| Revision as of 14:54, 14 October 2008 editEpbr123 (talk | contribs)291,700 editsm Reverted edits by 204.38.171.25 to last version by Frankenpuppy (HG)← Previous edit | Latest revision as of 19:37, 19 December 2024 edit undo156.57.90.101 (talk) Fixed grammar/terminologyTags: Mobile edit Mobile app edit iOS app edit App section source | ||
| Line 1: | Line 1: | ||
| {{short description| Inflammation of the eye}} | |||
| {{DiseaseDisorder infobox | | |||
| {{Redirect|Pinkeye|other uses|Pinkeye (disambiguation)}} | |||
| Name = Conjunctivitis | | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| ICD10 = {{ICD10|H|10||h|10}} | | |||
| {{Use dmy dates|date=January 2018}} | |||
| ICD9 = {{ICD9|372.0}} | | |||
| {{More citations needed|date=May 2024}}{{Infobox medical condition (new) | |||
| Image = Pink_eye.jpg | | |||
| |
| name = Conjunctivitis | ||
| |
| image = An eye with viral conjunctivitis.jpg | ||
| | caption = An eye with viral conjunctivitis | |||
| MedlinePlus = 001010 | | |||
| | field = ], ] | |||
| eMedicineSubj = emerg | | |||
| | synonyms = Pink eye | |||
| eMedicineTopic = 110 | | |||
| | symptoms = ], scratchiness<ref name=NIH2015/> | |||
| DiseasesDB = 3067 | | |||
| | complications = | |||
| | onset = | |||
| | duration = Viral conjunctivitis: up to two weeks<ref>{{Cite book | vauthors = Long SS, Prober CG, Fischer M |url=https://books.google.com/books?id=Xw7VDgAAQBAJ&pg=PA502 |title=Principles and Practice of Pediatric Infectious Diseases E-Book |date=2017 |publisher=Elsevier Health Sciences |isbn=978-0-323-46132-0 |page=502 |language=en}}</ref> | |||
| | causes = ], ], allergies<ref name=Az2013/> | |||
| | risks = | |||
| | diagnosis = Based on symptoms, ]<ref name=NIH2015/> | |||
| | differential = | |||
| | prevention = ]<ref name=NIH2015/> | |||
| | treatment = Based on underlying cause<ref name=Az2013/> | |||
| | medication = | |||
| | prognosis = | |||
| | frequency = 3–6 million per year (US)<ref name=NIH2015/><ref name=Az2013/> | |||
| | deaths = | |||
| }} | }} | ||
| '''Conjunctivitis''' (commonly called "'''Pink Eye'''" or "'''Red Eye'''" in North America, and "'''Madras eye'''" in India <ref></ref>) is an inflammation of the ] (the outermost layer of the ] and the inner surface of the ]s), most commonly due to an ] or an ] (usually ], but sometimes ]). | |||
| '''Conjunctivitis''', also known as '''pink eye''' or '''Madras eye''',<ref>{{Cite web |title=What is Viral Conjunctivitis a.k.a. Sore Eyes? | National Institutes of Health |url=http://nih.upm.edu.ph/health/what-viral-conjunctivitis-aka-sore-eyes}}</ref><ref>{{cite journal | vauthors = Mohanasundaram AS, Gurnani B, Kaur K, Manikkam R | title = Madras eye outbreak in India: Why should we foster a better understanding of acute conjunctivitis? | journal = Indian Journal of Ophthalmology | volume = 71 | issue = 5 | pages = 2298–2299 | date = May 2023 | pmid = 37202982 | pmc = 10391441 | doi = 10.4103/IJO.IJO_3317_22 | doi-access = free }}</ref> is ] of the ] and the inner surface of the ].<ref name="Peads10">{{cite journal | vauthors = Richards A, Guzman-Cottrill JA | title = Conjunctivitis | journal = Pediatrics in Review | volume = 31 | issue = 5 | pages = 196–208 | date = May 2010 | pmid = 20435711 | doi = 10.1542/pir.31-5-196 | s2cid = 245084568 }}</ref> It makes the eye appear pink or reddish.<ref name=NIH2015/> Pain, burning, scratchiness, or itchiness may occur.<ref name=NIH2015/> The affected eye may have increased tears or be "stuck shut" in the morning.<ref name=NIH2015/> Swelling of the ] may also occur.<ref name=NIH2015/> Itching is more common in cases due to allergies.<ref name=Az2013/> Conjunctivitis can affect one or both eyes.<ref name=NIH2015/> | |||
| ==Variants== | |||
| '''Blepharoconjunctivitis''' is the combination of conjunctivitis with ] (inflammation of the ]s). | |||
| The most common infectious causes in adults are viral, whereas in children bacterial causes predominate.<ref name="Durand 2023">{{cite journal | vauthors = Durand ML, Barshak MB, Sobrin L | title = Eye Infections | journal = The New England Journal of Medicine | volume = 389 | issue = 25 | pages = 2363–2375 | date = December 2023 | pmid = 38118024 | doi = 10.1056/NEJMra2216081 | s2cid = 266433325 }}</ref><ref name="Az2013">{{cite journal | vauthors = Azari AA, Barney NP | title = Conjunctivitis: a systematic review of diagnosis and treatment | journal = JAMA | volume = 310 | issue = 16 | pages = 1721–1729 | date = October 2013 | pmid = 24150468 | pmc = 4049531 | doi = 10.1001/jama.2013.280318 }}</ref> The viral infection may occur along with other symptoms of a ].<ref name=NIH2015/> Both viral and bacterial cases are easily spread between people.<ref name=NIH2015/> Allergies to pollen or animal hair are also a common cause.<ref name=Az2013/> Diagnosis is often based on signs and symptoms.<ref name=NIH2015/> Occasionally, a sample of the discharge is sent for ].<ref name=NIH2015/> | |||
| ''']''' is the combination of conjunctivitis and ] (]l inflammation). | |||
| <!-- Prevention and treatment --> | |||
| ''']''' is an ] condition that produces a similar appearance to conjunctivitis, but without discharge or tearing. | |||
| Prevention is partly by ].<ref name=NIH2015/> Treatment depends on the underlying cause.<ref name="NIH2015">{{Cite web |date=November 2015 |title=Facts About Pink Eye |url=https://nei.nih.gov/health/pinkeye/pink_facts |url-status=live |archive-url=https://web.archive.org/web/20160309104846/https://nei.nih.gov/health/pinkeye/pink_facts |archive-date=9 March 2016 |access-date=8 March 2016 |website=National Eye Institute |df=dmy-all}}</ref> In the majority of viral cases, there is no specific treatment.<ref name=Az2013/> Most cases due to a bacterial infection also resolve without treatment; however, ]s can shorten the illness.<ref name=NIH2015/><ref name=Az2013/> People who wear ] and those whose infection is caused by ] or ] should be treated.<ref name=Az2013/> Allergic cases can be treated with ]s or ] drops.<ref name=Az2013/> | |||
| About 3 to 6 million people get acute conjunctivitis each year in the United States.<ref name=NIH2015/><ref name=Az2013/> Typically, people get better in one or two weeks.<ref name=NIH2015/><ref name=Az2013/> If visual loss, significant pain, sensitivity to light or signs of ] occur, or if symptoms do not improve after a week, further diagnosis and treatment may be required.<ref name=Az2013/> Conjunctivitis in a newborn, known as ], may also require specific treatment.<ref name=NIH2015/> | |||
| Conjunctivitis has many different possible causes. It can be caused by ], ] (including ]), ], or ]s such as ], feces particles, dirt, smoke, or ] (from pool water).<ref name=webmd></ref> | |||
| {{TOC limit}} | |||
| == Signs and symptoms == | |||
| The viral and bacterial forms of conjunctivitis are contagious, and can therefore be caused by coming in contact with another individual who is already infected.<ref name=webmd /> | |||
| ] | |||
| ], ], and ] of the eyes are symptoms common to all forms of conjunctivitis. However, the pupils should be normally reactive, and the visual acuity normal.<ref>{{cite book | vauthors = Hashmi MF, Gurnani B, Benson S | chapter = Conjunctivitis |date=2023 | title = StatPearls | chapter-url=http://www.ncbi.nlm.nih.gov/books/NBK541034/ |access-date=2023-05-23 |place=Treasure Island (FL) |publisher=StatPearls Publishing |pmid=31082078 }}</ref> | |||
| ===Symptoms=== | |||
| ] | |||
| Redness (]), irritation (]) and watering (]) of the eyes are symptoms common to all forms of conjunctivitis. Itch and the closing of the throat is variable. | |||
| Conjunctivitis is identified by inflammation of the conjunctiva, manifested by irritation and redness. Examination using a ] (biomicroscope) may improve diagnostic accuracy. Examination of the palpebral conjunctiva, that overlying the inner aspects of the eyelids, is usually more diagnostic than examination of the bulbal conjunctiva, that overlying the sclera.{{citation needed|date=September 2022}} | |||
| Acute ''allergic conjunctivitis'' is typically itchy, sometimes distressingly so, and often involves some lid swelling. Chronic allergy often causes just itch or irritation. | |||
| === Viral === | |||
| <!-- Image with unknown copyright status removed: ] --> | |||
| ] | |||
| ''Viral conjunctivitis'' is often associated with an infection of the upper ], a ], and/or a ]. Its symptoms include watery discharge and variable itch. The infection usually begins with one eye, but may spread easily to the other. | |||
| Approximately 80% of cases of conjunctivitis in adults and less than 20% in children are due to viruses, with 65% to 90% of these cases being attributed to adenoviruses.<ref name="Az2013"/><ref name="Durand 2023" /> | |||
| Viral conjunctivitis is often associated with an infection of the upper respiratory tract, a common cold, or a sore throat. Other associated signs may include ] lymph node swelling and contact with another person with a red eye.<ref name="Durand 2023" /> Eye pain may be present if the cornea is also involved.<ref name="Durand 2023" /> Its symptoms include excessive watering and itching. The discharge in viral conjunctivitis is usually (but not always) watery in nature.<ref name="Durand 2023" /> The infection usually begins in one eye but may spread easily to the other eye.{{citation needed|date=February 2023}} | |||
| Viral conjunctivitis manifests as a fine, diffuse pinkness of the conjunctiva which may be mistaken for ], but corroborative signs on ], particularly numerous ]s on the ] conjunctiva, and sometimes a ] are seen.{{citation needed|date=February 2023}} | |||
| ''Bacterial conjunctivitis'' due to the common ] (pus-producing) bacteria causes marked grittiness/irritation and a stringy, opaque, grey or yellowish ] (''gowl'', ''goop'', "gunk", "]", ''sleep'', or other regional names) that may cause the lids to stick together (''matting''), especially after sleeping. Another symptom that could be caused by Bacterial Conjunctivitis is severe crusting of the infected eye and the surrounding skin. However discharge is not essential to the diagnosis, contrary to popular belief. Many other bacteria (e.g., '']'' form of ('']''), '']'') can cause a non-exudative but very persistent conjunctivitis without much redness. The gritty and/or scratchy feeling is sometimes localised enough for patients to insist they must have a foreign body in the eye. The more acute ] infections can be painful. Like viral conjunctivitis, it usually affects only one eye but may spread easily to the other eye. However, it is dormant in the eye for three days before the patient shows signs of symptoms. | |||
| === Allergic === | |||
| ''Irritant'' or ''toxic conjunctivitis'' is irritable or painful when the infected eye is pointed far down or far up. Discharge and itch are usually absent. This is the only group in which severe pain may occur. | |||
| ] showing conjunctival edema]] | |||
| ] is ] of the conjunctiva due to allergy.<ref name="Bielory">{{cite journal | vauthors = Bielory L, Friedlaender MH | title = Allergic conjunctivitis | journal = Immunology and Allergy Clinics of North America | volume = 28 | issue = 1 | pages = 43–58, vi | date = February 2008 | pmid = 18282545 | doi = 10.1016/j.iac.2007.12.005 | s2cid = 34371872 }}</ref> The specific ]s may differ among patients. Symptoms result from the release of ] and other active substances by ]s, and consist of redness (mainly due to ] of the peripheral small blood vessels), swelling of the conjunctiva, itching, and increased production of tears.{{citation needed|date=September 2022}} | |||
| === |
=== Bacterial === | ||
| ] | |||
| Infection (redness) of the conjunctiva on one or both eyes should be apparent, but may be quite mild. Except in obvious pyogenic or toxic/chemical conjunctivitis, a ] (biomicroscope) is needed to have any confidence in the diagnosis. Examination of the tarsal conjunctiva is usually more diagnostic than the bulbar conjunctiva. | |||
| ] | |||
| ''Allergic conjunctivitis'' shows pale watery swelling or ] of the conjunctiva and sometimes the whole eyelid, often with a ropy, ''non-purulent'' mucoid discharge. There is variable redness. | |||
| Bacteria are responsible for approximately 70% of conjunctivitis in children and less than 20% of cases in adults.<ref name="Durand 2023" /> Common bacteria responsible for bacterial conjunctivitis are '']'' including ], '']'' such as ],<ref>{{Cite web |title=Pink Eye (Conjunctivitis) |url=http://www.medicinenet.com/pink_eye/article.htm |url-status=live |archive-url=https://web.archive.org/web/20130622062209/http://www.medicinenet.com/pink_eye/article.htm |archive-date=22 June 2013 |publisher=MedicineNet |df=dmy-all}}</ref> '']'' species and ].<ref name="Durand 2023" /> Less commonly, ''Chlamydia'' spp. and Niesseria species (] and ]) may be the cause.<ref name="Durand 2023" /><ref name="merck">{{Cite web |title=Acute Bacterial Conjunctivitis – Eye Disorders |url=http://www.merckmanuals.com/professional/eye-disorders/conjunctival-and-scleral-disorders/acute-bacterial-conjunctivitis |url-status=live |archive-url=https://web.archive.org/web/20161228184316/http://www.merckmanuals.com/professional/eye-disorders/conjunctival-and-scleral-disorders/acute-bacterial-conjunctivitis |archive-date=28 December 2016 |access-date=31 December 2016 |website=Merck Manuals Professional Edition |df=dmy-all}}</ref> Infection with '']'' may also cause conjunctivitis, particularly in the ] subtype ].<ref>{{cite journal | vauthors = Saadeh-Jackson S, Rodriguez L, Leffler CT, Freymiller C, Wolf E, Wijesooriya N, Couser NL | title = Ophthalmia neonatorum due to ''Escherichia coli'': A rare cause or an emerging bacterial etiology of neonatal conjunctivitis? | journal = Clinical Case Reports | volume = 10 | issue = 8 | pages = e6201 | date = August 2022 | pmid = 35949413 | pmc = 9354094 | doi = 10.1002/ccr3.6201 }}</ref> Bacterial conjunctivitis usually causes a rapid onset of conjunctival redness, swelling of the eyelid, and a sticky discharge. Typically, symptoms develop first in one eye, but may spread to the other eye within 2–5 days. Conjunctivitis due to common ] bacteria causes marked grittiness or irritation and a stringy, opaque, greyish or yellowish ] that may cause the lids to stick together, especially after sleep. Severe crusting of the infected eye and the surrounding skin may also occur. The gritty or scratchy feeling is sometimes localized enough that patients may insist that they have a foreign body in the eye.{{citation needed|date=September 2022}} | |||
| ] | |||
| ''Viral conjunctivitis'', commonly known as "pink eye", shows a fine diffuse pinkness of the conjunctiva which is easily mistaken for the 'ciliary injection' of ], but there are usually corroborative signs on biomicroscopy, particularly numerous ]s on the tarsal conjunctiva, and sometimes a punctate keratitis. | |||
| Bacteria such as '']'' or '']'' spp. can cause a nonexudative but persistent conjunctivitis without much redness. Bacterial conjunctivitis may cause the production of membranes or pseudomembranes that cover the conjunctiva. Pseudomembranes consist of a combination of ]s and exudates and adhere loosely to the conjunctiva, while true membranes are more tightly adherent and cannot be easily peeled away. Cases of bacterial conjunctivitis that involve the production of membranes or pseudomembranes are associated with '']'', β-hemolytic streptococci, and '']''. ''C. diphtheriae'' causes membrane formation in conjunctiva of unimmunized children.<ref>{{Cite book |title=Epidemiology and Prevention of Vaccine-Preventable Diseases |publisher=U.S. Dept. of Health & Human Services, Centers for Disease Control and Prevention |year=2015 |isbn=978-0-9904491-1-9 |veditors=Hamborsky J, Kroger A, Wolfe C |pages=112}}</ref> | |||
| Pyogenic ''bacterial conjunctivitis'' shows an opaque purulent discharge, a very red eye, and on biomicroscopy there are numerous white cells and desquamated ]s seen in the 'tear gutter' along the lid margin. The tarsal conjunctiva is a velvety red and not particularly follicular. Non-pyogenic infections can show just mild infection and be difficult to diagnose. Scarring of the tarsal conjunctiva is occasionally seen in chronic infections, especially in trachoma. | |||
| === Chemical === | |||
| ''Irritant'' or ''toxic conjunctivitis'' show primarily marked redness. If due to splash injury, it is often present only in the lower conjunctival sac. With some chemicals—above all with caustic alkalis such as ]—there may be necrosis of the conjunctiva with a deceptively white eye due to vascular closure, followed by sloughing of the dead epithelium. This is likely to be associated with slit-lamp evidence of ]. | |||
| Chemical eye injury may result when an ] or ]ne substance gets in the eye.<ref name="Bet09">{{cite journal | vauthors = Zentani A, Burslem J | title = Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 4: use of litmus paper in chemical eye injury | journal = Emergency Medicine Journal | volume = 26 | issue = 12 | pages = 887 | date = December 2009 | pmid = 19934140 | doi = 10.1136/emj.2009.086124 | s2cid = 38124735 }}</ref> Alkali burns are typically worse than acidic burns.<ref name=AFP08/> Mild burns produce conjunctivitis, while more severe burns may cause the ] to turn white.<ref name=AFP08/> ] may be used to test for chemical causes.<ref name=Bet09/> When a chemical cause has been confirmed, the eye or eyes should be flushed until the ] is in the range 6–8.<ref name="AFP08">{{cite journal | vauthors = Hodge C, Lawless M | title = Ocular emergencies | journal = Australian Family Physician | volume = 37 | issue = 7 | pages = 506–509 | date = July 2008 | pmid = 18592066 }}</ref> Anaesthetic eye drops can be used to decrease the pain.<ref name=AFP08/> | |||
| Irritant or toxic conjunctivitis is primarily marked by redness. If due to a chemical splash, it is often present in only the lower conjunctival sac. With some chemicals, above all with caustic alkalis such as ], ] of the conjunctiva marked by a deceptively white eye due to vascular closure may occur, followed by sloughing off of the dead ]. A slit lamp examination is likely to show evidence of ].{{citation needed|date=September 2022}} | |||
| ==Causes== | |||
| === Biomarkers === | |||
| The leading cause of a red, inflamed eye is a bacterial infection. A number of different bacteria can be responsible for the infection. Bacterial pink eye symptoms are usually associated with more of a watery discharge that is not green or yellow in color. Often, bacterial "cold-like" symptoms, such as sinus congestion and runny nose, are also present. The eyelids may be swollen. Sometimes looking at bright lights is painful. While bacterial pink eye may not require an antibiotic, those affected should see a doctor, as occasionally this form of pink eye can be associated with infection of the cornea (the clear portion of the front of the eyeball). This infection must be correctly detected and treated. Bacterial pink eye is highly contagious, but usually resolves in seven to 10 days after symptoms appear. Other causes of a red eye includes drug intake. Notably, marijuana use causes the eyes to turn red temporarily. | |||
| Omics technologies have been used to identify biomarkers that inform on the emergence and progression of conjunctivitis. For example, in chronic inflammatory cicatrizing conjunctivitis, active ], ]s, ]s, and ]s alterations, from which potential biomarkers linked to inflammatory processes were identified.<ref>{{cite journal | vauthors = Di Zazzo A, Yang W, Coassin M, Micera A, Antonini M, Piccinni F, De Piano M, Kohler I, Harms AC, Hankemeier T, Boinini S, Mashaghi A | title = Signaling lipids as diagnostic biomarkers for ocular surface cicatrizing conjunctivitis | journal = Journal of Molecular Medicine | volume = 98 | issue = 5 | pages = 751–760 | date = May 2020 | pmid = 32313985 | pmc = 7220886 | doi = 10.1007/s00109-020-01907-w }}</ref> | |||
| === Other === | |||
| ==Differential diagnosis== | |||
| Conjunctivitis symptoms and signs are relatively non-specific. Even after ], laboratory tests are often necessary if proof of etiology is needed. | |||
| ] | |||
| A ] discharge strongly suggests bacterial cause, unless there is known exposure to toxins. Infection with '']'' should be suspected if the discharge is particularly thick and copious. | |||
| Inclusion conjunctivitis of the newborn is a conjunctivitis that may be caused by the bacterium ''Chlamydia trachomatis'', and may lead to acute, ] conjunctivitis.<ref name="Microbiology">{{Cite book | vauthors = Fisher B, Harvey RP, Champe PC |title=Lippincott's Illustrated Reviews: Microbiology (Lippincott's Illustrated Reviews Series) |publisher=Lippincott Williams & Wilkins |year=2007 |isbn=978-0-7817-8215-9 |location=Hagerstown MD}}</ref> However, it is usually self-healing.<ref name=Microbiology/> | |||
| == Causes == | |||
| Itching (rubbing eyes) is the hallmark symptom of allergic conjunctivitis. Other symptoms include past history of eczema, or asthma. | |||
| Infective conjunctivitis is most commonly caused by a virus.<ref name=Az2013/> Bacterial infections, allergies, other irritants, and dryness are also common causes. Both bacterial and viral infections are contagious, passing from person to person or spread through contaminated objects or water. Contact with contaminated fingers is a common cause of conjunctivitis. Bacteria may also reach the conjunctiva from the edges of the eyelids and the surrounding skin, from the nasopharynx, from infected eye drops or contact lenses, from the genitals or the bloodstream.<ref name=":1" /> Infection by human adenovirus accounts for 65% to 90% of cases of viral conjunctivitis.<ref>{{cite journal | vauthors = Singh MP, Ram J, Kumar A, Rungta T, Gupta A, Khurana J, Ratho RK | title = Molecular epidemiology of circulating human adenovirus types in acute conjunctivitis cases in Chandigarh, North India | journal = Indian Journal of Medical Microbiology | volume = 36 | issue = 1 | pages = 113–115 | date = 2018 | pmid = 29735838 | doi = 10.4103/ijmm.ijmm_17_258 | doi-access = free }}</ref> | |||
| === Viral === | |||
| A diffuse, less "injected" conjunctivitis (looking pink rather than red) suggests a viral cause, especially if numerous follicles are present on the lower tarsal conjunctiva on ]. | |||
| ] are the most common cause of viral conjunctivitis (]).<ref name=Yanoff/> ], caused by ] viruses, can be serious and requires treatment with ]. Acute hemorrhagic conjunctivitis is a highly contagious disease caused by one of two ]es, enterovirus 70 and ] A24. These were first identified in an outbreak in Ghana in 1969, and have spread worldwide since then, causing several epidemics.<ref>{{cite journal | vauthors = Lévêque N, Huguet P, Norder H, Chomel JJ | title = | language = fr | journal = Médecine et Maladies Infectieuses | volume = 40 | issue = 4 | pages = 212–218 | date = April 2010 | pmid = 19836177 | doi = 10.1016/j.medmal.2009.09.006 }}</ref> | |||
| === Bacterial === | |||
| Scarring of the tarsal conjunctiva suggests ], especially if seen in endemic areas, if the scarring is linear (von Arlt's line), or if there is also corneal vascularisation. | |||
| The most common causes of acute bacterial conjunctivitis are '']'', '']'', and '']''.<ref name="Yanoff">{{Cite book | vauthors = Yanoff M, Duker JS |title=Ophthalmology |publisher=Mosby |year=2008 |isbn=978-0-323-05751-6 |edition=3rd |location=Edinburgh |pages=227–236}}</ref><ref>{{Cite web |date=2017-10-02 |title=Protect Yourself From Pink Eye |url=https://www.cdc.gov/conjunctivitis/about/causes.html |access-date=2018-12-07 |website=Centers for Disease Control and Prevention (CDC) |language=en-us}}</ref> Though very rare, hyperacute cases are usually caused by '']'' or '']''. Chronic cases of bacterial conjunctivitis are those lasting longer than 3 weeks, and are typically caused by ''S. aureus'', '']'', or Gram-negative enteric flora.{{citation needed|date=September 2022}} | |||
| === Allergic === | |||
| Clinical tests for lagophthalmos, dry eye (]) and unstable tear film may help distinguish the various types of dry eye. | |||
| Conjunctivitis may also be caused by allergens such as pollen, perfumes, cosmetics, smoke,<ref name="FD">{{Cite web |title=Allergic Conjunctivitis |url=http://familydoctor.org/familydoctor/en/diseases-conditions/allergic-conjunctivitis/causes-risk-factors.html |url-status=live |archive-url=https://web.archive.org/web/20150906031026/http://familydoctor.org/familydoctor/en/diseases-conditions/allergic-conjunctivitis/causes-risk-factors.html |archive-date=6 September 2015 |access-date=18 September 2015 |publisher=familydoctor.org |df=dmy-all}}</ref>{{Unreliable medical source|date=September 2015}} dust mites, ],<ref name="google1">{{Cite book | vauthors = Brooks P |url=https://books.google.com/books?id=eReGG6UtxbcC&pg=PT413 |title=The Daily Telegraph: Complete Guide to Allergies |date=25 October 2012 |publisher=Little, Brown Book |isbn=978-1-4721-0394-9 |access-date=15 April 2014}}{{Dead link|date=September 2023 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> or eye drops.<ref name="MedNews">{{Cite web |title=What Is Allergic Conjunctivitis? What Causes Allergic Conjunctivitis? |url=http://www.medicalnewstoday.com/articles/157692.php |url-status=live |archive-url=https://web.archive.org/web/20100316174827/http://www.medicalnewstoday.com/articles/157692.php |archive-date=16 March 2010 |access-date=6 April 2010 |publisher=medicalnewstoday.com |df=dmy-all}}</ref> The most frequent cause of conjunctivitis is allergic conjunctivitis and it affects 15% to 40% of the population.<ref name=":0" /> Allergic conjunctivitis accounts for 15% of eye related primary care consultations; most including seasonal exposures in the spring and summer or perpetual conditions.<ref>{{cite journal | vauthors = Perkin MR, Bader T, Rudnicka AR, Strachan DP, Owen CG | title = Inter-Relationship between Rhinitis and Conjunctivitis in Allergic Rhinoconjunctivitis and Associated Risk Factors in Rural UK Children | journal = PLOS ONE | volume = 10 | issue = 11 | pages = e0143651 | date = 2015-11-24 | pmid = 26600465 | pmc = 4658044 | doi = 10.1371/journal.pone.0143651 | bibcode = 2015PLoSO..1043651P | doi-access = free }}</ref> | |||
| === Other === | |||
| Other symptoms including pain, blurring of vision and ] should not be prominent in conjunctivitis. Fluctuating blurring is common, due to tearing and mucoid discharge. Mild photophobia is common. However, if any of these symptoms are prominent, it is important to exclude other diseases such as ], ], ] and even ] or ]. | |||
| * ] | |||
| * ] | |||
| * ]: Conjunctivitis is part of the triad of ], which is thought to be caused by ] cross-reactivity following certain bacterial infections. Reactive arthritis is highly associated with ]. Conjunctivitis is associated with the autoimmune disease ].<ref name="Puechal 2014">{{cite journal | vauthors = Puéchal X, Terrier B, Mouthon L, Costedoat-Chalumeau N, Guillevin L, Le Jeunne C | title = Relapsing polychondritis | journal = Joint Bone Spine | volume = 81 | issue = 2 | pages = 118–124 | date = March 2014 | pmid = 24556284 | doi = 10.1016/j.jbspin.2014.01.001 | s2cid = 205754989 }}</ref><ref name="Cantarini 2014">{{cite journal | vauthors = Cantarini L, Vitale A, Brizi MG, Caso F, Frediani B, Punzi L, Galeazzi M, Rigante D | title = Diagnosis and classification of relapsing polychondritis | journal = Journal of Autoimmunity | volume = 48-49 | pages = 53–59 | year = 2014 | pmid = 24461536 | doi = 10.1016/j.jaut.2014.01.026 }}</ref> | |||
| == Diagnosis == | |||
| Many people who have conjunctivitis have trouble opening their eyes in the morning because of the dried mucus on their eyelids. There is often excess mucus over the eye after sleeping for a long period of time. | |||
| ] | |||
| Cultures are not often taken or needed as most cases resolve either with time or typical antibiotics. If bacterial conjunctivitis is suspected, but no response to topical antibiotics is seen, swabs for bacterial culture should be taken and tested. Viral culture may be appropriate in epidemic case clusters.<ref>{{cite book | vauthors = Sheikh A, Hurwitz B | chapter = BACTERIAL CONJUNCTIVITIS 372.05 (Infective Conjunctivitis, Mucopurulent Conjunctivitis, Purulent Conjunctivitis) |date=2008 | title = Roy and Fraunfelder's Current Ocular Therapy |pages=332–334 |publisher=Elsevier |doi=10.1016/b978-1-4160-2447-7.50182-1 |isbn=978-1-4160-2447-7 }}</ref> | |||
| ===Investigations=== | |||
| These are done infrequently because most cases of conjunctivitis are treated empirically and (eventually) successfully, but often only after running the gamut of the common possibilities. | |||
| A ] is used to identify the causative allergen in allergic conjunctivitis.<ref name="google2">{{Cite book | vauthors = Mannis MJ, Macsai MS, Huntley AC |url=https://books.google.com/books?id=FtlsAAAAMAAJ&q=Conjunctivitis+%22patch+test%22 |title=Eye and skin disease |date=1996 |publisher=Lippincott-Raven |isbn=978-0-7817-0269-0 |access-date=23 April 2014 |archive-url=https://web.archive.org/web/20140705035958/http://books.google.com/books?id=FtlsAAAAMAAJ&q=Conjunctivitis+%22patch+test%22&dq=Conjunctivitis+%22patch+test%22&hl=en&sa=X&ei=oY9UU932MMPjsAT5j4KYCg&ved=0CF8Q6AEwBg |archive-date=5 July 2014 |url-status=live |df=dmy-all}}</ref> | |||
| Swabs for bacterial culture are necessary if the history and signs suggest bacterial conjunctivitis, but there is no response to topical ]s. Research studies indicate that many bacteria implicated in low-grade conjunctivitis are not detected by the usual culture methods of medical microbiology labs, so negative results are common. Viral culture may be appropriate in epidemic case clusters. Conjunctival scrapes for ] can be useful in detecting ] and ] infections, ] and ], but are rarely done because of the cost and the general lack of laboratory staff experienced in handling ocular specimens. Conjunctival incisional ] is occasionally done when ] diseases (e.g., ]) or ] are suspected. | |||
| Although conjunctival scrapes for ] can be useful in detecting chlamydial and ] infections, allergies, and ], they are rarely done because of the cost and the general dearth of laboratory staff experienced in handling ocular specimens. Conjunctival incisional biopsy is occasionally done when ] diseases (''e.g.'', ])<ref>{{cite journal | vauthors = Korkmaz Ekren P, Mogulkoc N, Toreyin ZN, Egrilmez S, Veral A, Akalın T, Bacakoglu F | title = Conjunctival Biopsy as a First Choice to Confirm a Diagnosis of Sarcoidosis | journal = Sarcoidosis, Vasculitis, and Diffuse Lung Diseases | volume = 33 | issue = 3 | pages = 196–200 | date = October 2016 | pmid = 27758983 | url = https://pubmed.ncbi.nlm.nih.gov/27758983/ }}</ref> or dysplasia are suspected.<ref>{{cite book | vauthors = Roberts F, Thum CK | chapter = The Conjunctival Biopsy |date=2021 | title = Lee's Ophthalmic Histopathology |pages=343–388 | veditors = Roberts F |place=Cham |publisher=Springer International Publishing |language=en |doi=10.1007/978-3-030-76525-5_11 |isbn=978-3-030-76525-5 }}</ref> | |||
| ==Treatment and management== | |||
| === Classification === | |||
| Conjunctivitis sometimes requires medical attention. The appropriate treatment depends on the cause of the problem. For the allergic type, cool water constricts capillaries, and ] sometimes relieve discomfort in mild cases. In more severe cases, ] and ]s may be prescribed. Some patients with persistent allergic conjunctivitis may also require topical steroid drops. | |||
| Conjunctivitis may be classified either by cause or by extent of the inflamed area.{{citation needed|date=February 2023}} | |||
| ==== Causes ==== | |||
| Bacterial conjunctivitis is usually treated with ] eye drops or ] that cover a broad range of bacteria (] or ] used in UK). However evidence suggests that this does not affect symptom severity and gains only modest reduction in duration from an average of 4.8 days (untreated controls) to 3.3 days for those given immediate antibiotics. Deferring antibiotics yields almost the same duration as those immediately starting treatment with 3.9 days duration, but with half the two-week clinic reattendance rate.<ref>{{cite journal | author=Hazel A Everitt, Paul S Little, Peter W F Smith | title=A randomised controlled trial of management strategies for acute infective conjunctivitis in general practice | journal=BMJ | month=July 16 | year=2006 |doi= 10.1136/bmj.38891.551088.7C | url=http://bmj.bmjjournals.com/cgi/content/short/bmj.38891.551088.7Cv1?etoc | pmid=16847013 | volume=333 | pages=321}}</ref> | |||
| * Allergy | |||
| * Bacteria | |||
| * Viruses | |||
| * Chemicals | |||
| * Autoimmune | |||
| Neonatal conjunctivitis is often grouped separately from bacterial conjunctivitis because it is caused by different bacteria than the more common cases of bacterial conjunctivitis.{{citation needed|date=February 2023}}<!-- Source? --> | |||
| Although there is no specific treatment for viral conjunctivitis, symptomatic relief may be achieved with warm compresses<ref>Medline Plus Medical Encyclopedia, http://www.nlm.nih.gov/medlineplus/ency/article/001010.htm#Treatment, Retrieved 7 April 2008</ref> and artificial tears. For the worst cases, topical corticosteroid drops may be prescribed to reduce the discomfort from inflammation. However prolonged usage of corticosteroid drops increases the risk of side effects. Antibiotic drops may also be used for treatment of complementary infections. Patients are often advised to avoid touching their eyes or sharing towels and washcloths. Viral conjunctivitis usually resolves within 3 weeks. However, in worst cases it may take over a month. | |||
| ==== By extent of involvement ==== | |||
| Conjunctivitis due to burns, toxic and chemical require careful wash-out with ], especially beneath the lids, and may require topical steroids. The more acute chemical injuries are medical emergencies, particularly alkali burns, which can lead to severe scarring, and intraocular damage. Fortunately, such injuries are uncommon. | |||
| Blepharoconjunctivitis is the dual combination of conjunctivitis with ] (inflammation of the eyelids).{{citation needed|date=February 2023}} | |||
| ] is the combination of conjunctivitis and ] (]l inflammation).{{citation needed|date=February 2023}}<!-- Two good bullet points, but try to find a source for them. --> | |||
| ==References== | |||
| <references /> | |||
| Blepharokeratoconjunctivitis is the combination of conjunctivitis with blepharitis and keratitis. It is clinically defined by changes of the lid margin, meibomian gland dysfunction, redness of the eye, conjunctival chemosis and inflammation of the cornea.<ref name="OGallagher">{{cite journal | vauthors = O'Gallagher M, Banteka M, Bunce C, Larkin F, Tuft S, Dahlmann-Noor A | title = Systemic treatment for blepharokeratoconjunctivitis in children | journal = The Cochrane Database of Systematic Reviews | volume = 2016 | issue = 5 | pages = CD011750 | date = May 2016 | pmid = 27236587 | pmc = 9257284 | doi = 10.1002/14651858.CD011750.pub2 }}</ref> | |||
| ==External links== | |||
| * The National Eye Institute (NEI). | |||
| === Differential diagnosis === | |||
| Some more serious conditions can present with a red eye, such as infectious keratitis, angle-closure glaucoma, or iritis. These conditions require the urgent attention of an ophthalmologist. Signs of such conditions include decreased vision, significantly increased sensitivity to light, inability to keep the eye open, a pupil that does not respond to light, or a severe headache with nausea.<ref name="McGra-Hill">{{Cite book |title=Harrison's Principles of Internal Medicine |vauthors=Longo DL |date=2012 |publisher=McGra-Hill |chapter=Disorders of the Eye(Horton JC)}}</ref> Fluctuating blurring is common, due to tearing and mucoid discharge. Mild photophobia is common. However, if any of these symptoms is prominent, considering other diseases such as ], ], ], and even ] or ] is important.{{citation needed|date=September 2022}} | |||
| A more comprehensive differential diagnosis for the red or painful eye includes:<ref name="McGra-Hill" /> | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] (dry eye) | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] – an ] condition that produces a similar appearance to conjunctivitis, but without discharge or tearing | |||
| * ] | |||
| * ] | |||
| * ] | |||
| * ] | |||
| == Prevention == | |||
| The most effective prevention is good hygiene, especially avoiding rubbing the eyes with infected hands. Vaccination against some of the causative pathogens such as ''Haemophilus influenzae'', pneumococcus, and ''Neisseria meningitidis'' is also effective.<ref>{{Cite news |date=2 October 2017 |title=Protect Yourself From Pink Eye |url=https://www.cdc.gov/conjunctivitis/about/prevention.html |access-date=18 October 2017 |work=Centers for Disease Control and Prevention |language=en-us}}</ref> | |||
| ] eye solution has been found to prevent neonatal conjunctivitis.<ref name=Is2003/> It is becoming more commonly used globally because of its low cost.<ref name="Is2003">{{cite journal | vauthors = Isenberg SJ | title = The ocular application of povidone-iodine | journal = Community Eye Health | volume = 16 | issue = 46 | pages = 30–31 | date = 2003 | pmid = 17491857 | pmc = 1705857 }}</ref> | |||
| == Management == | |||
| Conjunctivitis resolves in 65% of cases without treatment, within 2–5 days. The prescription of antibiotics is not necessary in most cases.<ref>{{cite journal | vauthors = Rose P | title = Management strategies for acute infective conjunctivitis in primary care: a systematic review | journal = Expert Opinion on Pharmacotherapy | volume = 8 | issue = 12 | pages = 1903–1921 | date = August 2007 | pmid = 17696792 | doi = 10.1517/14656566.8.12.1903 | s2cid = 45899988 }}</ref> | |||
| === Viral === | |||
| Viral conjunctivitis usually resolves on its own and does not require any specific treatment.<ref name=Az2013/> Antihistamines (e.g., ]) or mast cell stabilizers (e.g., ]) may be used to help with the symptoms.<ref name=Az2013/> Povidone-iodine has been suggested as a treatment, but as of 2008, evidence to support it was poor.<ref name="BartlettJaanus2008">{{Cite book | vauthors = Bartlett JD, Jaanus SD |url=https://books.google.com/books?id=Eybg7fbs65MC&pg=PA454 |title=Clinical Ocular Pharmacology |publisher=Elsevier Health Sciences |year=2008 |isbn=978-0-7506-7576-5 |pages=454– |archive-url=https://web.archive.org/web/20161203204429/https://books.google.com/books?id=Eybg7fbs65MC&pg=PA454 |archive-date=3 December 2016 |url-status=live |df=dmy-all}}</ref> | |||
| === Allergic === | |||
| For allergic conjunctivitis, cool water poured over the face with the head inclined downward constricts capillaries, and ] sometimes relieve discomfort in mild cases. In more severe cases, ] and ]s may be prescribed. Persistent allergic conjunctivitis may also require topical steroid drops.<ref>{{cite journal | vauthors = Patel DS, Arunakirinathan M, Stuart A, Angunawela R | title = Allergic eye disease | journal = BMJ | volume = 359 | pages = j4706 | date = November 2017 | pmid = 29097360 | doi = 10.1136/bmj.j4706 | s2cid = 5316455 }}</ref> | |||
| === Bacterial === | |||
| Bacterial conjunctivitis usually resolves without treatment.<ref name=Az2013/> Topical antibiotics may be needed only if no improvement is observed after 3 days.<ref>{{cite journal | vauthors = Visscher KL, Hutnik CM, Thomas M | title = Evidence-based treatment of acute infective conjunctivitis: Breaking the cycle of antibiotic prescribing | journal = Canadian Family Physician | volume = 55 | issue = 11 | pages = 1071–1075 | date = November 2009 | pmid = 19910590 | pmc = 2776793 }}</ref> No serious effects were noted either with or without treatment.<ref name=":2">{{cite journal | vauthors = Chen YY, Liu SH, Nurmatov U, van Schayck OC, Kuo IC | title = Antibiotics versus placebo for acute bacterial conjunctivitis | journal = The Cochrane Database of Systematic Reviews | volume = 3 | issue = 3 | pages = CD001211 | date = March 2023 | pmid = 36912752 | pmc = 10014114 | doi = 10.1002/14651858.CD001211.pub4 }}</ref> Because antibiotics do speed healing in bacterial conjunctivitis, their use may be considered.<ref name=":2" /> Antibiotics are also recommended for those who wear contact lenses, are ], have disease which is thought to be due to chlamydia or gonorrhea, have a fair bit of pain, or have copious discharge.<ref name=Az2013/> Gonorrheal or chlamydial infections require both oral and topical antibiotics.<ref name=Az2013/> | |||
| The choice of antibiotic varies based on the strain or suspected strain of bacteria causing the infection. ], ], or ] may be used, typically for 7–10 days.<ref name="Yanoff" /> Cases of meningococcal conjunctivitis can also be treated with systemic penicillin, as long as the strain is sensitive to penicillin.{{citation needed|date=September 2022}} | |||
| When investigated as a treatment, povidone-iodine ophthalmic solution has also been observed to have some effectiveness against bacterial and chlamydial conjunctivitis, with a possible role suggested in locations where topical antibiotics are unavailable or costly.<ref name="Am J Ophthalmol 2002">{{cite journal | vauthors = Isenberg SJ, Apt L, Valenton M, Del Signore M, Cubillan L, Labrador MA, Chan P, Berman NG | title = A controlled trial of povidone-iodine to treat infectious conjunctivitis in children | journal = American Journal of Ophthalmology | volume = 134 | issue = 5 | pages = 681–688 | date = November 2002 | pmid = 12429243 | doi = 10.1016/S0002-9394(02)01701-4 }}</ref> | |||
| === Chemical === | |||
| Conjunctivitis due to chemicals is treated via ] with ] or ]. Chemical injuries, particularly alkali burns, are medical emergencies, as they can lead to severe scarring and intraocular damage. People with chemically induced conjunctivitis should not touch their eyes to avoid spreading the chemical.<ref>{{Cite web |title=Conjunctivitis |url=https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/conjunctivitis?sso=y |access-date=March 15, 2024 |website=American Optometric Association}}</ref> | |||
| == Epidemiology == | |||
| Conjunctivitis is the most common eye disease.<ref>{{Cite book | vauthors = Smeltzer SC |url=https://books.google.com/books?id=SmtjSD1x688C&pg=RA1-PA1787 |title=Brunner & Suddarth's textbook of medical-surgical nursing. |date=2010 |publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins |isbn=978-0-7817-8589-1 |edition=12th |location=Philadelphia |page=1787 |archive-url=https://web.archive.org/web/20160815203433/https://books.google.ca/books?id=SmtjSD1x688C&pg=RA1-PA1787 |archive-date=15 August 2016 |url-status=live |df=dmy-all}}</ref> Rates of disease is related to the underlying cause which varies by the age as well as the time of year. Acute conjunctivitis is most frequently found in infants, school-age children and the elderly.<ref name=":1">{{cite journal | vauthors = Høvding G | title = Acute bacterial conjunctivitis | journal = Acta Ophthalmologica | volume = 86 | issue = 1 | pages = 5–17 | date = February 2008 | pmid = 17970823 | doi = 10.1111/j.1600-0420.2007.01006.x | s2cid = 20629824 | doi-access = free }}</ref> The most common cause of infectious conjunctivitis is viral conjunctivitis.<ref name=":0">{{Cite journal | vauthors = Mourad MS, Rihan RA |date=April 2018 |title=Prevalence of Different Eye Diseases excluding Refractive Errors Presented at the Outpatient Clinic in Beheira Eye Hospital |journal=The Egyptian Journal of Hospital Medicine |language=en |volume=71 |issue=2 |pages=2484–2489 |doi=10.12816/0045645 |s2cid=80882721}}</ref> | |||
| It is estimated that acute conjunctivitis affects 6 million people annually in the United States.<ref name=Az2013/> | |||
| Some seasonal trends have been observed for the occurrence of different forms of conjunctivitis. In the northern hemisphere, the occurrence of bacterial conjunctivitis peaks from December to April, viral conjunctivitis peaks in the summer months and allergic conjunctivitis is more prevalent throughout the spring and summer.<ref name=":1" /><!-- Include more on epidemiology if more info can be found. --> | |||
| == History == | |||
| An adenovirus was first isolated by Rowe et al. in 1953. Two years later, Jawetz et al. published on epidemic keratoconjunctivitis.<ref>{{cite journal | vauthors = Jhanji V, Chan TC, Li EY, Agarwal K, Vajpayee RB | title = Adenoviral keratoconjunctivitis | journal = Survey of Ophthalmology | volume = 60 | issue = 5 | pages = 435–443 | date = September–October 2015 | pmid = 26077630 | doi = 10.1016/j.survophthal.2015.04.001 }}</ref>{{rp|437}} "Madras eye" is a colloquial term that has been used in ] for the disease.<!-- Try to elaborate on the history a bit more. --> | |||
| ===Outbreak in Pakistan=== | |||
| {{Main|Pink eye outbreak in Pakistan}} | |||
| In September 2023, a significant outbreak of conjunctivitis occurred in ]. The outbreak began in ] and quickly spread to ], ], and ]. By the end of the month, over 86,133 cases had been reported in ] alone. The rapid spread of the disease led to the temporary closure of schools in the region. This event marked one of the largest outbreaks of Pink Eye in the country's recent history.<ref>{{Cite web |date=28 September 2023 |title=From pink eye to blindness |url=https://tribune.com.pk/story/2438104/from-pink-eye-to-blindness}}</ref><ref>{{Cite web |date=28 September 2023 |title=86,133 pink eye cases in Punjab in September and counting |url=https://www.dawn.com/news/1778214}}</ref><ref>{{Cite news |last=Ahmed |first=Salman |date=27 September 2023 |title=Punjab Announces Holiday for Schools Amid Pink Eye Outbreak |url=https://propakistani.pk/2023/09/27/punjab-announces-holiday-for-schools-amid-pink-eye-outbreak/ |work=Propakistani}}</ref><ref>{{Cite web |title=85 new cases of Pink Eye infection reported in Pakistan's Lahore |url=https://health.economictimes.indiatimes.com/news/industry/85-new-cases-of-pink-eye-infection-reported-in-pakistans-lahore/103921170 |website=ETHealthworld.com |agency=]}}</ref> | |||
| ==Society and culture== | |||
| Conjunctivitis imposes economic and social burdens. The cost of treating bacterial conjunctivitis in the United States was estimated to be $377 million to $857 million per year.<ref name=Az2013/> Approximately 1% of all primary care office visits in the United States are related to conjunctivitis. Approximately 70% of all people with acute conjunctivitis present to primary care and urgent care.<ref name=Az2013/> | |||
| == See also == | |||
| * ] | |||
| * ] | |||
| == References == | |||
| {{Reflist}} | |||
| == External links == | |||
| {{commons category|Conjunctivitis}} | |||
| * | |||
| * {{Cite web |title=Pink Eye |url=https://medlineplus.gov/pinkeye.html |website=MedlinePlus |publisher=U.S. National Library of Medicine}} | |||
| * {{Cite web |date=28 February 2021 |title=Metabolomics for Ocular Surface Disease |url=https://www.youtube.com/watch?v=PuG1hvcdZBQ |publisher=MSBB Group, Leiden University}} | |||
| {{Medical condition classification and resources | |||
| |ICD10 = {{ICD10|H|10||h|10}} | |||
| |ICD9 = {{ICD9|372.0}} | |||
| |OMIM = | |||
| |MedlinePlus = 001010 | |||
| |eMedicineSubj = emerg | |||
| |eMedicineTopic = 110 | |||
| |DiseasesDB = 3067 | |||
| |MeshID = D003231 | | |||
| }} | |||
| {{Eye pathology}} | {{Eye pathology}} | ||
| {{Authority control}} | |||
| {{Inflammation}} | |||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 19:37, 19 December 2024
Inflammation of the eye "Pinkeye" redirects here. For other uses, see Pinkeye (disambiguation).
| This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. Find sources: "Conjunctivitis" – news · newspapers · books · scholar · JSTOR (May 2024) (Learn how and when to remove this message) |
| Conjunctivitis | |
|---|---|
| Other names | Pink eye |
 | |
| An eye with viral conjunctivitis | |
| Specialty | Ophthalmology, optometry |
| Symptoms | Reddish eye, scratchiness |
| Duration | Viral conjunctivitis: up to two weeks |
| Causes | Viral, bacterial, allergies |
| Diagnostic method | Based on symptoms, microbial culture |
| Prevention | Handwashing |
| Treatment | Based on underlying cause |
| Frequency | 3–6 million per year (US) |
Conjunctivitis, also known as pink eye or Madras eye, is inflammation of the conjunctiva and the inner surface of the eyelid. It makes the eye appear pink or reddish. Pain, burning, scratchiness, or itchiness may occur. The affected eye may have increased tears or be "stuck shut" in the morning. Swelling of the sclera may also occur. Itching is more common in cases due to allergies. Conjunctivitis can affect one or both eyes.
The most common infectious causes in adults are viral, whereas in children bacterial causes predominate. The viral infection may occur along with other symptoms of a common cold. Both viral and bacterial cases are easily spread between people. Allergies to pollen or animal hair are also a common cause. Diagnosis is often based on signs and symptoms. Occasionally, a sample of the discharge is sent for culture.
Prevention is partly by handwashing. Treatment depends on the underlying cause. In the majority of viral cases, there is no specific treatment. Most cases due to a bacterial infection also resolve without treatment; however, antibiotics can shorten the illness. People who wear contact lenses and those whose infection is caused by gonorrhea or chlamydia should be treated. Allergic cases can be treated with antihistamines or mast cell inhibitor drops.
About 3 to 6 million people get acute conjunctivitis each year in the United States. Typically, people get better in one or two weeks. If visual loss, significant pain, sensitivity to light or signs of herpes occur, or if symptoms do not improve after a week, further diagnosis and treatment may be required. Conjunctivitis in a newborn, known as neonatal conjunctivitis, may also require specific treatment.
Signs and symptoms

Red eye, swelling of the conjunctiva, and watering of the eyes are symptoms common to all forms of conjunctivitis. However, the pupils should be normally reactive, and the visual acuity normal.
Conjunctivitis is identified by inflammation of the conjunctiva, manifested by irritation and redness. Examination using a slit lamp (biomicroscope) may improve diagnostic accuracy. Examination of the palpebral conjunctiva, that overlying the inner aspects of the eyelids, is usually more diagnostic than examination of the bulbal conjunctiva, that overlying the sclera.
Viral
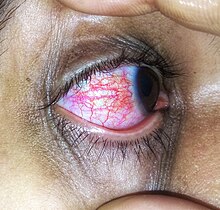
Approximately 80% of cases of conjunctivitis in adults and less than 20% in children are due to viruses, with 65% to 90% of these cases being attributed to adenoviruses. Viral conjunctivitis is often associated with an infection of the upper respiratory tract, a common cold, or a sore throat. Other associated signs may include pre-auricular lymph node swelling and contact with another person with a red eye. Eye pain may be present if the cornea is also involved. Its symptoms include excessive watering and itching. The discharge in viral conjunctivitis is usually (but not always) watery in nature. The infection usually begins in one eye but may spread easily to the other eye.
Viral conjunctivitis manifests as a fine, diffuse pinkness of the conjunctiva which may be mistaken for iritis, but corroborative signs on microscopy, particularly numerous lymphoid follicles on the tarsal conjunctiva, and sometimes a punctate keratitis are seen.
Allergic

Allergic conjunctivitis is inflammation of the conjunctiva due to allergy. The specific allergens may differ among patients. Symptoms result from the release of histamine and other active substances by mast cells, and consist of redness (mainly due to vasodilation of the peripheral small blood vessels), swelling of the conjunctiva, itching, and increased production of tears.
Bacterial

Bacteria are responsible for approximately 70% of conjunctivitis in children and less than 20% of cases in adults. Common bacteria responsible for bacterial conjunctivitis are Staphylococcus including Staph aureus, Streptococcus such as strep pneumoniae, Haemophilus species and Moraxella catarrhalis. Less commonly, Chlamydia spp. and Niesseria species (Neisseria gonorrhoeae and Neisseria meningitidis) may be the cause. Infection with Escherichia coli may also cause conjunctivitis, particularly in the neonatal subtype ophthalmia neonatorum. Bacterial conjunctivitis usually causes a rapid onset of conjunctival redness, swelling of the eyelid, and a sticky discharge. Typically, symptoms develop first in one eye, but may spread to the other eye within 2–5 days. Conjunctivitis due to common pus-producing bacteria causes marked grittiness or irritation and a stringy, opaque, greyish or yellowish discharge that may cause the lids to stick together, especially after sleep. Severe crusting of the infected eye and the surrounding skin may also occur. The gritty or scratchy feeling is sometimes localized enough that patients may insist that they have a foreign body in the eye.

Bacteria such as Chlamydia trachomatis or Moraxella spp. can cause a nonexudative but persistent conjunctivitis without much redness. Bacterial conjunctivitis may cause the production of membranes or pseudomembranes that cover the conjunctiva. Pseudomembranes consist of a combination of inflammatory cells and exudates and adhere loosely to the conjunctiva, while true membranes are more tightly adherent and cannot be easily peeled away. Cases of bacterial conjunctivitis that involve the production of membranes or pseudomembranes are associated with Neisseria gonorrhoeae, β-hemolytic streptococci, and Corynebacterium diphtheriae. C. diphtheriae causes membrane formation in conjunctiva of unimmunized children.
Chemical
Chemical eye injury may result when an acidic or alkaline substance gets in the eye. Alkali burns are typically worse than acidic burns. Mild burns produce conjunctivitis, while more severe burns may cause the cornea to turn white. Litmus paper may be used to test for chemical causes. When a chemical cause has been confirmed, the eye or eyes should be flushed until the pH is in the range 6–8. Anaesthetic eye drops can be used to decrease the pain.
Irritant or toxic conjunctivitis is primarily marked by redness. If due to a chemical splash, it is often present in only the lower conjunctival sac. With some chemicals, above all with caustic alkalis such as sodium hydroxide, necrosis of the conjunctiva marked by a deceptively white eye due to vascular closure may occur, followed by sloughing off of the dead epithelium. A slit lamp examination is likely to show evidence of anterior uveitis.
Biomarkers
Omics technologies have been used to identify biomarkers that inform on the emergence and progression of conjunctivitis. For example, in chronic inflammatory cicatrizing conjunctivitis, active oxylipins, lysophospholipids, fatty acids, and endocannabinoids alterations, from which potential biomarkers linked to inflammatory processes were identified.
Other

Inclusion conjunctivitis of the newborn is a conjunctivitis that may be caused by the bacterium Chlamydia trachomatis, and may lead to acute, purulent conjunctivitis. However, it is usually self-healing.
Causes
Infective conjunctivitis is most commonly caused by a virus. Bacterial infections, allergies, other irritants, and dryness are also common causes. Both bacterial and viral infections are contagious, passing from person to person or spread through contaminated objects or water. Contact with contaminated fingers is a common cause of conjunctivitis. Bacteria may also reach the conjunctiva from the edges of the eyelids and the surrounding skin, from the nasopharynx, from infected eye drops or contact lenses, from the genitals or the bloodstream. Infection by human adenovirus accounts for 65% to 90% of cases of viral conjunctivitis.
Viral
Adenoviruses are the most common cause of viral conjunctivitis (adenoviral keratoconjunctivitis). Herpetic keratoconjunctivitis, caused by herpes simplex viruses, can be serious and requires treatment with aciclovir. Acute hemorrhagic conjunctivitis is a highly contagious disease caused by one of two enteroviruses, enterovirus 70 and coxsackievirus A24. These were first identified in an outbreak in Ghana in 1969, and have spread worldwide since then, causing several epidemics.
Bacterial
The most common causes of acute bacterial conjunctivitis are Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae. Though very rare, hyperacute cases are usually caused by Neisseria gonorrhoeae or Neisseria meningitidis. Chronic cases of bacterial conjunctivitis are those lasting longer than 3 weeks, and are typically caused by S. aureus, Moraxella lacunata, or Gram-negative enteric flora.
Allergic
Conjunctivitis may also be caused by allergens such as pollen, perfumes, cosmetics, smoke, dust mites, Balsam of Peru, or eye drops. The most frequent cause of conjunctivitis is allergic conjunctivitis and it affects 15% to 40% of the population. Allergic conjunctivitis accounts for 15% of eye related primary care consultations; most including seasonal exposures in the spring and summer or perpetual conditions.
Other
- Computer vision syndrome
- Dry eye syndrome
- Reactive arthritis: Conjunctivitis is part of the triad of reactive arthritis, which is thought to be caused by autoimmune cross-reactivity following certain bacterial infections. Reactive arthritis is highly associated with HLA-B27. Conjunctivitis is associated with the autoimmune disease relapsing polychondritis.
Diagnosis

Cultures are not often taken or needed as most cases resolve either with time or typical antibiotics. If bacterial conjunctivitis is suspected, but no response to topical antibiotics is seen, swabs for bacterial culture should be taken and tested. Viral culture may be appropriate in epidemic case clusters.
A patch test is used to identify the causative allergen in allergic conjunctivitis.
Although conjunctival scrapes for cytology can be useful in detecting chlamydial and fungal infections, allergies, and dysplasia, they are rarely done because of the cost and the general dearth of laboratory staff experienced in handling ocular specimens. Conjunctival incisional biopsy is occasionally done when granulomatous diseases (e.g., sarcoidosis) or dysplasia are suspected.
Classification
Conjunctivitis may be classified either by cause or by extent of the inflamed area.
Causes
- Allergy
- Bacteria
- Viruses
- Chemicals
- Autoimmune
Neonatal conjunctivitis is often grouped separately from bacterial conjunctivitis because it is caused by different bacteria than the more common cases of bacterial conjunctivitis.
By extent of involvement
Blepharoconjunctivitis is the dual combination of conjunctivitis with blepharitis (inflammation of the eyelids).
Keratoconjunctivitis is the combination of conjunctivitis and keratitis (corneal inflammation).
Blepharokeratoconjunctivitis is the combination of conjunctivitis with blepharitis and keratitis. It is clinically defined by changes of the lid margin, meibomian gland dysfunction, redness of the eye, conjunctival chemosis and inflammation of the cornea.
Differential diagnosis
Some more serious conditions can present with a red eye, such as infectious keratitis, angle-closure glaucoma, or iritis. These conditions require the urgent attention of an ophthalmologist. Signs of such conditions include decreased vision, significantly increased sensitivity to light, inability to keep the eye open, a pupil that does not respond to light, or a severe headache with nausea. Fluctuating blurring is common, due to tearing and mucoid discharge. Mild photophobia is common. However, if any of these symptoms is prominent, considering other diseases such as glaucoma, uveitis, keratitis, and even meningitis or carotico-cavernous fistula is important.
A more comprehensive differential diagnosis for the red or painful eye includes:
- Corneal abrasion
- Subconjunctival hemorrhage
- Pinguecula
- Blepharitis
- Dacryocystitis
- Keratoconjunctivitis sicca (dry eye)
- Keratitis
- Herpes simplex
- Herpes zoster
- Episcleritis – an inflammatory condition that produces a similar appearance to conjunctivitis, but without discharge or tearing
- Uveitis
- Acute angle-closure glaucoma
- Endophthalmitis
- Orbital cellulitis
Prevention
The most effective prevention is good hygiene, especially avoiding rubbing the eyes with infected hands. Vaccination against some of the causative pathogens such as Haemophilus influenzae, pneumococcus, and Neisseria meningitidis is also effective.
Povidone-iodine eye solution has been found to prevent neonatal conjunctivitis. It is becoming more commonly used globally because of its low cost.
Management
Conjunctivitis resolves in 65% of cases without treatment, within 2–5 days. The prescription of antibiotics is not necessary in most cases.
Viral
Viral conjunctivitis usually resolves on its own and does not require any specific treatment. Antihistamines (e.g., diphenhydramine) or mast cell stabilizers (e.g., cromolyn) may be used to help with the symptoms. Povidone-iodine has been suggested as a treatment, but as of 2008, evidence to support it was poor.
Allergic
For allergic conjunctivitis, cool water poured over the face with the head inclined downward constricts capillaries, and artificial tears sometimes relieve discomfort in mild cases. In more severe cases, nonsteroidal anti-inflammatory medications and antihistamines may be prescribed. Persistent allergic conjunctivitis may also require topical steroid drops.
Bacterial
Bacterial conjunctivitis usually resolves without treatment. Topical antibiotics may be needed only if no improvement is observed after 3 days. No serious effects were noted either with or without treatment. Because antibiotics do speed healing in bacterial conjunctivitis, their use may be considered. Antibiotics are also recommended for those who wear contact lenses, are immunocompromised, have disease which is thought to be due to chlamydia or gonorrhea, have a fair bit of pain, or have copious discharge. Gonorrheal or chlamydial infections require both oral and topical antibiotics.
The choice of antibiotic varies based on the strain or suspected strain of bacteria causing the infection. Fluoroquinolones, sodium sulfacetamide, or trimethoprim/polymyxin may be used, typically for 7–10 days. Cases of meningococcal conjunctivitis can also be treated with systemic penicillin, as long as the strain is sensitive to penicillin.
When investigated as a treatment, povidone-iodine ophthalmic solution has also been observed to have some effectiveness against bacterial and chlamydial conjunctivitis, with a possible role suggested in locations where topical antibiotics are unavailable or costly.
Chemical
Conjunctivitis due to chemicals is treated via irrigation with Ringer's lactate or saline solution. Chemical injuries, particularly alkali burns, are medical emergencies, as they can lead to severe scarring and intraocular damage. People with chemically induced conjunctivitis should not touch their eyes to avoid spreading the chemical.
Epidemiology
Conjunctivitis is the most common eye disease. Rates of disease is related to the underlying cause which varies by the age as well as the time of year. Acute conjunctivitis is most frequently found in infants, school-age children and the elderly. The most common cause of infectious conjunctivitis is viral conjunctivitis.
It is estimated that acute conjunctivitis affects 6 million people annually in the United States.
Some seasonal trends have been observed for the occurrence of different forms of conjunctivitis. In the northern hemisphere, the occurrence of bacterial conjunctivitis peaks from December to April, viral conjunctivitis peaks in the summer months and allergic conjunctivitis is more prevalent throughout the spring and summer.
History
An adenovirus was first isolated by Rowe et al. in 1953. Two years later, Jawetz et al. published on epidemic keratoconjunctivitis. "Madras eye" is a colloquial term that has been used in India for the disease.
Outbreak in Pakistan
Main article: Pink eye outbreak in PakistanIn September 2023, a significant outbreak of conjunctivitis occurred in Pakistan. The outbreak began in Karachi and quickly spread to Lahore, Rawalpindi, and Islamabad. By the end of the month, over 86,133 cases had been reported in Punjab alone. The rapid spread of the disease led to the temporary closure of schools in the region. This event marked one of the largest outbreaks of Pink Eye in the country's recent history.
Society and culture
Conjunctivitis imposes economic and social burdens. The cost of treating bacterial conjunctivitis in the United States was estimated to be $377 million to $857 million per year. Approximately 1% of all primary care office visits in the United States are related to conjunctivitis. Approximately 70% of all people with acute conjunctivitis present to primary care and urgent care.
See also
References
- ^ "Facts About Pink Eye". National Eye Institute. November 2015. Archived from the original on 9 March 2016. Retrieved 8 March 2016.
- Long SS, Prober CG, Fischer M (2017). Principles and Practice of Pediatric Infectious Diseases E-Book. Elsevier Health Sciences. p. 502. ISBN 978-0-323-46132-0.
- ^ Azari AA, Barney NP (October 2013). "Conjunctivitis: a systematic review of diagnosis and treatment". JAMA. 310 (16): 1721–1729. doi:10.1001/jama.2013.280318. PMC 4049531. PMID 24150468.
- "What is Viral Conjunctivitis a.k.a. Sore Eyes? | National Institutes of Health".
- Mohanasundaram AS, Gurnani B, Kaur K, Manikkam R (May 2023). "Madras eye outbreak in India: Why should we foster a better understanding of acute conjunctivitis?". Indian Journal of Ophthalmology. 71 (5): 2298–2299. doi:10.4103/IJO.IJO_3317_22. PMC 10391441. PMID 37202982.
- Richards A, Guzman-Cottrill JA (May 2010). "Conjunctivitis". Pediatrics in Review. 31 (5): 196–208. doi:10.1542/pir.31-5-196. PMID 20435711. S2CID 245084568.
- ^ Durand ML, Barshak MB, Sobrin L (December 2023). "Eye Infections". The New England Journal of Medicine. 389 (25): 2363–2375. doi:10.1056/NEJMra2216081. PMID 38118024. S2CID 266433325.
- Hashmi MF, Gurnani B, Benson S (2023). "Conjunctivitis". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 31082078. Retrieved 23 May 2023.
- Bielory L, Friedlaender MH (February 2008). "Allergic conjunctivitis". Immunology and Allergy Clinics of North America. 28 (1): 43–58, vi. doi:10.1016/j.iac.2007.12.005. PMID 18282545. S2CID 34371872.
- "Pink Eye (Conjunctivitis)". MedicineNet. Archived from the original on 22 June 2013.
- "Acute Bacterial Conjunctivitis – Eye Disorders". Merck Manuals Professional Edition. Archived from the original on 28 December 2016. Retrieved 31 December 2016.
- Saadeh-Jackson S, Rodriguez L, Leffler CT, Freymiller C, Wolf E, Wijesooriya N, et al. (August 2022). "Ophthalmia neonatorum due to Escherichia coli: A rare cause or an emerging bacterial etiology of neonatal conjunctivitis?". Clinical Case Reports. 10 (8): e6201. doi:10.1002/ccr3.6201. PMC 9354094. PMID 35949413.
- Hamborsky J, Kroger A, Wolfe C, eds. (2015). Epidemiology and Prevention of Vaccine-Preventable Diseases. U.S. Dept. of Health & Human Services, Centers for Disease Control and Prevention. p. 112. ISBN 978-0-9904491-1-9.
- ^ Zentani A, Burslem J (December 2009). "Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 4: use of litmus paper in chemical eye injury". Emergency Medicine Journal. 26 (12): 887. doi:10.1136/emj.2009.086124. PMID 19934140. S2CID 38124735.
- ^ Hodge C, Lawless M (July 2008). "Ocular emergencies". Australian Family Physician. 37 (7): 506–509. PMID 18592066.
- Di Zazzo A, Yang W, Coassin M, Micera A, Antonini M, Piccinni F, et al. (May 2020). "Signaling lipids as diagnostic biomarkers for ocular surface cicatrizing conjunctivitis". Journal of Molecular Medicine. 98 (5): 751–760. doi:10.1007/s00109-020-01907-w. PMC 7220886. PMID 32313985.
- ^ Fisher B, Harvey RP, Champe PC (2007). Lippincott's Illustrated Reviews: Microbiology (Lippincott's Illustrated Reviews Series). Hagerstown MD: Lippincott Williams & Wilkins. ISBN 978-0-7817-8215-9.
- ^ Høvding G (February 2008). "Acute bacterial conjunctivitis". Acta Ophthalmologica. 86 (1): 5–17. doi:10.1111/j.1600-0420.2007.01006.x. PMID 17970823. S2CID 20629824.
- Singh MP, Ram J, Kumar A, Rungta T, Gupta A, Khurana J, et al. (2018). "Molecular epidemiology of circulating human adenovirus types in acute conjunctivitis cases in Chandigarh, North India". Indian Journal of Medical Microbiology. 36 (1): 113–115. doi:10.4103/ijmm.ijmm_17_258. PMID 29735838.
- ^ Yanoff M, Duker JS (2008). Ophthalmology (3rd ed.). Edinburgh: Mosby. pp. 227–236. ISBN 978-0-323-05751-6.
- Lévêque N, Huguet P, Norder H, Chomel JJ (April 2010). "". Médecine et Maladies Infectieuses (in French). 40 (4): 212–218. doi:10.1016/j.medmal.2009.09.006. PMID 19836177.
- "Protect Yourself From Pink Eye". Centers for Disease Control and Prevention (CDC). 2 October 2017. Retrieved 7 December 2018.
- "Allergic Conjunctivitis". familydoctor.org. Archived from the original on 6 September 2015. Retrieved 18 September 2015.
- Brooks P (25 October 2012). The Daily Telegraph: Complete Guide to Allergies. Little, Brown Book. ISBN 978-1-4721-0394-9. Retrieved 15 April 2014.
- "What Is Allergic Conjunctivitis? What Causes Allergic Conjunctivitis?". medicalnewstoday.com. Archived from the original on 16 March 2010. Retrieved 6 April 2010.
- ^ Mourad MS, Rihan RA (April 2018). "Prevalence of Different Eye Diseases excluding Refractive Errors Presented at the Outpatient Clinic in Beheira Eye Hospital". The Egyptian Journal of Hospital Medicine. 71 (2): 2484–2489. doi:10.12816/0045645. S2CID 80882721.
- Perkin MR, Bader T, Rudnicka AR, Strachan DP, Owen CG (24 November 2015). "Inter-Relationship between Rhinitis and Conjunctivitis in Allergic Rhinoconjunctivitis and Associated Risk Factors in Rural UK Children". PLOS ONE. 10 (11): e0143651. Bibcode:2015PLoSO..1043651P. doi:10.1371/journal.pone.0143651. PMC 4658044. PMID 26600465.
- Puéchal X, Terrier B, Mouthon L, Costedoat-Chalumeau N, Guillevin L, Le Jeunne C (March 2014). "Relapsing polychondritis". Joint Bone Spine. 81 (2): 118–124. doi:10.1016/j.jbspin.2014.01.001. PMID 24556284. S2CID 205754989.
- Cantarini L, Vitale A, Brizi MG, Caso F, Frediani B, Punzi L, et al. (2014). "Diagnosis and classification of relapsing polychondritis". Journal of Autoimmunity. 48–49: 53–59. doi:10.1016/j.jaut.2014.01.026. PMID 24461536.
- Sheikh A, Hurwitz B (2008). "BACTERIAL CONJUNCTIVITIS 372.05 (Infective Conjunctivitis, Mucopurulent Conjunctivitis, Purulent Conjunctivitis)". Roy and Fraunfelder's Current Ocular Therapy. Elsevier. pp. 332–334. doi:10.1016/b978-1-4160-2447-7.50182-1. ISBN 978-1-4160-2447-7.
- Mannis MJ, Macsai MS, Huntley AC (1996). Eye and skin disease. Lippincott-Raven. ISBN 978-0-7817-0269-0. Archived from the original on 5 July 2014. Retrieved 23 April 2014.
- Korkmaz Ekren P, Mogulkoc N, Toreyin ZN, Egrilmez S, Veral A, Akalın T, et al. (October 2016). "Conjunctival Biopsy as a First Choice to Confirm a Diagnosis of Sarcoidosis". Sarcoidosis, Vasculitis, and Diffuse Lung Diseases. 33 (3): 196–200. PMID 27758983.
- Roberts F, Thum CK (2021). "The Conjunctival Biopsy". In Roberts F (ed.). Lee's Ophthalmic Histopathology. Cham: Springer International Publishing. pp. 343–388. doi:10.1007/978-3-030-76525-5_11. ISBN 978-3-030-76525-5.
- O'Gallagher M, Banteka M, Bunce C, Larkin F, Tuft S, Dahlmann-Noor A (May 2016). "Systemic treatment for blepharokeratoconjunctivitis in children". The Cochrane Database of Systematic Reviews. 2016 (5): CD011750. doi:10.1002/14651858.CD011750.pub2. PMC 9257284. PMID 27236587.
- ^ Longo DL (2012). "Disorders of the Eye(Horton JC)". Harrison's Principles of Internal Medicine. McGra-Hill.
- "Protect Yourself From Pink Eye". Centers for Disease Control and Prevention. 2 October 2017. Retrieved 18 October 2017.
- ^ Isenberg SJ (2003). "The ocular application of povidone-iodine". Community Eye Health. 16 (46): 30–31. PMC 1705857. PMID 17491857.
- Rose P (August 2007). "Management strategies for acute infective conjunctivitis in primary care: a systematic review". Expert Opinion on Pharmacotherapy. 8 (12): 1903–1921. doi:10.1517/14656566.8.12.1903. PMID 17696792. S2CID 45899988.
- Bartlett JD, Jaanus SD (2008). Clinical Ocular Pharmacology. Elsevier Health Sciences. pp. 454–. ISBN 978-0-7506-7576-5. Archived from the original on 3 December 2016.
- Patel DS, Arunakirinathan M, Stuart A, Angunawela R (November 2017). "Allergic eye disease". BMJ. 359: j4706. doi:10.1136/bmj.j4706. PMID 29097360. S2CID 5316455.
- Visscher KL, Hutnik CM, Thomas M (November 2009). "Evidence-based treatment of acute infective conjunctivitis: Breaking the cycle of antibiotic prescribing". Canadian Family Physician. 55 (11): 1071–1075. PMC 2776793. PMID 19910590.
- ^ Chen YY, Liu SH, Nurmatov U, van Schayck OC, Kuo IC (March 2023). "Antibiotics versus placebo for acute bacterial conjunctivitis". The Cochrane Database of Systematic Reviews. 3 (3): CD001211. doi:10.1002/14651858.CD001211.pub4. PMC 10014114. PMID 36912752.
- Isenberg SJ, Apt L, Valenton M, Del Signore M, Cubillan L, Labrador MA, et al. (November 2002). "A controlled trial of povidone-iodine to treat infectious conjunctivitis in children". American Journal of Ophthalmology. 134 (5): 681–688. doi:10.1016/S0002-9394(02)01701-4. PMID 12429243.
- "Conjunctivitis". American Optometric Association. Retrieved 15 March 2024.
- Smeltzer SC (2010). Brunner & Suddarth's textbook of medical-surgical nursing (12th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1787. ISBN 978-0-7817-8589-1. Archived from the original on 15 August 2016.
- Jhanji V, Chan TC, Li EY, Agarwal K, Vajpayee RB (September–October 2015). "Adenoviral keratoconjunctivitis". Survey of Ophthalmology. 60 (5): 435–443. doi:10.1016/j.survophthal.2015.04.001. PMID 26077630.
- "From pink eye to blindness". 28 September 2023.
- "86,133 pink eye cases in Punjab in September and counting". 28 September 2023.
- Ahmed S (27 September 2023). "Punjab Announces Holiday for Schools Amid Pink Eye Outbreak". Propakistani.
- "85 new cases of Pink Eye infection reported in Pakistan's Lahore". ETHealthworld.com. Asian News International.
External links
- "Pink Eye". MedlinePlus. U.S. National Library of Medicine.
- "Metabolomics for Ocular Surface Disease". MSBB Group, Leiden University. 28 February 2021.
| Classification | D |
|---|---|
| External resources |