Body Composition, and Aerobic Performance in Women with Obesity". Journal of Obesity & Metabolic Syndrome. 29 (1): 67–75. doi:10.7570/jomes19063. PMC 7118007. PMID 32045515.
- ^ Pinto AM, Geenen R, Wager TD, Lumley MA, Häuser W, Kosek E, et al. (January 2023). "Emotion regulation and the salience network: a hypothetical integrative model of fibromyalgia". Nature Reviews. Rheumatology. 19 (1): 44–60. doi:10.1038/s41584-022-00873-6. hdl:1874/426650. PMID 36471023. S2CID 254273384.
- ^ Singh L, Kaur A, Bhatti MS, Bhatti R (July 2019). "Possible Molecular Mediators Involved and Mechanistic Insight into Fibromyalgia and Associated Co-morbidities". Neurochemical Research. 44 (7): 1517–1532. doi:10.1007/s11064-019-02805-5. PMID 31004261. S2CID 123945497.
- ^ Bellato E, Marini E, Castoldi F, Barbasetti N, Mattei L, Bonasia DE, Blonna D (1 January 2012). "Fibromyalgia syndrome: etiology, pathogenesis, diagnosis, and treatment". Pain Research and Treatment. 2012: 426130. doi:10.1155/2012/426130. PMC 3503476. PMID 23213512.
- ^ Feraco P, Bacci A, Pedrabissi F, Passamonti L, Zampogna G, Pedrabissi F, et al. (October 2011). "Metabolic abnormalities in pain-processing regions of patients with fibromyalgia: a 3T MR spectroscopy study". AJNR. American Journal of Neuroradiology. 32 (9): 1585–1590. doi:10.3174/ajnr.A2550. PMC 7965402. PMID 21799042.
- ^ Xin M, Qu Y, Peng X, Zhu D, Cheng S (9 May 2023). "A systematic review and meta-analysis of voxel-based morphometric studies of fibromyalgia". Frontiers in Neuroscience. 17. doi:10.3389/fnins.2023.1164145. ISSN 1662-453X. PMC 10203234. PMID 37229427.
- ^ Lin C, Lee SH, Weng HH (1 January 2016). "Gray Matter Atrophy within the Default Mode Network of Fibromyalgia: A Meta-Analysis of Voxel-Based Morphometry Studies". BioMed Research International. 2016: 7296125. doi:10.1155/2016/7296125. PMC 5220433. PMID 28105430.
- ^ Assavarittirong C, Samborski W, Grygiel-Górniak B (2022). "Oxidative Stress in Fibromyalgia: From Pathology to Treatment". Oxidative Medicine and Cellular Longevity. 2022: 1582432. doi:10.1155/2022/1582432. PMC 9556195. PMID 36246401.
- Coskun Benlidayi I (May 2019). "Role of inflammation in the pathogenesis and treatment of fibromyalgia". Rheumatology International. 39 (5): 781–791. doi:10.1007/s00296-019-04251-6. PMID 30756137. S2CID 131775636.
- ^ Uçeyler N, Häuser W, Sommer C (October 2011). "Systematic review with meta-analysis: cytokines in fibromyalgia syndrome". BMC Musculoskeletal Disorders. 12: 245. doi:10.1186/1471-2474-12-245. PMC 3234198. PMID 22034969.
- ^ Rodriguez-Pintó I, Agmon-Levin N, Howard A, Shoenfeld Y (October 2014). "Fibromyalgia and cytokines". Immunology Letters. 161 (2): 200–203. doi:10.1016/j.imlet.2014.01.009. PMID 24462815.
- Dell'Osso L, Bazzichi L, Baroni S, Falaschi V, Conversano C, Carmassi C, Marazziti D (1 January 2015). "The inflammatory hypothesis of mood spectrum broadened to fibromyalgia and chronic fatigue syndrome". Clinical and Experimental Rheumatology. 33 (1 Suppl 88): S109 – S116. PMID 25786052.
- ^ Bazzichi L, Giacomelli C, Consensi A, Giorgi V, Batticciotto A, Di Franco M, Sarzi-Puttini P (2020). "One year in review 2020: fibromyalgia". Clinical and Experimental Rheumatology. 38 (1): 3–8. PMID 32116216.
- Littlejohn G (November 2015). "Neurogenic neuroinflammation in fibromyalgia and complex regional pain syndrome". Nature Reviews. Rheumatology. 11 (11): 639–648. doi:10.1038/nrrheum.2015.100. PMID 26241184. S2CID 4368913.
- Erdrich S, Hawrelak JA, Myers SP, Harnett JE (March 2020). "Determining the association between fibromyalgia, the gut microbiome and its biomarkers: A systematic review". BMC Musculoskeletal Disorders. 21 (1): 181. doi:10.1186/s12891-020-03201-9. PMC 7083062. PMID 32192466.
- Wang Y, Wei J, Zhang W, Doherty M, Zhang Y, Xie H, et al. (June 2022). "Gut dysbiosis in rheumatic diseases: A systematic review and meta-analysis of 92 observational studies". eBioMedicine. 80: 104055. doi:10.1016/j.ebiom.2022.104055. PMC 9120231. PMID 35594658.
- Minerbi A, Fitzcharles MA (January 2020). "Gut microbiome: pertinence in fibromyalgia". Clinical and Experimental Rheumatology. 38 (1): 99–104. PMID 32116215.
- Clos-Garcia M, Andrés-Marin N, Fernández-Eulate G, Abecia L, Lavín JL, van Liempd S, et al. (August 2019). "Gut microbiome and serum metabolome analyses identify molecular biomarkers and altered glutamate metabolism in fibromyalgia". eBioMedicine. 46: 499–511. doi:10.1016/j.ebiom.2019.07.031. PMC 6710987. PMID 31327695.
- Borenstein D (April 1995). "Prevalence and treatment outcome of primary and secondary fibromyalgia in patients with spinal pain". Spine. 20 (7): 796–800. doi:10.1097/00007632-199504000-00011. PMID 7701393. S2CID 30837539.
- Bengtsson A, Henriksson KG, Larsson J (July 1986). "Reduced high-energy phosphate levels in the painful muscles of patients with primary fibromyalgia". Arthritis and Rheumatism. 29 (7): 817–821. doi:10.1002/art.1780290701. PMID 3741498.
- Gerdle B, Ghafouri B, Lund E, Bengtsson A, Lundberg P, Ettinger-Veenstra HV, et al. (October 2020). "Evidence of Mitochondrial Dysfunction in Fibromyalgia: Deviating Muscle Energy Metabolism Detected Using Microdialysis and Magnetic Resonance". Journal of Clinical Medicine. 9 (11): 3527. doi:10.3390/jcm9113527. PMC 7693920. PMID 33142767.
- Srikuea R, Symons TB, Long DE, Lee JD, Shang Y, Chomentowski PJ, et al. (February 2013). "Association of fibromyalgia with altered skeletal muscle characteristics which may contribute to postexertional fatigue in postmenopausal women". Arthritis and Rheumatism. 65 (2): 519–528. doi:10.1002/art.37763. PMC 3558634. PMID 23124535.
- Shang Y, Gurley K, Symons B, Long D, Srikuea R, Crofford LJ, et al. (November 2012). "Noninvasive optical characterization of muscle blood flow, oxygenation, and metabolism in women with fibromyalgia". Arthritis Research & Therapy. 14 (6): R236. doi:10.1186/ar4079. PMC 3674608. PMID 23116302.
- Häuser W, Fitzcharles MA (March 2018). "Facts and myths pertaining to fibromyalgia". Dialogues in Clinical Neuroscience. 20 (1): 53–62. doi:10.31887/DCNS.2018.20.1/whauser. PMC 6016048. PMID 29946212.
- Wolfe F (August 2003). "Stop using the American College of Rheumatology criteria in the clinic". The Journal of Rheumatology. 30 (8): 1671–1672. PMID 12913920. Archived from the original on 14 October 2011.
- Wang SM, Han C, Lee SJ, Patkar AA, Masand PS, Pae CU (June 2015). "Fibromyalgia diagnosis: a review of the past, present and future". Expert Review of Neurotherapeutics. 15 (6): 667–679. doi:10.1586/14737175.2015.1046841. PMID 26035624. S2CID 2412984.
- Burckhardt CS, Clark SR, Bennett RM (May 1991). "The fibromyalgia impact questionnaire: development and validation". The Journal of Rheumatology. 18 (5): 728–733. PMID 1865419. Archived from the original on 16 May 2022. Retrieved 18 June 2022.
- ^ Bennett RM, Friend R, Jones KD, Ward R, Han BK, Ross RL (1 January 2009). "The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties". Arthritis Research & Therapy. 11 (4): R120. doi:10.1186/ar2783. PMC 2745803. PMID 19664287.
- "Fibromyalgia Impact Questionnaire (FIQ)". American College of Rheumatology. Archived from the original on 1 July 2022. Retrieved 18 June 2022.
- Seidenberg M, Haltiner A, Taylor MA, Hermann BB, Wyler A (February 1994). "Development and validation of a Multiple Ability Self-Report Questionnaire". Journal of Clinical and Experimental Neuropsychology. 16 (1): 93–104. doi:10.1080/01688639408402620. PMID 8150893.
- ^ Goldenberg DL (December 2009). "Diagnosis and differential diagnosis of fibromyalgia". The American Journal of Medicine (Review). 122 (12 Suppl): S14 – S21. doi:10.1016/j.amjmed.2009.09.007. PMID 19962492.
- ^ Häuser W, Perrot S, Sommer C, Shir Y, Fitzcharles MA (May 2017). "Diagnostic confounders of chronic widespread pain: not always fibromyalgia". Pain Reports. 2 (3): e598. doi:10.1097/PR9.0000000000000598. PMC 5741304. PMID 29392213.
- ^ Rossi A, Di Lollo AC, Guzzo MP, Giacomelli C, Atzeni F, Bazzichi L, Di Franco M (2015). "Fibromyalgia and nutrition: what news?". Clinical and Experimental Rheumatology. 33 (1 Suppl 88): S117 – S125. PMID 25786053.
- ^ Marchesoni A, De Marco G, Merashli M, McKenna F, Tinazzi I, Marzo-Ortega H, McGonagle DG (January 2018). "The problem in differentiation between psoriatic-related polyenthesitis and fibromyalgia". Rheumatology (Review). 57 (1): 32–40. doi:10.1093/rheumatology/kex079. PMID 28387854. S2CID 205309871.
- ^ Palazzi C, D'Amico E, D'Angelo S, Gilio M, Olivieri I (January 2016). "Rheumatic manifestations of hepatitis C virus chronic infection: Indications for a correct diagnosis". World Journal of Gastroenterology (Review). 22 (4): 1405–1410. doi:10.3748/wjg.v22.i4.1405. PMC 4721975. PMID 26819509.
- ^ Sommer C, Häuser W, Alten R, Petzke F, Späth M, Tölle T, et al. (June 2012). "[Drug therapy of fibromyalgia syndrome. Systematic review, meta-analysis and guideline]" (PDF). Schmerz. 26 (3): 297–310. doi:10.1007/s00482-012-1172-2. PMID 22760463. S2CID 1348989. Archived from the original (PDF) on 16 February 2013.
- ^ Fitzcharles MA, Shir Y, Ablin JN, Buskila D, Amital H, Henningsen P, Häuser W (2013). "Classification and clinical diagnosis of fibromyalgia syndrome: recommendations of recent evidence-based interdisciplinary guidelines". Evidence-Based Complementary and Alternative Medicine. 2013: 528952. doi:10.1155/2013/528952. PMC 3860136. PMID 24379886.
- ^ "Management | Canadian Guidelines for the Diagnosis and Management of Fibromyalgia". Archived from the original on 11 June 2013.
- Busch AJ, Barber KA, Overend TJ, Peloso PM, Schachter CL (October 2007). "Exercise for treating fibromyalgia syndrome". The Cochrane Database of Systematic Reviews (4): CD003786. doi:10.1002/14651858.CD003786.pub2. PMID 17943797.
- ^ Andrade A, Dominski FH, Sieczkowska SM (December 2020). "What we already know about the effects of exercise in patients with fibromyalgia: An umbrella review". Seminars in Arthritis and Rheumatism. 50 (6): 1465–1480. doi:10.1016/j.semarthrit.2020.02.003. PMID 32147091. S2CID 212638860.
- Masquelier E, D'haeyere J (October 2021). "Physical activity in the treatment of fibromyalgia". Joint Bone Spine. 88 (5): 105202. doi:10.1016/j.jbspin.2021.105202. PMID 33962033.
- McLoughlin MJ, Stegner AJ, Cook DB (June 2011). "The relationship between physical activity and brain responses to pain in fibromyalgia". The Journal of Pain. 12 (6): 640–651. doi:10.1016/j.jpain.2010.12.004. PMC 3111901. PMID 21330218.
- ^ Valim V, Natour J, Xiao Y, Pereira AF, Lopes BB, Pollak DF, et al. (November 2013). "Effects of physical exercise on serum levels of serotonin and its metabolite in fibromyalgia: a randomized pilot study". Revista Brasileira de Reumatologia (in Spanish). 53 (6): 538–541. doi:10.1016/j.rbr.2013.02.001. PMID 24477734.
- Genc A, Tur BS, Aytur YK, Oztuna D, Erdogan MF (July 2015). "Does aerobic exercise affect the hypothalamic-pituitary-adrenal hormonal response in patients with fibromyalgia syndrome?". Journal of Physical Therapy Science. 27 (7): 2225–2231. doi:10.1589/jpts.27.2225. PMC 4540854. PMID 26311959.
- ^ El-Shewy KM, Kunbaz A, Gad MM, Al-Husseini MJ, Saad AM, Sammour YM, Abdel-Daim MM (January 2019). "Hyperbaric oxygen and aerobic exercise in the long-term treatment of fibromyalgia: A narrative review". Biomedicine & Pharmacotherapy. 109: 629–638. doi:10.1016/j.biopha.2018.10.157. PMID 30399600. S2CID 53240356.
- Andrade A, Vilarino GT, Sieczkowska SM, Coimbra DR, Steffens RA, Vietta GG (March 2018). "Acute effects of physical exercises on the inflammatory markers of patients with fibromyalgia syndrome: A systematic review". Journal of Neuroimmunology. 316: 40–49. doi:10.1016/j.jneuroim.2017.12.007. PMID 29254627. S2CID 46879701.
- ^ Andrade A, Vilarino GT, Serafim TT, Pereira Júnior AA, de Souza CA, Sieczkowska SM (October 2019). "Modulation of Autonomic Function by Physical Exercise in Patients with Fibromyalgia Syndrome: A Systematic Review". PM&R. 11 (10): 1121–1131. doi:10.1002/pmrj.12158. PMID 30900831. S2CID 85448644.
- ^ Albuquerque ML, Monteiro D, Marinho DA, Vilarino GT, Andrade A, Neiva HP (November 2022). "Effects of different protocols of physical exercise on fibromyalgia syndrome treatment: systematic review and meta-analysis of randomized controlled trials". Rheumatology International. 42 (11): 1893–1908. doi:10.1007/s00296-022-05140-1. hdl:10400.8/7188. PMID 35604435. S2CID 248970279.
- ^ Estévez-López F, Maestre-Cascales C, Russell D, Álvarez-Gallardo IC, Rodriguez-Ayllon M, Hughes CM, et al. (April 2021). "Effectiveness of Exercise on Fatigue and Sleep Quality in Fibromyalgia: A Systematic Review and Meta-analysis of Randomized Trials". Archives of Physical Medicine and Rehabilitation. 102 (4): 752–761. doi:10.1016/j.apmr.2020.06.019. hdl:10481/68683. PMID 32721388. S2CID 220847961.
- Cuenca-Martínez F, Suso-Martí L, Fernández-Carnero J, Muñoz-Alarcos V, Sempere-Rubio N (2023). "Exercise-based interventions on sleep quality in patients with fibromyalgia syndrome: An umbrella and mapping review with meta-analysis". Seminars in Arthritis and Rheumatism. 61: 152216. doi:10.1016/j.semarthrit.2023.152216. PMID 37229847. S2CID 258597720.
- McVeigh JG, Lucas A, Hurley DA, Basford JR, Baxter GD (September 2003). "Patients' perceptions of exercise therapy in the treatment of fibromyalgia syndrome: a survey". Musculoskeletal Care. 1 (2): 98–107. doi:10.1002/msc.45. PMID 20217670.
- ^ Russell D, Álvarez Gallardo IC, Wilson I, Hughes CM, Davison GW, Sañudo B, McVeigh JG (March 2018). "'Exercise to me is a scary word': perceptions of fatigue, sleep dysfunction, and exercise in people with fibromyalgia syndrome-a focus group study". Rheumatology International. 38 (3): 507–515. doi:10.1007/s00296-018-3932-5. PMID 29340774. S2CID 3395036.
- Sanz-Baños Y, Pastor-Mira MÁ, Lledó A, López-Roig S, Peñacoba C, Sánchez-Meca J (October 2018). "Do women with fibromyalgia adhere to walking for exercise programs to improve their health? Systematic review and meta-analysis". Disability and Rehabilitation. 40 (21): 2475–2487. doi:10.1080/09638288.2017.1347722. PMID 28687050. S2CID 9032840.
- Barhorst EE, Andrae WE, Rayne TJ, Falvo MJ, Cook DB, Lindheimer JB (December 2020). "Elevated Perceived Exertion in People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Fibromyalgia: A Meta-analysis". Medicine and Science in Sports and Exercise. 52 (12): 2615–2627. doi:10.1249/MSS.0000000000002421. PMC 10200687. PMID 32555018. S2CID 219918068.
- Vancampfort D, McGrath RL, Hemmings L, Gillis V, Bernar K, Van Damme T (November 2022). "Physical activity correlates in people with fibromyalgia: a systematic review". Disability and Rehabilitation. 45 (25): 4165–4174. doi:10.1080/09638288.2022.2146911. PMID 36398698. S2CID 253627372.
- Ryan S (2013). "Care of patients with fibromyalgia: assessment and management". Nursing Standard. 28 (13): 37–43. doi:10.7748/ns2013.11.28.13.37.e7722. PMID 24279570.
- Majdoub F, Ben Nessib D, Ferjani HL, Kaffel D, Triki W, Maatallah K, Hamdi W (February 2023). "Non-pharmacological therapies in Fibromyalgia: New horizons for physicians, new hopes for patients". Musculoskeletal Care. 21 (3): 603–610. doi:10.1002/msc.1741. PMID 36757930. S2CID 256696861.
- Bidonde J, Busch AJ, Schachter CL, Overend TJ, Kim SY, Góes SM, et al. (June 2017). "Aerobic exercise training for adults with fibromyalgia". The Cochrane Database of Systematic Reviews. 2017 (6): CD012700. doi:10.1002/14651858.cd012700. PMC 6481524. PMID 28636204.
- ^ Bidonde J, Busch AJ, Schachter CL, Webber SC, Musselman KE, Overend TJ, et al. (May 2019). "Mixed exercise training for adults with fibromyalgia". The Cochrane Database of Systematic Reviews. 2019 (5): CD013340. doi:10.1002/14651858.cd013340. PMC 6931522. PMID 31124142.
- Kim SY, Busch AJ, Overend TJ, Schachter CL, van der Spuy I, Boden C, et al. (September 2019). "Flexibility exercise training for adults with fibromyalgia". The Cochrane Database of Systematic Reviews. 2019 (9): CD013419. doi:10.1002/14651858.CD013419. PMC 6718217. PMID 31476271.
- Vilarino GT, Andreato LV, de Souza LC, Branco JH, Andrade A (November 2021). "Effects of resistance training on the mental health of patients with fibromyalgia: a systematic review". Clinical Rheumatology. 40 (11): 4417–4425. doi:10.1007/s10067-021-05738-z. PMID 33987785. S2CID 234489153.
- Rodríguez-Domínguez ÁJ, Rebollo-Salas M, Chillón-Martínez R, Rosales-Tristancho A, Jiménez-Rejano JJ (17 July 2023). "Clinical relevance of resistance training in women with fibromyalgia: A systematic review and meta-analysis". European Journal of Pain. 28 (1): 21–36. doi:10.1002/ejp.2161. ISSN 1090-3801. PMID 37458315. S2CID 259949000.
- Bastos AC, Vilarino GT, de Souza LC, Dominski FH, Branco JH, Andrade A (15 May 2023). "Effects of resistance training on sleep of patients with fibromyalgia: A systematic review". Journal of Health Psychology. 28 (11): 1072–1084. doi:10.1177/13591053231172288. ISSN 1359-1053. PMID 37183814. S2CID 258687258. Archived from the original on 28 July 2023. Retrieved 28 July 2023.
- ^ da Silva JM, de Barros BS, Almeida GJ, O'Neil J, Imoto AM (March 2022). "Dosage of resistance exercises in fibromyalgia: evidence synthesis for a systematic literature review up-date and meta-analysis". Rheumatology International. 42 (3): 413–429. doi:10.1007/s00296-021-05025-9. PMID 34652480. S2CID 238991065.
- Li H, Chen J, Xu G, Duan Y, Huang D, Tang C, Liu J (September 2020). "The Effect of Tai Chi for Improving Sleep Quality: A Systematic Review and Meta-analysis". Journal of Affective Disorders. 274: 1102–1112. doi:10.1016/j.jad.2020.05.076. PMID 32663938. S2CID 219743962.
- Vasileios P, Styliani P, Nifon G, Pavlos S, Aris F, Ioannis P (November 2022). "Managing fibromyalgia with complementary and alternative medical exercise: a systematic review and meta-analysis of clinical trials". Rheumatology International. 42 (11): 1909–1923. doi:10.1007/s00296-022-05151-y. PMID 35796820. S2CID 250317143.
- Cheng CA, Chiu YW, Wu D, Kuan YC, Chen SN, Tam KW (October 2019). "Effectiveness of Tai Chi on fibromyalgia patients: A meta-analysis of randomized controlled trials". Complementary Therapies in Medicine. 46: 1–8. doi:10.1016/j.ctim.2019.07.007. PMID 31519264. S2CID 199039433.
- Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, et al. (October 2014). "Aquatic exercise training for fibromyalgia". The Cochrane Database of Systematic Reviews. 2014 (10): CD011336. doi:10.1002/14651858.cd011336. PMC 10638613. PMID 25350761.
- Lima TB, Dias JM, Mazuquin BF, da Silva CT, Nogueira RM, Marques AP, et al. (October 2013). "The effectiveness of aquatic physical therapy in the treatment of fibromyalgia: a systematic review with meta-analysis". Clinical Rehabilitation. 27 (10): 892–908. doi:10.1177/0269215513484772. PMID 23818412. S2CID 25701866.
- Perraton L, Machotka Z, Kumar S (November 2009). "Components of effective randomized controlled trials of hydrotherapy programs for fibromyalgia syndrome: A systematic review". Journal of Pain Research. 2: 165–173. doi:10.2147/JPR.S8052. PMC 3004626. PMID 21197303.
- Galvão-Moreira LV, de Castro LO, Moura EC, de Oliveira CM, Nogueira Neto J, Gomes LM, Leal PD (July 2021). "Pool-based exercise for amelioration of pain in adults with fibromyalgia syndrome: A systematic review and meta-analysis". Modern Rheumatology. 31 (4): 904–911. doi:10.1080/14397595.2020.1829339. PMID 32990113. S2CID 222167851.
- ^ Calles Plata I, Ortiz-Rubio A, Torres Sánchez I, Cabrera Martos I, Calvache Mateo A, Heredia-Ciuró A, Valenza MC (February 2023). "Effectiveness of aquatic therapy on sleep in persons with fibromyalgia. A meta-analysis". Sleep Medicine. 102: 76–83. doi:10.1016/j.sleep.2022.12.016. PMID 36603514. S2CID 255217819.
- Ma J, Zhang T, Li X, Chen X, Zhao Q (September 2022). "Effects of aquatic physical therapy on clinical symptoms, physical function, and quality of life in patients with fibromyalgia: A systematic review and meta-analysis". Physiotherapy Theory and Practice. 40 (2): 205–223. doi:10.1080/09593985.2022.2119906. PMID 36062580. S2CID 252079586.
- Correyero-León M, Medrano-de-la-Fuente R, Hernando-Garijo I, Jiménez-Del-Barrio S, Hernández-Lázaro H, Ceballos-Laita L, Mingo-Gómez MT (July 2023). "Effectiveness of aquatic training based on aerobic and strengthening exercises in patients with fibromyalgia: systematic review with meta-analysis". Explore. 20 (1): 27–38. doi:10.1016/j.explore.2023.07.003. PMID 37460329. S2CID 259580881.
- Bidonde J, Busch AJ, van der Spuy I, Tupper S, Kim SY, Boden C (September 2017). "Whole body vibration exercise training for fibromyalgia". The Cochrane Database of Systematic Reviews. 2017 (9): CD011755. doi:10.1002/14651858.cd011755.pub2. PMC 6483692. PMID 28950401.
- "FDA Approves First Drug for Treating Fibromyalgia" (Press release). U.S. Food and Drug Administration. 21 June 2007. Archived from the original on 21 February 2008. Retrieved 14 January 2008.
- European Medicines Agency. "Questions and answers on the recommendation for the refusal of the marketing authorisation for Milnacipran Pierre Fabre Médicament/Impulsor" (PDF). European Medicines Agency. Archived (PDF) from the original on 22 February 2014. Retrieved 30 May 2013.
- Martinez JE, Guimarães I (February 2024). ""Fibromyalgia - are there any new approaches?"". Best Pract Res Clin Rheumatol: 101933. doi:10.1016/j.berh.2024.101933. PMID 38355316.
- Häuser W, Wolfe F, Tölle T, Uçeyler N, Sommer C (April 2012). "The role of antidepressants in the management of fibromyalgia syndrome: a systematic review and meta-analysis". CNS Drugs. 26 (4): 297–307. doi:10.2165/11598970-000000000-00000. PMID 22452526. S2CID 207301478.
- Cording M, Derry S, Phillips T, Moore RA, Wiffen PJ (October 2015). "Milnacipran for pain in fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 2015 (10): CD008244. doi:10.1002/14651858.CD008244.pub3. PMC 6481368. PMID 26482422.
- ^ Welsch P, Üçeyler N, Klose P, Walitt B, Häuser W (February 2018). "Serotonin and noradrenaline reuptake inhibitors (SNRIs) for fibromyalgia". The Cochrane Database of Systematic Reviews. 2 (2): CD010292. doi:10.1002/14651858.CD010292.pub2. PMC 5846183. PMID 29489029.
- Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ (May 2019). "Amitriptyline for fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 5 (7): CD011824. doi:10.1002/14651858.CD011824. PMC 6485478. PMID 35658166.
- Migliorini F, Maffulli N, Eschweiler J, Baroncini A, Bell A, Colarossi G (17 July 2023). "Duloxetine for fibromyalgia syndrome: a systematic review and meta-analysis". Journal of Orthopaedic Surgery and Research. 18 (1): 504. doi:10.1186/s13018-023-03995-z. ISSN 1749-799X. PMC 10351165. PMID 37461044.
- Walitt B, Urrútia G, Nishishinya MB, Cantrell SE, Häuser W (June 2015). "Selective serotonin reuptake inhibitors for fibromyalgia syndrome". The Cochrane Database of Systematic Reviews. 2015 (6): CD011735. doi:10.1002/14651858.cd011735. PMC 4755337. PMID 26046493.
- ^ Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ (July 2015). "Amitriptyline for neuropathic pain in adults". The Cochrane Database of Systematic Reviews. 2015 (7): CD008242. doi:10.1002/14651858.CD011824. PMC 6485478. PMID 26146793.
- Welsch P, Bernardy K, Derry S, Moore RA, Häuser W (August 2018). "Mirtazapine for fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 8 (8): CD012708. doi:10.1002/14651858.CD012708.pub2. PMC 6513659. PMID 30080242.
- ^ Tort S, Urrútia G, Nishishinya MB, Walitt B (April 2012). "Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome". The Cochrane Database of Systematic Reviews (4): CD009807. doi:10.1002/14651858.cd009807. PMID 22513976.
- Wiffen PJ, Derry S, Bell RF, Rice AS, Tölle TR, Phillips T, Moore RA (June 2017). "Gabapentin for chronic neuropathic pain in adults". The Cochrane Database of Systematic Reviews. 6 (6): CD007938. doi:10.1002/14651858.CD007938.pub4. PMC 6452908. PMID 28597471.
- Derry S, Cording M, Wiffen PJ, Law S, Phillips T, Moore RA (September 2016). "Pregabalin for pain in fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 9 (9): CD011790. doi:10.1002/14651858.CD011790.pub2. PMC 6457745. PMID 27684492.
- Straube S, Moore RA, Paine J, Derry S, Phillips CJ, Hallier E, McQuay HJ (June 2011). "Interference with work in fibromyalgia: effect of treatment with pregabalin and relation to pain response". BMC Musculoskeletal Disorders. 12: 125. doi:10.1186/1471-2474-12-125. PMC 3118156. PMID 21639874.
- Nowell WB, Gavigan K, L Silverman S (May 2022). "Cannabis for Rheumatic Disease Pain: a Review of Current Literature". Current Rheumatology Reports. 24 (5): 119–131. doi:10.1007/s11926-022-01065-7. PMID 35486218. S2CID 248423563.
- Boehnke KF, Häuser W, Fitzcharles MA (July 2022). "Cannabidiol (CBD) in Rheumatic Diseases (Musculoskeletal Pain)". Current Rheumatology Reports. 24 (7): 238–246. doi:10.1007/s11926-022-01077-3. PMC 9062628. PMID 35503198.
- Bourke SL, Schlag AK, O'Sullivan SE, Nutt DJ, Finn DP (December 2022). "Cannabinoids and the endocannabinoid system in fibromyalgia: A review of preclinical and clinical research". Pharmacology & Therapeutics. 240: 108216. doi:10.1016/j.pharmthera.2022.108216. PMID 35609718. S2CID 248973512.
- Jain N, Moorthy A (June 2022). "Cannabinoids in rheumatology: Friend, foe or a bystander?". Musculoskeletal Care. 20 (2): 416–428. doi:10.1002/msc.1636. PMC 9322323. PMID 35476898.
- ^ MacLean AJ, Schwartz TL (May 2015). "Tramadol for the treatment of fibromyalgia". Expert Review of Neurotherapeutics. 15 (5): 469–475. doi:10.1586/14737175.2015.1034693. PMID 25896486. S2CID 26613022.
- Gaskell H, Moore RA, Derry S, Stannard C, et al. (Cochrane Pain, Palliative and Supportive Care Group) (September 2016). "Oxycodone for pain in fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 2016 (9): CD012329. doi:10.1002/14651858.CD012329. PMC 6457853. PMID 27582266.
- Thorpe J, Shum B, Moore RA, Wiffen PJ, Gilron I (February 2018). "Combination pharmacotherapy for the treatment of fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 2 (2): CD010585. doi:10.1002/14651858.CD010585.pub2. PMC 6491103. PMID 29457627.
- Goldenberg DL, Clauw DJ, Palmer RE, Clair AG (May 2016). "Opioid Use in Fibromyalgia: A Cautionary Tale". Mayo Clinic Proceedings (Review). 91 (5): 640–648. doi:10.1016/j.mayocp.2016.02.002. PMID 26975749. S2CID 20228209.
- Berger A. Patterns of use of opioids in patients with fibromyalgia In: EULAR; 2009:SAT0461
- Elijah J, Powell K, Smith MA (June 2022). "The Efficacy of Capsaicin on Sleep Quality and Fatigue in Fibromyalgia". Journal of Pain & Palliative Care Pharmacotherapy. 36 (2): 112–116. doi:10.1080/15360288.2022.2063468. PMID 35471125. S2CID 248389141.
- Staud R (August 2011). "Sodium oxybate for the treatment of fibromyalgia". Expert Opinion on Pharmacotherapy. 12 (11): 1789–1798. doi:10.1517/14656566.2011.589836. PMID 21679091. S2CID 33026097.
- See S, Ginzburg R (August 2008). "Choosing a skeletal muscle relaxant". American Family Physician. 78 (3): 365–370. PMID 18711953. Archived from the original on 1 April 2016.
- Kaltsas G, Tsiveriotis K (2000). "Fibromyalgia". Endotext. MDText.com, Inc. PMID 25905317. Archived from the original on 6 August 2020. Retrieved 20 February 2017.
- Heymann RE, Paiva ED, Helfenstein M, Pollak DF, Martinez JE, Provenza JR, et al. (2010). "Brazilian consensus on the treatment of fibromyalgia". Revista Brasileira de Reumatologia. 50 (1): 56–66. doi:10.1590/S0482-50042010000100006. PMID 21125141.
- Derry S, Wiffen PJ, Häuser W, Mücke M, Tölle TR, Bell RF, Moore RA (March 2017). "Oral nonsteroidal anti-inflammatory drugs for fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 3 (3): CD012332. doi:10.1002/14651858.CD012332.pub2. PMC 6464559. PMID 28349517.
- Walitt B, Klose P, Üçeyler N, Phillips T, Häuser W (June 2016). "Antipsychotics for fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 2016 (6): CD011804. doi:10.1002/14651858.cd011804.pub2. PMC 6457603. PMID 27251337.
- Walitt B, Klose P, Fitzcharles MA, Phillips T, Häuser W (July 2016). "Cannabinoids for fibromyalgia". The Cochrane Database of Systematic Reviews. 7 (7): CD011694. doi:10.1002/14651858.cd011694.pub2. PMC 6457965. PMID 27428009.
- ^ Kadayifci FZ, Bradley MJ, Onat AM, Shi HN, Zheng S (November 2022). "Review of nutritional approaches to fibromyalgia". Nutrition Reviews. 80 (12): 2260–2274. doi:10.1093/nutrit/nuac036. PMID 35674686.
- Nadal-Nicolás Y, Miralles-Amorós L, Martínez-Olcina M, Sánchez-Ortega M, Mora J, Martínez-Rodríguez A (May 2021). "Vegetarian and Vegan Diet in Fibromyalgia: A Systematic Review". International Journal of Environmental Research and Public Health. 18 (9): 4955. doi:10.3390/ijerph18094955. PMC 8125538. PMID 34066603.
- Haddad HW, Mallepalli NR, Scheinuk JE, Bhargava P, Cornett EM, Urits I, Kaye AD (December 2021). "The Role of Nutrient Supplementation in the Management of Chronic Pain in Fibromyalgia: A Narrative Review". Pain and Therapy. 10 (2): 827–848. doi:10.1007/s40122-021-00266-9. PMC 8586285. PMID 33909266.
- ^ Qu K, Li MX, Zhou YL, Yu P, Dong M (April 2022). "The efficacy of vitamin D in treatment of fibromyalgia: a meta-analysis of randomized controlled studies and systematic review". Expert Review of Clinical Pharmacology. 15 (4): 433–442. doi:10.1080/17512433.2022.2081151. PMID 35596576. S2CID 248948241.
- Mehrabani S, Askari G, Miraghajani M, Tavakoly R, Arab A (April 2019). "Effect of coenzyme Q10 supplementation on fatigue: A systematic review of interventional studies". Complementary Therapies in Medicine. 43: 181–187. doi:10.1016/j.ctim.2019.01.022. PMID 30935528. S2CID 86467031.
- Hargreaves IP, Mantle D (2021). "Targeted Treatment of Age-Related Fibromyalgia with Supplemental Coenzyme Q10" (PDF). In Guest PC (ed.). Reviews on New Drug Targets in Age-Related Disorders. Advances in Experimental Medicine and Biology. Vol. 1286. Cham: Springer International Publishing. pp. 77–85. doi:10.1007/978-3-030-55035-6_5. ISBN 978-3-030-55034-9. PMID 33725346. S2CID 232261388. Archived (PDF) from the original on 30 May 2023. Retrieved 17 May 2023.
- Erkilic B, Dalgic GS (January 2023). "The preventive role of vitamin D in the prevention and management of Fibromyalgia syndrome". Nutrition and Health. 29 (2): 223–229. doi:10.1177/02601060221144801. PMID 36591895. S2CID 255471623.
- ^ Hemati K, Amini Kadijani A, Sayehmiri F, Mehrzadi S, Zabihiyeganeh M, Hosseinzadeh A, Mirzaei A (February 2020). "Melatonin in the treatment of fibromyalgia symptoms: A systematic review". Complementary Therapies in Clinical Practice. 38: 101072. doi:10.1016/j.ctcp.2019.101072. PMID 31783341. S2CID 208497324.
- de Carvalho JF, Skare TL (2023). "Melatonin supplementation improves rheumatological disease activity: A systematic review". Clinical Nutrition ESPEN. 55: 414–419. doi:10.1016/j.clnesp.2023.04.011. PMID 37202076. S2CID 258273314. Archived from the original on 5 January 2024. Retrieved 28 July 2023.
- Arnold LM, Gebke KB, Choy EH (February 2016). "Fibromyalgia: management strategies for primary care providers". International Journal of Clinical Practice. 70 (2): 99–112. doi:10.1111/ijcp.12757. PMC 6093261. PMID 26817567.
- Okifuji A, Hare BD (December 2013). "Management of fibromyalgia syndrome: review of evidence". Pain and Therapy. 2 (2): 87–104. doi:10.1007/s40122-013-0016-9. PMC 4107911. PMID 25135147.
- Williams AC, Fisher E, Hearn L, Eccleston C (August 2020). "Psychological therapies for the management of chronic pain (excluding headache) in adults". The Cochrane Database of Systematic Reviews. 8 (8): CD007407. doi:10.1002/14651858.CD007407.pub4. PMC 7437545. PMID 32794606.
- Bernardy K, Klose P, Busch AJ, Choy EH, Häuser W (September 2013). "Cognitive behavioural therapies for fibromyalgia". The Cochrane Database of Systematic Reviews. 2013 (9): CD009796. doi:10.1002/14651858.CD009796.pub2. PMC 6481397. PMID 24018611.
- ^ Glombiewski JA, Sawyer AT, Gutermann J, Koenig K, Rief W, Hofmann SG (November 2010). "Psychological treatments for fibromyalgia: a meta-analysis". Pain. 151 (2): 280–295. doi:10.1016/j.pain.2010.06.011. PMID 20727679. S2CID 10513179.
- Bernardy K, Füber N, Köllner V, Häuser W (October 2010). "Efficacy of cognitive-behavioral therapies in fibromyalgia syndrome - a systematic review and metaanalysis of randomized controlled trials". The Journal of Rheumatology. 37 (10): 1991–2005. doi:10.3899/jrheum.100104. PMID 20682676. S2CID 11357808.
- ^ Whale K, Dennis J, Wylde V, Beswick A, Gooberman-Hill R (May 2022). "The effectiveness of non-pharmacological sleep interventions for people with chronic pain: a systematic review and meta-analysis". BMC Musculoskeletal Disorders. 23 (1): 440. doi:10.1186/s12891-022-05318-5. PMC 9092772. PMID 35546397.
- Eastwood F, Godfrey E (12 December 2023). "The efficacy, acceptability and safety of acceptance and commitment therapy for fibromyalgia – a systematic review and meta-analysis". British Journal of Pain. 18 (3): 243–256. doi:10.1177/20494637231221451. ISSN 2049-4637. PMC 11092929. PMID 38751564.
- Suso-Martí L, Cuenca-Martínez F, Alba-Quesada P, Muñoz-Alarcos V, Herranz-Gómez A, Varangot-Reille C, et al. (October 2022). "Effectiveness of Pain Neuroscience Education in Patients with Fibromyalgia: A Systematic Review and Meta-Analysis". Pain Medicine. 23 (11): 1837–1850. doi:10.1093/pm/pnac077. PMID 35587171.
- Duhn P, Wæhrens E, Pedersen M, Nielsen S, Locht H, Bliddal H, Christensen R, Amris K (10 May 2023). "Effectiveness of patient education as a stand-alone intervention for patients with chronic widespread pain and fibromyalgia: a systematic review and meta-analysis of randomized trials". Scandinavian Journal of Rheumatology. 52 (6): 654–663. doi:10.1080/03009742.2023.2192450. ISSN 0300-9742. PMID 37162478. S2CID 258588927. Archived from the original on 28 July 2023. Retrieved 28 July 2023.
- ^ Navarro-Ledesma S, Hamed-Hamed D, Gonzalez-Muñoz A, Pruimboom L (2024). "Impact of physical therapy techniques and common interventions on sleep quality in patients with chronic pain: A systematic review". Sleep Medicine Reviews. 76: 101937. doi:10.1016/j.smrv.2024.101937. hdl:10481/92720. PMID 38669729.
- Theadom A, Cropley M, Smith HE, Feigin VL, McPherson K (April 2015). "Mind and body therapy for fibromyalgia". The Cochrane Database of Systematic Reviews. 2015 (4): CD001980. doi:10.1002/14651858.CD001980.pub3. PMC 8409283. PMID 25856658.
- Deare JC, Zheng Z, Xue CC, Liu JP, Shang J, Scott SW, Littlejohn G (May 2013). "Acupuncture for treating fibromyalgia". The Cochrane Database of Systematic Reviews. 2013 (5): CD007070. doi:10.1002/14651858.CD007070.pub2. PMC 4105202. PMID 23728665.
- Cheng YC, Hsiao CY, Su MI, Chiu CC, Huang YC, Huang WL (February 2023). "Treating fibromyalgia with electrical neuromodulation: A systematic review and meta-analysis". Clinical Neurophysiology. 148: 17–28. doi:10.1016/j.clinph.2023.01.011. PMID 36774784. S2CID 256461558.
- Gikaro JM, Bigambo FM, Minde VM, Swai EA (20 April 2023). "Efficacy of electrophysical agents in fibromyalgia: A systematic review and network meta-analysis". Clinical Rehabilitation. 37 (10): 1295–1310. doi:10.1177/02692155231170450. ISSN 0269-2155. PMID 37082791. S2CID 258258250. Archived from the original on 28 July 2023. Retrieved 28 July 2023.
- Johnson MI, Claydon LS, Herbison GP, Jones G, Paley CA, et al. (Cochrane Pain, Palliative and Supportive Care Group) (October 2017). "Transcutaneous electrical nerve stimulation (TENS) for fibromyalgia in adults". The Cochrane Database of Systematic Reviews. 2017 (10): CD012172. doi:10.1002/14651858.CD012172.pub2. PMC 6485914. PMID 28990665.
- ^ Gibson W, Wand BM, Meads C, Catley MJ, O'Connell NE (April 2019). "Transcutaneous electrical nerve stimulation (TENS) for chronic pain - an overview of Cochrane Reviews". The Cochrane Database of Systematic Reviews. 4 (4): CD011890. doi:10.1002/14651858.CD011890.pub3. PMC 6446021. PMID 30941745.
- ^ Lange G, Janal MN, Maniker A, Fitzgibbons J, Fobler M, Cook D, Natelson BH (September 2011). "Safety and efficacy of vagus nerve stimulation in fibromyalgia: a phase I/II proof of concept trial". Pain Medicine. 12 (9): 1406–1413. doi:10.1111/j.1526-4637.2011.01203.x. PMC 3173600. PMID 21812908.
- Gao C, Zhu Q, Gao Z, Zhao J, Jia M, Li T (October 2022). "Can noninvasive Brain Stimulation Improve Pain and Depressive Symptoms in Patients With Neuropathic Pain? A Systematic Review and Meta-Analysis". Journal of Pain and Symptom Management. 64 (4): e203 – e215. doi:10.1016/j.jpainsymman.2022.05.002. PMID 35550165. S2CID 248715312.
- Teixeira PE, Pacheco-Barrios K, Branco LC, de Melo PS, Marduy A, Caumo W, et al. (November 2022). "The Analgesic Effect of Transcranial Direct Current Stimulation in Fibromyalgia: A Systematic Review, Meta-Analysis, and Meta-Regression of Potential Influencers of Clinical Effect". Neuromodulation. 26 (4): 715–727. doi:10.1016/j.neurom.2022.10.044. PMC 10203058. PMID 36435660. S2CID 253933442.
- Fernandes AM, Graven-Nielsen T, de Andrade DC (June 2022). "New updates on transcranial magnetic stimulation in chronic pain". Current Opinion in Supportive and Palliative Care. 16 (2): 65–70. doi:10.1097/SPC.0000000000000591. PMID 35639571. S2CID 249208885.
- ^ Choo YJ, Kwak SG, Chang MC (July 2022). "Effectiveness of Repetitive Transcranial Magnetic Stimulation on Managing Fibromyalgia: A Systematic Meta-Analysis". Pain Medicine. 23 (7): 1272–1282. doi:10.1093/pm/pnab354. PMID 34983056.
- ^ Sun P, Fang L, Zhang J, Liu Y, Wang G, Qi R (March 2022). "Repetitive Transcranial Magnetic Stimulation for Patients with Fibromyalgia: A Systematic Review with Meta-Analysis". Pain Medicine. 23 (3): 499–514. doi:10.1093/pm/pnab276. PMID 34542624.
- ^ Torres CB, Barona E, Manso J (2023). "A systematic review of EEG neurofeedback in fibromyalgia to treat psychological variables, chronic pain and general health". European Archives of Psychiatry and Clinical Neuroscience. 274 (4): 981–999. doi:10.1007/s00406-023-01612-y. PMC 11127810. PMID 37179502.
- Chen X, You J, Ma H, Zhou M, Huang C (January 2023). "Efficacy and safety of hyperbaric oxygen therapy for fibromyalgia: a systematic review and meta-analysis". BMJ Open. 13 (1): e062322. doi:10.1136/bmjopen-2022-062322. PMC 9872467. PMID 36690401.
- ^ Walitt B, Fitzcharles MA, Hassett AL, Katz RS, Häuser W, Wolfe F (October 2011). "The longitudinal outcome of fibromyalgia: a study of 1555 patients". The Journal of Rheumatology. 38 (10): 2238–2246. doi:10.3899/jrheum.110026. PMID 21765102. S2CID 207672626.
- Kashikar-Zuck S, Cunningham N, Peugh J, Black WR, Nelson S, Lynch-Jordan AM, et al. (February 2019). "Long-term outcomes of adolescents with juvenile-onset fibromyalgia into adulthood and impact of depressive symptoms on functioning over time". Pain. 160 (2): 433–441. doi:10.1097/j.pain.0000000000001415. PMC 6344278. PMID 30335681.
- Leino-Arjas P, Rajaleid K, Mekuria G, Nummi T, Virtanen P, Hammarström A (January 2018). "Trajectories of musculoskeletal pain from adolescence to middle age: the role of early depressive symptoms, a 27-year follow-up of the Northern Swedish Cohort". Pain. 159 (1): 67–74. doi:10.1097/j.pain.0000000000001065. PMID 28937577. S2CID 22164186.
- Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S (September 2001). "Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology". Pain. 93 (3): 247–257. doi:10.1016/s0304-3959(01)00324-4. PMID 11514084. S2CID 25457728.
- Treister-Goltzman Y, Peleg R (2023). "Fibromyalgia and mortality: a systematic review and meta-analysis". RMD Open. 9 (3): e003005. doi:10.1136/rmdopen-2023-003005. PMC 10335452. PMID 37429737. S2CID 259502501.
- Heidari F, Afshari M, Moosazadeh M (September 2017). "Prevalence of fibromyalgia in the general population and patients, a systematic review and meta-analysis". Rheumatology International. 37 (9): 1527–1539. doi:10.1007/s00296-017-3725-2. ISSN 0172-8172. PMID 28447207. S2CID 5043754.
- Wolfe F, Walitt B, Perrot S, Rasker JJ, Häuser W (13 September 2018). Sommer C (ed.). "Fibromyalgia diagnosis and biased assessment: Sex, prevalence and bias". PLOS ONE. 13 (9): e0203755. Bibcode:2018PLoSO..1303755W. doi:10.1371/journal.pone.0203755. ISSN 1932-6203. PMC 6136749. PMID 30212526.
- ^ D'Onghia M, Ciaffi J, Ruscitti P, Cipriani P, Giacomelli R, Ablin JN, Ursini F (October 2022). "The economic burden of fibromyalgia: A systematic literature review". Seminars in Arthritis and Rheumatism. 56: 152060. doi:10.1016/j.semarthrit.2022.152060. PMID 35849890. S2CID 250271053.
- Berenson A (14 January 2008). "Drug Approved. Is Disease Real?". The New York Times. Archived from the original on 10 May 2015. Retrieved 26 March 2014.
- "Fibromyalgia: An interview with Dr Frederick Wolfe, University of Kansas School of Medicine". 22 March 2013. Archived from the original on 29 May 2014. Retrieved 28 May 2014.
- Goldenberg DL (January 1995). "Fibromyalgia: why such controversy?". Annals of the Rheumatic Diseases. 54 (1): 3–5. doi:10.1136/ard.54.1.3. PMC 1005499. PMID 7880118.
- Hadlandsmyth K, Dailey DL, Rakel BA, Zimmerman MB, Vance CG, Merriwether EN, et al. (May 2020). "Somatic symptom presentations in women with fibromyalgia are differentially associated with elevated depression and anxiety". Journal of Health Psychology. 25 (6): 819–829. doi:10.1177/1359105317736577. PMC 6287969. PMID 29076404.
- Yunus MB (June 2007). "Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes". Seminars in Arthritis and Rheumatism. 36 (6): 339–356. doi:10.1016/j.semarthrit.2006.12.009. PMID 17350675.
External links
- Arthritis – Types – Fibromyalgia by the CDC
- Fibromyalgia by the National Institute of Arthritis and Musculoskeletal and Skin Diseases
- Fibromyalgia by the American College of Rheumatology
- Fibromyalgia by the NHS
| Classification | D |
|---|---|
| External resources |
| Neuropathic pain and fibromyalgia pharmacotherapies | |
|---|---|
| Monoaminergics |
|
| Ion channel blockers |
|
| Others |
|