| Revision as of 20:50, 15 October 2007 view sourceMatt Lewis (talk | contribs)Extended confirmed users, Rollbackers9,196 edits →Risk reducers: Added a fuller picture to Vitamin E. Needs a few citations, which are available...← Previous edit | Latest revision as of 07:07, 26 December 2024 view source FropFrop (talk | contribs)Extended confirmed users1,008 editsm →Causes: Seems like the content has been moved a couple of times without anyone updating the article links | ||
| Line 1: | Line 1: | ||
| {{Short description|Progressive neurodegenerative disease}} | |||
| {{DiseaseDisorder infobox | |||
| {{Redirect|Alzheimer|the ]|Alois Alzheimer|other uses|Alzheimer (disambiguation)}} | |||
| | Name = Alzheimer's disease | |||
| {{Pp-semi-indef}} | |||
| | Image = Alzheimer dementia (3) presenile onset.jpg | |||
| {{Pp-move}} | |||
| | Caption = ] image of senile plaques seen in the cerebral cortex in a patient with Alzheimer disease of presenile onset. Silver impregnation. | |||
| {{Use British English|date=March 2022}} | |||
| | DiseasesDB = 490 | |||
| {{Use dmy dates|date=July 2023}} | |||
| | ICD10 = {{ICD10|G|30||g|30}}, {{ICD10|F|00||f|00}} | |||
| {{Cs1 config|name-list-style=vanc|display-authors=6}} | |||
| | ICD9 = {{ICD9|331.0}}, {{ICD9|290.1}} | |||
| {{Infobox medical condition (new) | |||
| | ICDO = | |||
| | name = Alzheimer's disease | |||
| | OMIM = 104300 | |||
| | image = Brain-ALZH.png | |||
| | MedlinePlus = 000760 | |||
| | caption = Diagram of a normal ] compared to the brain of a person with Alzheimer's | |||
| | eMedicineSubj = neuro | |||
| | pronounce = {{IPAc-en|ˈ|æ|l|t|s|h|aɪ|m|ər|z}}, {{IPAc-en|usalso|ˈ|ɑː|l|t|s|-}} | |||
| | eMedicineTopic = 13 | |||
| | field = ] | |||
| | MeshID = | |||
| | synonyms = Alzheimer's dementia | |||
| |}} | |||
| | symptoms = ], ], ], ]s<ref name=Knopman2021 /><ref name=WHO2023/> | |||
| | complications = ]s, ] and ] in the terminal stage<ref name=":0">{{Cite web |title=Ask the Doctors - What is the cause of death in Alzheimer's disease? |url=https://www.uclahealth.org/news/ask-the-doctors-what-is-the-cause-of-death-in-alzheimers-disease |access-date=2024-03-18 |website=www.uclahealth.org |language=en}}</ref> | |||
| | onset = Over 65 years old<ref name=Mend2012 /> | |||
| | duration = Long term<ref name=WHO2023/> | |||
| | causes = Poorly understood<ref name=Knopman2021 /> | |||
| | risks = ], ], ], ],<ref name=Knopman2021 /> ],<ref name="Yu 1201–1209"/> lack of physical<ref name=Cheng2016/> and mental<ref name="Yu 1201–1209"/><ref name=Vina2018/> exercise | |||
| | diagnosis = Based on symptoms and ]ing after ruling out other possible causes<ref name=NICE2014Diag /> | |||
| | differential = ],<ref name=Knopman2021 /> ],<ref name=Gomperts2016>{{cite journal | vauthors = Gomperts SN | title = Lewy Body Dementias: Dementia With Lewy Bodies and Parkinson Disease Dementia | journal = Continuum | volume = 22 | issue = 2 Dementia | pages = 435–463 | date = April 2016 | pmid = 27042903 | pmc = 5390937 | doi = 10.1212/CON.0000000000000309 | type = Review |issn = 1080-2371}}</ref> ]<ref name=Lott2019>{{cite journal |vauthors=Lott IT, Head E |title=Dementia in Down syndrome: unique insights for Alzheimer disease research |journal=Nat Rev Neurol |volume=15 |issue=3 |pages=135–147 |date=March 2019 |pmid=30733618 |pmc=8061428 |doi=10.1038/s41582-018-0132-6 }}</ref> | |||
| | prevention = | |||
| | treatment = | |||
| | medication = ]s, ]s<ref name="mayo">{{Cite web |date=2023-08-30 |title=How Alzheimer's drugs help manage symptoms |url=https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers/art-20048103 |access-date=2024-03-19 |website=Mayo Clinic |language=en}}</ref> | |||
| | prognosis = Life expectancy 3–12 years<ref name="mayo" /><ref name="schaffert">{{cite journal | vauthors = Schaffert J, LoBue C, Hynan LS, Hart J, Rossetti H, Carlew AR, Lacritz L, White CL, Cullum CM | title = Predictors of Life Expectancy in Autopsy-Confirmed Alzheimer's Disease | journal = Journal of Alzheimer's Disease | volume = 86 | issue = 1 | pages = 271–281 | date = 2022 | pmid = 35034898 | pmc = 8966055 | doi = 10.3233/JAD-215200 }}</ref><ref name="todd">{{cite journal | vauthors = Todd S, Barr S, Roberts M, Passmore AP | title = Survival in dementia and predictors of mortality: a review | journal = International Journal of Geriatric Psychiatry | volume = 28 | issue = 11 | pages = 1109–1124 | date = November 2013 | pmid = 23526458 | doi = 10.1002/gps.3946 }}</ref> | |||
| | frequency = 50 million (2020)<ref name=Breijyeh2020 /> | |||
| | deaths = | |||
| | named after = ] | |||
| }} | |||
| <!-- Definition and symptoms --> | |||
| '''Alzheimer's disease''' ('''AD'''), also known simply as '''Alzheimer's''', is a ] that, in its most common form, is found in people over age 65. Approximately 24 million people worldwide have dementia of which the majority (~60%) is due to Alzheimer's.<ref> {{cite journal |author=Ferri CP, Prince M, Brayne C, ''et al'' |title=Global prevalence of dementia: a Delphi consensus study |journal=Lancet |volume=366 |issue=9503 |pages=2112-7 |year=2005 |pmid=16360788 |doi=10.1016/S0140-6736(05)67889-0}} </ref> | |||
| '''Alzheimer's disease''' ('''AD''') is a ] that usually starts slowly and progressively worsens.<ref name=WHO2023>{{cite web|date=15 March 2023|title=Dementia Fact sheet|url=https://www.who.int/en/news-room/fact-sheets/detail/dementia|publisher=World Health Organization|access-date=10 July 2023 }}</ref> It is the cause of 60–70% of cases of ].<ref name=WHO2023/><ref name=Simon2018p111 /> The most common early symptom is difficulty in ].<ref name=Knopman2021 /> As the disease advances, symptoms can include ], ] (including easily getting lost), ]s, loss of ], ], and ].<ref name=WHO2023/> As a person's condition declines, they often ].<ref name=BMJ2009>{{cite journal | vauthors = Burns A, Iliffe S | title = Alzheimer's disease | journal = BMJ | volume = 338 | pages = b158 | date = February 2009 | pmid = 19196745 | doi = 10.1136/bmj.b158 | s2cid = 8570146 }}</ref> Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to twelve years.<ref name="mayo" /><ref name="schaffert" /><ref name="todd" /> | |||
| <!-- Cause, diagnosis and prevention --> | |||
| Clinical signs of Alzheimer's disease are characterized by progressive cognitive deterioration, together with declining activities of daily living and by ] symptoms or behavioral changes. It is the most common type of ]. Plaques which contain misfolded peptides called amyloid beta (Aβ) are formed in the brain many years before the clinical signs of Alzheimer's are observed. Together, these plaques and ] form the pathological hallmarks of the disease. These features can only be discovered at autopsy and help to confirm the clinical diagnosis. Medications can help reduce the symptoms of the disease, but they cannot change the course of the underlying pathology. | |||
| The causes of Alzheimer's disease remain poorly understood.<ref name=BMJ2009 /> There are many environmental and genetic ]s associated with its development. The strongest genetic risk factor is from an ] of ].<ref name=Long /><ref name=NIA2021>{{cite web |title=Study reveals how APOE4 gene may increase risk for dementia |url=https://www.nia.nih.gov/news/study-reveals-how-apoe4-gene-may-increase-risk-dementia |publisher=National Institute on Aging |date=16 March 2021 |access-date=17 March 2021 |archive-date=17 March 2021 |archive-url=https://web.archive.org/web/20210317180050/https://www.nia.nih.gov/news/study-reveals-how-apoe4-gene-may-increase-risk-dementia |url-status=live }}</ref> Other risk factors include a history of ], ], and ].<ref name=Knopman2021 /> The progression of the disease is largely characterized by the accumulation of ] in the ], called ] and ]. These misfolded ] interfere with normal cell function, and over time lead to irreversible ] and loss of ] in the ].<ref name="NIA2023">{{cite web |title=Alzheimer's Disease Fact Sheet |url=https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet |url-status=dead |archive-url=https://web.archive.org/web/20220323200727/https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet |archive-date=23 March 2022 |access-date=23 March 2022 |publisher=National Institute on Aging}}</ref> A probable diagnosis is based on the history of the illness and ]ing, with ] and ]s to rule out other possible causes.<ref name=NICE2014Diag>{{cite web |title=Dementia diagnosis and assessment |publisher=National Institute for Health and Care Excellence (NICE) |url=http://pathways.nice.org.uk/pathways/dementia/dementia-diagnosis-and-assessment.pdf|access-date=30 November 2014|url-status=dead |archive-url=https://web.archive.org/web/20141205184403/http://pathways.nice.org.uk/pathways/dementia/dementia-diagnosis-and-assessment.pdf|archive-date=5 December 2014}}</ref><ref>{{cite report | title=Dementia: assessment, management and support for people living with dementia and their carers | publisher=] (NICE) | date=20 June 2018 | url=https://www.nice.org.uk/guidance/ng97 | access-date=8 July 2023 | id=NG97 }}</ref> Initial symptoms are often mistaken for ].<ref name=BMJ2009 /> ] is needed for a definite diagnosis, but this can only take place ].<ref name=Khan2020 /><ref name=Gauthreaux2020 /> | |||
| <!-- Management --> | |||
| The ultimate cause of Alzheimer's is unknown. Genetic factors are clearly indicated as evidenced by dominant ] in three different genes have been identified that account for the small number of cases of ]. For the more common form of late onset AD (LOAD), ] is the only clearly established susceptibility gene. All four genes can contain mutations or variants that confer increased risk for AD, but account for only 30% of the genetic picture of AD. These four genes have in common the fact that mutations in each lead to the excessive accumulation in the brain of Aβ, the main component of the senile plaques that litter the brains of AD patients.<ref name="decoding darkness"> "Decoding Darkness: The Search for the Genetics Causes of Alzheimer's Disease", Rudolph Tanzi and Ann Parson, Perseus Press, 2000</ref>. | |||
| No treatments can stop or reverse its progression, though some may temporarily improve symptoms.<ref name=WHO2023/> A healthy diet, physical activity, and ] are generally beneficial in aging, and may help in reducing the risk of cognitive decline and Alzheimer's.<ref name="NIA2023" /> Affected people become increasingly reliant on others for assistance, often placing a burden on ].<ref name=Thom2007 /> The pressures can include social, psychological, physical, and economic elements.<ref name=Thom2007>{{cite journal | vauthors = Thompson CA, Spilsbury K, Hall J, Birks Y, Barnes C, Adamson J | title = Systematic review of information and support interventions for caregivers of people with dementia | journal = BMC Geriatrics | volume = 7 | pages = 18 | date = July 2007 | pmid = 17662119 | pmc = 1951962 | doi = 10.1186/1471-2318-7-18 | doi-access = free }}</ref> Exercise programs may be beneficial with respect to ] and can potentially improve outcomes.<ref name=Forb2015>{{cite journal | vauthors = Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S | title = Exercise programs for people with dementia | journal = The Cochrane Database of Systematic Reviews | volume = 132 | issue = 4 | pages = CD006489 | date = April 2015 | pmid = 25874613 | doi = 10.1002/14651858.CD006489.pub4 | pmc = 9426996 | type = Submitted manuscript }}</ref> Behavioral problems or ] due to dementia are sometimes treated with ]s, but this has an increased risk of early death.<ref>{{cite web |title=Low-dose antipsychotics in people with dementia |publisher=National Institute for Health and Care Excellence (NICE) |url=https://www.nice.org.uk/advice/ktt7/resources/non-guidance-lowdose-antipsychotics-in-people-with-dementia-pdf|access-date=29 November 2014|url-status=dead |archive-url=https://web.archive.org/web/20141205183329/https://www.nice.org.uk/advice/ktt7/resources/non-guidance-lowdose-antipsychotics-in-people-with-dementia-pdf|archive-date=5 December 2014}}</ref><ref>{{cite web |date=16 June 2008 |title=Information for Healthcare Professionals: Conventional Antipsychotics |publisher=US Food and Drug Administration |url=https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124830.htm|access-date=29 November 2014 |archive-url=https://web.archive.org/web/20141129015823/https://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm124830.htm|archive-date=29 November 2014 | url-status=dead }}</ref> | |||
| <!-- Epidemiology, history, society, and research--> | |||
| ==History== | |||
| As of 2020, there were approximately 50 million people worldwide with Alzheimer's disease.<ref name=Breijyeh2020 /> It most often begins in people over 65 years of age, although up to 10% of cases are ] impacting those in their 30s to mid-60s.<ref name=NIA2019>{{cite web |title=Alzheimer's Disease Fact Sheet |url=https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet |publisher=National Institute on Aging |access-date=25 January 2021 |archive-date=24 January 2021 |archive-url=https://web.archive.org/web/20210124194838/https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet |url-status=live }}</ref><ref name=Mend2012>{{cite journal | vauthors = Mendez MF | title = Early-onset Alzheimer's disease: nonamnestic subtypes and type 2 AD | journal = Archives of Medical Research | volume = 43 | issue = 8 | pages = 677–685 | date = November 2012 | pmid = 23178565 | pmc = 3532551 | doi = 10.1016/j.arcmed.2012.11.009 }}</ref> It affects about 6% of people 65 years and older,<ref name=BMJ2009 /> and women more often than men.<ref>{{cite journal |vauthors=Zhu D, Montagne A, Zhao Z |title=Alzheimer's pathogenic mechanisms and underlying sex difference |journal=Cell Mol Life Sci |volume=78 |issue=11 |pages=4907–4920 |date=June 2021 |pmid=33844047 |pmc=8720296 |doi=10.1007/s00018-021-03830-w }}</ref> The disease is named after German psychiatrist and pathologist ], who first described it in 1906.<ref name=pmid9661992 /> Alzheimer's financial burden on society is large, with an estimated global annual cost of {{US$|1}}{{nbsp}}trillion.<ref name=Breijyeh2020 /> It is ranked as the ] worldwide.<ref>{{Cite web |title=The top 10 causes of death |url=https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death |access-date=2024-03-19 |website=www.who.int |language=en}}</ref> | |||
| ].]] | |||
| <!-- Public and private funding of Alzheimer's research --> | |||
| In 1901, ], a German psychiatrist, identified the first case of what became known as Alzheimer's disease, in a 50 year-old patient ] and followed her to her death in 1906, when he first reported the case publicly.<ref> {{cite book | last =Maurer | first =Konrad | coauthors =Maurer, Ulrike | title = Alzheimer: the life of a physician and the career of a disease | publisher = Columbia University Press | date =2003 | location =New York | id= ISBN 0-231-11896-1}}</ref> | |||
| Given the widespread impacts of Alzheimer's disease, both basic-science and health funders in many countries support Alzheimer's research at large scales. For example, the US ] program for Alzheimer's research, the National Plan to Address Alzheimer’s Disease, has a budget of US$3.98 billion for fiscal year 2026.<ref>{{Cite web|vauthors=Bertagnolli MM|title=Fiscal Year 2026 NIH Professional Judgment Budget for Alzheimer's Disease and Related Dementias Research: Advancing Progress in Dementia Research |url=https://www.nia.nih.gov/about/budget/fy26-professional-judgment-budget-proposal|date=5 August 2024|access-date=23 September 2024 |publisher=US National Institutes of Health}}</ref> In the ], the 2020 ] research programme awarded over €570 million for dementia-related projects.<ref>{{Cite journal|url=https://www.alzheimer-europe.org/policy/eu-action/horizon-europe-research-programme-0?language_content_entity=en|title=Horizon Europe research programme|via=www.alzheimer-europe.org}}</ref> | |||
| For most of the twentieth century, the diagnosis of Alzheimer's disease was reserved for individuals between the ages of 45 and 65 who developed symptoms of ''presenile'' ]. ''Senile'' dementia, as a set of symptoms, was considered to be a relatively normal outcome of the aging process, and thought to be due to age-related brain arterial "hardening." In the ] and early-], because the symptoms and brain pathology were identical for any age, the name "Alzheimer's disease" became used equally for afflicted individuals of all ages; however, the term ''senile dementia of the Alzheimer type'' (SDAT) was often used to describe the condition in those over 65. Eventually, the term Alzheimer's disease was formally adopted in medical nomenclature to describe individuals of all ages with the characteristic common symptom pattern, disease course, and neuropathology. The term ''Alzheimer disease'' (without the apostrophe and s) is also sometimes used in literature for learning. | |||
| {{TOC limit|3}} | |||
| ==Signs and symptoms== | |||
| ==Etiology== | |||
| The course of Alzheimer's is generally described in three stages, with a progressive pattern of ] and ] ].<ref name=NHS2018>{{cite web|title=Alzheimer's disease – Symptoms|url=https://www.nhs.uk/conditions/alzheimers-disease/symptoms/|website=] (NHS)|date=10 May 2018|access-date=25 January 2021|archive-date=30 January 2021|archive-url=https://web.archive.org/web/20210130034141/https://www.nhs.uk/conditions/alzheimers-disease/symptoms/|url-status=live}}</ref><ref name=NIA2019 /> The three stages are described as early or mild, middle or moderate, and late or severe.<ref name=NHS2018 /> The disease is known to target the ] which is associated with ], and this is responsible for the first symptoms of memory impairment. As the disease progresses so does the degree of memory impairment.<ref name=NIA2023/> | |||
| Most cases of Alzheimer's disease are sporadic, i.e., do not exhibit familial inheritance requiring the patient to have two or more first-degree relatives with the disease. Nonetheless, at least 80% of sporadic AD cases most likely involve genetic risk factors based on twin studies. 5-10% of AD cases involve a clear familial pattern of inheritance in which the patient has at least two first-degree relatives with a history of AD <ref> From the ]</ref> The relative contribution of genetics and environment to the sporadic cases is unclear, but are accepted to be of multifactorial origin. In early-onset (<60 years) familial AD, genetic defects identified include mutations in the presenlin 1 gene on chromosome 14, the presenilin 2 gene on chromosome 1, and the amyloid precursor protein (APP) gene on chromosome 21. ApoE is contributes to risk in roughly half of all late-onset sporadic AD cases which comprise 90-95% of total AD. <ref name="decoding darkness">. | |||
| == |
===First symptoms=== | ||
| ] in Alzheimer's]] | |||
| The first readily identified symptoms of Alzheimer's disease are usually short-term memory loss and visual-spatial confusion. These initial symptoms progress from seemingly simple and often fluctuating ] and difficulty orienting oneself in space such as in a traffic lane while driving, to a more pervasive loss of ] and difficulty navigating through familiar areas such as one's neighborhood, then to loss of other familiar and well-known skills as well as recognition of objects and persons.<ref>Kumru, Liz. UNMC. Accessed 22 July 2007.</ref><ref>Rickey, Tom. (31 January 2002) Accessed 21 July 2007.</ref> | |||
| The first symptoms are often mistakenly attributed to ] or ].<ref name=Waldemar2007>{{cite journal | vauthors = Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rossor M, Scheltens P, Tariska P, Winblad B |title = Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline | journal = European Journal of Neurology | volume = 14 | issue = 1 | pages = e1-26 | date = January 2007 | pmid = 17222085 | doi = 10.1111/j.1468-1331.2006.01605.x | s2cid = 2725064 | doi-access = free | title-link = doi | author6-link = Martin Rossor }}</ref> Detailed ]ing can reveal mild cognitive difficulties up to eight years before a person fulfills the clinical criteria for ] of Alzheimer's disease.<ref name=pmid15324363>{{cite journal | vauthors = Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ | title = Multiple cognitive deficits during the transition to Alzheimer's disease | journal = Journal of Internal Medicine | volume = 256 | issue = 3 | pages = 195–204 | date = September 2004 | pmid = 15324363 | doi = 10.1111/j.1365-2796.2004.01386.x | s2cid = 37005854 | doi-access = free | title-link = doi }}</ref> These early symptoms can affect the most complex ].<ref>{{cite journal | vauthors = Nygård L | title = Instrumental activities of daily living: a stepping-stone towards Alzheimer's disease diagnosis in subjects with mild cognitive impairment? | journal = Acta Neurologica Scandinavica. Supplementum | volume = 179 | issue = s179 | pages = 42–46 | year = 2003 | pmid = 12603250 | doi = 10.1034/j.1600-0404.107.s179.8.x | s2cid = 25313065 }}</ref> The most noticeable deficit is ] loss, which shows up as difficulty in remembering recently learned facts and inability to acquire new information.<ref name=pmid15324363 /> | |||
| Subtle problems with the ] of ], ], flexibility, and ], or impairments in ] (memory of meanings, and concept relationships) can also be symptomatic of the early stages of Alzheimer's disease.<ref name=pmid15324363 /> ] and depression can be seen at this stage, with apathy remaining as the most persistent symptom throughout the course of the disease.<ref name=Deardorff>{{cite book | vauthors = Deardorff WJ, Grossberg GT | title = Psychopharmacology of Neurologic Disease | chapter = Behavioral and psychological symptoms in Alzheimer's dementia and vascular dementia | series = Handbook of Clinical Neurology | volume = 165 | pages = 5–32 | date = 2019 | publisher = Elsevier | pmid = 31727229 | doi = 10.1016/B978-0-444-64012-3.00002-2 | isbn = 978-0-444-64012-3 | s2cid = 208037448 }}</ref><ref>{{cite book |title=Bradley's neurology in clinical practice|year=2012 |publisher=Elsevier/Saunders|location=Philadelphia, PA|isbn=978-1-4377-0434-1 |vauthors=Murray ED, Buttner N, Price BH|edition=6th|veditors=Bradley WG, Daroff RB, Fenichel GM, Jankovic J |chapter=Depression and Psychosis in Neurological Practice}}</ref> People with objective signs of cognitive impairment, but not more severe symptoms, may be diagnosed with ] (MCI). If memory loss is the predominant symptom of MCI, it is termed ] and is frequently seen as a ] or early stage of Alzheimer's disease.<ref name=Petersen>{{cite journal | vauthors = Petersen RC, Lopez O, Armstrong MJ, Getchius TS, Ganguli M, Gloss D, Gronseth GS, Marson D, Pringsheim T, Day GS, Sager M, Stevens J, Rae-Grant A | title = Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology | journal = Neurology | volume = 90 | issue = 3 | pages = 126–135 | date = January 2018 | pmid = 29282327 | pmc = 5772157 | doi = 10.1212/WNL.0000000000004826 }}</ref> Amnestic MCI has a greater than 90% likelihood of being associated with Alzheimer's.<ref name=Atri2019 /> | |||
| Since family members are often the first to notice changes that might indicate the onset of Alzheimer's they should learn the early warning signs and serve as informants during initial evaluation of patients clinically.<ref></ref> ], ] and ] often accompany the loss of memory. Alzheimer's disease (AD) may also include behavioral changes, such as outbursts of ] or excessive passivity in people who have no previous history of such behavior. | |||
| ===Early stage=== | |||
| In the later stages of the disease, deterioration of musculature and mobility, leading to bedfastness, inability to feed oneself, and ], will be seen if death from some external cause (e.g. ] or ]) does not intervene. Once identified, the average lifespan of patients living with Alzheimer's disease is approximately 7-10 years, although cases are known where reaching the final stage occurs within 4-5 years or at the other extreme they may survive up to 21 years. | |||
| In people with Alzheimer's disease, the increasing impairment of learning and memory eventually leads to a definitive diagnosis. In a small percentage, difficulties with language, executive functions, ] (]), or execution of movements (]) are more prominent than memory problems.<ref name=pmid10653284>{{cite journal | vauthors = Förstl H, Kurz A | title = Clinical features of Alzheimer's disease | journal = European Archives of Psychiatry and Clinical Neuroscience | volume = 249 | issue = 6 | pages = 288–290 | year = 1999 | pmid = 10653284 | doi = 10.1007/s004060050101 | s2cid = 26142779 }}</ref> Alzheimer's disease does not affect all memory capacities equally. ] of the person's life (]), facts learned (]), and ] (the memory of the body on how to do things, such as using a fork to eat or how to drink from a glass) are affected to a lesser degree than new facts or memories.<ref name=pmid1300219>{{cite journal | vauthors = Carlesimo GA, Oscar-Berman M | title = Memory deficits in Alzheimer's patients: a comprehensive review | journal = Neuropsychology Review | volume = 3 | issue = 2 | pages = 119–169 | date = June 1992 | pmid = 1300219 | doi = 10.1007/BF01108841 | s2cid = 19548915 }}</ref><ref name=pmid8821346>{{cite journal | vauthors = Jelicic M, Bonebakker AE, Bonke B | title = Implicit memory performance of patients with Alzheimer's disease: a brief review | journal = International Psychogeriatrics | volume = 7 | issue = 3 | pages = 385–392 | year = 1995 | pmid = 8821346 | doi = 10.1017/S1041610295002134 | s2cid = 9419442 }}</ref> | |||
| ] are mainly characterised by a shrinking ] and decreased word ], leading to a general impoverishment of oral and ].<ref name=pmid10653284 /><ref name=pmid1856925>{{cite journal | vauthors = Taler V, Phillips NA | title = Language performance in Alzheimer's disease and mild cognitive impairment: a comparative review | journal = Journal of Clinical and Experimental Neuropsychology | volume = 30 | issue = 5 | pages = 501–556 | date = July 2008 | pmid = 18569251 | doi = 10.1080/13803390701550128 | s2cid = 37153159 }}</ref> In this stage, the person with Alzheimer's is usually capable of communicating basic ideas adequately.<ref name=pmid10653284 /><ref name=pmid1856925 /><ref name=pmid7967534>{{cite journal | vauthors = Frank EM | title = Effect of Alzheimer's disease on communication function | journal = Journal of the South Carolina Medical Association | volume = 90 | issue = 9 | pages = 417–423 | date = September 1994 | pmid = 7967534 }}</ref> While performing ] such as writing, drawing, or dressing, certain movement coordination and planning difficulties (]) may be present; however, they are commonly unnoticed.<ref name=pmid10653284 /> As the disease progresses, people with Alzheimer's disease can often continue to perform many tasks independently; however, they may need assistance or supervision with the most cognitively demanding activities.<ref name=pmid10653284 /> | |||
| === Stages and symptoms === | |||
| *'''Mild''' — In the '''early stage''' of the disease, patients have a tendency to become less energetic or spontaneous, though changes in their behavior often go unnoticed even by the patients' immediate family. This stage of the disease has also been termed ] (MCI), when the patient does not meet the criteria for a diagnosis of dementia.<ref>. Ronald C Petersen, Nature Clinical Practice Neurology (2007) 3, 60-61.</ref> | |||
| *'''Moderate''' — As the disease progresses to the '''middle stage''', patients might still be able to perform tasks independently (such as using the bathroom), but may need assistance with more complicated activities (such as paying bills). | |||
| *'''Severe''' — As the disease progresses from the middle to the '''late stage''', patients will not be able to perform even simple tasks independently and will require constant supervision. They become incontinent of bladder and then incontinent of bowel. They will eventually lose the ability to walk and eat without assistance. Language becomes severely disorganized, and then is lost altogether. They may eventually lose the ability to swallow food and fluid, and this can ultimately lead to death. | |||
| == |
===Middle stage=== | ||
| Progressive deterioration eventually hinders independence, with subjects being unable to perform most common activities of daily living.<ref name=pmid10653284 /> Speech difficulties become evident due to an inability to ], which leads to frequent incorrect word substitutions (]s). Reading and writing skills are also progressively lost.<ref name=pmid10653284 /><ref name=pmid7967534 /> Complex motor sequences become less coordinated as time passes and Alzheimer's disease progresses, so the risk of falling increases.<ref name=pmid10653284 /> During this phase, memory problems worsen, and the person may fail to recognise close relatives.<ref name=pmid10653284 /> ], which was previously intact, becomes impaired.<ref name=pmid10653284 /> | |||
| Behavioral and ] changes become more prevalent. Common manifestations are ], ] and ], leading to crying, outbursts of unpremeditated ], or resistance to caregiving.<ref name=pmid10653284 /> ] can also appear.<ref>{{cite journal | vauthors = Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A | title = Sundowning and circadian rhythms in Alzheimer's disease | journal = The American Journal of Psychiatry | volume = 158 | issue = 5 | pages = 704–711 | date = May 2001 | pmid = 11329390 | doi = 10.1176/appi.ajp.158.5.704 | s2cid = 10492607 }}</ref> Approximately 30% of people with Alzheimer's disease develop ] and other ]al symptoms.<ref name=pmid10653284 /> Subjects also lose insight of their disease process and limitations (]).<ref name=pmid10653284 /> ] can develop.<ref name=pmid10653284 /> These symptoms create ] for relatives and caregivers, which can be reduced by moving the person from ] to other ].<ref name=pmid10653284 /><ref name=pmid7806732>{{cite journal | vauthors = Gold DP, Reis MF, Markiewicz D, Andres D | title = When home caregiving ends: a longitudinal study of outcomes for caregivers of relatives with dementia | journal = Journal of the American Geriatrics Society | volume = 43 | issue = 1 | pages = 10–16 | date = January 1995 | pmid = 7806732 | doi = 10.1111/j.1532-5415.1995.tb06235.x | s2cid = 29847950 }}</ref> | |||
| Alzheimer's disease (AD) is primarily a clinically ] condition based on the presence of characteristic ] and neuropsychological features and the ]. Determination of neurological characteristics is made utilizing patient history and clinical observation, while neuropsychological evaluation includes memory testing and assessment of intellectual functioning over a series of weeks or months. Supplemental physical testing, including ]s and ], is utilized to rule out other diagnoses. ], to include screening for ] and a ], can be helpful in establishing the presence and severity of ]. Although certain clues from history may suggest a diagnosis of vascular dementias instead of, or in addition to, AD (for example, see the Hachinski scale ), the ability of certain neuroimaging modalities such as ] to differentiate vascular type from Alzheimer disease types of dementias, appears to be superior to clinical exam (PMID 15545324). | |||
| ===Late stage=== | |||
| Interviews with family members and/or caregivers are also utilized in the initial assessment of the disease, as a patient with Alzheimer's may tend to minimize his or her symptoms, or may undergo evaluation at a time when his or her symptoms are less apparent, as ] fluctuations ("good days and bad days") are a common feature of the disease. Observations noting that a patient's good memory function decreases over time plays a critical role in the diagnosis of Alzheimer's. | |||
| ] | |||
| During the final stage, known as the late-stage or severe stage, there is complete dependence on caregivers.<ref name=NIA2023/><ref name=NHS2018 /><ref name=pmid10653284 /> Language is reduced to simple phrases or even single words, eventually leading to complete loss of speech.<ref name=pmid10653284 /><ref name=pmid7967534 /> Despite the loss of verbal language abilities, people can often understand and return emotional signals. Although aggressiveness can still be present, extreme ] and ] are much more common symptoms. People with Alzheimer's disease will ultimately not be able to perform even the simplest tasks independently; ] and mobility deteriorates to the point where they are bedridden and unable to feed themselves. The cause of death is usually an external factor, such as infection of ]s or ], not the disease itself.<ref name=pmid10653284 /><!-- cites previous 4 sentences --> In some cases, there is a ] immediately before death, where there is an unexpected recovery of mental clarity.<ref>{{cite journal |vauthors = Mashour GA, Frank L, Batthyany A, Kolanowski AM, Nahm M, Schulman-Green D, Greyson B, Pakhomov S, Karlawish J, Shah RC |title=Paradoxical lucidity: A potential paradigm shift for the neurobiology and treatment of severe dementias |journal=Alzheimer's & Dementia |volume=15 |issue=8 |pages=1107–1114 |date=August 2019 |pmid=31229433 |doi=10.1016/j.jalz.2019.04.002 |s2cid=195063786 |hdl=2027.42/153062 |hdl-access=free }}</ref> | |||
| ==Causes== | |||
| ''']''' | |||
| Alzheimer's disease is believed to occur when abnormal amounts of ] (Aβ), accumulating extracellularly as ] and ]s, or intracellularly as ]s, form in the brain, affecting neuronal functioning and connectivity, resulting in a progressive loss of brain function.<ref>{{cite web | title=Alzheimer's disease – Causes | website=] (NHS) | date=24 April 2023 | url=https://www.nhs.uk/conditions/alzheimers-disease/causes/ | access-date=10 July 2023 | archive-url=https://web.archive.org/web/20200929103158/https://www.nhs.uk/conditions/alzheimers-disease/causes/ |archive-date=29 September 2020 | url-status = live }}</ref><ref name=Tackenberg>{{cite journal | vauthors = Tackenberg C, Kulic L, Nitsch RM | title = Familial Alzheimer's disease mutations at position 22 of the amyloid β-peptide sequence differentially affect synaptic loss, tau phosphorylation and neuronal cell death in an ex vivo system | journal = PLOS ONE | volume = 15 | issue = 9 | pages = e0239584 | date = 2020 | pmid = 32966331 | pmc = 7510992 | doi = 10.1371/journal.pone.0239584 | bibcode = 2020PLoSO..1539584T | doi-access = free | title-link = doi }}</ref> This altered ] is age-related, regulated by brain cholesterol,<ref name=WangHao>{{cite journal | vauthors = Wang H, Kulas JA, Wang C, Holtzman DM, Ferris HA, Hansen SB | title = Regulation of beta-amyloid production in neurons by astrocyte-derived cholesterol | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 118 | issue = 33 | pages = e2102191118 | date = August 2021 | pmid = 34385305 | pmc = 8379952 | doi = 10.1073/pnas.2102191118|issn=0027-8424 | s2cid = 236998499 | doi-access = free | title-link = doi | bibcode = 2021PNAS..11802191W }}</ref> and associated with other neurodegenerative diseases.<ref name=Vilchez>{{cite journal | vauthors = Vilchez D, Saez I, Dillin A | title = The role of protein clearance mechanisms in organismal ageing and age-related diseases | journal = Nature Communications | volume = 5 | issue = | pages = 5659 | date = December 2014 | pmid = 25482515 | doi = 10.1038/ncomms6659 | bibcode = 2014NatCo...5.5659V | doi-access = free | title-link = doi }}</ref><ref name=OUP>{{cite book| vauthors = Jacobson M, McCarthy N |title=Apoptosis |date=2002|publisher=Oxford University Press|location=Oxford, OX|isbn=0-19-963849-7|page=290}}</ref> | |||
| New imaging technologies have revolutionized our understanding of the structure and function of the living brain. Structural imaging provides information about the shape, position or volume of brain tissue. Structural techniques include magnetic resonance imaging (]) and computed tomography (]). Functional imaging reveals how well cells in various brain regions are working by showing how actively the cells use sugar or oxygen. Functional techniques include positron emission tomography (]) and ] (fMRI). | |||
| The cause for most Alzheimer's cases is still mostly unknown,<ref name=Breijyeh2020>{{cite journal | vauthors = Breijyeh Z, Karaman R | title = Comprehensive Review on Alzheimer's Disease: Causes and Treatment | journal = Molecules | volume = 25 | issue = 24 | date = December 2020 | page = 5789 | pmid = 33302541 | pmc = 7764106 | doi = 10.3390/molecules25245789 | type = Review | doi-access = free | title-link = doi }}</ref> except for 1–2% of cases where deterministic genetic differences have been identified.<ref name=Long /> Several competing ] attempt to explain the underlying cause; the most predominant hypothesis is the amyloid beta (Aβ) hypothesis.<ref name=Breijyeh2020 /> | |||
| No medical tests are available to diagnose Alzheimer's disease conclusively pre-]. Expert clinicians who specialize in memory disorders can now diagnose AD with an accuracy of 85 - 90%. However, a definitive diagnosis of Alzheimer's disease must await microscopic examination of brain tissue which generally occurs at ]. | |||
| The oldest hypothesis, on which most drug therapies are based, is the ], which proposes that Alzheimer's disease is caused by reduced synthesis of the neurotransmitter ].<ref name=Breijyeh2020 /> The loss of ]s noted in the ] and cerebral cortex, is a key feature in the progression of Alzheimer's.<ref name=Petersen /> The 1991 ] postulated that extracellular amyloid beta (Aβ) deposits are the fundamental cause of the disease.<ref name=pmid1763432>{{cite journal | vauthors = Hardy J, Allsop D | title = Amyloid deposition as the central event in the aetiology of Alzheimer's disease | journal = Trends in Pharmacological Sciences | volume = 12 | issue = 10 | pages = 383–388 | date = October 1991 | pmid = 1763432 | doi = 10.1016/0165-6147(91)90609-V }}</ref><ref name=pmid11801334>{{cite journal | vauthors = Mudher A, Lovestone S | title = Alzheimer's disease-do tauists and baptists finally shake hands? | journal = Trends in Neurosciences | volume = 25 | issue = 1 | pages = 22–26 | date = January 2002 | pmid = 11801334 | doi = 10.1016/S0166-2236(00)02031-2 | s2cid = 37380445 }}</ref> Support for this postulate comes from the location of the gene for the ] (APP) on ], together with the fact that people with ] (Down syndrome) who have an extra ] almost universally exhibit at least the earliest symptoms of Alzheimer's disease by 40 years of age.<ref name=Lott2019 /> A specific ] of apolipoprotein, ], is a major genetic risk factor for Alzheimer's disease.<ref name=Simon2018p111 /> While apolipoproteins enhance the breakdown of beta amyloid, some isoforms are not very effective at this task (such as APOE4), leading to excess amyloid buildup in the brain.<ref name=pmid7566000>{{cite journal | vauthors = Polvikoski T, Sulkava R, Haltia M, Kainulainen K, Vuorio A, Verkkoniemi A, Niinistö L, Halonen P, Kontula K | title = Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein | journal = The New England Journal of Medicine | volume = 333 | issue = 19 | pages = 1242–1247 | date = November 1995 | pmid = 7566000 | doi = 10.1056/NEJM199511093331902 | doi-access = free }}</ref> | |||
| ==Pathology== | |||
| {{main|Biochemistry of Alzheimer's disease}} | |||
| ===Biochemical characteristics=== | |||
| Alzheimer's disease has been identified as a ] disease, or ], due to the accumulation of abnormally folded A-beta and tau proteins in the brains of AD patients.<ref name="Hashimoto"> {{cite journal | author = Hashimoto M, Rockenstein E, Crews L, Masliah E | title = Role of protein aggregation in mitochondrial dysfunction and neurodegeneration in Alzheimer's and Parkinson's diseases. | journal = Neuromolecular Med | volume = 4 | issue = 1-2 | pages = 21-36 | year = 2003 | id = PMID 14528050}}</ref> A-beta, also written Aβ, is a short ] that is a ] byproduct of the ] ] (APP), whose function is unclear but thought to be involved in neuronal development.<ref name="decoding darkness"> | |||
| The ]s are components of a proteolytic complex involved in APP processing and degradation.<ref name="Cai"> {{cite journal | author = Cai D, Netzer W, Zhong M, Lin Y, Du G, Frohman M, Foster D, Sisodia S, Xu H, Gorelick F, Greengard P | title = Presenilin-1 uses phospholipase D1 as a negative regulator of beta-amyloid formation. | journal = Proc Natl Acad Sci U S A | volume = 103 | issue = 6 | pages = 1941-6 | year = 2006 | id = PMID 16449386}}</ref> Although amyloid beta ]s are soluble and harmless, they undergo a dramatic ] at sufficiently high concentration to form a ]-rich ] that aggregates to form ]<ref name="Ohnishi">{{cite journal | author = Ohnishi S, Takano K | title = Amyloid fibrils from the viewpoint of protein folding. | journal = Cell Mol Life Sci | volume = 61 | issue = 5 | pages = 511-24 | year = 2004 | id = PMID 15004691}}</ref> that deposit outside neurons in dense formations known as ''senile plaques'' or ''neuritic plaques'', in less dense aggregates as ''diffuse plaques'', and sometimes in the walls of small blood vessels in the brain in a process called amyloid angiopathy or ]. | |||
| ===Genetic=== | |||
| AD is also considered a ] due to abnormal aggregation of the ], a ] expressed in neurons that normally acts to stabilize ] in the cell ]. Like most microtubule-associated proteins, tau is normally regulated by ]; however, in AD patients, hyperphosphorylated tau accumulates as paired helical filaments<ref name="Goedert">{{cite journal | author = Goedert M, Klug A, Crowther R | title = Tau protein, the paired helical filament and Alzheimer's disease. | journal = J Alzheimers Dis | volume = 9 | issue = 3 Suppl | pages = 195-207 | year = 2006 | id = PMID 16914859}}</ref> that in turn aggregate into masses inside nerve cell bodies known as ''neurofibrillary tangles'' and as dystrophic ]s associated with amyloid plaques. | |||
| ==== Late onset ==== | |||
| Late-onset Alzheimer's is about 70% ].<ref name=Andrews2023>{{cite journal |vauthors=Andrews SJ, Renton AE, Fulton-Howard B, Podlesny-Drabiniok A, Marcora E, Goate AM |date=April 2023 |title=The complex genetic architecture of Alzheimer's disease: novel insights and future directions |url= |journal=eBioMedicine |volume=90 |pages=104511 |doi=10.1016/j.ebiom.2023.104511 |pmc=10024184 |pmid=36907103}}</ref><ref name=Scheltens2021>{{cite journal |vauthors=Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, Cummings J, van der Flier WM |date=April 2021 |title=Alzheimer's disease |url= |journal=Lancet |volume=397 |issue=10284 |pages=1577–1590 |doi=10.1016/S0140-6736(20)32205-4 |pmc=8354300 |pmid=33667416}}</ref> Genetic models in 2020 predict Alzheimer's disease with 90% accuracy.<ref>{{cite journal |vauthors=Sims R, Hill M, Williams J |date=March 2020 |title=The multiplex model of the genetics of Alzheimer's disease |url= https://orca.cardiff.ac.uk/id/eprint/129659/1/Nature%20Neuroscience.pdf|journal=Nat Neurosci |volume=23 |issue=3 |pages=311–322 |doi=10.1038/s41593-020-0599-5 |pmid=32112059|s2cid=256839971 }}</ref> Most cases of Alzheimer's are not ], and so they are termed sporadic Alzheimer's disease.<ref>{{Cite journal |last1=Chávez-Gutiérrez |first1=Lucía |last2=Szaruga |first2=Maria |date=2020-09-01 |title=Mechanisms of neurodegeneration — Insights from familial Alzheimer's disease |url=https://www.sciencedirect.com/science/article/pii/S1084952118302969 |journal=Seminars in Cell & Developmental Biology |series=Gamma Secretase |volume=105 |pages=75–85 |doi=10.1016/j.semcdb.2020.03.005 |pmid=32418657 |issn=1084-9521}}</ref> Of the cases of sporadic Alzheimer's disease, most are classified as late onset where they are developed after the age of 65 years.<ref>{{cite journal |vauthors=Piaceri I, Nacmias B, Sorbi S |title=Genetics of familial and sporadic Alzheimer's disease |journal=Frontiers in Bioscience (Elite Edition) |volume=5 |issue=1 |pages=167–177 |date=January 2013 |pmid=23276979 |doi=10.2741/e605|doi-access=free }}</ref> | |||
| The strongest genetic risk factor for sporadic Alzheimer's disease is ].<ref name="NIA2021" /> APOEε4 is one of four alleles of ] (APOE). APOE plays a major role in lipid-binding proteins in lipoprotein particles and the ] allele disrupts this function.<ref name="Perea">{{cite journal |vauthors=Perea JR, Bolós M, Avila J |date=October 2020 |title=Microglia in Alzheimer's Disease in the Context of Tau Pathology |journal=Biomolecules |volume=10 |issue=10 |page=1439 |doi=10.3390/biom10101439 |pmc=7602223 |pmid=33066368 |doi-access=free |title-link=doi}}</ref> Between 40% and 80% of people with Alzheimer's disease possess at least one APOEε4 allele.<ref name="pmid16567625">{{cite journal |vauthors=Mahley RW, Weisgraber KH, Huang Y |date=April 2006 |title=Apolipoprotein E4: a causative factor and therapeutic target in neuropathology, including Alzheimer's disease |journal=Proceedings of the National Academy of Sciences of the United States of America |volume=103 |issue=15 |pages=5644–5651 |bibcode=2006PNAS..103.5644M |doi=10.1073/pnas.0600549103 |pmc=1414631 |pmid=16567625 |doi-access=free |title-link=doi}}</ref> The APOEε4 allele increases the risk of the disease by three times in ] and by 15 times in ].<ref name="pmid16876668">{{cite journal |vauthors=Blennow K, de Leon MJ, Zetterberg H |date=July 2006 |title=Alzheimer's disease |journal=Lancet |volume=368 |issue=9533 |pages=387–403 |doi=10.1016/S0140-6736(06)69113-7 |pmid=16876668 |s2cid=47544338}}</ref> Like many human diseases, environmental effects and genetic modifiers result in incomplete ]. For example, Nigerian ] people do not show the relationship between dose of APOEε4 and incidence or age-of-onset for Alzheimer's disease seen in other human populations.<ref name="pmid16434658">{{cite journal |vauthors=Hall K, Murrell J, Ogunniyi A, Deeg M, Baiyewu O, Gao S, Gureje O, Dickens J, Evans R, Smith-Gamble V, Unverzagt FW, Shen J, Hendrie H |date=January 2006 |title=Cholesterol, APOE genotype, and Alzheimer disease: an epidemiologic study of Nigerian Yoruba |journal=Neurology |volume=66 |issue=2 |pages=223–227 |doi=10.1212/01.wnl.0000194507.39504.17 |pmc=2860622 |pmid=16434658}}</ref><ref name="pmid16278853">{{cite journal |vauthors=Gureje O, Ogunniyi A, Baiyewu O, Price B, Unverzagt FW, Evans RM, Smith-Gamble V, Lane KA, Gao S, Hall KS, Hendrie HC, Murrell JR |date=January 2006 |title=APOE epsilon4 is not associated with Alzheimer's disease in elderly Nigerians |journal=Annals of Neurology |volume=59 |issue=1 |pages=182–185 |doi=10.1002/ana.20694 |pmc=2855121 |pmid=16278853}}</ref> | |||
| ==== Early onset ==== | |||
| {{further|Early-onset Alzheimer's disease}} | |||
| Only 1–2% of Alzheimer's cases are ] due to ] effects, as Alzheimer's is highly polygenic. When the disease is caused by autosomal dominant variants, it is known as ], which is rarer and has a faster rate of progression.<ref name="Long">{{cite journal | vauthors = Long JM, Holtzman DM | title = Alzheimer Disease: An Update on Pathobiology and Treatment Strategies | journal = Cell | volume = 179 | issue = 2 | pages = 312–339 | date = October 2019 | pmid = 31564456 | pmc = 6778042 | doi = 10.1016/j.cell.2019.09.001 }}</ref> Less than 5% of sporadic Alzheimer's disease have an earlier onset,<ref name="Long" /> and early-onset Alzheimer's is about 90% heritable.<ref name=Andrews2023/><ref name=Scheltens2021/> Familial Alzheimer's disease usually implies two or more persons affected in one or more generations.<ref>{{Cite journal |last1=Schramm |first1=C. |last2=Wallon |first2=D. |last3=Nicolas |first3=G. |last4=Charbonnier |first4=C. |date=2022-05-01 |title=What contribution can genetics make to predict the risk of Alzheimer's disease? |url=https://www.sciencedirect.com/science/article/abs/pii/S0035378722005537 |journal=Revue Neurologique |series=International meeting of the French society of neurology : NeuroDegenerative Disease : What will the future bring ? |volume=178 |issue=5 |pages=414–421 |doi=10.1016/j.neurol.2022.03.005 |pmid=35491248 |issn=0035-3787}}</ref><ref>{{Cite journal |last1=Goldman |first1=Jill S. |last2=Van Deerlin |first2=Vivianna M. |date=2018-10-01 |title=Alzheimer's Disease and Frontotemporal Dementia: The Current State of Genetics and Genetic Testing Since the Advent of Next-Generation Sequencing |journal=Molecular Diagnosis & Therapy |language=en |volume=22 |issue=5 |pages=505–513 |doi=10.1007/s40291-018-0347-7 |issn=1179-2000 |pmc=6472481 |pmid=29971646}}</ref><ref>{{cite journal |vauthors=Piaceri I |date=2013 |title=Genetics of familial and sporadic Alzheimer s disease |journal=Frontiers in Bioscience |volume=E5 |issue=1 |pages=167–177 |doi=10.2741/E605 |issn=1945-0494 |pmid=23276979 |doi-access=free}}</ref> | |||
| Early onset familial Alzheimer's disease can be attributed to mutations in one of three genes: those encoding ] (APP) and ]s ] and ].<ref name="Atri2019" /> Most mutations in the APP and presenilin genes increase the production of a small protein called ] (Aβ)42, which is the main component of ].<ref name="Selkoe">{{cite journal | vauthors = Selkoe DJ | title = Translating cell biology into therapeutic advances in Alzheimer's disease | journal = Nature | volume = 399 | issue = 6738 Suppl | pages = A23–A31 | date = June 1999 | pmid = 10392577 | doi = 10.1038/19866 | s2cid = 42287088 | doi-access = free | title-link = doi }}</ref> Some of the mutations merely alter the ratio between Aβ42 and the other major forms—particularly Aβ40—without increasing Aβ42 levels in the brain.<ref name="Borchelt">{{cite journal | vauthors = Borchelt DR, Thinakaran G, Eckman CB, Lee MK, Davenport F, Ratovitsky T, Prada CM, Kim G, Seekins S, Yager D, Slunt HH, Wang R, Seeger M, Levey AI, Gandy SE, Copeland NG, Jenkins NA, Price DL, Younkin SG, Sisodia SS | title = Familial Alzheimer's disease-linked presenilin 1 variants elevate Abeta1-42/1-40 ratio in vitro and in vivo | journal = Neuron | volume = 17 | issue = 5 | pages = 1005–1013 | date = November 1996 | pmid = 8938131 | doi = 10.1016/S0896-6273(00)80230-5 | s2cid = 18315650 | doi-access = free | title-link = doi }}</ref> Two other genes associated with autosomal dominant Alzheimer's disease are ] and ].<ref>{{cite journal | vauthors = Kim JH | title = Genetics of Alzheimer's Disease | journal = Dementia and Neurocognitive Disorders | volume = 17 | issue = 4 | pages = 131–136 | date = December 2018 | pmid = 30906402 | pmc = 6425887 | doi = 10.12779/dnd.2018.17.4.131 }}</ref> | |||
| ]s in the ] gene have been associated with a three to five times higher risk of developing Alzheimer's disease.<ref>{{cite journal |vauthors=Carmona S, Zahs K, Wu E, Dakin K, Bras J, Guerreiro R |title=The role of TREM2 in Alzheimer's disease and other neurodegenerative disorders |journal=Lancet Neurol |volume=17 |issue=8 |pages=721–730 |date=August 2018 |pmid=30033062 |doi=10.1016/S1474-4422(18)30232-1 |s2cid=51706988 |url=https://discovery.ucl.ac.uk/id/eprint/10056337/ |access-date=21 February 2022 |archive-date=27 March 2022 |archive-url=https://web.archive.org/web/20220327190158/https://discovery.ucl.ac.uk/id/eprint/10056337/ |url-status=live }}</ref> | |||
| A Japanese pedigree of familial Alzheimer's disease was found to be associated with a deletion mutation of codon 693 of APP.<ref name=Tomiyama2010>{{cite journal | vauthors = Tomiyama T | title = | journal = Brain and Nerve = Shinkei Kenkyu No Shinpo | volume = 62 | issue = 7 | pages = 691–699 | date = July 2010 | pmid = 20675873 }}</ref> This mutation and its association with Alzheimer's disease was first reported in 2008,<ref name=Tomiyama2008>{{cite journal | vauthors = Tomiyama T, Nagata T, Shimada H, Teraoka R, Fukushima A, Kanemitsu H, Takuma H, Kuwano R, Imagawa M, Ataka S, Wada Y, Yoshioka E, Nishizaki T, Watanabe Y, Mori H | title = A new amyloid beta variant favoring oligomerization in Alzheimer's-type dementia | journal = Annals of Neurology | volume = 63 | issue = 3 | pages = 377–387 | date = March 2008 | pmid = 18300294 | doi = 10.1002/ana.21321 | s2cid = 42311988 }}</ref> and is known as the Osaka mutation. Only homozygotes with this mutation have an increased risk of developing Alzheimer's disease. This mutation accelerates Aβ oligomerization but the proteins do not form the amyloid fibrils that aggregate into amyloid plaques, suggesting that it is the Aβ oligomerization rather than the fibrils that may be the cause of this disease. Mice expressing this mutation have all the usual pathologies of Alzheimer's disease.<ref name=Tomiyama>{{cite journal | vauthors = Tomiyama T, Shimada H | title = APP Osaka Mutation in Familial Alzheimer's Disease-Its Discovery, Phenotypes, and Mechanism of Recessive Inheritance | journal = International Journal of Molecular Sciences | volume = 21 | issue = 4 | page = 1413 | date = February 2020 | pmid = 32093100 | pmc = 7073033 | doi = 10.3390/ijms21041413 | doi-access = free | title-link = doi }}</ref> | |||
| ===Hypotheses=== | |||
| ==== Amyloid beta and tau protein ==== | |||
| ] | |||
| The ] proposes that ] abnormalities initiate the disease cascade.<ref name=tzi/> In this model, ] tau begins to pair with other threads of tau as ]s. Eventually, they form ]s inside neurons.<ref name="tzi">{{cite journal |vauthors=Tzioras M, Davies C, Newman A, Jackson R, Spires-Jones T |title=Invited Review: APOE at the interface of inflammation, neurodegeneration and pathological protein spread in Alzheimer's disease |journal=Neuropathology and Applied Neurobiology |volume=45 |issue=4 |pages=327–346 |date=June 2019 |pmid=30394574 |pmc=6563457 |doi=10.1111/nan.12529}}</ref> When this occurs, the ]s disintegrate, destroying the structure of the cell's ] which collapses the neuron's transport system.<ref name=tzi/> | |||
| A number of studies connect the misfolded amyloid beta and tau proteins associated with the pathology of Alzheimer's disease, as bringing about ] that leads to ].<ref name=Sinyor>{{cite journal | vauthors = Sinyor B, Mineo J, Ochner C | title = Alzheimer's Disease, Inflammation, and the Role of Antioxidants | journal = Journal of Alzheimer's Disease Reports | volume = 4 | issue = 1 | pages = 175–183 | date = June 2020 | pmid = 32715278 | pmc = 7369138 | doi = 10.3233/ADR-200171 }}</ref> This chronic inflammation is also a feature of other neurodegenerative diseases including ], and ].<ref name=Kinney>{{cite journal | vauthors = Kinney JW, Bemiller SM, Murtishaw AS, Leisgang AM, Salazar AM, Lamb BT | title = Inflammation as a central mechanism in Alzheimer's disease | journal = Alzheimer's & Dementia | volume = 4 | issue = | pages = 575–590 | date = 2018 | pmid = 30406177 | pmc = 6214864 | doi = 10.1016/j.trci.2018.06.014 }}</ref> ]s have also been linked to dementia.<ref name=Breijyeh2020 /> ] accumulate in Alzheimer's diseased brains; ] may be the major source of this DNA damage.<ref>{{cite journal |vauthors=Lin X, Kapoor A, Gu Y, Chow MJ, Peng J, Zhao K, Tang D |title=Contributions of DNA Damage to Alzheimer's Disease |journal=Int J Mol Sci |volume=21 |issue=5 |date=February 2020 |page=1666 |pmid=32121304 |pmc=7084447 |doi=10.3390/ijms21051666 |doi-access=free }}</ref> | |||
| ==== Sleep ==== | |||
| ]s are seen as a possible ] for inflammation in Alzheimer's disease.<ref name="Irwin">{{cite journal | vauthors = Irwin MR, Vitiello MV | title = Implications of sleep disturbance and inflammation for Alzheimer's disease dementia | journal = The Lancet. Neurology | volume = 18 | issue = 3 | pages = 296–306 | date = March 2019 | pmid = 30661858 | doi = 10.1016/S1474-4422(18)30450-2 | s2cid = 58546748 }}</ref> Sleep disruption was previously only seen as a consequence of Alzheimer's disease, but {{As of|2020|lc=y}}, accumulating evidence suggests that this relationship may be ].<ref>{{cite journal | vauthors = Lloret MA, Cervera-Ferri A, Nepomuceno M, Monllor P, Esteve D, Lloret A | title = Is Sleep Disruption a Cause or Consequence of Alzheimer's Disease? Reviewing Its Possible Role as a Biomarker | journal = International Journal of Molecular Sciences | volume = 21 | issue = 3 | pages = 1168 | date = February 2020 | pmid = 32050587 | pmc = 7037733 | doi = 10.3390/ijms21031168 | doi-access = free }}</ref> | |||
| ==== Metal toxicity, smoking, neuroinflammation and air pollution ==== | |||
| The cellular ] of ] such as ionic copper, iron, and zinc is disrupted in Alzheimer's disease, though it remains unclear whether this is produced by or causes the changes in proteins.<ref name=Breijyeh2020 /><ref>{{cite journal |vauthors=Huat TJ, Camats-Perna J, Newcombe EA, Valmas N, Kitazawa M, Medeiros R |title=Metal Toxicity Links to Alzheimer's Disease and Neuroinflammation |journal=J Mol Biol |volume=431 |issue=9 |pages=1843–1868 |date=April 2019 |pmid=30664867 |pmc=6475603 |doi=10.1016/j.jmb.2019.01.018 }}</ref> Smoking is a significant Alzheimer's disease risk factor.<ref name=Knopman2021>{{cite journal |vauthors = Knopman DS, Amieva H, Petersen RC, Chételat G, Holtzman DM, Hyman BT, Nixon RA, Jones DT |title=Alzheimer disease |journal=Nature Reviews Disease Primers |volume=7 |issue=1 |pages=33 |date=May 2021 |pmid=33986301 |pmc=8574196 |doi=10.1038/s41572-021-00269-y }}</ref> ] of the ] are risk factors for late-onset Alzheimer's disease.<ref>{{cite journal | vauthors = Eikelenboom P, van Exel E, Hoozemans JJ, Veerhuis R, Rozemuller AJ, van Gool WA | title = Neuroinflammation – an early event in both the history and pathogenesis of Alzheimer's disease | journal = Neuro-Degenerative Diseases | volume = 7 | issue = 1–3 | pages = 38–41 | year = 2010 | pmid = 20160456 | doi = 10.1159/000283480 | s2cid = 40048333 }}</ref> ] may be a contributing factor to the development of Alzheimer's disease.<ref name=Breijyeh2020 /> | |||
| ==== Age-related myelin decline ==== | |||
| Retrogenesis is a medical ] that just as the fetus goes through a process of ] beginning with ] and ending with ], the brains of people with Alzheimer's disease go through a reverse ] process starting with ] and death of axons (white matter) and ending with the death of grey matter.<ref name="Laks2015">{{cite journal |vauthors=Alves GS, Oertel Knöchel V, Knöchel C, Carvalho AF, Pantel J, Engelhardt E, Laks J |date=2015 |title=Integrating retrogenesis theory to Alzheimer's disease pathology: insight from DTI-TBSS investigation of the white matter microstructural integrity |journal=BioMed Research International |volume=2015 |pages=291658 |doi=10.1155/2015/291658 |pmc=4320890 |pmid=25685779 |doi-access=free |title-link=doi}}</ref> Likewise the hypothesis is, that as infants go through states of ], people with Alzheimer's disease go through the reverse process of progressive ].<ref name="Kluger1999">{{cite journal |vauthors=Reisberg B, Franssen EH, Hasan SM, Monteiro I, Boksay I, Souren LE, Kenowsky S, Auer SR, Elahi S, Kluger A |date=1999 |title=Retrogenesis: clinical, physiologic, and pathologic mechanisms in brain aging, Alzheimer's and other dementing processes |journal=European Archives of Psychiatry and Clinical Neuroscience |volume=249 |issue=3 |pages=28–36 |doi=10.1007/pl00014170 |pmid=10654097 |s2cid=23410069}}</ref> | |||
| According to one theory, dysfunction of ] and their associated ] during aging contributes to ] damage, which in turn generates in amyloid production and tau ].<ref>{{cite journal | vauthors = Bartzokis G | title = Alzheimer's disease as homeostatic responses to age-related myelin breakdown | journal = Neurobiology of Aging | volume = 32 | issue = 8 | pages = 1341–1371 | date = August 2011 | pmid = 19775776 | pmc = 3128664 | doi = 10.1016/j.neurobiolaging.2009.08.007 }}</ref><ref>{{cite journal | vauthors = Cai Z, Xiao M | title = Oligodendrocytes and Alzheimer's disease | journal = The International Journal of Neuroscience | volume = 126 | issue = 2 | pages = 97–104 | date = 2016 | pmid = 26000818 | doi = 10.3109/00207454.2015.1025778 | s2cid = 21448714 }}</ref> An '']'' study employing genetic mouse models to simulate myelin dysfunction and ] further reveal that age-related myelin degradation increases sites of Aβ production and distracts ] from Aβ plaques, with both mechanisms dually exacerbating amyloidosis.<ref>{{cite journal | vauthors = Depp C, Sun T, Sasmita AO, Spieth L, Berghoff SA, Nazarenko T, Overhoff K, Steixner-Kumar AA, Subramanian S, Arinrad S, Ruhwedel T, Möbius W, Göbbels S, Saher G, Werner HB, Damkou A, Zampar S, Wirths O, Thalmann M, Simons M, Saito T, Saido T, Krueger-Burg D, Kawaguchi R, Willem M, Haass C, Geschwind D, Ehrenreich H, Stassart R, Nave KA | title = Myelin dysfunction drives amyloid-β deposition in models of Alzheimer's disease | journal = Nature | volume = 618 | issue = 7964 | pages = 349–357 | date = June 2023 | pmid = 37258678 | pmc = 10247380 | doi = 10.1038/s41586-023-06120-6 | bibcode = 2023Natur.618..349D }}</ref> Additionally, ] between the demyelinating disease, ], and Alzheimer's disease have been reported.<ref>{{cite journal | vauthors = Luczynski P, Laule C, Hsiung GR, Moore GR, Tremlett H | title = Coexistence of Multiple Sclerosis and Alzheimer's disease: A review | journal = Multiple Sclerosis and Related Disorders | volume = 27 | pages = 232–238 | date = January 2019 | pmid = 30415025 | doi = 10.1016/j.msard.2018.10.109 }}</ref><ref>{{cite journal | vauthors = Londoño DP, Arumaithurai K, Constantopoulos E, Basso MR, Reichard RR, Flanagan EP, Keegan BM | title = Diagnosis of coexistent neurodegenerative dementias in multiple sclerosis | journal = Brain Communications | volume = 4 | issue = 4 | pages = fcac167 | date = 2022-07-04 | pmid = 35822102 | pmc = 9272064 | doi = 10.1093/braincomms/fcac167 }}</ref> | |||
| ==== Other hypotheses ==== | |||
| {{Anchor|Retrogenesis}} | |||
| {{See also|Cell cycle hypothesis of Alzheimer's disease|Ion channel hypothesis of Alzheimer's disease}}The association with ] is unclear, with a 2019 study finding no increase in dementia overall in those with celiac disease while a 2018 review found an association with several types of dementia including Alzheimer's disease.<ref>{{cite journal | vauthors = Zis P, Hadjivassiliou M | title = Treatment of Neurological Manifestations of Gluten Sensitivity and Coeliac Disease | journal = Current Treatment Options in Neurology | volume = 21 | issue = 3 | pages = 10 | date = February 2019 | pmid = 30806821 | doi = 10.1007/s11940-019-0552-7 | s2cid = 73466457 | doi-access = free | title-link = doi }}</ref><ref name=MakhloufMesselmani2018>{{cite journal | vauthors = Makhlouf S, Messelmani M, Zaouali J, Mrissa R | title = Cognitive impairment in celiac disease and non-celiac gluten sensitivity: review of literature on the main cognitive impairments, the imaging and the effect of gluten free diet | journal = Acta Neurologica Belgica | volume = 118 | issue = 1 | pages = 21–27 | date = March 2018 | pmid = 29247390 | doi = 10.1007/s13760-017-0870-z | type = Review | s2cid = 3943047 }}</ref> | |||
| Studies have shown a potential link between infection with certain viruses and developing Alzheimer's disease later in life.<ref>{{cite journal | vauthors = Zhou L, Miranda-Saksena M, Saksena NK | title = Viruses and neurodegeneration | journal = Virology Journal | volume = 10 | issue = 1 | pages = 172 | date = May 2013 | pmid = 23724961 | pmc = 3679988 | doi = 10.1186/1743-422X-10-172 | doi-access = free }}</ref> Notably, a large scale study conducted on 6,245,282 patients has shown an increased risk of developing ] in cognitively normal individuals over 65.<ref>{{cite journal | vauthors = Gonzalez-Fernandez E, Huang J | title = Cognitive Aspects of COVID-19 | journal = Current Neurology and Neuroscience Reports | volume = 23 | issue = 9 | pages = 531–538 | date = September 2023 | pmid = 37490194 | doi = 10.1007/s11910-023-01286-y | s2cid = 260132167 }}</ref> | |||
| == Pathophysiology == | |||
| ] images of Alzheimer's disease, in the ], showing an amyloid plaque (top right), neurofibrillary tangles (bottom left), and ] (bottom center)]] | |||
| ===Neuropathology=== | ===Neuropathology=== | ||
| Both amyloid plaques and neurofibrillary tangles are clearly visible by ] in AD brains.<ref name="Tiraboschi">{{cite journal | author = Tiraboschi P, Hansen L, Thal L, Corey-Bloom J | title = The importance of neuritic plaques and tangles to the development and evolution of AD. | journal = Neurology | volume = 62 | issue = 11 | pages = 1984-9 | year = 2004 | id = PMID 15184601}}</ref> At an anatomical level, AD is characterized by gross diffuse atrophy of the brain and loss of neurons, neuronal processes and synapses in the ] and certain subcortical regions. This results in gross ] of the affected regions, including degeneration in the ] and ], and parts of the ] and ].<ref name="Wenk">{{cite journal | author = Wenk G | title = Neuropathologic changes in Alzheimer's disease. | journal = J Clin Psychiatry | volume = 64 Suppl 9 | issue = | pages = 7-10 | year = | id = PMID 12934968}}</ref> Levels of the neurotransmitter ] are reduced. Levels of the neurotransmitters ], ], and ] are also often reduced. ] levels are usually elevated.<ref> | |||
| Alzheimer's disease is characterised by loss of ]s and ]s in the ] and certain subcortical regions. This loss results in gross ] of the affected regions, including degeneration in the ] and ], and parts of the ] and ].<ref name=pmid12934968>{{cite journal | vauthors = Wenk GL | title = Neuropathologic changes in Alzheimer's disease | journal = The Journal of Clinical Psychiatry | volume = 64 | issue = Suppl 9 | pages = 7–10 | year = 2003 | pmid = 12934968 }}</ref> Degeneration is also present in ] nuclei particularly the ] in the ].<ref>{{cite journal | vauthors = Braak H, Del Tredici K | title = Where, when, and in what form does sporadic Alzheimer's disease begin? | journal = Current Opinion in Neurology | volume = 25 | issue = 6 | pages = 708–714 | date = December 2012 | pmid = 23160422 | doi = 10.1097/WCO.0b013e32835a3432 }}</ref> Studies using ] and ] have documented reductions in the size of specific brain regions in people with Alzheimer's disease as they progressed from mild cognitive impairment to Alzheimer's disease, and in comparison with similar images from healthy older adults.<ref>{{cite journal | vauthors = Desikan RS, Cabral HJ, Hess CP, Dillon WP, Glastonbury CM, Weiner MW, Schmansky NJ, Greve DN, Salat DH, Buckner RL, Fischl B | title = Automated MRI measures identify individuals with mild cognitive impairment and Alzheimer's disease | journal = Brain | volume = 132 | issue = Pt 8 | pages = 2048–2057 | date = August 2009 | pmid = 19460794 | pmc = 2714061 | doi = 10.1093/brain/awp123 }}</ref><ref>{{cite journal |vauthors=Moan R |title=MRI Software Accurately IDs Preclinical Alzheimer's Disease |journal=Diagnostic Imaging |date=July 2009 |url=https://www.diagnosticimaging.com/view/mri-software-accurately-ids-preclinical-alzheimers-disease |access-date=21 February 2022 |archive-date=21 February 2022 |archive-url=https://web.archive.org/web/20220221050502/https://www.diagnosticimaging.com/view/mri-software-accurately-ids-preclinical-alzheimers-disease |url-status=live }}</ref> | |||
| {{cite web | |||
| | last = Baskys | |||
| Both ] ] and ]s are clearly visible by ] in brains of those with Alzheimer's disease,<ref name=pmid15184601>{{cite journal | vauthors = Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J | title = The importance of neuritic plaques and tangles to the development and evolution of AD | journal = Neurology | volume = 62 | issue = 11 | pages = 1984–1989 | date = June 2004 | pmid = 15184601 | doi = 10.1212/01.WNL.0000129697.01779.0A | s2cid = 25017332 }}</ref> especially in the ].<ref name=DeTureDickson2019>{{cite journal | vauthors = DeTure MA, Dickson DW | title = The neuropathological diagnosis of Alzheimer's disease | journal = Molecular Neurodegeneration | volume = 14 | issue = 1 | pages = 32 | date = August 2019 | pmid = 31375134 | pmc = 6679484 | doi = 10.1186/s13024-019-0333-5 | doi-access = free }}</ref> However, Alzheimer's disease may occur without neurofibrillary tangles in the ].<ref name=pmid15079014>{{cite journal | vauthors = Tiraboschi P, Sabbagh MN, Hansen LA, Salmon DP, Merdes A, Gamst A, Masliah E, Alford M, Thal LJ, Corey-Bloom J | title = Alzheimer disease without neocortical neurofibrillary tangles: "a second look" | journal = Neurology | volume = 62 | issue = 7 | pages = 1141–1147 | date = April 2004 | pmid = 15079014 | doi = 10.1212/01.wnl.0000118212.41542.e7 | s2cid = 22832110 }}</ref> Plaques are dense, mostly ] deposits of ] peptide and ] material outside and around ]. Neurofibrillary tangles are aggregates of the microtubule-associated protein tau which has become hyperphosphorylated and accumulate inside the cells themselves. Although many older individuals develop some plaques and tangles as a consequence of aging, the brains of people with Alzheimer's disease have a greater number of them in specific brain regions such as the ].<ref name=pmid8038565>{{cite journal | vauthors = Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH | title = Regional distribution of neurofibrillary tangles and senile plaques in the cerebral cortex of elderly patients: a quantitative evaluation of a one-year autopsy population from a geriatric hospital | journal = Cerebral Cortex | volume = 4 | issue = 2 | pages = 138–150 | year = 1994 | pmid = 8038565 | doi = 10.1093/cercor/4.2.138 }}</ref> ] are not rare in the brains of people with Alzheimer's disease.<ref name=pmid11816795>{{cite journal | vauthors = Kotzbauer PT, Trojanowsk JQ, Lee VM | title = Lewy body pathology in Alzheimer's disease | journal = Journal of Molecular Neuroscience | volume = 17 | issue = 2 | pages = 225–232 | date = October 2001 | pmid = 11816795 | doi = 10.1385/JMN:17:2:225 | s2cid = 44407971 }}</ref> | |||
| | first = | |||
| | title = Receptor found that could lead to better treatments for stroke, alzheimer's disease | |||
| ===Biochemistry=== | |||
| | publisher = UCI Medical Center | |||
| {{Main|Biochemistry of Alzheimer's disease}} | |||
| | url = http://www.ucihealth.com/News/Releases/Receptor_found_treat_stroke_alzheimers_9-13-00.htm | |||
| | accessdate = 2006-11-04 }} | |||
| ==== Amyloid beta ==== | |||
| </ref> | |||
| {{Multiple image|footer=Enzymes act on the amyloid-beta precursor protein and cut it into fragments. The beta-amyloid fragment is crucial in the formation of amyloid plaques in Alzheimer's disease.|image1=Amyloid 01big1.jpg|image2=Amyloid 02big1.jpg|image3=Amyloid 03big1.jpg}} | |||
| Alzheimer's disease has been identified as a ], a ], caused by the accumulation of abnormally folded ] protein into amyloid plaques, and ] into neurofibrillary tangles in the brain.<ref name=tzi/> Plaques are made up of small ]s, 39–43 ]s in length, called amyloid beta. Amyloid beta is a fragment from the larger ] (APP) a ] that penetrates the ]. APP is critical to neuron growth, survival, and post-injury repair.<ref name=tzi/> In Alzheimer's disease, ] and ] act together in a ] process which causes APP to be divided into smaller fragments.<ref name=tzi/> Although commonly researched as neuronal proteins, APP and its processing enzymes are abundantly expressed by other brain cells. One of these fragments gives rise to ] of amyloid beta, which then form clumps that deposit outside neurons in dense formations known as amyloid plaques.<ref name=tzi/> Excitatory neurons are known to be the major producers of amyloid beta that contribute to major extracellular plaque deposition.<ref name=tzi/> | |||
| ==== Phosphorylated tau ==== | |||
| Alzheimer's disease is also considered a ] due to abnormal aggregation of the ]. Every neuron has a ], an internal support structure partly made up of structures called ]. These microtubules act like tracks, guiding nutrients and molecules from the body of the cell to the ends of the ] and back. A protein called ''tau'' stabilises the microtubules when ], and is therefore called a ]. In Alzheimer's disease, tau undergoes chemical changes, becoming hyperphosphorylated; it then begins to pair with other threads, creating neurofibrillary tangles and disintegrating the neuron's transport system.<ref name="pmid17604998">{{cite journal | vauthors = Hernández F, Avila J | title = Tauopathies | journal = Cellular and Molecular Life Sciences | volume = 64 | issue = 17 | pages = 2219–2233 | date = September 2007 | pmid = 17604998 | doi = 10.1007/s00018-007-7220-x | s2cid = 261121643 | pmc = 11136052 }}</ref> Pathogenic tau can also cause neuronal death through ] dysregulation.<ref>{{cite journal | vauthors = Sun W, Samimi H, Gamez M, Zare H, Frost B | title = Pathogenic tau-induced piRNA depletion promotes neuronal death through transposable element dysregulation in neurodegenerative tauopathies | journal = Nature Neuroscience | volume = 21 | issue = 8 | pages = 1038–1048 | date = August 2018 | pmid = 30038280 | pmc = 6095477 | doi = 10.1038/s41593-018-0194-1 }}</ref> ] has also been reported as a mechanism of cell death in brain cells affected with tau tangles.<ref>Balusu S, Horré K, Thrupp N, Craessaerts K, Snellinx A, Serneels L, T'Syen D, Chrysidou I, Arranz AM, Sierksma A, Simrén J, Karikari TK, Zetterberg H, Chen WT, Thal DR, Salta E, Fiers M, De Strooper B. MEG3 activates necroptosis in human neuron xenografts modeling Alzheimer's disease. ''Science''. 2023 Sep 15;381(6663):1176-1182. {{doi|10.1126/science.abp9556}} {{PMID|37708272}}</ref><ref>{{cite news |date=2023-09-15 |title=Scientists discover how brain cells die in Alzheimer's |language=en-GB |work=BBC News |url=https://www.bbc.com/news/health-66816268 |access-date=2023-09-27}}</ref> | |||
| ===Disease mechanism=== | ===Disease mechanism=== | ||
| Exactly how disturbances of production and aggregation of the beta-amyloid ] give rise to the pathology of Alzheimer's disease is not known.<ref name=pmid17622778>{{cite journal | vauthors = Van Broeck B, Van Broeckhoven C, Kumar-Singh S | title = Current insights into molecular mechanisms of Alzheimer disease and their implications for therapeutic approaches | journal = Neuro-Degenerative Diseases | volume = 4 | issue = 5 | pages = 349–365 | year = 2007 | pmid = 17622778 | doi = 10.1159/000105156 | s2cid = 7949658 }}</ref><ref>{{cite journal | vauthors = Huang Y, Mucke L | title = Alzheimer mechanisms and therapeutic strategies | journal = Cell | volume = 148 | issue = 6 | pages = 1204–1222 | date = March 2012 | pmid = 22424230 | pmc = 3319071 | doi = 10.1016/j.cell.2012.02.040 }}</ref> The amyloid hypothesis traditionally points to the accumulation of beta-amyloid peptides as the central event triggering neuron degeneration. Accumulation of aggregated ]s, which are believed to be the toxic form of the protein responsible for disrupting the cell's ] ion ], induces ] (]).<ref name=pmid2218531>{{cite journal | vauthors = Yankner BA, Duffy LK, Kirschner DA | title = Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides | journal = Science | volume = 250 | issue = 4978 | pages = 279–282 | date = October 1990 | pmid = 2218531 | doi = 10.1126/science.2218531 | bibcode = 1990Sci...250..279Y }}</ref> It is also known that A<sub>β</sub> selectively builds up in the ] in the cells of Alzheimer's-affected brains, and it also inhibits certain ] functions and the utilisation of ] by neurons.<ref name=pmid17424907>{{cite journal | vauthors = Chen X, Yan SD | title = Mitochondrial Abeta: a potential cause of metabolic dysfunction in Alzheimer's disease | journal = IUBMB Life | volume = 58 | issue = 12 | pages = 686–694 | date = December 2006 | pmid = 17424907 | doi = 10.1080/15216540601047767 | s2cid = 85423830 }}</ref> | |||
| Three major competing hypotheses exist to explain the cause of the disease. The oldest, on which most currently available drug therapies are based, is known as the "] hypothesis" and suggests that AD is due to reduced biosynthesis of the ] ]. The medications that treat acetylcholine deficiency have served to only treat symptoms of the disease and have neither halted nor reversed it.<ref name="Rosen">{{cite journal | author = Walker LC, Rosen RF | title = Alzheimer therapeutics: What after the cholinesterase inhibitors? | journal = Age Ageing | volume = 35 | pages = 332-335 | year = 2006 | id = PMID 16644763}}</ref> The cholinergic hypothesis has not maintained widespread support in the face of this evidence, although cholingeric effects have been proposed to initiate large-scale aggregation<ref name="Shen">{{cite journal | author = Shen Z | title = Brain cholinesterases: II. The molecular and cellular basis of Alzheimer's disease. | journal = Med Hypotheses | volume = 63 | issue = 2 | pages = 308-21 | year = 2004 | id = PMID 15236795}} </ref> leading to generalized neuroinflammation.<ref name="Wenk" /> | |||
| Iron dyshomeostasis is linked to disease progression, an iron-dependent form of regulated cell death called ] could be involved. Products of ] are also elevated in AD brain compared with controls.<ref>{{cite journal | vauthors = Ryan SK, Ugalde CL, Rolland AS, Skidmore J, Devos D, Hammond TR | title = Therapeutic inhibition of ferroptosis in neurodegenerative disease | journal = Trends in Pharmacological Sciences | volume = 44 | issue = 10 | pages = 674–688 | date = October 2023 | pmid = 37657967 | doi = 10.1016/j.tips.2023.07.007 | doi-access = free }}</ref> | |||
| Research after 2000 includes hypotheses centered on the effects of the misfolded and aggregated proteins, amyloid beta and tau. The two positions differ with one stating that the ] abnormalities initiate the disease cascade, while the other states that ] (Aβ) deposits are the causative factor in the disease.<ref name="Mudher">{{cite journal | author = Mudher A, Lovestone S | title = Alzheimer's disease-do tauists and baptists finally shake hands? | journal = Trends Neurosci | volume = 25 | issue = 1 | pages = 22-6 | year = 2002 | id = PMID 11801334}}</ref> The tau hypothesis is supported by the long-standing observation that deposition of amyloid plaques do not correlate well with neuron loss;<ref name="Schmitz"> {{cite journal | author = Schmitz C, Rutten B, Pielen A, Schäfer S, Wirths O, Tremp G, Czech C, Blanchard V, Multhaup G, Rezaie P, Korr H, Steinbusch H, Pradier L, Bayer T | title = Hippocampal neuron loss exceeds amyloid plaque load in a transgenic mouse model of Alzheimer's disease. | journal = Am J Pathol | volume = 164 | issue = 4 | pages = 1495-502 | year = 2004 | id = PMID 15039236}}</ref> however, a majority of researchers support the alternative hypothesis that Aβ is the primary causative agent.<ref name="Mudher" /> | |||
| Various inflammatory processes and ]s may also have a role in the pathology of Alzheimer's disease. ] is a general marker of ] damage in any disease, and may be either secondary to tissue damage in Alzheimer's disease or a marker of an ].<ref name=pmid15681814>{{cite journal | vauthors = Greig NH, Mattson MP, Perry T, Chan SL, Giordano T, Sambamurti K, Rogers JT, Ovadia H, Lahiri DK | title = New therapeutic strategies and drug candidates for neurodegenerative diseases: p53 and TNF-alpha inhibitors, and GLP-1 receptor agonists | journal = Annals of the New York Academy of Sciences | volume = 1035 | pages = 290–315 | date = December 2004 | issue = 1 | pmid = 15681814 | doi = 10.1196/annals.1332.018 | bibcode = 2004NYASA1035..290G | s2cid = 84659695 | url = https://zenodo.org/record/1235888 | access-date = 19 July 2019 | archive-date = 3 June 2020 | archive-url = https://web.archive.org/web/20200603200152/https://zenodo.org/record/1235888/ | url-status = live }}</ref> There is increasing evidence of a strong interaction between the neurons and the immunological mechanisms in the brain. Obesity and systemic inflammation may interfere with immunological processes which promote disease progression.<ref>{{cite journal | vauthors = Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, Jacobs AH, Wyss-Coray T, Vitorica J, Ransohoff RM, Herrup K, Frautschy SA, Finsen B, Brown GC, Verkhratsky A, Yamanaka K, Koistinaho J, Latz E, Halle A, Petzold GC, Town T, Morgan D, Shinohara ML, Perry VH, Holmes C, Bazan NG, Brooks DJ, Hunot S, Joseph B, Deigendesch N, Garaschuk O, Boddeke E, Dinarello CA, Breitner JC, Cole GM, Golenbock DT, Kummer MP | title = Neuroinflammation in Alzheimer's disease | journal = The Lancet. Neurology | volume = 14 | issue = 4 | pages = 388–405 | date = April 2015 | pmid = 25792098 | pmc = 5909703 | doi = 10.1016/S1474-4422(15)70016-5 }}</ref> | |||
| The amyloid hypothesis is initially compelling because the gene for the amyloid beta precursor (APP) is located on ], and patients with ] (Down Syndrome) who thus have an extra ] almost universally exhibit AD-like disorders by 40 years of age.<ref name="Nistor">{{cite journal | author =Nistor M, Don M, Parekh M, Sarsoza F, Goodus M, Lopez GE, Kawas C, Leverenz J, Doran E, Lott IT, Hill M, Head E | title = Alpha- and beta-secretase activity as a function of age and Aβ in Down syndrome and normal brain. | journal = Neurobiol Aging | volume = | issue =epub | pages = | year =2006 | id = PMID 16904243}}</ref><ref name="Lott">{{cite journal | author = Lott I, Head E | title = Alzheimer disease and Down syndrome: factors in pathogenesis. | journal = Neurobiol Aging | volume = 26 | issue = 3 | pages = 383-9 | year = 2005 | id = PMID 15639317}} </ref> The traditional formulation of the amyloid hypothesis points to the cytotoxicity of mature aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis and thus inducing ].<ref name="Yankner">{{cite journal | author = Yankner B, Duffy L, Kirschner D | title = Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides. | journal = Science | volume = 250 | issue = 4978 | pages = 279-82 | year = 1990 | id = PMID 2218531}}</ref> A more recent and widely supported hypothesis suggests that the cytotoxic species is an intermediate misfolded form of Aβ, neither a soluble monomer nor a mature aggregated polymer but an ]ic species.<ref name="Blanchard1">{{cite journal | author =Blanchard BJ, Hiniker AE, Lu CC, Margolin Y, Yu AS, Ingram VM | title = Elimination of Amyloid beta Neurotoxicity. | journal = J Alzheimers Dis | volume = 2 | issue = 2 | pages = 137-149 | year = 2000 | id = PMID 12214104}} </ref> Relevantly, much early development work on ]s has focused on the inhibition of fibrillization,<ref name="Blanchard2">{{cite journal | author = Blanchard B, Chen A, Rozeboom L, Stafford K, Weigele P, Ingram V | title = Efficient reversal of Alzheimer's disease fibril formation and elimination of neurotoxicity by a small molecule. | journal = Proc Natl Acad Sci U S A | volume = 101 | issue = 40 | pages = 14326-32 | year = 2004 | id = PMID 15388848}}</ref><ref name="Porat">{{cite journal | author = Porat Y, Abramowitz A, Gazit E | title = Inhibition of amyloid fibril formation by polyphenols: structural similarity and aromatic interactions as a common inhibition mechanism. | journal = Chem Biol Drug Des | volume = 67 | issue = 1 | pages = 27-37 | year = 2006 | id = PMID 16492146}}</ref><ref name="Kanapathipillai">{{cite journal | author = Kanapathipillai M, Lentzen G, Sierks M, Park C | title = Ectoine and hydroxyectoine inhibit aggregation and neurotoxicity of Alzheimer's beta-amyloid. | journal = FEBS Lett | volume = 579 | issue = 21 | pages = 4775-80 | year = 2005 | id = PMID 16098972}}</ref> but the toxic-oligomer theory would imply that prevention of oligomeric assembly is the more important process<ref name="Lee">{{cite journal | author = Lee K, Shin B, Shin K, Kim D, Yu J | title = A hybrid molecule that prohibits amyloid fibrils and alleviates neuronal toxicity induced by beta-amyloid (1-42). | journal = Biochem Biophys Res Commun | volume = 328 | issue = 4 | pages = 816-23 | year = 2005 | id = PMID 15707952}}</ref> or that a better target lies upstream, for example in the inhibition of APP processing to amyloid beta.<ref name="Espeseth">{{cite journal | author = Espeseth A, Xu M, Huang Q, Coburn C, Jones K, Ferrer M, Zuck P, Strulovici B, Price E, Wu G, Wolfe A, Lineberger J, Sardana M, Tugusheva K, Pietrak B, Crouthamel M, Lai M, Dodson E, Bazzo R, Shi X, Simon A, Li Y, Hazuda D | title = Compounds that bind APP and inhibit Abeta processing ''in vitro'' suggest a novel approach to Alzheimer disease therapeutics. | journal = J Biol Chem | volume = 280 | issue = 18 | pages = 17792-7 | year = 2005 | id = PMID 15737955}}</ref> | |||
| Alterations in the distribution of different ]s and in the expression of their receptors such as the ] (BDNF) have been described in Alzheimer's disease.<ref>{{cite journal | vauthors = Tapia-Arancibia L, Aliaga E, Silhol M, Arancibia S | title = New insights into brain BDNF function in normal aging and Alzheimer disease | journal = Brain Research Reviews | volume = 59 | issue = 1 | pages = 201–220 | date = November 2008 | pmid = 18708092 | doi = 10.1016/j.brainresrev.2008.07.007 | hdl-access = free | s2cid = 6589846 | hdl = 10533/142174 }}</ref><ref>{{cite journal | vauthors = Schindowski K, Belarbi K, Buée L | title = Neurotrophic factors in Alzheimer's disease: role of axonal transport | journal = Genes, Brain and Behavior | volume = 7 | issue = Suppl 1 | pages = 43–56 | date = February 2008 | pmid = 18184369 | pmc = 2228393 | doi = 10.1111/j.1601-183X.2007.00378.x }}</ref> | |||
| It should be noted further that ApoE4, the major genetic risk factor for AD, leads to excess amyloid build up in the brain before AD symptoms arise. Thus, Aβ deposition precedes clinical AD.<ref>{{cite journal | author = Polvikoski T, Sulkava R, Haltia M, Kainulainen K, Vuorio A, Verkkoniemi A, Niinistö L, Halonen P, Kontula K | title = Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein. | journal = N Engl J Med | volume = 333 | issue = 19 | pages = 1242-7 | year = 1995 | id = PMID 7566000}}</ref> Another strong support for the amyloid hypothesis, which looks at Aβ as the common initiating factor for Alzheimer's disease, is that transgenic mice solely expressing a mutant human APP gene develop first diffuse and then fibrillar amyloid plaques, associated with neuronal and microglial damage.<ref>{{cite journal | author = Games D, Adams D, Alessandrini R, Barbour R, Berthelette P, Blackwell C, Carr T, Clemens J, Donaldson T, Gillespie F | title = Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein. | journal = Nature | volume = 373 | issue = 6514 | pages = 523-7 | year = 1995 | id = PMID 7845465}}</ref><ref>{{cite journal | author = Masliah E, Sisk A, Mallory M, Mucke L, Schenk D, Games D | title = Comparison of neurodegenerative pathology in transgenic mice overexpressing V717F beta-amyloid precursor protein and Alzheimer's disease. | journal = J Neurosci | volume = 16 | issue = 18 | pages = 5795-811 | year = 1996 | id = PMID 8795633}}</ref><ref>{{cite journal | author = Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, Younkin S, Yang F, Cole G | title = Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. | journal = Science | volume = 274 | issue = 5284 | pages = 99-102 | year = 1996 | id = PMID 8810256}}</ref> | |||
| == |
==Diagnosis== | ||
| {{See also|Early-onset Alzheimer's disease#Diagnosis}} | |||
| Rare cases of Alzheimer's are caused by dominant genes that run in families. These cases often have an early age of onset (usually <60 years). Nearly 200 different mutations in the presenilin-1 or presenilin-2 genes have been documented in over 500 families. Mutations of presenilin 1 (PS1) lead to the most aggressive form of ] (FAD). Over 20 different mutations in the APP gene on ] 21 can also cause early onset disease. APP was the first AD gene to be discovered in 1987.<ref name="decoding darkness"> The presenilins have been identified as essential components of the proteolytic processing machinery that produces beta amyloid peptides through cleavage of APP. Most mutations in the APP and presenilin genes increase the production of a small protein (peptide) called Abeta42, the main component of senile plaques in brains of AD patients. Inheritance of the ε4 allele of the ApoE gene is regarded as a risk factor for development of up to 50% of late-onset sporadic Alzheimer's. However, genetic experts agree that there are other risk and protective factor genes that influence the development of late onset Alzheimer's disease (LOAD). Over 400 genes have been tested for association with late-onset sproadic AD. The full list of these genes along with which genes exhibit the strongest association with AD are updated weekly and available at AlzGene.org <http://alzgene.org>. | |||
| ] of the brain of a person with Alzheimer's disease showing a loss of function in the temporal lobe]] | |||
| Alzheimer's disease (AD) can only be definitively diagnosed with autopsy findings; in the absence of autopsy, clinical diagnoses of AD are "possible" or "probable", based on other findings.<ref name=Khan2020>{{cite journal |vauthors=Khan S, Barve KH, Kumar MS |title=Recent Advancements in Pathogenesis, Diagnostics and Treatment of Alzheimer's Disease |journal=Curr Neuropharmacol |volume=18 |issue=11 |pages=1106–1125 |date=2020 |pmid=32484110 |pmc=7709159 |doi=10.2174/1570159X18666200528142429}}</ref><ref name=Gauthreaux2020>{{cite journal |vauthors = Gauthreaux K, Bonnett TA, Besser LM, Brenowitz WD, Teylan M, Mock C, Chen YC, Chan KC, Keene CD, Zhou XH, Kukull WA |title=Concordance of Clinical Alzheimer Diagnosis and Neuropathological Features at Autopsy |journal=Journal of Neuropathology and Experimental Neurology |volume=79 |issue=5 |pages=465–473 |date=May 2020 |pmid=32186726 |pmc=7160616 |doi=10.1093/jnen/nlaa014 }}</ref><ref name=Sachdev2014 /> Up to 23% of those clinically diagnosed with AD may be misdiagnosed and may have pathology suggestive of another condition with symptoms that mimic those of AD.<ref name=Gauthreaux2020 /> | |||
| AD is usually clinically diagnosed based on a person's ], observations from friends or relatives, and behavioral changes. The presence of characteristic ] changes with impairments in at least two cognitive domains that are severe enough to affect a person's functional abilities are required for the diagnosis. Domains that may be impaired include memory (most commonly impaired), language, ], ] functioning, or other areas of cognition. The neurocognitive changes must be a decline from a prior level of function and the diagnosis requires ruling out other common causes of neurocognitive decline.<ref name="Arvanitakis 2019" /><ref name=pmid17407994>{{cite journal | vauthors = Mendez MF | title = The accurate diagnosis of early-onset dementia | journal = International Journal of Psychiatry in Medicine | volume = 36 | issue = 4 | pages = 401–412 | year = 2006 | pmid = 17407994 | doi = 10.2190/Q6J4-R143-P630-KW41 | s2cid = 43715976 | url = https://zenodo.org/record/1236421 | access-date = 25 May 2020 | archive-date = 3 June 2020 | archive-url = https://web.archive.org/web/20200603200156/https://zenodo.org/record/1236421/ | url-status = live }}</ref><ref name=pmid17018549>{{cite journal | vauthors = Klafki HW, Staufenbiel M, Kornhuber J, Wiltfang J | title = Therapeutic approaches to Alzheimer's disease | journal = Brain | volume = 129 | issue = Pt 11 | pages = 2840–2855 | date = November 2006 | pmid = 17018549 | doi = 10.1093/brain/awl280 | doi-access = free | title-link = doi }}</ref> Advanced ] with ] (CT) or ] (MRI), and with ] (SPECT) or ] (PET), can be used to help exclude other cerebral pathology or subtypes of dementia.<ref>{{cite book |url=http://www.nice.org.uk/nicemedia/pdf/CG042quickrefguide.pdf |title=Dementia: Quick Reference Guide |publisher=(UK) ]|location=London|year=2006|isbn=978-1-84629-312-2|access-date=22 February 2008 |archive-url=https://web.archive.org/web/20080227161412/http://www.nice.org.uk/nicemedia/pdf/CG042quickrefguide.pdf|archive-date=27 February 2008|url-status=dead}}</ref> On MRI or CT, Alzheimer's disease usually shows a generalized or focal cortical atrophy, which may be asymmetric. Atrophy of the hippocampus is also commonly seen. Brain imaging commonly also shows cerebrovascular disease, most commonly previous strokes (small or large territory strokes), and this is thought to be a contributing cause of many cases of dementia (up to 46% cases of dementia also have cerebrovascular disease on imaging).<ref name="Arvanitakis 2019">{{cite journal |last1=Arvanitakis |first1=Zoe |last2=Shah |first2=Raj C. |last3=Bennett |first3=David A. |title=Diagnosis and Management of Dementia: Review |journal=JAMA |date=22 October 2019 |volume=322 |issue=16 |pages=1589–1599 |doi=10.1001/jama.2019.4782|pmid=31638686 |pmc=7462122 }}</ref> FDG-PET scan is not required for the diagnosis but it is sometimes used when standard testing is unclear. FDG-PET shows a bilateral, asymetric, temporal and parietal reduced activity.<ref name="Arvanitakis 2019" /> Advanced imaging may predict conversion from ] stages (mild cognitive impairment) to Alzheimer's disease.<ref name=Schroeter>{{cite journal | vauthors = Schroeter ML, Stein T, Maslowski N, Neumann J | title = Neural correlates of Alzheimer's disease and mild cognitive impairment: a systematic and quantitative meta-analysis involving 1351 patients | journal = NeuroImage | volume = 47 | issue = 4 | pages = 1196–1206 | date = October 2009 | pmid = 19463961 | pmc = 2730171 | doi = 10.1016/j.neuroimage.2009.05.037 }}</ref> FDA-approved ] diagnostic agents used in PET for Alzheimer's disease are ] (2012), ] (2013), ] (2014), and ] (2020).<ref name=pmid33573211>{{cite journal | vauthors = Jie CV, Treyer V, Schibli R, Mu L | title = Tauvid: The First FDA-Approved PET Tracer for Imaging Tau Pathology in Alzheimer's Disease | journal = Pharmaceuticals | volume = 14 | issue = 2 | date = January 2021 | page = 110 | pmid = 33573211 | pmc = 7911942 | doi = 10.3390/ph14020110 | doi-access = free | title-link = doi }}</ref> Because many insurance companies in the United States do not cover this procedure, its use in clinical practice is largely limited to clinical trials {{as of|2018|lc=y}}.<ref name=Weller2018 /> | |||
| ] including memory testing can further characterise the state of the disease.<ref name=Knopman2021 /> Medical organizations have created diagnostic criteria to ease and standardise the diagnostic process for practising physicians. Definitive diagnosis can only be confirmed with ] evaluations when brain material is available and can be examined ] for senile plaques and neurofibrillary tangles.<ref name=Weller2018 /><ref>{{cite journal | vauthors = Silva MV, Loures CM, Alves LC, de Souza LC, Borges KB, Carvalho MD | title = Alzheimer's disease: risk factors and potentially protective measures | journal = Journal of Biomedical Science | volume = 26 | issue = 1 | pages = 33 | date = May 2019 | pmid = 31072403 | pmc = 6507104 | doi = 10.1186/s12929-019-0524-y | doi-access = free }}</ref> | |||
| ===Criteria=== | |||
| There are three sets of criteria for the clinical diagnoses of the spectrum of Alzheimer's disease: the 2013 fifth edition of the '']'' (]); the ]-] (NIA-AA) definition as revised in 2011; and the International Working Group criteria as revised in 2010.<ref name=Atri2019>{{cite journal | vauthors = Atri A | title = The Alzheimer's Disease Clinical Spectrum: Diagnosis and Management | journal = The Medical Clinics of North America | volume = 103 | issue = 2 | pages = 263–293 | date = March 2019 | pmid = 30704681 | doi = 10.1016/j.mcna.2018.10.009 | s2cid = 73432842 | type = Review | doi-access = free }}</ref><ref name=Weller2018>{{cite journal | vauthors = Weller J, Budson A | title = Current understanding of Alzheimer's disease diagnosis and treatment | journal = F1000Research | volume = 7 | date = 2018 | page = 1161 | pmid = 30135715 | pmc = 6073093 | doi = 10.12688/f1000research.14506.1 | type = Review | doi-access = free }}</ref> | |||
| Eight intellectual domains are most commonly impaired in AD—], ], ], ], ]s, ], ] and ]al abilities, as listed in the fourth text revision of the DSM (DSM-IV-TR).<ref>{{cite book |title=Diagnostic and statistical manual of mental disorders: DSM-IV-TR |edition=4th Text Revision|publisher=American Psychiatric Association|year=2000|location=Washington, DC|isbn=978-0-89042-025-6}}</ref> | |||
| The ] defines criteria for probable or possible AD for both major and mild neurocognitive disorder.<ref name=APA611>{{cite book|publisher=American Psychiatric Association|title=Diagnostic and statistical manual of mental disorders: DSM-5|year=2013|isbn=978-0-89042-555-8|location=Washington, D.C.|page=611}}</ref><ref>{{cite journal | vauthors = Sachs-Ericsson N, Blazer DG | title = The new DSM-5 diagnosis of mild neurocognitive disorder and its relation to research in mild cognitive impairment | journal = Aging & Mental Health | volume = 19 | issue = 1 | pages = 2–12 | date = January 2015 | pmid = 24914889 | doi = 10.1080/13607863.2014.920303 | s2cid = 46244321 }}</ref><ref name=Sachdev2014>{{cite journal | vauthors = Sachdev PS, Blacker D, Blazer DG, Ganguli M, Jeste DV, Paulsen JS, Petersen RC | title = Classifying neurocognitive disorders: the DSM-5 approach | journal = Nature Reviews. Neurology | volume = 10 | issue = 11 | pages = 634–642 | date = November 2014 | pmid = 25266297 | doi = 10.1038/nrneurol.2014.181 | s2cid = 20635070 | url = https://escholarship.org/uc/item/77g8t63q | access-date = 27 November 2021 | archive-date = 20 March 2022 | archive-url = https://web.archive.org/web/20220320083424/https://escholarship.org/uc/item/77g8t63q | url-status = live }}</ref> Major or mild neurocognitive disorder must be present along with at least one cognitive deficit for a diagnosis of either probable or possible AD.<ref name=APA611 /><ref>{{cite journal | vauthors = Stokin GB, Krell-Roesch J, Petersen RC, Geda YE | title = Mild Neurocognitive Disorder: An Old Wine in a New Bottle | journal = Harvard Review of Psychiatry | volume = 23 | issue = 5 | pages = 368–376 | date = 2015 | pmid = 26332219 | pmc = 4894762 | doi = 10.1097/HRP.0000000000000084 | type = Review }}</ref> For major neurocognitive disorder due to AD, probable Alzheimer's disease can be diagnosed if the individual has genetic evidence of AD<ref>{{cite book|url=https://www.taylorfrancis.com/books/edit/10.4324/9780203772287/psychopathology-psychotherapy-len-sperry-jon-carlson-jill-duba-sauerheber-jon-sperry|title=Psychopathology and Psychotherapy: DSM-5 Diagnosis, Case Conceptualization, and Treatment|journal=Taylor & Francis |year=2014|publisher=Routledge|isbn=978-0-203-77228-7|veditors=Sperry L, Carlson J, Sauerheber J, Sperry J|edition=3|location=New York|pages=342–343|doi=10.4324/9780203772287|access-date=16 November 2021|archive-date=16 November 2021|archive-url=https://web.archive.org/web/20211116213230/https://www.taylorfrancis.com/books/edit/10.4324/9780203772287/psychopathology-psychotherapy-len-sperry-jon-carlson-jill-duba-sauerheber-jon-sperry|url-status=live}}</ref> or if two or more acquired cognitive deficits, and a functional disability that is not from another disorder, are present.<ref>{{cite book|vauthors = Fink HA, Hemmy LS, Linskens EJ, Silverman PC, MacDonald R, McCarten JR, Talley KM, Desai PJ, Forte ML, Miller MA, Brasure M, Nelson VA, Taylor BC, Ng W, Ouellette JM, Greer NL, Sheets KM, Wilt TJ, Butler M |url=http://www.ncbi.nlm.nih.gov/books/NBK556556/|title=Diagnosis and Treatment of Clinical Alzheimer's-Type Dementia: A Systematic Review|date=2020|publisher=Agency for Healthcare Research and Quality (US)|series=AHRQ Comparative Effectiveness Reviews|location=Rockville (MD)|pmid=32369312|access-date=16 November 2021|archive-date=7 July 2023|archive-url=https://web.archive.org/web/20230707063441/https://www.ncbi.nlm.nih.gov/books/NBK556556/|url-status=live }}</ref> Otherwise, possible AD can be diagnosed as the diagnosis follows an atypical route.<ref>{{cite journal | vauthors = Stokin GB, Krell-Roesch J, Petersen RC, Geda YE | title = Mild Neurocognitive Disorder: An Old Wine in a New Bottle | journal = Harvard Review of Psychiatry | volume = 23 | issue = 5 | pages = 368–376 | date = September 2015 | pmid = 26332219 | pmc = 4894762 | doi = 10.1097/HRP.0000000000000084 | publisher = Wolters Kluwer Health }}</ref> For mild neurocognitive disorder due to AD, probable Alzheimer's disease can be diagnosed if there is genetic evidence, whereas possible AD can be met if all of the following are present: no genetic evidence, decline in both learning and memory, two or more cognitive deficits, and a functional disability not from another disorder.<ref name=APA611 /><ref>{{cite journal | vauthors = Bradfield NI, Ames D | title = Mild cognitive impairment: narrative review of taxonomies and systematic review of their prediction of incident Alzheimer's disease dementia | journal = BJPsych Bulletin | volume = 44 | issue = 2 | pages = 67–74 | date = April 2020 | pmid = 31724527 | pmc = 7283119 | doi = 10.1192/bjb.2019.77 | type = Review }}</ref> | |||
| The NIA-AA criteria are used mainly in research rather than in clinical assessments.<ref name=Vega2014>{{cite journal | vauthors = Vega JN, Newhouse PA | title = Mild cognitive impairment: diagnosis, longitudinal course, and emerging treatments | journal = Current Psychiatry Reports | volume = 16 | issue = 10 | pages = 490 | date = October 2014 | pmid = 25160795 | pmc = 4169219 | doi = 10.1007/s11920-014-0490-8 | publisher = SpringerLink }}</ref> They define AD through three major stages: preclinical, mild cognitive impairment (MCI), and Alzheimer's dementia.<ref>{{cite journal | vauthors = Parnetti L, Chipi E, Salvadori N, D'Andrea K, Eusebi P | title = Prevalence and risk of progression of preclinical Alzheimer's disease stages: a systematic review and meta-analysis | journal = Alzheimer's Research & Therapy | volume = 11 | issue = 1 | pages = 7 | date = January 2019 | pmid = 30646955 | pmc = 6334406 | doi = 10.1186/s13195-018-0459-7 | publisher = Springer Nature | doi-access = free }}</ref><ref name=Jack2018>{{cite journal | vauthors = Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, Holtzman DM, Jagust W, Jessen F, Karlawish J, Liu E, Molinuevo JL, Montine T, Phelps C, Rankin KP, Rowe CC, Scheltens P, Siemers E, Snyder HM, Sperling R | title = NIA-AA Research Framework: Toward a biological definition of Alzheimer's disease | journal = Alzheimer's & Dementia | volume = 14 | issue = 4 | pages = 535–562 | date = April 2018 | pmid = 29653606 | pmc = 5958625 | doi = 10.1016/j.jalz.2018.02.018 }}</ref> Diagnosis in the preclinical stage is complex and focuses on asymptomatic individuals;<ref name=Jack2018 /><ref>{{cite journal | vauthors = Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, Iwatsubo T, Jack CR, Kaye J, Montine TJ, Park DC, Reiman EM, Rowe CC, Siemers E, Stern Y, Yaffe K, Carrillo MC, Thies B, Morrison-Bogorad M, Wagster MV, Phelps CH | title = Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease | journal = Alzheimer's & Dementia | volume = 7 | issue = 3 | pages = 280–292 | date = May 2011 | pmid = 21514248 | pmc = 3220946 | doi = 10.1016/j.jalz.2011.03.003 }}</ref> the latter two stages describe individuals experiencing symptoms,<ref name=Jack2018 /> along with biomarkers,<ref>{{cite journal | vauthors = Cheng YW, Chen TF, Chiu MJ | title = From mild cognitive impairment to subjective cognitive decline: conceptual and methodological evolution | journal = Neuropsychiatric Disease and Treatment | volume = 13 | pages = 491–498 | date = 16 February 2017 | pmid = 28243102 | pmc = 5317337 | doi = 10.2147/NDT.S123428 | publisher = Dove Medical Press Limited | doi-access = free }}</ref> predominantly those for neuronal injury (mainly tau-related) and amyloid beta deposition.<ref name=Vega2014 /><ref name=Jack2018 /> The core clinical criteria itself rests on the presence of cognitive impairment<ref name=Jack2018 /> without the presence of comorbidities.<ref>{{cite journal | vauthors = Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, Snyder PJ, Carrillo MC, Thies B, Phelps CH | title = The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease | journal = Alzheimer's & Dementia | volume = 7 | issue = 3 | pages = 270–279 | date = May 2011 | pmid = 21514249 | pmc = 3312027 | doi = 10.1016/j.jalz.2011.03.008 }}</ref><ref name=Chertkow2013 /> The third stage is divided into probable and possible AD dementia.<ref name=Chertkow2013>{{cite journal | vauthors = Chertkow H, Feldman HH, Jacova C, Massoud F | title = Definitions of dementia and predementia states in Alzheimer's disease and vascular cognitive impairment: consensus from the Canadian conference on diagnosis of dementia | journal = Alzheimer's Research & Therapy | volume = 5 | issue = Suppl 1 | pages = S2 | date = July 2013 | pmid = 24565215 | pmc = 3981054 | doi = 10.1186/alzrt198 | publisher = BMC | doi-access = free }}</ref> In probable AD dementia there is steady impairment of cognition over time and a memory-related or non-memory-related cognitive dysfunction.<ref name=Chertkow2013 /> In possible AD dementia, another causal disease such as ] is present.<ref name=Chertkow2013 /> | |||
| ===Techniques=== | |||
| ]s such as the mini–mental state examination (MMSE) can help in the diagnosis of Alzheimer's disease. In this test instructions are given to copy drawings like the one shown, remember some words, read, and subtract numbers serially.]] | |||
| ]s including ]s such as the ] (MMSE), the ] (MoCA) and the Mini-Cog are widely used to aid in diagnosis of the cognitive impairments in AD.<ref name=Papadakis2021p1760>{{cite book|title=Current medical diagnosis & treatment |date=2021|vauthors=Papadakis MA, McPhee SJ, Rabow MW|isbn=978-1-260-46986-8|edition=Sixtieth |publisher= McGraw Hill|location=New York|page=1760|oclc=1195972209}}</ref> These tests may not always be accurate, as they lack sensitivity to mild cognitive impairment, and can be biased by language or attention problems;<ref name=Papadakis2021p1760 /> more comprehensive test arrays are necessary for high reliability of results, particularly in the earliest stages of the disease.<ref name=pmid1512391>{{cite journal | vauthors = Tombaugh TN, McIntyre NJ | title = The mini-mental state examination: a comprehensive review | journal = Journal of the American Geriatrics Society | volume = 40 | issue = 9 | pages = 922–935 | date = September 1992 | pmid = 1512391 | doi = 10.1111/j.1532-5415.1992.tb01992.x | s2cid = 25169596 }}</ref><ref name=pmid9987708>{{cite journal | vauthors = Pasquier F | title = Early diagnosis of dementia: neuropsychology | journal = Journal of Neurology | volume = 246 | issue = 1 | pages = 6–15 | date = January 1999 | pmid = 9987708 | doi = 10.1007/s004150050299 | s2cid = 2108587 }}</ref> | |||
| Further neurological examinations are crucial in the ] of Alzheimer's disease and other diseases.<ref name=Waldemar2007 /> Interviews with family members are used in assessment; caregivers can supply important information on daily living abilities and on the decrease in the person's ].<ref name=pmid16327345>{{cite journal | vauthors = Harvey PD, Moriarty PJ, Kleinman L, Coyne K, Sadowsky CH, Chen M, Mirski DF | title = The validation of a caregiver assessment of dementia: the Dementia Severity Scale | journal = Alzheimer Disease and Associated Disorders | volume = 19 | issue = 4 | pages = 186–194 | year = 2005 | pmid = 16327345 | doi = 10.1097/01.wad.0000189034.43203.60 | s2cid = 20238911 }}</ref> A caregiver's viewpoint is particularly important, since a person with Alzheimer's disease is commonly ].<ref name=pmid15738860>{{cite journal | vauthors = Antoine C, Antoine P, Guermonprez P, Frigard B | title = | language = fr | journal = L'Encéphale | volume = 30 | issue = 6 | pages = 570–577 | year = 2004 | pmid = 15738860 | doi = 10.1016/S0013-7006(04)95472-3 }}</ref> Many times, families have difficulties in the detection of initial dementia symptoms and may not communicate accurate information to a physician.<ref name=pmid16197855>{{cite journal | vauthors = Cruz VT, Pais J, Teixeira A, Nunes B | title = | language = pt | journal = Acta Médica Portuguesa | volume = 17 | issue = 6 | pages = 435–444 | year = 2004 | pmid = 16197855 }}</ref> | |||
| Supplemental testing can rule out other potentially treatable diagnoses and help avoid misdiagnoses.<ref name=Stern2020>{{cite book| vauthors = Stern SD, Cifu AS, Altkorn D |title=Symptom to diagnosis: an evidence-based guide|date=2020 |isbn=978-1-260-12111-7|edition=4th|location=New York | publisher = McGraw-Hill Medical |pages=209–210|oclc=1121597721}}</ref> Common supplemental tests include ]s, ], as well as tests to assess vitamin ] levels, rule out ] and rule out metabolic problems (including tests for ], electrolyte levels and for ]).<ref name=Stern2020 /> MRI or CT scans might also be used to rule out other potential causes of the symptoms – including tumors or strokes.<ref name=Papadakis2021p1760 /> ] and depression can be common among individuals and are important to rule out.<ref>{{cite book|vauthors= Jha A, Mukhopadhaya K|title=Alzheimer's disease: diagnosis and treatment guide|date=2021|isbn=978-3-030-56739-2|publisher= Springer|location=Cham, Switzerland|page=32|oclc=1202472277}}</ref> | |||
| ] for ] are used, since depression can either be concurrent with AD (see ]), an early sign of cognitive impairment,<ref>{{cite journal | vauthors = Sun X, Steffens DC, Au R, Folstein M, Summergrad P, Yee J, Rosenberg I, Mwamburi DM, Qiu WQ | title = Amyloid-associated depression: a prodromal depression of Alzheimer disease? | journal = Archives of General Psychiatry | volume = 65 | issue = 5 | pages = 542–550 | date = May 2008 | pmid = 18458206 | pmc = 3042807 | doi = 10.1001/archpsyc.65.5.542 }}</ref> or even the cause.<ref name=pmid9153154>{{cite journal | vauthors = Geldmacher DS, Whitehouse PJ | title = Differential diagnosis of Alzheimer's disease | journal = Neurology | volume = 48 | issue = 5 Suppl 6 | pages = S2–S9 | date = May 1997 | pmid = 9153154 | doi = 10.1212/WNL.48.5_Suppl_6.2S | s2cid = 30018544 }}</ref><ref name=pmid17495754>{{cite journal | vauthors = Potter GG, Steffens DC | title = Contribution of depression to cognitive impairment and dementia in older adults | journal = The Neurologist | volume = 13 | issue = 3 | pages = 105–117 | date = May 2007 | pmid = 17495754 | doi = 10.1097/01.nrl.0000252947.15389.a9 | s2cid = 24569198 }}</ref> | |||
| ==Epidemiology== | |||
| Due to low accuracy, the C-PIB-PET scan is not recommended as an early diagnostic tool or for predicting the development of AD when people show signs of mild cognitive impairment (MCI).<ref>{{cite journal | vauthors = Zhang S, Smailagic N, Hyde C, Noel-Storr AH, Takwoingi Y, McShane R, Feng J | title = (11)C-PIB-PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI) | journal = The Cochrane Database of Systematic Reviews | issue = 7 | pages = CD010386 | date = July 2014 | volume = 2014 | pmid = 25052054 | pmc = 6464750 | doi = 10.1002/14651858.CD010386.pub2 }}</ref> The use of <sup>18</sup>F-FDG PET scans, as a single test, to identify people who may develop Alzheimer's disease is not supported by evidence.<ref>{{cite journal | vauthors = Smailagic N, Vacante M, Hyde C, Martin S, Ukoumunne O, Sachpekidis C | title = <sup>18</sup>F-FDG PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI) | journal = The Cochrane Database of Systematic Reviews | volume = 1 | pages = CD010632 | date = January 2015 | issue = 1 | pmid = 25629415 | pmc = 7081123 | doi = 10.1002/14651858.CD010632.pub2 }}</ref> | |||
| ==Prevention== | ==Prevention== | ||
| ] or regular social interaction have been linked to a reduced risk of Alzheimer's disease in epidemiological studies, although no causal relationship has been found.]] | |||
| Aging itself cannot be prevented, but the ] of it can be mitigated. However, the evidence relating certain behaviors, dietary intakes, environmental exposures, and diseases to the likelihood of developing Alzheimer's varies in quality and its acceptance by the medical community.<ref>{{cite journal | last = Small | first = Gary W | title = What we need to know about age related memory loss | journal = British Medical Journal | pages = 1502-1507 | date = ] | url = http://bmj.bmjjournals.com/cgi/content/full/324/7352/1502#B21 | accessdate = 2006-11-05}}</ref> It is important to understand that interventions that reduce the risk of developing disease in the first place may not alter disease progression after symptoms become apparent. Due to their observational ], studies examining disease risk factors are often at risk from ]s. Several recent large, ]s—in particular the ]—have called into question preventive measures based on ]. Some proposed preventive measures are even based on studies conducted solely in animals or in cell cultures but are not listed here. | |||
| There are no ]s available to cure Alzheimer's disease and because of this, AD research has focused on interventions to prevent the onset and progression.<ref>{{cite journal | vauthors = Viña J, Sanz-Ros J | title = Alzheimer's disease: Only prevention makes sense | journal = European Journal of Clinical Investigation | volume = 48 | issue = 10 | pages = e13005 | date = October 2018 | pmid = 30028503 | doi = 10.1111/eci.13005 | s2cid = 51703879 | doi-access = free }}</ref> There is no evidence that supports any particular measure in preventing AD,<ref name=Knopman2021 /> and studies of measures to prevent the onset or progression have produced inconsistent results. Epidemiological studies have proposed relationships between an individual's likelihood of developing AD and modifiable factors, such as medications, lifestyle, and diet. There are some challenges in determining whether interventions for AD act as a primary prevention method, preventing the disease itself, or a secondary prevention method, identifying the early stages of the disease.<ref name=Hsu2017>{{cite journal |vauthors=Hsu D, Marshall GA |title=Primary and secondary prevention trials in Alzheimer disease: looking back, moving forward |journal=Curr Alzheimer Res |volume=14 |issue=4 |pages=426–440 |date=2017 |pmid=27697063 |pmc=5329133 |doi=10.2174/1567205013666160930112125 }}</ref> These challenges include duration of intervention, different stages of disease at which intervention begins, and lack of standardization of inclusion criteria regarding biomarkers specific for AD.<ref name=Hsu2017 /> Further research is needed to determine factors that can help prevent AD.<ref name=Hsu2017 /> | |||
| Adults with damaged blood vessels in the brain or atrophy in their ] are more likely to develop Alzheimer's disease. It is known that blood vessel damage in the brain is more likely to occur in patients with high blood pressure, high cholesterol or diabetes. Therefore, prevention of these conditions can lower risk of developing Alzheimer's, as well as ] and ]. | |||
| === |
===Medication=== | ||
| Cardiovascular risk factors, such as ], ], ], and ], are associated with a higher risk of onset and worsened course of AD.<ref name=pmid18299540>{{cite journal | vauthors = Patterson C, Feightner JW, Garcia A, Hsiung GY, MacKnight C, Sadovnick AD | title = Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease | journal = CMAJ | volume = 178 | issue = 5 | pages = 548–556 | date = February 2008 | pmid = 18299540 | pmc = 2244657 | doi = 10.1503/cmaj.070796 }}</ref><ref name=pmid17483665>{{cite journal | vauthors = Rosendorff C, Beeri MS, Silverman JM | title = Cardiovascular risk factors for Alzheimer's disease | journal = The American Journal of Geriatric Cardiology | volume = 16 | issue = 3 | pages = 143–149 | year = 2007 | pmid = 17483665 | doi = 10.1111/j.1076-7460.2007.06696.x }}</ref> The use of ]s to lower ] may be of benefit in AD.<ref name=Chu>{{cite journal | vauthors = Chu CS, Tseng PT, Stubbs B, Chen TY, Tang CH, Li DJ, Yang WC, Chen YW, Wu CK, Veronese N, Carvalho AF, Fernandes BS, Herrmann N, Lin PY | title = Use of statins and the risk of dementia and mild cognitive impairment: A systematic review and meta-analysis | journal = Scientific Reports | volume = 8 | issue = 1 | pages = 5804 | date = April 2018 | pmid = 29643479 | pmc = 5895617 | doi = 10.1038/s41598-018-24248-8 | bibcode = 2018NatSR...8.5804C }}</ref> ] and ] medications in individuals without overt cognitive impairment may decrease the risk of dementia by influencing cerebrovascular ].<ref name=Knopman2021 /><ref>{{cite journal |vauthors = Ungvari Z, Toth P, Tarantini S, Prodan CI, Sorond F, Merkely B, Csiszar A |title=Hypertension-induced cognitive impairment: from pathophysiology to public health |journal=Nature Reviews Nephrology |volume=17 |issue=10 |pages=639–654 |date=October 2021 |pmid=34127835 |pmc=8202227 |doi=10.1038/s41581-021-00430-6 }}</ref> More research is needed to examine the relationship with AD specifically; clarification of the direct role medications play versus other concurrent lifestyle changes (diet, exercise, smoking) is needed.<ref name=Knopman2021 /> | |||
| *Intellectual stimulation (e.g., playing ] or doing ])<ref> {{cite journal | author = Verghese J, Lipton R, Katz M, Hall C, Derby C, Kuslansky G, Ambrose A, Sliwinski M, Buschke H | title = Leisure activities and the risk of dementia in the elderly. | journal = N Engl J Med | volume = 348 | issue = 25 | pages = 2508-16 | year = 2003 | id = PMID 12815136}} </ref> | |||
| *Regular physical exercise<ref>{{cite journal | author = Larson E, Wang L, Bowen J, McCormick W, Teri L, Crane P, Kukull W | title = Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. | journal = Ann Intern Med | volume = 144 | issue = 2 | pages = 73-81 | year = 2006 | id = PMID 16418406}}</ref> | |||
| *Regular social interaction . Lonely individuals may be twice as likely to develop the type of dementia linked to Alzheimer’s disease in late life as those who are not lonely. | |||
| *A ] with fruits and vegetables and low in saturated fat,<ref> {{cite journal | author = Scarmeas N, Stern Y, Mayeux R, Luchsinger J | title = Mediterranean diet, Alzheimer disease, and vascular mediation. | journal = Arch Neurol | volume = 63 | issue = 12 | pages = 1709-17 | year = 2006 | id = PMID 17030648}} </ref> supplemented in particular with: | |||
| **]<ref> {{cite journal | author = Morris M, Schneider J, Tangney C | title = Thoughts on B-vitamins and dementia. | journal = J Alzheimers Dis | volume = 9 | issue = 4 | pages = 429-33 | year = 2006 | id = PMID 16917152}}</ref> in particular, ].<ref> {{cite journal | author = Inna I. Kruman1, T. S. Kumaravel2, Althaf Lohani2, Ward A. Pedersen1, Roy G. Cutler1, Yuri Kruman1, Norman Haughey1, Jaewon Lee1, Michele Evans2, and Mark P. Mattson1, 3 | title = Folic Acid Deficiency and Homocysteine Impair DNA Repair in Hippocampal Neurons and Sensitize Them to Amyloid Toxicity in Experimental Models of Alzheimer's Disease . | journal = The Journal of Neuroscience, | volume = 22 | issue = 5 | year = March 1, 2002 | website = http://www.jneurosci.org/cgi/content/abstract/22/5/1752?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&author1=Kruman&titleabstract=folic%2Bacid&searchid=1056979885583_2657&stored_search=&FIRSTINDEX=0&journalcode=jneuro}} A simplified report can be found at: </ref><ref>CBS news, reporting from WebMD </ref><ref></ref><ref>Alzheimer's and Dementia journal, reported at USA today</ref> | |||
| **] in ] (from the yellow spice ])<ref> {{cite journal | author = Giselle P. Lim1, Teresa Chu1, Fusheng Yang, Walter Beech1, Sally A. Frautschy1, and Greg M. Cole1 | title = The Curry Spice Curcumin Reduces Oxidative Damage and Amyloid Pathology in an Alzheimer Transgenic Mouse | journal = The Journal of Neuroscience | volume = 21 | issue = 4 | pages = 8370-8377 | |||
| | year = 2001 | id = PMID 11606625}}</ref> | |||
| **], especially ] (DHA, often found in fish oil)<ref>{{cite journal | author = Lim W, Gammack J, Van Niekerk J, Dangour A | title = Omega 3 fatty acid for the prevention of dementia. | journal = Cochrane Database Syst Rev | volume = | issue = | pages = CD005379 | year = | id = PMID 16437528}}</ref><ref>{{cite journal | author = Morris M, Evans D, Tangney C, Bienias J, Wilson R | title = Fish consumption and cognitive decline with age in a large community study. | journal = Arch Neurol | volume = 62 | issue = 12 | pages = 1849-53 | year = 2005 | id = PMID 16216930}} </ref> | |||
| **Fresh fruit and vegetables high in the ] (berries, apples, grapes, brocolli, ] like kidney beans, etc)<ref> {{cite journal | author = Dai Q, Borenstein A, Wu Y, Jackson J, Larson E | title = Fruit and vegetable juices and Alzheimer's disease: the Kame Project. | journal = Am J Med | volume = 119 | issue = 9 | pages = 751-9 | year = 2006 | id = PMID 16945610}}</ref><ref>{{cite journal | author = Joseph J, Fisher D, Carey A | title = Fruit extracts antagonize Abeta- or DA-induced deficits in Ca2+ flux in M1-transfected COS-7 cells. | journal = J Alzheimers Dis | volume = 6 | issue = 4 | pages = 403-11; discussion 443-9 | year = 2004 | id = PMID 15345811}} </ref> | |||
| **]. High doses (up to 2000IU, especially in combination with ] to aid absorption) have been shown to reduce Alzheimer's risk in cross sectional studies, but not in a randomized trial<ref>{{cite journal | author = Petersen R, Thomas R, Grundman M, Bennett D, Doody R, Ferris S, Galasko D, Jin S, Kaye J, Levey A, Pfeiffer E, Sano M, van Dyck C, Thal L | title = Vitamin E and donepezil for the treatment of mild cognitive impairment. | journal = N Engl J Med | volume = 352 | issue = 23 | pages = 2379-88 | year = 2005 | id = PMID 15829527}}</ref><ref>{{cite journal | author = Zandi P, Anthony J, Khachaturian A, Stone S, Gustafson D, Tschanz J, Norton M, Welsh-Bohmer K, Breitner J | title = Reduced risk of Alzheimer disease in users of antioxidant vitamin supplements: the Cache County Study. | journal = Arch Neurol | volume = 61 | issue = 1 | pages = 82-8 | year = 2004 | id = PMID 14732624}} </ref>. Vitamin E is routinely recommended by family doctors to AD patients. Research has shown that a more 'full spectrum' Vitamin E with mixed tocopherols and tocotrienols can be more beneficial than just taking the commonly available d-alpha tocopherol. The cheaper synthetic version, dl-alpha tocopherol (note the l), is often regarded as less effective still. There has been a report that taking over 1000IU a day may lead to an increase risk of stroke. | |||
| **The moderate consumption of alcohol (beer, wine or distilled spirits) <ref> Scarmeas, N., et al. Mediterranean diet and risk for Alzheimer’s disease. Annals of Neurology, 2006 (published online April 18, 2006). Other research is consistent with the finding that moderate alcohol consumption is associated with lower risk of Alzheimer’s and other forms of dementia: Mulkamal, K.J., et al. Prospective study of alcohol consumption and risk of dementia in older adults. Journal of the American Medical Association, 2003 (March 19), 289, 1405-1413; Ganguli, M., et al. Alcohol consumption and cognitive function in late life: A longitudinal community study. Neurology, 2005, 65, 1210-12-17; Huang, W., et al. Alcohol consumption and incidence of dementia in a community sample aged 75 years and older. Journal of Clinical Epidemiology, 2002, 55(10), 959-964; Rodgers, B., et al. Non-linear relationships between cognitive function and alcohol consumption in young, middle-aged and older adults: The PATH Through Life Project. Addiction, 2005, 100(9), 1280-1290; Anstey, K. J., et al. Lower cognitive test scores observed in alcohol are associated with demographic, personality, and biological factors: The PATH Through Life Project. Addiction, 2005, 100(9), 1291-1301; Espeland, M., et al. Association between alcohol intake and domain-specific cognitive function in older women. Neuroepidemiology, 2006, 1(27), 1-12; Stampfer, M.J., et al. Effects of moderate alcohol consumption on cognitive function in women. New England Journal of Medicine, 2005, 352, 245-253; Ruitenberg, A., et al. Alcohol consumption and risk of dementia: the Rotterdam Study. Lancet, 2002, 359(9303), 281-286.</ref> | |||
| *]-lowering drugs (]) reduce Alzheimer's risk in observational studies but so far not in randomized controlled trials<ref>{{cite journal | author = Rockwood K | title = Epidemiological and clinical trials evidence about a preventive role for statins in Alzheimer's disease. | journal = Acta Neurol Scand Suppl | volume = 185 | issue = | pages = 71-7 | year = | id = PMID 16866914}}</ref> | |||
| *Female ] is no longer thought to prevent dementia based on data from the ] | |||
| *Long-term usage of non-steroidal anti-inflammatory drugs (NSAIDs), used to reduce joint inflammation and pain, are associated with a reduced likelihood of developing AD, according to some observational studies.<ref> {{cite journal |author=Zandi P, Anthony J, Hayden K, Mehta K, Mayer L, Breitner J |title=Reduced incidence of AD with NSAID but not H2 receptor antagonists: the Cache County Study |journal=Neurology |volume=59 |issue=6 |pages=880-6 |year=2002 |id=PMID 12297571}} </ref><ref> {{cite journal |author=in t' Veld B, Ruitenberg A, Hofman A, Launer L, van Duijn C, Stijnen T, Breteler M, Stricker B |title=Nonsteroidal antiinflammatory drugs and the risk of Alzheimer's disease |journal=N Engl J Med |volume=345 |issue=21 |pages=1515-21 |year=2001 |id=PMID 11794217}} </ref> The risks appear to outweigh the drugs' benefit as a method of ].<ref name="2006AAGP"> {{cite journal | author = Lyketsos C, Colenda C, Beck C, Blank K, Doraiswamy M, Kalunian D, Yaffe K | title = Position statement of the American Association for Geriatric Psychiatry (AAGP) regarding principles of care for patients with dementia resulting from Alzheimer disease. | journal = Am J Geriatr Psychiatry | volume = 14 | issue = 7 | pages = 561-72 | year = 2006 | id = PMID 16816009}} </ref> | |||
| Depression is associated with an increased risk for AD; management with antidepressant medications may provide a preventative measure.<ref name="Yu 1201–1209">{{cite journal |vauthors = Yu JT, Xu W, Tan CC, Andrieu S, Suckling J, Evangelou E, Pan A, Zhang C, Jia J, Feng L, Kua EH, Wang YJ, Wang HF, Tan MS, Li JQ, Hou XH, Wan Y, Tan L, Mok V, Tan L, Dong Q, Touchon J, Gauthier S, Aisen PS, Vellas B |title=Evidence-based prevention of Alzheimer's disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials |journal=Journal of Neurology, Neurosurgery, and Psychiatry |volume=91 |issue=11 |pages=1201–1209 |date= November 2020 |pmid=32690803 |pmc=7569385 |doi=10.1136/jnnp-2019-321913 }}</ref> | |||
| ===Risk factors=== | |||
| * ] | |||
| * ApoE epsilon 4 genotype (in some populations) | |||
| * ]<ref> {{cite journal |author=Mayeux R, Ottman R, Tang M, Noboa-Bauza L, Marder K, Gurland B, Stern Y |title=Genetic susceptibility and head injury as risk factors for Alzheimer's disease among community-dwelling elderly persons and their first-degree relatives |journal=Ann. Neurol. |volume=33 |issue=5 |pages=494-501 |year=1993 |pmid=8498827}} </ref> | |||
| * Poor cardiovascular health (including ],<ref>{{cite journal | author = Kofman OS, MacMillan VH | title = Diffuse Cerebral Atrophy. | journal = Applied Therapeutics | volume = 12 | issue = 4 | pages = 24-26 | year = 1970}}</ref> ],<ref> {{cite journal |author=Kehoe P, Wilcock G |title=Is inhibition of the renin-angiotensin system a new treatment option for Alzheimer's disease? |journal=Lancet neurology |volume=6 |issue=4 |pages=373-8 |year=2007 |pmid=17362841}}</ref> ]<ref> {{cite journal |author=Crisby M, Carlson L, Winblad B |title=Statins in the prevention and treatment of Alzheimer disease |journal=Alzheimer disease and associated disorders |volume=16 |issue=3 |pages=131-6 |year=2002 |pmid=12218642}}</ref> and ]s)<ref>BBC 4 June 2007</ref> | |||
| *]<ref>{{cite journal |author=Anstey KJ, von Sanden C, Salim A, O'kearney R |title=Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies |journal=Am. J. Epidemiol. |volume=166 |issue=4 |pages=367-78 |year=2007 |pmid=17573335 |doi=10.1093/aje/kwm116}}</ref> | |||
| Historically, long-term usage of ] (NSAIDs) were thought to be associated with a reduced likelihood of developing AD as it reduces inflammation, but NSAIDs do not appear to be useful as a treatment.<ref name=Weller2018 /> Additionally, because women have a higher incidence of AD than men, it was once thought that ] during ] was a risk factor, but there is a lack of evidence to show that ] decreases risk of cognitive decline.<ref>{{cite journal |vauthors=Lethaby A, Hogervorst E, Richards M, Yesufu A, Yaffe K |title=Hormone replacement therapy for cognitive function in postmenopausal women |journal=Cochrane Database Syst Rev |volume= 2008|issue=1 |pages=CD003122 |date=January 2008 |pmid=18254016 |pmc=6599876 |doi=10.1002/14651858.CD003122.pub2}}</ref> | |||
| ==Treatment== | |||
| There is currently no cure for Alzheimer's disease. Currently available medications offer relatively small symptomatic benefit for some patients but do not slow disease progression. It helps a little for the memory. The American Association for Geriatric Psychiatry published a consensus statement on Alzheimer's treatment in 2006.<ref name="2006AAGP"/> | |||
| ===Acetylcholinesterase inhibitors=== | |||
| ]s were thought to be important because there is a reduction in activity of the ] neurons. AChE-inhibitors reduce the rate at which ] (ACh) is broken down and hence increase the concentration of ACh in the brain (combatting the loss of ACh caused by the death of the cholinergin neurons). Acetylcholinesterase-inhibitors seemed to modestly moderate symptoms but do not alter the course of the underlying dementing process.<ref> Ortho-McNeil Neurologics, “Razadyne ER US Product Insert”, May 2006. </ref><ref name=”ProductInsert”> Novartis Pharmaceuticals Corporation “Exelon Product Insert” June 2006. </ref><ref> Eisai Inc, “Aricept and Aricept ODT Product Insert”, March 2005. </ref> | |||
| ===Lifestyle=== | |||
| Examples include: | |||
| {{Further|Neurobiological effects of physical exercise}} | |||
| * ] - no longer clinically used (formerly marketed as Cognex) | |||
| Certain lifestyle activities, such as physical and cognitive exercises, higher education and occupational attainment, cigarette smoking, stress, sleep, and the management of other comorbidities, including diabetes and hypertension, may affect the risk of developing AD.<ref name="Yu 1201–1209"/> | |||
| * ] - (marketed as Aricept) | |||
| * ] - (marketed as Razadyne in the U.S.A. Marketed as Reminyl or Nivalin in the rest of the world) | |||
| * ] - (marketed as Exelon) | |||
| Physical exercise is associated with a decreased rate of dementia,<ref name=Cheng2016>{{cite journal |vauthors=Cheng ST |date=September 2016 |title=Cognitive Reserve and the Prevention of Dementia: the Role of Physical and Cognitive Activities |journal=Current Psychiatry Reports |type=Review |volume=18 |issue=9 |pages=85 |doi=10.1007/s11920-016-0721-2 |pmc=4969323 |pmid=27481112}}</ref> and is effective in reducing symptom severity in those with AD.<ref name=Farina2014>{{cite journal |vauthors=Farina N, Rusted J, Tabet N |date=January 2014 |title=The effect of exercise interventions on cognitive outcome in Alzheimer's disease: a systematic review |journal=International Psychogeriatrics |type=Review |volume=26 |issue=1 |pages=9–18 |doi=10.1017/S1041610213001385 |pmid=23962667 |s2cid=24936334}}</ref> Memory and cognitive functions can be improved with aerobic exercises including brisk walking three times weekly for forty minutes.<ref name=Bernard2014>{{cite journal |vauthors = Barnard ND, Bush AI, Ceccarelli A, Cooper J, de Jager CA, Erickson KI, Fraser G, Kesler S, Levin SM, Lucey B, Morris MC, Squitti R |date=September 2014 |title=Dietary and lifestyle guidelines for the prevention of Alzheimer's disease |journal=Neurobiology of Aging |volume=35 |issue= Suppl 2|pages=S74–S78 |doi=10.1016/j.neurobiolaging.2014.03.033 |pmid=24913896 |s2cid=8265377|doi-access=free | title-link = doi |hdl=11343/52774 |hdl-access=free }}</ref> It may also induce ] of the brain.<ref name=Bhatti20192>{{cite journal |vauthors=Bhatti GK, Reddy AP, Reddy PH, Bhatti JS |date=2019 |title=Lifestyle Modifications and Nutritional Interventions in Aging-Associated Cognitive Decline and Alzheimer's Disease |journal=Frontiers in Aging Neuroscience |type=Review |volume=11 |pages=369 |doi=10.3389/fnagi.2019.00369 |pmc=6966236 |pmid=31998117 |doi-access=free |title-link=doi}}</ref> Participating in mental exercises, such as reading, crossword puzzles, and chess have shown potential to be preventive.<ref name="Yu 1201–1209"/> Meeting the ] recommendations for physical activity is associated with a lower risk of AD.<ref>{{cite journal | vauthors = López-Ortiz S, Lista S, Valenzuela PL, Pinto-Fraga J, Carmona R, Caraci F, Caruso G, Toschi N, Emanuele E, Gabelle A, Nisticò R, Garaci F, Lucia A, Santos-Lozano A | title = Effects of physical activity and exercise interventions on Alzheimer's disease: an umbrella review of existing meta-analyses | journal = Journal of Neurology | date = November 2022 | volume = 270 | issue = 2 | pages = 711–725 | pmid = 36342524 | doi = 10.1007/s00415-022-11454-8 | s2cid = 253382289 }}</ref> | |||
| The three currently marketed products each comes in an oral form taken once or twice a day. Rivastigmine is also available as a once-daily ]. | |||
| Higher education and occupational attainment, and participation in leisure activities, contribute to a reduced risk of developing AD,<ref name=Vina2018>{{cite journal |vauthors=Viña J, Sanz-Ros J |date=October 2018 |title=Alzheimer's disease: Only prevention makes sense |journal=European Journal of Clinical Investigation |type=Review |volume=48 |issue=10 |pages=e13005 |doi=10.1111/eci.13005 |pmid=30028503 |s2cid=51703879|doi-access=free }}</ref> or of delaying the onset of symptoms. This is compatible with the ] theory, which states that some life experiences result in more efficient neural functioning providing the individual a cognitive reserve that delays the onset of dementia manifestations.<ref name=Vina2018 /> ] delays the onset of Alzheimer's disease syndrome without changing the duration of the disease.<ref name=Imtiaz2014>{{cite journal |vauthors=Imtiaz B, Tolppanen AM, Kivipelto M, Soininen H |date=April 2014 |title=Future directions in Alzheimer's disease from risk factors to prevention |journal=Biochemical Pharmacology |type=Review |volume=88 |issue=4 |pages=661–670 |doi=10.1016/j.bcp.2014.01.003 |pmid=24418410}}</ref> | |||
| There is some question as to the effectiveness of cholinesterase inhibitors. A number of recent articles have criticized the design of studies reporting benefit from these drugs, concluding that they have doubtful clinical utility, are costly, and confer many side effects.<ref>{{cite journal | author = Courtney C, '''Farrell D''', Gray R, Hills R, Lynch L, Sellwood E, Edwards S, Hardyman W, Raftery J, Crome P, Lendon C, Shaw H, Bentham P | title = Long-term donepezil treatment in 565 patients with Alzheimer's disease (AD2000): randomised double-blind trial. | journal = Lancet | volume = 363 | issue = 9427 | pages = 2105-15 | year = 2004 | id = PMID 15220031}}</ref><ref> {{cite journal | author = Kaduszkiewicz H, Zimmermann T, Beck-Bornholdt H, van den Bussche H | title = Cholinesterase inhibitors for patients with Alzheimer's disease: systematic review of randomised clinical trials. | journal = BMJ | volume = 331 | issue = 7512 | pages = 321-7 | year = 2005 | id = PMID 16081444}} </ref> The pharmaceutical companies, but also some independent clinicians, dispute the conclusions of these articles. | |||
| Cessation in smoking may reduce risk of developing AD, specifically in those who carry the ] allele.<ref>{{cite journal |vauthors=Imtiaz B, Tolppanen AM, Kivipelto M, Soininen H |title=Future directions in Alzheimer's disease from risk factors to prevention |journal=Biochem Pharmacol |volume=88 |issue=4 |pages=661–70 |date=April 2014 |pmid=24418410 |doi=10.1016/j.bcp.2014.01.003}}</ref><ref name="Yu 1201–1209"/> The increased oxidative stress caused by smoking results in downstream inflammatory or neurodegenerative processes that may increase risk of developing AD.<ref>{{cite journal |vauthors=Kivipelto M, Mangialasche F, Ngandu T |title=Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease |journal=Nat Rev Neurol |volume=14 |issue=11 |pages=653–666 |date=November 2018 |pmid=30291317 |doi=10.1038/s41582-018-0070-3 |s2cid=52925352 }}</ref> Avoidance of smoking, counseling and pharmacotherapies to quit smoking are used, and avoidance of environmental tobacco smoke is recommended.<ref name="Yu 1201–1209"/> | |||
| ===Ginkgo biloba=== | |||
| ] in ], a ] (]) movie about a man affected by Alzheimers]] | |||
| Examining over 52 studies conducted on ] for the treatment of "cognitive impairment and dementia," a Cochrane Review concludes that "there is promising evidence of improvement in cognition and function associated with Ginkgo." According to this review, the two randomized controlled studies that focused on Alzheimer's patients both showed significant improvement in these areas. <ref name="alzheim"> {{cite journal| author = Birks J, Grimley E, Van Dongen M | title = Ginkgo biloba for cognitive impairment and dementia. | journal = Cochrane Database Syst Rev | volume = | issue = | pages = CD003120 | year = | id = PMID 12519586}}.</ref> The AAGP review<ref name="2006AAGP"/> did not recommend Ginkgo, nor did it warn against its use. A large, randomized clinical study in the US called the GEM study is now underway (fully enrolled), which examines the effect (or effects) of Ginkgo to prevent dementia. Results are expected in late 2007 or early 2008. <ref> {{cite journal | author = DeKosky S, Fitzpatrick A, Ives D, Saxton J, Williamson J, Lopez O, Burke G, Fried L, Kuller L, Robbins J, Tracy R, Woolard N, Dunn L, Kronmal R, Nahin R, Furberg C | title = The Ginkgo Evaluation of Memory (GEM) study: design and baseline data of a randomized trial of Ginkgo biloba extract in prevention of dementia. | journal = Contemp Clin Trials | volume = 27 | issue = 3 | pages = 238-53 | year = 2006 | id = PMID 16627007}}.</ref> | |||
| Alzheimer's disease is associated with ] but the precise relationship is unclear.<ref name=Borges2019>{{cite journal |vauthors=Borges CR, Poyares D, Piovezan R, Nitrini R, Brucki S |title=Alzheimer's disease and sleep disturbances: a review |journal=Arq Neuropsiquiatr |volume=77 |issue=11 |pages=815–824 |date=November 2019 |pmid=31826138 |doi=10.1590/0004-282X20190149 |s2cid=209327994 |doi-access=free }}</ref><ref name=Uddin2020>{{cite journal |vauthors = Uddin MS, Tewari D, Mamun AA, Kabir MT, Niaz K, Wahed MI, Barreto GE, Ashraf GM |title=Circadian and sleep dysfunction in Alzheimer's disease |journal=Ageing Research Reviews |volume=60 |pages=101046 |date=July 2020 |pmid=32171783 |doi=10.1016/j.arr.2020.101046|s2cid=212729131 }}</ref> It was once thought that as people get older, the risk of developing sleep disorders and AD independently increase, but research is examining whether sleep disorders may increase the prevalence of AD.<ref name=Borges2019 /> One theory is that the mechanisms to increase clearance of toxic substances, including ], are active during sleep.<ref name=Borges2019 /><ref>{{cite journal |vauthors=Rasmussen MK, Mestre H, Nedergaard M |title=The glymphatic pathway in neurological disorders |journal=Lancet Neurol |volume=17 |issue=11 |pages=1016–1024 |date=November 2018 |pmid=30353860 |pmc=6261373 |doi=10.1016/S1474-4422(18)30318-1}}</ref> With decreased sleep, a person is increasing Aβ production and decreasing Aβ clearance, resulting in Aβ accumulation.<ref>{{cite journal |vauthors=Irwin MR, Vitiello MV |title=Implications of sleep disturbance and inflammation for Alzheimer's disease dementia |journal=Lancet Neurol |volume=18 |issue=3 |pages=296–306 |date=March 2019 |pmid=30661858 |doi=10.1016/S1474-4422(18)30450-2 |s2cid=58546748 }}</ref><ref name=Borges2019 /><ref name=Uddin2020 /> Receiving adequate sleep (approximately 7–8 hours) every night has become a potential lifestyle intervention to prevent the development of AD.<ref name="Yu 1201–1209"/> | |||
| ===NMDA antagonists=== | |||
| Recent evidence of the involvement of ]rgic neuronal ] in Alzheimer's disease led to the development and introduction of ]. ] is a novel ] ], and has been shown to be moderately clinically efficacious.<ref name="Areosa">{{cite journal | author = Areosa Sastre A, McShane R, Sherriff F | title = Memantine for dementia. | journal = Cochrane Database Syst Rev | volume = | issue = | pages = CD003154 | year = | id = PMID 15495043}}</ref> Memantine is marketed as Akatinol, Axura, Ebixa and Namenda. | |||
| Stress is a risk factor for the development of AD.<ref name="Yu 1201–1209"/> The mechanism by which stress predisposes someone to development of AD is unclear, but it is suggested that lifetime stressors may affect a person's ], leading to an overexpression or under expression of specific genes.<ref>{{cite journal |vauthors = Hampel H, Vergallo A, Aguilar LF, Benda N, Broich K, Cuello AC, Cummings J, Dubois B, Federoff HJ, Fiandaca M, Genthon R, Haberkamp M, Karran E, Mapstone M, Perry G, Schneider LS, Welikovitch LA, Woodcock J, Baldacci F, Lista S |title=Precision pharmacology for Alzheimer's disease |journal=Pharmacological Research |volume=130 |issue= |pages=331–365 |date=April 2018 |pmid=29458203 |pmc=8505114 |doi=10.1016/j.phrs.2018.02.014 }}</ref> Although the relationship of stress and AD is unclear, strategies to reduce stress and relax the mind may be helpful strategies in preventing the progression or Alzheimer's disease.<ref>{{cite journal |vauthors = Chen Y, Zhang J, Zhang T, Cao L, You Y, Zhang C, Liu X, Zhang Q |title=Meditation treatment of Alzheimer disease and mild cognitive impairment: A protocol for systematic review |journal=Medicine |volume=99 |issue=10 |pages=e19313 |date=March 2020 |pmid=32150066 |pmc=7478420 |doi=10.1097/MD.0000000000019313 }}</ref> Meditation, for instance, is a helpful lifestyle change to support cognition and well-being, though further research is needed to assess long-term effects.<ref name=Bhatti20192 /> | |||
| ===Psychosocial interventions=== | |||
| Cognitive and behavioral interventions and rehabilitation strategies may be used as an adjunct to pharmacological treatment, especially in the early to moderately advanced stages of disease. Treatment modalities include counseling, psychotherapy (if cognitive functioning is adequate), reminiscent therapy, reality orientation therapy, and behavioral reinforcements as well as cognitive rehabilitation training.<ref>{{cite journal | author = Olazarán J, Muñiz R, Reisberg B, Peña-Casanova J, del Ser T, Cruz-Jentoft A, Serrano P, Navarro E, García de la Rocha M, Frank A, Galiano M, Fernández-Bullido Y, Serra J, González-Salvador M, Sevilla C | title = Benefits of cognitive-motor intervention in MCI and mild to moderate Alzheimer disease. | journal = Neurology | volume = 63 | issue = 12 | pages = 2348-53 | year = 2004 | id = PMID 15623698}}</ref><ref>{{cite journal | author = Clare L, Woods R, Moniz Cook E, Orrell M, Spector A | title = Cognitive rehabilitation and cognitive training for early-stage Alzheimer's disease and vascular dementia. | journal = Cochrane Database Syst Rev | volume = | issue = | pages = CD003260 | year = | id = PMID 14583963}}</ref> | |||
| ==Management== | |||
| ===Treatments in clinical development=== | |||
| There is no cure for AD;<ref>{{cite journal | vauthors = Winkelman MJ, Szabo A, Frecska E | title = The potential of psychedelics for the treatment of Alzheimer's disease and related dementias | journal = European Neuropsychopharmacology | volume = 76 | pages = 3–16 | date = November 2023 | pmid = 37451163 | doi = 10.1016/j.euroneuro.2023.07.003 | hdl-access = free | doi-access = free | hdl = 10852/108211 }}</ref> available treatments offer relatively small symptomatic benefits but remain ] in nature.<ref name=Breijyeh2020 /><ref>{{cite book|title=Blueprints neurology|date=2019|vauthors= Drislane F, Hovauimian A, Tarulli A, Boegle AK, McIiduff C, Caplan LR |isbn=978-1-4963-8739-4|edition=Fifth|publisher= Wolters Kluwer|location=Philadelphia|page=146|oclc=1048659425}}</ref> Treatments can be divided into pharmaceutical, psychosocial, and caregiving. | |||
| A large number of potential treatments for Alzheimer's disease are currently under investigation, including four compounds being studied in ] clinical trials. ] had been shown to reduce neurodegeneration in animal studies.<ref>{{cite journal | author = Lemaire L, | |||
| Fournier J, Ponthus C, Le Fur Y, Confort-Gouny S, Vion-Dury J, Keane P, Cozzone P | |||
| | title = Magnetic resonance imaging of the neuroprotective effect of xaliproden in rats. | |||
| | journal = Invest Radiol | volume = 37 | issue = 6 | pages = 321-7 | year = 2002 | |||
| | id = PMID 12021588}} | |||
| </ref> ] (3APS or Alzhemed) is a GAG-mimetic molecule that is believed to act by binding to soluble amyloid beta to prevent the accumulation of the toxic plaques. ] (MPC-7869, formerly R-flubiprofen) is a gamma secretase modulator sometimes called a selective amyloid beta 42 lowering agent. It is believed to reduce the production of the toxic amyloid beta in favor of shorter forms of the peptide.<ref> | |||
| {{cite journal | |||
| | author = Zamrini E | title = Emerging Drug Therapies for Dementia. | |||
| | journal = Geriatrics Aging | volume = 9 | issue = 2 | pages = 107,110-113 | |||
| | year = 2006}} .</ref><ref> | |||
| {{cite journal | |||
| | author = Eriksen J, Sagi S, Smith T, Weggen S, Das P, McLendon D, Ozols V, | |||
| Jessing K, Zavitz K, Koo E, Golde T | |||
| | title = NSAIDs and enantiomers of flurbiprofen target gamma-secretase and lower Abeta 42 ''in vivo''. | |||
| | journal = J Clin Invest | volume = 112 | issue = 3 | pages = 440-9 | year = 2003 | |||
| | id = PMID 12897211}}. | |||
| </ref> ] has also been studied for Alzheimer’s. It is hypothesized to work by reducing luteinizing hormone levels which may be causing damage in the brain as one ages.<ref> {{cite journal | author | |||
| = Casadesus G, Garrett M, Webber K, Hartzler A, Atwood C, Perry G, Bowen R, Smith M | |||
| | title = The estrogen myth: potential use of gonadotropin-releasing hormone agonists for the treatment of Alzheimer's disease. | |||
| | journal = Drugs R D | volume = 7 | issue = 3 | pages = 187-93 | year = 2006 | |||
| | id = PMID 16752944}}.</ref> | |||
| ===Pharmaceutical=== | |||
| *'''Vaccines''' or ] for Alzheimer's, unlike typical ], would be used to treat diagnosed patients rather than for disease prevention. Ongoing efforts are based on the idea that, by training the immune system to recognize and attack beta-amyloid, the immune system might reverse deposition of amyloid and thus stop the disease. Initial results using this approach in animals were promising, and clinical trials of the drug candidate AN-1792 showed results in 20% of patients. However, in 2002 it was reported that 6% of multi-dosed participants (18 of 300) developed symptoms resembling ], and the trials were stopped. Participants in the halted trials continued to be followed, and 20% "developed high levels of antibodies to beta-amyloid" and some showed slower progression of the disease, maintaining memory-test levels while placebo-patients worsened. Microcerebral haemorrhages with passive immunisation and meningoencephalitis with active immunisation still remain potent threats to this strategy.<ref>{{cite web | |||
| ] of ], an ] used in the treatment of Alzheimer's disease symptoms]] | |||
| | title=Alzheimer’s Association Fact Sheet: AN-1792 (2006, on ALZ.org) | |||
| ], a medication approved for advanced Alzheimer's disease symptoms]] | |||
| | url=http://www.alz.org/Resources/TopicIndex/AN1792.asp | |||
| Medications used to treat the cognitive symptoms of AD rather than the underlying cause include: four ]s (], ], ], and ]) and ], an ]. The acetylcholinesterase inhibitors are intended for those with mild to severe AD, whereas memantine is intended for those with moderate or severe Alzheimer's disease.<ref name=Weller2018 /> The benefit from their use is small.<ref name=Birks2018 /><ref>{{cite journal | vauthors = Fink HA, Linskens EJ, MacDonald R, Silverman PC, McCarten JR, Talley KM, Forte ML, Desai PJ, Nelson VA, Miller MA, Hemmy LS, Brasure M, Taylor BC, Ng W, Ouellette JM, Sheets KM, Wilt TJ, Butler M |title = Benefits and Harms of Prescription Drugs and Supplements for Treatment of Clinical Alzheimer-Type Dementia | journal = Annals of Internal Medicine | volume = 172 | issue = 10 | pages = 656–668 | date = May 2020 | pmid = 32340037 | doi = 10.7326/M19-3887 | s2cid = 216595473 }}</ref><ref name=Berkowitz236>{{cite book|vauthors=Berkowitz A|title=Clinical neurology and neuroanatomy: a localization-based approach|date=2017|isbn=978-1-259-83440-0|publisher= McGraw Hill|location=New York|page=236|oclc=948547621}}</ref><ref name=Simon2018p111 /> | |||
| | accessdate=2006-11-06}}. | |||
| </ref> Work is continuing on less toxic ] vaccines. | |||
| Reduction in the activity of the ] neurons is a well-known feature of AD.<ref name=pmid8534419>{{cite journal | vauthors = Geula C, Mesulam MM | title = Cholinesterases and the pathology of Alzheimer disease | journal = Alzheimer Disease and Associated Disorders | volume = 9 | issue = Suppl 2 | pages = 23–28 | year = 1995 | pmid = 8534419 | doi = 10.1097/00002093-199501002-00005 }}</ref> Acetylcholinesterase inhibitors are employed to reduce the rate at which ] (ACh) is broken down, thereby increasing the concentration of ACh in the brain and combating the loss of ACh caused by the death of cholinergic neurons.<ref name=pmid11105732>{{cite journal | vauthors = Stahl SM | title = The new cholinesterase inhibitors for Alzheimer's disease, Part 2: illustrating their mechanisms of action | journal = The Journal of Clinical Psychiatry | volume = 61 | issue = 11 | pages = 813–814 | date = November 2000 | pmid = 11105732 | doi = 10.4088/JCP.v61n1101 | doi-access = free }}</ref> There is evidence for the efficacy of these medications in mild to moderate AD,<ref name=pmid16437532>{{cite journal | vauthors = Birks J | title = Cholinesterase inhibitors for Alzheimer's disease | journal = The Cochrane Database of Systematic Reviews | issue = 1 | pages = CD005593 | date = January 2006 | volume = 2016 | pmid = 16437532 | doi = 10.1002/14651858.CD005593 | pmc = 9006343 | veditors = Birks J }}</ref><ref name=Birks2018>{{cite journal | vauthors = Birks JS, Harvey RJ | title = Donepezil for dementia due to Alzheimer's disease | journal = The Cochrane Database of Systematic Reviews | volume = 2018 | issue = 6 | pages = CD001190 | date = June 2018 | pmid = 29923184 | pmc = 6513124 | doi = 10.1002/14651858.CD001190.pub3 }}</ref> and some evidence for their use in the advanced stage.<ref name=Birks2018 /> The use of these drugs in ] has not shown any effect in a delay of the onset of Alzheimer's disease.<ref name=pmid18044984>{{cite journal | vauthors = Raschetti R, Albanese E, Vanacore N, Maggini M | title = Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials | journal = PLOS Medicine | volume = 4 | issue = 11 | pages = e338 | date = November 2007 | pmid = 18044984 | pmc = 2082649 | doi = 10.1371/journal.pmed.0040338 | doi-access = free }}</ref> The most common ] are ] and ], both of which are linked to cholinergic excess. These side effects arise in approximately 10–20% of users, are mild to moderate in severity, and can be managed by slowly adjusting medication doses.<ref>{{cite book |vauthors=Alldredge BK, Corelli RL, Ernst ME, Guglielmo BJ, Jacobson PA, Kradjan WA, Williams BR |title=Applied therapeutics : the clinical use of drugs |date=2013 |publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins|location=Baltimore|isbn=978-1-60913-713-7|page=2385|edition=10th}}</ref> Less common secondary effects include muscle ]s, decreased ] (]), decreased ] and weight, and increased ] production.<ref name=pmid16437532 /> | |||
| *'''The statin simvastatin''' has been found to reduce the incidence of Alzheimer's disease and ] disease by almost 50 percent by resarchers from Boston University School of Medicine (BUSM).<ref> | |||
| {{cite web | |||
| | title=Researchers Find Specific Statin Significantly Reduces Alzheimer's and Parkinson's Disease Risk | |||
| | url=http://www.michaeljfox.org/newsEvents_parkinsonsInTheNews_article.cfm?ID=227 | |||
| | accessdate=2007-08-06}}.</ref><ref> | |||
| {{cite web | |||
| | title=Simvastatin is associated with a reduced incidence of dementia and Parkinson's disease | |||
| | url=http://www.biomedcentral.com/1741-7015/5/20 | |||
| | accessdate=2007-09-10}}. | |||
| </ref> | |||
| ] is an excitatory ] of the ], although excessive amounts in the ] can lead to ] death through a process called ] which consists of the overstimulation of glutamate ]. Excitotoxicity occurs not only in AD, but also in other neurological diseases such as ] and ].<ref name=pmid16424917>{{cite journal | vauthors = Lipton SA | title = Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond | journal = Nature Reviews. Drug Discovery | volume = 5 | issue = 2 | pages = 160–170 | date = February 2006 | pmid = 16424917 | doi = 10.1038/nrd1958 | s2cid = 21379258 }}</ref> ] is a noncompetitive ] first used as an anti-] agent. It acts on the ] by blocking ]s and inhibiting their overstimulation by glutamate.<ref name=pmid16424917 /><ref>{{cite web |url=https://www.nlm.nih.gov/medlineplus/druginfo/meds/a604006.html |title=Memantine |access-date=3 February 2010|date=4 January 2004|publisher=US National Library of Medicine (Medline) |archive-url=https://web.archive.org/web/20100222203921/https://www.nlm.nih.gov/medlineplus/druginfo/meds/a604006.html |archive-date=22 February 2010 | url-status=live | |||
| *'''Proposed alternative treatments''' for Alzheimer's include a range of herbal compounds and ]. In the AAGP review from 2006,<ref name="2006AAGP"/> ] in doses below 400 IU was mentioned as having conflicting evidence in efficacy to prevent AD. Higher doses were discouraged as these may be linked with higher mortality related to cardiac events. | |||
| }}</ref> Memantine has been shown to have a small benefit in the treatment of moderate to severe AD.<ref>{{cite journal | vauthors = McShane R, Westby MJ, Roberts E, Minakaran N, Schneider L, Farrimond LE, Maayan N, Ware J, Debarros J | title = Memantine for dementia | journal = The Cochrane Database of Systematic Reviews | volume = 3 | issue = 3 | pages = CD003154 | date = March 2019 | pmid = 30891742 | pmc = 6425228 | doi = 10.1002/14651858.CD003154.pub6 }}</ref> Reported adverse events with memantine are infrequent and mild, including ]s, ], ], ] and ].<ref>{{cite web | title=Namenda- memantine hydrochloride tablet Namenda- memantine hydrochloride kit | website=DailyMed | date=15 November 2018 | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=b9f27baf-aa2a-443a-9ef5-e002d23407ba | access-date=20 February 2022 | archive-date=27 January 2022 | archive-url=https://web.archive.org/web/20220127063519/https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=b9f27baf-aa2a-443a-9ef5-e002d23407ba | url-status=live }}</ref><ref>{{cite web | title=Namenda XR- memantine hydrochloride capsule, extended release Namenda XR- memantine hydrochloride kit | website=DailyMed | date=15 November 2019 | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=710f523f-0158-4639-8ce7-57598247d48c | access-date=20 February 2022 | archive-date=21 February 2022 | archive-url=https://web.archive.org/web/20220221050503/https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=710f523f-0158-4639-8ce7-57598247d48c | url-status=live }}</ref> The combination of memantine and donepezil<ref>{{cite web | title=Namzaric- memantine hydrochloride and donepezil hydrochloride capsule Namzaric- memantine hydrochloride and donepezil hydrochloride kit | website=DailyMed | date=22 January 2019 | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=90fedc32-19e5-480c-afc6-f35a5cf4b9aa | access-date=20 February 2022 | archive-date=20 January 2022 | archive-url=https://web.archive.org/web/20220120050522/https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=90fedc32-19e5-480c-afc6-f35a5cf4b9aa | url-status=live }}</ref> has been shown to be "of ] but clinically marginal effectiveness".<ref name=pmid18316756>{{cite journal | vauthors = Raina P, Santaguida P, Ismaila A, Patterson C, Cowan D, Levine M, Booker L, Oremus M | title = Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline | journal = Annals of Internal Medicine | volume = 148 | issue = 5 | pages = 379–397 | date = March 2008 | pmid = 18316756 | doi = 10.7326/0003-4819-148-5-200803040-00009 | s2cid = 22235353 }}</ref> | |||
| An extract of '']'' known as ''EGb 761'' has been used for treating AD and other neuropsychiatric disorders.<ref name=Kandia>{{cite journal | vauthors = Kandiah N, Ong PA, Yuda T, Ng LL, Mamun K, Merchant RA, Chen C, Dominguez J, Marasigan S, Ampil E, Nguyen VT, Yusoff S, Chan YF, Yong FM, Krairit O, Suthisisang C, Senanarong V, Ji Y, Thukral R, Ihl R | title = Treatment of dementia and mild cognitive impairment with or without cerebrovascular disease: Expert consensus on the use of Ginkgo biloba extract, EGb 761 | journal = CNS Neuroscience & Therapeutics | volume = 25 | issue = 2 | pages = 288–298 | date = February 2019 | pmid = 30648358 | pmc = 6488894 | doi = 10.1111/cns.13095 }}</ref> Its use is approved throughout Europe.<ref name=McKeage>{{cite journal | vauthors = McKeage K, Lyseng-Williamson KA | title = ''Ginkgo biloba'' extract EGb 761 in the symptomatic treatment of mild-to-moderate dementia: a profile of its use | journal = Drugs & Therapy Perspectives | volume = 34 | issue = 8 | pages = 358–366 | date = 2018 | pmid = 30546253 | pmc = 6267544 | doi = 10.1007/s40267-018-0537-8 }}</ref> The World Federation of Biological Psychiatry guidelines lists EGb 761 with the same weight of evidence (level B) given to acetylcholinesterase inhibitors and memantine. EGb 761 is the only one that showed improvement of symptoms in both AD and vascular dementia. EGb 761 may have a role either on its own or as an add-on if other therapies prove ineffective.<ref name=Kandia /> A 2016 review concluded that the quality of evidence from clinical trials on ''Ginkgo biloba'' has been insufficient to warrant its use for treating AD.<ref name=yang>{{cite journal | vauthors = Yang G, Wang Y, Sun J, Zhang K, Liu J | title = Ginkgo Biloba for Mild Cognitive Impairment and Alzheimer's Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials | journal = Current Topics in Medicinal Chemistry | volume = 16 | issue = 5 | pages = 520–528 | date = 22 October 2015 | pmid = 26268332 | doi = 10.2174/1568026615666150813143520 }}</ref> | |||
| Laboratory studies with cells and animals continually fuel the pipeline of potential treatments. Some currently approved drugs such as ]s and ]s<ref> {{cite journal | |||
| | author = Landreth G | title | |||
| = PPARgamma agonists as new therapeutic agents for treatment of Alzheimer's disease. | |||
| | journal = Exp Neurol | volume = 199 | issue = 2 | pages = 245-8 | year = 2006 | |||
| | id = PMID 16733054}} | |||
| </ref> have also been under investigation for the treatment and prevention of Alzheimer’s. | |||
| Recent ]s for Phase 2 and Phase 3 in this category have taken 12 to 18 months under study drug, plus additional months for patient enrollment and analysis. Compounds that are just entering into human trials or are in pre-clinical trials would be at least 4 years from being available to the public and would be available only if they can demonstrate safety and efficacy in human trials. | |||
| ]s are modestly useful in reducing ] and ] in people with AD, but their advantages are offset by serious adverse effects, such as ], ] or cognitive decline.<ref>{{cite journal | vauthors = Ballard C, Waite J | title = The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer's disease | journal = The Cochrane Database of Systematic Reviews | issue = 1 | pages = CD003476 | date = January 2006 | pmid = 16437455 | doi = 10.1002/14651858.CD003476.pub2 | veditors = Ballard CG | pmc = 11365591 }}</ref> When used in the long-term, they have been shown to associate with increased mortality.<ref name=pmid19138567>{{cite journal | vauthors = Ballard C, Hanney ML, Theodoulou M, Douglas S, McShane R, Kossakowski K, Gill R, Juszczak E, Yu LM, Jacoby R | title = The dementia antipsychotic withdrawal trial (DART-AD): long-term follow-up of a randomised placebo-controlled trial | journal = The Lancet. Neurology | volume = 8 | issue = 2 | pages = 151–157 | date = February 2009 | pmid = 19138567 | doi = 10.1016/S1474-4422(08)70295-3 | s2cid = 23000439}} See , January 2009.</ref> They are recommended in dementia only after first line therapies such as behavior modification have failed, and due to the risk of adverse effects, they should be used for the shortest amount of time possible.<ref name="Arvanitakis 2019" /> Stopping antipsychotic use in this group of people appears to be safe.<ref>{{cite journal | vauthors = Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter AI, van Driel ML, Christiaens T | title = Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia | journal = The Cochrane Database of Systematic Reviews | volume = 3 | issue = 3 | pages = CD007726 | date = March 2013 | pmid = 23543555 | doi = 10.1002/14651858.CD007726.pub2 | hdl-access = free | hdl = 1854/LU-3109108 }}</ref> | |||
| ===Occupational and lifestyle therapies=== | |||
| Modifications to the living environment and lifestyle of the Alzheimer's patient can improve functional performance and ease caretaker burden. Assessment by an ] is often indicated. Adherence to simplified routines and labeling of household items to cue the patient can aid with ], while placing safety locks on cabinets, doors, and gates and securing hazardous chemicals and guns can prevent accidents and wandering. Changes in routine or environment can trigger or exacerbate agitation, whereas well-lit rooms, adequate rest, and avoidance of excess stimulation all help prevent such episodes.<ref>Treating behavioral and psychiatric symptoms. Alzheimer's Association. Accessed Oct. 15, 2006.</ref> Appropriate social and visual stimulation, however, can improve function by increasing awareness and orientation. For instance, boldly colored tableware aids those with severe AD, helping people overcome a diminished sensitivity to visual contrast to increase food and beverage intake.<ref> {{cite journal | author = Dunne TE, Neargarder SA, Cipolloni PB, Cronin-Golomb A. | title = Visual contrast enhances food and liquid intake in advanced Alzheimer's disease | journal = Clin Nutr | volume = 23 | issue = 4 | pages = 533-8 | year = 2004 | id = PMID 15297089}} </ref> | |||
| == |
===Psychosocial=== | ||
| ] interventions are used as an adjunct to pharmaceutical treatment and can be classified within behavior-, emotion-, cognition- or stimulation-oriented approaches.{{update after|2022|2|16}}<ref name=pracGuideAPA>{{update after|2022|2|16}} {{cite journal | vauthors = Rabins PV, Blacker D, Rovner BW, Rummans T, Schneider LS, Tariot PN, Blass DM, McIntyre JS, Charles SC, Anzia DJ, Cook IA, Finnerty MT, Johnson BR, Nininger JE, Schneidman B, Summergrad P, Woods SM, Berger J, Cross CD, Brandt HA, Margolis PM, Shemo JP, Blinder BJ, Duncan DL, Barnovitz MA, Carino AJ, Freyberg ZZ, Gray SH, Tonnu T, Kunkle R, Albert AB, Craig TJ, Regier DA, Fochtmann LJ | title = American Psychiatric Association practice guideline for the treatment of patients with Alzheimer's disease and other dementias. Second edition | journal = The American Journal of Psychiatry | volume = 164 | issue = 12 Suppl | pages = 5–56 | date = December 2007 | pmid = 18340692 | collaboration = Steering Committee on Practice Guidelines }}</ref> | |||
| Alzheimer's is a major public health challenge since the median age of the industrialized world's population is increasing gradually.<ref> {{cite journal | author = Sloane P, Zimmerman S, Suchindran C, Reed P, Wang L, Boustani M, Sudha S | title = The public health impact of Alzheimer's disease, 2000-2050: potential implication of treatment advances. | journal = Annu Rev Public Health | volume = 23 | issue = | pages = 213-31 | year = | id = PMID 11910061}} </ref> Indeed, much of the concern about the solvency of governmental social safety nets is founded on estimates of the costs of caring for ], assuming that they develop Alzheimer's in the same proportions as earlier generations. For this reason, money spent informing the public of available effective prevention methods may yield disproportionate benefits. | |||
| ] attempt to identify and reduce the antecedents and consequences of problem behaviors. This approach has not shown success in improving overall functioning,<ref name=pmid16323385>{{cite journal | vauthors = Bottino CM, Carvalho IA, Alvarez AM, Avila R, Zukauskas PR, Bustamante SE, Andrade FC, Hototian SR, Saffi F, Câmargo CH | title = Cognitive rehabilitation combined with drug treatment in Alzheimer's disease patients: a pilot study | journal = Clinical Rehabilitation | volume = 19 | issue = 8 | pages = 861–869 | date = December 2005 | pmid = 16323385 | doi = 10.1191/0269215505cr911oa | s2cid = 21290731 }}</ref> but can help to reduce some specific problem behaviors, such as ].<ref name=pmid11342679>{{cite journal | vauthors = Doody RS, Stevens JC, Beck C, Dubinsky RM, Kaye JA, Gwyther L, Mohs RC, Thal LJ, Whitehouse PJ, DeKosky ST, Cummings JL | author-link1= Rachelle Doody| title = Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology | journal = Neurology | volume = 56 | issue = 9 | pages = 1154–1166 | date = May 2001 | pmid = 11342679 | doi = 10.1212/WNL.56.9.1154 | s2cid = 10711725 | doi-access = free | title-link = doi }}</ref> There is a lack of high quality data on the effectiveness of these techniques in other behavior problems such as wandering.<ref name=pmid17253573>{{cite journal | vauthors = Hermans DG, Htay UH, McShane R | title = Non-pharmacological interventions for wandering of people with dementia in the domestic setting | journal = The Cochrane Database of Systematic Reviews | issue = 1 | pages = CD005994 | date = January 2007 | volume = 2010 | pmid = 17253573 | pmc = 6669244 | doi = 10.1002/14651858.CD005994.pub2 }}</ref><ref name=pmid17096455>{{cite journal | vauthors = Robinson L, Hutchings D, Dickinson HO, Corner L, Beyer F, Finch T, Hughes J, Vanoli A, Ballard C, Bond J | title = Effectiveness and acceptability of non-pharmacological interventions to reduce wandering in dementia: a systematic review | journal = International Journal of Geriatric Psychiatry | volume = 22 | issue = 1 | pages = 9–22 | date = January 2007 | pmid = 17096455 | doi = 10.1002/gps.1643 | s2cid = 45660235 }}</ref> ] is effective in reducing behavioral and psychological symptoms.<ref>{{cite journal | vauthors = Abraha I, Rimland JM, Trotta FM, Dell'Aquila G, Cruz-Jentoft A, Petrovic M, Gudmundsson A, Soiza R, O'Mahony D, Guaita A, Cherubini A | title = Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series | journal = BMJ Open | volume = 7 | issue = 3 | pages = e012759 | date = March 2017 | pmid = 28302633 | pmc = 5372076 | doi = 10.1136/bmjopen-2016-012759 }}</ref> | |||
| The role of family ]s has also become more prominent, as care in the familiar surroundings of home may delay onset of some symptoms and delay or eliminate the need for more professional and costly levels of care. However, home-based care may entail tremendous economic, emotional, and even psychological costs as well (see ]). Family caregivers often give up time from work and forego pay to spend 47 hours per week on average with an affected loved one who frequently cannot be left alone. From a survey of patients with ], direct and indirect costs of caring for an Alzheimer's patient average $77,500 per year.<ref>{{cite journal |author = | title= The MetLife Study of Alzheimer’s Disease: The Caregiving Experience | journal= MetLife Mature Market Institute ® | issue= August 2006 | }} </ref> | |||
| Emotion-oriented interventions include ], ], supportive ], ], also called ], and ]. A Cochrane review has found no evidence that this is effective.<ref>{{cite journal | vauthors = Chung JC, Lai CK, Chung PM, French HP | title = Snoezelen for dementia | journal = The Cochrane Database of Systematic Reviews | issue = 4 | pages = CD003152 | date = 2002 | volume = 2010 | pmid = 12519587 | doi = 10.1002/14651858.CD003152 | pmc = 9002239 }}</ref> Reminiscence therapy (RT) involves the discussion of past experiences individually or in group, many times with the aid of photographs, household items, music and sound recordings, or other familiar items from the past. A 2018 review of the effectiveness of RT found that effects were inconsistent, small in size and of doubtful clinical significance, and varied by setting.<ref>{{cite journal | vauthors = Woods B, O'Philbin L, Farrell EM, Spector AE, Orrell M | title = Reminiscence therapy for dementia | journal = The Cochrane Database of Systematic Reviews | volume = 2018 | issue = 3 | pages = CD001120 | date = March 2018 | pmid = 29493789 | pmc = 6494367 | doi = 10.1002/14651858.CD001120.pub3 }}</ref> Simulated presence therapy (SPT) is based on ] and involves playing a recording with voices of the closest relatives of the person with AD. There is partial evidence indicating that SPT may reduce ]s.<ref name=pmid19023729>{{cite journal | vauthors = Zetteler J | title = Effectiveness of simulated presence therapy for individuals with dementia: a systematic review and meta-analysis | journal = Aging & Mental Health | volume = 12 | issue = 6 | pages = 779–785 | date = November 2008 | pmid = 19023729 | doi = 10.1080/13607860802380631 | s2cid = 39529938 }}</ref> | |||
| == Statistics on Alzheimer's disease == | |||
| ], former President of the United States was diagnosed in 1994]] | |||
| * In the United States of America, AD was the 7th leading cause of death in 2004, with 65,829 number of deaths (and rising).<ref> National Center for Health Statistics</ref> | |||
| * At over $100 billion per year, AD is the third most costly disease in the U.S., after heart disease and cancer.<ref> </ref> | |||
| * There are an estimated 24 million people with dementia worldwide.<ref></ref> By 2040, it is projected that this figure will have increased to 81 million. | |||
| * More than 5 million Americans are estimated to have Alzheimer’s disease.<ref name="AboutAD"> Alzheimer's Association</ref> It is projected that 14.3 million Americans will have the disease by mid-century: a 350 percent increase from 2000.<ref> | |||
| </ref> | |||
| * The federal government estimates spending approximately $647 million for Alzheimer’s disease research in fiscal year 2005.<ref name="AboutAD"/> | |||
| The aim of cognition-oriented treatments, which include reality orientation and ], is the reduction of ]s. Reality orientation consists of the presentation of information about time, place, or person to ease the understanding of the person about its surroundings and his or her place in them. On the other hand, cognitive retraining tries to improve impaired capacities by exercising mental abilities. Both have shown some efficacy improving cognitive capacities.<ref name=pmid12948999>{{cite journal | vauthors = Spector A, Thorgrimsen L, Woods B, Royan L, Davies S, Butterworth M, Orrell M | title = Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial | journal = The British Journal of Psychiatry | volume = 183 | issue = 3 | pages = 248–254 | date = September 2003 | pmid = 12948999 | doi = 10.1192/bjp.183.3.248 | doi-access = free | title-link = doi }}</ref> | |||
| ==Notable cases== | |||
| Notable cases of Alzheimer's disease have included ], ], ], ], ], ],<ref>{{cite book | last =Shenk | first =David | title = The Forgetting Alzheimer’s: Portrait of an Epidemic | publisher = Anchor Books| date =2003 | location =New York | id= ISBN 0-385-49838-1}}</ref> ], ], ], and Australia's ]. | |||
| Stimulation-oriented treatments include ], ] and ] therapies, ], and any other kind of ]. Stimulation has modest support for improving behavior, mood, and, to a lesser extent, function. Nevertheless, as important as these effects are, the main support for the use of stimulation therapies is the change in the person's routine.<ref name=pracGuideAPA /> | |||
| ==Alzheimer's in the media== | |||
| TV documentaries ''Malcolm and Barbara - A Love Story''(1999) and ''Malcolm and Barbara: Love’s Farewell'' (2007), featured ] who was diagnosed with Alzheimer's at the age of 51. Over a period of 14 years ] followed Malcolm and Barbara Pointon's lives. The documentary follows the couple as Malcolm succumbs to the disease and shows the harsh reality faced by carers. The 2007 programme was the target of controversy when initial media claims that the finale purported to show Malcolm's death from the disease, but insider sources revealed that in the closing shots of the documentary actually show Malcolm slipping into a coma from which he never recovered. The argument overshadowed the importance of the documentary, and when it aired on 8th August 2007 the narrator informs us that "Malcolm is in a coma, and dies three days later."<ref>{{cite website | title =Alzheimer's film-maker to face ITV lawyers | url =http://media.guardian.co.uk/site/story/0,,2143286,00.html}}</ref> | |||
| ===Caregiving=== | |||
| '']'' (Malayalam:''Molecule'') (]) is a ] film directed by ] which portrays the effects of Alzheimer's disease on the life of an individual and his family. | |||
| {{Further|Caring for people with dementia|Palliative care}} | |||
| Since AD has no cure and it gradually renders people incapable of tending to their own needs, caregiving is essentially the treatment and must be carefully managed over the course of the disease. | |||
| During the early and moderate stages, modifications to the living environment and lifestyle can increase ] and reduce caretaker burden.<ref name=pmid11220813>{{cite journal | vauthors = Gitlin LN, Corcoran M, Winter L, Boyce A, Hauck WW | title = A randomized, controlled trial of a home environmental intervention: effect on efficacy and upset in caregivers and on daily function of persons with dementia | journal = The Gerontologist | volume = 41 | issue = 1 | pages = 4–14 | date = February 2001 | pmid = 11220813 | doi = 10.1093/geront/41.1.4 | doi-access = free | title-link = doi }}</ref><ref name=pmid15860476>{{cite journal | vauthors = Gitlin LN, Hauck WW, Dennis MP, Winter L | title = Maintenance of effects of the home environmental skill-building program for family caregivers and individuals with Alzheimer's disease and related disorders | journal = The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences | volume = 60 | issue = 3 | pages = 368–374 | date = March 2005 | pmid = 15860476 | doi = 10.1093/gerona/60.3.368 | doi-access = free | title-link = doi }}</ref> Examples of such modifications are the adherence to simplified routines, the placing of safety locks, the labeling of household items to cue the person with the disease or the use of modified daily life objects.<ref name=pracGuideAPA /><ref>{{cite web |url=http://www.alz.org/Health/Treating/agitation.asp |title=Treating Behavioral and Psychiatric Symptoms |year=2006|access-date=25 September 2006|publisher=Alzheimer's Association |archive-url=https://web.archive.org/web/20060925112503/http://www.alz.org/Health/Treating/agitation.asp|archive-date=25 September 2006}}</ref><ref name=pmid15297089>{{cite journal | vauthors = Dunne TE, Neargarder SA, Cipolloni PB, Cronin-Golomb A | title = Visual contrast enhances food and liquid intake in advanced Alzheimer's disease | journal = Clinical Nutrition | volume = 23 | issue = 4 | pages = 533–538 | date = August 2004 | pmid = 15297089 | doi = 10.1016/j.clnu.2003.09.015 }}</ref> If eating becomes problematic, food will need to be prepared in smaller pieces or even ]d.<ref>{{cite book |vauthors=Dudek SB |title=Nutrition Essentials for Nursing Practice |publisher=Lippincott Williams & Wilkins|location=Hagerstown, Maryland|year=2007|page=360|isbn=978-0-7817-6651-7 |url=https://books.google.com/books?id=01zo6yf0IUEC&pg=PA360 |access-date=19 August 2008}}</ref> When ] arise, the use of ]s may be required. In such cases, the medical efficacy and ethics of continuing feeding is an important consideration of the caregivers and family members.<ref name=pmid16415742>{{cite journal | vauthors = Dennehy C | title = Analysis of patients' rights: dementia and PEG insertion | journal = British Journal of Nursing | volume = 15 | issue = 1 | pages = 18–20 | year = 2006 | pmid = 16415742 | doi = 10.12968/bjon.2006.15.1.20303 }}</ref><ref name=pmid16556924>{{cite journal | vauthors = Chernoff R | title = Tube feeding patients with dementia | journal = Nutrition in Clinical Practice | volume = 21 | issue = 2 | pages = 142–146 | date = April 2006 | pmid = 16556924 | doi = 10.1177/0115426506021002142 | s2cid = 20841502 }}</ref> The use of physical restraints is rarely indicated in any stage of the disease, although there are situations when they are necessary to prevent harm to the person with Alzheimer's disease or their caregivers.<ref name=pracGuideAPA /> | |||
| '']'' is a ] ] that tells the story of Irish novelist ] and her relationship with ]. The film contrasts the start of their relationship and their later life, when Murdoch (played by Dame ]) was suffering from Alzheimer's disease. The film is based on Bayley's memoir ''].'' | |||
| During the final stages of the disease, treatment is centred on relieving discomfort until death, often with the help of ].<ref name=pmid12854952>{{cite journal | vauthors = Shega JW, ], Hougham GW, Cox-Hayley D, Luchins D, Hanrahan P, Stocking C, Sachs GA | title = Palliative Excellence in Alzheimer Care Efforts (PEACE): a program description | journal = Journal of Palliative Medicine | volume = 6 | issue = 2 | pages = 315–320 | date = April 2003 | pmid = 12854952 | doi = 10.1089/109662103764978641 | s2cid = 6072807 }}</ref> | |||
| In the popular television show ] the mother of the main character ] dies after battling Alzheimer's disease. | |||
| == |
===Diet=== | ||
| Diet may be a modifiable risk factor for the development of Alzheimer's disease. The ], and the ] are both associated with less cognitive decline. A different approach has been to incorporate elements of both of these diets into one known as the ].<ref name=Acta>{{cite journal | vauthors = Dominguez LJ, Barbagallo M | title = Nutritional prevention of cognitive decline and dementia | journal = Acta Bio-Medica | volume = 89 | issue = 2 | pages = 276–290 | date = June 2018 | pmid = 29957766 | pmc = 6179018 | doi = 10.23750/abm.v89i2.7401 }}</ref> Studies of individual dietary components, minerals and supplements are conflicting as to whether they reduce AD risk or cognitive decline.<ref name=Acta /> Preliminary research indicates that abnormal eating behaviors and dietary changes are common in people with dementia, especially in later stages.<ref>{{Cite journal |last1=Cipriani |first1=Gabriele |last2=Carlesi |first2=Cecilia |last3=Lucetti |first3=Claudio |last4=Danti |first4=Sabrina |last5=Nuti |first5=Angelo |date=2016-12-01 |title=Eating Behaviors and Dietary Changes in Patients With Dementia |journal=American Journal of Alzheimer's Disease & Other Dementias |language=en |volume=31 |issue=8 |pages=706–716 |doi=10.1177/1533317516673155 |issn=1533-3175 |pmc=10852764 |pmid=27756815}}</ref> | |||
| * ] | |||
| * Other major ]s including ], ], and ] | |||
| * Diseases included in the ] of Alzheimer's, including ], ], ], and ] | |||
| * ] | |||
| * Information on the molecular pathogenesis of Alzheimer's disease, including ], ], and ] | |||
| * Articles related to ], including ], ], and ] | |||
| * ] concerning the diagnosis and therapy of protein-misfolding diseases | |||
| * ] | |||
| * Related societies, organizations and publications: | |||
| **], based in the United States | |||
| **], based in the United Kingdom | |||
| **], based in the United Kingdom | |||
| **], based in Ontario, Canada | |||
| **], a division of the U.S. National Institutes of Health | |||
| **] | |||
| **], based in ] | |||
| **], based in New York at Rockefeller University | |||
| == |
==Prognosis== | ||
| The early stages of AD are difficult to diagnose. A definitive diagnosis is usually made once cognitive impairment compromises daily living activities, although the person may still be living independently. The symptoms will progress from mild cognitive problems, such as memory loss through increasing stages of cognitive and non-cognitive disturbances, eliminating any possibility of independent living, especially in the late stages of the disease.<ref name=pmid10653284 /> | |||
| {{reflist|2}} | |||
| ] of people with AD is reduced.<ref name=Za2009>{{cite journal | vauthors = Zanetti O, Solerte SB, Cantoni F | title = Life expectancy in Alzheimer's disease (AD) | journal = Archives of Gerontology and Geriatrics | volume = 49 | issue = Suppl 1 | pages = 237–243 | date = 2009 | pmid = 19836639 | doi = 10.1016/j.archger.2009.09.035 }}</ref> The normal life expectancy for 60 to 70 years old is 23 to 15 years; for 90 years old it is 4.5 years.<ref>{{cite web |title=United States Life Tables, 2017 |url=https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_07-508.pdf |work=National Vital Statistics Reports, CDC |access-date=10 June 2021 |archive-date=24 May 2021 |archive-url=https://web.archive.org/web/20210524202524/https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_07-508.pdf |url-status=live }}</ref> Following AD diagnosis it ranges from 7 to 10 years for those in their 60s and early 70s (a loss of 13 to 8 years), to only about 3 years or less (a loss of 1.5 years) for those in their 90s.<ref name=Za2009 /> | |||
| ==External links== | |||
| * | |||
| {{commonscat}} | |||
| * {{DMOZ|Health/Conditions_and_Diseases/Neurological_Disorders/Alzheimer%27s/}} | |||
| * | |||
| * | |||
| {{Mental and behavioural disorders}} | |||
| {{Diseases of the nervous system}} | |||
| Fewer than 3% of people live more than fourteen years after diagnosis.<ref name=Molsa1995>{{cite journal | vauthors = Mölsä PK, Marttila RJ, Rinne UK | title = Long-term survival and predictors of mortality in Alzheimer's disease and multi-infarct dementia | journal = Acta Neurologica Scandinavica | volume = 91 | issue = 3 | pages = 159–164 | date = March 1995 | pmid = 7793228 | doi = 10.1111/j.1600-0404.1995.tb00426.x | s2cid = 19724937 }}</ref> Disease features significantly associated with reduced survival are an increased severity of cognitive impairment, decreased functional level, disturbances in the neurological examination, history of ], ], ] and ].<ref name=":0" /> Other coincident diseases such as ], ], or history of ] are also related with shortened survival.<ref name=pmid8757016>{{cite journal | vauthors = Bowen JD, Malter AD, Sheppard L, Kukull WA, McCormick WC, Teri L, Larson EB | title = Predictors of mortality in patients diagnosed with probable Alzheimer's disease | journal = Neurology | volume = 47 | issue = 2 | pages = 433–439 | date = August 1996 | pmid = 8757016 | doi = 10.1212/wnl.47.2.433 | s2cid = 24961809 }}</ref><ref name=pmid15068977>{{cite journal | vauthors = Larson EB, Shadlen MF, Wang L, McCormick WC, Bowen JD, Teri L, Kukull WA | title = Survival after initial diagnosis of Alzheimer disease | journal = Annals of Internal Medicine | volume = 140 | issue = 7 | pages = 501–509 | date = April 2004 | pmid = 15068977 | doi = 10.7326/0003-4819-140-7-200404060-00008 | s2cid = 27410149 }}</ref><ref name=pmid7792352>{{cite journal | vauthors = Jagger C, Clarke M, Stone A | title = Predictors of survival with Alzheimer's disease: a community-based study | journal = Psychological Medicine | volume = 25 | issue = 1 | pages = 171–177 | date = January 1995 | pmid = 7792352 | doi = 10.1017/S0033291700028191 | s2cid = 34066330 }}</ref> While the earlier the age at onset the higher the total survival years, life expectancy is particularly reduced when compared to the healthy population among those who are younger.<ref name=pmid12580712>{{cite journal | vauthors = Dodge HH, Shen C, Pandav R, DeKosky ST, Ganguli M | title = Functional transitions and active life expectancy associated with Alzheimer disease | journal = Archives of Neurology | volume = 60 | issue = 2 | pages = 253–259 | date = February 2003 | pmid = 12580712 | doi = 10.1001/archneur.60.2.253 | doi-access = free | title-link = doi }}</ref> Men have a less favourable survival prognosis than women.{{update after|2023|7|10}}<ref name=Molsa1995/><ref name=Ganguli2005>{{cite journal | vauthors = Ganguli M, Dodge HH, Shen C, Pandav RS, DeKosky ST | title = Alzheimer disease and mortality: a 15-year epidemiological study | journal = Archives of Neurology | volume = 62 | issue = 5 | pages = 779–784 | date = May 2005 | pmid = 15883266 | doi = 10.1001/archneur.62.5.779 | doi-access = free | title-link = doi }}</ref> | |||
| ] is the most frequent immediate cause of death brought by AD.<ref name=":0" /> While the reasons behind the lower prevalence of ] in AD patients remain unclear, some researchers hypothesize that biological mechanisms shared by both diseases might play a role. However, this requires further investigation.<ref>{{cite journal | vauthors = Lanni C, Masi M, Racchi M, Govoni S | title = Cancer and Alzheimer's disease inverse relationship: an age-associated diverging derailment of shared pathways | journal = Molecular Psychiatry | volume = 26 | issue = 1 | pages = 280–295 | date = January 2021 | pmid = 32382138 | doi = 10.1038/s41380-020-0760-2 }}</ref> | |||
| ==Epidemiology== | |||
| {{See also|Alzheimer's disease in African Americans|Alzheimer's Disease in the East Asian Population}} | |||
| Two main measures are used in ] studies: incidence and prevalence. ] is the number of new cases per unit of person-time at risk (usually number of new cases per thousand person-years); while ] is the total number of cases of the disease in the population at any given time. | |||
| [[File:Alzheimer's disease and other dementias world map-Deaths per million persons-WHO2012.svg|thumb|upright=1.3|Deaths per million persons in 2012 due to dementias including Alzheimer's disease | |||
| {{Div col|small=yes|colwidth=10em}} | |||
| {{legend|#ffff20|0–4}} | |||
| {{legend|#ffe820|5–8}} | |||
| {{legend|#ffd820|9–10}} | |||
| {{legend|#ffc020|11–13}} | |||
| {{legend|#ffa020|14–17}} | |||
| {{legend|#ff9a20|18–24}} | |||
| {{legend|#f08015|25–45}} | |||
| {{legend|#e06815|46–114}} | |||
| {{legend|#d85010|115–375}} | |||
| {{legend|#d02010|376–1266}} | |||
| {{div col end}}]] | |||
| Regarding incidence, ] ] (studies where a disease-free population is followed over the years) provide rates between 10 and 15 per thousand person-years for all dementias and 5–8 for AD,<ref name=pmid17727890>{{cite journal | vauthors = Bermejo-Pareja F, Benito-León J, Vega S, Medrano MJ, Román GC | title = Incidence and subtypes of dementia in three elderly populations of central Spain | journal = Journal of the Neurological Sciences | volume = 264 | issue = 1–2 | pages = 63–72 | date = January 2008 | pmid = 17727890 | doi = 10.1016/j.jns.2007.07.021 | s2cid = 34341344 }}</ref><ref name=pmid12028245>{{cite journal | vauthors = Di Carlo A, Baldereschi M, Amaducci L, Lepore V, Bracco L, Maggi S, Bonaiuto S, Perissinotto E, Scarlato G, Farchi G, Inzitari D | title = Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study | journal = Journal of the American Geriatrics Society | volume = 50 | issue = 1 | pages = 41–48 | date = January 2002 | pmid = 12028245 | doi = 10.1046/j.1532-5415.2002.50006.x | s2cid = 22576935 }}</ref> which means that half of new dementia cases each year are Alzheimer's disease. Advancing age is a primary risk factor for the disease and incidence rates are not equal for all ages: every 5 years after the age of 65, the risk of acquiring the disease approximately doubles, increasing from 3 to as much as 69 per thousand person years.<ref name=pmid17727890 /><ref name=pmid12028245 /> Females with AD are more common than males, but this difference is likely due to women's longer life spans. When adjusted for age, both sexes are affected by Alzheimer's at equal rates.<ref name=Simon2018p111>{{cite book|vauthors= Simon RP, Greenberg DA, Aminoff MJ|title=Clinical neurology|date=2018|isbn=978-1-259-86173-4|edition=Tenth |publisher= McGraw Hill |location=|page=111|oclc=1012400314}}</ref> In the United States, the risk of dying from AD in 2010 was 26% higher among the non-Hispanic white population than among the non-Hispanic black population, and the Hispanic population had a 30% lower risk than the non-Hispanic white population.<ref>Tejada-Vera B. (2013). Hyattsville, MD: ], ], ].</ref> However, much AD research remains to be done in minority groups, such as the ], ] and ] populations.<ref>{{cite journal | vauthors = Reitz C, Rogaeva E, Beecham GW | title = Late-onset vs nonmendelian early-onset Alzheimer disease: A distinction without a difference? | journal = Neurology. Genetics | volume = 6 | issue = 5 | pages = e512 | date = October 2020 | pmid = 33225065 | pmc = 7673282 | doi = 10.1212/NXG.0000000000000512 }}</ref><ref name="Liu-2013">{{cite journal | vauthors = Liu CC, Liu CC, Kanekiyo T, Xu H, Bu G | title = Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy | journal = Nature Reviews. Neurology | volume = 9 | issue = 2 | pages = 106–118 | date = February 2013 | pmid = 23296339 | pmc = 3726719 | doi = 10.1038/nrneurol.2012.263 }}</ref> Studies have shown that these groups are underrepresented in clinical trials and do not have the same risk of developing AD when carrying certain genetic risk factors (i.e. APOE4), compared to their caucasian counterparts.<ref name="Liu-2013"/><ref>{{cite journal | vauthors = Massett HA, Mitchell AK, Alley L, Simoneau E, Burke P, Han SH, Gallop-Goodman G, McGowan M | title = Facilitators, Challenges, and Messaging Strategies for Hispanic/Latino Populations Participating in Alzheimer's Disease and Related Dementias Clinical Research: A Literature Review | journal = Journal of Alzheimer's Disease | volume = 82 | issue = 1 | pages = 107–127 | date = 29 June 2021 | pmid = 33998537 | doi = 10.3233/JAD-201463 | s2cid = 234745473 }}</ref><ref>{{cite journal | vauthors = Huynh RA, Mohan C | title = Alzheimer's Disease: Biomarkers in the Genome, Blood, and Cerebrospinal Fluid | journal = Frontiers in Neurology | volume = 8 | pages = 102 | date = 2017 | pmid = 28373857 | doi = 10.3389/fneur.2017.00102 | pmc = 5357660 | doi-access = free }}</ref> | |||
| The prevalence of AD in populations is dependent upon factors including incidence and survival. Since the incidence of AD increases with age, prevalence depends on the mean age of the population for which prevalence is given. In the United States in 2020, AD dementia prevalence was estimated to be 5.3% for those in the 60–74 age group, with the rate increasing to 13.8% in the 74–84 group and to 34.6% in those greater than 85.<ref>{{cite journal |vauthors=Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA |title=Population estimate of people with clinical Alzheimer's disease and mild cognitive impairment in the United States (2020-2060) |journal=Alzheimer's & Dementia |date=May 2021 |volume=17 |issue=12 |pages=1966–1975 |pmid=34043283 |doi=10.1002/alz.12362 |pmc=9013315 |s2cid=235215290 }}</ref> Prevalence rates in some less developed regions around the globe are lower.<ref>{{cite journal |vauthors=Rizzi L, Rosset I, Roriz-Cruz M |title=Global epidemiology of dementia: Alzheimer's and vascular types |journal=Biomed Res Int |volume=2014 |issue= |pages=908915 |date=2014 |pmid=25089278 |pmc=4095986 |doi=10.1155/2014/908915 |doi-access=free | title-link=doi }}</ref><ref name=pmid16360788>{{cite journal|vauthors=Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, Hasegawa K, Hendrie H, Huang Y, Jorm A, Mathers C, Menezes PR, Rimmer E, Scazufca M|date=December 2005|title=Global prevalence of dementia: a Delphi consensus study|journal=Lancet|volume=366|issue=9503|pages=2112–2117|doi=10.1016/S0140-6736(05)67889-0|pmc=2850264|pmid=16360788}}</ref> Both the prevalence and incidence rates of AD are steadily increasing, however the prevalence rate is estimated to triple by 2050 reaching 152 million, compared to the 50 million people with AD globally in 2020.<ref name=Breijyeh2020/><ref>{{cite journal | vauthors = Li F, Qin W, Zhu M, Jia J | title = Model-Based Projection of Dementia Prevalence in China and Worldwide: 2020-2050 | journal = Journal of Alzheimer's Disease | volume = 82 | issue = 4 | pages = 1823–1831 | date = 1 January 2021 | pmid = 34219732 | doi = 10.3233/JAD-210493 | publisher = IOS Press | s2cid = 235735045 }}</ref><ref>{{Cite journal |last1=Nichols |first1=Emma |last2=Steinmetz |first2=Jaimie D |last3=Vollset |first3=Stein Emil |last4=Vos |first4=Theo |last5=Fukutaki |first5=Kai |last6=Chalek |first6=Julian |date=January 6, 2022 |title=Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019 |journal=The Lancet Public Health |volume=7 |issue=2 |pages=e105–e125 |doi=10.1016/S2468-2667(21)00249-8 |issn=2468-2667 |pmid=34998485 |pmc=8810394 |hdl=2440/135555 }}</ref> | |||
| ==History== | |||
| ] in 1902. Hers was the first described case of what became known as Alzheimer's disease.]] | |||
| The ] philosophers and ]s associated old age with increasing ].<ref name=pmid9661992 /> It was not until 1901 that German psychiatrist ] identified the first case of what became known as Alzheimer's disease, named after him, in a fifty-year-old woman he called ]. He followed her case until she died in 1906 when he first reported publicly on it.<ref>Auguste D.: | |||
| * {{cite journal | vauthors = Alzheimer A |title=Über eine eigenartige Erkrankung der Hirnrinde|trans-title=About a peculiar disease of the cerebral cortex |journal=Allgemeine Zeitschrift für Psychiatrie und Psychisch-Gerichtlich Medizin|volume=64|issue=1–2|pages=146–148|year=1907|language=de}} | |||
| * {{cite journal | vauthors = | title = About a peculiar disease of the cerebral cortex. By Alois Alzheimer, 1907 (Translated by L. Jarvik and H. Greenson) | journal = Alzheimer Disease and Associated Disorders | volume = 1 | issue = 1 | pages = 3–8 | year = 1987 | pmid = 3331112 | translator = H. Greenson }} | |||
| * {{cite book | vauthors = Maurer U, Maurer K |title=Alzheimer: The Life of a Physician and the Career of a Disease |publisher=Columbia University Press |location=New York|year=2003|page=|isbn=978-0-231-11896-5 |url=https://archive.org/details/alzheimerlifeofp00maur/page/270}}</ref> During the next five years, eleven similar cases were reported in the ], some of them already using the term Alzheimer's disease.<ref name=pmid9661992>{{cite journal | vauthors = Berchtold NC, Cotman CW | title = Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s | journal = Neurobiology of Aging | volume = 19 | issue = 3 | pages = 173–189 | year = 1998 | pmid = 9661992 | doi = 10.1016/S0197-4580(98)00052-9 | s2cid = 24808582 }}</ref> The disease was first described as a distinctive disease by ] after suppressing some of the clinical (delusions and hallucinations) and pathological features (arteriosclerotic changes) contained in the original report of Auguste D.<ref>{{cite journal |vauthors=Berrios GE |title=Alzheimer's Disease: A Conceptual History |journal=Int. J. Geriatr. Psychiatry |volume=5|issue=6|pages=355–365|year=1990|doi=10.1002/gps.930050603|s2cid=145155424}}</ref> He included ''Alzheimer's disease'', also named ''presenile'' ] by Kraepelin, as a subtype of ''senile dementia'' in the eighth edition of his ''Textbook of Psychiatry'', published on 15 July 1910.<ref name=isbn1-4325-0833-4>{{cite book | vauthors = Kraepelin E |translator=Diefendorf AR |title=Clinical Psychiatry: A Textbook For Students And Physicians (Reprint) |publisher=Kessinger Publishing|year=2007|page=568|isbn=978-1-4325-0833-3}}</ref> | |||
| For most of the 20th century, the diagnosis of Alzheimer's disease was reserved for individuals between the ages of 45 and 65 who developed symptoms of dementia. The terminology changed after 1977 when a conference on Alzheimer's disease concluded that the clinical and ] manifestations of presenile and senile dementia were almost identical, although the authors also added that this did not rule out the possibility that they had different causes.<ref name=isbn0-89004-225-X>{{cite book |veditors=Katzman R, Terry RD, Bick KL |title=Alzheimer's Disease: Senile Dementia and Related Disorders |publisher=Raven Press|location=New York|year=1978|page=595|isbn=978-0-89004-225-0}}</ref> This eventually led to the diagnosis of ''Alzheimer's disease'' independent of age.<ref name=pmid9702682>{{cite journal | vauthors = Boller F, Forbes MM | title = History of dementia and dementia in history: an overview | journal = Journal of the Neurological Sciences | volume = 158 | issue = 2 | pages = 125–133 | date = June 1998 | pmid = 9702682 | doi = 10.1016/S0022-510X(98)00128-2 | s2cid = 42399340 }}</ref> The term ''senile dementia of the Alzheimer type'' (SDAT) was used for a time to describe the condition in those over 65, with classical Alzheimer's disease being used to describe those who were younger. Eventually, the term Alzheimer's disease was formally adopted in medical ] to describe individuals of all ages with a characteristic common symptom pattern, disease course, and ].<ref name=pmid3531918>{{cite journal | vauthors = Amaducci LA, Rocca WA, Schoenberg BS | title = Origin of the distinction between Alzheimer's disease and senile dementia: how history can clarify nosology | journal = Neurology | volume = 36 | issue = 11 | pages = 1497–1499 | date = November 1986 | pmid = 3531918 | doi = 10.1212/wnl.36.11.1497 | s2cid = 7689479 }}</ref> | |||
| The ] (NINCDS) and the ] (ADRDA, now known as the ]) established the most commonly used ] for diagnosis in 1984,<ref name=pmid6610841>{{cite journal|vauthors=McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM|date=July 1984|title=Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease|journal=Neurology|volume=34|issue=7|pages=939–944|doi=10.1212/wnl.34.7.939|pmid=6610841|doi-access=free | title-link=doi|s2cid=11646075}}</ref> extensively updated in 2007.<ref name=pmid17616482>{{cite journal | vauthors = Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O'brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P | title = Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria | journal = The Lancet. Neurology | volume = 6 | issue = 8 | pages = 734–746 | date = August 2007 | pmid = 17616482 | doi = 10.1016/S1474-4422(07)70178-3 | s2cid = 7356809 }}</ref><ref name=Stern2020 /> These criteria require that the presence of ], and a suspected dementia syndrome, be confirmed by ] for a clinical diagnosis of possible or probable Alzheimer's disease. A ] confirmation including a ] examination of ] is required for a definitive diagnosis. Good ] and ] have been shown between the diagnostic criteria and definitive histopathological confirmation.<ref name=pmid7986174>{{cite journal | vauthors = Blacker D, Albert MS, Bassett SS, Go RC, Harrell LE, Folstein MF | title = Reliability and validity of NINCDS-ADRDA criteria for Alzheimer's disease. The National Institute of Mental Health Genetics Initiative | journal = Archives of Neurology | volume = 51 | issue = 12 | pages = 1198–1204 | date = December 1994 | pmid = 7986174 | doi = 10.1001/archneur.1994.00540240042014 }}</ref> | |||
| ==Society and culture== | |||
| {{See also|Alzheimer's disease organizations}} | |||
| ===Social costs=== | |||
| Dementia, and specifically Alzheimer's disease, may be among the most costly diseases for societies worldwide.<ref name=El-Hayek2019>{{cite journal |vauthors = El-Hayek YH, Wiley RE, Khoury CP, Daya RP, Ballard C, Evans AR, Karran M, Molinuevo JL, Norton M, Atri A |title=Tip of the Iceberg: Assessing the Global Socioeconomic Costs of Alzheimer's Disease and Related Dementias and Strategic Implications for Stakeholders |journal=Journal of Alzheimer's Disease |volume=70 |issue=2 |pages=323–341 |date=2019 |pmid=31256142 |pmc=6700654 |doi=10.3233/JAD-190426 }}</ref> As populations age, these costs will probably increase and become an important ] and economic burden.<ref name=Wong2020>{{cite journal |vauthors=Wong W |title=Economic burden of Alzheimer disease and managed care considerations |journal=Am J Manag Care |volume=26 |issue=8 Suppl |pages=S177–S183 |date=August 2020 |pmid=32840331 |doi=10.37765/ajmc.2020.88482 |s2cid=221308149 |url=https://www.ajmc.com/view/economic-burden-of-alzheimer-disease-and-managed-care-considerations |doi-access=free |access-date=17 March 2022 |archive-date=25 February 2022 |archive-url=https://web.archive.org/web/20220225012224/https://www.ajmc.com/view/economic-burden-of-alzheimer-disease-and-managed-care-considerations |url-status=live }}</ref> Costs associated with AD include direct and indirect medical costs, which vary between countries depending on social care for a person with AD.<ref name=El-Hayek2019 /><ref name=Tahami2022>{{cite journal |vauthors=Tahami Monfared AA, Byrnes MJ, White LA, Zhang Q |title=The Humanistic and Economic Burden of Alzheimer's Disease |journal=Neurol Ther |date=February 2022 |volume=11 |issue=2 |pages=525–551 |pmid=35192176 |doi=10.1007/s40120-022-00335-x |pmc=9095804 |s2cid=247014076 }}</ref><ref name=Kosaner2021>{{cite journal |vauthors=Kosaner Kließ M, Martins R, Connolly MP |title=Major Cost Drivers in Assessing the Economic Burden of Alzheimer's Disease: A Structured, Rapid Review |journal=J Prev Alzheimers Dis |volume=8 |issue=3 |pages=362–370 |date=2021 |pmid=34101795 |doi=10.14283/jpad.2021.17 |s2cid=233403683 |doi-access=free }}</ref> Direct costs include doctor visits, hospital care, medical treatments, ], specialized equipment, and household expenses.<ref name=El-Hayek2019 /><ref name=Wong2020 /> Indirect costs include the cost of informal care and the loss in ] of informal caregivers.<ref name=Wong2020 /> | |||
| In the United States {{as of|2019|lc=y}}, informal (family) care is estimated to constitute nearly three-fourths of caregiving for people with AD at a cost of US$234 billion per year and approximately 18.5 billion hours of care.<ref name=El-Hayek2019 /> The cost to society worldwide to care for individuals with AD is projected to increase nearly ten-fold, and reach about US$9.1 trillion by 2050.<ref name=Tahami2022 /> | |||
| Costs for those with more severe dementia or behavioral disturbances are higher and are related to the additional caregiving time to provide physical care.<ref name=Kosaner2021 /> | |||
| ===Caregiving burden=== | |||
| {{Further|Caregiving and dementia}} | |||
| {{update section|date=February 2022}} | |||
| Individuals with Alzheimer's will require assistance in their lifetime, and care will most likely come in the form of a full-time ] which is often a role that is taken on by the spouse or a close relative. Caregiving tends to include physical and emotional burdens as well as time and financial strain at times on the person administering the aid.<ref>{{cite journal | vauthors = Demirbas M, Hahn-Pedersen JH, Jørgensen HL | title = Comparison Between Burden of Care Partners of Individuals with Alzheimer's Disease Versus Individuals with Other Chronic Diseases | journal = Neurology and Therapy | volume = 12 | issue = 4 | pages = 1051–1068 | date = August 2023 | pmid = 37222859 | pmc = 10310688 | doi = 10.1007/s40120-023-00493-6 }}</ref><ref name=metlife.com>{{cite web |title=The MetLife study of Alzheimer's disease: The caregiving experience |date=August 2006|publisher=MetLife Mature Market Institute|access-date=5 February 2011 |url=http://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf |archive-url=https://web.archive.org/web/20110108073750/http://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf|archive-date=8 January 2011|url-status=dead}}</ref> Alzheimer's disease is known for placing a great burden on caregivers which includes social, psychological, physical, or economic aspects.<ref name=Thom2007 /><ref name=pmid10489656>{{cite journal | vauthors = Schneider J, Murray J, Banerjee S, Mann A | title = EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: I—Factors associated with carer burden | journal = International Journal of Geriatric Psychiatry | volume = 14 | issue = 8 | pages = 651–661 | date = August 1999 | pmid = 10489656 | doi = 10.1002/(SICI)1099-1166(199908)14:8<651::AID-GPS992>3.0.CO;2-B | s2cid = 27346798 | doi-access = free }}</ref><ref name=pmid10489657>{{cite journal | vauthors = Murray J, Schneider J, Banerjee S, Mann A | title = EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: II—A qualitative analysis of the experience of caregiving | journal = International Journal of Geriatric Psychiatry | volume = 14 | issue = 8 | pages = 662–667 | date = August 1999 | pmid = 10489657 | doi = 10.1002/(SICI)1099-1166(199908)14:8<662::AID-GPS993>3.0.CO;2-4 | s2cid = 41741923 }}</ref> Home care is usually preferred by both those people with Alzheimer's disease as well as their families.<ref name=pmid18044111>{{cite journal | vauthors = Zhu CW, Sano M | title = Economic considerations in the management of Alzheimer's disease | journal = Clinical Interventions in Aging | volume = 1 | issue = 2 | pages = 143–154 | year = 2006 | pmid = 18044111 | pmc = 2695165 | doi = 10.2147/ciia.2006.1.2.143 | doi-access = free }}</ref> This option also delays or eliminates the need for more professional and costly levels of care.<ref name=pmid18044111 /><ref>{{cite journal | vauthors = Gaugler JE, Kane RL, Kane RA, Newcomer R | title = Early community-based service utilization and its effects on institutionalization in dementia caregiving | journal = The Gerontologist | volume = 45 | issue = 2 | pages = 177–185 | date = April 2005 | pmid = 15799982 | doi = 10.1093/geront/45.2.177 | doi-access = free | title-link = doi }}</ref> Nevertheless, two-thirds of nursing home residents have dementias.<ref name=pracGuideAPA /> | |||
| ] caregivers are subject to high rates of physical and ] disorders.<ref name=pmid12480441>{{cite journal | vauthors = Ritchie K, Lovestone S | title = The dementias | journal = Lancet | volume = 360 | issue = 9347 | pages = 1759–1766 | date = November 2002 | pmid = 12480441 | doi = 10.1016/S0140-6736(02)11667-9 | s2cid = 21404062 }}</ref> Factors associated with greater psychosocial problems of the primary caregivers include having an affected person at home, the caregiver being a spouse, demanding behaviors of the cared person such as depression, behavioral disturbances, hallucinations, sleep problems or walking disruptions and ].<ref name=pmid2241719>{{cite journal | vauthors = Brodaty H, Hadzi-Pavlovic D | title = Psychosocial effects on carers of living with persons with dementia | journal = The Australian and New Zealand Journal of Psychiatry | volume = 24 | issue = 3 | pages = 351–361 | date = September 1990 | pmid = 2241719 | doi = 10.3109/00048679009077702 | s2cid = 11788466 }}</ref><ref name=pmid9646153>{{cite journal | vauthors = Donaldson C, Tarrier N, Burns A | title = Determinants of carer stress in Alzheimer's disease | journal = International Journal of Geriatric Psychiatry | volume = 13 | issue = 4 | pages = 248–256 | date = April 1998 | pmid = 9646153 | doi = 10.1002/(SICI)1099-1166(199804)13:4<248::AID-GPS770>3.0.CO;2-0 | s2cid = 22187694 }}</ref> In the United States, the yearly cost of caring for a person with dementia ranges from $41,689-$56,290 per year.<ref name="Hurd 2013">{{cite journal |last1=Hurd |first1=Michael D. |last2=Martorell |first2=Paco |last3=Delavande |first3=Adeline |last4=Mullen |first4=Kathleen J. |last5=Langa |first5=Kenneth M. |title=Monetary Costs of Dementia in the United States |journal=New England Journal of Medicine |date=4 April 2013 |volume=368 |issue=14 |pages=1326–1334 |doi=10.1056/NEJMsa1204629|pmid=23550670 |pmc=3959992 }}</ref> Other estimates range from $28,078-$56,022 per year for formal medical care and $36,667-$92,689 for informal care provided by a relative or friend (assuming market value replacement costs for the care provided by the informal caregiver) and $15,792-$71,813 in lost wages.<ref name="Nandi 2024">{{cite journal |last1=Nandi |first1=Arindam |last2=Counts |first2=Nathaniel |last3=Bröker |first3=Janina |last4=Malik |first4=Sabrina |last5=Chen |first5=Simiao |last6=Han |first6=Rachael |last7=Klusty |first7=Jessica |last8=Seligman |first8=Benjamin |last9=Tortorice |first9=Daniel |last10=Vigo |first10=Daniel |last11=Bloom |first11=David E. |title=Cost of care for Alzheimer's disease and related dementias in the United States: 2016 to 2060 |journal=npj Aging |date=8 February 2024 |volume=10 |issue=1 |page=13 |doi=10.1038/s41514-024-00136-6|pmid=38331952 |pmc=10853249 }}</ref> | |||
| ] and the teaching of ] either individually or in group have demonstrated their efficacy in improving caregivers' psychological health.<ref name=Thom2007 /><ref name=pmid11511058>{{cite journal | vauthors = Pusey H, Richards D | title = A systematic review of the effectiveness of psychosocial interventions for carers of people with dementia | journal = Aging & Mental Health | volume = 5 | issue = 2 | pages = 107–119 | date = May 2001 | pmid = 11511058 | doi = 10.1080/13607860120038302 | s2cid = 32517015 }}</ref> | |||
| ===Media=== | |||
| {{Main|Alzheimer's disease in the media}} | |||
| Alzheimer's disease has been portrayed in films such as: '']'' (2001), based on ]'s memoir of his wife ];<ref>{{cite book |title=Iris: A Memoir of Iris Murdoch | vauthors = Bayley J |publisher=Abacus|location=London|year=2000|isbn=978-0-349-11215-2|oclc=41960006}}</ref> '']'' (2004), based on ]'s 1996 ];<ref>{{cite book |title=The notebook| vauthors = Sparks N |year=1996 |publisher=Thorndike Press |location=Thorndike, Maine|page=|isbn=978-0-7862-0821-0 |url=https://archive.org/details/notebook00spar_1/page/268}}</ref> '']'' (2004); '']'' (2005);<ref>{{cite web |url=http://www.webindia123.com/movie/regional/thanmatra/index.htm |title=Thanmathra |publisher=Webindia123.com |access-date=24 January 2008 |archive-url=https://web.archive.org/web/20071106105455/http://www.webindia123.com/movie/regional/thanmatra/index.htm|archive-date=6 November 2007}}</ref> '']'' (2006), based on Hiroshi Ogiwara's novel of the same name;<ref>{{cite book | vauthors = Ogiwara H |year=2004 |title=Ashita no Kioku |location=Tōkyō|publisher=Kōbunsha|isbn=978-4-334-92446-1|oclc=57352130|language=ja}}</ref> '']'' (2006), based on ]'s ] '']'';<ref>{{cite book|title=Hateship, Friendship, Courtship, Loveship, Marriage: Stories | vauthors = Munro A |location=New York|publisher=A.A. Knopf|year=2001|isbn=978-0-375-41300-1|oclc=46929223|title-link=Hateship, Friendship, Courtship, Loveship, Marriage}}</ref> '']'' (2014), about a ] professor who has early onset Alzheimer's disease, based on ]'s ] and featuring ] in the title role. Documentaries on Alzheimer's disease include ''Malcolm and Barbara: A Love Story'' (1999) and ''Malcolm and Barbara: Love's Farewell'' (2007), both featuring ].<ref>{{cite web |url=http://www.dfgdocs.com/Directory/Titles/700.aspx |title=Malcolm and Barbara: A love story |publisher=Dfgdocs|access-date=24 January 2008|url-status=dead |archive-url=https://web.archive.org/web/20080524213821/http://www.dfgdocs.com/Directory/Titles/700.aspx|archive-date=24 May 2008}}</ref><ref>{{cite web |url=https://www.bbc.co.uk/cambridgeshire/content/articles/2007/08/06/pointon_audio_feature.shtml |title=Malcolm and Barbara: A love story |publisher=BBC Cambridgeshire|access-date=2 March 2008 |archive-url=https://web.archive.org/web/20121110084233/http://www.bbc.co.uk/cambridgeshire/content/articles/2007/08/06/pointon_audio_feature.shtml|archive-date=10 November 2012}}</ref><ref>{{cite news |url=https://www.theguardian.com/media/2007/aug/07/broadcasting.itv |title=Alzheimer's film-maker to face ITV lawyers |publisher=Guardian Media|date=7 August 2007|access-date=24 January 2008|location=London|vauthors=Plunkett J |archive-url=https://web.archive.org/web/20080115132419/http://www.guardian.co.uk/media/2007/aug/07/broadcasting.itv|archive-date=15 January 2008}}</ref> | |||
| Alzheimer's disease has also been portrayed in music by English musician ] in releases such as '']'' (2008), '']'' (2011), and '']'' (2016{{endash}}2019).<ref>{{cite web |url=https://www.factmag.com/2009/08/26/the-caretaker-persistent-repetition-of-phrases/ |title=The Caretaker: ''Persistent Repetition of Phrases'' |date=26 August 2009|access-date=9 April 2021|website=] |archive-url=https://web.archive.org/web/20210415031615/https://www.factmag.com/2009/08/26/the-caretaker-persistent-repetition-of-phrases/|archive-date=15 April 2021|url-status=live}}</ref><ref>{{cite web |url=https://pitchfork.com/reviews/albums/15518-an-empty-bliss-beyond-this-world/ |title=The Caretaker: ''An Empty Bliss Beyond This World'' Album Review |date=14 June 2011|access-date=19 February 2021|website=]| vauthors = Powell M |archive-url=https://web.archive.org/web/20110618005627/http://www.pitchfork.com/reviews/albums/15518-an-empty-bliss-beyond-this-world|archive-date=18 June 2011|url-status=live}}</ref><ref>{{cite web |url=https://www.nytimes.com/2020/10/23/style/tiktok-caretaker-challenge-dementia.html |title=Why Are TikTok Teens Listening to an Album About Dementia? |date=23 October 2020|access-date=21 April 2021 |website=The New York Times| vauthors = Ezra M |archive-url=https://web.archive.org/web/20201023171008/https://www.nytimes.com/2020/10/23/style/tiktok-caretaker-challenge-dementia.html|archive-date=23 October 2020|url-status=live|url-access=limited}}</ref> Paintings depicting the disorder include the late works by American artist ], who drew self-portraits from 1995 to 2000 as an experiment of showing his disease through art.<ref>{{cite web |url=https://www.theguardian.com/culture/2015/jul/19/dementia-and-the-arts-fiction-films-drama-poetry-painting |title=Words fail us: dementia and the arts |date=19 July 2015|access-date=14 June 2021 |website=]| vauthors = Gerrard N |archive-url=https://web.archive.org/web/20150719073843/https://www.theguardian.com/culture/2015/jul/19/dementia-and-the-arts-fiction-films-drama-poetry-painting |archive-date=19 July 2015|url-status=live}}</ref><ref>{{cite news |url=https://www.nytimes.com/2006/10/24/health/24alzh.html |title=Self-Portraits Chronicle a Descent Into Alzheimer's |date=24 October 2006|access-date=14 June 2021 |website=The New York Times | vauthors = Grady D |archive-url=https://web.archive.org/web/20061024065357/https://www.nytimes.com/2006/10/24/health/24alzh.html|archive-date=24 October 2006|url-status=live|url-access=limited}}</ref> | |||
| ==Research directions== | |||
| {{see also|Anti-amyloid drugs}} | |||
| Antibodies may have the ability to alter the disease course by targeting amyloid beta with immunotherapy medications such as ], ], and ].<ref>{{cite journal | vauthors = Shi M, Chu F, Zhu F, Zhu J | title = Impact of Anti-amyloid-β Monoclonal Antibodies on the Pathology and Clinical Profile of Alzheimer's Disease: A Focus on Aducanumab and Lecanemab | journal = Frontiers in Aging Neuroscience | volume = 14 | issue = | pages = 870517 | date = 2022 | pmid = 35493943 | pmc = 9039457 | doi = 10.3389/fnagi.2022.870517 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Cummings J, Zhou Y, Lee G, Zhong K, Fonseca J, Cheng F | title = Alzheimer's disease drug development pipeline: 2023 | journal = Alzheimer's & Dementia | volume = 9 | issue = 2 | pages = e12385 | date = 2023 | pmid = 37251912 | pmc = 10210334 | doi = 10.1002/trc2.12385 }}</ref><ref>{{cite web |url= https://www.nia.nih.gov/health/how-alzheimers-disease-treated |title= How Is Alzheimer's Disease Treated? |publisher= U.S. ] |date= 1 April 2023 |access-date= 10 July 2023}}</ref> Aducanumab was approved by the US ] (FDA) in 2021, using the ], although the approval generated controversy and more evidence is needed to address administration, safety, and effectiveness.<ref name=Vaz2022>{{cite journal | vauthors = Vaz M, Silva V, Monteiro C, Silvestre S | title = Role of Aducanumab in the Treatment of Alzheimer's Disease: Challenges and Opportunities | journal = Clinical Interventions in Aging | volume = 17 | issue = | pages = 797–810 | date = 2022 | pmid = 35611326 | pmc = 9124475 | doi = 10.2147/CIA.S325026 | doi-access = free }}</ref><ref name=Day2022>{{cite journal | vauthors = Day GS, Scarmeas N, Dubinsky R, Coerver K, Mostacero A, West B, Wessels SR, Armstrong MJ | title = Aducanumab Use in Symptomatic Alzheimer Disease Evidence in Focus: A Report of the AAN Guidelines Subcommittee | journal = Neurology | volume = 98 | issue = 15 | pages = 619–631 | date = April 2022 | pmid = 35197360 | pmc = 9012273 | doi = 10.1212/wnl.0000000000200176 }}</ref><ref name=Mahase2021>{{cite journal | vauthors = Mahase E | title = Three FDA advisory panel members resign over approval of Alzheimer's drug | journal = BMJ | volume = 373 | issue = | pages = n1503 | date = June 2021 | pmid = 34117086 | doi = 10.1136/bmj.n1503 | url = https://www.bmj.com/content/373/bmj.n1503.long | access-date = 7 July 2023 | url-status = live | s2cid = 235405355 | archive-url = https://web.archive.org/web/20230708042005/https://www.bmj.com/content/373/bmj.n1503.long | archive-date = 8 July 2023 }}</ref><ref name=NYT2021>{{cite news |url= https://www.nytimes.com/2021/06/10/health/aduhelm-fda-resign-alzheimers.html |title= Three F.D.A. Advisers Resign Over Agency's Approval of Alzheimer's Drug |work= The New York Times |vauthors= Belluck P, Robbins R |date= June 10, 2021 |access-date= July 7, 2023 |archive-date= 14 November 2021 |archive-url= https://web.archive.org/web/20211114103425/https://www.nytimes.com/2021/06/10/health/aduhelm-fda-resign-alzheimers.html |url-status= live }}</ref> It has less effectiveness in people who already had severe Alzheimer's symptoms.<ref>{{cite journal | vauthors = Abyadeh M, Gupta V, Gupta V, Chitranshi N, Wu Y, Amirkhani A, Meyfour A, Sheriff S, Shen T, Dhiman K, Ghasem HS, Paul AH, Stuart LG, Mirzaei M | title = Comparative Analysis of Aducanumab, Zagotenemab and Pioglitazone as Targeted Treatment Strategies for Alzheimer's Disease | journal = Aging and Disease | volume = 12 | issue = 8 | pages = 1964–1976 | date = December 2021 | pmid = 34881080 | pmc = 8612603 | doi = 10.14336/AD.2021.0719 }}</ref> In early 2024, Biogen announced it would discontinue aducanumab.<ref name=":1">{{Cite news |last=Wade |first=Grace |date=August 3, 2024 |title=The truth about Alzheimer's drugs |work=New Scientist |page=14}}</ref> | |||
| Lecanemab, which clears plaques and reduces amyloid proteins,<ref name=":2">{{Cite news |last=Wade |first=Grace |date=August 3, 2024 |title=The truth about Alzheimer's drugs |work=New Scientist |page=15}}</ref> was approved via the FDA accelerated approval process,<ref>{{cite journal | vauthors = Marsool MD, Prajjwal P, Reddy YB, Marsool AD, Lam JR, Nandwana V | title = Newer modalities in the management of Alzheimer's dementia along with the role of aducanumab and lecanemab in the treatment of its refractory cases | journal = Disease-a-Month | volume = 69 | issue = 5 | pages = 101547 | date = May 2023 | pmid = 36931947 | doi = 10.1016/j.disamonth.2023.101547 | s2cid = 257568052 }}</ref><ref name="FDA PR 20230106">{{cite press release | title=FDA Grants Accelerated Approval for Alzheimer's Disease Treatment | publisher=U.S. ] (FDA) | date=6 January 2023 | url=https://www.fda.gov/news-events/press-announcements/fda-grants-accelerated-approval-alzheimers-disease-treatment | access-date=7 January 2023 | archive-date=7 January 2023 | archive-url=https://web.archive.org/web/20230107000220/https://www.fda.gov/news-events/press-announcements/fda-grants-accelerated-approval-alzheimers-disease-treatment | url-status=live }} {{PD-notice}}</ref><ref>{{cite web |url=https://www.accessdata.fda.gov/drugsatfda_docs/summary_review/2023/761269Orig1s000SumR.pdf |title=Lecanemab Summary Review | publisher = U.S. ] (FDA) |access-date=7 January 2023 |archive-date=7 January 2023 |archive-url=https://web.archive.org/web/20230107005316/https://www.accessdata.fda.gov/drugsatfda_docs/summary_review/2023/761269Orig1s000SumR.pdf |url-status=live }}</ref> and was converted to traditional approval in July 2023, after further testing, along with the addition of a ] about ].<ref name="FDA PR 20230706">{{cite press release |title=FDA Converts Novel Alzheimer's Disease Treatment to Traditional Approval |website=U.S. ] (FDA) |date=6 July 2023 |url=https://www.fda.gov/news-events/press-announcements/fda-converts-novel-alzheimers-disease-treatment-traditional-approval |access-date=6 July 2023}} {{PD-notice}}</ref><ref name="NYT20230706">{{cite news | title=FDA Makes Alzheimer's Drug Leqembi Widely Accessible | website=] | date=6 July 2023 | url=https://www.nytimes.com/2023/07/06/health/alzheimers-leqembi-medicare.html | access-date=8 July 2023 | archive-date=7 July 2023 | archive-url=https://web.archive.org/web/20230707193529/https://www.nytimes.com/2023/07/06/health/alzheimers-leqembi-medicare.html | url-status=live }}</ref> As of early August 2024, lecanemab was approved for sale in Japan, South Korea, China, Hong Kong and Israel although it was recommended against approval by an advisory body of the European Union on July 26, citing its side effects.<ref name=":1" /> | |||
| ], which clears plaques,<ref name=":2" /> was approved by the FDA in July 2024.<ref name="FDA PR 20240702">{{cite press release | title=FDA approves treatment for adults with Alzheimer's disease | website=U.S. ] (FDA) | date=2 July 2024 | url=https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-treatment-adults-alzheimers-disease | access-date=2 July 2024 | archive-date=2 July 2024 | archive-url=https://web.archive.org/web/20240702222134/https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-treatment-adults-alzheimers-disease | url-status=live }}</ref> Anti-amyloid drugs also cause brain shrinkage.<ref>{{cite journal | vauthors = Alves F, Kalinowski P, Ayton S | title = Accelerated Brain Volume Loss Caused by Anti-β-Amyloid Drugs: A Systematic Review and Meta-analysis | journal = Neurology | volume = 100 | issue = 20 | pages = e2114–e2124 | date = May 2023 | pmid = 36973044 | pmc = 10186239 | doi = 10.1212/WNL.0000000000207156 }}</ref> The cholinesterase inhibitor ] was approved by the FDA in July 2024.<ref>{{cite press release | title=Alpha Cognition's Oral Therapy Zunveyl Receives FDA Approval to Treat Alzheimer's Disease | publisher=Alpha Cognition | via=Business Wire | date=29 July 2024 | url=https://www.businesswire.com/news/home/20240729327804/en/ | access-date=4 August 2024}}</ref> | |||
| Specific medications that may reduce the risk or progression of Alzheimer's disease have been studied.<ref name=McDade2021 /> The research trials investigating medications generally impact ] ], inflammation, ], neurotransmitter receptors, neurogenesis, ]s or hormones.<ref name=McDade2021>{{cite journal |vauthors=McDade E, Llibre-Guerra JJ, Holtzman DM, Morris JC, Bateman RJ |title=The informed road map to prevention of Alzheimer Disease: A call to arms |journal=Mol Neurodegener |volume=16 |issue=1 |pages=49 |date=July 2021 |pmid=34289882 |pmc=8293489 |doi=10.1186/s13024-021-00467-y |doi-access=free }}</ref><ref name=Lemche2018>{{cite journal |vauthors=Lemche E |title=Early Life Stress and Epigenetics in Late-onset Alzheimer's Dementia: A Systematic Review |journal=Curr Genomics |volume=19 |issue=7 |pages=522–602 |date=November 2018 |pmid=30386171 |pmc=6194433 |doi=10.2174/1389202919666171229145156}}</ref><ref>{{cite journal |vauthors=Galle SA, Geraedts IK, Deijen JB, Milders MV, Drent ML |title=The Interrelationship between Insulin-Like Growth Factor 1, Apolipoprotein E ε4, Lifestyle Factors, and the Aging Body and Brain |journal=J Prev Alzheimers Dis |volume=7 |issue=4 |pages=265–273 |date=2020 |pmid=32920629 |doi=10.14283/jpad.2020.11 |s2cid=214784366 |doi-access=free | title-link=doi }}</ref> | |||
| ] algorithms with ]s are being studied as a way to predict Alzheimer's disease earlier.<ref>{{cite journal |vauthors = Li Q, Yang X, Xu J, Guo Y, He X, Hu H, Lyu T, Marra D, Miller A, Smith G, DeKosky S, Boyce RD, Schliep K, Shenkman E, Maraganore D, Wu Y, Bian J |date=February 2023 |title=Early prediction of Alzheimer's disease and related dementias using real-world electronic health records |journal=Alzheimer's & Dementia |volume= 19|issue= 8|pages=3506–3518 |doi=10.1002/alz.12967 |pmid=36815661 |s2cid=257101613 |doi-access=free |pmc=10976442 }}</ref> | |||
| === Focused ultrasound for medication delivery === | |||
| In 2024, a new technique of using ] for the delivery of medication past the ] (BBB) is being tested. At the point where the ultrasound beams converge, the focused ultrasound produces several therapeutic effects without incisions or radiation. This can cause opening of the blood-brain barrier (BBB), which may aid in the removal of beta amyloid or tao from the brain.<ref name="Scott 2024">{{cite journal |last1=Scott |first1=Kurt |last2=Klaus |first2=Stephen P. |title=Focused ultrasound therapy for Alzheimer's disease: exploring the potential for targeted amyloid disaggregation |journal=Frontiers in Neurology |date=6 August 2024 |volume=15 |doi=10.3389/fneur.2024.1426075|doi-access=free |pmid=39165269 |pmc=11333319 }}</ref> | |||
| == References == | |||
| {{Reflist}} | |||
| == Further reading == | |||
| {{refbegin}} | |||
| * {{cite journal | vauthors = Van Acker ZP, Perdok A, Bretou M, Annaert W | title = The microglial lysosomal system in Alzheimer's disease: Guardian against proteinopathy | journal = Ageing Research Reviews | volume = 71 | issue = | pages = 101444 | date = November 2021 | pmid = 34391945 | doi = 10.1016/j.arr.2021.101444 | s2cid = 236994329 | url = https://lirias.kuleuven.be/handle/123456789/685536 }} | |||
| * {{cite journal | vauthors = Xi Y, Chen Y, Jin Y, Han G, Song M, Song T, Shi Y, Tao L, Huang Z, Zhou J, Ding Y, Zhang H | title = Versatile nanomaterials for Alzheimer's disease: Pathogenesis inspired disease-modifying therapy | journal = Journal of Controlled Release | volume = 345 | issue = | pages = 38–61 | date = May 2022 | pmid = 35257810 | doi = 10.1016/j.jconrel.2022.02.034 | s2cid = 247285338 }} | |||
| * {{cite journal | vauthors = Prasanalakshmi B, Mousmi A, Syeda M, Anandhavalli M, Linda E | title = Hybridized Deep Learning Approach for Detecting Alzheimer's Disease | journal = Biomedicines | volume = 11 | issue = 4| date = January 2023 | pages = 4–8 | pmid = 9855764 | doi = 10.3390/biomedicines11010149 | doi-access = free | s2cid = 255745038| pmc = 9855764 }} | |||
| {{refend}} | |||
| == External links == | |||
| {{Commons category|Alzheimer's disease}} | |||
| {{Wiktionary|Alzheimer's disease}} | |||
| * {{cite web |title=Alzheimer's Disease Research Timeline – Alzforum |url=http://www.alzforum.org/timeline/alzheimers-disease|website=www.alzforum.org}} | |||
| * {{cite web |title=Alzheimer's Disease Brain Cell Atlas- brain-map.org |url=https://portal.brain-map.org/explore/seattle-alzheimers-disease |website=portal.brain-map.org}} | |||
| {{Medical condition classification and resources | |||
| |DiseasesDB=490 | |||
| |ICD11={{ICD11|8A20}} | |||
| |ICD10={{ICD10|G30}}, {{ICD10|F00}} | |||
| |ICD9={{ICD9|331.0}}, {{ICD9|290.1}} | |||
| |ICDO= | |||
| |Curlie= Health/Conditions_and_Diseases/Neurological_Disorders/Alzheimer's/ | |||
| |OMIM=104300 | |||
| |MedlinePlus=000760 | |||
| |eMedicineSubj=neuro | |||
| |eMedicineTopic=13 | |||
| |MeshID=D000544 | |||
| |GeneReviewsNBK=NBK1161 | |||
| |Scholia=Q11081 | |||
| }} | |||
| {{Mental and behavioural disorders|selected=neurological}} | |||
| {{CNS diseases of the nervous system}} | |||
| {{Amyloidosis}} | |||
| {{Authority control}} | |||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | |||
| ] | |||
| {{Link FA|ro}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 07:07, 26 December 2024
Progressive neurodegenerative disease "Alzheimer" redirects here. For the eponym, see Alois Alzheimer. For other uses, see Alzheimer (disambiguation).Medical condition
| Alzheimer's disease | |
|---|---|
| Other names | Alzheimer's dementia |
 | |
| Diagram of a normal brain compared to the brain of a person with Alzheimer's | |
| Pronunciation |
|
| Specialty | Neurology |
| Symptoms | Memory loss, problems with language, disorientation, mood swings |
| Complications | Infections, falls and aspiration pneumonia in the terminal stage |
| Usual onset | Over 65 years old |
| Duration | Long term |
| Causes | Poorly understood |
| Risk factors | Genetics, head injuries, clinical depression, hypertension, psychological stress, lack of physical and mental exercise |
| Diagnostic method | Based on symptoms and cognitive testing after ruling out other possible causes |
| Differential diagnosis | Normal brain aging, Lewy body dementia, Trisomy 21 |
| Medication | Acetylcholinesterase inhibitors, NMDA receptor antagonists |
| Prognosis | Life expectancy 3–12 years |
| Frequency | 50 million (2020) |
| Named after | Alois Alzheimer |
Alzheimer's disease (AD) is a neurodegenerative disease that usually starts slowly and progressively worsens. It is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with language, disorientation (including easily getting lost), mood swings, loss of motivation, self-neglect, and behavioral issues. As a person's condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to twelve years.
The causes of Alzheimer's disease remain poorly understood. There are many environmental and genetic risk factors associated with its development. The strongest genetic risk factor is from an allele of apolipoprotein E. Other risk factors include a history of head injury, clinical depression, and high blood pressure. The progression of the disease is largely characterized by the accumulation of malformed protein deposits in the cerebral cortex, called amyloid plaques and neurofibrillary tangles. These misfolded protein aggregates interfere with normal cell function, and over time lead to irreversible degeneration of neurons and loss of synaptic connections in the brain. A probable diagnosis is based on the history of the illness and cognitive testing, with medical imaging and blood tests to rule out other possible causes. Initial symptoms are often mistaken for normal brain aging. Examination of brain tissue is needed for a definite diagnosis, but this can only take place after death.
No treatments can stop or reverse its progression, though some may temporarily improve symptoms. A healthy diet, physical activity, and social engagement are generally beneficial in aging, and may help in reducing the risk of cognitive decline and Alzheimer's. Affected people become increasingly reliant on others for assistance, often placing a burden on caregivers. The pressures can include social, psychological, physical, and economic elements. Exercise programs may be beneficial with respect to activities of daily living and can potentially improve outcomes. Behavioral problems or psychosis due to dementia are sometimes treated with antipsychotics, but this has an increased risk of early death.
As of 2020, there were approximately 50 million people worldwide with Alzheimer's disease. It most often begins in people over 65 years of age, although up to 10% of cases are early-onset impacting those in their 30s to mid-60s. It affects about 6% of people 65 years and older, and women more often than men. The disease is named after German psychiatrist and pathologist Alois Alzheimer, who first described it in 1906. Alzheimer's financial burden on society is large, with an estimated global annual cost of US$1 trillion. It is ranked as the seventh leading cause of death worldwide.
Given the widespread impacts of Alzheimer's disease, both basic-science and health funders in many countries support Alzheimer's research at large scales. For example, the US National Institutes of Health program for Alzheimer's research, the National Plan to Address Alzheimer’s Disease, has a budget of US$3.98 billion for fiscal year 2026. In the European Union, the 2020 Horizon Europe research programme awarded over €570 million for dementia-related projects.
Signs and symptoms
The course of Alzheimer's is generally described in three stages, with a progressive pattern of cognitive and functional impairment. The three stages are described as early or mild, middle or moderate, and late or severe. The disease is known to target the hippocampus which is associated with memory, and this is responsible for the first symptoms of memory impairment. As the disease progresses so does the degree of memory impairment.
First symptoms

The first symptoms are often mistakenly attributed to aging or stress. Detailed neuropsychological testing can reveal mild cognitive difficulties up to eight years before a person fulfills the clinical criteria for diagnosis of Alzheimer's disease. These early symptoms can affect the most complex activities of daily living. The most noticeable deficit is short term memory loss, which shows up as difficulty in remembering recently learned facts and inability to acquire new information.
Subtle problems with the executive functions of attentiveness, planning, flexibility, and abstract thinking, or impairments in semantic memory (memory of meanings, and concept relationships) can also be symptomatic of the early stages of Alzheimer's disease. Apathy and depression can be seen at this stage, with apathy remaining as the most persistent symptom throughout the course of the disease. People with objective signs of cognitive impairment, but not more severe symptoms, may be diagnosed with mild cognitive impairment (MCI). If memory loss is the predominant symptom of MCI, it is termed amnestic MCI and is frequently seen as a prodromal or early stage of Alzheimer's disease. Amnestic MCI has a greater than 90% likelihood of being associated with Alzheimer's.
Early stage
In people with Alzheimer's disease, the increasing impairment of learning and memory eventually leads to a definitive diagnosis. In a small percentage, difficulties with language, executive functions, perception (agnosia), or execution of movements (apraxia) are more prominent than memory problems. Alzheimer's disease does not affect all memory capacities equally. Older memories of the person's life (episodic memory), facts learned (semantic memory), and implicit memory (the memory of the body on how to do things, such as using a fork to eat or how to drink from a glass) are affected to a lesser degree than new facts or memories.
Language problems are mainly characterised by a shrinking vocabulary and decreased word fluency, leading to a general impoverishment of oral and written language. In this stage, the person with Alzheimer's is usually capable of communicating basic ideas adequately. While performing fine motor tasks such as writing, drawing, or dressing, certain movement coordination and planning difficulties (apraxia) may be present; however, they are commonly unnoticed. As the disease progresses, people with Alzheimer's disease can often continue to perform many tasks independently; however, they may need assistance or supervision with the most cognitively demanding activities.
Middle stage
Progressive deterioration eventually hinders independence, with subjects being unable to perform most common activities of daily living. Speech difficulties become evident due to an inability to recall vocabulary, which leads to frequent incorrect word substitutions (paraphasias). Reading and writing skills are also progressively lost. Complex motor sequences become less coordinated as time passes and Alzheimer's disease progresses, so the risk of falling increases. During this phase, memory problems worsen, and the person may fail to recognise close relatives. Long-term memory, which was previously intact, becomes impaired.
Behavioral and neuropsychiatric changes become more prevalent. Common manifestations are wandering, irritability and emotional lability, leading to crying, outbursts of unpremeditated aggression, or resistance to caregiving. Sundowning can also appear. Approximately 30% of people with Alzheimer's disease develop illusionary misidentifications and other delusional symptoms. Subjects also lose insight of their disease process and limitations (anosognosia). Urinary incontinence can develop. These symptoms create stress for relatives and caregivers, which can be reduced by moving the person from home care to other long-term care facilities.
Late stage

During the final stage, known as the late-stage or severe stage, there is complete dependence on caregivers. Language is reduced to simple phrases or even single words, eventually leading to complete loss of speech. Despite the loss of verbal language abilities, people can often understand and return emotional signals. Although aggressiveness can still be present, extreme apathy and exhaustion are much more common symptoms. People with Alzheimer's disease will ultimately not be able to perform even the simplest tasks independently; muscle mass and mobility deteriorates to the point where they are bedridden and unable to feed themselves. The cause of death is usually an external factor, such as infection of pressure ulcers or pneumonia, not the disease itself. In some cases, there is a paradoxical lucidity immediately before death, where there is an unexpected recovery of mental clarity.
Causes
Alzheimer's disease is believed to occur when abnormal amounts of amyloid beta (Aβ), accumulating extracellularly as amyloid plaques and tau proteins, or intracellularly as neurofibrillary tangles, form in the brain, affecting neuronal functioning and connectivity, resulting in a progressive loss of brain function. This altered protein clearance ability is age-related, regulated by brain cholesterol, and associated with other neurodegenerative diseases.
The cause for most Alzheimer's cases is still mostly unknown, except for 1–2% of cases where deterministic genetic differences have been identified. Several competing hypotheses attempt to explain the underlying cause; the most predominant hypothesis is the amyloid beta (Aβ) hypothesis.
The oldest hypothesis, on which most drug therapies are based, is the cholinergic hypothesis, which proposes that Alzheimer's disease is caused by reduced synthesis of the neurotransmitter acetylcholine. The loss of cholinergic neurons noted in the limbic system and cerebral cortex, is a key feature in the progression of Alzheimer's. The 1991 amyloid hypothesis postulated that extracellular amyloid beta (Aβ) deposits are the fundamental cause of the disease. Support for this postulate comes from the location of the gene for the amyloid precursor protein (APP) on chromosome 21, together with the fact that people with trisomy 21 (Down syndrome) who have an extra gene copy almost universally exhibit at least the earliest symptoms of Alzheimer's disease by 40 years of age. A specific isoform of apolipoprotein, APOE4, is a major genetic risk factor for Alzheimer's disease. While apolipoproteins enhance the breakdown of beta amyloid, some isoforms are not very effective at this task (such as APOE4), leading to excess amyloid buildup in the brain.
Genetic
Late onset
Late-onset Alzheimer's is about 70% heritable. Genetic models in 2020 predict Alzheimer's disease with 90% accuracy. Most cases of Alzheimer's are not familial, and so they are termed sporadic Alzheimer's disease. Of the cases of sporadic Alzheimer's disease, most are classified as late onset where they are developed after the age of 65 years.
The strongest genetic risk factor for sporadic Alzheimer's disease is APOEε4. APOEε4 is one of four alleles of apolipoprotein E (APOE). APOE plays a major role in lipid-binding proteins in lipoprotein particles and the ε4 allele disrupts this function. Between 40% and 80% of people with Alzheimer's disease possess at least one APOEε4 allele. The APOEε4 allele increases the risk of the disease by three times in heterozygotes and by 15 times in homozygotes. Like many human diseases, environmental effects and genetic modifiers result in incomplete penetrance. For example, Nigerian Yoruba people do not show the relationship between dose of APOEε4 and incidence or age-of-onset for Alzheimer's disease seen in other human populations.
Early onset
Further information: Early-onset Alzheimer's diseaseOnly 1–2% of Alzheimer's cases are inherited due to autosomal dominant effects, as Alzheimer's is highly polygenic. When the disease is caused by autosomal dominant variants, it is known as early onset familial Alzheimer's disease, which is rarer and has a faster rate of progression. Less than 5% of sporadic Alzheimer's disease have an earlier onset, and early-onset Alzheimer's is about 90% heritable. Familial Alzheimer's disease usually implies two or more persons affected in one or more generations.
Early onset familial Alzheimer's disease can be attributed to mutations in one of three genes: those encoding amyloid-beta precursor protein (APP) and presenilins PSEN1 and PSEN2. Most mutations in the APP and presenilin genes increase the production of a small protein called amyloid beta (Aβ)42, which is the main component of amyloid plaques. Some of the mutations merely alter the ratio between Aβ42 and the other major forms—particularly Aβ40—without increasing Aβ42 levels in the brain. Two other genes associated with autosomal dominant Alzheimer's disease are ABCA7 and SORL1.
Alleles in the TREM2 gene have been associated with a three to five times higher risk of developing Alzheimer's disease.
A Japanese pedigree of familial Alzheimer's disease was found to be associated with a deletion mutation of codon 693 of APP. This mutation and its association with Alzheimer's disease was first reported in 2008, and is known as the Osaka mutation. Only homozygotes with this mutation have an increased risk of developing Alzheimer's disease. This mutation accelerates Aβ oligomerization but the proteins do not form the amyloid fibrils that aggregate into amyloid plaques, suggesting that it is the Aβ oligomerization rather than the fibrils that may be the cause of this disease. Mice expressing this mutation have all the usual pathologies of Alzheimer's disease.
Hypotheses
Amyloid beta and tau protein

The tau hypothesis proposes that tau protein abnormalities initiate the disease cascade. In this model, hyperphosphorylated tau begins to pair with other threads of tau as paired helical filaments. Eventually, they form neurofibrillary tangles inside neurons. When this occurs, the microtubules disintegrate, destroying the structure of the cell's cytoskeleton which collapses the neuron's transport system.
A number of studies connect the misfolded amyloid beta and tau proteins associated with the pathology of Alzheimer's disease, as bringing about oxidative stress that leads to neuroinflammation. This chronic inflammation is also a feature of other neurodegenerative diseases including Parkinson's disease, and ALS. Spirochete infections have also been linked to dementia. DNA damages accumulate in Alzheimer's diseased brains; reactive oxygen species may be the major source of this DNA damage.
Sleep
Sleep disturbances are seen as a possible risk factor for inflammation in Alzheimer's disease. Sleep disruption was previously only seen as a consequence of Alzheimer's disease, but as of 2020, accumulating evidence suggests that this relationship may be bidirectional.
Metal toxicity, smoking, neuroinflammation and air pollution
The cellular homeostasis of biometals such as ionic copper, iron, and zinc is disrupted in Alzheimer's disease, though it remains unclear whether this is produced by or causes the changes in proteins. Smoking is a significant Alzheimer's disease risk factor. Systemic markers of the innate immune system are risk factors for late-onset Alzheimer's disease. Exposure to air pollution may be a contributing factor to the development of Alzheimer's disease.
Age-related myelin decline
Retrogenesis is a medical hypothesis that just as the fetus goes through a process of neurodevelopment beginning with neurulation and ending with myelination, the brains of people with Alzheimer's disease go through a reverse neurodegeneration process starting with demyelination and death of axons (white matter) and ending with the death of grey matter. Likewise the hypothesis is, that as infants go through states of cognitive development, people with Alzheimer's disease go through the reverse process of progressive cognitive impairment.
According to one theory, dysfunction of oligodendrocytes and their associated myelin during aging contributes to axon damage, which in turn generates in amyloid production and tau hyperphosphorylation. An in vivo study employing genetic mouse models to simulate myelin dysfunction and amyloidosis further reveal that age-related myelin degradation increases sites of Aβ production and distracts microglia from Aβ plaques, with both mechanisms dually exacerbating amyloidosis. Additionally, comorbidities between the demyelinating disease, multiple sclerosis, and Alzheimer's disease have been reported.
Other hypotheses
See also: Cell cycle hypothesis of Alzheimer's disease and Ion channel hypothesis of Alzheimer's disease
The association with celiac disease is unclear, with a 2019 study finding no increase in dementia overall in those with celiac disease while a 2018 review found an association with several types of dementia including Alzheimer's disease.
Studies have shown a potential link between infection with certain viruses and developing Alzheimer's disease later in life. Notably, a large scale study conducted on 6,245,282 patients has shown an increased risk of developing Alzheimer's disease following COVID-19 infection in cognitively normal individuals over 65.
Pathophysiology
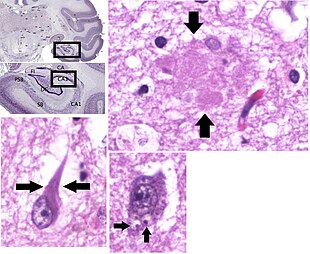
Neuropathology
Alzheimer's disease is characterised by loss of neurons and synapses in the cerebral cortex and certain subcortical regions. This loss results in gross atrophy of the affected regions, including degeneration in the temporal lobe and parietal lobe, and parts of the frontal cortex and cingulate gyrus. Degeneration is also present in brainstem nuclei particularly the locus coeruleus in the pons. Studies using MRI and PET have documented reductions in the size of specific brain regions in people with Alzheimer's disease as they progressed from mild cognitive impairment to Alzheimer's disease, and in comparison with similar images from healthy older adults.
Both Aβ plaques and neurofibrillary tangles are clearly visible by microscopy in brains of those with Alzheimer's disease, especially in the hippocampus. However, Alzheimer's disease may occur without neurofibrillary tangles in the neocortex. Plaques are dense, mostly insoluble deposits of beta-amyloid peptide and cellular material outside and around neurons. Neurofibrillary tangles are aggregates of the microtubule-associated protein tau which has become hyperphosphorylated and accumulate inside the cells themselves. Although many older individuals develop some plaques and tangles as a consequence of aging, the brains of people with Alzheimer's disease have a greater number of them in specific brain regions such as the temporal lobe. Lewy bodies are not rare in the brains of people with Alzheimer's disease.
Biochemistry
Main article: Biochemistry of Alzheimer's diseaseAmyloid beta


 Enzymes act on the amyloid-beta precursor protein and cut it into fragments. The beta-amyloid fragment is crucial in the formation of amyloid plaques in Alzheimer's disease.
Enzymes act on the amyloid-beta precursor protein and cut it into fragments. The beta-amyloid fragment is crucial in the formation of amyloid plaques in Alzheimer's disease.
Alzheimer's disease has been identified as a protein misfolding disease, a proteopathy, caused by the accumulation of abnormally folded amyloid beta protein into amyloid plaques, and tau protein into neurofibrillary tangles in the brain. Plaques are made up of small peptides, 39–43 amino acids in length, called amyloid beta. Amyloid beta is a fragment from the larger amyloid-beta precursor protein (APP) a transmembrane protein that penetrates the cell's membrane. APP is critical to neuron growth, survival, and post-injury repair. In Alzheimer's disease, gamma secretase and beta secretase act together in a proteolytic process which causes APP to be divided into smaller fragments. Although commonly researched as neuronal proteins, APP and its processing enzymes are abundantly expressed by other brain cells. One of these fragments gives rise to fibrils of amyloid beta, which then form clumps that deposit outside neurons in dense formations known as amyloid plaques. Excitatory neurons are known to be the major producers of amyloid beta that contribute to major extracellular plaque deposition.
Phosphorylated tau
Alzheimer's disease is also considered a tauopathy due to abnormal aggregation of the tau protein. Every neuron has a cytoskeleton, an internal support structure partly made up of structures called microtubules. These microtubules act like tracks, guiding nutrients and molecules from the body of the cell to the ends of the axon and back. A protein called tau stabilises the microtubules when phosphorylated, and is therefore called a microtubule-associated protein. In Alzheimer's disease, tau undergoes chemical changes, becoming hyperphosphorylated; it then begins to pair with other threads, creating neurofibrillary tangles and disintegrating the neuron's transport system. Pathogenic tau can also cause neuronal death through transposable element dysregulation. Necroptosis has also been reported as a mechanism of cell death in brain cells affected with tau tangles.
Disease mechanism
Exactly how disturbances of production and aggregation of the beta-amyloid peptide give rise to the pathology of Alzheimer's disease is not known. The amyloid hypothesis traditionally points to the accumulation of beta-amyloid peptides as the central event triggering neuron degeneration. Accumulation of aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis, induces programmed cell death (apoptosis). It is also known that Aβ selectively builds up in the mitochondria in the cells of Alzheimer's-affected brains, and it also inhibits certain enzyme functions and the utilisation of glucose by neurons.
Iron dyshomeostasis is linked to disease progression, an iron-dependent form of regulated cell death called ferroptosis could be involved. Products of lipid peroxidation are also elevated in AD brain compared with controls.
Various inflammatory processes and cytokines may also have a role in the pathology of Alzheimer's disease. Inflammation is a general marker of tissue damage in any disease, and may be either secondary to tissue damage in Alzheimer's disease or a marker of an immunological response. There is increasing evidence of a strong interaction between the neurons and the immunological mechanisms in the brain. Obesity and systemic inflammation may interfere with immunological processes which promote disease progression.
Alterations in the distribution of different neurotrophic factors and in the expression of their receptors such as the brain-derived neurotrophic factor (BDNF) have been described in Alzheimer's disease.
Diagnosis
See also: Early-onset Alzheimer's disease § Diagnosis
Alzheimer's disease (AD) can only be definitively diagnosed with autopsy findings; in the absence of autopsy, clinical diagnoses of AD are "possible" or "probable", based on other findings. Up to 23% of those clinically diagnosed with AD may be misdiagnosed and may have pathology suggestive of another condition with symptoms that mimic those of AD.
AD is usually clinically diagnosed based on a person's medical history, observations from friends or relatives, and behavioral changes. The presence of characteristic neuropsychological changes with impairments in at least two cognitive domains that are severe enough to affect a person's functional abilities are required for the diagnosis. Domains that may be impaired include memory (most commonly impaired), language, executive function, visuospatial functioning, or other areas of cognition. The neurocognitive changes must be a decline from a prior level of function and the diagnosis requires ruling out other common causes of neurocognitive decline. Advanced medical imaging with computed tomography (CT) or magnetic resonance imaging (MRI), and with single-photon emission computed tomography (SPECT) or positron emission tomography (PET), can be used to help exclude other cerebral pathology or subtypes of dementia. On MRI or CT, Alzheimer's disease usually shows a generalized or focal cortical atrophy, which may be asymmetric. Atrophy of the hippocampus is also commonly seen. Brain imaging commonly also shows cerebrovascular disease, most commonly previous strokes (small or large territory strokes), and this is thought to be a contributing cause of many cases of dementia (up to 46% cases of dementia also have cerebrovascular disease on imaging). FDG-PET scan is not required for the diagnosis but it is sometimes used when standard testing is unclear. FDG-PET shows a bilateral, asymetric, temporal and parietal reduced activity. Advanced imaging may predict conversion from prodromal stages (mild cognitive impairment) to Alzheimer's disease. FDA-approved radiopharmaceutical diagnostic agents used in PET for Alzheimer's disease are florbetapir (2012), flutemetamol (2013), florbetaben (2014), and flortaucipir (2020). Because many insurance companies in the United States do not cover this procedure, its use in clinical practice is largely limited to clinical trials as of 2018.
Assessment of intellectual functioning including memory testing can further characterise the state of the disease. Medical organizations have created diagnostic criteria to ease and standardise the diagnostic process for practising physicians. Definitive diagnosis can only be confirmed with post-mortem evaluations when brain material is available and can be examined histologically for senile plaques and neurofibrillary tangles.
Criteria
There are three sets of criteria for the clinical diagnoses of the spectrum of Alzheimer's disease: the 2013 fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5); the National Institute on Aging-Alzheimer's Association (NIA-AA) definition as revised in 2011; and the International Working Group criteria as revised in 2010.
Eight intellectual domains are most commonly impaired in AD—memory, language, perceptual skills, attention, motor skills, orientation, problem solving and executive functional abilities, as listed in the fourth text revision of the DSM (DSM-IV-TR).
The DSM-5 defines criteria for probable or possible AD for both major and mild neurocognitive disorder. Major or mild neurocognitive disorder must be present along with at least one cognitive deficit for a diagnosis of either probable or possible AD. For major neurocognitive disorder due to AD, probable Alzheimer's disease can be diagnosed if the individual has genetic evidence of AD or if two or more acquired cognitive deficits, and a functional disability that is not from another disorder, are present. Otherwise, possible AD can be diagnosed as the diagnosis follows an atypical route. For mild neurocognitive disorder due to AD, probable Alzheimer's disease can be diagnosed if there is genetic evidence, whereas possible AD can be met if all of the following are present: no genetic evidence, decline in both learning and memory, two or more cognitive deficits, and a functional disability not from another disorder.
The NIA-AA criteria are used mainly in research rather than in clinical assessments. They define AD through three major stages: preclinical, mild cognitive impairment (MCI), and Alzheimer's dementia. Diagnosis in the preclinical stage is complex and focuses on asymptomatic individuals; the latter two stages describe individuals experiencing symptoms, along with biomarkers, predominantly those for neuronal injury (mainly tau-related) and amyloid beta deposition. The core clinical criteria itself rests on the presence of cognitive impairment without the presence of comorbidities. The third stage is divided into probable and possible AD dementia. In probable AD dementia there is steady impairment of cognition over time and a memory-related or non-memory-related cognitive dysfunction. In possible AD dementia, another causal disease such as cerebrovascular disease is present.
Techniques

Neuropsychological tests including cognitive tests such as the mini–mental state examination (MMSE), the Montreal Cognitive Assessment (MoCA) and the Mini-Cog are widely used to aid in diagnosis of the cognitive impairments in AD. These tests may not always be accurate, as they lack sensitivity to mild cognitive impairment, and can be biased by language or attention problems; more comprehensive test arrays are necessary for high reliability of results, particularly in the earliest stages of the disease.
Further neurological examinations are crucial in the differential diagnosis of Alzheimer's disease and other diseases. Interviews with family members are used in assessment; caregivers can supply important information on daily living abilities and on the decrease in the person's mental function. A caregiver's viewpoint is particularly important, since a person with Alzheimer's disease is commonly unaware of their deficits. Many times, families have difficulties in the detection of initial dementia symptoms and may not communicate accurate information to a physician.
Supplemental testing can rule out other potentially treatable diagnoses and help avoid misdiagnoses. Common supplemental tests include blood tests, thyroid function tests, as well as tests to assess vitamin B12 levels, rule out neurosyphilis and rule out metabolic problems (including tests for kidney function, electrolyte levels and for diabetes). MRI or CT scans might also be used to rule out other potential causes of the symptoms – including tumors or strokes. Delirium and depression can be common among individuals and are important to rule out.
Psychological tests for depression are used, since depression can either be concurrent with AD (see Depression of Alzheimer disease), an early sign of cognitive impairment, or even the cause.
Due to low accuracy, the C-PIB-PET scan is not recommended as an early diagnostic tool or for predicting the development of AD when people show signs of mild cognitive impairment (MCI). The use of F-FDG PET scans, as a single test, to identify people who may develop Alzheimer's disease is not supported by evidence.
Prevention
There are no disease-modifying treatments available to cure Alzheimer's disease and because of this, AD research has focused on interventions to prevent the onset and progression. There is no evidence that supports any particular measure in preventing AD, and studies of measures to prevent the onset or progression have produced inconsistent results. Epidemiological studies have proposed relationships between an individual's likelihood of developing AD and modifiable factors, such as medications, lifestyle, and diet. There are some challenges in determining whether interventions for AD act as a primary prevention method, preventing the disease itself, or a secondary prevention method, identifying the early stages of the disease. These challenges include duration of intervention, different stages of disease at which intervention begins, and lack of standardization of inclusion criteria regarding biomarkers specific for AD. Further research is needed to determine factors that can help prevent AD.
Medication
Cardiovascular risk factors, such as hypercholesterolaemia, hypertension, diabetes, and smoking, are associated with a higher risk of onset and worsened course of AD. The use of statins to lower cholesterol may be of benefit in AD. Antihypertensive and antidiabetic medications in individuals without overt cognitive impairment may decrease the risk of dementia by influencing cerebrovascular pathology. More research is needed to examine the relationship with AD specifically; clarification of the direct role medications play versus other concurrent lifestyle changes (diet, exercise, smoking) is needed.
Depression is associated with an increased risk for AD; management with antidepressant medications may provide a preventative measure.
Historically, long-term usage of non-steroidal anti-inflammatory drugs (NSAIDs) were thought to be associated with a reduced likelihood of developing AD as it reduces inflammation, but NSAIDs do not appear to be useful as a treatment. Additionally, because women have a higher incidence of AD than men, it was once thought that estrogen deficiency during menopause was a risk factor, but there is a lack of evidence to show that hormone replacement therapy (HRT) in menopause decreases risk of cognitive decline.
Lifestyle
Further information: Neurobiological effects of physical exerciseCertain lifestyle activities, such as physical and cognitive exercises, higher education and occupational attainment, cigarette smoking, stress, sleep, and the management of other comorbidities, including diabetes and hypertension, may affect the risk of developing AD.
Physical exercise is associated with a decreased rate of dementia, and is effective in reducing symptom severity in those with AD. Memory and cognitive functions can be improved with aerobic exercises including brisk walking three times weekly for forty minutes. It may also induce neuroplasticity of the brain. Participating in mental exercises, such as reading, crossword puzzles, and chess have shown potential to be preventive. Meeting the WHO recommendations for physical activity is associated with a lower risk of AD.
Higher education and occupational attainment, and participation in leisure activities, contribute to a reduced risk of developing AD, or of delaying the onset of symptoms. This is compatible with the cognitive reserve theory, which states that some life experiences result in more efficient neural functioning providing the individual a cognitive reserve that delays the onset of dementia manifestations. Education delays the onset of Alzheimer's disease syndrome without changing the duration of the disease.
Cessation in smoking may reduce risk of developing AD, specifically in those who carry the APOE ɛ4 allele. The increased oxidative stress caused by smoking results in downstream inflammatory or neurodegenerative processes that may increase risk of developing AD. Avoidance of smoking, counseling and pharmacotherapies to quit smoking are used, and avoidance of environmental tobacco smoke is recommended.
Alzheimer's disease is associated with sleep disorders but the precise relationship is unclear. It was once thought that as people get older, the risk of developing sleep disorders and AD independently increase, but research is examining whether sleep disorders may increase the prevalence of AD. One theory is that the mechanisms to increase clearance of toxic substances, including Aβ, are active during sleep. With decreased sleep, a person is increasing Aβ production and decreasing Aβ clearance, resulting in Aβ accumulation. Receiving adequate sleep (approximately 7–8 hours) every night has become a potential lifestyle intervention to prevent the development of AD.
Stress is a risk factor for the development of AD. The mechanism by which stress predisposes someone to development of AD is unclear, but it is suggested that lifetime stressors may affect a person's epigenome, leading to an overexpression or under expression of specific genes. Although the relationship of stress and AD is unclear, strategies to reduce stress and relax the mind may be helpful strategies in preventing the progression or Alzheimer's disease. Meditation, for instance, is a helpful lifestyle change to support cognition and well-being, though further research is needed to assess long-term effects.
Management
There is no cure for AD; available treatments offer relatively small symptomatic benefits but remain palliative in nature. Treatments can be divided into pharmaceutical, psychosocial, and caregiving.
Pharmaceutical


Medications used to treat the cognitive symptoms of AD rather than the underlying cause include: four acetylcholinesterase inhibitors (tacrine, rivastigmine, galantamine, and donepezil) and memantine, an NMDA receptor antagonist. The acetylcholinesterase inhibitors are intended for those with mild to severe AD, whereas memantine is intended for those with moderate or severe Alzheimer's disease. The benefit from their use is small.
Reduction in the activity of the cholinergic neurons is a well-known feature of AD. Acetylcholinesterase inhibitors are employed to reduce the rate at which acetylcholine (ACh) is broken down, thereby increasing the concentration of ACh in the brain and combating the loss of ACh caused by the death of cholinergic neurons. There is evidence for the efficacy of these medications in mild to moderate AD, and some evidence for their use in the advanced stage. The use of these drugs in mild cognitive impairment has not shown any effect in a delay of the onset of Alzheimer's disease. The most common side effects are nausea and vomiting, both of which are linked to cholinergic excess. These side effects arise in approximately 10–20% of users, are mild to moderate in severity, and can be managed by slowly adjusting medication doses. Less common secondary effects include muscle cramps, decreased heart rate (bradycardia), decreased appetite and weight, and increased gastric acid production.
Glutamate is an excitatory neurotransmitter of the nervous system, although excessive amounts in the brain can lead to cell death through a process called excitotoxicity which consists of the overstimulation of glutamate receptors. Excitotoxicity occurs not only in AD, but also in other neurological diseases such as Parkinson's disease and multiple sclerosis. Memantine is a noncompetitive NMDA receptor antagonist first used as an anti-influenza agent. It acts on the glutamatergic system by blocking NMDA receptors and inhibiting their overstimulation by glutamate. Memantine has been shown to have a small benefit in the treatment of moderate to severe AD. Reported adverse events with memantine are infrequent and mild, including hallucinations, confusion, dizziness, headache and fatigue. The combination of memantine and donepezil has been shown to be "of statistically significant but clinically marginal effectiveness".
An extract of Ginkgo biloba known as EGb 761 has been used for treating AD and other neuropsychiatric disorders. Its use is approved throughout Europe. The World Federation of Biological Psychiatry guidelines lists EGb 761 with the same weight of evidence (level B) given to acetylcholinesterase inhibitors and memantine. EGb 761 is the only one that showed improvement of symptoms in both AD and vascular dementia. EGb 761 may have a role either on its own or as an add-on if other therapies prove ineffective. A 2016 review concluded that the quality of evidence from clinical trials on Ginkgo biloba has been insufficient to warrant its use for treating AD.
Atypical antipsychotics are modestly useful in reducing aggression and psychosis in people with AD, but their advantages are offset by serious adverse effects, such as stroke, movement difficulties or cognitive decline. When used in the long-term, they have been shown to associate with increased mortality. They are recommended in dementia only after first line therapies such as behavior modification have failed, and due to the risk of adverse effects, they should be used for the shortest amount of time possible. Stopping antipsychotic use in this group of people appears to be safe.
Psychosocial
Psychosocial interventions are used as an adjunct to pharmaceutical treatment and can be classified within behavior-, emotion-, cognition- or stimulation-oriented approaches.
Behavioral interventions attempt to identify and reduce the antecedents and consequences of problem behaviors. This approach has not shown success in improving overall functioning, but can help to reduce some specific problem behaviors, such as incontinence. There is a lack of high quality data on the effectiveness of these techniques in other behavior problems such as wandering. Music therapy is effective in reducing behavioral and psychological symptoms.
Emotion-oriented interventions include reminiscence therapy, validation therapy, supportive psychotherapy, sensory integration, also called snoezelen, and simulated presence therapy. A Cochrane review has found no evidence that this is effective. Reminiscence therapy (RT) involves the discussion of past experiences individually or in group, many times with the aid of photographs, household items, music and sound recordings, or other familiar items from the past. A 2018 review of the effectiveness of RT found that effects were inconsistent, small in size and of doubtful clinical significance, and varied by setting. Simulated presence therapy (SPT) is based on attachment theories and involves playing a recording with voices of the closest relatives of the person with AD. There is partial evidence indicating that SPT may reduce challenging behaviors.
The aim of cognition-oriented treatments, which include reality orientation and cognitive retraining, is the reduction of cognitive deficits. Reality orientation consists of the presentation of information about time, place, or person to ease the understanding of the person about its surroundings and his or her place in them. On the other hand, cognitive retraining tries to improve impaired capacities by exercising mental abilities. Both have shown some efficacy improving cognitive capacities.
Stimulation-oriented treatments include art, music and pet therapies, exercise, and any other kind of recreational activities. Stimulation has modest support for improving behavior, mood, and, to a lesser extent, function. Nevertheless, as important as these effects are, the main support for the use of stimulation therapies is the change in the person's routine.
Caregiving
Further information: Caring for people with dementia and Palliative careSince AD has no cure and it gradually renders people incapable of tending to their own needs, caregiving is essentially the treatment and must be carefully managed over the course of the disease.
During the early and moderate stages, modifications to the living environment and lifestyle can increase safety and reduce caretaker burden. Examples of such modifications are the adherence to simplified routines, the placing of safety locks, the labeling of household items to cue the person with the disease or the use of modified daily life objects. If eating becomes problematic, food will need to be prepared in smaller pieces or even puréed. When swallowing difficulties arise, the use of feeding tubes may be required. In such cases, the medical efficacy and ethics of continuing feeding is an important consideration of the caregivers and family members. The use of physical restraints is rarely indicated in any stage of the disease, although there are situations when they are necessary to prevent harm to the person with Alzheimer's disease or their caregivers.
During the final stages of the disease, treatment is centred on relieving discomfort until death, often with the help of hospice.
Diet
Diet may be a modifiable risk factor for the development of Alzheimer's disease. The Mediterranean diet, and the DASH diet are both associated with less cognitive decline. A different approach has been to incorporate elements of both of these diets into one known as the MIND diet. Studies of individual dietary components, minerals and supplements are conflicting as to whether they reduce AD risk or cognitive decline. Preliminary research indicates that abnormal eating behaviors and dietary changes are common in people with dementia, especially in later stages.
Prognosis
The early stages of AD are difficult to diagnose. A definitive diagnosis is usually made once cognitive impairment compromises daily living activities, although the person may still be living independently. The symptoms will progress from mild cognitive problems, such as memory loss through increasing stages of cognitive and non-cognitive disturbances, eliminating any possibility of independent living, especially in the late stages of the disease.
Life expectancy of people with AD is reduced. The normal life expectancy for 60 to 70 years old is 23 to 15 years; for 90 years old it is 4.5 years. Following AD diagnosis it ranges from 7 to 10 years for those in their 60s and early 70s (a loss of 13 to 8 years), to only about 3 years or less (a loss of 1.5 years) for those in their 90s.
Fewer than 3% of people live more than fourteen years after diagnosis. Disease features significantly associated with reduced survival are an increased severity of cognitive impairment, decreased functional level, disturbances in the neurological examination, history of falls, malnutrition, dehydration and weight loss. Other coincident diseases such as heart problems, diabetes, or history of alcohol abuse are also related with shortened survival. While the earlier the age at onset the higher the total survival years, life expectancy is particularly reduced when compared to the healthy population among those who are younger. Men have a less favourable survival prognosis than women.
Aspiration pneumonia is the most frequent immediate cause of death brought by AD. While the reasons behind the lower prevalence of cancer in AD patients remain unclear, some researchers hypothesize that biological mechanisms shared by both diseases might play a role. However, this requires further investigation.
Epidemiology
See also: Alzheimer's disease in African Americans and Alzheimer's Disease in the East Asian PopulationTwo main measures are used in epidemiological studies: incidence and prevalence. Incidence is the number of new cases per unit of person-time at risk (usually number of new cases per thousand person-years); while prevalence is the total number of cases of the disease in the population at any given time.
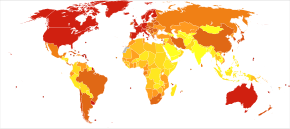
Regarding incidence, cohort longitudinal studies (studies where a disease-free population is followed over the years) provide rates between 10 and 15 per thousand person-years for all dementias and 5–8 for AD, which means that half of new dementia cases each year are Alzheimer's disease. Advancing age is a primary risk factor for the disease and incidence rates are not equal for all ages: every 5 years after the age of 65, the risk of acquiring the disease approximately doubles, increasing from 3 to as much as 69 per thousand person years. Females with AD are more common than males, but this difference is likely due to women's longer life spans. When adjusted for age, both sexes are affected by Alzheimer's at equal rates. In the United States, the risk of dying from AD in 2010 was 26% higher among the non-Hispanic white population than among the non-Hispanic black population, and the Hispanic population had a 30% lower risk than the non-Hispanic white population. However, much AD research remains to be done in minority groups, such as the African American, East Asian and Hispanic/Latino populations. Studies have shown that these groups are underrepresented in clinical trials and do not have the same risk of developing AD when carrying certain genetic risk factors (i.e. APOE4), compared to their caucasian counterparts.
The prevalence of AD in populations is dependent upon factors including incidence and survival. Since the incidence of AD increases with age, prevalence depends on the mean age of the population for which prevalence is given. In the United States in 2020, AD dementia prevalence was estimated to be 5.3% for those in the 60–74 age group, with the rate increasing to 13.8% in the 74–84 group and to 34.6% in those greater than 85. Prevalence rates in some less developed regions around the globe are lower. Both the prevalence and incidence rates of AD are steadily increasing, however the prevalence rate is estimated to triple by 2050 reaching 152 million, compared to the 50 million people with AD globally in 2020.
History
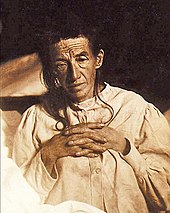
The ancient Greek and Roman philosophers and physicians associated old age with increasing dementia. It was not until 1901 that German psychiatrist Alois Alzheimer identified the first case of what became known as Alzheimer's disease, named after him, in a fifty-year-old woman he called Auguste D. He followed her case until she died in 1906 when he first reported publicly on it. During the next five years, eleven similar cases were reported in the medical literature, some of them already using the term Alzheimer's disease. The disease was first described as a distinctive disease by Emil Kraepelin after suppressing some of the clinical (delusions and hallucinations) and pathological features (arteriosclerotic changes) contained in the original report of Auguste D. He included Alzheimer's disease, also named presenile dementia by Kraepelin, as a subtype of senile dementia in the eighth edition of his Textbook of Psychiatry, published on 15 July 1910.
For most of the 20th century, the diagnosis of Alzheimer's disease was reserved for individuals between the ages of 45 and 65 who developed symptoms of dementia. The terminology changed after 1977 when a conference on Alzheimer's disease concluded that the clinical and pathological manifestations of presenile and senile dementia were almost identical, although the authors also added that this did not rule out the possibility that they had different causes. This eventually led to the diagnosis of Alzheimer's disease independent of age. The term senile dementia of the Alzheimer type (SDAT) was used for a time to describe the condition in those over 65, with classical Alzheimer's disease being used to describe those who were younger. Eventually, the term Alzheimer's disease was formally adopted in medical nomenclature to describe individuals of all ages with a characteristic common symptom pattern, disease course, and neuropathology.
The National Institute of Neurological and Communicative Disorders and Stroke (NINCDS) and the Alzheimer's Disease and Related Disorders Association (ADRDA, now known as the Alzheimer's Association) established the most commonly used NINCDS-ADRDA Alzheimer's Criteria for diagnosis in 1984, extensively updated in 2007. These criteria require that the presence of cognitive impairment, and a suspected dementia syndrome, be confirmed by neuropsychological testing for a clinical diagnosis of possible or probable Alzheimer's disease. A histopathologic confirmation including a microscopic examination of brain tissue is required for a definitive diagnosis. Good statistical reliability and validity have been shown between the diagnostic criteria and definitive histopathological confirmation.
Society and culture
See also: Alzheimer's disease organizationsSocial costs
Dementia, and specifically Alzheimer's disease, may be among the most costly diseases for societies worldwide. As populations age, these costs will probably increase and become an important social problem and economic burden. Costs associated with AD include direct and indirect medical costs, which vary between countries depending on social care for a person with AD. Direct costs include doctor visits, hospital care, medical treatments, nursing home care, specialized equipment, and household expenses. Indirect costs include the cost of informal care and the loss in productivity of informal caregivers.
In the United States as of 2019, informal (family) care is estimated to constitute nearly three-fourths of caregiving for people with AD at a cost of US$234 billion per year and approximately 18.5 billion hours of care. The cost to society worldwide to care for individuals with AD is projected to increase nearly ten-fold, and reach about US$9.1 trillion by 2050.
Costs for those with more severe dementia or behavioral disturbances are higher and are related to the additional caregiving time to provide physical care.
Caregiving burden
Further information: Caregiving and dementia| This section needs to be updated. Please help update this article to reflect recent events or newly available information. (February 2022) |
Individuals with Alzheimer's will require assistance in their lifetime, and care will most likely come in the form of a full-time caregiver which is often a role that is taken on by the spouse or a close relative. Caregiving tends to include physical and emotional burdens as well as time and financial strain at times on the person administering the aid. Alzheimer's disease is known for placing a great burden on caregivers which includes social, psychological, physical, or economic aspects. Home care is usually preferred by both those people with Alzheimer's disease as well as their families. This option also delays or eliminates the need for more professional and costly levels of care. Nevertheless, two-thirds of nursing home residents have dementias.
Dementia caregivers are subject to high rates of physical and mental disorders. Factors associated with greater psychosocial problems of the primary caregivers include having an affected person at home, the caregiver being a spouse, demanding behaviors of the cared person such as depression, behavioral disturbances, hallucinations, sleep problems or walking disruptions and social isolation. In the United States, the yearly cost of caring for a person with dementia ranges from $41,689-$56,290 per year. Other estimates range from $28,078-$56,022 per year for formal medical care and $36,667-$92,689 for informal care provided by a relative or friend (assuming market value replacement costs for the care provided by the informal caregiver) and $15,792-$71,813 in lost wages.
Cognitive behavioral therapy and the teaching of coping strategies either individually or in group have demonstrated their efficacy in improving caregivers' psychological health.
Media
Main article: Alzheimer's disease in the mediaAlzheimer's disease has been portrayed in films such as: Iris (2001), based on John Bayley's memoir of his wife Iris Murdoch; The Notebook (2004), based on Nicholas Sparks's 1996 novel of the same name; A Moment to Remember (2004); Thanmathra (2005); Memories of Tomorrow (Ashita no Kioku) (2006), based on Hiroshi Ogiwara's novel of the same name; Away from Her (2006), based on Alice Munro's short story The Bear Came over the Mountain; Still Alice (2014), about a Columbia University professor who has early onset Alzheimer's disease, based on Lisa Genova's 2007 novel of the same name and featuring Julianne Moore in the title role. Documentaries on Alzheimer's disease include Malcolm and Barbara: A Love Story (1999) and Malcolm and Barbara: Love's Farewell (2007), both featuring Malcolm Pointon.
Alzheimer's disease has also been portrayed in music by English musician the Caretaker in releases such as Persistent Repetition of Phrases (2008), An Empty Bliss Beyond This World (2011), and Everywhere at the End of Time (2016–2019). Paintings depicting the disorder include the late works by American artist William Utermohlen, who drew self-portraits from 1995 to 2000 as an experiment of showing his disease through art.
Research directions
See also: Anti-amyloid drugsAntibodies may have the ability to alter the disease course by targeting amyloid beta with immunotherapy medications such as donanemab, aducanumab, and lecanemab. Aducanumab was approved by the US Food and Drug Administration (FDA) in 2021, using the accelerated approval process, although the approval generated controversy and more evidence is needed to address administration, safety, and effectiveness. It has less effectiveness in people who already had severe Alzheimer's symptoms. In early 2024, Biogen announced it would discontinue aducanumab.
Lecanemab, which clears plaques and reduces amyloid proteins, was approved via the FDA accelerated approval process, and was converted to traditional approval in July 2023, after further testing, along with the addition of a boxed warning about amyloid-related imaging abnormalities. As of early August 2024, lecanemab was approved for sale in Japan, South Korea, China, Hong Kong and Israel although it was recommended against approval by an advisory body of the European Union on July 26, citing its side effects.
Donanemab, which clears plaques, was approved by the FDA in July 2024. Anti-amyloid drugs also cause brain shrinkage. The cholinesterase inhibitor benzgalantamine was approved by the FDA in July 2024.
Specific medications that may reduce the risk or progression of Alzheimer's disease have been studied. The research trials investigating medications generally impact Aβ plaques, inflammation, APOE, neurotransmitter receptors, neurogenesis, growth factors or hormones.
Machine learning algorithms with electronic health records are being studied as a way to predict Alzheimer's disease earlier.
Focused ultrasound for medication delivery
In 2024, a new technique of using focused ultrasound for the delivery of medication past the blood-brain barrier (BBB) is being tested. At the point where the ultrasound beams converge, the focused ultrasound produces several therapeutic effects without incisions or radiation. This can cause opening of the blood-brain barrier (BBB), which may aid in the removal of beta amyloid or tao from the brain.
References
- ^ Knopman DS, Amieva H, Petersen RC, Chételat G, Holtzman DM, Hyman BT, et al. (May 2021). "Alzheimer disease". Nature Reviews Disease Primers. 7 (1): 33. doi:10.1038/s41572-021-00269-y. PMC 8574196. PMID 33986301.
- ^ "Dementia Fact sheet". World Health Organization. 15 March 2023. Retrieved 10 July 2023.
- ^ "Ask the Doctors - What is the cause of death in Alzheimer's disease?". www.uclahealth.org. Retrieved 18 March 2024.
- ^ Mendez MF (November 2012). "Early-onset Alzheimer's disease: nonamnestic subtypes and type 2 AD". Archives of Medical Research. 43 (8): 677–685. doi:10.1016/j.arcmed.2012.11.009. PMC 3532551. PMID 23178565.
- ^ Yu JT, Xu W, Tan CC, Andrieu S, Suckling J, Evangelou E, et al. (November 2020). "Evidence-based prevention of Alzheimer's disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials". Journal of Neurology, Neurosurgery, and Psychiatry. 91 (11): 1201–1209. doi:10.1136/jnnp-2019-321913. PMC 7569385. PMID 32690803.
- ^ Cheng ST (September 2016). "Cognitive Reserve and the Prevention of Dementia: the Role of Physical and Cognitive Activities". Current Psychiatry Reports (Review). 18 (9): 85. doi:10.1007/s11920-016-0721-2. PMC 4969323. PMID 27481112.
- ^ Viña J, Sanz-Ros J (October 2018). "Alzheimer's disease: Only prevention makes sense". European Journal of Clinical Investigation (Review). 48 (10): e13005. doi:10.1111/eci.13005. PMID 30028503. S2CID 51703879.
- ^ "Dementia diagnosis and assessment" (PDF). National Institute for Health and Care Excellence (NICE). Archived from the original (PDF) on 5 December 2014. Retrieved 30 November 2014.
- Gomperts SN (April 2016). "Lewy Body Dementias: Dementia With Lewy Bodies and Parkinson Disease Dementia". Continuum (Review). 22 (2 Dementia): 435–463. doi:10.1212/CON.0000000000000309. ISSN 1080-2371. PMC 5390937. PMID 27042903.
- ^ Lott IT, Head E (March 2019). "Dementia in Down syndrome: unique insights for Alzheimer disease research". Nat Rev Neurol. 15 (3): 135–147. doi:10.1038/s41582-018-0132-6. PMC 8061428. PMID 30733618.
- ^ "How Alzheimer's drugs help manage symptoms". Mayo Clinic. 30 August 2023. Retrieved 19 March 2024.
- ^ Schaffert J, LoBue C, Hynan LS, Hart J, Rossetti H, Carlew AR, et al. (2022). "Predictors of Life Expectancy in Autopsy-Confirmed Alzheimer's Disease". Journal of Alzheimer's Disease. 86 (1): 271–281. doi:10.3233/JAD-215200. PMC 8966055. PMID 35034898.
- ^ Todd S, Barr S, Roberts M, Passmore AP (November 2013). "Survival in dementia and predictors of mortality: a review". International Journal of Geriatric Psychiatry. 28 (11): 1109–1124. doi:10.1002/gps.3946. PMID 23526458.
- ^ Breijyeh Z, Karaman R (December 2020). "Comprehensive Review on Alzheimer's Disease: Causes and Treatment". Molecules (Review). 25 (24): 5789. doi:10.3390/molecules25245789. PMC 7764106. PMID 33302541.
- ^ Simon RP, Greenberg DA, Aminoff MJ (2018). Clinical neurology (Tenth ed.). : McGraw Hill. p. 111. ISBN 978-1-259-86173-4. OCLC 1012400314.
- ^ Burns A, Iliffe S (February 2009). "Alzheimer's disease". BMJ. 338: b158. doi:10.1136/bmj.b158. PMID 19196745. S2CID 8570146.
- ^ Long JM, Holtzman DM (October 2019). "Alzheimer Disease: An Update on Pathobiology and Treatment Strategies". Cell. 179 (2): 312–339. doi:10.1016/j.cell.2019.09.001. PMC 6778042. PMID 31564456.
- ^ "Study reveals how APOE4 gene may increase risk for dementia". National Institute on Aging. 16 March 2021. Archived from the original on 17 March 2021. Retrieved 17 March 2021.
- ^ "Alzheimer's Disease Fact Sheet". National Institute on Aging. Archived from the original on 23 March 2022. Retrieved 23 March 2022.
- Dementia: assessment, management and support for people living with dementia and their carers (Report). National Institute for Health and Care Excellence (NICE). 20 June 2018. NG97. Retrieved 8 July 2023.
- ^ Khan S, Barve KH, Kumar MS (2020). "Recent Advancements in Pathogenesis, Diagnostics and Treatment of Alzheimer's Disease". Curr Neuropharmacol. 18 (11): 1106–1125. doi:10.2174/1570159X18666200528142429. PMC 7709159. PMID 32484110.
- ^ Gauthreaux K, Bonnett TA, Besser LM, Brenowitz WD, Teylan M, Mock C, et al. (May 2020). "Concordance of Clinical Alzheimer Diagnosis and Neuropathological Features at Autopsy". Journal of Neuropathology and Experimental Neurology. 79 (5): 465–473. doi:10.1093/jnen/nlaa014. PMC 7160616. PMID 32186726.
- ^ Thompson CA, Spilsbury K, Hall J, Birks Y, Barnes C, Adamson J (July 2007). "Systematic review of information and support interventions for caregivers of people with dementia". BMC Geriatrics. 7: 18. doi:10.1186/1471-2318-7-18. PMC 1951962. PMID 17662119.
- Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S (April 2015). "Exercise programs for people with dementia". The Cochrane Database of Systematic Reviews (Submitted manuscript). 132 (4): CD006489. doi:10.1002/14651858.CD006489.pub4. PMC 9426996. PMID 25874613.
- "Low-dose antipsychotics in people with dementia". National Institute for Health and Care Excellence (NICE). Archived from the original on 5 December 2014. Retrieved 29 November 2014.
- "Information for Healthcare Professionals: Conventional Antipsychotics". US Food and Drug Administration. 16 June 2008. Archived from the original on 29 November 2014. Retrieved 29 November 2014.
- ^ "Alzheimer's Disease Fact Sheet". National Institute on Aging. Archived from the original on 24 January 2021. Retrieved 25 January 2021.
- Zhu D, Montagne A, Zhao Z (June 2021). "Alzheimer's pathogenic mechanisms and underlying sex difference". Cell Mol Life Sci. 78 (11): 4907–4920. doi:10.1007/s00018-021-03830-w. PMC 8720296. PMID 33844047.
- ^ Berchtold NC, Cotman CW (1998). "Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s". Neurobiology of Aging. 19 (3): 173–189. doi:10.1016/S0197-4580(98)00052-9. PMID 9661992. S2CID 24808582.
- "The top 10 causes of death". www.who.int. Retrieved 19 March 2024.
- Bertagnolli MM (5 August 2024). "Fiscal Year 2026 NIH Professional Judgment Budget for Alzheimer's Disease and Related Dementias Research: Advancing Progress in Dementia Research". US National Institutes of Health. Retrieved 23 September 2024.
- "Horizon Europe research programme" – via www.alzheimer-europe.org.
{{cite journal}}: Cite journal requires|journal=(help) - ^ "Alzheimer's disease – Symptoms". National Health Service (NHS). 10 May 2018. Archived from the original on 30 January 2021. Retrieved 25 January 2021.
- ^ Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rossor M, et al. (January 2007). "Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline". European Journal of Neurology. 14 (1): e1-26. doi:10.1111/j.1468-1331.2006.01605.x. PMID 17222085. S2CID 2725064.
- ^ Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ (September 2004). "Multiple cognitive deficits during the transition to Alzheimer's disease". Journal of Internal Medicine. 256 (3): 195–204. doi:10.1111/j.1365-2796.2004.01386.x. PMID 15324363. S2CID 37005854.
- Nygård L (2003). "Instrumental activities of daily living: a stepping-stone towards Alzheimer's disease diagnosis in subjects with mild cognitive impairment?". Acta Neurologica Scandinavica. Supplementum. 179 (s179): 42–46. doi:10.1034/j.1600-0404.107.s179.8.x. PMID 12603250. S2CID 25313065.
- Deardorff WJ, Grossberg GT (2019). "Behavioral and psychological symptoms in Alzheimer's dementia and vascular dementia". Psychopharmacology of Neurologic Disease. Handbook of Clinical Neurology. Vol. 165. Elsevier. pp. 5–32. doi:10.1016/B978-0-444-64012-3.00002-2. ISBN 978-0-444-64012-3. PMID 31727229. S2CID 208037448.
- Murray ED, Buttner N, Price BH (2012). "Depression and Psychosis in Neurological Practice". In Bradley WG, Daroff RB, Fenichel GM, Jankovic J (eds.). Bradley's neurology in clinical practice (6th ed.). Philadelphia, PA: Elsevier/Saunders. ISBN 978-1-4377-0434-1.
- ^ Petersen RC, Lopez O, Armstrong MJ, Getchius TS, Ganguli M, Gloss D, et al. (January 2018). "Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology". Neurology. 90 (3): 126–135. doi:10.1212/WNL.0000000000004826. PMC 5772157. PMID 29282327.
- ^ Atri A (March 2019). "The Alzheimer's Disease Clinical Spectrum: Diagnosis and Management". The Medical Clinics of North America (Review). 103 (2): 263–293. doi:10.1016/j.mcna.2018.10.009. PMID 30704681. S2CID 73432842.
- ^ Förstl H, Kurz A (1999). "Clinical features of Alzheimer's disease". European Archives of Psychiatry and Clinical Neuroscience. 249 (6): 288–290. doi:10.1007/s004060050101. PMID 10653284. S2CID 26142779.
- Carlesimo GA, Oscar-Berman M (June 1992). "Memory deficits in Alzheimer's patients: a comprehensive review". Neuropsychology Review. 3 (2): 119–169. doi:10.1007/BF01108841. PMID 1300219. S2CID 19548915.
- Jelicic M, Bonebakker AE, Bonke B (1995). "Implicit memory performance of patients with Alzheimer's disease: a brief review". International Psychogeriatrics. 7 (3): 385–392. doi:10.1017/S1041610295002134. PMID 8821346. S2CID 9419442.
- ^ Taler V, Phillips NA (July 2008). "Language performance in Alzheimer's disease and mild cognitive impairment: a comparative review". Journal of Clinical and Experimental Neuropsychology. 30 (5): 501–556. doi:10.1080/13803390701550128. PMID 18569251. S2CID 37153159.
- ^ Frank EM (September 1994). "Effect of Alzheimer's disease on communication function". Journal of the South Carolina Medical Association. 90 (9): 417–423. PMID 7967534.
- Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A (May 2001). "Sundowning and circadian rhythms in Alzheimer's disease". The American Journal of Psychiatry. 158 (5): 704–711. doi:10.1176/appi.ajp.158.5.704. PMID 11329390. S2CID 10492607.
- Gold DP, Reis MF, Markiewicz D, Andres D (January 1995). "When home caregiving ends: a longitudinal study of outcomes for caregivers of relatives with dementia". Journal of the American Geriatrics Society. 43 (1): 10–16. doi:10.1111/j.1532-5415.1995.tb06235.x. PMID 7806732. S2CID 29847950.
- Mashour GA, Frank L, Batthyany A, Kolanowski AM, Nahm M, Schulman-Green D, et al. (August 2019). "Paradoxical lucidity: A potential paradigm shift for the neurobiology and treatment of severe dementias". Alzheimer's & Dementia. 15 (8): 1107–1114. doi:10.1016/j.jalz.2019.04.002. hdl:2027.42/153062. PMID 31229433. S2CID 195063786.
- "Alzheimer's disease – Causes". National Health Service (NHS). 24 April 2023. Archived from the original on 29 September 2020. Retrieved 10 July 2023.
- Tackenberg C, Kulic L, Nitsch RM (2020). "Familial Alzheimer's disease mutations at position 22 of the amyloid β-peptide sequence differentially affect synaptic loss, tau phosphorylation and neuronal cell death in an ex vivo system". PLOS ONE. 15 (9): e0239584. Bibcode:2020PLoSO..1539584T. doi:10.1371/journal.pone.0239584. PMC 7510992. PMID 32966331.
- Wang H, Kulas JA, Wang C, Holtzman DM, Ferris HA, Hansen SB (August 2021). "Regulation of beta-amyloid production in neurons by astrocyte-derived cholesterol". Proceedings of the National Academy of Sciences of the United States of America. 118 (33): e2102191118. Bibcode:2021PNAS..11802191W. doi:10.1073/pnas.2102191118. ISSN 0027-8424. PMC 8379952. PMID 34385305. S2CID 236998499.
- Vilchez D, Saez I, Dillin A (December 2014). "The role of protein clearance mechanisms in organismal ageing and age-related diseases". Nature Communications. 5: 5659. Bibcode:2014NatCo...5.5659V. doi:10.1038/ncomms6659. PMID 25482515.
- Jacobson M, McCarthy N (2002). Apoptosis. Oxford, OX: Oxford University Press. p. 290. ISBN 0-19-963849-7.
- Hardy J, Allsop D (October 1991). "Amyloid deposition as the central event in the aetiology of Alzheimer's disease". Trends in Pharmacological Sciences. 12 (10): 383–388. doi:10.1016/0165-6147(91)90609-V. PMID 1763432.
- Mudher A, Lovestone S (January 2002). "Alzheimer's disease-do tauists and baptists finally shake hands?". Trends in Neurosciences. 25 (1): 22–26. doi:10.1016/S0166-2236(00)02031-2. PMID 11801334. S2CID 37380445.
- Polvikoski T, Sulkava R, Haltia M, Kainulainen K, Vuorio A, Verkkoniemi A, et al. (November 1995). "Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein". The New England Journal of Medicine. 333 (19): 1242–1247. doi:10.1056/NEJM199511093331902. PMID 7566000.
- ^ Andrews SJ, Renton AE, Fulton-Howard B, Podlesny-Drabiniok A, Marcora E, Goate AM (April 2023). "The complex genetic architecture of Alzheimer's disease: novel insights and future directions". eBioMedicine. 90: 104511. doi:10.1016/j.ebiom.2023.104511. PMC 10024184. PMID 36907103.
- ^ Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, et al. (April 2021). "Alzheimer's disease". Lancet. 397 (10284): 1577–1590. doi:10.1016/S0140-6736(20)32205-4. PMC 8354300. PMID 33667416.
- Sims R, Hill M, Williams J (March 2020). "The multiplex model of the genetics of Alzheimer's disease" (PDF). Nat Neurosci. 23 (3): 311–322. doi:10.1038/s41593-020-0599-5. PMID 32112059. S2CID 256839971.
- Chávez-Gutiérrez L, Szaruga M (1 September 2020). "Mechanisms of neurodegeneration — Insights from familial Alzheimer's disease". Seminars in Cell & Developmental Biology. Gamma Secretase. 105: 75–85. doi:10.1016/j.semcdb.2020.03.005. ISSN 1084-9521. PMID 32418657.
- Piaceri I, Nacmias B, Sorbi S (January 2013). "Genetics of familial and sporadic Alzheimer's disease". Frontiers in Bioscience (Elite Edition). 5 (1): 167–177. doi:10.2741/e605. PMID 23276979.
- Perea JR, Bolós M, Avila J (October 2020). "Microglia in Alzheimer's Disease in the Context of Tau Pathology". Biomolecules. 10 (10): 1439. doi:10.3390/biom10101439. PMC 7602223. PMID 33066368.
- Mahley RW, Weisgraber KH, Huang Y (April 2006). "Apolipoprotein E4: a causative factor and therapeutic target in neuropathology, including Alzheimer's disease". Proceedings of the National Academy of Sciences of the United States of America. 103 (15): 5644–5651. Bibcode:2006PNAS..103.5644M. doi:10.1073/pnas.0600549103. PMC 1414631. PMID 16567625.
- Blennow K, de Leon MJ, Zetterberg H (July 2006). "Alzheimer's disease". Lancet. 368 (9533): 387–403. doi:10.1016/S0140-6736(06)69113-7. PMID 16876668. S2CID 47544338.
- Hall K, Murrell J, Ogunniyi A, Deeg M, Baiyewu O, Gao S, et al. (January 2006). "Cholesterol, APOE genotype, and Alzheimer disease: an epidemiologic study of Nigerian Yoruba". Neurology. 66 (2): 223–227. doi:10.1212/01.wnl.0000194507.39504.17. PMC 2860622. PMID 16434658.
- Gureje O, Ogunniyi A, Baiyewu O, Price B, Unverzagt FW, Evans RM, et al. (January 2006). "APOE epsilon4 is not associated with Alzheimer's disease in elderly Nigerians". Annals of Neurology. 59 (1): 182–185. doi:10.1002/ana.20694. PMC 2855121. PMID 16278853.
- Schramm C, Wallon D, Nicolas G, Charbonnier C (1 May 2022). "What contribution can genetics make to predict the risk of Alzheimer's disease?". Revue Neurologique. International meeting of the French society of neurology : NeuroDegenerative Disease : What will the future bring ?. 178 (5): 414–421. doi:10.1016/j.neurol.2022.03.005. ISSN 0035-3787. PMID 35491248.
- Goldman JS, Van Deerlin VM (1 October 2018). "Alzheimer's Disease and Frontotemporal Dementia: The Current State of Genetics and Genetic Testing Since the Advent of Next-Generation Sequencing". Molecular Diagnosis & Therapy. 22 (5): 505–513. doi:10.1007/s40291-018-0347-7. ISSN 1179-2000. PMC 6472481. PMID 29971646.
- Piaceri I (2013). "Genetics of familial and sporadic Alzheimer s disease". Frontiers in Bioscience. E5 (1): 167–177. doi:10.2741/E605. ISSN 1945-0494. PMID 23276979.
- Selkoe DJ (June 1999). "Translating cell biology into therapeutic advances in Alzheimer's disease". Nature. 399 (6738 Suppl): A23 – A31. doi:10.1038/19866. PMID 10392577. S2CID 42287088.
- Borchelt DR, Thinakaran G, Eckman CB, Lee MK, Davenport F, Ratovitsky T, et al. (November 1996). "Familial Alzheimer's disease-linked presenilin 1 variants elevate Abeta1-42/1-40 ratio in vitro and in vivo". Neuron. 17 (5): 1005–1013. doi:10.1016/S0896-6273(00)80230-5. PMID 8938131. S2CID 18315650.
- Kim JH (December 2018). "Genetics of Alzheimer's Disease". Dementia and Neurocognitive Disorders. 17 (4): 131–136. doi:10.12779/dnd.2018.17.4.131. PMC 6425887. PMID 30906402.
- Carmona S, Zahs K, Wu E, Dakin K, Bras J, Guerreiro R (August 2018). "The role of TREM2 in Alzheimer's disease and other neurodegenerative disorders". Lancet Neurol. 17 (8): 721–730. doi:10.1016/S1474-4422(18)30232-1. PMID 30033062. S2CID 51706988. Archived from the original on 27 March 2022. Retrieved 21 February 2022.
- Tomiyama T (July 2010). "". Brain and Nerve = Shinkei Kenkyu No Shinpo. 62 (7): 691–699. PMID 20675873.
- Tomiyama T, Nagata T, Shimada H, Teraoka R, Fukushima A, Kanemitsu H, et al. (March 2008). "A new amyloid beta variant favoring oligomerization in Alzheimer's-type dementia". Annals of Neurology. 63 (3): 377–387. doi:10.1002/ana.21321. PMID 18300294. S2CID 42311988.
- Tomiyama T, Shimada H (February 2020). "APP Osaka Mutation in Familial Alzheimer's Disease-Its Discovery, Phenotypes, and Mechanism of Recessive Inheritance". International Journal of Molecular Sciences. 21 (4): 1413. doi:10.3390/ijms21041413. PMC 7073033. PMID 32093100.
- ^ Tzioras M, Davies C, Newman A, Jackson R, Spires-Jones T (June 2019). "Invited Review: APOE at the interface of inflammation, neurodegeneration and pathological protein spread in Alzheimer's disease". Neuropathology and Applied Neurobiology. 45 (4): 327–346. doi:10.1111/nan.12529. PMC 6563457. PMID 30394574.
- Sinyor B, Mineo J, Ochner C (June 2020). "Alzheimer's Disease, Inflammation, and the Role of Antioxidants". Journal of Alzheimer's Disease Reports. 4 (1): 175–183. doi:10.3233/ADR-200171. PMC 7369138. PMID 32715278.
- Kinney JW, Bemiller SM, Murtishaw AS, Leisgang AM, Salazar AM, Lamb BT (2018). "Inflammation as a central mechanism in Alzheimer's disease". Alzheimer's & Dementia. 4: 575–590. doi:10.1016/j.trci.2018.06.014. PMC 6214864. PMID 30406177.
- Lin X, Kapoor A, Gu Y, Chow MJ, Peng J, Zhao K, et al. (February 2020). "Contributions of DNA Damage to Alzheimer's Disease". Int J Mol Sci. 21 (5): 1666. doi:10.3390/ijms21051666. PMC 7084447. PMID 32121304.
- Irwin MR, Vitiello MV (March 2019). "Implications of sleep disturbance and inflammation for Alzheimer's disease dementia". The Lancet. Neurology. 18 (3): 296–306. doi:10.1016/S1474-4422(18)30450-2. PMID 30661858. S2CID 58546748.
- Lloret MA, Cervera-Ferri A, Nepomuceno M, Monllor P, Esteve D, Lloret A (February 2020). "Is Sleep Disruption a Cause or Consequence of Alzheimer's Disease? Reviewing Its Possible Role as a Biomarker". International Journal of Molecular Sciences. 21 (3): 1168. doi:10.3390/ijms21031168. PMC 7037733. PMID 32050587.
- Huat TJ, Camats-Perna J, Newcombe EA, Valmas N, Kitazawa M, Medeiros R (April 2019). "Metal Toxicity Links to Alzheimer's Disease and Neuroinflammation". J Mol Biol. 431 (9): 1843–1868. doi:10.1016/j.jmb.2019.01.018. PMC 6475603. PMID 30664867.
- Eikelenboom P, van Exel E, Hoozemans JJ, Veerhuis R, Rozemuller AJ, van Gool WA (2010). "Neuroinflammation – an early event in both the history and pathogenesis of Alzheimer's disease". Neuro-Degenerative Diseases. 7 (1–3): 38–41. doi:10.1159/000283480. PMID 20160456. S2CID 40048333.
- Alves GS, Oertel Knöchel V, Knöchel C, Carvalho AF, Pantel J, Engelhardt E, et al. (2015). "Integrating retrogenesis theory to Alzheimer's disease pathology: insight from DTI-TBSS investigation of the white matter microstructural integrity". BioMed Research International. 2015: 291658. doi:10.1155/2015/291658. PMC 4320890. PMID 25685779.
- Reisberg B, Franssen EH, Hasan SM, Monteiro I, Boksay I, Souren LE, et al. (1999). "Retrogenesis: clinical, physiologic, and pathologic mechanisms in brain aging, Alzheimer's and other dementing processes". European Archives of Psychiatry and Clinical Neuroscience. 249 (3): 28–36. doi:10.1007/pl00014170. PMID 10654097. S2CID 23410069.
- Bartzokis G (August 2011). "Alzheimer's disease as homeostatic responses to age-related myelin breakdown". Neurobiology of Aging. 32 (8): 1341–1371. doi:10.1016/j.neurobiolaging.2009.08.007. PMC 3128664. PMID 19775776.
- Cai Z, Xiao M (2016). "Oligodendrocytes and Alzheimer's disease". The International Journal of Neuroscience. 126 (2): 97–104. doi:10.3109/00207454.2015.1025778. PMID 26000818. S2CID 21448714.
- Depp C, Sun T, Sasmita AO, Spieth L, Berghoff SA, Nazarenko T, et al. (June 2023). "Myelin dysfunction drives amyloid-β deposition in models of Alzheimer's disease". Nature. 618 (7964): 349–357. Bibcode:2023Natur.618..349D. doi:10.1038/s41586-023-06120-6. PMC 10247380. PMID 37258678.
- Luczynski P, Laule C, Hsiung GR, Moore GR, Tremlett H (January 2019). "Coexistence of Multiple Sclerosis and Alzheimer's disease: A review". Multiple Sclerosis and Related Disorders. 27: 232–238. doi:10.1016/j.msard.2018.10.109. PMID 30415025.
- Londoño DP, Arumaithurai K, Constantopoulos E, Basso MR, Reichard RR, Flanagan EP, et al. (4 July 2022). "Diagnosis of coexistent neurodegenerative dementias in multiple sclerosis". Brain Communications. 4 (4): fcac167. doi:10.1093/braincomms/fcac167. PMC 9272064. PMID 35822102.
- Zis P, Hadjivassiliou M (February 2019). "Treatment of Neurological Manifestations of Gluten Sensitivity and Coeliac Disease". Current Treatment Options in Neurology. 21 (3): 10. doi:10.1007/s11940-019-0552-7. PMID 30806821. S2CID 73466457.
- Makhlouf S, Messelmani M, Zaouali J, Mrissa R (March 2018). "Cognitive impairment in celiac disease and non-celiac gluten sensitivity: review of literature on the main cognitive impairments, the imaging and the effect of gluten free diet". Acta Neurologica Belgica (Review). 118 (1): 21–27. doi:10.1007/s13760-017-0870-z. PMID 29247390. S2CID 3943047.
- Zhou L, Miranda-Saksena M, Saksena NK (May 2013). "Viruses and neurodegeneration". Virology Journal. 10 (1): 172. doi:10.1186/1743-422X-10-172. PMC 3679988. PMID 23724961.
- Gonzalez-Fernandez E, Huang J (September 2023). "Cognitive Aspects of COVID-19". Current Neurology and Neuroscience Reports. 23 (9): 531–538. doi:10.1007/s11910-023-01286-y. PMID 37490194. S2CID 260132167.
- Wenk GL (2003). "Neuropathologic changes in Alzheimer's disease". The Journal of Clinical Psychiatry. 64 (Suppl 9): 7–10. PMID 12934968.
- Braak H, Del Tredici K (December 2012). "Where, when, and in what form does sporadic Alzheimer's disease begin?". Current Opinion in Neurology. 25 (6): 708–714. doi:10.1097/WCO.0b013e32835a3432. PMID 23160422.
- Desikan RS, Cabral HJ, Hess CP, Dillon WP, Glastonbury CM, Weiner MW, et al. (August 2009). "Automated MRI measures identify individuals with mild cognitive impairment and Alzheimer's disease". Brain. 132 (Pt 8): 2048–2057. doi:10.1093/brain/awp123. PMC 2714061. PMID 19460794.
- Moan R (July 2009). "MRI Software Accurately IDs Preclinical Alzheimer's Disease". Diagnostic Imaging. Archived from the original on 21 February 2022. Retrieved 21 February 2022.
- Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J (June 2004). "The importance of neuritic plaques and tangles to the development and evolution of AD". Neurology. 62 (11): 1984–1989. doi:10.1212/01.WNL.0000129697.01779.0A. PMID 15184601. S2CID 25017332.
- DeTure MA, Dickson DW (August 2019). "The neuropathological diagnosis of Alzheimer's disease". Molecular Neurodegeneration. 14 (1): 32. doi:10.1186/s13024-019-0333-5. PMC 6679484. PMID 31375134.
- Tiraboschi P, Sabbagh MN, Hansen LA, Salmon DP, Merdes A, Gamst A, et al. (April 2004). "Alzheimer disease without neocortical neurofibrillary tangles: "a second look"". Neurology. 62 (7): 1141–1147. doi:10.1212/01.wnl.0000118212.41542.e7. PMID 15079014. S2CID 22832110.
- Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH (1994). "Regional distribution of neurofibrillary tangles and senile plaques in the cerebral cortex of elderly patients: a quantitative evaluation of a one-year autopsy population from a geriatric hospital". Cerebral Cortex. 4 (2): 138–150. doi:10.1093/cercor/4.2.138. PMID 8038565.
- Kotzbauer PT, Trojanowsk JQ, Lee VM (October 2001). "Lewy body pathology in Alzheimer's disease". Journal of Molecular Neuroscience. 17 (2): 225–232. doi:10.1385/JMN:17:2:225. PMID 11816795. S2CID 44407971.
- Hernández F, Avila J (September 2007). "Tauopathies". Cellular and Molecular Life Sciences. 64 (17): 2219–2233. doi:10.1007/s00018-007-7220-x. PMC 11136052. PMID 17604998. S2CID 261121643.
- Sun W, Samimi H, Gamez M, Zare H, Frost B (August 2018). "Pathogenic tau-induced piRNA depletion promotes neuronal death through transposable element dysregulation in neurodegenerative tauopathies". Nature Neuroscience. 21 (8): 1038–1048. doi:10.1038/s41593-018-0194-1. PMC 6095477. PMID 30038280.
- Balusu S, Horré K, Thrupp N, Craessaerts K, Snellinx A, Serneels L, T'Syen D, Chrysidou I, Arranz AM, Sierksma A, Simrén J, Karikari TK, Zetterberg H, Chen WT, Thal DR, Salta E, Fiers M, De Strooper B. MEG3 activates necroptosis in human neuron xenografts modeling Alzheimer's disease. Science. 2023 Sep 15;381(6663):1176-1182. doi:10.1126/science.abp9556 PMID 37708272
- "Scientists discover how brain cells die in Alzheimer's". BBC News. 15 September 2023. Retrieved 27 September 2023.
- Van Broeck B, Van Broeckhoven C, Kumar-Singh S (2007). "Current insights into molecular mechanisms of Alzheimer disease and their implications for therapeutic approaches". Neuro-Degenerative Diseases. 4 (5): 349–365. doi:10.1159/000105156. PMID 17622778. S2CID 7949658.
- Huang Y, Mucke L (March 2012). "Alzheimer mechanisms and therapeutic strategies". Cell. 148 (6): 1204–1222. doi:10.1016/j.cell.2012.02.040. PMC 3319071. PMID 22424230.
- Yankner BA, Duffy LK, Kirschner DA (October 1990). "Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides". Science. 250 (4978): 279–282. Bibcode:1990Sci...250..279Y. doi:10.1126/science.2218531. PMID 2218531.
- Chen X, Yan SD (December 2006). "Mitochondrial Abeta: a potential cause of metabolic dysfunction in Alzheimer's disease". IUBMB Life. 58 (12): 686–694. doi:10.1080/15216540601047767. PMID 17424907. S2CID 85423830.
- Ryan SK, Ugalde CL, Rolland AS, Skidmore J, Devos D, Hammond TR (October 2023). "Therapeutic inhibition of ferroptosis in neurodegenerative disease". Trends in Pharmacological Sciences. 44 (10): 674–688. doi:10.1016/j.tips.2023.07.007. PMID 37657967.
- Greig NH, Mattson MP, Perry T, Chan SL, Giordano T, Sambamurti K, et al. (December 2004). "New therapeutic strategies and drug candidates for neurodegenerative diseases: p53 and TNF-alpha inhibitors, and GLP-1 receptor agonists". Annals of the New York Academy of Sciences. 1035 (1): 290–315. Bibcode:2004NYASA1035..290G. doi:10.1196/annals.1332.018. PMID 15681814. S2CID 84659695. Archived from the original on 3 June 2020. Retrieved 19 July 2019.
- Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, et al. (April 2015). "Neuroinflammation in Alzheimer's disease". The Lancet. Neurology. 14 (4): 388–405. doi:10.1016/S1474-4422(15)70016-5. PMC 5909703. PMID 25792098.
- Tapia-Arancibia L, Aliaga E, Silhol M, Arancibia S (November 2008). "New insights into brain BDNF function in normal aging and Alzheimer disease". Brain Research Reviews. 59 (1): 201–220. doi:10.1016/j.brainresrev.2008.07.007. hdl:10533/142174. PMID 18708092. S2CID 6589846.
- Schindowski K, Belarbi K, Buée L (February 2008). "Neurotrophic factors in Alzheimer's disease: role of axonal transport". Genes, Brain and Behavior. 7 (Suppl 1): 43–56. doi:10.1111/j.1601-183X.2007.00378.x. PMC 2228393. PMID 18184369.
- ^ Sachdev PS, Blacker D, Blazer DG, Ganguli M, Jeste DV, Paulsen JS, et al. (November 2014). "Classifying neurocognitive disorders: the DSM-5 approach". Nature Reviews. Neurology. 10 (11): 634–642. doi:10.1038/nrneurol.2014.181. PMID 25266297. S2CID 20635070. Archived from the original on 20 March 2022. Retrieved 27 November 2021.
- ^ Arvanitakis Z, Shah RC, Bennett DA (22 October 2019). "Diagnosis and Management of Dementia: Review". JAMA. 322 (16): 1589–1599. doi:10.1001/jama.2019.4782. PMC 7462122. PMID 31638686.
- Mendez MF (2006). "The accurate diagnosis of early-onset dementia". International Journal of Psychiatry in Medicine. 36 (4): 401–412. doi:10.2190/Q6J4-R143-P630-KW41. PMID 17407994. S2CID 43715976. Archived from the original on 3 June 2020. Retrieved 25 May 2020.
- Klafki HW, Staufenbiel M, Kornhuber J, Wiltfang J (November 2006). "Therapeutic approaches to Alzheimer's disease". Brain. 129 (Pt 11): 2840–2855. doi:10.1093/brain/awl280. PMID 17018549.
- Dementia: Quick Reference Guide (PDF). London: (UK) National Institute for Health and Clinical Excellence. 2006. ISBN 978-1-84629-312-2. Archived from the original (PDF) on 27 February 2008. Retrieved 22 February 2008.
- Schroeter ML, Stein T, Maslowski N, Neumann J (October 2009). "Neural correlates of Alzheimer's disease and mild cognitive impairment: a systematic and quantitative meta-analysis involving 1351 patients". NeuroImage. 47 (4): 1196–1206. doi:10.1016/j.neuroimage.2009.05.037. PMC 2730171. PMID 19463961.
- Jie CV, Treyer V, Schibli R, Mu L (January 2021). "Tauvid: The First FDA-Approved PET Tracer for Imaging Tau Pathology in Alzheimer's Disease". Pharmaceuticals. 14 (2): 110. doi:10.3390/ph14020110. PMC 7911942. PMID 33573211.
- ^ Weller J, Budson A (2018). "Current understanding of Alzheimer's disease diagnosis and treatment". F1000Research (Review). 7: 1161. doi:10.12688/f1000research.14506.1. PMC 6073093. PMID 30135715.
- Silva MV, Loures CM, Alves LC, de Souza LC, Borges KB, Carvalho MD (May 2019). "Alzheimer's disease: risk factors and potentially protective measures". Journal of Biomedical Science. 26 (1): 33. doi:10.1186/s12929-019-0524-y. PMC 6507104. PMID 31072403.
- Diagnostic and statistical manual of mental disorders: DSM-IV-TR (4th Text Revision ed.). Washington, DC: American Psychiatric Association. 2000. ISBN 978-0-89042-025-6.
- ^ Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C.: American Psychiatric Association. 2013. p. 611. ISBN 978-0-89042-555-8.
- Sachs-Ericsson N, Blazer DG (January 2015). "The new DSM-5 diagnosis of mild neurocognitive disorder and its relation to research in mild cognitive impairment". Aging & Mental Health. 19 (1): 2–12. doi:10.1080/13607863.2014.920303. PMID 24914889. S2CID 46244321.
- Stokin GB, Krell-Roesch J, Petersen RC, Geda YE (2015). "Mild Neurocognitive Disorder: An Old Wine in a New Bottle". Harvard Review of Psychiatry (Review). 23 (5): 368–376. doi:10.1097/HRP.0000000000000084. PMC 4894762. PMID 26332219.
- Sperry L, Carlson J, Sauerheber J, Sperry J, eds. (2014). Psychopathology and Psychotherapy: DSM-5 Diagnosis, Case Conceptualization, and Treatment (3 ed.). New York: Routledge. pp. 342–343. doi:10.4324/9780203772287. ISBN 978-0-203-77228-7. Archived from the original on 16 November 2021. Retrieved 16 November 2021.
{{cite book}}:|journal=ignored (help) - Fink HA, Hemmy LS, Linskens EJ, Silverman PC, MacDonald R, McCarten JR, et al. (2020). Diagnosis and Treatment of Clinical Alzheimer's-Type Dementia: A Systematic Review. AHRQ Comparative Effectiveness Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US). PMID 32369312. Archived from the original on 7 July 2023. Retrieved 16 November 2021.
- Stokin GB, Krell-Roesch J, Petersen RC, Geda YE (September 2015). "Mild Neurocognitive Disorder: An Old Wine in a New Bottle". Harvard Review of Psychiatry. 23 (5). Wolters Kluwer Health: 368–376. doi:10.1097/HRP.0000000000000084. PMC 4894762. PMID 26332219.
- Bradfield NI, Ames D (April 2020). "Mild cognitive impairment: narrative review of taxonomies and systematic review of their prediction of incident Alzheimer's disease dementia". BJPsych Bulletin (Review). 44 (2): 67–74. doi:10.1192/bjb.2019.77. PMC 7283119. PMID 31724527.
- ^ Vega JN, Newhouse PA (October 2014). "Mild cognitive impairment: diagnosis, longitudinal course, and emerging treatments". Current Psychiatry Reports. 16 (10). SpringerLink: 490. doi:10.1007/s11920-014-0490-8. PMC 4169219. PMID 25160795.
- Parnetti L, Chipi E, Salvadori N, D'Andrea K, Eusebi P (January 2019). "Prevalence and risk of progression of preclinical Alzheimer's disease stages: a systematic review and meta-analysis". Alzheimer's Research & Therapy. 11 (1). Springer Nature: 7. doi:10.1186/s13195-018-0459-7. PMC 6334406. PMID 30646955.
- ^ Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. (April 2018). "NIA-AA Research Framework: Toward a biological definition of Alzheimer's disease". Alzheimer's & Dementia. 14 (4): 535–562. doi:10.1016/j.jalz.2018.02.018. PMC 5958625. PMID 29653606.
- Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. (May 2011). "Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease". Alzheimer's & Dementia. 7 (3): 280–292. doi:10.1016/j.jalz.2011.03.003. PMC 3220946. PMID 21514248.
- Cheng YW, Chen TF, Chiu MJ (16 February 2017). "From mild cognitive impairment to subjective cognitive decline: conceptual and methodological evolution". Neuropsychiatric Disease and Treatment. 13. Dove Medical Press Limited: 491–498. doi:10.2147/NDT.S123428. PMC 5317337. PMID 28243102.
- Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. (May 2011). "The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease". Alzheimer's & Dementia. 7 (3): 270–279. doi:10.1016/j.jalz.2011.03.008. PMC 3312027. PMID 21514249.
- ^ Chertkow H, Feldman HH, Jacova C, Massoud F (July 2013). "Definitions of dementia and predementia states in Alzheimer's disease and vascular cognitive impairment: consensus from the Canadian conference on diagnosis of dementia". Alzheimer's Research & Therapy. 5 (Suppl 1). BMC: S2. doi:10.1186/alzrt198. PMC 3981054. PMID 24565215.
- ^ Papadakis MA, McPhee SJ, Rabow MW (2021). Current medical diagnosis & treatment (Sixtieth ed.). New York: McGraw Hill. p. 1760. ISBN 978-1-260-46986-8. OCLC 1195972209.
- Tombaugh TN, McIntyre NJ (September 1992). "The mini-mental state examination: a comprehensive review". Journal of the American Geriatrics Society. 40 (9): 922–935. doi:10.1111/j.1532-5415.1992.tb01992.x. PMID 1512391. S2CID 25169596.
- Pasquier F (January 1999). "Early diagnosis of dementia: neuropsychology". Journal of Neurology. 246 (1): 6–15. doi:10.1007/s004150050299. PMID 9987708. S2CID 2108587.
- Harvey PD, Moriarty PJ, Kleinman L, Coyne K, Sadowsky CH, Chen M, et al. (2005). "The validation of a caregiver assessment of dementia: the Dementia Severity Scale". Alzheimer Disease and Associated Disorders. 19 (4): 186–194. doi:10.1097/01.wad.0000189034.43203.60. PMID 16327345. S2CID 20238911.
- Antoine C, Antoine P, Guermonprez P, Frigard B (2004). "". L'Encéphale (in French). 30 (6): 570–577. doi:10.1016/S0013-7006(04)95472-3. PMID 15738860.
- Cruz VT, Pais J, Teixeira A, Nunes B (2004). "". Acta Médica Portuguesa (in Portuguese). 17 (6): 435–444. PMID 16197855.
- ^ Stern SD, Cifu AS, Altkorn D (2020). Symptom to diagnosis: an evidence-based guide (4th ed.). New York: McGraw-Hill Medical. pp. 209–210. ISBN 978-1-260-12111-7. OCLC 1121597721.
- Jha A, Mukhopadhaya K (2021). Alzheimer's disease: diagnosis and treatment guide. Cham, Switzerland: Springer. p. 32. ISBN 978-3-030-56739-2. OCLC 1202472277.
- Sun X, Steffens DC, Au R, Folstein M, Summergrad P, Yee J, et al. (May 2008). "Amyloid-associated depression: a prodromal depression of Alzheimer disease?". Archives of General Psychiatry. 65 (5): 542–550. doi:10.1001/archpsyc.65.5.542. PMC 3042807. PMID 18458206.
- Geldmacher DS, Whitehouse PJ (May 1997). "Differential diagnosis of Alzheimer's disease". Neurology. 48 (5 Suppl 6): S2 – S9. doi:10.1212/WNL.48.5_Suppl_6.2S. PMID 9153154. S2CID 30018544.
- Potter GG, Steffens DC (May 2007). "Contribution of depression to cognitive impairment and dementia in older adults". The Neurologist. 13 (3): 105–117. doi:10.1097/01.nrl.0000252947.15389.a9. PMID 17495754. S2CID 24569198.
- Zhang S, Smailagic N, Hyde C, Noel-Storr AH, Takwoingi Y, McShane R, et al. (July 2014). "(11)C-PIB-PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI)". The Cochrane Database of Systematic Reviews. 2014 (7): CD010386. doi:10.1002/14651858.CD010386.pub2. PMC 6464750. PMID 25052054.
- Smailagic N, Vacante M, Hyde C, Martin S, Ukoumunne O, Sachpekidis C (January 2015). "F-FDG PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI)". The Cochrane Database of Systematic Reviews. 1 (1): CD010632. doi:10.1002/14651858.CD010632.pub2. PMC 7081123. PMID 25629415.
- Viña J, Sanz-Ros J (October 2018). "Alzheimer's disease: Only prevention makes sense". European Journal of Clinical Investigation. 48 (10): e13005. doi:10.1111/eci.13005. PMID 30028503. S2CID 51703879.
- ^ Hsu D, Marshall GA (2017). "Primary and secondary prevention trials in Alzheimer disease: looking back, moving forward". Curr Alzheimer Res. 14 (4): 426–440. doi:10.2174/1567205013666160930112125. PMC 5329133. PMID 27697063.
- Patterson C, Feightner JW, Garcia A, Hsiung GY, MacKnight C, Sadovnick AD (February 2008). "Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease". CMAJ. 178 (5): 548–556. doi:10.1503/cmaj.070796. PMC 2244657. PMID 18299540.
- Rosendorff C, Beeri MS, Silverman JM (2007). "Cardiovascular risk factors for Alzheimer's disease". The American Journal of Geriatric Cardiology. 16 (3): 143–149. doi:10.1111/j.1076-7460.2007.06696.x. PMID 17483665.
- Chu CS, Tseng PT, Stubbs B, Chen TY, Tang CH, Li DJ, et al. (April 2018). "Use of statins and the risk of dementia and mild cognitive impairment: A systematic review and meta-analysis". Scientific Reports. 8 (1): 5804. Bibcode:2018NatSR...8.5804C. doi:10.1038/s41598-018-24248-8. PMC 5895617. PMID 29643479.
- Ungvari Z, Toth P, Tarantini S, Prodan CI, Sorond F, Merkely B, et al. (October 2021). "Hypertension-induced cognitive impairment: from pathophysiology to public health". Nature Reviews Nephrology. 17 (10): 639–654. doi:10.1038/s41581-021-00430-6. PMC 8202227. PMID 34127835.
- Lethaby A, Hogervorst E, Richards M, Yesufu A, Yaffe K (January 2008). "Hormone replacement therapy for cognitive function in postmenopausal women". Cochrane Database Syst Rev. 2008 (1): CD003122. doi:10.1002/14651858.CD003122.pub2. PMC 6599876. PMID 18254016.
- Farina N, Rusted J, Tabet N (January 2014). "The effect of exercise interventions on cognitive outcome in Alzheimer's disease: a systematic review". International Psychogeriatrics (Review). 26 (1): 9–18. doi:10.1017/S1041610213001385. PMID 23962667. S2CID 24936334.
- Barnard ND, Bush AI, Ceccarelli A, Cooper J, de Jager CA, Erickson KI, et al. (September 2014). "Dietary and lifestyle guidelines for the prevention of Alzheimer's disease". Neurobiology of Aging. 35 (Suppl 2): S74 – S78. doi:10.1016/j.neurobiolaging.2014.03.033. hdl:11343/52774. PMID 24913896. S2CID 8265377.
- ^ Bhatti GK, Reddy AP, Reddy PH, Bhatti JS (2019). "Lifestyle Modifications and Nutritional Interventions in Aging-Associated Cognitive Decline and Alzheimer's Disease". Frontiers in Aging Neuroscience (Review). 11: 369. doi:10.3389/fnagi.2019.00369. PMC 6966236. PMID 31998117.
- López-Ortiz S, Lista S, Valenzuela PL, Pinto-Fraga J, Carmona R, Caraci F, et al. (November 2022). "Effects of physical activity and exercise interventions on Alzheimer's disease: an umbrella review of existing meta-analyses". Journal of Neurology. 270 (2): 711–725. doi:10.1007/s00415-022-11454-8. PMID 36342524. S2CID 253382289.
- Imtiaz B, Tolppanen AM, Kivipelto M, Soininen H (April 2014). "Future directions in Alzheimer's disease from risk factors to prevention". Biochemical Pharmacology (Review). 88 (4): 661–670. doi:10.1016/j.bcp.2014.01.003. PMID 24418410.
- Imtiaz B, Tolppanen AM, Kivipelto M, Soininen H (April 2014). "Future directions in Alzheimer's disease from risk factors to prevention". Biochem Pharmacol. 88 (4): 661–70. doi:10.1016/j.bcp.2014.01.003. PMID 24418410.
- Kivipelto M, Mangialasche F, Ngandu T (November 2018). "Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease". Nat Rev Neurol. 14 (11): 653–666. doi:10.1038/s41582-018-0070-3. PMID 30291317. S2CID 52925352.
- ^ Borges CR, Poyares D, Piovezan R, Nitrini R, Brucki S (November 2019). "Alzheimer's disease and sleep disturbances: a review". Arq Neuropsiquiatr. 77 (11): 815–824. doi:10.1590/0004-282X20190149. PMID 31826138. S2CID 209327994.
- ^ Uddin MS, Tewari D, Mamun AA, Kabir MT, Niaz K, Wahed MI, et al. (July 2020). "Circadian and sleep dysfunction in Alzheimer's disease". Ageing Research Reviews. 60: 101046. doi:10.1016/j.arr.2020.101046. PMID 32171783. S2CID 212729131.
- Rasmussen MK, Mestre H, Nedergaard M (November 2018). "The glymphatic pathway in neurological disorders". Lancet Neurol. 17 (11): 1016–1024. doi:10.1016/S1474-4422(18)30318-1. PMC 6261373. PMID 30353860.
- Irwin MR, Vitiello MV (March 2019). "Implications of sleep disturbance and inflammation for Alzheimer's disease dementia". Lancet Neurol. 18 (3): 296–306. doi:10.1016/S1474-4422(18)30450-2. PMID 30661858. S2CID 58546748.
- Hampel H, Vergallo A, Aguilar LF, Benda N, Broich K, Cuello AC, et al. (April 2018). "Precision pharmacology for Alzheimer's disease". Pharmacological Research. 130: 331–365. doi:10.1016/j.phrs.2018.02.014. PMC 8505114. PMID 29458203.
- Chen Y, Zhang J, Zhang T, Cao L, You Y, Zhang C, et al. (March 2020). "Meditation treatment of Alzheimer disease and mild cognitive impairment: A protocol for systematic review". Medicine. 99 (10): e19313. doi:10.1097/MD.0000000000019313. PMC 7478420. PMID 32150066.
- Winkelman MJ, Szabo A, Frecska E (November 2023). "The potential of psychedelics for the treatment of Alzheimer's disease and related dementias". European Neuropsychopharmacology. 76: 3–16. doi:10.1016/j.euroneuro.2023.07.003. hdl:10852/108211. PMID 37451163.
- Drislane F, Hovauimian A, Tarulli A, Boegle AK, McIiduff C, Caplan LR (2019). Blueprints neurology (Fifth ed.). Philadelphia: Wolters Kluwer. p. 146. ISBN 978-1-4963-8739-4. OCLC 1048659425.
- ^ Birks JS, Harvey RJ (June 2018). "Donepezil for dementia due to Alzheimer's disease". The Cochrane Database of Systematic Reviews. 2018 (6): CD001190. doi:10.1002/14651858.CD001190.pub3. PMC 6513124. PMID 29923184.
- Fink HA, Linskens EJ, MacDonald R, Silverman PC, McCarten JR, Talley KM, et al. (May 2020). "Benefits and Harms of Prescription Drugs and Supplements for Treatment of Clinical Alzheimer-Type Dementia". Annals of Internal Medicine. 172 (10): 656–668. doi:10.7326/M19-3887. PMID 32340037. S2CID 216595473.
- Berkowitz A (2017). Clinical neurology and neuroanatomy: a localization-based approach. New York: McGraw Hill. p. 236. ISBN 978-1-259-83440-0. OCLC 948547621.
- Geula C, Mesulam MM (1995). "Cholinesterases and the pathology of Alzheimer disease". Alzheimer Disease and Associated Disorders. 9 (Suppl 2): 23–28. doi:10.1097/00002093-199501002-00005. PMID 8534419.
- Stahl SM (November 2000). "The new cholinesterase inhibitors for Alzheimer's disease, Part 2: illustrating their mechanisms of action". The Journal of Clinical Psychiatry. 61 (11): 813–814. doi:10.4088/JCP.v61n1101. PMID 11105732.
- ^ Birks J (January 2006). Birks J (ed.). "Cholinesterase inhibitors for Alzheimer's disease". The Cochrane Database of Systematic Reviews. 2016 (1): CD005593. doi:10.1002/14651858.CD005593. PMC 9006343. PMID 16437532.
- Raschetti R, Albanese E, Vanacore N, Maggini M (November 2007). "Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials". PLOS Medicine. 4 (11): e338. doi:10.1371/journal.pmed.0040338. PMC 2082649. PMID 18044984.
- Alldredge BK, Corelli RL, Ernst ME, Guglielmo BJ, Jacobson PA, Kradjan WA, et al. (2013). Applied therapeutics : the clinical use of drugs (10th ed.). Baltimore: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 2385. ISBN 978-1-60913-713-7.
- ^ Lipton SA (February 2006). "Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond". Nature Reviews. Drug Discovery. 5 (2): 160–170. doi:10.1038/nrd1958. PMID 16424917. S2CID 21379258.
- "Memantine". US National Library of Medicine (Medline). 4 January 2004. Archived from the original on 22 February 2010. Retrieved 3 February 2010.
- McShane R, Westby MJ, Roberts E, Minakaran N, Schneider L, Farrimond LE, et al. (March 2019). "Memantine for dementia". The Cochrane Database of Systematic Reviews. 3 (3): CD003154. doi:10.1002/14651858.CD003154.pub6. PMC 6425228. PMID 30891742.
- "Namenda- memantine hydrochloride tablet Namenda- memantine hydrochloride kit". DailyMed. 15 November 2018. Archived from the original on 27 January 2022. Retrieved 20 February 2022.
- "Namenda XR- memantine hydrochloride capsule, extended release Namenda XR- memantine hydrochloride kit". DailyMed. 15 November 2019. Archived from the original on 21 February 2022. Retrieved 20 February 2022.
- "Namzaric- memantine hydrochloride and donepezil hydrochloride capsule Namzaric- memantine hydrochloride and donepezil hydrochloride kit". DailyMed. 22 January 2019. Archived from the original on 20 January 2022. Retrieved 20 February 2022.
- Raina P, Santaguida P, Ismaila A, Patterson C, Cowan D, Levine M, et al. (March 2008). "Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline". Annals of Internal Medicine. 148 (5): 379–397. doi:10.7326/0003-4819-148-5-200803040-00009. PMID 18316756. S2CID 22235353.
- ^ Kandiah N, Ong PA, Yuda T, Ng LL, Mamun K, Merchant RA, et al. (February 2019). "Treatment of dementia and mild cognitive impairment with or without cerebrovascular disease: Expert consensus on the use of Ginkgo biloba extract, EGb 761". CNS Neuroscience & Therapeutics. 25 (2): 288–298. doi:10.1111/cns.13095. PMC 6488894. PMID 30648358.
- McKeage K, Lyseng-Williamson KA (2018). "Ginkgo biloba extract EGb 761 in the symptomatic treatment of mild-to-moderate dementia: a profile of its use". Drugs & Therapy Perspectives. 34 (8): 358–366. doi:10.1007/s40267-018-0537-8. PMC 6267544. PMID 30546253.
- Yang G, Wang Y, Sun J, Zhang K, Liu J (22 October 2015). "Ginkgo Biloba for Mild Cognitive Impairment and Alzheimer's Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Current Topics in Medicinal Chemistry. 16 (5): 520–528. doi:10.2174/1568026615666150813143520. PMID 26268332.
- Ballard C, Waite J (January 2006). Ballard CG (ed.). "The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer's disease". The Cochrane Database of Systematic Reviews (1): CD003476. doi:10.1002/14651858.CD003476.pub2. PMC 11365591. PMID 16437455.
- Ballard C, Hanney ML, Theodoulou M, Douglas S, McShane R, Kossakowski K, et al. (February 2009). "The dementia antipsychotic withdrawal trial (DART-AD): long-term follow-up of a randomised placebo-controlled trial". The Lancet. Neurology. 8 (2): 151–157. doi:10.1016/S1474-4422(08)70295-3. PMID 19138567. S2CID 23000439. See lay summary, January 2009.
- Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter AI, van Driel ML, et al. (March 2013). "Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia". The Cochrane Database of Systematic Reviews. 3 (3): CD007726. doi:10.1002/14651858.CD007726.pub2. hdl:1854/LU-3109108. PMID 23543555.
- ^ Rabins PV, Blacker D, Rovner BW, Rummans T, Schneider LS, Tariot PN, et al. (Steering Committee on Practice Guidelines) (December 2007). "American Psychiatric Association practice guideline for the treatment of patients with Alzheimer's disease and other dementias. Second edition". The American Journal of Psychiatry. 164 (12 Suppl): 5–56. PMID 18340692.
- Bottino CM, Carvalho IA, Alvarez AM, Avila R, Zukauskas PR, Bustamante SE, et al. (December 2005). "Cognitive rehabilitation combined with drug treatment in Alzheimer's disease patients: a pilot study". Clinical Rehabilitation. 19 (8): 861–869. doi:10.1191/0269215505cr911oa. PMID 16323385. S2CID 21290731.
- Doody RS, Stevens JC, Beck C, Dubinsky RM, Kaye JA, Gwyther L, et al. (May 2001). "Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 56 (9): 1154–1166. doi:10.1212/WNL.56.9.1154. PMID 11342679. S2CID 10711725.
- Hermans DG, Htay UH, McShane R (January 2007). "Non-pharmacological interventions for wandering of people with dementia in the domestic setting". The Cochrane Database of Systematic Reviews. 2010 (1): CD005994. doi:10.1002/14651858.CD005994.pub2. PMC 6669244. PMID 17253573.
- Robinson L, Hutchings D, Dickinson HO, Corner L, Beyer F, Finch T, et al. (January 2007). "Effectiveness and acceptability of non-pharmacological interventions to reduce wandering in dementia: a systematic review". International Journal of Geriatric Psychiatry. 22 (1): 9–22. doi:10.1002/gps.1643. PMID 17096455. S2CID 45660235.
- Abraha I, Rimland JM, Trotta FM, Dell'Aquila G, Cruz-Jentoft A, Petrovic M, et al. (March 2017). "Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series". BMJ Open. 7 (3): e012759. doi:10.1136/bmjopen-2016-012759. PMC 5372076. PMID 28302633.
- Chung JC, Lai CK, Chung PM, French HP (2002). "Snoezelen for dementia". The Cochrane Database of Systematic Reviews. 2010 (4): CD003152. doi:10.1002/14651858.CD003152. PMC 9002239. PMID 12519587.
- Woods B, O'Philbin L, Farrell EM, Spector AE, Orrell M (March 2018). "Reminiscence therapy for dementia". The Cochrane Database of Systematic Reviews. 2018 (3): CD001120. doi:10.1002/14651858.CD001120.pub3. PMC 6494367. PMID 29493789.
- Zetteler J (November 2008). "Effectiveness of simulated presence therapy for individuals with dementia: a systematic review and meta-analysis". Aging & Mental Health. 12 (6): 779–785. doi:10.1080/13607860802380631. PMID 19023729. S2CID 39529938.
- Spector A, Thorgrimsen L, Woods B, Royan L, Davies S, Butterworth M, et al. (September 2003). "Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial". The British Journal of Psychiatry. 183 (3): 248–254. doi:10.1192/bjp.183.3.248. PMID 12948999.
- Gitlin LN, Corcoran M, Winter L, Boyce A, Hauck WW (February 2001). "A randomized, controlled trial of a home environmental intervention: effect on efficacy and upset in caregivers and on daily function of persons with dementia". The Gerontologist. 41 (1): 4–14. doi:10.1093/geront/41.1.4. PMID 11220813.
- Gitlin LN, Hauck WW, Dennis MP, Winter L (March 2005). "Maintenance of effects of the home environmental skill-building program for family caregivers and individuals with Alzheimer's disease and related disorders". The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 60 (3): 368–374. doi:10.1093/gerona/60.3.368. PMID 15860476.
- "Treating Behavioral and Psychiatric Symptoms". Alzheimer's Association. 2006. Archived from the original on 25 September 2006. Retrieved 25 September 2006.
- Dunne TE, Neargarder SA, Cipolloni PB, Cronin-Golomb A (August 2004). "Visual contrast enhances food and liquid intake in advanced Alzheimer's disease". Clinical Nutrition. 23 (4): 533–538. doi:10.1016/j.clnu.2003.09.015. PMID 15297089.
- Dudek SB (2007). Nutrition Essentials for Nursing Practice. Hagerstown, Maryland: Lippincott Williams & Wilkins. p. 360. ISBN 978-0-7817-6651-7. Retrieved 19 August 2008.
- Dennehy C (2006). "Analysis of patients' rights: dementia and PEG insertion". British Journal of Nursing. 15 (1): 18–20. doi:10.12968/bjon.2006.15.1.20303. PMID 16415742.
- Chernoff R (April 2006). "Tube feeding patients with dementia". Nutrition in Clinical Practice. 21 (2): 142–146. doi:10.1177/0115426506021002142. PMID 16556924. S2CID 20841502.
- Shega JW, Levin A, Hougham GW, Cox-Hayley D, Luchins D, Hanrahan P, et al. (April 2003). "Palliative Excellence in Alzheimer Care Efforts (PEACE): a program description". Journal of Palliative Medicine. 6 (2): 315–320. doi:10.1089/109662103764978641. PMID 12854952. S2CID 6072807.
- ^ Dominguez LJ, Barbagallo M (June 2018). "Nutritional prevention of cognitive decline and dementia". Acta Bio-Medica. 89 (2): 276–290. doi:10.23750/abm.v89i2.7401. PMC 6179018. PMID 29957766.
- Cipriani G, Carlesi C, Lucetti C, Danti S, Nuti A (1 December 2016). "Eating Behaviors and Dietary Changes in Patients With Dementia". American Journal of Alzheimer's Disease & Other Dementias. 31 (8): 706–716. doi:10.1177/1533317516673155. ISSN 1533-3175. PMC 10852764. PMID 27756815.
- ^ Zanetti O, Solerte SB, Cantoni F (2009). "Life expectancy in Alzheimer's disease (AD)". Archives of Gerontology and Geriatrics. 49 (Suppl 1): 237–243. doi:10.1016/j.archger.2009.09.035. PMID 19836639.
- "United States Life Tables, 2017" (PDF). National Vital Statistics Reports, CDC. Archived (PDF) from the original on 24 May 2021. Retrieved 10 June 2021.
- ^ Mölsä PK, Marttila RJ, Rinne UK (March 1995). "Long-term survival and predictors of mortality in Alzheimer's disease and multi-infarct dementia". Acta Neurologica Scandinavica. 91 (3): 159–164. doi:10.1111/j.1600-0404.1995.tb00426.x. PMID 7793228. S2CID 19724937.
- Bowen JD, Malter AD, Sheppard L, Kukull WA, McCormick WC, Teri L, et al. (August 1996). "Predictors of mortality in patients diagnosed with probable Alzheimer's disease". Neurology. 47 (2): 433–439. doi:10.1212/wnl.47.2.433. PMID 8757016. S2CID 24961809.
- Larson EB, Shadlen MF, Wang L, McCormick WC, Bowen JD, Teri L, et al. (April 2004). "Survival after initial diagnosis of Alzheimer disease". Annals of Internal Medicine. 140 (7): 501–509. doi:10.7326/0003-4819-140-7-200404060-00008. PMID 15068977. S2CID 27410149.
- Jagger C, Clarke M, Stone A (January 1995). "Predictors of survival with Alzheimer's disease: a community-based study". Psychological Medicine. 25 (1): 171–177. doi:10.1017/S0033291700028191. PMID 7792352. S2CID 34066330.
- Dodge HH, Shen C, Pandav R, DeKosky ST, Ganguli M (February 2003). "Functional transitions and active life expectancy associated with Alzheimer disease". Archives of Neurology. 60 (2): 253–259. doi:10.1001/archneur.60.2.253. PMID 12580712.
- Ganguli M, Dodge HH, Shen C, Pandav RS, DeKosky ST (May 2005). "Alzheimer disease and mortality: a 15-year epidemiological study". Archives of Neurology. 62 (5): 779–784. doi:10.1001/archneur.62.5.779. PMID 15883266.
- Lanni C, Masi M, Racchi M, Govoni S (January 2021). "Cancer and Alzheimer's disease inverse relationship: an age-associated diverging derailment of shared pathways". Molecular Psychiatry. 26 (1): 280–295. doi:10.1038/s41380-020-0760-2. PMID 32382138.
- ^ Bermejo-Pareja F, Benito-León J, Vega S, Medrano MJ, Román GC (January 2008). "Incidence and subtypes of dementia in three elderly populations of central Spain". Journal of the Neurological Sciences. 264 (1–2): 63–72. doi:10.1016/j.jns.2007.07.021. PMID 17727890. S2CID 34341344.
- ^ Di Carlo A, Baldereschi M, Amaducci L, Lepore V, Bracco L, Maggi S, et al. (January 2002). "Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study". Journal of the American Geriatrics Society. 50 (1): 41–48. doi:10.1046/j.1532-5415.2002.50006.x. PMID 12028245. S2CID 22576935.
- Tejada-Vera B. (2013). Mortality from Alzheimer's Disease in the United States: Data for 2000 and 2010. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
- Reitz C, Rogaeva E, Beecham GW (October 2020). "Late-onset vs nonmendelian early-onset Alzheimer disease: A distinction without a difference?". Neurology. Genetics. 6 (5): e512. doi:10.1212/NXG.0000000000000512. PMC 7673282. PMID 33225065.
- ^ Liu CC, Liu CC, Kanekiyo T, Xu H, Bu G (February 2013). "Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy". Nature Reviews. Neurology. 9 (2): 106–118. doi:10.1038/nrneurol.2012.263. PMC 3726719. PMID 23296339.
- Massett HA, Mitchell AK, Alley L, Simoneau E, Burke P, Han SH, et al. (29 June 2021). "Facilitators, Challenges, and Messaging Strategies for Hispanic/Latino Populations Participating in Alzheimer's Disease and Related Dementias Clinical Research: A Literature Review". Journal of Alzheimer's Disease. 82 (1): 107–127. doi:10.3233/JAD-201463. PMID 33998537. S2CID 234745473.
- Huynh RA, Mohan C (2017). "Alzheimer's Disease: Biomarkers in the Genome, Blood, and Cerebrospinal Fluid". Frontiers in Neurology. 8: 102. doi:10.3389/fneur.2017.00102. PMC 5357660. PMID 28373857.
- Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA (May 2021). "Population estimate of people with clinical Alzheimer's disease and mild cognitive impairment in the United States (2020-2060)". Alzheimer's & Dementia. 17 (12): 1966–1975. doi:10.1002/alz.12362. PMC 9013315. PMID 34043283. S2CID 235215290.
- Rizzi L, Rosset I, Roriz-Cruz M (2014). "Global epidemiology of dementia: Alzheimer's and vascular types". Biomed Res Int. 2014: 908915. doi:10.1155/2014/908915. PMC 4095986. PMID 25089278.
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. (December 2005). "Global prevalence of dementia: a Delphi consensus study". Lancet. 366 (9503): 2112–2117. doi:10.1016/S0140-6736(05)67889-0. PMC 2850264. PMID 16360788.
- Li F, Qin W, Zhu M, Jia J (1 January 2021). "Model-Based Projection of Dementia Prevalence in China and Worldwide: 2020-2050". Journal of Alzheimer's Disease. 82 (4). IOS Press: 1823–1831. doi:10.3233/JAD-210493. PMID 34219732. S2CID 235735045.
- Nichols E, Steinmetz JD, Vollset SE, Vos T, Fukutaki K, Chalek J (6 January 2022). "Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019". The Lancet Public Health. 7 (2): e105 – e125. doi:10.1016/S2468-2667(21)00249-8. hdl:2440/135555. ISSN 2468-2667. PMC 8810394. PMID 34998485.
- Auguste D.:
- Alzheimer A (1907). "Über eine eigenartige Erkrankung der Hirnrinde" [About a peculiar disease of the cerebral cortex]. Allgemeine Zeitschrift für Psychiatrie und Psychisch-Gerichtlich Medizin (in German). 64 (1–2): 146–148.
- "About a peculiar disease of the cerebral cortex. By Alois Alzheimer, 1907 (Translated by L. Jarvik and H. Greenson)". Alzheimer Disease and Associated Disorders. 1 (1). Translated by H. Greenson: 3–8. 1987. PMID 3331112.
- Maurer U, Maurer K (2003). Alzheimer: The Life of a Physician and the Career of a Disease. New York: Columbia University Press. p. 270. ISBN 978-0-231-11896-5.
- Berrios GE (1990). "Alzheimer's Disease: A Conceptual History". Int. J. Geriatr. Psychiatry. 5 (6): 355–365. doi:10.1002/gps.930050603. S2CID 145155424.
- Kraepelin E (2007). Clinical Psychiatry: A Textbook For Students And Physicians (Reprint). Translated by Diefendorf AR. Kessinger Publishing. p. 568. ISBN 978-1-4325-0833-3.
- Katzman R, Terry RD, Bick KL, eds. (1978). Alzheimer's Disease: Senile Dementia and Related Disorders. New York: Raven Press. p. 595. ISBN 978-0-89004-225-0.
- Boller F, Forbes MM (June 1998). "History of dementia and dementia in history: an overview". Journal of the Neurological Sciences. 158 (2): 125–133. doi:10.1016/S0022-510X(98)00128-2. PMID 9702682. S2CID 42399340.
- Amaducci LA, Rocca WA, Schoenberg BS (November 1986). "Origin of the distinction between Alzheimer's disease and senile dementia: how history can clarify nosology". Neurology. 36 (11): 1497–1499. doi:10.1212/wnl.36.11.1497. PMID 3531918. S2CID 7689479.
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (July 1984). "Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease". Neurology. 34 (7): 939–944. doi:10.1212/wnl.34.7.939. PMID 6610841. S2CID 11646075.
- Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, et al. (August 2007). "Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria". The Lancet. Neurology. 6 (8): 734–746. doi:10.1016/S1474-4422(07)70178-3. PMID 17616482. S2CID 7356809.
- Blacker D, Albert MS, Bassett SS, Go RC, Harrell LE, Folstein MF (December 1994). "Reliability and validity of NINCDS-ADRDA criteria for Alzheimer's disease. The National Institute of Mental Health Genetics Initiative". Archives of Neurology. 51 (12): 1198–1204. doi:10.1001/archneur.1994.00540240042014. PMID 7986174.
- ^ El-Hayek YH, Wiley RE, Khoury CP, Daya RP, Ballard C, Evans AR, et al. (2019). "Tip of the Iceberg: Assessing the Global Socioeconomic Costs of Alzheimer's Disease and Related Dementias and Strategic Implications for Stakeholders". Journal of Alzheimer's Disease. 70 (2): 323–341. doi:10.3233/JAD-190426. PMC 6700654. PMID 31256142.
- ^ Wong W (August 2020). "Economic burden of Alzheimer disease and managed care considerations". Am J Manag Care. 26 (8 Suppl): S177 – S183. doi:10.37765/ajmc.2020.88482. PMID 32840331. S2CID 221308149. Archived from the original on 25 February 2022. Retrieved 17 March 2022.
- ^ Tahami Monfared AA, Byrnes MJ, White LA, Zhang Q (February 2022). "The Humanistic and Economic Burden of Alzheimer's Disease". Neurol Ther. 11 (2): 525–551. doi:10.1007/s40120-022-00335-x. PMC 9095804. PMID 35192176. S2CID 247014076.
- ^ Kosaner Kließ M, Martins R, Connolly MP (2021). "Major Cost Drivers in Assessing the Economic Burden of Alzheimer's Disease: A Structured, Rapid Review". J Prev Alzheimers Dis. 8 (3): 362–370. doi:10.14283/jpad.2021.17. PMID 34101795. S2CID 233403683.
- Demirbas M, Hahn-Pedersen JH, Jørgensen HL (August 2023). "Comparison Between Burden of Care Partners of Individuals with Alzheimer's Disease Versus Individuals with Other Chronic Diseases". Neurology and Therapy. 12 (4): 1051–1068. doi:10.1007/s40120-023-00493-6. PMC 10310688. PMID 37222859.
- "The MetLife study of Alzheimer's disease: The caregiving experience" (PDF). MetLife Mature Market Institute. August 2006. Archived from the original (PDF) on 8 January 2011. Retrieved 5 February 2011.
- Schneider J, Murray J, Banerjee S, Mann A (August 1999). "EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: I—Factors associated with carer burden". International Journal of Geriatric Psychiatry. 14 (8): 651–661. doi:10.1002/(SICI)1099-1166(199908)14:8<651::AID-GPS992>3.0.CO;2-B. PMID 10489656. S2CID 27346798.
- Murray J, Schneider J, Banerjee S, Mann A (August 1999). "EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: II—A qualitative analysis of the experience of caregiving". International Journal of Geriatric Psychiatry. 14 (8): 662–667. doi:10.1002/(SICI)1099-1166(199908)14:8<662::AID-GPS993>3.0.CO;2-4. PMID 10489657. S2CID 41741923.
- ^ Zhu CW, Sano M (2006). "Economic considerations in the management of Alzheimer's disease". Clinical Interventions in Aging. 1 (2): 143–154. doi:10.2147/ciia.2006.1.2.143. PMC 2695165. PMID 18044111.
- Gaugler JE, Kane RL, Kane RA, Newcomer R (April 2005). "Early community-based service utilization and its effects on institutionalization in dementia caregiving". The Gerontologist. 45 (2): 177–185. doi:10.1093/geront/45.2.177. PMID 15799982.
- Ritchie K, Lovestone S (November 2002). "The dementias". Lancet. 360 (9347): 1759–1766. doi:10.1016/S0140-6736(02)11667-9. PMID 12480441. S2CID 21404062.
- Brodaty H, Hadzi-Pavlovic D (September 1990). "Psychosocial effects on carers of living with persons with dementia". The Australian and New Zealand Journal of Psychiatry. 24 (3): 351–361. doi:10.3109/00048679009077702. PMID 2241719. S2CID 11788466.
- Donaldson C, Tarrier N, Burns A (April 1998). "Determinants of carer stress in Alzheimer's disease". International Journal of Geriatric Psychiatry. 13 (4): 248–256. doi:10.1002/(SICI)1099-1166(199804)13:4<248::AID-GPS770>3.0.CO;2-0. PMID 9646153. S2CID 22187694.
- Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM (4 April 2013). "Monetary Costs of Dementia in the United States". New England Journal of Medicine. 368 (14): 1326–1334. doi:10.1056/NEJMsa1204629. PMC 3959992. PMID 23550670.
- Nandi A, Counts N, Bröker J, Malik S, Chen S, Han R, et al. (8 February 2024). "Cost of care for Alzheimer's disease and related dementias in the United States: 2016 to 2060". npj Aging. 10 (1): 13. doi:10.1038/s41514-024-00136-6. PMC 10853249. PMID 38331952.
- Pusey H, Richards D (May 2001). "A systematic review of the effectiveness of psychosocial interventions for carers of people with dementia". Aging & Mental Health. 5 (2): 107–119. doi:10.1080/13607860120038302. PMID 11511058. S2CID 32517015.
- Bayley J (2000). Iris: A Memoir of Iris Murdoch. London: Abacus. ISBN 978-0-349-11215-2. OCLC 41960006.
- Sparks N (1996). The notebook. Thorndike, Maine: Thorndike Press. p. 268. ISBN 978-0-7862-0821-0.
- "Thanmathra". Webindia123.com. Archived from the original on 6 November 2007. Retrieved 24 January 2008.
- Ogiwara H (2004). Ashita no Kioku (in Japanese). Tōkyō: Kōbunsha. ISBN 978-4-334-92446-1. OCLC 57352130.
- Munro A (2001). Hateship, Friendship, Courtship, Loveship, Marriage: Stories. New York: A.A. Knopf. ISBN 978-0-375-41300-1. OCLC 46929223.
- "Malcolm and Barbara: A love story". Dfgdocs. Archived from the original on 24 May 2008. Retrieved 24 January 2008.
- "Malcolm and Barbara: A love story". BBC Cambridgeshire. Archived from the original on 10 November 2012. Retrieved 2 March 2008.
- Plunkett J (7 August 2007). "Alzheimer's film-maker to face ITV lawyers". London: Guardian Media. Archived from the original on 15 January 2008. Retrieved 24 January 2008.
- "The Caretaker: Persistent Repetition of Phrases". Fact. 26 August 2009. Archived from the original on 15 April 2021. Retrieved 9 April 2021.
- Powell M (14 June 2011). "The Caretaker: An Empty Bliss Beyond This World Album Review". Pitchfork. Archived from the original on 18 June 2011. Retrieved 19 February 2021.
- Ezra M (23 October 2020). "Why Are TikTok Teens Listening to an Album About Dementia?". The New York Times. Archived from the original on 23 October 2020. Retrieved 21 April 2021.
- Gerrard N (19 July 2015). "Words fail us: dementia and the arts". The Guardian. Archived from the original on 19 July 2015. Retrieved 14 June 2021.
- Grady D (24 October 2006). "Self-Portraits Chronicle a Descent Into Alzheimer's". The New York Times. Archived from the original on 24 October 2006. Retrieved 14 June 2021.
- Shi M, Chu F, Zhu F, Zhu J (2022). "Impact of Anti-amyloid-β Monoclonal Antibodies on the Pathology and Clinical Profile of Alzheimer's Disease: A Focus on Aducanumab and Lecanemab". Frontiers in Aging Neuroscience. 14: 870517. doi:10.3389/fnagi.2022.870517. PMC 9039457. PMID 35493943.
- Cummings J, Zhou Y, Lee G, Zhong K, Fonseca J, Cheng F (2023). "Alzheimer's disease drug development pipeline: 2023". Alzheimer's & Dementia. 9 (2): e12385. doi:10.1002/trc2.12385. PMC 10210334. PMID 37251912.
- "How Is Alzheimer's Disease Treated?". U.S. National Institute on Aging. 1 April 2023. Retrieved 10 July 2023.
- Vaz M, Silva V, Monteiro C, Silvestre S (2022). "Role of Aducanumab in the Treatment of Alzheimer's Disease: Challenges and Opportunities". Clinical Interventions in Aging. 17: 797–810. doi:10.2147/CIA.S325026. PMC 9124475. PMID 35611326.
- Day GS, Scarmeas N, Dubinsky R, Coerver K, Mostacero A, West B, et al. (April 2022). "Aducanumab Use in Symptomatic Alzheimer Disease Evidence in Focus: A Report of the AAN Guidelines Subcommittee". Neurology. 98 (15): 619–631. doi:10.1212/wnl.0000000000200176. PMC 9012273. PMID 35197360.
- Mahase E (June 2021). "Three FDA advisory panel members resign over approval of Alzheimer's drug". BMJ. 373: n1503. doi:10.1136/bmj.n1503. PMID 34117086. S2CID 235405355. Archived from the original on 8 July 2023. Retrieved 7 July 2023.
- Belluck P, Robbins R (10 June 2021). "Three F.D.A. Advisers Resign Over Agency's Approval of Alzheimer's Drug". The New York Times. Archived from the original on 14 November 2021. Retrieved 7 July 2023.
- Abyadeh M, Gupta V, Gupta V, Chitranshi N, Wu Y, Amirkhani A, et al. (December 2021). "Comparative Analysis of Aducanumab, Zagotenemab and Pioglitazone as Targeted Treatment Strategies for Alzheimer's Disease". Aging and Disease. 12 (8): 1964–1976. doi:10.14336/AD.2021.0719. PMC 8612603. PMID 34881080.
- ^ Wade G (3 August 2024). "The truth about Alzheimer's drugs". New Scientist. p. 14.
- ^ Wade G (3 August 2024). "The truth about Alzheimer's drugs". New Scientist. p. 15.
- Marsool MD, Prajjwal P, Reddy YB, Marsool AD, Lam JR, Nandwana V (May 2023). "Newer modalities in the management of Alzheimer's dementia along with the role of aducanumab and lecanemab in the treatment of its refractory cases". Disease-a-Month. 69 (5): 101547. doi:10.1016/j.disamonth.2023.101547. PMID 36931947. S2CID 257568052.
- "FDA Grants Accelerated Approval for Alzheimer's Disease Treatment" (Press release). U.S. Food and Drug Administration (FDA). 6 January 2023. Archived from the original on 7 January 2023. Retrieved 7 January 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "Lecanemab Summary Review" (PDF). U.S. Food and Drug Administration (FDA). Archived (PDF) from the original on 7 January 2023. Retrieved 7 January 2023.
- "FDA Converts Novel Alzheimer's Disease Treatment to Traditional Approval". U.S. Food and Drug Administration (FDA) (Press release). 6 July 2023. Retrieved 6 July 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "FDA Makes Alzheimer's Drug Leqembi Widely Accessible". The New York Times. 6 July 2023. Archived from the original on 7 July 2023. Retrieved 8 July 2023.
- "FDA approves treatment for adults with Alzheimer's disease". U.S. Food and Drug Administration (FDA) (Press release). 2 July 2024. Archived from the original on 2 July 2024. Retrieved 2 July 2024.
- Alves F, Kalinowski P, Ayton S (May 2023). "Accelerated Brain Volume Loss Caused by Anti-β-Amyloid Drugs: A Systematic Review and Meta-analysis". Neurology. 100 (20): e2114 – e2124. doi:10.1212/WNL.0000000000207156. PMC 10186239. PMID 36973044.
- "Alpha Cognition's Oral Therapy Zunveyl Receives FDA Approval to Treat Alzheimer's Disease" (Press release). Alpha Cognition. 29 July 2024. Retrieved 4 August 2024 – via Business Wire.
- ^ McDade E, Llibre-Guerra JJ, Holtzman DM, Morris JC, Bateman RJ (July 2021). "The informed road map to prevention of Alzheimer Disease: A call to arms". Mol Neurodegener. 16 (1): 49. doi:10.1186/s13024-021-00467-y. PMC 8293489. PMID 34289882.
- Lemche E (November 2018). "Early Life Stress and Epigenetics in Late-onset Alzheimer's Dementia: A Systematic Review". Curr Genomics. 19 (7): 522–602. doi:10.2174/1389202919666171229145156. PMC 6194433. PMID 30386171.
- Galle SA, Geraedts IK, Deijen JB, Milders MV, Drent ML (2020). "The Interrelationship between Insulin-Like Growth Factor 1, Apolipoprotein E ε4, Lifestyle Factors, and the Aging Body and Brain". J Prev Alzheimers Dis. 7 (4): 265–273. doi:10.14283/jpad.2020.11. PMID 32920629. S2CID 214784366.
- Li Q, Yang X, Xu J, Guo Y, He X, Hu H, et al. (February 2023). "Early prediction of Alzheimer's disease and related dementias using real-world electronic health records". Alzheimer's & Dementia. 19 (8): 3506–3518. doi:10.1002/alz.12967. PMC 10976442. PMID 36815661. S2CID 257101613.
- Scott K, Klaus SP (6 August 2024). "Focused ultrasound therapy for Alzheimer's disease: exploring the potential for targeted amyloid disaggregation". Frontiers in Neurology. 15. doi:10.3389/fneur.2024.1426075. PMC 11333319. PMID 39165269.
Further reading
- Van Acker ZP, Perdok A, Bretou M, Annaert W (November 2021). "The microglial lysosomal system in Alzheimer's disease: Guardian against proteinopathy". Ageing Research Reviews. 71: 101444. doi:10.1016/j.arr.2021.101444. PMID 34391945. S2CID 236994329.
- Xi Y, Chen Y, Jin Y, Han G, Song M, Song T, et al. (May 2022). "Versatile nanomaterials for Alzheimer's disease: Pathogenesis inspired disease-modifying therapy". Journal of Controlled Release. 345: 38–61. doi:10.1016/j.jconrel.2022.02.034. PMID 35257810. S2CID 247285338.
- Prasanalakshmi B, Mousmi A, Syeda M, Anandhavalli M, Linda E (January 2023). "Hybridized Deep Learning Approach for Detecting Alzheimer's Disease". Biomedicines. 11 (4): 4–8. doi:10.3390/biomedicines11010149. PMC 9855764. PMID 9855764. S2CID 255745038.
External links
- "Alzheimer's Disease Research Timeline – Alzforum". www.alzforum.org.
- "Alzheimer's Disease Brain Cell Atlas- brain-map.org". portal.brain-map.org.
| Classification | D |
|---|---|
| External resources |
| Mental disorders (Classification) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
| Diseases of the nervous system, primarily CNS | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inflammation |
| ||||||||||||||||||||||||
| Brain/ encephalopathy |
| ||||||||||||||||||||||||
| Both/either |
| ||||||||||||||||||||||||
| Amyloidosis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Common amyloid forming proteins | |||||||||||
| Systemic amyloidosis | |||||||||||
| Organ-limited amyloidosis |
| ||||||||||