| Revision as of 13:48, 9 May 2021 editAnomieBOT (talk | contribs)Bots6,573,090 editsm Dating maintenance tags: {{Cn}}← Previous edit | Latest revision as of 12:04, 6 January 2025 edit undoRich Farmbrough (talk | contribs)Edit filter managers, Autopatrolled, Extended confirmed users, File movers, Pending changes reviewers, Rollbackers, Template editors1,725,566 edits Copyedit. Update tag. | ||
| (35 intermediate revisions by 22 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Use dmy dates|date=January 2025}} | |||
| {{short description|Genital medical condition}} | {{short description|Genital medical condition}} | ||
| {{Infobox medical condition (new) | {{Infobox medical condition (new) | ||
| | name |
| name = Diphallia | ||
| | synonyms |
| synonyms = | ||
| | image |
| image = Diphallia 01.jpg | ||
| | image_size |
| image_size = 220px | ||
| | alt = The external male genitalia of a prepubescent male with a form of bifid diphallia with an anomaly around the mons pubis | |||
| | alt = | |||
| | caption = The external male genitalia of a prepubescent male with a form of bifid diphallia | |||
| | caption = Diphallia | |||
| | pronounce |
| pronounce = | ||
| | field |
| field = | ||
| | symptoms |
| symptoms = | ||
| | complications |
| complications = | ||
| | onset |
| onset = | ||
| | duration |
| duration = | ||
| | types |
| types = | ||
| | causes |
| causes = | ||
| | risks |
| risks = | ||
| | diagnosis |
| diagnosis = | ||
| | differential |
| differential = | ||
| | prevention |
| prevention = | ||
| | treatment |
| treatment = | ||
| | medication |
| medication = | ||
| | prognosis |
| prognosis = | ||
| | frequency |
| frequency = | ||
| | deaths |
| deaths = | ||
| }} | }} | ||
| '''Diphallia''', '''penile duplication''' ('''PD'''), '''diphallic terata''', or '''diphallasparatus''' |
'''Diphallia''', '''penile duplication''' ('''PD'''), '''diphallic terata''', or '''diphallasparatus''' is an extremely rare ] in which a male is born with two ].<ref name=":0">{{Cite journal|last=Tirtayasa|first=Pande|date=2013|title=Diphallia with Associated Anomalies: A Case Report and Literature Review|journal=Case Reports in Urology|volume=2013|page=192960|pmc=3870645|pmid=24383036|doi=10.1155/2013/192960|doi-access=free}}</ref><ref name=":1">{{Cite journal|last=Aparicio-Rodríguez|first=J|date=2010|title=Disorders of sexual development in genetic pediatrics: Three different ambiguous genitalia cases report from hospital para el Nino Poblano, Mexico|url=https://www.researchgate.net/publication/259764332|journal=International Journal of Genetics and Molecular Biology|volume=2 |issue=10|pages=207–216}}</ref> The first reported case was by ] in 1609.<ref name=j1>{{cite journal|url=http://www.jiaps.com/article.asp?issn=0971-9261;year=2000;volume=5;issue=1;spage=18;epage=21;aulast=Sharma;type=0|title=Concealed diphallus :a Case report and review of the literature|journal=Journal of Indian Association of Pediatric Surgeons |year = 2000 |volume = 5 | issue = 1 | pages =18–21|vauthors=Sharma KK, Jain R, Jain SK, Purohit A }}</ref><ref name=j2>{{cite journal|pmid=23056729|year=2010|last1=Mirshemirani|first1=AR|last2=Sadeghyian|first2=N|last3=Mohajerzadeh|first3=L|last4=Molayee|first4=H|last5=Ghaffari|first5=P|title=Diphallus: Report on six cases and review of the literature|volume=20|issue=3|pages=353–7|pmc=3446048|journal=Iranian Journal of Pediatrics}}</ref> Its occurrence is 1 in 5.5 million boys in the United States.<ref name=r1>{{cite web|url=http://today.reuters.com/News/CrisesArticle.aspx?storyId=DEL270522|title=Indian man wants op to remove extra organ|publisher=Reuters|access-date=18 August 2006|archive-url=https://web.archive.org/web/20070122012925/http://today.reuters.com/News/CrisesArticle.aspx?storyId=DEL270522|archive-date=22 January 2007|url-status=dead|date=19 August 2006}}</ref> | ||
| When diphallia is present, it is usually accompanied by ], ]l, ], ] or other ] anomalies. There is also a higher risk of ].<ref name=j2/> Infants born with |
When diphallia is present, it is usually accompanied by ], ]l, ], ] or other ] anomalies. There is also a higher risk of ].<ref name=j2 /> Infants born with diphallia and its related conditions have a higher death rate from various infections associated with their more complex renal or colorectal systems.{{Citation needed|date=January 2023}} | ||
| It is |
It is generally believed diphallia occurs in the ] between the 23rd and 25th days of ] when an injury, chemical stress, or malfunctioning ] genes hamper proper function of the ] of the fetal ] as the ] separates from the ] and ] to form the penis.{{Citation needed|date=January 2023}} | ||
| The first case was reported by Wecker in Bologna, Italy, in 1609, and since then, about one hundred cases have been reported.<ref name=":0" /><ref name=":2">{{Cite journal|last=Mirshemirani|first=Ali-Reza|date=2010|title=Diphallus: Report on Six Cases and Review of the Literature|journal=Iranian Journal of Pediatrics|volume=20 |issue=3|pages=353–357|pmid=23056729}}</ref> This condition has existed in humans since ancient times.<ref name=":3">{{Cite journal|last=Karabagli|first=Murat|date=2017|title=Bifid phallus with complete duplication and a separate scrotum in a German shepherd dog: a case report|journal=Veterinarni Medicina|volume=62 |issue=4|pages=226–230|doi=10.17221/16/2017-VETMED|doi-access=free}}</ref> The two external genitalia may vary in size and shape,<ref name=":4">{{Cite journal|last=Gyftopoulos|first=Kostis|date=2002|title=Clinical and embryologic aspects of penile duplication and associated anomalies|journal=Urology|volume=60 |issue=4|pages=675–679|doi=10.1016/S0090-4295(02)01874-5|pmid=12385932}}</ref> either lying beside each other in a ] plane or one above the other in a ] plane.<ref>{{Cite journal|last=Wojewski|first=A|date=1964|title=Total diphallia: A case of plastic repair|journal=Plastic and Reconstructive Surgery|volume=34 |issue=1|pages=84–6|doi=10.1097/00006534-196407000-00032|pmid=14104422}}</ref> | The first case was reported by Wecker in Bologna, Italy, in 1609, and since then, about one hundred cases have been reported.<ref name=":0" /><ref name=":2">{{Cite journal|last=Mirshemirani|first=Ali-Reza|date=2010|title=Diphallus: Report on Six Cases and Review of the Literature|journal=Iranian Journal of Pediatrics|volume=20 |issue=3|pages=353–357|pmid=23056729|pmc=3446048}}</ref> This condition has existed in humans since ancient times.<ref name=":3">{{Cite journal|last=Karabagli|first=Murat|date=2017|title=Bifid phallus with complete duplication and a separate scrotum in a German shepherd dog: a case report|journal=Veterinarni Medicina|volume=62 |issue=4|pages=226–230|doi=10.17221/16/2017-VETMED|doi-access=free}}</ref> The two external genitalia may vary in size and shape,<ref name=":4">{{Cite journal|last=Gyftopoulos|first=Kostis|date=2002|title=Clinical and embryologic aspects of penile duplication and associated anomalies|journal=Urology|volume=60 |issue=4|pages=675–679|doi=10.1016/S0090-4295(02)01874-5|pmid=12385932}}</ref> either lying beside each other in a ] plane or one above the other in a ] plane.<ref>{{Cite journal|last=Wojewski|first=A|date=1964|title=Total diphallia: A case of plastic repair|journal=Plastic and Reconstructive Surgery|volume=34 |issue=1|pages=84–6|doi=10.1097/00006534-196407000-00032|pmid=14104422}}</ref> | ||
| According to Schneider classification in 1928, double penis is classified into three groups: (a) glans diphallia, (b) bifid diphallia and (c) complete diphallia or double penis.<ref name=":5">{{Cite journal|last=Aboodi|first=M.d M|date=2005|title=Accessory Pseudophallus With Accessory Pseudoscrotum Detected During Antenatal Sonographic Scanning|journal=Journal of Ultrasound in Medicine|volume=24 |issue=8|pages=1163–1166|doi=10.7863/jum.2005.24.8.1163|pmid=16040834}}</ref> According to Vilanora and Raventos, in 1954, a fourth group called pseudodiphallia |
According to Schneider classification in 1928, double penis is classified into three groups: (a) glans diphallia, (b) bifid diphallia and (c) complete diphallia or double penis.<ref name=":5">{{Cite journal|last=Aboodi|first=M.d M|date=2005|title=Accessory Pseudophallus With Accessory Pseudoscrotum Detected During Antenatal Sonographic Scanning|journal=Journal of Ultrasound in Medicine|volume=24 |issue=8|pages=1163–1166|doi=10.7863/jum.2005.24.8.1163|pmid=16040834|s2cid=42171596}}</ref> According to Vilanora and Raventos, in 1954, a fourth group called pseudodiphallia was added.<ref name=":6">{{Cite journal|last=Kundal|first=Vijay|date=2013|title=A rare case of isolated complete diphallia and review of the literature|journal=BMJ Case Reports|volume=2013|pages=bcr2012008117|pmc=3603707|pmid=23413289|doi=10.1136/bcr-2012-008117}}</ref> | ||
| The current widely accepted classification, introduced by Aleem in 1972, classifies double penis into two groups: true diphallia and bifid phallus.<ref name=":4" /> True diphallia is caused by cleavage of pubic tubercle; bifid phallus is caused by separation of ].<ref name=":4" /><ref name=":7">{{Cite web|url=https://www.siu-urology.org/themes/web/assets/files/ICUD/pdf/congenital_anomalies.pdf|title=Congenital anomalies in children|last=deVries|first=Catherine|date=2013|access-date=18 April 2018}}</ref> Each of these two groups is further subdivided into partial or complete.<ref name=":4" /> True diphallia is where each phallus has two ] and a single ] containing a urethra.<ref name=":4" /><ref name=":7" /> True diphallia can be either complete with both penises similar in size, or partial when one of the phallia is smaller in size or immature, though structurally same as the larger phallus.<ref name=":4" /> In bifid phallus, each phallus has only one corpus cavernosum and one corpus spongiosum containing a urethra.<ref name=":4" /><ref name=":7" /> Separation of penises down to the base of the penile shaft is complete bifid, whereas to glans is partial bifid.<ref name=":4" /> For complete bifid phallus associated with anomalies, the anterior urethra is absent from each penis and the ] is situated in the skin between the two penises.<ref name=":8">{{Cite journal|last=Rossete-Cervantes|first=H|date=2016|title=Diphallia: a case report|url=http://revistamedica.imss.gob.mx/editorial/index.php/revista_medica/article/view/349/1149|journal=Revista Médica del Instituto Mexicano del Seguro Social|volume=54 |issue=3|pages=401–3|pmid=27100989|via=PubMed}}</ref> In partial bifid phallus, the duplication of urethra, ] and corpus spongiosum in one penis is incomplete, and there is only a corpus cavernosum and a spongiosum surrounding the functioning urethra in the other penis.<ref name=":9">{{Cite journal|last=Karagöz|first=Yeşim|s2cid=35108939|date=2014|title=Isolated penile duplication: case report and literature review|journal=Causapedia|volume=3|pages=762}}</ref> | The current widely accepted classification, introduced by Aleem in 1972, classifies double penis into two groups: true diphallia and bifid phallus.<ref name=":4" /> True diphallia is caused by cleavage of pubic tubercle; bifid phallus is caused by separation of ].<ref name=":4" /><ref name=":7">{{Cite web|url=https://www.siu-urology.org/themes/web/assets/files/ICUD/pdf/congenital_anomalies.pdf|title=Congenital anomalies in children|last=deVries|first=Catherine|date=2013|access-date=18 April 2018}}</ref> Each of these two groups is further subdivided into partial or complete.<ref name=":4" /> True diphallia is where each phallus has two ] and a single ] containing a urethra.<ref name=":4" /><ref name=":7" /> True diphallia can be either complete with both penises similar in size, or partial when one of the phallia is smaller in size or immature, though structurally same as the larger phallus.<ref name=":4" /> In bifid phallus, each phallus has only one corpus cavernosum and one corpus spongiosum containing a urethra.<ref name=":4" /><ref name=":7" /> Separation of penises down to the base of the penile shaft is complete bifid, whereas to glans is partial bifid.<ref name=":4" /> For complete bifid phallus associated with anomalies, the anterior urethra is absent from each penis and the ] is situated in the skin between the two penises.<ref name=":8">{{Cite journal|last=Rossete-Cervantes|first=H|date=2016|title=Diphallia: a case report|url=http://revistamedica.imss.gob.mx/editorial/index.php/revista_medica/article/view/349/1149|journal=Revista Médica del Instituto Mexicano del Seguro Social|volume=54 |issue=3|pages=401–3|pmid=27100989|via=PubMed}}</ref> In partial bifid phallus, the duplication of urethra, ] and corpus spongiosum in one penis is incomplete, and there is only a corpus cavernosum and a spongiosum surrounding the functioning urethra in the other penis.<ref name=":9">{{Cite journal|last=Karagöz|first=Yeşim|s2cid=35108939|date=2014|title=Isolated penile duplication: case report and literature review|journal=Causapedia|volume=3|pages=762}}</ref> | ||
| ==Notable clinical cases== | == Notable clinical cases == | ||
| Diphallia is usually accompanied by systemic anomalies; their extent varies, ranging from no associated anomaly to multiple anomalies including urogenital, gastrointestinal and musculoskeletal systems.<ref name=":0" /><ref name=":4" /> Penile duplication also varies from a single penis with double glans to complete double penises.<ref name=":2" /> The meatus may be normal at tip of glans, hypospadiac, or epispadiac; the scrotum may be normal or bifid.<ref name=":9" /> True diphallia is more likely accompanied with associated anomalies and malformations compared with bifid phallus.<ref name=":0" /> Infants born with diphallia have higher death rate due to infections associated with anomalies.<ref name=":8" /> | Diphallia is usually accompanied by systemic anomalies; their extent varies, ranging from no associated anomaly to multiple anomalies including urogenital, gastrointestinal and musculoskeletal systems.<ref name=":0" /><ref name=":4" /> Penile duplication also varies from a single penis with double glans to complete double penises.<ref name=":2" /> The meatus may be normal at tip of glans, hypospadiac, or epispadiac; the scrotum may be normal or bifid.<ref name=":9" /> True diphallia is more likely accompanied with associated anomalies and malformations compared with bifid phallus.<ref name=":0" /> Infants born with diphallia have higher death rate due to infections associated with anomalies.<ref name=":8" /> | ||
| === Complete true diphallia with associated anomalies === | |||
| ⚫ | A two-day-old male newborn,<ref name=":2" /> associated with complex genitourinary and ano-rectal malformation. He had imperforated anus, ], bifid scrotum, ]es on both glandes, two ] and two ], and had normal ], ]s and ]s. | ||
| ⚫ | === Partial true diphallia or pseudodiphallia, without associated anomalies === | ||
| ⚫ | A two-day-old male newborn,<ref name=":2" /> associated with complex genitourinary and ano-rectal malformation. He had imperforated anus, ], bifid scrotum, ]es on both glandes, two ] and two ], and had |
||
| ⚫ | Partial true diphallia corresponds to pseudodiphallia.<ref name=":0" /> Pseudodiphallia is formed from erectile tissue only, undifferentiated and non-functional.<ref name=":8" /> It is independent of the normal penis<ref name=":5" /> and can be removed surgically without problem.<ref name=":8" /> This rare case was reported,<ref name=":8" /> based on the age of the 83-year-old man when diphallia was only detected then when he was hospitalised, and also because of the absence of other anatomical malformations. The small, immature and nonfunctional penis protruded on one side of the large, normal penis. The secondary penis had glans but without urinary meatus. | ||
| === Complete bifid diphallia with associated anomalies === | |||
| ⚫ | A 12-year-old boy,<ref name=":0" /> associated with bifid ], ] and ]. He had two separate penises, similar in size and shape, each penis had an epispadia urethral meatus. He had bifid scrotum, one testicle on each side of the scrotum. A bowel loop-like structure was over the pubis region. This structure had no communication with any other structures. He had a single normal bladder and ureter. | ||
| ⚫ | === Partial bifid diphallia without associated anomalies === | ||
| ⚫ | Partial true diphallia corresponds to pseudodiphallia.<ref name=":0" /> Pseudodiphallia is formed from erectile tissue only, undifferentiated and non-functional.<ref name=":8" /> It is independent of the normal penis |
||
| ⚫ | A 15-year-old boy,<ref name=":9" /> apart from having two penises, had normal external genitalia. His two testicles were within normal scrotum and normally positioned. He had two unequal sized glans at tip of a thick penile ], and only urinated through the larger glans. He had a patent anus, one bladder, one normal urethra, normal ] and ] systems. | ||
| ⚫ | |||
| ⚫ | A 12-year-old boy,<ref name=":0" /> associated with bifid ], ] and ]. He had two separate penises, similar in size and shape, each penis had an epispadia urethral meatus. He had bifid scrotum, one testicle on each side of the scrotum. A bowel loop-like structure was over the pubis region. This structure had no communication with any other structures. He had a single normal bladder and ureter. |
||
| ⚫ | |||
| ⚫ | A 15-year-old boy,<ref name=":9" /> apart from having two penises, had normal external genitalia. His two testicles were within normal scrotum and normally positioned. He had two unequal sized glans at tip of a thick penile ], and only urinated through the larger glans. He had a patent anus, one bladder, one |
||
| == Male sex determination == | |||
| A male typically inherits an ] from ] and a ] from ]. The presence of the sex-determining-region of the Y chromosome, or ], determines the embryo being a male. Internal and external male genitalia development from bipotential gonad in embryo. ''SRY'' gene encodes testis-determining SRY factor (TDF) protein that promotes expression of several other genes such as SRY-box 9 ('']'') gene and ] (''SF1'') gene, causing differentiation of the medulla of bipotential gonad into testis by week six.<ref name=":10">{{Cite book|title=Human physiology: an integrated approach|last=Silverthorn|first=Dee|publisher=Pearson|year=2016|isbn=9781292094939|location=London|pages=827–829}}</ref> | |||
| == Internal genitalia development == | |||
| Sertoli cells of testes secrete ] (AMH) causing ] to degenerate, and Leydig cells of testes secrete testosterone and its derivative dihydrotestosterone (DHT) which is converted from ] by ], causing the ] to convert into ]s, ] and ] by week ten.{{cn|date=May 2021}} | |||
| == External genitalia development == | |||
| Initial development of external genital is independent of androgens before indifferent gonads differentiate into testes.<ref name=":7" /> It occurs by week eight of gestation, as directed by a number of genes. External genitalia develop from ] underlying ] lining ] on posterior wall of ].<ref name=":11">{{Cite web|url=http://www.columbia.edu/itc/hs/medical/humandev/2004/Chpt14-GonadalDev.pdf|title=Gonadal Development|last=Silverman|first=Ann|website=Department of Anatomy & Cell Biology|access-date=16 April 2018}}</ref> ] (PGCs), precursors of gametes,<ref>{{Cite journal|last=Magnúsdóttir|first=Erna|date=2014|title=How to make a primordial germ cell|journal=Development|volume=141 |issue=2|pages=245–252|doi=10.1242/dev.098269|pmid=24381195|doi-access=free}}</ref> migrate from egg sac into urogenital ridges, the site of gonad development in early embryonic development, by week six.<ref name=":12">{{Cite book|title=Histology: a text and atlas : with correlated cell and molecular biology|last=Ross|first=Michael|publisher=Wolters Kluwer/Lippincott Williams & Wilkins Health|year=2015|isbn=9781451187427|pages=791–792}}</ref> Genital ridges secrete a chemoattractant causing PGCs migration.<ref name=":11" /> Around week three, the ] cells migrate around the cloacal membrane forming a pair of cloacal folds laterally around the cloacal membrane.<ref name=":5" /><ref name=":7" /> From week six, the anterior cloacal folds fuse to form genital tubercle, the posterior cloacal folds divide into anterior urogenital folds and posterior anal folds.<ref name=":5" /><ref name=":13">{{Cite book|title=Campbell-Walsh urology|last=Wein|first=Alan|publisher=Elsevier|year=2016|isbn=9780323341486|location=Philadelphia}}</ref> The cloacal membrane, divides into urogenital and anal membranes,<ref name=":14">{{Cite web|url=https://discovery.lifemapsc.com/library/review-of-medical-embryology/chapter-102-development-of-the-male-external-genital-organs|title=Development of The Male External Genital Organs|last=Pansky|first=Ben|date=2015|website=LifeMap Discovery|access-date=13 April 2018}}</ref> breaks to form anterior urogenital opening and posterior anal opening respectively.<ref name=":14" /><ref>{{Cite journal|last=Van Der Werff|first=J|date=2000|title=Normal development of the male anterior urethra|url=ftp://newftp.epa.gov/COMPTOX/NCCT_Publication_Data/Knudsen/Virtual_Tissues_Male_Repro_Tox/Leung_2016_RTX/@Knowledgebase/vanderZanden00T61.pdf|journal=Teratology|volume=61 |issue=3|pages=172–83|pmid=10661906|doi=10.1002/(SICI)1096-9926(200003)61:3<172::AID-TERA4>3.0.CO;2-B}}</ref> Also from week six, ]s develop laterally of urogenital folds,<ref name=":5" /><ref name=":13" /> and labioscrotal swellings later form scrotal swellings.<ref name=":5" /><ref name=":13" /><ref name=":7" /> | |||
| Hormone-dependent development of external genitalia begins at about week eight.<ref name=":7" /> External genitalia differentiates under the action of ] and ]. DHT causes development of other male sex characteristics, such as prostate development, differentiation of external genitalia including genital tubercle elongation forming glans penis, urogenital folds forming penile shaft and labioscrotal swellings forming ] by week ten.<ref name=":10" /> Without DHT, male external genitalia will not develop during embryo growth.<ref name=":10" /><ref name=":12" /> Cells of urogenital ridges and underlying mesenchyme proliferate and form primary sex cords, which then undergo a series of mitotic division, under influence of TDF, develop into male gonad.<ref name=":12" /><ref name=":11" /> Elongation of genital tubercle forms developing glans penis.<ref name=":10" /> As phallus elongates, it pulls forward urethral folds that surrounds urogenital sinus together.<ref name=":14" /> Fusion of urogenital folds forms urogenital groove on ventral (under) side of phallus, and the groove gradually closes towards the glans forming the penile urethra.<ref name=":14" /><ref name=":15">{{Cite journal|url=https://www.academia.edu/31567090|title="PENILE DUPLICATION" Embryological basis and its clinical importance|last=Elumalai|first=Ganesh|date=2017|website=Elixir Embryology|access-date=14 April 2018}}</ref> The urogenital sinus differentiates into bladder and prostatic and posterior urethra.<ref name=":16">{{Cite journal|last=Levin|first=Terry|date=2007|title=Congenital anomalies of the male urethra|journal=Pediatric Radiology|volume=37|issue=9|pages=851–862|doi=10.1007/s00247-007-0495-0|pmid=17572890|pmc=1950215}}</ref> Erectile mesenchymal tissue develops into corpus spongiosum around the urethra and forms the glans penis, and into corpora cavenosa in the penile shaft.<ref name=":14" /> | |||
| == Cause == | == Cause == | ||
| Cause of diphallia is unknown,<ref name=":8" /> and also because its associated anomalies vary largely, it is impossible to give a simple, single explanation of its cause.<ref name=":7" /> But it is thought to have started from duplication of cloacal membrane in early embryonic development stages in the fetus, between third and sixth week of gestation,<ref name=":8" /><ref name=":3" /> because normal development of cloacal folds in the fetus is complete between this time.<ref name=":5" /><ref name=":15" /> | Cause of diphallia is unknown,<ref name=":8" /> and also because its associated anomalies vary largely, it is impossible to give a simple, single explanation of its cause.<ref name=":7" /> But it is thought to have started from duplication of cloacal membrane in early embryonic development stages in the fetus, between third and sixth week of gestation,<ref name=":8" /><ref name=":3" /> because normal development of cloacal folds in the fetus is complete between this time.<ref name=":5" /><ref name=":15">{{Cite journal|url=https://www.academia.edu/31567090|title="PENILE DUPLICATION" Embryological basis and its clinical importance|last=Elumalai|first=Ganesh|date=2017|website=Elixir Embryology|access-date=14 April 2018}}</ref> | ||
| Normal development of penis occurs with the fusion of cloacal tubercles at anterior end of urogenital sinus.<ref name=":0" /><ref name=":8" /> Mesenchyme migrate around cloacal membrane, proliferate and expand around cloacal plate, forming a pair of cloacal folds that fuse to form genital tubercle which develops into penis.<ref name=":8" /><ref name=":0" /><ref name=":7" /> If cloacal membrane is doubled, mesenchyme will migrate and surround both cloacal membranes, leading to the formation of two pairs of cloacal folds around two cloacal membranes, resulting in formation of two genital tubercles and thus two penises.<ref name=":0" /><ref name=":7" /> The concept of caudal duplication syndrome is used to explain the symptoms of diphallia with associated complex anomalies in lower abdomen and urinary tract.<ref name=":15" /><ref name=":7" /> Further, as mesenchyme migrate from more than one area, failure in migration and in the fusion of mesoderm results in formation of two genital tubercles <ref name=":0" /> and double penises, as well as producing associated anomalies such as double bladders, double urethra, double colons and imperforated anus.<ref name=":8" /><ref name=":7" /> Failure in proper fusion of urethral folds results in hypospadias.<ref>{{Cite journal|last=Elumalai|first=Ganesh|date=2017|title="HYPOSPADIAS" ITS EMBRYOLOGICAL BASIS AND CLINICAL IMPORTANCE|url=https://www.researchgate.net/publication/313468678|journal=Elixir Embryology|pages=44481–44487}}</ref> Failure in mesoderm cell migration results in epispadia.<ref name=":16" /> | Normal development of penis occurs with the fusion of cloacal tubercles at anterior end of urogenital sinus.<ref name=":0" /><ref name=":8" /> Mesenchyme migrate around cloacal membrane, proliferate and expand around cloacal plate, forming a pair of cloacal folds that fuse to form genital tubercle which develops into penis.<ref name=":8" /><ref name=":0" /><ref name=":7" /> If cloacal membrane is doubled, mesenchyme will migrate and surround both cloacal membranes, leading to the formation of two pairs of cloacal folds around two cloacal membranes, resulting in formation of two genital tubercles and thus two penises.<ref name=":0" /><ref name=":7" /> The concept of caudal duplication syndrome is used to explain the symptoms of diphallia with associated complex anomalies in lower abdomen and urinary tract.<ref name=":15" /><ref name=":7" /> Further, as mesenchyme migrate from more than one area, failure in migration and in the fusion of mesoderm results in formation of two genital tubercles <ref name=":0" /> and double penises, as well as producing associated anomalies such as double bladders, double urethra, double colons and imperforated anus.<ref name=":8" /><ref name=":7" /> Failure in proper fusion of urethral folds results in hypospadias.<ref>{{Cite journal|last=Elumalai|first=Ganesh|date=2017|title="HYPOSPADIAS" ITS EMBRYOLOGICAL BASIS AND CLINICAL IMPORTANCE|url=https://www.researchgate.net/publication/313468678|journal=Elixir Embryology|pages=44481–44487}}</ref> Failure in mesoderm cell migration results in epispadia.<ref name=":16">{{Cite journal|last=Levin|first=Terry|date=2007|title=Congenital anomalies of the male urethra|journal=Pediatric Radiology|volume=37|issue=9|pages=851–862|doi=10.1007/s00247-007-0495-0|pmid=17572890|pmc=1950215}}</ref> | ||
| Diphallia is a rare abnormal external genitalia. The cause is uncertain, but most scientists agree that diphallia is a defect of genital tubercle, and occurs at about week three of gestation, when caudal cell mass of mesoderm is affected by various external environmental factors including drugs, infections and malfunctioning ].<ref name=":6" /><ref name=":1" /> | Diphallia is a rare abnormal external genitalia. The cause is uncertain, but most scientists agree that diphallia is a defect of genital tubercle, and occurs at about week three of gestation, when caudal cell mass of mesoderm is affected by various external environmental factors including drugs, infections and malfunctioning ].<ref name=":6" /><ref name=":1" /> | ||
| Line 76: | Line 62: | ||
| == Treatment == | == Treatment == | ||
| Treatment is a case-by-case analysis taking into account considerations for medical and ethical reasons, and involves surgical excision of the non-functioning penis.<ref name=":0" /> | Treatment is a case-by-case analysis taking into account considerations for medical and ethical reasons, and involves surgical excision of the non-functioning penis.<ref name=":0" /> | ||
| ==See also== | == See also == | ||
| * ] | * ] | ||
| ⚫ | * ] | ||
| ⚫ | * ] | ||
| * ] | * ] | ||
| ⚫ | * ] | ||
| ⚫ | * ] | ||
| * ] | * ] | ||
| * ] | * ] | ||
| == References == | == References == | ||
| {{reflist}} | |||
| <references /> | |||
| ==Notes== | == Notes == | ||
| * A scientific paper of ''triphallia'' (three penises) in a marine snail was reported.({{cite journal|doi=10.4067/S0717-95022012000300003 |title=One Case of Triphallia in the Marine Snail ''Echinolittorina peruviana'' (Caenogastropoda: Littorinidae)|year=2012|last1=Castillo|first1=Viviana M|last2=Brown|first2=Donald I|journal=International Journal of Morphology|volume=30|issue=3|pages=791–796|doi-access=free}}) | * A scientific paper of ''triphallia'' (three penises) in a marine snail was reported.({{cite journal|doi=10.4067/S0717-95022012000300003 |title=One Case of Triphallia in the Marine Snail ''Echinolittorina peruviana'' (Caenogastropoda: Littorinidae)|year=2012|last1=Castillo|first1=Viviana M|last2=Brown|first2=Donald I|journal=International Journal of Morphology|volume=30|issue=3|pages=791–796|doi-access=free}}) | ||
| * In 2021, the first known case of a human with triphallia was recorded in Iraq.({{cite web|url=https://www.sciencetimes.com/articles/30463/20210403/baby-iraq-first-known-case-humans-born-three-male-genitalia.htm|title=Triphallia: First Human Case of Baby Born With Three Male Genitalia Reported}}) | * In 2021, the first known case of a human with triphallia was recorded in Iraq.({{cite web|url=https://www.sciencetimes.com/articles/30463/20210403/baby-iraq-first-known-case-humans-born-three-male-genitalia.htm|title=Triphallia: First Human Case of Baby Born With Three Male Genitalia Reported|date=3 April 2021}}) | ||
| ==Further reading== | == Further reading == | ||
| * Chadha R, Bagga D, Gupta S, Mahajan JK. (July 2001). 36 (7): E12, ]. ], ], ] | * Chadha R, Bagga D, Gupta S, Mahajan JK. (July 2001). 36 (7): E12, ]. ], ], ] | ||
| * Fleishman, Cooper (May 15, 2012). . HyperVocal. | |||
| == External links == | == External links == | ||
| Line 108: | Line 94: | ||
| | Orphanet = 227 | | Orphanet = 227 | ||
| }} | }} | ||
| {{Male congenital malformations of genital organs, indeterminate sex and pseudohermaphroditism}} | {{Male congenital malformations of genital organs, indeterminate sex and pseudohermaphroditism}} | ||
| {{Authority control}} | |||
| ] | ] | ||
| Line 114: | Line 102: | ||
| ] | ] | ||
| ] | ] | ||
| ] | |||
Latest revision as of 12:04, 6 January 2025
Genital medical condition Medical condition
| Diphallia | |
|---|---|
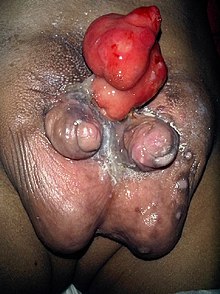 | |
| The external male genitalia of a prepubescent male with a form of bifid diphallia |
Diphallia, penile duplication (PD), diphallic terata, or diphallasparatus is an extremely rare developmental abnormality in which a male is born with two penises. The first reported case was by Johannes Jacob Wecker in 1609. Its occurrence is 1 in 5.5 million boys in the United States.
When diphallia is present, it is usually accompanied by renal, vertebral, hindgut, anorectal or other congenital anomalies. There is also a higher risk of spina bifida. Infants born with diphallia and its related conditions have a higher death rate from various infections associated with their more complex renal or colorectal systems.
It is generally believed diphallia occurs in the fetus between the 23rd and 25th days of gestation when an injury, chemical stress, or malfunctioning homeobox genes hamper proper function of the caudal cell mass of the fetal mesoderm as the urogenital sinus separates from the genital tubercle and rectum to form the penis.
The first case was reported by Wecker in Bologna, Italy, in 1609, and since then, about one hundred cases have been reported. This condition has existed in humans since ancient times. The two external genitalia may vary in size and shape, either lying beside each other in a sagittal plane or one above the other in a frontal plane.
According to Schneider classification in 1928, double penis is classified into three groups: (a) glans diphallia, (b) bifid diphallia and (c) complete diphallia or double penis. According to Vilanora and Raventos, in 1954, a fourth group called pseudodiphallia was added.
The current widely accepted classification, introduced by Aleem in 1972, classifies double penis into two groups: true diphallia and bifid phallus. True diphallia is caused by cleavage of pubic tubercle; bifid phallus is caused by separation of pubic tubercle. Each of these two groups is further subdivided into partial or complete. True diphallia is where each phallus has two corpora cavernosa and a single corpus spongiosum containing a urethra. True diphallia can be either complete with both penises similar in size, or partial when one of the phallia is smaller in size or immature, though structurally same as the larger phallus. In bifid phallus, each phallus has only one corpus cavernosum and one corpus spongiosum containing a urethra. Separation of penises down to the base of the penile shaft is complete bifid, whereas to glans is partial bifid. For complete bifid phallus associated with anomalies, the anterior urethra is absent from each penis and the prostatic urethra is situated in the skin between the two penises. In partial bifid phallus, the duplication of urethra, corpora cavernosa and corpus spongiosum in one penis is incomplete, and there is only a corpus cavernosum and a spongiosum surrounding the functioning urethra in the other penis.
Notable clinical cases
Diphallia is usually accompanied by systemic anomalies; their extent varies, ranging from no associated anomaly to multiple anomalies including urogenital, gastrointestinal and musculoskeletal systems. Penile duplication also varies from a single penis with double glans to complete double penises. The meatus may be normal at tip of glans, hypospadiac, or epispadiac; the scrotum may be normal or bifid. True diphallia is more likely accompanied with associated anomalies and malformations compared with bifid phallus. Infants born with diphallia have higher death rate due to infections associated with anomalies.
Complete true diphallia with associated anomalies
A two-day-old male newborn, associated with complex genitourinary and ano-rectal malformation. He had imperforated anus, hypospadias, bifid scrotum, meatuses on both glandes, two bladders and two colons, and had normal testes, kidneys and ureters.
Partial true diphallia or pseudodiphallia, without associated anomalies
Partial true diphallia corresponds to pseudodiphallia. Pseudodiphallia is formed from erectile tissue only, undifferentiated and non-functional. It is independent of the normal penis and can be removed surgically without problem. This rare case was reported, based on the age of the 83-year-old man when diphallia was only detected then when he was hospitalised, and also because of the absence of other anatomical malformations. The small, immature and nonfunctional penis protruded on one side of the large, normal penis. The secondary penis had glans but without urinary meatus.
Complete bifid diphallia with associated anomalies
A 12-year-old boy, associated with bifid scrotum, epispadia and pubic symphysis diastasis. He had two separate penises, similar in size and shape, each penis had an epispadia urethral meatus. He had bifid scrotum, one testicle on each side of the scrotum. A bowel loop-like structure was over the pubis region. This structure had no communication with any other structures. He had a single normal bladder and ureter.
Partial bifid diphallia without associated anomalies
A 15-year-old boy, apart from having two penises, had normal external genitalia. His two testicles were within normal scrotum and normally positioned. He had two unequal sized glans at tip of a thick penile shaft, and only urinated through the larger glans. He had a patent anus, one bladder, one normal urethra, normal gastrointestinal and genitourinary systems.
Cause
Cause of diphallia is unknown, and also because its associated anomalies vary largely, it is impossible to give a simple, single explanation of its cause. But it is thought to have started from duplication of cloacal membrane in early embryonic development stages in the fetus, between third and sixth week of gestation, because normal development of cloacal folds in the fetus is complete between this time.
Normal development of penis occurs with the fusion of cloacal tubercles at anterior end of urogenital sinus. Mesenchyme migrate around cloacal membrane, proliferate and expand around cloacal plate, forming a pair of cloacal folds that fuse to form genital tubercle which develops into penis. If cloacal membrane is doubled, mesenchyme will migrate and surround both cloacal membranes, leading to the formation of two pairs of cloacal folds around two cloacal membranes, resulting in formation of two genital tubercles and thus two penises. The concept of caudal duplication syndrome is used to explain the symptoms of diphallia with associated complex anomalies in lower abdomen and urinary tract. Further, as mesenchyme migrate from more than one area, failure in migration and in the fusion of mesoderm results in formation of two genital tubercles and double penises, as well as producing associated anomalies such as double bladders, double urethra, double colons and imperforated anus. Failure in proper fusion of urethral folds results in hypospadias. Failure in mesoderm cell migration results in epispadia.
Diphallia is a rare abnormal external genitalia. The cause is uncertain, but most scientists agree that diphallia is a defect of genital tubercle, and occurs at about week three of gestation, when caudal cell mass of mesoderm is affected by various external environmental factors including drugs, infections and malfunctioning homeobox genes.
Treatment
Treatment is a case-by-case analysis taking into account considerations for medical and ethical reasons, and involves surgical excision of the non-functioning penis.
See also
References
- ^ Tirtayasa, Pande (2013). "Diphallia with Associated Anomalies: A Case Report and Literature Review". Case Reports in Urology. 2013: 192960. doi:10.1155/2013/192960. PMC 3870645. PMID 24383036.
- ^ Aparicio-Rodríguez, J (2010). "Disorders of sexual development in genetic pediatrics: Three different ambiguous genitalia cases report from hospital para el Nino Poblano, Mexico". International Journal of Genetics and Molecular Biology. 2 (10): 207–216.
- Sharma KK, Jain R, Jain SK, Purohit A (2000). "Concealed diphallus :a Case report and review of the literature". Journal of Indian Association of Pediatric Surgeons. 5 (1): 18–21.
- ^ Mirshemirani, AR; Sadeghyian, N; Mohajerzadeh, L; Molayee, H; Ghaffari, P (2010). "Diphallus: Report on six cases and review of the literature". Iranian Journal of Pediatrics. 20 (3): 353–7. PMC 3446048. PMID 23056729.
- "Indian man wants op to remove extra organ". Reuters. 19 August 2006. Archived from the original on 22 January 2007. Retrieved 18 August 2006.
- ^ Mirshemirani, Ali-Reza (2010). "Diphallus: Report on Six Cases and Review of the Literature". Iranian Journal of Pediatrics. 20 (3): 353–357. PMC 3446048. PMID 23056729.
- ^ Karabagli, Murat (2017). "Bifid phallus with complete duplication and a separate scrotum in a German shepherd dog: a case report". Veterinarni Medicina. 62 (4): 226–230. doi:10.17221/16/2017-VETMED.
- ^ Gyftopoulos, Kostis (2002). "Clinical and embryologic aspects of penile duplication and associated anomalies". Urology. 60 (4): 675–679. doi:10.1016/S0090-4295(02)01874-5. PMID 12385932.
- Wojewski, A (1964). "Total diphallia: A case of plastic repair". Plastic and Reconstructive Surgery. 34 (1): 84–6. doi:10.1097/00006534-196407000-00032. PMID 14104422.
- ^ Aboodi, M.d M (2005). "Accessory Pseudophallus With Accessory Pseudoscrotum Detected During Antenatal Sonographic Scanning". Journal of Ultrasound in Medicine. 24 (8): 1163–1166. doi:10.7863/jum.2005.24.8.1163. PMID 16040834. S2CID 42171596.
- ^ Kundal, Vijay (2013). "A rare case of isolated complete diphallia and review of the literature". BMJ Case Reports. 2013: bcr2012008117. doi:10.1136/bcr-2012-008117. PMC 3603707. PMID 23413289.
- ^ deVries, Catherine (2013). "Congenital anomalies in children" (PDF). Retrieved 18 April 2018.
- ^ Rossete-Cervantes, H (2016). "Diphallia: a case report". Revista Médica del Instituto Mexicano del Seguro Social. 54 (3): 401–3. PMID 27100989 – via PubMed.
- ^ Karagöz, Yeşim (2014). "Isolated penile duplication: case report and literature review". Causapedia. 3: 762. S2CID 35108939.
- ^ Elumalai, Ganesh (2017). ""PENILE DUPLICATION" Embryological basis and its clinical importance". Elixir Embryology. Retrieved 14 April 2018.
- Elumalai, Ganesh (2017). ""HYPOSPADIAS" ITS EMBRYOLOGICAL BASIS AND CLINICAL IMPORTANCE". Elixir Embryology: 44481–44487.
- Levin, Terry (2007). "Congenital anomalies of the male urethra". Pediatric Radiology. 37 (9): 851–862. doi:10.1007/s00247-007-0495-0. PMC 1950215. PMID 17572890.
Notes
- A scientific paper of triphallia (three penises) in a marine snail was reported.(Castillo, Viviana M; Brown, Donald I (2012). "One Case of Triphallia in the Marine Snail Echinolittorina peruviana (Caenogastropoda: Littorinidae)". International Journal of Morphology. 30 (3): 791–796. doi:10.4067/S0717-95022012000300003.)
- In 2021, the first known case of a human with triphallia was recorded in Iraq.("Triphallia: First Human Case of Baby Born With Three Male Genitalia Reported". 3 April 2021.)
Further reading
- Chadha R, Bagga D, Gupta S, Mahajan JK. (July 2001). "Complete diphallia associated with features of covered exstrophy." 36 (7): E12, W.B. Saunders Company. National Center for Biotechnology Information, US National Library of Medicine, National Institutes of Health
External links
| Classification | D |
|---|---|
| External resources |
| Female and male congenital anomalies of the genitalia, including intersex and DSD | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Internal |
| ||||||||||||||||
| External |
| ||||||||||||||||