| Revision as of 11:04, 21 July 2014 editTechnophant (talk | contribs)Extended confirmed users, Pending changes reviewers, Rollbackers4,780 editsm add url to ref← Previous edit | Latest revision as of 16:31, 23 December 2024 edit undoOrenburg1 (talk | contribs)Extended confirmed users166,165 editsm sp | ||
| Line 1: | Line 1: | ||
| {{Short description|Infectious disease caused by Borrelia bacteria, spread by ticks}} | |||
| {{Infobox disease | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| | Name = Lyme disease | |||
| {{Distinguish|text=], also known as "lime disease"}} | |||
| | Image = Adult deer tick.jpg | |||
| {{Use dmy dates|date=September 2017}} | |||
| | Caption = Nymphal and adult ]s can be carriers of Lyme disease. Nymphs are about the size of a poppy seed. | |||
| {{Infobox medical condition (new) | |||
| | DiseasesDB = 1531 | |||
| | name = Lyme disease | |||
| | ICD10 = {{ICD10|A|69|2|a|65}} | |||
| | synonyms = Lyme borreliosis | |||
| | ICD9 = {{ICD9|088.81}} | |||
| | image = Adult deer tick.jpg | |||
| | MedlinePlus = 001319 | |||
| | caption = An adult ] (most cases of Lyme are caused by nymphal rather than adult ticks) | |||
| | eMedicineSubj = article | |||
| | field = ] | |||
| | eMedicineTopic = 330178 | |||
| | symptoms = Expanding area of redness at the site of a ] bite, ], ], ]<ref name=CDC2013S/> | |||
| | eMedicine_mult = {{eMedicine2|article|965922}} {{eMedicine2|article|786767}} | |||
| | complications = ], ], ],<ref name="CDC2024">{{cite web |title=Clinical Care and Treatment of Neurologic Lyme Disease |url=https://www.cdc.gov/lyme/hcp/clinical-care/neurologic-lyme-disease.html#:~:text=Neurological%20complications%20most%20often%20occur,stiff%20neck%2C%20and%20severe%20headache. |website=Lyme Disease |access-date=27 May 2024 |language=en-us |date=20 May 2024}}</ref> Heart rhythm irregularities<ref>{{cite web |title=Lyme disease - Symptoms and causes |url=https://www.mayoclinic.org/diseases-conditions/lyme-disease/symptoms-causes/syc-20374651 |website=Mayo Clinic |access-date=7 June 2022 |language=en}}</ref> | |||
| | MeshID = D008193 | |||
| | onset = A week after a bite<ref name=CDC2013S/> | |||
| | duration = | |||
| | causes = '']'' spread by ticks<ref name=NEJM2014/> | |||
| | risks = | |||
| | diagnosis = Based on symptoms, tick exposure, blood tests<ref name=CDC2013Diag/> | |||
| | differential = | |||
| | prevention = Prevention of tick bites (clothing the limbs, ]), ]<ref name=NEJM2014/> | |||
| | treatment = | |||
| | medication = ], ], ], ]<ref name=NEJM2014/> | |||
| | prognosis = | |||
| | frequency = ~476k/year in U.S. (a likely overestimate), 200k/year in Europe<ref name="cdc-how-many">{{cite web |title=Lyme Disease Surveillance and Data | |||
| |url=https://www.cdc.gov/lyme/data-research/facts-stats/index.html |website=Centers for Disease Control and Prevention |access-date=16 August 2024 |language=en-us |date=15 May 2024}}</ref><ref name="cdc-estimate-2021">{{cite journal | vauthors = Kugeler KJ, Schwartz AM, Delorey MJ, Mead PS, Hinckley AF | title = Estimating the Frequency of Lyme Disease Diagnoses, United States, 2010-2018 | journal = Emerging Infectious Diseases | volume = 27 | issue = 2 | pages = 616–619 | date = February 2021 | pmid = 33496229 | pmc = 7853543 | doi = 10.3201/eid2702.202731 }}</ref><ref name="comparison-2021">{{cite journal | vauthors = Marques AR, Strle F, Wormser GP | title = Comparison of Lyme Disease in the United States and Europe | journal = Emerging Infectious Diseases | volume = 27 | issue = 8 | pages = 2017–2024 | date = August 2021 | pmid = 34286689 | pmc = 8314816 | doi = 10.3201/eid2708.204763 }}</ref> | |||
| | deaths = | |||
| }} | }} | ||
| <!-- Definition and |
<!-- Definition and symptoms --> | ||
| '''Lyme disease''' is an infectious disease caused by at least three ] of ] belonging to the ] '']''.<ref>{{cite journal|last=Westervelt|first=Holly James|author2=McCaffrey, Robert|title=Neuropsychological Functioning in Chronic Lyme Disease|journal=Neuropsychology Review|date=September 2002|volume=12|issue=3|pages=153–177|doi=10.1023/A:1020381913563 |accessdate=10 October 2013}}</ref><ref name="Samuels DS; Radolf, JD editors 2010"/><ref name=Sherris/> Early symptoms may include ], ], and ]. A ] occurs in 70–80% of infected persons at the site of the tick bite after a delay of 3–30 days (average is about 7 days), and may or may not appear as the well-publicized bull's-eye (erythema migrans). The rash is only rarely painful or itchy, although it may be warm to the touch. About 20–30% of infected persons do not experience a rash.<ref name=CDC-Signs-Symptoms-April-2011/><ref name=WebMD-October-2012/> Left untreated, later symptoms may involve the joints, heart, and ]. In most cases, the infection and its symptoms are eliminated by ], especially if the illness is treated early.<ref name=IDSA_FAQ /><ref name=cdc_signs_symptoms>http://www.cdc.gov/lyme/signs_symptoms/index.html</ref> Delayed or inadequate treatment can lead to more serious symptoms, which can be disabling and difficult to treat.<ref name="Cairns"/> | |||
| '''Lyme disease''', also known as '''Lyme borreliosis''', is a ] caused by species of '']'' bacteria, ] blood-feeding ] in the genus '']''.<ref name="NEJM2014" /><ref name="NYT-20210611" /><ref name="sciencedirect.com">{{cite journal | vauthors = Wolcott KA, Margos G, Fingerle V, Becker NS | title = Host association of Borrelia burgdorferi sensu lato: A review | journal = Ticks and Tick-Borne Diseases | volume = 12 | issue = 5 | pages = 101766 | date = September 2021 | pmid = 34161868 | doi = 10.1016/j.ttbdis.2021.101766 }}</ref> The most common sign of infection is an expanding red ], known as ] (EM), which appears at the site of the tick bite about a week afterwards.<ref name="CDC2013S">{{cite web |date=11 January 2013 |title=Signs and Symptoms of Lyme Disease |url=https://www.cdc.gov/lyme/signs_symptoms/index.html |archive-url=https://web.archive.org/web/20130116063305/http://www.cdc.gov/lyme/signs_symptoms/index.html |archive-date=16 January 2013 |access-date=2 March 2015 |website=cdc.gov}}</ref> The rash is typically neither itchy nor painful.<ref name="CDC2013S" /> Approximately 70–80% of infected people develop a rash.<ref name="CDC2013S" /> Early diagnosis can be difficult.<ref>{{cite journal | vauthors = Aucott J, Morrison C, Munoz B, Rowe PC, Schwarzwalder A, West SK | title = Diagnostic challenges of early Lyme disease: lessons from a community case series | journal = BMC Infectious Diseases | volume = 9 | pages = 79 | date = June 2009 | pmid = 19486523 | pmc = 2698836 | doi = 10.1186/1471-2334-9-79 | doi-access = free }}</ref> Other early symptoms may include fever, headaches and ].<ref name="CDC2013S" /> If untreated, symptoms may include ], ], ] or ]s.<ref name="CDC2013S" /> Months to years later, repeated episodes of joint pain and swelling may occur.<ref name="CDC2013S" /> Occasionally, shooting pains or tingling in the arms and legs may develop.<ref name="CDC2013S" /> | |||
| <!-- Cause --> | |||
| ''] ]''<ref name=Hu/> is the main cause of Lyme disease in ], whereas '']'' and '']'' cause most ]an cases. ''Borrelia'' is transmitted to humans by the bite of infected ticks belonging to a few species of the genus '']'' ("hard ticks").<ref name=Baron/> Lyme disease is the most common tick-borne disease in the ].<ref name=fell_2000/> | |||
| <!-- |
<!-- Cause and diagnosis --> | ||
| Lyme disease is transmitted to humans by the bites of infected ticks of the genus ''Ixodes''.<ref>{{cite book |vauthors=Johnson RC |chapter=Borrelia |title=Baron's Medical Microbiology |veditors=Baron S |display-editors=etal |edition=4th |publisher=Univ of Texas Medical Branch |year=1996 |chapter-url=https://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=mmed.section.1965 |isbn=978-0-9631172-1-2 |pmid=21413339 |archive-url=https://web.archive.org/web/20090207104450/http://www.ncbi.nlm.nih.gov/books/bv.fcgi |archive-date=7 February 2009 |url-status=live}}</ref> In the United States, ticks of concern are usually of the '']'' type. According to the ], "In most cases, a tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted. If you remove a tick quickly (within 24 hours), you can greatly reduce your chances of getting Lyme disease."<ref name=CDC2013T>{{cite web |title=Lyme disease transmission|website=cdc.gov |date=11 January 2013 |url=https://www.cdc.gov/lyme/transmission/index.html |access-date=2 March 2015|url-status=live|archive-url=https://web.archive.org/web/20150303002640/http://www.cdc.gov/Lyme/transmission/index.html|archive-date=3 March 2015}}</ref><!-- Quote = In most cases, the tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted. --><ref name=Ste2016>{{cite journal | vauthors = Steere AC, Strle F, Wormser GP, Hu LT, Branda JA, Hovius JW, Li X, Mead PS | title = Lyme borreliosis | journal = Nature Reviews. Disease Primers | volume = 2 | pages = 16090 | date = December 2016 | pmid = 27976670 | pmc = 5539539 | doi = 10.1038/nrdp.2016.90 }}</ref> In Europe, '']'' ticks may spread the bacteria more quickly.<ref name=Ste2016/><ref>{{cite web |url=https://ecdc.europa.eu/sites/portal/files/media/en/healthtopics/emerging_and_vector-borne_diseases/tick_borne_diseases/public_health_measures/Documents/HCP_factsheet_LB_highres.pdf |title=Lyme borreliosis|website=]|access-date=29 September 2018|url-status=live|archive-url=https://web.archive.org/web/20180929000428/https://ecdc.europa.eu/sites/portal/files/media/en/healthtopics/emerging_and_vector-borne_diseases/tick_borne_diseases/public_health_measures/Documents/HCP_factsheet_LB_highres.pdf |archive-date=29 September 2018}}</ref> In North America, the bacterial species ''] ''and ] cause Lyme disease.<ref name="NEJM2014" /><ref name="Lancet2016">{{cite journal | vauthors = Pritt BS, Mead PS, Johnson DK, Neitzel DF, Respicio-Kingry LB, Davis JP, Schiffman E, Sloan LM, Schriefer ME, Replogle AJ, Paskewitz SM, Ray JA, Bjork J, Steward CR, Deedon A, Lee X, Kingry LC, Miller TK, Feist MA, Theel ES, Patel R, Irish CL, Petersen JM | title = Identification of a novel pathogenic Borrelia species causing Lyme borreliosis with unusually high spirochaetaemia: a descriptive study | journal = The Lancet. Infectious Diseases | volume = 16 | issue = 5 | pages = 556–564 | date = May 2016 | pmid = 26856777 | pmc = 4975683 | doi = 10.1016/S1473-3099(15)00464-8 }}</ref> In Europe and Asia,'' ], ], ]'' and four other species also cause the disease.<ref name="NEJM2014">{{cite journal | vauthors = Shapiro ED | title = Clinical practice. Lyme disease | journal = The New England Journal of Medicine | volume = 370 | issue = 18 | pages = 1724–1731 | date = May 2014 | pmid = 24785207 | pmc = 4487875 | doi = 10.1056/NEJMcp1314325 | url = http://portal.mah.harvard.edu/templatesnew/departments/MTA/Lyme/uploaded_documents/NEJMcp1314325.pdf | access-date = 5 July 2016 | url-status = dead | archive-url = https://web.archive.org/web/20160821071927/http://portal.mah.harvard.edu/templatesnew/departments/MTA/Lyme/uploaded_documents/NEJMcp1314325.pdf | archive-date = 21 August 2016 }}</ref> The disease does not appear to be transmissible between people, by other animals nor through food.<ref name="CDC2013T"/> Diagnosis is based on a combination of symptoms, history of tick exposure and possibly testing for specific ] in the blood.<ref name="CDC2013Diag">{{cite web|title=Lyme Disease Diagnosis and Testing|website=cdc.gov|date=10 January 2013|url=https://www.cdc.gov/lyme/diagnosistesting/index.html|access-date=2 March 2015|archive-url=https://web.archive.org/web/20150302013440/http://www.cdc.gov/lyme/diagnosistesting/index.html|archive-date=2 March 2015|url-status=live}}</ref><ref>{{cite web|title=Two-step Laboratory Testing Process |url=https://www.cdc.gov/lyme/diagnosistesting/LabTest/TwoStep/index.html|website=cdc.gov|access-date=2 March 2015|date=15 November 2011|url-status=live|archive-date=12 March 2015|archive-url=https://web.archive.org/web/20150312123313/http://www.cdc.gov/lyme/diagnosistesting/labtest/twostep/index.html}}</ref> Blood tests are often falsely negative in the early stages of the disease.<ref name="NEJM2014"/> Testing of individual ticks is not typically useful.<ref>{{cite web|title=Testing of Ticks|url=https://www.cdc.gov/lyme/diagnosistesting/LabTest/Testing/index.html|website=cdc.gov|access-date=2 March 2015|date=4 June 2013|url-status=live|archive-date=19 February 2015|archive-url=https://web.archive.org/web/20150219183735/http://www.cdc.gov/lyme/diagnosistesting/LabTest/Testing/index.html|quote=Although some commercial groups offer testing, in general it is not recommended}}</ref> | |||
| The term "]" is controversial and not recognized in the medical literature,<ref name="nejm-feder"/> and most medical authorities advise against long-term antibiotic treatment for "chronic Lyme disease".<ref name="idsa guideline"/><ref name="pmid17522387"/><ref name="nih-cld"/> | |||
| <!-- |
<!-- Prevention and treatment --> | ||
| Prevention includes efforts to prevent tick bites by wearing clothing to cover the arms and legs and using ] or ]-based ]s.<ref name=NEJM2014/><ref name="NYT-20210611">{{cite news | vauthors = Wenner M |title=Let's Do a Tick Check - These pervasive bloodsuckers can give you more than just Lyme disease. Here's how to protect yourself. (Interactive) |url=https://www.nytimes.com/interactive/2021/06/11/well/tick-disease-lyme.html |date=11 June 2021 |work=] |access-date=19 June 2021 }}</ref> Using ]s to reduce tick numbers may also be effective.<ref name=NEJM2014/> Ticks can be removed using ]s.<ref>{{cite web|title=Tick Removal|url=https://www.cdc.gov/lyme/removal/index.html|website=cdc.gov|access-date=2 March 2015|date=23 June 2014|url-status=live|archive-url=https://web.archive.org/web/20150310141610/http://www.cdc.gov/lyme/removal/index.html|archive-date=10 March 2015}}</ref> If the removed tick is full of blood a single dose of ] may be used to prevent the development of infection but is not generally recommended since the development of infection is rare.<ref name=NEJM2014/> If an infection develops, a number of antibiotics are effective, including doxycycline, ] and ].<ref name=NEJM2014/> Standard treatment usually lasts for two or three weeks.<ref name=NEJM2014/> Some people develop a fever and muscle and joint pains from treatment, which may last for one or two days.<ref name=NEJM2014/> In those who develop persistent symptoms, long-term antibiotic therapy has not been found to be useful.<ref name=NEJM2014/><ref name=CDC2017PT/> | |||
| The first known existence of the ''Borrelia'' bacteria dates back to up to 20 million years ago.<ref>http://news.discovery.com/human/health/lyme-disease-bacteria-older-than-the-human-race-140529.htm</ref> The disease is named after the towns of ] and ], US, where a number of cases were identified in 1975. Although it was known that Lyme disease was a ] as far back as 1978, the cause of the disease remained a mystery until 1981, when ''B. burgdorferi'' was identified by entomologist Dr. ]. | |||
| <!-- Epidemiology, history and society --> | |||
| Lyme disease is the most common disease spread by ticks in the Northern Hemisphere.<ref>{{cite book|title=Regional Disease Vector Ecology Profile: Central Europe|date=April 2001|publisher=DIANE Publishing|isbn=978-1-4289-1143-7 |page=136|url=https://books.google.com/books?id=Hpr10wAwoE0C&pg=PA136|url-status=live|archive-url=https://web.archive.org/web/20170908151350/https://books.google.com/books?id=Hpr10wAwoE0C&pg=PA136|archive-date=8 September 2017}}</ref><ref name="comparison-2021"/> Infections are most common in the spring and early summer.<ref name=NEJM2014/> Lyme disease was diagnosed as a separate condition for the first time in 1975 in ]. It was originally mistaken for ].<ref name=Car2007>{{cite book| vauthors = Williams C |title=Infectious disease epidemiology : theory and practice|date=2007|publisher=Jones and Bartlett Publishers|location=Sudbury, Mass.|isbn=978-0-7637-2879-3|page=447|edition=2nd|url=https://books.google.com/books?id=o_j-G4zJ4cQC&pg=PA447|url-status=live|archive-url=https://web.archive.org/web/20170908151350/https://books.google.com/books?id=o_j-G4zJ4cQC&pg=PA447|archive-date=8 September 2017}}</ref> The bacterium involved was first described in 1981 by ].<ref name=Tele2014>{{cite news|url=https://www.telegraph.co.uk/news/obituaries/11265730/Willy-Burgdorfer-obituary.html|title=Willy Burgdorfer – obituary|work=Daily Telegraph|date=1 December 2014|access-date=1 December 2014|url-status=live|archive-url=https://web.archive.org/web/20141201213904/http://www.telegraph.co.uk/news/obituaries/11265730/Willy-Burgdorfer-obituary.html|archive-date=1 December 2014}}</ref> People with persistent symptoms after appropriate treatments are said to have Post-Treatment Lyme Disease Syndrome (PTLDS).<ref name=":0">{{Cite web |last=CDC |date=2024-06-11 |title=Chronic Symptoms and Lyme Disease |url=https://www.cdc.gov/lyme/signs-symptoms/chronic-symptoms-and-lyme-disease.html |access-date=2024-07-27 |website=Lyme Disease |language=en-us}}</ref> PTLDS is different from ], a term no longer supported by scientists and used in different ways by different groups.<ref name=CDC2017PT>{{cite web|title=Post-Treatment Lyme Disease Syndrome|url=https://www.cdc.gov/lyme/postLDS/index.html|website=cdc.gov|access-date=20 June 2018|date=1 December 2017|archive-url=https://web.archive.org/web/20150227054926/http://www.cdc.gov/lyme/postLDS/index.html|archive-date=27 February 2015|url-status=live}}</ref><ref>{{cite journal | vauthors = Baker PJ | title = Chronic Lyme disease: in defense of the scientific enterprise | journal = FASEB Journal | volume = 24 | issue = 11 | pages = 4175–4177 | date = November 2010 | pmid = 20631327 | doi = 10.1096/fj.10-167247 | doi-access = free | s2cid = 36141950 }}</ref> Some healthcare providers claim that chronic Lyme is caused by persistent infection, but this is not believed to be true because no evidence of persistent infection can be found after standard treatment.<ref name=Lantos2015>{{cite journal | vauthors = Lantos PM | title = Chronic Lyme disease | journal = Infectious Disease Clinics of North America | volume = 29 | issue = 2 | pages = 325–340 | date = June 2015 | pmid = 25999227 | pmc = 4477530 | doi = 10.1016/j.idc.2015.02.006 }}</ref> | |||
| {{As of|2023}}, clinical trials of proposed human ] were being carried out, but no vaccine was available. A vaccine, LYMERix, was produced, but discontinued in 2002 due to insufficient demand.<ref name="cdc-vaccine" /> There are several vaccines for the prevention of Lyme disease in dogs. | |||
| {{TOC limit}} | |||
| {{TOC limit|3}} | |||
| ==Signs and symptoms== | ==Signs and symptoms== | ||
| , CDC, page last reviewed: April 12, 2011.</ref><ref name=WebMD-October-2012>, WedMD Rheumatoid Arthritis Health Center, reviewed by David Zelman, MD on Oct. 1, 2012.</ref>]] | |||
| <!-- ] --> | |||
| ] | |||
| Lyme disease can produce a broad range of symptoms. | |||
| Lyme disease can affect multiple body systems and produce a range of symptoms. Not all patients with Lyme disease will have all symptoms, and many of the symptoms are not specific to Lyme disease, but can occur with other diseases, as well. The ] from infection to the onset of symptoms is usually one to two weeks, but can be much shorter (days), or much longer (months to years).<ref name="Lymedisease"/> | |||
| {{Gallery | |||
| Symptoms most often occur from May to September, because the nymphal stage of the tick is responsible for most cases.<ref name="Lymedisease" /> ] infection exists, but occurs in less than 7% of infected individuals in the United States.<ref name="pmid12905137"/> Asymptomatic infection may be much more common among those infected in Europe.<ref name="pmid23319969"/><ref name="pmid9556169"/> | |||
| |width=150 | |||
| |align=right | |||
| |File:Erythema migrans - erythematous rash in Lyme disease - PHIL 9875.jpg|20% of Lyme rashes in the United States show a "bull's eye" or "target-like" appearance.<ref name=wright_2012/><ref name=CDC_Lyme_rashes>{{cite web |title=Lyme disease rashes and look-alikes |url=https://www.cdc.gov/lyme/signs_symptoms/rashes.html |website=Lyme Disease |publisher=Centers for Disease Control and Prevention |date=December 21, 2018 |archive-url=https://web.archive.org/web/20190402185303/https://www.cdc.gov/lyme/signs_symptoms/rashes.html |archive-date=April 2, 2019 |url-status=live |access-date=April 18, 2019}}</ref><ref name=lyme_rashes_uk>{{cite web |title=Lyme disease: erythema migrans |url=https://www.nice.org.uk/guidance/ng95/resources/lyme-disease-rash-images-pdf-4792273597 |website=Lyme disease NICE guideline |publisher=National Institute for Health and Care Excellence |access-date=May 8, 2019 |archive-url=https://web.archive.org/web/20190509035408/https://www.nice.org.uk/guidance/ng95/resources/lyme-disease-rash-images-pdf-4792273597 |archive-date=May 9, 2019 |url-status=live}}</ref> | |||
| |File:Solid_erythema_migrans_rash_on_the_neck_of_a_woman_with_Lyme_disease.jpg|] ("migrating redness") on a woman's neck.<ref name="boyce">{{cite journal |last1=Boyce |first1=RM |last2=Pretsch |first2=P |last3=Tyrlik |first3=K |last4=Schulz |first4=A |last5=Giandomenico |first5=DA |last6=Barbarin |first6=AM |last7=Williams |first7=C |title=Delayed Diagnosis of Locally Acquired Lyme Disease, Central North Carolina, USA. |journal=Emerging Infectious Diseases |date=March 2024 |volume=30 |issue=3 |pages=564–567 |doi=10.3201/eid3003.231302 |pmid=38407256 |pmc=10902532}}</ref> Rashes from non-Lyme causes may look similar.<ref name=tibbles_2007/><ref name="annular">{{cite journal |last1=Trayes |first1=KP |last2=Savage |first2=K |last3=Studdiford |first3=JS |title=Annular Lesions: Diagnosis and Treatment. |journal=American Family Physician |date=1 September 2018 |volume=98 |issue=5 |pages=283–291 |pmid=30216021 |url=https://www.aafp.org/pubs/afp/issues/2018/0901/p283.html}}</ref> | |||
| }} | |||
| The ] is usually one to two weeks, but can be much shorter (days) or much longer (months to years).<ref name="Lymedisease"/> Lyme symptoms most often occur from the month of May to September in the Northern Hemisphere because the nymphal stage of the tick is responsible for most cases.<ref name="Lymedisease" /> | |||
| ===Early localized infection=== | ===Early localized infection=== | ||
| 80% of Lyme infections begin with a rash of some sort at the site of a tick bite, often near skin folds such as the ], ], ], or the ] under clothing straps, or in children's hair, ears, or neck.<ref name=wright_2012/><ref name=NEJM2014/> Most people who get infected do not remember seeing a tick or a bite. The rash appears typically one or two weeks (range 3–32 days) after the bite and expands 2–3 cm per day up to a diameter of 5–70 cm (median is 16 cm).<ref name=wright_2012/><ref name=NEJM2014/><ref name=tibbles_2007>{{cite journal | vauthors = Tibbles CD, Edlow JA | title = Does this patient have erythema migrans? | journal = JAMA | volume = 297 | issue = 23 | pages = 2617–2627 | date = June 2007 | pmid = 17579230 | doi = 10.1001/jama.297.23.2617 }}</ref> | |||
| Early localized infection can occur when the infection has not yet spread throughout the body. Only the site where the infection has first come into contact with the skin is affected. The classic sign of early local infection with Lyme disease is a circular, outwardly expanding rash called ] (also erythema migrans or EM), which occurs at the site of the tick bite three to 30 days after the tick bite.<ref name=emed_ophth/><ref name="isbn0-07-159991-6"/> The rash is red, and may be warm, but is generally painless. Classically, the innermost portion remains dark red and becomes ] (is thicker and firmer); the outer edge remains red; and the portion in between clears, giving the appearance of a ]. However, partial clearing is uncommon, and the bull's-eye pattern more often involves central redness.<ref name="pmid11900494"/> | |||
| The rash is usually circular or oval, red or bluish, and may have an elevated or darker center.<ref name=NEJM2014/><ref name=CDC_Lyme_rashes/><ref name=lyme_rashes_uk/> This rash is termed an ] which translates as "Migrating Redness." In about 79% of cases in Europe, this rash gradually clears from the center toward the edges possibly forming a "bull's eye" or "target-like" pattern, but this clearing only happens in 19% of cases in endemic areas of the United States.<ref name=tibbles_2007/><ref name=CDC_Lyme_rashes/><ref name=lyme_rashes_uk/> The rash may feel warm, usually is not itchy, is rarely tender or painful, and takes up to four weeks to resolve if untreated.<ref name=NEJM2014/> | |||
| The EM rash associated with early infection is found in about 80% of patients<ref name="isbn0-07-159991-6"/> and can have a range of appearances including the classic target bull's-eye lesion and nontarget appearing lesions. The 20% without the EM and the nontarget lesions can often cause misidentification of Lyme disease.<ref name=aucott_2012/> Patients can also experience ], such as ], ], ], and ].<ref name="pmid14987414"/> Lyme disease can progress to later stages even in patients who do not develop a rash.<ref name="pmid23319969"/><ref name="pmid12543291"/> | |||
| The Lyme rash is often accompanied by symptoms of a flu-like illness, including fatigue, headache, body aches, fever, and chills . These symptoms may also appear without a rash or linger after the rash has disappeared. Lyme can progress to later stages without a rash or these symptoms.<ref name=NEJM2014/> | |||
| People with high fever for more than two days or whose other symptoms of viral-like illness do not improve despite ] treatment for Lyme disease, or who have abnormally low levels of ] or ] cells or ] in the blood, should be investigated for possible coinfection with other ] such as ] and ].<ref name="idsa guideline"/> | |||
| Not everyone with Lyme disease has all the symptoms, and many of these symptoms can also occur with other diseases.<ref>{{cite web |url=https://www.lecturio.com/concepts/lyme-disease/| title=Lyme Disease|website=The Lecturio Medical Concept Library |access-date= 9 July 2021}}</ref> | |||
| ] infection exists, but occurs in less than 7% of infected individuals in the United States.<ref name="pmid12905137"/> Asymptomatic infection may be much more common among those infected in Europe.<ref name="pmid23319969"/> | |||
| ===Early disseminated infection=== | ===Early disseminated infection=== | ||
| Within days to weeks after the onset of local infection, the '' |
Within days to weeks after the onset of local infection, the ''Borrelia'' bacteria may spread through the lymphatic system or bloodstream. In 10–20% of untreated cases, EM rashes develop at sites across the body that bear no relation to the original tick bite.<ref name=wright_2012/> Transient ] and ] are also common.<ref name=wright_2012/> | ||
| ] on the cheek (very uncommon)]] | |||
| Various acute neurological problems, termed ], appear in 10–15% of untreated patients.<ref name="pmid14987414"/><ref name="Halperin2008"/> These include ], which is the loss of muscle tone on one or both sides of the face, as well as ], which involves severe headaches, neck stiffness, and sensitivity to light. ] causes shooting pains that may interfere with sleep, as well as abnormal skin sensations. Mild ] may lead to ], ], or mood changes. In addition, some ]s have described altered mental status as the only symptom seen in a few cases of early neuroborreliosis.<ref name=chabria_2007/> The disease may also have cardiac manifestations such as ].{{citation needed|date=January 2012}} | |||
| In about 10–15% of untreated people, Lyme causes neurological problems known as ].<ref name="Halperin2008"/> Early neuroborreliosis typically appears 4–6 weeks (range 1–12 weeks) after the tick bite and involves some combination of lymphocytic meningitis, cranial neuritis, radiculopathy, and/or mononeuritis multiplex.<ref name="idsa guideline"/><ref name=efns_guidelines>{{cite journal | vauthors = Mygland A, Ljøstad U, Fingerle V, Rupprecht T, Schmutzhard E, Steiner I | title = EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis | journal = European Journal of Neurology | volume = 17 | issue = 1 | pages = 8–16 | date = January 2010 | pmid = 19930447 | doi = 10.1111/j.1468-1331.2009.02862.x | url = https://www.eaneurology.org/fileadmin/user_upload/guidline_papers/EFNS_guideline_2010_European_lyme_neuroborreliosis.pdf | access-date = 30 April 2019 | url-status = live | s2cid = 14166137 | doi-access = free | archive-url = https://web.archive.org/web/20170808101146/https://www.eaneurology.org/fileadmin/user_upload/guidline_papers/EFNS_guideline_2010_European_lyme_neuroborreliosis.pdf | archive-date = 8 August 2017 }}</ref> ] causes ] in the ] (CSF) and may be accompanied for several weeks by variable headache and, less commonly, usually mild ] such as ] and ] but typically no or only very low fever.<ref name=steere_neuro_findings>{{cite journal | vauthors = Pachner AR, Steere AC | title = Neurological findings of Lyme disease | journal = The Yale Journal of Biology and Medicine | volume = 57 | issue = 4 | pages = 481–483 | date = July 1984 | pmid = 6516450 | pmc = 2590042 }}</ref> After several months neuroborreliosis can also present ]. Up to 76.5% of them present as ], the most common symptom. ] and dizziness (53.7%) and hearing loss (16.7%) were the next most common symptoms.<ref>{{cite journal | vauthors = Moscatello AL, Worden DL, Nadelman RB, Wormser G, Lucente F | title = Otolaryngologic aspects of Lyme disease | journal = The Laryngoscope | volume = 101 | issue = 6 Pt 1 | pages = 592–595 | date = June 1991 | pmid = 2041438 | doi = 10.1288/00005537-199106000-00004 | s2cid = 35345898 }}</ref> In children, ] may also occur.<ref name="idsa guideline"/> Cranial ] is an inflammation of ]. When due to Lyme, it most typically causes ], impairing blinking, smiling, and chewing on one or both sides of the face. It may also cause intermittent ].<ref name="idsa guideline"/><ref name=steere_neuro_findings/> Lyme ] is an inflammation of spinal ]s that often causes ] and less often ], ], or ] in the ], e.g. limb(s) or part(s) of trunk. The pain is often described as unlike any other previously felt, excruciating, migrating, worse at night, rarely symmetrical, and often accompanied by extreme sleep disturbance.<ref name=efns_guidelines/><ref name=ogrinc_bannwarth>{{cite journal | vauthors = Ogrinc K, Lusa L, Lotrič-Furlan S, Bogovič P, Stupica D, Cerar T, Ružić-Sabljić E, Strle F | title = Course and Outcome of Early European Lyme Neuroborreliosis (Bannwarth Syndrome): Clinical and Laboratory Findings | journal = Clinical Infectious Diseases | volume = 63 | issue = 3 | pages = 346–353 | date = August 2016 | pmid = 27161773 | doi = 10.1093/cid/ciw299 | doi-access = free }}</ref> ] is an inflammation causing similar symptoms in one or more unrelated peripheral nerves.<ref name="Halperin2008"/><ref name="idsa guideline"/> Rarely, early neuroborreliosis may involve inflammation of the ] or ], with symptoms such as confusion, ], ], ], or ].<ref name="idsa guideline"/><ref name=efns_guidelines/> | |||
| ==={{anchor|Bannwarth syndrome}} Late disseminated infection=== | |||
| After several months, untreated or inadequately treated patients may go on to develop severe and chronic symptoms that affect many parts of the body, including the brain, nerves, eyes, joints, and heart. Many disabling symptoms can occur, including permanent ] of the lower extremities in extreme cases.<ref name="pmid23319969"/> The associated nerve pain radiating out from the spine is termed Bannwarth syndrome,<ref name="pmid19562015"/> named after ]. | |||
| In North America, facial palsy is the typical early neuroborreliosis presentation, occurring in 5–10% of untreated people, in about 75% of cases accompanied by lymphocytic meningitis.<ref name="idsa guideline"/><ref name=garro_2018/> Lyme radiculopathy is reported half as frequently, but many cases may be unrecognized.<ref name=halperin_2010>{{cite journal | vauthors = Halperin JJ | title = Nervous system Lyme disease | journal = The Journal of the Royal College of Physicians of Edinburgh | volume = 40 | issue = 3 | pages = 248–255 | date = September 2010 | pmid = 21127770 | doi = 10.4997/JRCPE.2010.314 | doi-broken-date = 1 December 2024 | doi-access = free }}</ref> In European adults, the most common presentation is a combination of lymphocytic meningitis and radiculopathy known as ], accompanied in 36-89% of cases by facial palsy.<ref name=efns_guidelines/><ref name=ogrinc_bannwarth/> In this syndrome, radicular pain tends to start in the same body region as the initial ] rash, if there was one, and precedes possible ] and other ].<ref name=ogrinc_bannwarth/> In extreme cases, permanent ] of the lower limbs may occur.<ref name="pmid23319969"/> In European children, the most common manifestations are facial palsy (in 55%), other cranial neuritis, and lymphocytic meningitis (in 27%).<ref name=efns_guidelines/> | |||
| The late disseminated stage is where the infection has fully spread throughout the body. Chronic neurologic symptoms occur in up to 5% of untreated patients.<ref name="pmid14987414"/> A ] that involves shooting pains, numbness, and tingling in the hands or feet may develop. A neurologic syndrome called Lyme encephalopathy is associated with subtle cognitive problems, such as difficulties with concentration and short-term memory. These patients may also experience fatigue.<ref name=Shadick/> However, other problems, such as ] and ], are no more common in people with Lyme disease than in the general population.<ref name=Shadick/><ref name=seltzer_2000/> | |||
| {{Anchor|Carditis2021-05-10}}In about 4–10% of untreated cases in the United States and 0.3–4% of untreated cases in Europe, typically between June and December, about one month (range 4 days to 7 months) after the tick bite, the infection may cause heart complications known as Lyme ].<ref name=fish_2008>{{cite journal | vauthors = Fish AE, Pride YB, Pinto DS | title = Lyme carditis | journal = Infectious Disease Clinics of North America | volume = 22 | issue = 2 | pages = 275–88, vi | date = June 2008 | pmid = 18452801 | doi = 10.1016/j.idc.2007.12.008 | url = https://www.cdc.gov/lyme/resources/Fish2008-508.pdf | access-date = 9 May 2019 | url-status = live | archive-url = https://web.archive.org/web/20170829030422/https://www.cdc.gov/lyme/resources/Fish2008-508.pdf | archive-date = 29 August 2017 }}</ref><ref name="Stanek2012">{{cite journal | vauthors = Stanek G, Wormser GP, Gray J, Strle F | title = Lyme borreliosis | journal = Lancet | volume = 379 | issue = 9814 | pages = 461–473 | date = February 2012 | pmid = 21903253 | doi = 10.1016/S0140-6736(11)60103-7 | s2cid = 31461047 }}</ref> Symptoms may include heart ] (in 69% of people), ], ], ], and ].<ref name=fish_2008/> Other symptoms of Lyme disease may also be present, such as ] rash, ], ], ], or ].<ref name=fish_2008/> In some people, however, carditis may be the first manifestation of Lyme disease.<ref name=fish_2008/> Lyme carditis in 19–87% of people adversely impacts the heart's electrical conduction system, causing atrioventricular ] that often manifests as heart rhythms that alternate within minutes between abnormally slow and abnormally fast.<ref name=fish_2008/><ref name="Stanek2012"/> In 10–15% of people, Lyme causes ] complications such as ], left ] dysfunction, or congestive heart failure.<ref name=fish_2008/> | |||
| Chronic ], which may be progressive, can involve cognitive impairment, weakness in the legs, awkward gait, facial palsy, bladder problems, ], and back pain. In rare cases, untreated Lyme disease may cause ], which has been misdiagnosed as ] or ]. Panic attacks and anxiety can occur; also, delusional behavior may be seen, including ] delusions, sometimes accompanied by a ] or derealization syndrome, where the patients begin to feel detached from themselves or from reality.<ref name=fallon_1994/><ref name=hess_1999/> | |||
| Another skin condition, found in Europe but not in North America, is ], a purplish lump that develops on the ear lobe, nipple, or ].<ref name="pmid18452805"/> | |||
| Lyme arthritis usually affects the knees.<ref name="pmid18452802"/> In a minority of patients, arthritis can occur in other joints, including the ankles, elbows, wrist, hips, and shoulders. Pain is often mild or moderate, usually with swelling at the involved joint. ]s may form and rupture. In some cases, joint erosion occurs. | |||
| ==={{anchor|Bannwarth syndrome}} Late disseminated infection=== | |||
| ] (ACA) is a chronic skin disorder observed primarily in Europe among the elderly.<ref name="pmid18452805"/> ACA begins as a reddish-blue patch of discolored skin, often on the backs of the hands or feet. The lesion slowly atrophies over several weeks or months, with the skin becoming first thin and wrinkled and then, if untreated, completely dry and hairless.<ref name=mullegger_2004/> | |||
| ] | |||
| Lyme arthritis occurs in up to 60% of untreated people, typically starting about six months after infection.<ref name=wright_2012/> It usually affects only one or a few joints, often a knee or possibly the ], other large joints, or the ].<ref name="idsa guideline"/><ref name="pmid18452802"/> Usually, large ] and swelling occur, but only mild or moderate pain.<ref name="idsa guideline"/> Without treatment, swelling and pain typically resolve over time, but periodically return.<ref name="idsa guideline"/> ]s may form and rupture. | |||
| In early US studies of Lyme disease, a rare ] was described that included numbness, tingling, or burning starting at the feet or hands and over time possibly moving up the limbs. In a later analysis that discovered poor documentation of this manifestation, experts wondered if it exists at all in the US or is merely very rare.<ref name="idsa guideline"/><ref name="axonal">{{cite journal | vauthors = Wormser GP, Strle F, Shapiro ED, Dattwyler RJ, Auwaerter PG | title = A critical appraisal of the mild axonal peripheral neuropathy of late neurologic Lyme disease | journal = Diagnostic Microbiology and Infectious Disease | volume = 87 | issue = 2 | pages = 163–167 | date = February 2017 | pmid = 27914746 | pmc = 5924701 | doi = 10.1016/j.diagmicrobio.2016.11.003 }}</ref> | |||
| A neurologic syndrome called Lyme encephalopathy is associated with subtle memory and cognitive difficulties, ], ], and changes in personality.<ref name=MayoClin2008>{{cite journal | vauthors = Bratton RL, Whiteside JW, Hovan MJ, Engle RL, Edwards FD | title = Diagnosis and treatment of Lyme disease | journal = Mayo Clinic Proceedings | volume = 83 | issue = 5 | pages = 566–571 | date = May 2008 | pmid = 18452688 | doi = 10.4065/83.5.566 | doi-access = free }}</ref> Lyme encephalopathy is controversial in the US and has not been reported in Europe.<ref name="comparison-2021"/> Problems such as depression and ] are as common in people with Lyme disease as in the general population.<ref name=Shadick/><ref name=seltzer_2000/> There is no compelling evidence that Lyme disease causes psychiatric disorders, behavioral disorders (e.g. ]), or developmental disorders (e.g. ]).<ref name="guidelines-2020"/> | |||
| ] is a chronic skin disorder observed primarily in Europe among the elderly.<ref name="pmid18452805"/> It begins as a reddish-blue patch of discolored skin, often on the backs of the hands or feet. The lesion slowly atrophies over several weeks or months, with the skin becoming first thin and wrinkled and then, if untreated, completely dry and hairless.<ref name=mullegger_2004/> It is also associated with peripheral neuropathy.<ref name="axonal"/> | |||
| ==Cause== | ==Cause== | ||
| {{Main|Lyme disease microbiology}} | {{Main|Lyme disease microbiology}} | ||
| {{Further|Weather and climate effects on Lyme disease exposure}} | |||
| ] | |||
| ]'' bacteria, the causative |
]'' bacteria, the causative agents of Lyme disease, magnified]] | ||
| Lyme disease is caused by ]s, ] from the ] '']''. Spirochetes are surrounded by ] and ].<ref name="Winslow">{{cite journal |vauthors=Winslow C, Coburn J |title=Recent discoveries and advancements in research on the Lyme disease spirochete Borrelia burgdorferi |journal=F1000Res |volume=8 |issue= |date=2019 |page=763 |pmid=31214329 |pmc=6545822 |doi=10.12688/f1000research.18379.1 |doi-access=free |url=}}</ref> The Lyme-related ''Borrelia'' species are collectively known as ''] ]'', and show a great deal of ].<ref>{{cite book |veditors= Radolf JD, Samuels DS | year=2021 |title=Lyme Disease and Relapsing Fever Spirochetes: Genomics, Molecular Biology, Host Interactions, and Disease Pathogenesis |url= https://www.caister.com/lyme | publisher=Caister Academic Press | isbn= 978-1-913652-61-6}}</ref> | |||
| ]'', the primary vector of Lyme disease in eastern North America]] | |||
| Lyme disease is caused by ] ] from the ] '']''. Spirochetes are surrounded by ] and ], along with an outer membrane similar to other Gram-negative bacteria. Because of their double-membrane envelope, ''Borrelia'' bacteria are often mistakenly described as ] despite the considerable differences in their envelope components from Gram-negative bacteria.<ref name=samuels_2010/> The Lyme-related ''Borrelia'' species are collectively known as ''Borrelia burgdorferi ]'', and show a great deal of ]. | |||
| ''B. burgdorferi sensu lato'' is made up of |
''B. burgdorferi sensu lato'' is a species complex made up of 20 accepted and three proposed genospecies. Eight species are known to cause Lyme disease: ''B. mayonii'' (found in North America), ''B. burgdorferi ]'' (found in North America and Europe), ''B. afzelii'', ''B. garinii, B. spielmanii,'' and ''B. lusitaniae'' (all found in ]).<ref name=Cutler2016>{{cite journal | vauthors = Cutler SJ, Ruzic-Sabljic E, Potkonjak A | title = Emerging borreliae - Expanding beyond Lyme borreliosis | journal = Molecular and Cellular Probes | volume = 31 | pages = 22–27 | date = February 2017 | pmid = 27523487 | doi = 10.1016/j.mcp.2016.08.003 | url = http://roar.uel.ac.uk/5199/1/RBG_Emerging%20borreliosis%20for%20submissionmodHPFAug10_corrected%20without%20track%20change%20SJC.pdf }}</ref><ref name=Stanek2011/><ref name=Lancet2016/><ref name="sciencedirect.com"/> | ||
| Some studies have also proposed that ''B. valaisiana'' may sometimes infect humans, but this species does not seem to be an important cause of disease.<ref name="pmid18454594"/><ref name="pmid18650352"/> | |||
| === Tick life cycle === | |||
| {{further|Weather and climate effects on Lyme disease exposure}} | |||
| ] | |||
| ]'', the primary vector of Lyme disease in eastern North America]] | |||
| Three stages occur in the life cycle of a tick - larva, nymph, and adult. During the nymph stage, ticks most frequently transmit Lyme disease and are usually most active in late spring and early summer in regions where the climate is mild. During the adult stage, Lyme disease transmission is less common because adult ticks are less likely to bite humans and tend to be larger in size, so can be easily seen and removed.<ref>{{Cite web|title=UpToDate|url=https://www.uptodate.com/contents/evaluation-of-a-tick-bite-for-possible-lyme-disease|access-date=2021-07-10|website=www.uptodate.com}}</ref> | |||
| ===Transmission=== | ===Transmission=== | ||
| Lyme disease is classified as a ], as it is transmitted to humans from a ] among |
Lyme disease is classified as a ], as it is ] to humans from a ] among small mammals and birds by ]s that feed on both sets of ].<ref name=pmid18452798/> Hard-bodied ticks of the genus ''Ixodes'' are the ] of Lyme disease (also the vector for '']'').<ref name=Sherris /> Most infections are caused by ticks in the ], because they are very small, thus may feed for long periods of time undetected.<ref name=pmid18452798/> Nymphal ticks are generally the size of a poppy seed and sometimes with a dark head and a translucent body.<ref name=Rut2005>{{cite web | url = https://ocean.njaes.rutgers.edu/garden/documents/fs443.pdf | title = 2005 Fact Sheet, Prevent Tick Bites: Prevent Lyme Disease | archive-url = https://web.archive.org/web/20130626133450/http://ocean.njaes.rutgers.edu/garden/documents/fs443.pdf | archive-date=26 June 2013 | publisher = Rutgers University, Rutgers Cooperative Research & Extension, New Jersey Agricultural Experiment Station | vauthors = Smith-Fiola D, Hamilton GC | date = March 2005 }}</ref> Or, the nymphal ticks can be darker.<ref>{{cite web | url = https://www.deseret.com/2019/5/31/20674560/people-are-freaking-out-over-the-cdc-s-photo-of-a-muffin-with-ticks-in-it | title = People are freaking out over the CDC's photo of a muffin with ticks in it | archive-url = https://web.archive.org/web/20200125192618/https://www.deseret.com/2019/5/31/20674560/people-are-freaking-out-over-the-cdc-s-photo-of-a-muffin-with-ticks-in-it | archive-date=25 January 2020 | work = Deseret News | location = Utah | vauthors = Scribner H | date = 31 May 2019 | quote = The U.S. CDC published a picture of a poppy seed muffin in which some of the "poppy seeds" were actually ticks }}</ref> The younger larval ticks are very rarely infected.<ref name=pmid15117014/> Although deer are the preferred hosts of adult deer ticks, and tick populations are much lower in the absence of deer, ticks generally do not acquire ''Borrelia'' from deer, instead they obtain them from infected small mammals such as the ], and occasionally birds.<ref name="Westport">{{cite web |title = Westport Weston Health District |url = http://www.wwhd.org/TLD_CD/deertick.htm |year = 2004 |access-date = 26 September 2013 |url-status=dead |archive-url = https://web.archive.org/web/20130929110519/http://www.wwhd.org/TLD_CD/deertick.htm |archive-date = 29 September 2013}}</ref> Areas where Lyme is common are expanding.<ref name=CDC-Lyme-Data/> | ||
| | title = Westport Weston Health District | |||
| | url =http://www.wwhd.org/TLD_CD/deertick.htm | |||
| | year = 2004 | |||
| | accessdate = 2013-09-26}}</ref> | |||
| Within the tick midgut, the ''Borrelia'''s outer surface protein A (OspA) binds to the tick receptor for OspA, known as TROSPA. When the tick feeds, the'' Borrelia'' downregulates OspA and upregulates OspC, another surface protein. |
Within the tick midgut, the ''Borrelia''{{'}}s ] A (OspA) binds to the tick receptor for OspA, known as TROSPA. When the tick feeds, the'' Borrelia'' ] OspA and ] OspC, another surface protein. After the bacteria migrate from the midgut to the salivary glands, OspC binds to Salp15, a tick salivary protein that appears to have immunosuppressive effects that enhance infection.<ref name=hovius_2007/> Successful infection of the mammalian host depends on bacterial expression of OspC.<ref name="pmid15085185"/> | ||
| Tick bites often go unnoticed because of the small size of the tick in its nymphal stage, as well as tick secretions that prevent the host from feeling any itch or pain from the bite. However, transmission is quite rare, with only about 1 |
Tick bites often go unnoticed because of the small size of the tick in its nymphal stage, as well as tick secretions that prevent the host from feeling any itch or pain from the bite. However, transmission is quite rare, with only about 1.2 to 1.4 percent of recognized tick bites resulting in Lyme disease.<ref>{{Cite web|url=https://www.uptodate.com/contents/what-to-do-after-a-tick-bite-to-prevent-lyme-disease-beyond-the-basics|title=Patient education: What to do after a tick bite to prevent Lyme disease (Beyond the Basics)| vauthors = Hu L |date=13 May 2019|website=www.uptodate.com|publisher=UpToDate|url-status=live|archive-url=https://web.archive.org/web/20200101124546/https://www.uptodate.com/contents/what-to-do-after-a-tick-bite-to-prevent-lyme-disease-beyond-the-basics|archive-date=1 January 2020|access-date=30 January 2020}}</ref> | ||
| While '']'' is most associated with ticks hosted by ] and ], '']'' is most frequently detected in rodent-feeding ] ticks, and '']'' and '']'' appear to be associated with birds. Both rodents and birds are competent reservoir hosts for ''B. burgdorferi sensu stricto''. The resistance of a genospecies of Lyme disease ] to the ] activities of the alternative complement pathway of various host species may determine its reservoir host association.<ref name="pmid16820453" /> | |||
| In Europe, the vector is '']'', which is also called the sheep tick or castor bean tick.<ref name=de_1997/> In China, '']'' (the taiga tick) is probably the most important vector.<ref name=Sun_2003/> In North America, the black-legged tick or deer tick ('']'') is the main vector on the east coast.<ref name=pmid15117014/> | |||
| Budding research has suggested that ''B. burgdorferi sensu lato'' may also be able to form ] cycle among lizard populations;<ref name="pmid17417956" /> this was previously assumed not to be possible in major areas containing populations of lizards, such as California. Except for one study in Europe,<ref name="pmid16820453"/> much of the data implicating lizards is based on DNA detection of the spirochete and has not demonstrated that lizards are able to infect ticks feeding upon them.<ref name="pmid17417956"/><ref name="pmid17626342"/><ref name="pmid17427701"/><ref name="pmid17326941"/> As some experiments suggest lizards are refractory to infection with ''Borrelia'', it appears likely their involvement in the enzootic cycle is more complex and species-specific.<ref name="pmid16995383"/> | |||
| The lone star tick ('']''), which is found throughout the ] as far west as ], is unlikely to transmit the Lyme disease ]s,<ref name=Ledin_2005/> though it may be implicated in a related syndrome called ], which resembles a mild form of Lyme disease.<ref name=Masters2008/> | |||
| ]'', developmental stages]] | |||
| On the ], the main vector is the western black-legged tick ('']'').<ref name="Clark"/> The tendency of this tick species to feed predominantly on host species such as lizards that are resistant to ''Borrelia'' infection appears to diminish transmission of Lyme disease in the West.<ref name="pmid15709249"/><ref name="pmid16995383"/> | |||
| In Europe, the main vector is '']'', which is also called the sheep tick or ] tick.<ref name=de_1997/> In China, '']'' (the taiga tick) is probably the most important vector.<ref name=Sun_2003/> In North America, the black-legged tick or deer tick ('']'') is the main vector on the East Coast.<ref name=pmid15117014/> | |||
| The lone star tick ('']''), which is found throughout the Southeastern United States as far west as ], is unlikely to transmit the Lyme disease ]s,<ref name=Ledin_2005/> though it may be implicated in a related syndrome called ], which resembles a mild form of Lyme disease.<ref name=Masters2008/> | |||
| Transmission across the ] during pregnancy has not been demonstrated, and no consistent pattern of teratogenicity or specific "congenital Lyme borreliosis" has been identified. As with a number of other spirochetal diseases, adverse pregnancy outcomes are possible with untreated infection; prompt treatment with antibiotics reduces or eliminates this risk.<ref name="Walsh2007" /><ref name="Lakos2010"/> | |||
| On the ], the main vector is the western black-legged tick ('']'').<ref name="Clark"/> The tendency of this tick species to feed predominantly on host species such as the ] that are resistant to ''Borrelia'' infection appears to diminish transmission of Lyme disease in the West.<ref name="pmid15709249"/><ref name="pmid16995383"/> | |||
| While Lyme spirochetes have been found in ]s as well as ticks,<ref name="Magnarelli"/> reports of actual infectious transmission appear to be rare.<ref name="Luger"/> Lyme spirochete DNA has been found in semen<ref name="Bach"/> and breast milk,<ref name="Schmidt"/> but transmission has not been known to take place through sexual contact.<ref name=Steere_2003/> | |||
| According to the CDC, live spirochetes have not been found in breast milk, urine, or semen.<ref name=CDC-FAQ/> However, more recent studies published in 2014, suggest there might be a link.<ref>{{cite journal | |||
| | author = Marianne Middelveen, Jennie Burke, Augustin Franco, Yean Wang, Peter Mayne, Eva Sapi, Cheryl Bandoski, Hilary Schlinger and Raphael Stricker | |||
| |date=January 2014 | |||
| | title = Lyme Disease May Be Sexually Transmitted | |||
| | journal = The Journal of Investigative Medicine | |||
| | volume = 62 | |||
| | issue = | |||
| | pages = 280–281 | |||
| | bibcode = | |||
| | doi = | |||
| | pmid = | |||
| | arxiv = | |||
| | id = | |||
| | url = http://www.prweb.com/releases/2014/01/prweb11506441.htm | |||
| | accessdate = January 26, 2014 | |||
| | language = | |||
| }}</ref> | |||
| Transmission can occur across the ] during pregnancy and as with a number of other spirochetal diseases, adverse pregnancy outcomes are possible with untreated infection; prompt treatment with antibiotics reduces or eliminates this risk.<ref name="Walsh2007" /><ref name="Dotters-Katz2013">{{cite journal | vauthors = Dotters-Katz SK, Kuller J, Heine RP | title = Arthropod-borne bacterial diseases in pregnancy | journal = Obstetrical & Gynecological Survey | volume = 68 | issue = 9 | pages = 635–649 | date = September 2013 | pmid = 25102120 | doi = 10.1097/OGX.0b013e3182a5ed46 | s2cid = 26801402 }}</ref><ref name="Lakos2010"/><ref name=NEJM1989AS>{{cite journal | vauthors = Steere AC | title = Lyme disease | journal = The New England Journal of Medicine | volume = 321 | issue = 9 | pages = 586–596 | date = August 1989 | pmid = 2668764 | doi = 10.1056/NEJM198908313210906 }}</ref> | |||
| ===Tick-borne coinfections=== | |||
| <!-- The CDC paper below backs up some of this but the language used doesn't really fit with the paper. --> | |||
| Ticks that transmit ''B. burgdorferi'' to humans can also carry and transmit several other parasites, such as '']'' and '']'', which cause the diseases ] and ] (HGA), respectively.<ref name=pmid17041141/> Among early Lyme disease patients, depending on their location, 2–12% will also have HGA and 2–40% will have babesiosis.<ref name="pmid16807416"/> Ticks in certain regions, including the lands along the eastern Baltic Sea, also transmit ].<ref name=Lindgren_2001/> | |||
| There is no scientific evidence to support Lyme disease transmission via blood transfusion, sexual contact, or breast milk.<ref name=CDC-FAQ/> | |||
| Coinfections complicate Lyme symptoms, especially diagnosis and treatment. It is possible for a tick to carry and transmit one of the coinfections and not ''Borrelia'', making diagnosis difficult and often elusive. The ] studied 100 ticks in rural ], and found 55% of the ticks were infected with at least one of the pathogens.<ref name="pmid9452402"/> | |||
| ===Tick-borne co-infections=== | |||
| ==Pathophysiology== | |||
| ''B. burgdorferi'' can spread throughout the body during the course of the disease, and has been found in the skin, heart, joints, peripheral nervous system, and central nervous system.<ref name="pmid15085185"/><ref name="pmid17509489"/> Many of the signs and symptoms of Lyme disease are a consequence of the immune response to the spirochete in those tissues.<ref name="pmid14987414" /> | |||
| {{Main|Tick-borne disease}} | |||
| ''B. burgdorferi'' is injected into the skin by the bite of an infected ''Ixodes'' tick. Tick saliva, which accompanies the spirochete into the skin during the feeding process, contains substances that disrupt the immune response at the site of the bite.<ref name="pmid16698304"/> This provides a protective environment where the spirochete can establish infection. The spirochetes multiply and migrate outward within the ]. The host inflammatory response to the bacteria in the skin causes the characteristic circular EM lesion.<ref name="pmid15085185" /> ], however, which are necessary to eliminate the spirochetes from the skin, fail to appear in the developing EM lesion. This allows the bacteria to survive and eventually spread throughout the body.<ref name="pmid17404293"/> | |||
| Ticks that transmit ''B. burgdorferi'' to humans can also carry and transmit several other microbes, such as '']'' and '']'', which cause the diseases ] and ] (HGA), respectively.<ref name=pmid17041141/> Among people with early Lyme disease, depending on their location, 2–12% will also have HGA and 2–10% will have babesiosis.<ref name="guidelines-2020">{{cite journal | vauthors = Lantos PM, Rumbaugh J, Bockenstedt LK, Falck-Ytter YT, Aguero-Rosenfeld ME, Auwaerter PG, Baldwin K, Bannuru RR, Belani KK, Bowie WR, Branda JA, Clifford DB, DiMario FJ, Halperin JJ, Krause PJ, Lavergne V, Liang MH, Meissner HC, Nigrovic LE, Nocton JJ, Osani MC, Pruitt AA, Rips J, Rosenfeld LE, Savoy ML, Sood SK, Steere AC, Strle F, Sundel R, Tsao J, Vaysbrot EE, Wormser GP, Zemel LS | title = Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease | journal = Clinical Infectious Diseases | volume = 72 | issue = 1 | pages = e1–e48 | date = January 2021 | pmid = 33417672 | doi = 10.1093/cid/ciaa1215 | doi-access = free }}</ref> Ticks in certain regions also transmit viruses that cause ] and ].<ref name=Lindgren_2001/><ref name="guidelines-2020"/> Co-infections of Lyme disease may not require additional treatment, since they may resolve on their own or—as in the case of HGA—can be treated with the doxycycline prescribed for Lyme.<ref name="idsa guideline"/> Persistent fever or compatible anomalous laboratory findings may be indicative of a co-infection.<ref name="guidelines-2020"/> | |||
| Days to weeks following the tick bite, the spirochetes spread via the bloodstream to joints, heart, nervous system, and distant skin sites, where their presence gives rise to the variety of symptoms of disseminated disease. The spread of ''B. burgdorferi'' is aided by the attachment of the host protease ] to the surface of the spirochete.<ref name="pmid9215633"/> | |||
| ==Pathophysiology== | |||
| If untreated, the bacteria may persist in the body for months or even years, despite the production of ''B. burgdorferi'' antibodies by the immune system.<ref name=pmid11450660/> The spirochetes may avoid the immune response by decreasing expression of surface proteins that are targeted by antibodies, ] of the VlsE surface protein, inactivating key immune components such as ], and hiding in the ], which may interfere with the function of immune factors.<ref name="pmid18097481"/><ref name="pmid17600717"/> | |||
| ''B. burgdorferi'' can spread throughout the body during the course of the disease, and has been found in the skin, heart, joints, peripheral nervous system, and central nervous system.<ref name="pmid15085185"/><ref name="pmid17509489"/> ''B. Burgdorferi'' does not produce toxins.<ref name="ALDF-toxins">{{cite web |title=Does Borrelia burgdorferi produce a neurotoxin ? |url=https://www.aldf.com/does-borrelia-burgdorferi-produce-a-neurotoxin-2/ |website=American Lyme Disease Foundation |access-date=30 July 2022}}</ref> Therefore, many of the signs and symptoms of Lyme disease are a consequence of the immune response to spirochete in those tissues.<ref name="pmid14987414" /> | |||
| ''B. burgdorferi'' is injected into the skin by the bite of an infected ''Ixodes'' tick.<ref name="Strand">{{cite journal |vauthors=Strnad M, Rudenko N, Rego RO |title=Pathogenicity and virulence of Borrelia burgdorferi |journal=Virulence |volume=14 |issue=1 |pages=2265015 |date=December 2023 |pmid=37814488 |pmc=10566445 |doi=10.1080/21505594.2023.2265015 |url=}}</ref> Tick saliva, which accompanies the spirochete into the skin during the feeding process, contains substances that disrupt the immune response at the site of the bite.<ref name="pmid16698304"/> This provides a protective environment where the spirochete can establish infection. The spirochetes multiply and migrate outward within the ]. The host inflammatory response to the bacteria in the skin causes the characteristic circular EM lesion.<ref name="pmid15085185"/> ], however, which are necessary to eliminate the spirochetes from the skin, fail to appear in necessary numbers in the developing EM lesion because tick saliva inhibits neutrophil function. This allows the bacteria to survive and eventually spread throughout the body.<ref name="pmid17404293"/> | |||
| In the brain, ''B. burgdorferi'' may induce ] to undergo astrogliosis (proliferation followed by ]), which may contribute to neurodysfunction.<ref name="pmid12938230"/> The spirochetes may also induce host cells to secrete products toxic to nerve cells, including ] and the ] IL-6 and TNF-alpha, which can produce ] and ].<ref name="pmid1531156"/><ref name="LTBDRC"/><ref name=Papanicolaou_1998/> Both ] and astrocytes secrete IL-6 and TNF-alpha in the presence of the spirochete.<ref name="pmid12938230"/><ref name=Rasley_2002/> This cytokine response may contribute to cognitive impairment.<ref name=Wright_2006/> | |||
| Days to weeks following the tick bite, the spirochetes spread via the bloodstream to joints, heart, nervous system, and distant skin sites, where their presence gives rise to the variety of symptoms of the disseminated disease. The spread of ''B. burgdorferi'' is aided by the attachment of the host protease ] to the surface of the spirochete.<ref name="pmid9215633"/> | |||
| In Lyme ], diffuse white matter pathology can disrupt ] connections, and could account for deficits in attention, memory, visuospatial ability, complex cognition, and emotional status. White matter disease may have a greater potential for recovery than gray matter disease, perhaps because neuronal loss is less common. Resolution of MRI white matter hyperintensities after antibiotic treatment has been observed.<ref name=Fallon_2003/> | |||
| If untreated, the bacteria may persist in the body for months or even years, despite the production of ''B. burgdorferi'' antibodies by the immune system.<ref name=pmid11450660/> The spirochetes may avoid the immune response by decreasing expression of surface proteins that are targeted by antibodies, ] of the VlsE surface protein, inactivating key immune components such as ], and hiding in the ], which may interfere with the function of immune factors.<ref name="pmid18097481"/><ref name="pmid17600717"/> | |||
| A developing hypothesis is that the chronic secretion of ] ]s as a result of ''Borrelia'' infection may reduce the effect of ]s, or other ] in the brain by cell-mediated proinflammatory pathways, thereby leading to the dysregulation of neurohormones, specifically ] and ], the major stress hormones.<ref name=Elenkov_2005/><ref name=Calcagni_2006/> | |||
| This process is mediated by the ]. Additionally, ], a precursor to ], appears to be reduced within the ] in a number of infectious diseases that affect the brain, including Lyme.<ref name=Gasse_1994/> Researchers are investigating if this neurohormone secretion is the cause of ] disorders developing in some patients with borreliosis.<ref name=Zajkowska_2006/> | |||
| ===Immunological studies=== | ===Immunological studies=== | ||
| Line 131: | Line 144: | ||
| Chronic symptoms from an autoimmune reaction could explain why some symptoms persist even after the spirochetes have been eliminated from the body. This hypothesis may explain why chronic arthritis persists after antibiotic therapy, similar to ], but its wider application is controversial.<ref name=Weinstein_2002/><ref name=Bolz_2004/> | Chronic symptoms from an autoimmune reaction could explain why some symptoms persist even after the spirochetes have been eliminated from the body. This hypothesis may explain why chronic arthritis persists after antibiotic therapy, similar to ], but its wider application is controversial.<ref name=Weinstein_2002/><ref name=Bolz_2004/> | ||
| ===Persistence=== | |||
| The National Institute of Health has supported research into bacterial resistance which has demonstrated persistence after antibiotic therapy in several animal models, including mice and primates. However, it was not possible to culture these bacteria and it is not known if they are infectious, or if they contribute to symptom persistence post-treatment.<ref>{{cite web|title=Chronic Lyme Disease|url=http://www.niaid.nih.gov/topics/lymedisease/understanding/pages/chronic.aspx|publisher=National Institute of Allergy and Infectious Diseases|accessdate=15 October 2013}}</ref> | |||
| An ''in vitro'' study of isolated B. burgdorferi persisters published in July 2014 showed that front-line antibiotics ] and ] are ineffective in eradicating persister populations, which may contribute to symptoms post-treatment. The study went on to show that 27 other drug candidates have a higher potential for eradicating these persister populations, and that those drugs may have implications in the development of treatment plans for patients suffering long-term symptoms of Lyme Disease.<ref>{{cite web|last1=Feng|first1=Jie|last2=Wang|first2=Ting|last3=Shi|first3=Wangliang|last4=Zhang|first4=Shuo|last5=Sullivan|first5=David|last6=Auwaerter|first6=Paul|last7=Zhang|first7=Ying|title=Identification of novel activity against Borrelia burgdorferi persisters using an FDA approved drug library|url=http://www.nature.com/emi/journal/v3/n7/full/emi201453a.html#bib24|website=Nature|publisher=Emerging Microbes & Infections|accessdate=11 July 2014}}</ref> | |||
| ==Diagnosis== | ==Diagnosis== | ||
| Lyme disease is ] based on symptoms, objective physical findings (such as ] (EM) rash, ], or ]), history of possible exposure to infected ], and possibly ].<ref name=NEJM2014/><ref name=wright_2012/> People with symptoms of early Lyme disease should have a total body skin examination for EM rashes and asked whether EM-type rashes had manifested within the last 1–2 months.<ref name="idsa guideline"/> Presence of an EM rash and recent tick exposure (i.e., being outdoors in a likely tick habitat where Lyme is ], within 30 days of the appearance of the rash) are sufficient for Lyme diagnosis; no laboratory confirmation is needed or recommended.<ref name=NEJM2014/><ref name=wright_2012/><ref name="Brown"/><ref name="Hofmann"/> Most people who get infected do not remember a tick or a bite, and the EM rash need not look like a bull's eye (most EM rashes in the U.S. do not) or be accompanied by any other symptoms.<ref name=NEJM2014/><ref name="Wormser"/> In the U.S., Lyme is most common in the ] and ] states and parts of ] and ], but it is expanding into other areas.<ref name=CDC-Lyme-Data>{{cite web |title=Lyme Disease Data and surveillance |url=https://www.cdc.gov/lyme/datasurveillance/ |website=Lyme Disease |publisher=Centers for Disease Control and Prevention |access-date=12 April 2019 |date=5 February 2019 |archive-url=https://web.archive.org/web/20190413133319/https://www.cdc.gov/lyme/datasurveillance/ |archive-date=13 April 2019 |url-status=live }}</ref> Several bordering areas of Canada also have high Lyme risk.<ref name=canada_lyme_map>{{cite web | title = Lyme Disease risk areas map | url = https://www.canada.ca/en/public-health/services/diseases/lyme-disease/risk-lyme-disease.html#map | website = Risk of Lyme disease to Canadians | publisher = Government of Canada | access-date = 8 May 2019 | date = 27 January 2015 | archive-url = https://web.archive.org/web/20190510195225/https://www.canada.ca/en/public-health/services/diseases/lyme-disease/risk-lyme-disease.html#map | archive-date = 10 May 2019 | url-status = live }}</ref> | |||
| Lyme disease is ] clinically based on symptoms, objective physical findings (such as ], facial palsy, or arthritis) or a history of possible exposure to infected ticks, as well as ]. The EM rash is not always a bull's eye, i.e., it can be solid red. When making a diagnosis of Lyme disease, health care providers should consider other diseases that may cause similar illness. Not all patients infected with Lyme disease develop the characteristic bull's-eye rash, and many may not recall a tick bite.<ref name="Wormser"/> | |||
| In the absence of an EM rash or history of tick exposure, Lyme diagnosis depends on laboratory confirmation.<ref name=Sherris /><ref name=aucott_2008>{{cite journal | vauthors = Aucott J, Morrison C, Munoz B, Rowe PC, Schwarzwalder A, West SK | title = Diagnostic challenges of early Lyme disease: lessons from a community case series | journal = BMC Infectious Diseases | volume = 9 | issue = 79 | pages = 79 | date = June 2009 | pmid = 19486523 | pmc = 2698836 | doi = 10.1186/1471-2334-9-79 | doi-access = free }}</ref> The bacteria that cause Lyme disease are difficult to observe directly in body tissues and also difficult and too time-consuming to ] in the laboratory.<ref name=NEJM2014/><ref name="Sherris" /> The most widely used tests look instead for presence of ] against those bacteria in the blood.<ref name="cdc-diagnosis"/> A positive antibody test result does not by itself prove active infection but can confirm an infection that is suspected because of symptoms, objective findings, and history of tick exposure in a person.<ref name=Sherris /> Because as many as 5–20% of the normal population have antibodies against Lyme, people without history and symptoms suggestive of Lyme disease should not be tested for Lyme antibodies: a positive result would likely be false, possibly causing unnecessary treatment.<ref name="idsa guideline"/><ref name=efns_guidelines/> | |||
| Because of the difficulty in ] ''Borrelia'' bacteria in the laboratory, diagnosis of Lyme disease is typically based on the clinical exam findings and a history of exposure to ] Lyme areas.<ref name="Sherris" /> The EM rash, which does not occur in all cases, is considered sufficient to establish a diagnosis of Lyme disease even when serologic blood tests are negative.<ref name="Brown"/><ref name="Hofmann"/> Serological testing can be used to support a clinically suspected case, but is not diagnostic by itself.<ref name=Sherris /> | |||
| In some cases, when history, signs, and symptoms are strongly suggestive of early disseminated Lyme disease, ] may be started and reevaluated as laboratory test results become available.<ref name=garro_2018/><ref name=lyme_guidelines_uk>{{cite web | title = Lyme disease | url = https://www.nice.org.uk/guidance/ng95/chapter/recommendations | website = NICE guideline | date = 11 April 2018 | publisher = National Institute for Health and Care Excellence | access-date = 24 May 2019 | archive-url = https://web.archive.org/web/20190511145123/https://www.nice.org.uk/guidance/ng95/chapter/Recommendations | archive-date = 11 May 2019 | url-status = live }}</ref> | |||
| Diagnosis of late-stage Lyme disease is often complicated by a multifaceted appearance and nonspecific symptoms, prompting one reviewer to call Lyme the new "great imitator".<ref name=Pachner_1989/> Lyme disease may be misdiagnosed as ], ], ], ], ], ], ], or other ] and ] diseases. As all patients with later stage infection will have a positive antibody test, simple blood tests can exclude Lyme disease as a possible cause of the patients symptoms.<ref name="Branda 541–7">{{cite journal|last=Branda|first=JA|author2=Linskey, K |author3=Kim, YA |author4=Steere, AC |author5= Ferraro, MJ |title=Two-tiered antibody testing for Lyme disease with use of 2 enzyme immunoassays, a whole-cell sonicate enzyme immunoassay followed by a VlsE C6 peptide enzyme immunoassay.|journal=Clinical infectious diseases : an official publication of the Infectious Diseases Society of America|date=Sep 2011|volume=53|issue=6|pages=541–7|pmid=21865190|doi=10.1093/cid/cir464}}</ref> | |||
| ===Laboratory testing=== | ===Laboratory testing=== | ||
| Tests for antibodies in the blood by ] and ] is the most widely used method for Lyme diagnosis. A two-tiered protocol is recommended by the ] (CDC): the ] ELISA test is performed first, and if it is positive or equivocal, then the more ] Western blot is run.<ref name=Wilske_2005/> The ] takes some time to produce antibodies in quantity. After Lyme infection onset, antibodies of types ] and ] usually can first be detected respectively at 2–4 weeks and 4–6 weeks, and peak at 6–8 weeks.<ref name=Depietropaolo-2005>{{cite journal | vauthors = DePietropaolo DL, Powers JH, Gill JM, Foy AJ | title = Diagnosis of lyme disease | journal = American Family Physician | volume = 72 | issue = 2 | pages = 297–304 | date = July 2005 | pmid = 16050454 | doi = 10.1093/cid/cir464 | doi-access = free }}</ref> When an EM rash first appears, detectable antibodies may not be present. Therefore, it is recommended that testing not be performed and diagnosis be based on the presence of the EM rash.<ref name="idsa guideline"/> Up to 30 days after suspected Lyme infection onset, infection can be confirmed by detection of IgM or IgG antibodies; after that, it is recommended that only IgG antibodies be considered.<ref name=Depietropaolo-2005/> A positive IgM and negative IgG test result after the first month of infection is generally indicative of a false-positive result.<ref name="ALDF-serologic-tests">{{cite web |title=Are serological tests of any value in the diagnosis of Lyme disease? |url=https://www.aldf.com/are-serological-tests-of-any-value-in-the-diagnosis-of-lyme-disease-2/ |website=American Lyme Disease Foundation |access-date=2 December 2019 |ref=ALDF-serologic-tests |archive-url=https://web.archive.org/web/20191219210825/https://www.aldf.com/are-serological-tests-of-any-value-in-the-diagnosis-of-lyme-disease-2/ |archive-date=19 December 2019 |url-status=live }}</ref> The number of IgM antibodies usually collapses 4–6 months after infection, while IgG antibodies can remain detectable for years.<ref name=Depietropaolo-2005/> | |||
| Several forms of laboratory testing for Lyme disease are available, some of which have not been adequately validated. The most widely used tests are ], which measure levels of specific antibodies in a patient's blood. These tests may be negative in early infection, as the body may not have produced a significant quantity of antibodies, but they are considered a reliable aid in the diagnosis of later stages of Lyme disease.<ref name="cdc-diagnosis"/> Serologic tests for Lyme disease are of limited use in people lacking objective signs of Lyme disease because of false positive results and cost.<ref name="idsa guideline"/> | |||
| Other tests may be used in neuroborreliosis cases. In Europe, neuroborreliosis is usually caused by ] and almost always involves ], i.e. the densities of ] (infection-fighting cells) and protein in the ] (CSF) typically rise to characteristically abnormal levels, while glucose level remains normal.<ref name=steere_neuro_findings/><ref name="idsa guideline"/><ref name=ogrinc_bannwarth/> Additionally, the immune system produces antibodies against Lyme inside the intrathecal space, which contains the CSF.<ref name="idsa guideline"/><ref name=ogrinc_bannwarth/> Demonstration by ] and CSF analysis of pleocytosis and intrathecal antibody production are required for definite diagnosis of neuroborreliosis in Europe (except in cases of peripheral neuropathy associated with ], which usually is caused by ] and confirmed by blood antibody tests).<ref name=efns_guidelines/> In North America, neuroborreliosis is caused by ] and may not be accompanied by the same CSF signs; they confirm a diagnosis of central nervous system (CNS) neuroborreliosis if positive, but do not exclude it if negative.<ref name=Coyle_1995/> American guidelines consider CSF analysis optional when symptoms appear to be confined to the peripheral nervous system (PNS), e.g. facial palsy without overt meningitis symptoms.<ref name="idsa guideline"/><ref name="pmid17522387"/> Unlike blood and intrathecal antibody tests, CSF pleocytosis tests revert to normal after infection ends and therefore can be used as objective markers of treatment success and inform decisions on whether to retreat.<ref name=ogrinc_bannwarth/> In infection involving the PNS, ] and ] can be used to monitor objectively the response to treatment.<ref name=steere_neuro_findings/> | |||
| The serological laboratory tests most widely available and employed are the ] and ]. A two-tiered protocol is recommended by the Centers for Disease Control and Prevention: the ] ELISA test is performed first, and if it is positive or equivocal, then the more ] Western blot is run.<ref name=Wilske_2005/> The reliability of testing in diagnosis remains controversial.<ref name=Sherris /> Studies show the Western blot ] has a specificity of 94–96% for patients with clinical symptoms of early Lyme disease.<ref name="Engstrom"/><ref name="Sivak"/> The initial ELISA test has a sensitivity of about 70%, and in two-tiered testing, the overall sensitivity is only 64%, although this rises to 100% in the subset of people with disseminated symptoms, such as arthritis.<ref name="Steere"/> | |||
| In Lyme carditis, ] are used to evidence heart conduction abnormalities, while ] may show ] dysfunction.<ref name=fish_2008/> ] and confirmation of Borrelia cells in myocardial tissue may be used in specific cases but are usually not done because of risk of the procedure.<ref name=fish_2008/> | |||
| Erroneous test results have been widely reported in both early and late stages of the disease, and can be caused by several factors, including antibody cross-reactions from other infections, including ] and ],<ref name="Gossens"/> as well as ].<ref name="Strasfeld"/> The overall rate of false positives is low, only about 1 to 3%, in comparison to a false negative rate of up to 36% in the early stages of infection using two-tiered testing.<ref name="Steere"/> | |||
| ] (PCR) tests for Lyme disease have also been developed to detect the genetic material (]) of the Lyme disease spirochete. PCR tests are susceptible to ] results |
] (PCR) tests for Lyme disease have also been developed to detect the genetic material (]) of the Lyme disease spirochete. Culture or PCR are the current means for detecting the presence of the organism, as ] studies only test for ] of ''Borrelia''. PCR has the advantage of being much faster than culture. However, PCR tests are susceptible to ] results, e.g. by detection of debris of dead Borrelia cells or specimen contamination.<ref name="pmid11438915"/><ref name=efns_guidelines/> Even when properly performed, PCR often shows false-negative results because few Borrelia cells can be found in blood and ] (CSF) during infection.<ref name="pmid16020686"/><ref name=efns_guidelines/> Hence, PCR tests are recommended only in special cases, e.g. diagnosis of Lyme arthritis, because it is a highly sensitive way of detecting ''ospA'' DNA in synovial fluid.<ref name="pmid8272083"/> Although sensitivity of PCR in CSF is low, its use may be considered when intrathecal antibody production test results are suspected of being falsely negative, e.g. in very early (< 6 weeks) neuroborreliosis or in ] people.<ref name=efns_guidelines/> | ||
| Several other forms of laboratory testing for Lyme disease are available, some of which have not been adequately validated. ], shed by live ''Borrelia'' bacteria into urine, are a promising technique being studied.<ref>{{cite journal | vauthors = Hyde FW, Johnson RC, White TJ, Shelburne CE | title = Detection of antigens in urine of mice and humans infected with Borrelia burgdorferi, etiologic agent of Lyme disease | journal = Journal of Clinical Microbiology | volume = 27 | issue = 1 | pages = 58–61 | date = January 1989 | pmid = 2913036 | pmc = 267232 | doi = 10.1128/JCM.27.1.58-61.1989 }}</ref> The use of nanotrap particles for their detection is being looked at and the OspA has been linked to active symptoms of Lyme.<ref>{{cite journal | vauthors = Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, Liotta L, Narayanan A, Lepene B, Kehn-Hall K | title = The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics | journal = Pathogens and Disease | volume = 71 | issue = 2 | pages = 164–176 | date = July 2014 | pmid = 24449537 | pmc = 7108521 | doi = 10.1111/2049-632X.12136 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, Liotta L, Narayanan A, Lepene B, Kehn-Hall K | title = The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics | journal = Pathogens and Disease | volume = 71 | issue = 2 | pages = 164–176 | date = July 2014 | pmid = 24449537 | pmc = 7108521 | doi = 10.1111/2049-632x.12136 | doi-access = free }}</ref> High ]s of either immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies to ''Borrelia'' antigens indicate disease, but lower titers can be misleading, because the IgM antibodies may remain after the initial infection, and IgG antibodies may remain for years.<ref name=Burdash_1991/> | |||
| With the exception of culture or PCR, no practical means for detecting the presence of the organism is currently available, as serologic studies only test for ] of ''Borrelia''. High ]s of either immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies to ''Borrelia'' antigens indicate disease, but lower titers can be misleading, because the IgM antibodies may remain after the initial infection, and IgG antibodies may remain for years.<ref name=Burdash_1991/> | |||
| The CDC does not recommend urine antigen tests, PCR tests on urine, immunofluorescent staining for cell-wall-deficient forms of ''B. burgdorferi'', and lymphocyte transformation tests.<ref name="pmid16020686"/> | |||
| Western blot, ELISA, and PCR can be performed by either blood test via ] or cerebrospinal fluid (CSF) via ]. Though lumbar puncture is more definitive of diagnosis, antigen capture in the CSF is much more elusive; reportedly, CSF yields positive results in only 10–30% of patients cultured. The diagnosis of neurologic infection by ''Borrelia'' should not be excluded solely on the basis of normal routine CSF or negative CSF antibody analyses.<ref name=Coyle_1995/> | |||
| ===Imaging=== | |||
| New techniques for clinical testing of ''Borrelia'' infection have been developed, such as LTT-],<ref name=Valentine_2007/> although the results of studies are contradictory, The first peer reviewed study assessing the diagnostic sensitivity and specificity of the test has been presented in 2012, showing potential for LTT to become a supportive diagnostic tool.<ref name=pmid23091571/> Others, such as focus floating microscopy, are under investigation.<ref name=Eisendle_2007/> New research indicates ] ] may also be a possible marker for neuroborreliosis.<ref name=Cadavid_2006/> | |||
| ] is controversial in whether it provides specific patterns unique to ], but may aid in ] and in understanding the pathophysiology of the disease.<ref name="Hildenbrand2009"/> Though controversial, some evidence shows certain neuroimaging tests can provide data that are helpful in the diagnosis of a person. ] (MRI) and ] (SPECT) are two of the tests that can identify abnormalities in the brain of a person affected with this disease. Neuroimaging findings in an MRI include lesions in the periventricular white matter, as well as enlarged ventricles and cortical atrophy. The findings are considered somewhat unexceptional because the lesions have been found to be reversible following antibiotic treatment. Images produced using SPECT show numerous areas where an insufficient amount of blood is being delivered to the cortex and subcortical white matter. However, SPECT images are known to be nonspecific because they show a heterogeneous pattern in the imaging. The abnormalities seen in the SPECT images are very similar to those seen in people with cerebral vasculitis and ], which makes them questionable.<ref>{{cite journal | vauthors = Westervelt HJ, McCaffrey RJ | title = Neuropsychological functioning in chronic Lyme disease | journal = Neuropsychology Review | volume = 12 | issue = 3 | pages = 153–177 | date = September 2002 | pmid = 12428915 | doi = 10.1023/A:1020381913563 | s2cid = 2807397 }}</ref> | |||
| ===Differential diagnosis=== | |||
| Some laboratories offer Lyme disease testing using assays whose accuracy and clinical usefulness have not been adequately established. These tests include urine antigen tests, PCR tests on urine, immunofluorescent staining for cell wall-deficient forms of ''B. burgdorferi'', and lymphocyte transformation tests. The CDC does not recommend these tests, and a stated their use is "of great concern and is strongly discouraged".<ref name="pmid16020686"/> | |||
| Community clinics have been reported to misdiagnose 23–28% of ] (EM) rashes and 83% of other objective manifestations of early Lyme disease.<ref name=aucott_2008/> EM rashes are often misdiagnosed as ], ], or ].<ref name=aucott_2008/> Many misdiagnoses are credited to the widespread misconception that EM rashes should look like a bull's eye.<ref name=NEJM2014/> Actually, the key distinguishing features of the EM rash are the speed and extent to which it expands, respectively up to 2–3 cm/day and a diameter of at least 5 cm, and in 50% of cases more than 16 cm. The rash expands away from its center, which may or may not look different or be separated by ring-like clearing from the rest of the rash.<ref name=wright_2012/><ref name=tibbles_2007/> Compared to EM rashes, ] are more common in the limbs, tend to be more painful and itchy or become swollen, and some may cause ] (sinking dark blue patch of dead skin).<ref name=wright_2012/><ref name=NEJM2014/> ] most commonly develops around a wound or ulcer, is rarely circular, and is more likely to become swollen and tender.<ref name=wright_2012/><ref name=NEJM2014/> EM rashes often appear at sites that are unusual for cellulitis, such as the armpit, groin, abdomen, or back of knee.<ref name=wright_2012/> Like Lyme, ] often begins with headache, fever, and fatigue, which are followed by pain or numbness. However, unlike Lyme, in shingles these symptoms are usually followed by appearance of rashes composed of multiple small blisters along with a nerve's ], and shingles can also be confirmed by quick laboratory tests.<ref name=Dwo2007>{{cite journal | vauthors = Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, Betts RF, Gershon AA, Haanpaa ML, McKendrick MW, Nurmikko TJ, Oaklander AL, Oxman MN, Pavan-Langston D, Petersen KL, Rowbotham MC, Schmader KE, Stacey BR, Tyring SK, van Wijck AJ, Wallace MS, Wassilew SW, Whitley RJ | title = Recommendations for the management of herpes zoster | journal = Clinical Infectious Diseases | volume = 44 | issue = Suppl 1 | pages = S1-26 | date = January 2007 | pmid = 17143845 | doi = 10.1086/510206 | s2cid = 10894629 | doi-access = free }}</ref> | |||
| ] caused by Lyme disease (LDFP) is often misdiagnosed as ].<ref name=garro_2018/> Although Bell's palsy is the most common type of one-sided facial palsy (about 70% of cases), LDFP can account for about 25% of cases of facial palsy in areas where Lyme disease is common.<ref name=garro_2018/> Compared to LDFP, Bell's palsy much less frequently affects both sides of the face.<ref name=garro_2018/> Even though LDFP and Bell's palsy have similar symptoms and evolve similarly if untreated, corticosteroid treatment is beneficial for Bell's Palsy, while being detrimental for LDFP.<ref name=garro_2018/> Recent history of exposure to a likely tick habitat during warmer months, EM rash, viral-like symptoms such as headache and fever, and/or palsy in both sides of the face should be evaluated for the likelihood of LDFP; if it is more than minimal, ] with antibiotics should be initiated, without corticosteroids, and reevaluated upon completion of laboratory tests for Lyme disease.<ref name=garro_2018/> | |||
| In addition to laboratory testing on patients, ticks can be tested after removal from the host. Several laboratories perform PCR testing on live or dead ticks for a panel of tick-borne diseases, including ''Borrelia'', '']'', and '']''.<ref name=ilads/> | |||
| Unlike ], Lyme lymphocytic meningitis tends to not cause fever, last longer, and recur.<ref name=steere_neuro_findings/><ref name="idsa guideline"/> Lymphocytic meningitis is also characterized by possibly co-occurring with ], ], or ] and having much lower percentage of polymorphonuclear leukocytes in ].<ref name="idsa guideline"/> | |||
| ===Imaging=== | |||
| ] is controversial in whether it provides specific patterns unique to ], but may aid in ] and in understanding the pathophysiology of the disease.<ref name="Hildenbrand2009"/> Though controversial, some evidence shows certain neuroimaging tests can provide data that are helpful in the diagnosis of a patient. ] (MRI), as well as ] (SPECT) are two of the tests that can identify abnormalities in the brain of a patient affected with this disease. Neuroimaging findings in an MRI include lesions in the periventricular white matter, as well as enlarged ventricles and cortical atrophy. The findings are considered somewhat unexceptional because the lesions have been found to be reversible following antibiotic treatment. Images produced using SPECT show numerous areas where an insufficient amount of blood is being delivered the cortex and subcortical white matter. However, SPECT images are known to be not specific because they show a heterogeneous pattern in the imaging. The abnormalities seen in the SPECT images are very similar to those seen in patients with cerebral vacuities and Creutzfeldt-Jakob disease, which makes them questionable.<ref>{{cite journal|last=Westervelt|first=Holly|author2=McCaffrey, Robert |title=Neuropsychological Functioning in Chronic Lyme Disease|journal=Neuropsychological Review|date=September 2002|volume=12|issue=3|pages=153–177|doi=10.1023/A:1020381913563|accessdate=10 October 2013}}</ref> | |||
| Lyme radiculopathy affecting the limbs is often misdiagnosed as a ] caused by nerve root compression, such as ].<ref name=aucott_2008/><ref name=halperin_chronic>{{cite journal | vauthors = Halperin JJ | title = Chronic Lyme disease: misconceptions and challenges for patient management | journal = Infection and Drug Resistance | volume = 8 | pages = 119–128 | date = May 2015 | pmid = 26028977 | pmc = 4440423 | doi = 10.2147/IDR.S66739 | doi-access = free }}</ref> Although most cases of radiculopathy are compressive and resolve with conservative treatment (e.g., rest) within 4–6 weeks, guidelines for managing radiculopathy recommend first evaluating risks of other possible causes that, although less frequent, require immediate diagnosis and treatment, including infections such as Lyme and shingles.<ref name=tarulli_radiculopathy>{{cite journal | vauthors = Tarulli AW, Raynor EM | title = Lumbosacral radiculopathy | journal = Neurologic Clinics | volume = 25 | issue = 2 | pages = 387–405 | date = May 2007 | pmid = 17445735 | doi = 10.1016/j.ncl.2007.01.008 | url = http://pdfs.semanticscholar.org/27a9/f13596f9bc2fdb873eb83302d14aaa176381.pdf | url-status = dead | s2cid = 15518713 | archive-url = https://web.archive.org/web/20190220113056/http://pdfs.semanticscholar.org/27a9/f13596f9bc2fdb873eb83302d14aaa176381.pdf | archive-date = 2019-02-20 }}</ref> A history of outdoor activities in likely tick habitats in the last 3 months possibly followed by a rash or viral-like symptoms, and current headache, other symptoms of lymphocytic meningitis, or facial palsy would lead to suspicion of Lyme disease and recommendation of ] and ] tests for confirmation.<ref name=tarulli_radiculopathy/> | |||
| Lyme radiculopathy affecting the trunk can be misdiagnosed as myriad other conditions, such as ] and ].<ref name=halperin_2010/><ref name=aucott_2008/> Diagnosis of late-stage Lyme disease is often complicated by a multifaceted appearance and nonspecific symptoms, prompting one reviewer to call Lyme the new "great imitator".<ref name=Pachner_1989/> As all people with later-stage infection will have a positive antibody test, simple blood tests can exclude Lyme disease as a possible cause of a person's symptoms.<ref name="Branda 541–7">{{cite journal | vauthors = Branda JA, Linskey K, Kim YA, Steere AC, Ferraro MJ | title = Two-tiered antibody testing for Lyme disease with use of 2 enzyme immunoassays, a whole-cell sonicate enzyme immunoassay followed by a VlsE C6 peptide enzyme immunoassay | journal = Clinical Infectious Diseases | volume = 53 | issue = 6 | pages = 541–547 | date = September 2011 | pmid = 21865190 | doi = 10.1093/cid/cir464 | doi-access = free }}</ref> | |||
| ==Prevention== | ==Prevention== | ||
| Tick bites may be prevented by avoiding or reducing time in likely tick habitats and taking precautions while in and when getting out of one.<ref name=CDC_Lyme_prev_on_people>{{cite web | title=Preventing tick bites on people | url=https://www.cdc.gov/lyme/prev/on_people.html | website=Lyme Disease | publisher=Centers for Disease Control and Prevention | access-date=21 May 2019 | date=8 March 2019 | archive-url=https://web.archive.org/web/20190615054936/https://www.cdc.gov/lyme/prev/on_people.html | archive-date=15 June 2019 | url-status=live }}</ref><ref name="NYT-20210611" /> | |||
| Protective clothing includes a hat, long-sleeved shirt, and long trousers tucked into socks or boots. Light-colored clothing makes the tick more easily visible before it attaches itself. People should use special care in handling and allowing outdoor pets inside homes because they can bring ticks into the house. | |||
| Most Lyme human infections are caused by ] nymph bites between April and September.<ref name=wright_2012/><ref name=CDC_Lyme_prev_on_people/> Ticks prefer moist, shaded locations in ]s, shrubs, tall grasses and ] or wood piles.<ref name=wright_2012/><ref name=CVBD_tick_preventative>{{cite web | title=About ticks – preventative measures | url=https://www.cvbd.org/en/tick-borne-diseases/about-ticks/preventative-measures/ | website=Tick-borne diseases | publisher=Companion Vector-Borne Diseases | access-date=21 May 2019 | archive-url=https://web.archive.org/web/20190607052340/http://www.cvbd.org/en/tick-borne-diseases/about-ticks/preventative-measures/ | archive-date=7 June 2019 | url-status=live }}</ref> Tick densities tend to be highest in woodlands, followed by unmaintained ] (about half as high), ornamental plants and perennial ] (about a quarter), and lawns (about 30 times less).<ref name=eisen_2016>{{cite journal | vauthors = Eisen L, Eisen RJ | title = Critical Evaluation of the Linkage Between Tick-Based Risk Measures and the Occurrence of Lyme Disease Cases | journal = Journal of Medical Entomology | volume = 53 | issue = 5 | pages = 1050–1062 | date = September 2016 | pmid = 27330093 | pmc = 5777907 | doi = 10.1093/jme/tjw092 }}</ref> Ixodes ]e and nymphs tend to be abundant also where mice nest, such as ] and wood logs.<ref name=eisen_2016/> Ixodes larvae and nymphs typically wait for potential ] ("quest") on leaves or grasses close to the ground with forelegs outstretched; when a host brushes against its limbs, the tick rapidly clings and climbs on the host looking for a skin location to bite.<ref name=CVBDhost>{{cite web |url=http://www.cvbd.org/en/tick-borne-diseases/about-ticks/tick-feeding/host-seeking/ |title=Host seeking |work=CVBD: Companion Vector-Borne Diseases |access-date=8 December 2016 |archive-url=https://web.archive.org/web/20161016105430/http://www.cvbd.org/en/tick-borne-diseases/about-ticks/tick-feeding/host-seeking/ |archive-date=16 October 2016 |url-status=live }}</ref> In Northeastern United States, 69% of tick bites are estimated to happen in residences, 11% in schools or camps, 9% in parks or recreational areas, 4% at work, 3% while hunting, and 4% in other areas.<ref name=eisen_2016/> Activities associated with tick bites around residences include yard work, brush clearing, gardening, playing in the yard, and letting dogs or cats that roam outside in woody or grassy areas into the house.<ref name=eisen_2016/><ref name=CDC_Lyme_prev_on_people/> In parks, tick bites often happen while hiking or camping.<ref name=eisen_2016/> Walking on a mown lawn or center of a trail without touching adjacent vegetation is less risky than crawling or sitting on a log or stone wall.<ref name=eisen_2016/><ref name=EPA_tick_prevention/> Pets should not be allowed to roam freely in likely tick habitats.<ref name=CVBD_tick_preventative/> | |||
| ] sprayed on clothing kills ticks on contact, and is sold for this purpose. Insect repellents with Picaridin, IR3535, DEET, or oil of lemon eucalyptus repel ticks, as well.<ref>list of chemical repellents http://www.ewg.org/research/ewgs-guide-bug-repellents/adults#block1</ref> | |||
| As a precaution, ] recommends soaking or spraying clothes, shoes, and camping gear such as tents, backpacks and sleeping bags with 0.5% ] solution and hanging them to dry before use.<ref name=CDC_Lyme_prev_on_people/><ref name=CDC_travelers_protection>{{cite web | title=Protection against Mosquitoes, Ticks, & Other Arthropods | url=https://wwwnc.cdc.gov/travel/yellowbook/2018/the-pre-travel-consultation/protection-against-mosquitoes-ticks-other-arthropods | website=Travelers' Health | publisher=Centers for Disease Control and Prevention | access-date=21 May 2019 | archive-url=https://web.archive.org/web/20190509191123/https://wwwnc.cdc.gov/travel/yellowbook/2018/the-pre-travel-consultation/protection-against-mosquitoes-ticks-other-arthropods | archive-date=9 May 2019 | url-status=live }}</ref> Permethrin is odorless and safe for humans but highly toxic to ticks.<ref name=miller_2011/> After crawling on permethrin-treated fabric for as few as 10–20 seconds, tick nymphs become irritated and fall off or die.<ref name=miller_2011/><ref name=eisen_2017>{{cite journal | vauthors = Eisen L, Rose D, Prose R, Breuner NE, Dolan MC, Thompson K, Connally N | title = Bioassays to evaluate non-contact spatial repellency, contact irritancy, and acute toxicity of permethrin-treated clothing against nymphal Ixodes scapularis ticks | journal = Ticks and Tick-Borne Diseases | volume = 8 | issue = 6 | pages = 837–849 | date = October 2017 | pmid = 28754599 | pmc = 5665650 | doi = 10.1016/j.ttbdis.2017.06.010 }}</ref> Permethrin-treated closed-toed shoes and socks reduce by 74 times the number of bites from nymphs that make first contact with a shoe of a person also wearing treated shorts (because nymphs usually quest near the ground, this is a typical contact scenario).<ref name=miller_2011>{{cite journal | vauthors = Miller NJ, Rainone EE, Dyer MC, González ML, Mather TN | title = Tick bite protection with permethrin-treated summer-weight clothing | journal = Journal of Medical Entomology | volume = 48 | issue = 2 | pages = 327–333 | date = March 2011 | pmid = 21485369 | doi = 10.1603/me10158 | doi-access = free }}</ref> Better protection can be achieved by tucking permethrin-treated trousers (pants) into treated socks and a treated long-sleeve shirt into the trousers so as to minimize gaps through which a tick might reach the wearer's skin.<ref name=EPA_tick_prevention>{{cite web | title=Tips to prevent tick bytes | url=https://www.epa.gov/insect-repellents/tips-prevent-tick-bites | website=Insect repellents | publisher=Environmental Protection Agency | access-date=21 May 2019 | date=15 July 2013 | archive-url=https://web.archive.org/web/20190415170027/https://www.epa.gov/insect-repellents/tips-prevent-tick-bites | archive-date=15 April 2019 | url-status=live }}</ref> Light-colored clothing may make it easier to see ticks and remove them before they bite.<ref name = EPA_tick_prevention/> Military and outdoor workers' uniforms treated with permethrin have been found to reduce the number of bite cases by 80–95%.<ref name=eisen_2017/> Permethrin protection lasts several weeks of wear and washings in customer-treated items and up to 70 washings for factory-treated items.<ref name=CDC_travelers_protection/> Permethrin should not be used on human skin, underwear or cats.<ref name=CDC_travelers_protection/><ref name=dymond_2008>{{cite journal | vauthors = Dymond NL, Swift IM | title = Permethrin toxicity in cats: a retrospective study of 20 cases | journal = Australian Veterinary Journal | volume = 86 | issue = 6 | pages = 219–223 | date = June 2008 | pmid = 18498556 | doi = 10.1111/j.1751-0813.2008.00298.x }}</ref> | |||
| A community can reduce the incidence of Lyme disease by reducing the numbers of primary hosts on which the deer tick depends, such as rodents, other small mammals, and deer. Reduction of the deer population may, over time, help break the reproductive cycle of the deer ticks and their ability to flourish in suburban and rural areas.<ref name=bulletin_2013/> | |||
| The ] recommends several tick ] for use on exposed skin, including ], ], ] (a derivative of amino acid beta-alanine), ] (OLE, a natural compound) and OLE's active ingredient ].<ref name=CDC_Lyme_prev_on_people/><ref name = EPA_insect_repellents>{{cite web | title=Repellents: protection against mosquitoes, ticks and other arthropods | url=https://www.epa.gov/insect-repellents/ | website=Insect repellents | publisher=Environmental Protection Agency | access-date=21 May 2019 | date=9 July 2013 | archive-url=https://web.archive.org/web/20190520074421/https://www.epa.gov/insect-repellents | archive-date=20 May 2019 | url-status=live }}</ref><ref name=nguyen_2018/> Unlike permethrin, repellents repel but do not kill ticks, protect for only several hours after application, and may be washed off by sweat or water.<ref name=CDC_travelers_protection/> The most popular repellent is DEET in the U.S. and picaridin in Europe.<ref name=nguyen_2018>{{cite journal | vauthors = Nguyen QD, Vu MN, Hebert AA | title = Insect repellents: An updated review for the clinician | journal = Journal of the American Academy of Dermatology | volume = 88 | issue = 1 | pages = 123–130 | date = January 2023 | pmid = 30395919 | doi = 10.1016/j.jaad.2018.10.053 | s2cid = 53246686 }}</ref> Unlike DEET, picaridin is odorless and is less likely to irritate the skin or harm fabric or plastics.<ref name=nguyen_2018/> Repellents with higher concentration may last longer but are not more effective; against ticks, 20% picaridin may work for 8 hours vs. 55–98.11% DEET for 5–6 hours or 30–40% OLE for 6 hours.<ref name=CDC_travelers_protection/><ref name=EPA_insect_repellents/> Repellents should not be used under clothes, on eyes, mouth, wounds or cuts, or on babies younger than 2 months (3 years for OLE or PMD).<ref name=CDC_travelers_protection/><ref name=CDC_Lyme_prev_on_people/> If ] is used, repellent should be applied on top of it.<ref name=CDC_travelers_protection/> Repellents should not be sprayed directly on a face, but should instead be sprayed on a hand and then rubbed on the face.<ref name = CDC_travelers_protection/> | |||
| An unusual, organic approach to control of ticks and prevention of Lyme disease involves the use of ]. Guineafowl are voracious consumers of insects and ]s, and have a particular fondness for ticks. Localized use of domesticated guineafowl may reduce dependence on chemical pest-control methods.<ref name="Duffy"/> | |||
| After coming indoors, clothes, gear and pets should be checked for ticks.<ref name = CDC_Lyme_prev_on_people/> Clothes can be put into a hot dryer for 10 minutes to kill ticks (just washing or warm dryer are not enough).<ref name=CDC_Lyme_prev_on_people/> Showering as soon as possible, looking for ticks over the entire body, and removing them reduce risk of infection.<ref name = CDC_Lyme_prev_on_people/> Unfed tick nymphs are the size of a poppy seed, but a day or two after biting and attaching themselves to a person, they look like a small ].<ref name=CT_tick-management>{{cite web | vauthors = Stafford KC | title=Tick management handbook (rev. ed.) | date=2007 | volume=1010 | url=https://portal.ct.gov/-/media/CAES/DOCUMENTS/Publications/Bulletins/b1010pdf.pdf?la=en | website=Bulletins | publisher=Connecticut Agricultural Experiment Station | access-date=21 May 2019 | archive-url=https://web.archive.org/web/20190403234108/https://portal.ct.gov/-/media/CAES/DOCUMENTS/Publications/Bulletins/b1010pdf.pdf?la=en | archive-date=3 April 2019 | url-status=live }}</ref> The following areas should be checked especially carefully: armpits, between legs, back of knee, bellybutton, trunk, and in children ears, neck and hair.<ref name=CDC_Lyme_prev_on_people/> | |||
| ===Management of host animals=== | |||
| Lyme and all other deer tick-borne diseases can be prevented on a regional level by reducing the deer population on which the ticks depend for reproductive success. (Although deer ticks do acquire Lyme disease pathogens from rodents and not from deer, the size of the tick population tends to parallel that of the deer population.)<ref name="Westport"/> This has been demonstrated in the communities of ]<ref name="Rand"/> and Mumford Cove, Connecticut.<ref name=managing_deer_2007/> | |||
| ===Tick removal=== | |||
| For example, in the U.S., reducing the deer population to levels of 8 to 10 per square mile (from the current levels of 60 or more deer per square mile in the areas of the country with the highest Lyme disease rates), the tick numbers can be brought down to levels too low to spread Lyme and other tick-borne diseases.<ref name=kirby_2004/> However, such a drastic reduction may be impractical in many areas. Routine veterinary control of ], including livestock, by use of chemical acaricides can contribute to reducing exposure of humans to ticks. However, the risk of acquiring Lyme disease does not depend on the existence of a local deer population, as is commonly assumed. Eliminating deer from smaller areas {{convert|2.5|ha|acre|abbr=on}} may in fact lead to an increase in tick density and the rise of "tick-borne disease hotspots".<ref name="Perkins"/> | |||
| ] | |||
| Attached ticks should be removed promptly. Risk of infection increases with time of attachment, but in North America risk of Lyme disease is small if the tick is removed within 36 hours.<ref name="piesman2002"/> ] recommends inserting a fine-tipped tweezer between the skin and the tick, grasping very firmly, and pulling the closed tweezer straight away from the skin without twisting, jerking, squeezing or crushing the tick.<ref name=CDC_tick_removal>{{cite web | title=Tick removal and testing | url=https://www.cdc.gov/lyme/removal/ | website=Lyme Disease | publisher=Centers for Disease Control and Prevention | access-date=21 May 2019 | date=22 April 2019 | archive-url=https://web.archive.org/web/20171123052303/https://www.cdc.gov/lyme/removal/ | archive-date=23 November 2017 | url-status=live }}</ref> After tick removal, any tick parts remaining in the skin should be removed with a clean tweezer, if possible.<ref name=CDC_tick_removal/> The wound and hands should then be cleaned with alcohol or soap and water.<ref name=CDC_tick_removal/> The tick may be disposed by placing it in a container with alcohol, sealed bag, tape or flushed down the toilet.<ref name=CDC_tick_removal/> The bitten person should write down where and when the bite happened so that this can be informed to a doctor if the person gets a rash or flu-like symptoms in the following several weeks.<ref name=CDC_tick_removal/> CDC recommends not using fingers, nail polish, petroleum jelly or heat on the tick to try to remove it.<ref name=CDC_tick_removal/> | |||
| In Australia, where the ] is prevalent, the ] recommends not using tweezers to remove ticks, because if the person is allergic, ] could result.<ref name=australia_tick_freeze>{{cite web|title=Tick Allergy|url=http://www.allergy.org.au/patients/insect-allergy-bites-and-stings/tick-allergy|access-date=30 April 2015|date=2014|url-status=live|archive-url=https://web.archive.org/web/20150514060441/http://www.allergy.org.au/patients/insect-allergy-bites-and-stings/tick-allergy|archive-date=14 May 2015}}</ref> Instead, a product should be sprayed on the tick to cause it to freeze and then drop off.<ref name=australia_tick_freeze/> Another method consists in using about 20 cm of dental floss or fishing line for slowly tying an overhand knot between the skin and the tick and then pulling it away from the skin.<ref>{{cite journal | vauthors = Röggla G | title = Death of unknown origin in alpine medicine | journal = Wilderness & Environmental Medicine | volume = 13 | issue = 2 | pages = 181 | year = 2002 | pmid = 12092975 | doi = 10.1580/1080-6032(2002)0132.0.co;2 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Ghirga G, Ghirga P | title = Effective tick removal with a fishing line knot | journal = Wilderness & Environmental Medicine | volume = 21 | issue = 3 | pages = 270–271 | date = September 2010 | pmid = 20832708 | doi = 10.1016/j.wem.2010.04.005 | doi-access = free }}</ref> | |||
| Action can be taken to avoid getting bitten by ticks by using insect repellants, for example those that contain ]. DEET-containing repellants are thought to be moderately effective in the prevention of tick bites.<ref name="pmid11929056"/> | |||
| ===Preventive antibiotics=== | |||
| In Europe, "The reservoir species that contain the most pathogens are the European roe deer '']'' (incompetent host for ''B. burgdorferi'' and TBE virus but important for feeding the ticks), in which two species of ''Rickettsia'' and two species of ''Borrelia'' were identified, and '']'', in which one ''Rickettsia'' and three ''Borrelia'' species were identified",<ref>Wodecka, B., Rymaszewska, A., & Skotarczak, B. (2013), . Experimental and Applied Acarology, 1-13 ().</ref> with high risks of coinfection in roe deer.<ref>Overzier E, Pfister K, Herb I, Mahling M, Böck G Jr, Silaghi C (2013) ''Detection of tick-borne pathogens in roe deer (Capreolus capreolus), in questing ticks (Ixodes ricinus), and in ticks infesting roe deer in southern Germany''. Ticks Tick Borne Dis. 2013 Jun; 4(4):320-8. Epub 2013 Apr 6. ()</ref> | |||
| <!-- prophylaxis if found early --> | |||
| The risk of infectious transmission increases with the duration of tick attachment.<ref name=wright_2012/> It requires between 36 and 48 hours of attachment for the bacteria that causes Lyme to travel from within the tick into its saliva.<ref name=wright_2012/> If a deer tick that is sufficiently likely to be carrying ''Borrelia'' is found attached to a person and removed, and if the tick has been attached for 36 hours or is engorged, a single dose of doxycycline administered within the 72 hours after removal may reduce the risk of Lyme disease. It is not generally recommended for all people bitten, as development of infection is rare: about 50 bitten people would have to be treated this way to prevent one case of erythema migrans (i.e. the typical rash found in about 70–80% of people infected).<ref name=NEJM2014/><ref name=wright_2012/> | |||
| === |
===Garden landscaping=== | ||
| Several landscaping practices may reduce the risk of tick bites in residential yards.<ref name=CT_tick-management/><ref name=CDC_Lyme_prev_in_yard>{{cite web | title=Preventing tick bites in the yard | url=https://www.cdc.gov/lyme/prev/in_the_yard.html | website=Lyme Disease | publisher=Centers for Disease Control and Prevention | access-date=21 May 2019 | date=8 March 2019 | archive-url=https://web.archive.org/web/20190615054940/https://www.cdc.gov/lyme/prev/in_the_yard.html | archive-date=15 June 2019 | url-status=live }}</ref> These include keeping lawns mown, removing ] and weeds and avoiding the use of ground cover.<ref name=CT_tick-management/> A 3-ft-wide rock or woodchip barrier is recommended to separate lawns from wood piles, ]s, ] and shrubs.<ref name = CDC_Lyme_prev_in_yard/> Without vegetation on the barrier, ticks will tend not to cross it; ] may also be sprayed on it to kill ticks.<ref name=CDC_Lyme_prev_in_yard/> A sun-exposed tick-safe zone at least 9 ft from the barrier should concentrate human activity on the yard, including any patios, playgrounds and gardening.<ref name=CDC_Lyme_prev_in_yard/> Materials such as wood decking, concrete, bricks, gravel or woodchips used on the ground under patios and playgrounds would discourage ticks there.<ref name=CT_tick-management/> An 8-ft-high fence may be added to keep deer away from the tick-safe zone.<ref name=CDC_Lyme_prev_in_yard/><ref name=CT_tick-management/> | |||
| A ] against Lyme disease, based on the outer surface protein A (ospA) of ''B. burgdorferi'', was developed by SmithKline Beecham. In ]s involving more than 10,000 people, the vaccine, called LYMErix, was found to confer protective immunity to ''Borrelia'' in 76% of adults and 100% of children with only mild or moderate and transient ]s.<ref name=Poland_2001/> LYMErix was approved on the basis of these trials by the ] (FDA) on December 21, 1998. | |||
| ===Occupational exposure=== | |||
| Following approval of the vaccine, its entry in clinical practice was slow for a variety of reasons, including its cost, which was often not reimbursed by insurance companies.<ref name=rowe_199/> Subsequently, hundreds of vaccine recipients reported they had developed ] side effects. Supported by some patient advocacy groups, a number of ]s were filed against GlaxoSmithKline, alleging the vaccine had caused these health problems. These claims were investigated by the FDA and the ], which found no connection between the vaccine and the autoimmune complaints.<ref name="uphill"/> | |||
| Outdoor workers are at risk of Lyme disease if they work at sites with infected ticks. This includes construction, landscaping, forestry, brush clearing, land surveying, farming, railroad work, oil field work, utility line work, park or wildlife management.<ref>{{Cite web|title = CDC – Lyme Disease – NIOSH Workplace Safety and Health Topic|url = https://www.cdc.gov/niosh/topics/lyme/|website = www.cdc.gov|access-date = 3 November 2015|url-status=live |archive-url = https://web.archive.org/web/20151113075310/http://www.cdc.gov/niosh/topics/lyme/|archive-date = 13 November 2015|date = 3 August 2017}}</ref><ref>{{cite web |title=Risks: Lyme Disease {{!}} NIOSH {{!}} CDC |url=https://www.cdc.gov/niosh/topics/lyme/risks.html |website=www.cdc.gov |access-date=26 April 2019 |language=en-us |date=14 November 2018 |archive-url=https://web.archive.org/web/20190426005009/https://www.cdc.gov/niosh/topics/lyme/risks.html |archive-date=26 April 2019 |url-status=live }}</ref> U.S. workers in the northeastern and north-central states are at highest risk of exposure to infected ticks. Ticks may also transmit other tick-borne diseases to workers in these and other regions of the country. Worksites with woods, bushes, high grass or ] are likely to have more ticks. Outdoor workers should be most careful to protect themselves in the late spring and summer when young ticks are most active.<ref name=cdclyme>{{cite web | publisher = The Centers for Disease Control and Prevention | url = https://www.cdc.gov/niosh/topics/lyme/ | date = 12 October 2016 | access-date = 22 June 2017 | title = Lyme disease | url-status=live | archive-url = https://web.archive.org/web/20170617203154/https://www.cdc.gov/niosh/topics/lyme/ | archive-date = 17 June 2017}}{{CDC}}</ref> | |||
| ===Host animals=== | |||
| Despite the lack of evidence that the complaints were caused by the vaccine, sales plummeted and LYMErix was withdrawn from the U.S. market by GlaxoSmithKline in February 2002,<ref name=vaccine_2008/> in the setting of negative media coverage and fears of vaccine side effects.<ref name="uphill"/><ref name="cautionary"/> The fate of LYMErix was described in the medical literature as a "cautionary tale";<ref name="cautionary"/> an editorial in '']'' cited the withdrawal of LYMErix as an instance in which "unfounded public fears place pressures on vaccine developers that go beyond reasonable safety considerations."<ref name="safe"/> The original developer of the OspA vaccine at the ] told ''Nature'': "This just shows how irrational the world can be... There was no scientific justification for the first OspA vaccine LYMErix being pulled."<ref name="uphill"/> | |||
| Ticks can feed upon the blood of a wide array of possible host species, including ], ], ], ], ], ], ] and ]. The extent to which a tick can feed, reproduce, and spread will depend on the type and availability of its hosts. Whether it will spread disease is also affected by its available hosts. Some species, such as lizards, are referred to as "dilution hosts" because they don't tend to support Lyme disease pathogens and so decrease the likelihood that the disease will be passed on by ticks feeding on them. ] are both a food source and a "reproductive host", where ticks tend to mate.<ref>{{Cite journal |last1=Levi |first1=Taal |last2=Kilpatrick |first2=A. Marm |last3=Mangel |first3=Marc |last4=Wilmers |first4=Christopher C. |date=2012-07-03 |title=Deer, predators, and the emergence of Lyme disease |journal=Proceedings of the National Academy of Sciences |volume=109 |issue=27 |pages=10942–10947 |doi=10.1073/pnas.1204536109 |doi-access=free |pmc=3390851 |pmid=22711825|bibcode=2012PNAS..10910942L }}</ref> The ] is a ] in which the pathogen for Lyme disease can survive. Availability of hosts can have significant impacts on the transmission of Lyme disease. A greater diversity of hosts, or of those that don't support the pathogen, tends to decrease the likelihood that the disease will be transmitted.<ref name="Chrobak">{{cite journal | vauthors = Chrobak U |title=Lyme and other tick-borne diseases are on the rise. But why? |journal=Knowable Magazine |date=3 February 2022 |doi=10.1146/knowable-020222-1 |doi-access=free |url=https://knowablemagazine.org/article/health-disease/2022/lyme-other-tickborne-diseases-rise |access-date=4 March 2022}}</ref> | |||
| In the United States, one approach to reducing the incidence of Lyme and other deer tick-borne diseases has been to greatly reduce the deer population on which the adult ticks depend for feeding and reproduction. Lyme disease cases fell following deer eradication on an island, ],<ref name="Rand"/> and following deer control in Mumford Cove, Connecticut.<ref name=managing_deer_2007/> Advocates have suggested reducing the deer population to levels of 8 to 10 deer per square mile, compared to levels of 60 or more deer per square mile in the areas of the country with the highest Lyme disease rates.<ref name=kirby_2004/> While these studies have found these effects, other studies have found opposite effects. A study done in Massachusetts removed deer and did not see a significant decrease in tick abundance afterwards.<ref>{{Cite journal |last1=Wilson |first1=Mark L |last2=Levine |first2=Jay F. |last3=Spielman |first3=Andrew |date=1984 |title=Effect of deer reduction on abundance of the deer tick (Ixodes dammini). |journal=Yale Journal of Biology and Medicine |volume=57 |issue=4 |pages=697–705 |pmid=6516462 |pmc=2589992 }}</ref> Another study done in New Jersey removed deer and also did not see a reduction in the number of questing ticks and determined that deer culling is an unlikely way to effectively control tick populations.<ref>{{Cite journal |last1=Jordan |first1=Robert A. |last2=Schulze |first2=Terry L. |last3=Jahn |first3=Margaret B. |date=2007-09-01 |title=Effects of Reduced Deer Density on the Abundance of<i>Ixodes scapularis</i>(Acari: Ixodidae) and Lyme Disease Incidence in a Northern New Jersey Endemic Area |url=https://academic.oup.com/jme/article/44/5/752/972557 |journal=Journal of Medical Entomology |volume=44 |issue=5 |pages=752–757 |doi=10.1093/jmedent/44.5.752 |pmid=17915504 |issn=0022-2585|doi-access=free }}</ref> One study summarized the results of multiple studies all looking at deer reduction controlling tick populations and determined that deer control can't be used as a standalone reduction for Lyme disease. It also claims that since most of the studies looking at this are not good representatives of areas with high human Lyme disease risk. <ref>{{Cite journal |last1=Kugeler |first1=K. J. |last2=Jordan |first2=R. A. |last3=Schulze |first3=T. L. |last4=Griffith |first4=K. S. |last5=Mead |first5=P. S. |date=2016 |title=Will Culling White-Tailed Deer Prevent Lyme Disease? |journal=Zoonoses and Public Health |language=en |volume=63 |issue=5 |pages=337–345 |doi=10.1111/zph.12245 |issn=1863-2378 |pmc=4912954 |pmid=26684932}}</ref> There is varying information on whether or not the removal of deer is actually a way to control the Lyme disease epidemic. Removal of smaller mammals that are fed on by juveniles who are more actively acquiring and spreading the pathogen, would decrease Lyme disease risk the most.<ref>{{Cite journal |last1=Van Buskirk |first1=Josh |last2=Ostfeld |first2=Richard S. |date=1995 |title=Controlling Lyme Disease by Modifying the Density and Species Composition of Tick Hosts |url=https://esajournals.onlinelibrary.wiley.com/doi/10.2307/2269360 |journal=Ecological Applications |language=en |volume=5 |issue=4 |pages=1133–1140 |doi=10.2307/2269360 |jstor=2269360 |bibcode=1995EcoAp...5.1133V |issn=1939-5582}}</ref> | |||
| New vaccines are being researched using outer surface protein C (OspC) and ] as methods of immunization.<ref name="Earnhart 2007"/><ref name=Pozsgay_2007/> Vaccines have been formulated and approved for prevention of Lyme disease in dogs. Currently, three Lyme disease vaccines are available. LymeVax, formulated by Fort Dodge Laboratories, contains intact dead spirochetes which expose the host to the organism. Galaxy Lyme, Intervet-]'s vaccine, targets proteins OspC and OspA. The OspC antibodies kill any of the bacteria that have not been killed by the OspA antibodies. Canine Recombinant Lyme, formulated by ], generates antibodies against the OspA protein so a tick feeding on a vaccinated dog draws in blood full of anti-OspA antibodies, which kill the spirochetes in the tick's gut before they are transmitted to the dog.<ref name="Brooks, DVM"/> | |||
| Others have noted that while deer are reproductive hosts, they are not ''Borrelia burgdorferi'' reservoirs. This is because it was found that white-tailed deer blood actually kills the ''Borrelia burgdorferi'' bacteria.<ref>{{Cite journal |last1=Pearson |first1=Patrick |last2=Rich |first2=Connor |last3=Feehan |first3=Martin J.R. |last4=Ditchkoff |first4=Stephen S. |last5=Rich |first5=Stephen M. |date=May 2023 |title=White-Tailed Deer Serum Kills the Lyme Disease Spirochete, Borrelia burgdorferi |journal=Vector-Borne and Zoonotic Diseases |volume=23 |issue=5 |pages=303–305 |doi=10.1089/vbz.2022.0095 |issn=1530-3667 |pmc=10178931 |pmid=36944114}}</ref> Researchers have suggested that smaller, less obviously visible Lyme reservoirs, like ] and ], may more strongly impact Lyme disease occurrence. Ecosystem studies in New York state suggest that white-footed mice thrive when forests are broken into smaller isolated chunks of woodland with fewer rodent predators. With more rodents harboring the disease, the odds increase that a tick will feed on a disease-harboring rodent and that someone will pick up a disease-carrying tick in their garden or walking in the woods. Data indicates that the smaller the wooded area, the more ticks it will contain and the likely they are to carry Lyme disease, supporting the idea that ] and habitat fragmentation affect ticks, hosts and disease transmission.<ref name="Chrobak"/> | |||
| ===Tick removal=== | |||
| Attached ticks should be removed promptly, as removal within 36 hours can reduce transmission rates.<ref name="piesman2002"/> Folk remedies for tick removal tend to be ineffective, offer no advantages in preventing the transfer of disease, and may increase the risks of transmission or infection.<ref>http://www.tickbitepreventionweek.org/tick-removal.html</ref> The best method is simply to pull the tick out with tweezers as close to the skin as possible, without twisting, and avoiding crushing the body of the tick or removing the head from the tick's body.<ref name=JAMA_2007/> The risk of infection increases with the time the tick is attached, and if a tick is attached for less than 24 hours, infection is unlikely. However, since these ticks are very small, especially in the nymph stage, prompt detection is quite difficult.<ref name="piesman2002"/> | |||
| Tick-borne diseases are estimated to affect ~80 % of ] worldwide.<ref name="Rochlin">{{cite journal | vauthors = Rochlin I, Toledo A | title = Emerging tick-borne pathogens of public health importance: a mini-review | journal = Journal of Medical Microbiology | volume = 69 | issue = 6 | pages = 781–791 | date = June 2020 | pmid = 32478654 | pmc = 7451033 | doi = 10.1099/jmm.0.001206 }}</ref> They also affect cats, dogs, and other pets. Routine veterinary control of ] through the use of ]s has been suggested as a way to reduce exposure of humans to ticks. However, chemical control with acaricides is now criticized on a number of grounds. Ticks appear to develop resistance to acaricides; acaricides are costly; and there are concerns over their toxicity and the potential for chemical residues to affect food and the environment.<ref name="Rajput">{{cite journal | vauthors = Rajput ZI, Hu SH, Chen WJ, Arijo AG, Xiao CW | title = Importance of ticks and their chemical and immunological control in livestock | journal = Journal of Zhejiang University. Science. B | volume = 7 | issue = 11 | pages = 912–921 | date = November 2006 | pmid = 17048307 | pmc = 1635821 | doi = 10.1631/jzus.2006.B0912 }}</ref> | |||
| In Europe, known reservoirs of ''Borrelia burgdorferi'' were 9 small mammals, 7 medium-sized mammals and 16 species of birds (including passerines, sea-birds and pheasants).<ref name=gern1998/> These animals seem to transmit spirochetes to ticks and thus participate in the natural circulation of B. burgdorferi in Europe. The ] is also suspected as well as other species of small rodents, particularly in Eastern Europe and Russia.<ref name=gern1998>{{cite journal | vauthors = Gern L, Estrada-Peña A, Frandsen F, Gray JS, Jaenson TG, Jongejan F, Kahl O, Korenberg E, Mehl R, Nuttall PA | title = European reservoir hosts of Borrelia burgdorferi sensu lato | journal = Zentralblatt für Bakteriologie | volume = 287 | issue = 3 | pages = 196–204 | date = March 1998 | pmid = 9580423 | doi = 10.1016/S0934-8840(98)80121-7 }}</ref> "The reservoir species that contain the most pathogens are the European roe deer '']'';<ref name="Wodecka2013" /> "''it does not appear to serve as a major reservoir of B. burgdorferi''" thought Jaenson & al. (1992)<ref>{{cite journal | vauthors = Jaenson TG, Tälleklint L | title = Incompetence of roe deer as reservoirs of the Lyme borreliosis spirochete | journal = Journal of Medical Entomology | volume = 29 | issue = 5 | pages = 813–817 | date = September 1992 | pmid = 1404260 | doi = 10.1093/jmedent/29.5.813 }}</ref> (incompetent host for ''B. burgdorferi'' and TBE virus) but it is important for feeding the ticks,<ref>{{cite journal | vauthors = Tälleklint L, Jaenson TG | title = Transmission of Borrelia burgdorferi s.l. from mammal reservoirs to the primary vector of Lyme borreliosis, Ixodes ricinus (Acari: Ixodidae), in Sweden | journal = Journal of Medical Entomology | volume = 31 | issue = 6 | pages = 880–886 | date = November 1994 | pmid = 7815401 | doi = 10.1093/jmedent/31.6.880 }}</ref> as ] and wild ] ('']''),<ref name="Wodecka2013">{{cite journal | vauthors = Wodecka B, Rymaszewska A, Skotarczak B | title = Host and pathogen DNA identification in blood meals of nymphal Ixodes ricinus ticks from forest parks and rural forests of Poland | journal = Experimental and Applied Acarology | volume = 62 | issue = 4 | pages = 543–555 | date = April 2014 | pmid = 24352572 | pmc = 3933768 | doi = 10.1007/s10493-013-9763-x }}</ref> in which one ''Rickettsia'' and three ''Borrelia'' species were identified",<ref name="Wodecka2013"/> with high risks of coinfection in roe deer.<ref>{{cite journal | vauthors = Overzier E, Pfister K, Herb I, Mahling M, Böck G, Silaghi C | title = Detection of tick-borne pathogens in roe deer (Capreolus capreolus), in questing ticks (Ixodes ricinus), and in ticks infesting roe deer in southern Germany | journal = Ticks and Tick-Borne Diseases | volume = 4 | issue = 4 | pages = 320–328 | date = June 2013 | pmid = 23571115 | doi = 10.1016/j.ttbdis.2013.01.004 }}{{Dead link|date=March 2022 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> Nevertheless, in the 2000s, in roe deer in Europe "''two species of Rickettsia and two species of Borrelia were identified''".<ref name="Wodecka2013"/> | |||
| ==Vaccination== | |||
| {{As of|2023}} no human vaccines for Lyme disease were available.<ref name="cdc-vaccine">{{Cite web |date=2022-08-11 |title=Lyme disease vaccine|url=https://www.cdc.gov/lyme/about/lyme-disease-vaccine.html?CDC_AAref_Val=https://www.cdc.gov/lyme/prev/vaccine.html |access-date=2024-11-13 |publisher=]}}</ref> The only human vaccine to advance to market was LYMErix, which was available from 1998, but discontinued in 2002.<ref name="O'Bier2021">{{cite journal | vauthors = O'Bier NS, Hatke AL, Camire AC, Marconi RT | title = Human and Veterinary Vaccines for Lyme Disease | journal = Current Issues in Molecular Biology | volume = 42 | issue = | pages = 191–222 | date = 2021 | pmid = 33289681 | pmc = 7946718 | doi = 10.21775/cimb.042.191 }}</ref> The vaccine candidate VLA15 was scheduled to start a phase 3 trial in the third quarter of 2022, with other research ongoing. Multiple vaccines are available for the prevention of Lyme disease in dogs. | |||
| ===LYMErix=== | |||
| The vaccine LYMErix was available from 1998 to 2002. The ] against Lyme disease, based on the outer surface protein A (OspA) of ''B. burgdorferi'' with aluminum hydroxide as adjuvant, was developed by ]. In ]s involving more than 10,000 people, the vaccine was found to confer protective immunity to Lyme disease in 76% of adults after three doses with only mild or moderate and transient ]s.<ref name=Poland_2001/><ref name=Poland2011/> On 21 December 1998, the ] (FDA) approved LYMErix on the basis of these trials for persons of ages 15 through 70.<ref name="Poland2011">{{cite journal | vauthors = Poland GA | title = Vaccines against Lyme disease: What happened and what lessons can we learn? | journal = Clinical Infectious Diseases | volume = 52 | issue = Suppl 3 | pages = s253–s258 | date = February 2011 | pmid = 21217172 | doi = 10.1093/cid/ciq116 | doi-access = free }}</ref><ref name="O'Bier2021"/> | |||
| Following approval of the ], its entry into clinical practice was slow for a variety of reasons, including its cost, which was often not reimbursed by insurance companies.<ref name=rowe_199/> Subsequently, hundreds of vaccine recipients reported they had developed ] and other side effects. Supported by some advocacy groups, a number of ]s were filed against ], alleging the vaccine had caused these health problems. These claims were investigated by the FDA and the Centers for Disease Control, which found no connection between the vaccine and the autoimmune complaints.<ref name="uphill"/> | |||
| Despite the lack of evidence that the complaints were caused by the vaccine, sales plummeted and LYMErix was withdrawn from the U.S. market by GlaxoSmithKline in February 2002,<ref name=vaccine_2008/> in the setting of negative media coverage and fears of vaccine side effects.<ref name="uphill"/><ref name="cautionary"/> The fate of LYMErix was described in the medical literature as a "cautionary tale";<ref name="cautionary"/> an editorial in '']'' cited the withdrawal of LYMErix as an instance in which "unfounded public fears place pressures on vaccine developers that go beyond reasonable safety considerations."<ref name="safe"/> The original developer of the OspA vaccine at the ] told ''Nature'': "This just shows how irrational the world can be ... There was no scientific justification for the first OspA vaccine LYMErix being pulled."<ref name="uphill"/><ref>{{cite journal | vauthors = Aronowitz RA | title = The rise and fall of the lyme disease vaccines: a cautionary tale for risk interventions in American medicine and public health | journal = The Milbank Quarterly | volume = 90 | issue = 2 | pages = 250–277 | date = June 2012 | pmid = 22709388 | pmc = 3460208 | doi = 10.1111/j.1468-0009.2012.00663.x }}</ref> | |||
| ===VLA15=== | |||
| The hexavalent (OspA) protein subunit-based vaccine candidate VLA15 was developed by ]. It was granted ] by the U.S. ] in July 2017.<ref>{{cite web|title=Anti-vaxxers stopped the last Lyme disease vaccine. The FDA has just fast-tracked a new one|url=http://www.newsweek.com/lyme-disease-vaccine-valneva-fda-approva-641796|website=Newsweek|access-date=25 December 2017|date=25 July 2017|archive-url=https://web.archive.org/web/20171225092005/http://www.newsweek.com/lyme-disease-vaccine-valneva-fda-approva-641796|archive-date=25 December 2017|url-status=live}}</ref><ref>{{cite web |url=https://www.concordmonitor.com/lyme-disease-vaccine-trials-18056240 |title=A Lyme vaccine for humans is getting closer, says French biotech firm |work=Concord Monitor | vauthors = Brooks D |date=6 August 2018 |access-date=20 July 2021 }}</ref> In April 2020 ] paid $130 million for the rights to the vaccine, and the companies are developing it together, performing multiple phase 2 trials.<ref name="fiercebt-022022">{{Cite web | vauthors = Taylor NP |date=2022-02-04 |title=Pfizer's $130M Lyme disease vaccine advances to phase 3 after 3rd shot shown to increase antibodies |url=https://www.fiercebiotech.com/biotech/pfizer-s-130m-lyme-disease-vaccine-advances-to-phase-3-after-booster-shown-to-increase |access-date=2022-06-05 |website=Fierce Biotech}}</ref> | |||
| A phase 3 trial of VLA15 was scheduled for late 2022, recruiting volunteers at test sites located across the northeastern United States and in Europe.<ref>{{cite news | vauthors = Neergaard L, Lum S |title=Major test of first possible Lyme vaccine in 20 years begins |url=https://apnews.com/article/science-health-ticks-73fab8e29f3e2243c2db5bc33b3265e1 |work=Associated Press |date=8 August 2022 |access-date=11 August 2022}}</ref><ref name=ClinicalTrial>{{cite journal |url=https://clinicaltrials.gov/ct2/show/NCT05477524 |title=An Efficacy, Safety, Tolerability, Immunogenicity, and Lot-Consistency Clinical Trial of a 6-Valent OspA-Based Lyme Disease Vaccine (VLA15) (VALOR) |author=<!--not stated--> |date=28 July 2022 |website=] |publisher=National Institute of Health |access-date=11 August 2022}}</ref> Participants were scheduled to receive an initial three-dose series of vaccines over the course of five to nine months, followed by a booster dose after twelve months, with both the initial series and the booster dose scheduled to be complete before the year's peak Lyme disease season.<ref name=ClinicalTrial /> | |||
| ===Other research=== | |||
| An ] designed to cause a strong fast immune response to tick saliva allowed the immune system to detect and remove the ticks from test animals before they were able to transmit the infectious bacteria.<ref>{{cite web | vauthors = Klein A | url = https://www.newscientist.com/article/2297648-mrna-vaccine-against-tick-bites-could-help-prevent-lyme-disease/ | title = An mRNA vaccine that causes a red, itchy skin rash in response to bites by ticks may allow them to be removed before they transmit Lyme disease-causing bacteria | work = ] | date = 17 November 2021 }}</ref> The vaccine contains mRNAs for the body to build 19 proteins in tick saliva which, by enabling quick development of ] (itchy redness) at the bite site, protects guinea pigs against Lyme disease. It also protected the test animals if the tick is not removed if only one tick, but not three, remain attached.<ref>{{cite news | vauthors = Hathaway B |title=Novel Lyme vaccine shows promise |url=https://medicalxpress.com/news/2021-11-lyme-vaccine.html |access-date=13 December 2021 |work=] |language=en |quote=Compared to non-immunized guinea pigs, vaccinated animals exposed to infected ticks quickly developed redness at the tick bite site. None of the immunized animals developed Lyme disease if ticks were removed when redness developed. In contrast, about half of the control group became infected with B. burgdorferi after tick removal. When a single infected tick was attached to immunized guinea pigs and not removed, none of vaccinated animals were infected compared to 60 percent of control animals. However, protection waned in immunized guinea pigs if three ticks remained attached to the animal. Ticks in immunized animals were unable to feed aggressively and dislodged more quickly than those on guinea pigs in the control group.}}</ref><ref>{{cite journal | vauthors = Sajid A, Matias J, Arora G, Kurokawa C, DePonte K, Tang X, Lynn G, Wu MJ, Pal U, Strank NO, Pardi N, Narasimhan S, Weissman D, Fikrig E | title = mRNA vaccination induces tick resistance and prevents transmission of the Lyme disease agent | journal = Science Translational Medicine | volume = 13 | issue = 620 | pages = eabj9827 | date = November 2021 | pmid = 34788080 | doi = 10.1126/scitranslmed.abj9827 | s2cid = 244375227 }}</ref> | |||
| ===Canine vaccines=== | |||
| ] have been formulated and approved for the prevention of Lyme disease in dogs. Currently, three Lyme disease vaccines are available. LymeVax, formulated by Fort Dodge Laboratories, contains intact dead spirochetes which expose the host to the organism. Galaxy Lyme, Intervet-]'s vaccine, targets ]. The OspC antibodies kill any of the bacteria that have not been killed by the OspA antibodies. Canine Recombinant Lyme, formulated by ], generates antibodies against the OspA protein so a tick feeding on a vaccinated dog draws in blood full of anti-OspA antibodies, which kill the spirochetes in the tick's gut before they are transmitted to the dog.<ref name="Brooks, DVM"/> | |||
| ==Treatment== | ==Treatment== | ||
| <!-- regimens --> | <!-- regimens --> | ||
| ] are the primary treatment.<ref name=wright_2012/> The specific approach to their use is dependent on the individual affected and the stage of the disease.<ref name=wright_2012/> For most people with early localized infection, oral administration of ] is widely recommended as the first choice, as it is effective against not only ''Borrelia'' bacteria but also a variety of other illnesses carried by ticks.<ref name=wright_2012/> Doxycycline is contraindicated in children younger than eight years of age and women who are pregnant or breastfeeding;<ref name=wright_2012/> alternatives to doxycycline are amoxicillin, cefuroxime axetil, and ].<ref name=wright_2012/> Individuals with early disseminated or late infection may have symptomatic cardiac disease, |
] are the primary treatment.<ref name=NEJM2014/><ref name=wright_2012/> The specific approach to their use is dependent on the individual affected and the stage of the disease.<ref name=wright_2012/> For most people with early localized infection, oral administration of ] is widely recommended as the first choice, as it is effective against not only ''Borrelia'' bacteria but also a variety of other illnesses carried by ticks.<ref name=wright_2012/> People taking doxycycline should avoid sun exposure because of ].<ref name="idsa guideline"/> Doxycycline is contraindicated in children younger than eight years of age and women who are pregnant or breastfeeding;<ref name=wright_2012/> alternatives to doxycycline are ], ], and ].<ref name=wright_2012/> Azithromycin is recommended only in case of intolerance to the other antibiotics.<ref name="idsa guideline"/> The standard treatment for ], ], is not useful for Lyme disease.<ref name="idsa guideline"/> When it is unclear if a rash is caused by Lyme or cellulitis, the ] recommends treatment with ] or ], as these are effective against both infections.<ref name="idsa guideline"/> Individuals with early disseminated or late Lyme infection may have symptomatic cardiac disease, Lyme arthritis, or neurologic symptoms like ], ], ], or ].<ref name=wright_2012/> Intravenous administration of ] is recommended as the first choice in these cases;<ref name=wright_2012/> ] and doxycycline are available as alternatives.<ref name=wright_2012/> | ||
| <!-- duration/time effects --> | <!-- duration/time effects --> | ||
| Treatment regimens for Lyme disease range from 7–14 days in early localized disease, to 14–21 days in early disseminated disease to 14–28 days in late disseminated disease.<ref name="guidelines-2020"/> ] may be treated with ] as it can be taken by mouth and has a lower cost, although in North America evidence of efficacy is only indirect.<ref name="pmid17522387"/> In case of failure, guidelines recommend retreatment with injectable ].<ref name="pmid17522387"/> Several months after treatment for Lyme arthritis, if joint swelling persists or returns, a second round of antibiotics may be considered; intravenous antibiotics are preferred for retreatment in case of poor response to oral antibiotics.<ref name=wright_2012/><ref name="idsa guideline"/> Outside of that, a prolonged antibiotic regimen lasting more than 28 days is not recommended as no evidence shows it to be effective.<ref name=wright_2012/><ref>{{cite journal | vauthors = Berende A, ter Hofstede HJ, Vos FJ, van Middendorp H, Vogelaar ML, Tromp M, van den Hoogen FH, Donders AR, Evers AW, Kullberg BJ | title = Randomized Trial of Longer-Term Therapy for Symptoms Attributed to Lyme Disease | journal = The New England Journal of Medicine | volume = 374 | issue = 13 | pages = 1209–1220 | date = March 2016 | pmid = 27028911 | doi = 10.1056/NEJMoa1505425 | doi-access = free }}</ref> IgM and IgG antibody levels may be elevated for years even after successful treatment with antibiotics.<ref name=wright_2012/> As antibody levels are not indicative of treatment success, testing for them is not recommended.<ref name=wright_2012/> | |||
| Facial palsy may resolve without treatment: however, antibiotic treatment is recommended to stop other Lyme complications.<ref name="idsa guideline"/> Corticosteroids are not recommended when facial palsy is caused by Lyme disease.<ref name=garro_2018>{{cite journal | vauthors = Garro A, Nigrovic LE | title = Managing Peripheral Facial Palsy | journal = Annals of Emergency Medicine | volume = 71 | issue = 5 | pages = 618–624 | date = May 2018 | pmid = 29110887 | doi = 10.1016/j.annemergmed.2017.08.039 | doi-access = free }}</ref> In those with facial palsy, frequent use of artificial tears while awake is recommended, along with ointment and a patch or taping the eye closed when sleeping.<ref name="garro_2018"/><ref name=OTC-Drops>{{cite web | vauthors = Stephenson M |title=OTC Drops: Telling the Tears Apart |url=https://www.reviewofophthalmology.com/article/otc-drops-telling-the-tears-apart |website=Review of Ophtalmology |publisher=Jobson Medical Information LLC |date=4 October 2012 |access-date=16 April 2019 |archive-url=https://web.archive.org/web/20190417202911/https://www.reviewofophthalmology.com/article/otc-drops-telling-the-tears-apart |archive-date=17 April 2019 |url-status=live }}</ref> | |||
| <!-- prophylaxis if found early --> | |||
| The risk of infectious transmission increases with the duration of tick attachment.<ref name=wright_2012/> It requires between 36 and 48 hours of attachment for the bacteria that causes Lyme to travel from within the tick into its saliva.<ref name=wright_2012/> If a deer tick sufficiently likely to be carrying ''Borrelia'' is found attached to a person and removed, and if the tick has been attached for 36 hours or is engorged, a single dose of doxycycline administered within the 72 hours after removal may reduce the risk of Lyme disease.<ref name=wright_2012/> | |||
| About a third of people with Lyme carditis need a temporary ] until their heart conduction abnormality resolves, and 21% need to be hospitalized.<ref name=fish_2008/> Lyme carditis should not be treated with corticosteroids.<ref name=fish_2008/> | |||
| People with Lyme arthritis should limit their level of physical activity to avoid damaging affected joints, and in case of limping should use crutches.<ref name=arvikar_2015/> Pain associated with Lyme disease may be treated with ]s (NSAIDs).<ref name="idsa guideline"/> Corticosteroid ]s are not recommended for Lyme arthritis that is being treated with antibiotics.<ref name="idsa guideline"/><ref name=arvikar_2015/> People with Lyme arthritis treated with intravenous antibiotics or two months of oral antibiotics who continue to have ] two months after treatment and have negative ] test for '']'' ] in the ] are said to have post-antibiotic Lyme arthritis; this is more common after infection by certain Borrelia strains in people with certain genetic and immunologic characteristics.<ref name="idsa guideline"/><ref name="guidelines-2020"/><ref name=arvikar_2015>{{cite journal | vauthors = Arvikar SL, Steere AC | title = Diagnosis and treatment of Lyme arthritis | journal = Infectious Disease Clinics of North America | volume = 29 | issue = 2 | pages = 269–280 | date = June 2015 | pmid = 25999223 | pmc = 4443866 | doi = 10.1016/j.idc.2015.02.004 }}</ref> Post-antibiotic Lyme arthritis may be symptomatically treated with NSAIDs, ] (DMARDs), arthroscopic ], or physical therapy.<ref name="guidelines-2020"/><ref name=arvikar_2015/> | |||
| People receiving treatment should be advised that reinfection is possible and ].<ref name=lyme_guidelines_uk/> | |||
| ==Prognosis== | ==Prognosis== | ||
| Lyme disease's typical first sign, the ] (EM) rash, resolves within several weeks even without treatment.<ref name=NEJM2014/> However, in untreated people, the infection often disseminates to the nervous system, heart or joints, possibly causing permanent damage to body tissues.<ref name="idsa guideline"/> | |||
| For early cases, prompt{{specific time}} treatment is usually curative.<ref name=Krause_2006/> However, the severity and treatment of Lyme disease may be complicated due to late diagnosis, failure of antibiotic treatment, and simultaneous infection with other tick-borne diseases (coinfections), including ], ], and immune suppression{{citation needed|date=May 2013}} in the patient. | |||
| People who receive recommended antibiotic treatment within several days of appearance of an initial EM rash have the best prospects.<ref name=aucott_2008/> Recovery may not be total or immediate. The percentage of people achieving full recovery in the United States increases from about 64–71% at end of treatment for EM rash to about 84–90% after 30 months; higher percentages are reported in Europe.<ref name=wormser_2003>{{cite journal | vauthors = Wormser GP, Ramanathan R, Nowakowski J, McKenna D, Holmgren D, Visintainer P, Dornbush R, Singh B, Nadelman RB | title = Duration of antibiotic therapy for early Lyme disease. A randomized, double-blind, placebo-controlled trial | journal = Annals of Internal Medicine | volume = 138 | issue = 9 | pages = 697–704 | date = May 2003 | pmid = 12729423 | doi = 10.7326/0003-4819-138-9-200305060-00005 | s2cid = 3083800 }}</ref><ref name=stupica_2012>{{cite journal | vauthors = Stupica D, Lusa L, Ruzić-Sabljić E, Cerar T, Strle F | title = Treatment of erythema migrans with doxycycline for 10 days versus 15 days | journal = Clinical Infectious Diseases | volume = 55 | issue = 3 | pages = 343–350 | date = August 2012 | pmid = 22523260 | doi = 10.1093/cid/cis402 | doi-access = free }}</ref> Treatment failure, i.e. persistence of original or appearance of new signs of the disease, occurs only in a few people.<ref name=wormser_2003/> Remaining people are considered cured but continue to experience subjective symptoms, e.g. ] or ] or ].<ref name=dattwyler_1997/> These symptoms are usually mild and nondisabling.<ref name=dattwyler_1997>{{cite journal | vauthors = Dattwyler RJ, Luft BJ, Kunkel MJ, Finkel MF, Wormser GP, Rush TJ, Grunwaldt E, Agger WA, Franklin M, Oswald D, Cockey L, Maladorno D | title = Ceftriaxone compared with doxycycline for the treatment of acute disseminated Lyme disease | journal = The New England Journal of Medicine | volume = 337 | issue = 5 | pages = 289–294 | date = July 1997 | pmid = 9233865 | doi = 10.1056/NEJM199707313370501 | doi-access = free }}</ref> | |||
| A ] published in 2005 found some patients with Lyme disease have fatigue, joint or muscle pain, and ] symptoms persisting for years, despite antibiotic treatment.<ref name="Cairns"/> Patients with late stage Lyme disease have been shown to experience a level of physical ] equivalent to that seen in ].<ref name="Klempner"/> | |||
| People treated only after nervous system manifestations of the disease may end up with objective neurological deficits, in addition to subjective symptoms.<ref name="idsa guideline"/> In Europe, an average of 32–33 months after initial Lyme symptoms in people treated mostly with doxycycline 200 mg for 14–21 days, the percentage of people with lingering symptoms was much higher among those diagnosed with ] (50%) than among those with only an EM rash (16%).<ref name=vrethem_2002>{{cite journal | vauthors = Vrethem M, Hellblom L, Widlund M, Ahl M, Danielsson O, Ernerudh J, Forsberg P | title = Chronic symptoms are common in patients with neuroborreliosis -- a questionnaire follow-up study | journal = Acta Neurologica Scandinavica | volume = 106 | issue = 4 | pages = 205–208 | date = October 2002 | pmid = 12225315 | doi = 10.1034/j.1600-0404.2002.01358.x | s2cid = 42290158 | doi-access = free }}</ref> In another European study, 5 years after treatment for neuroborreliosis lingering symptoms were less common among children (15%) than adults (30%), and in the latter were less common among those treated within 30 days of the first symptom (16%) than among those treated later (39%); among those with lingering symptoms, 54% had daily activities restricted and 19% were on sick leave or incapacitated.<ref name=berglund_2002>{{cite journal | vauthors = Berglund J, Stjernberg L, Ornstein K, Tykesson-Joelsson K, Walter H | title = 5-y Follow-up study of patients with neuroborreliosis | journal = Scandinavian Journal of Infectious Diseases | volume = 34 | issue = 6 | pages = 421–425 | date = 2002 | pmid = 12160168 | doi = 10.1080/00365540110080421 | s2cid = 28306612 }}</ref> | |||
| In dogs, a serious long-term prognosis may result in glomerular disease,<ref name=merck_2012/> which is a category of kidney damage that may cause chronic kidney disease.<ref name="Brooks, DVM"/> Dogs may also experience chronic joint disease if the disease is left untreated. However, the majority of cases of Lyme disease in dogs result in a complete recovery with, and sometimes without, treatment with antibiotics.<ref name=staubinger/>{{Verify source|date=July 2013}} In rare cases, Lyme disease can be fatal to both humans and dogs.<ref name="fatal-cases"/> | |||
| Some data suggest that about 90% of Lyme ] treated with antibiotics recover fully a median of 24 days after appearing and most of the rest recover with only mild abnormality.<ref name=clark_1985>{{cite journal | vauthors = Clark JR, Carlson RD, Sasaki CT, Pachner AR, Steere AC | title = Facial paralysis in Lyme disease | journal = The Laryngoscope | volume = 95 | issue = 11 | pages = 1341–1345 | date = November 1985 | pmid = 4058212 | doi = 10.1288/00005537-198511000-00009 | s2cid = 85021 }}</ref><ref name=dovetall_1999>{{cite journal | vauthors = Dotevall L, Hagberg L | title = Successful oral doxycycline treatment of Lyme disease-associated facial palsy and meningitis | journal = Clinical Infectious Diseases | volume = 28 | issue = 3 | pages = 569–574 | date = March 1999 | pmid = 10194080 | doi = 10.1086/515145 | doi-access = free }}</ref> However, in Europe 41% of people treated for facial palsy had other lingering symptoms at followup up to 6 months later, including 28% with ] or ] and 14% with ] or ] problems.<ref name=dovetall_1999/> Palsies in both sides of the face are associated with worse and longer time to recovery.<ref name=clark_1985/><ref name=dovetall_1999/> Historical data suggests that untreated people with facial palsies recover at nearly the same rate, but 88% subsequently have Lyme arthritis.<ref name=clark_1985/><ref name=kalish_2001>{{cite journal | vauthors = Kalish RA, Kaplan RF, Taylor E, Jones-Woodward L, Workman K, Steere AC | title = Evaluation of study patients with Lyme disease, 10-20-year follow-up | journal = The Journal of Infectious Diseases | volume = 183 | issue = 3 | pages = 453–460 | date = February 2001 | pmid = 11133377 | doi = 10.1086/318082 | doi-access = free }}</ref> Other research shows that ] (involuntary movement of a facial muscle when another one is voluntarily moved) can become evident only 6–12 months after facial palsy appears to be resolved, as damaged nerves regrow and sometimes connect to incorrect muscles.<ref name=jowett_2017>{{cite journal | vauthors = Jowett N, Gaudin RA, Banks CA, Hadlock TA | title = Steroid use in Lyme disease-associated facial palsy is associated with worse long-term outcomes | journal = The Laryngoscope | volume = 127 | issue = 6 | pages = 1451–1458 | date = June 2017 | pmid = 27598389 | doi = 10.1002/lary.26273 | s2cid = 25596860 }}</ref> Synkinesis is associated with ] use.<ref name=jowett_2017/> In longer-term follow-up, 16–23% of Lyme facial palsies do not fully recover.<ref name=jowett_2017/> | |||
| In Europe, about a quarter of people with ] (Lyme ] and ]) treated with ] ] for 14 days an average of 30 days after first symptoms had to be retreated 3–6 months later because of unsatisfactory clinical response or continued ] in ]; after 12 months, 64% recovered fully, 31% had nondisabling mild or infrequent symptoms that did not require regular use of analgesics, and 5% had symptoms that were disabling or required substantial use of analgesics.<ref name=ogrinc_bannwarth/> The most common lingering nondisabling symptoms were headache, ], ], ], ] disturbances, ], ], ] disturbances, ], and ] disturbances. Lingering disabling symptoms included ] and other ].<ref name=ogrinc_bannwarth/> | |||
| Recovery from late neuroborreliosis tends to take longer and be less complete than from early neuroborreliosis, probably because of irreversible neurologic damage.<ref name="idsa guideline"/> | |||
| About half the people with Lyme carditis progress to complete ], but it usually resolves in a week.<ref name=fish_2008/> Other Lyme heart conduction abnormalities resolve typically within 6 weeks.<ref name=fish_2008/> About 94% of people have full recovery, but 5% need a permanent ] and 1% end up with persistent heart block (the actual percentage may be higher because of unrecognized cases).<ref name=fish_2008/> Lyme ] complications usually are mild and self-limiting.<ref name=fish_2008/> However, in some cases Lyme carditis can be fatal.<ref name=fish_2008/> | |||
| Recommended antibiotic treatments are effective in about 90% of Lyme arthritis cases, although it can take several months for inflammation to resolve and a second round of antibiotics is often necessary.<ref name="idsa guideline"/> Antibiotic-refractory Lyme arthritis also eventually resolves, typically within 9–14 months (range 4 months – 4 years); ]s or ] can accelerate recovery.<ref name=arvikar_2015/> | |||
| Reinfection is not uncommon. In a U.S. study, 6–11% of people treated for an EM rash had another EM rash within 30 months.<ref name=wormser_2003/> The second rash typically is due to infection by a different ] strain.<ref name=nadelman_2012>{{cite journal | vauthors = Nadelman RB, Hanincová K, Mukherjee P, Liveris D, Nowakowski J, McKenna D, Brisson D, Cooper D, Bittker S, Madison G, Holmgren D, Schwartz I, Wormser GP | title = Differentiation of reinfection from relapse in recurrent Lyme disease | journal = The New England Journal of Medicine | volume = 367 | issue = 20 | pages = 1883–1890 | date = November 2012 | pmid = 23150958 | pmc = 3526003 | doi = 10.1056/NEJMoa1114362 }}</ref> | |||
| === Post-treatment Lyme disease syndrome === | |||
| Chronic symptoms like pain, fatigue, or cognitive impairment are experienced by 5–20% of people who contract Lyme disease, even after completing treatment. This is called Post-treatment Lyme disease syndrome, or PTLDS.<ref name=":0" /><ref name=":1">{{cite journal | vauthors = Bai NA, Richardson CS | title = Posttreatment Lyme disease syndrome and myalgic encephalomyelitis/chronic fatigue syndrome: A systematic review and comparison of pathogenesis | journal = Chronic Diseases and Translational Medicine | volume = 9 | issue = 3 | pages = 183–190 | date = September 2023 | pmid = 37711861 | pmc = 10497844 | doi = 10.1002/cdt3.74 }}</ref> | |||
| The cause is unknown. One hypothesis is that a persistent, difficult-to-detect infection remains. However, human and animal trials have not provided compelling evidence to support this hypothesis.<ref name="marques-2022">{{cite journal |last1=Marques |first1=Adriana |title=Persistent Symptoms After Treatment of Lyme Disease |journal=Infectious Disease Clinics of North America |date=September 2022 |volume=36 |issue=3 |pages=621–638 |doi=10.1016/j.idc.2022.04.004 |pmid=36116839 |pmc=9494579}}</ref> Another hypothesis is that autoimmunity has been triggered by the infection. Auto–immune responses are known to occur following other infections, including ''Campylobacter'' (]), ''Chlamydia'' (reactive arthritis), and strep throat (rheumatic heart disease). A third hypothesis is that debris from | |||
| a previous infection could remain.<ref name="marques-2022"/> | |||
| Another hypothesis is that symptoms are simply unrelated to a Lyme infection.<ref name="CDC_2016">{{cite web |date=3 November 2016 |title=Post-Treatment Lyme Disease Syndrome |url=https://www.cdc.gov/lyme/postLDS/index.html |url-status=dead |archive-url=https://web.archive.org/web/20170617203133/https://www.cdc.gov/lyme/postlds/index.html |archive-date=17 June 2017 |publisher=CDC}}{{PD-notice}}</ref><ref name="Post-treatment Lyme, Rebman">, ''Frontiers in Medicine'' (Lausanne), Alison W Rebman, John N Aucott, PMCID: PMC7052487, Feb. 25, 2020.</ref> Among 13 studies analyzing people who worried about Lyme disease, 47 to 80% had no evidence of Lyme infection while 15 to 55% (median 34%) were able to obtain other diagnoses.<ref name="marques-2022"/> | |||
| There is no proven treatment for Post-treatment Lyme disease syndrome. While short-term antibiotics are effective in early Lyme disease, prolonged antibiotics are not. They have been shown ineffective in placebo-controlled trials and carry the risk of serious, sometimes deadly complications. Generally, treatment is symptomatic and is similar to the management of ] or ]. PTLDS usually gets better over time, but recovery may take many months.<ref name="CDC_2016" /> | |||
| ==Epidemiology== | ==Epidemiology== | ||
| ] | ] | ||
| Lyme disease ] in ] temperate regions.<ref name=Higgins_2004/> An estimated 476,000 people a year are diagnosed and treated for the disease in the United States. This number is probably an overestimate due to overdiagnosis and overtreatment.<ref name="cdc-how-many"/><ref name="cdc-estimate-2021"/> Over 200,000 people a year are diagnosed and treated in Europe.<ref name="comparison-2021" /><ref name=NEJM2014/><ref name=Berg2014>{{cite book| vauthors = Berger S |title=Lyme disease: Global Status 2014 Edition|date=2014|publisher=GIDEON Informatics Inc|isbn=978-1-4988-0343-4|page=7|url=https://books.google.com/books?id=DuKCBQAAQBAJ&pg=PA7|url-status=live|archive-url=https://web.archive.org/web/20170908151350/https://books.google.com/books?id=DuKCBQAAQBAJ&pg=PA7|archive-date=8 September 2017}}</ref> There is a suggestion that tick populations and Lyme disease occurrence are increasing and spreading into new areas, owing in part to the warming temperatures of ]. However, tick-borne disease systems are complex, and determining whether changes are due to climate change or other drivers can be difficult.<ref name="Chrobak"/><ref name="Gilbert">{{cite journal | vauthors = Gilbert L | title = The Impacts of Climate Change on Ticks and Tick-Borne Disease Risk | journal = Annual Review of Entomology | volume = 66 | issue = 1 | pages = 373–388 | date = January 2021 | pmid = 33417823 | doi = 10.1146/annurev-ento-052720-094533 | s2cid = 231300522 | doi-access = free }}</ref> Lyme disease effects are comparable among males and females. A wide range of age groups is affected, though the number of cases is highest among 10- to 19-year-olds. | |||
| Lyme disease is ] in ] temperate regions.<ref name=Higgins_2004/> | |||
| ===Africa=== | ===Africa=== | ||
| In northern Africa, ''B. burgdorferi sensu lato'' has been identified in ], ], ] and ].<ref name=Bouattour_2004/><ref name=Dsouli_2006/><ref name=Helmy_2000/> | In northern Africa, ''B. burgdorferi sensu lato'' has been identified in ], ], ] and ].<ref name=Bouattour_2004/><ref name=Dsouli_2006/><ref name=Helmy_2000/> | ||
| Lyme disease in sub-Saharan Africa is presently unknown, but evidence indicates it may occur in humans in this region. The abundance of hosts and tick vectors would favor the establishment of Lyme infection in Africa.<ref name=Fivaz_1989/> In East Africa, two cases of Lyme disease have been reported in ].<ref name=Jowi_2005/> | Lyme disease in sub-Saharan Africa is presently unknown, but evidence indicates it may occur in humans in this region. The abundance of hosts and tick vectors would favor the establishment of Lyme infection in Africa.<ref name=Fivaz_1989/> In East Africa, two cases of Lyme disease have been reported in ].<ref name=Jowi_2005/> According The Federation of Infectious Diseases Societies of Southern Africa, Lyme disease is not known to be endemic in either South Africa or Mozambique.<ref>{{Cite web | title= Case of the Month | date = December 2015 |url=https://www.fidssa.co.za/news-events/case-2015-dec-issue-12 |access-date=2023-11-02 | work = Federation of Infectious Diseases Societies of Southern Africa (FIDSSA) |language=en}}</ref> | ||
| ===Asia=== | ===Asia=== | ||
| ''B. burgdorferi sensu lato''-infested ticks are being found more frequently in |
''B. burgdorferi sensu lato''-infested ticks are being found more frequently in Japan, as well as in northwest China, ], ] and far eastern Russia.<ref name=Li_1998/><ref name="pmid15623946"/> ''Borrelia'' has also been isolated in ].<ref name=Walder_2006/> | ||
| ===Australia=== | |||
| Lyme disease is not considered endemic to Australia.<ref name="pmid30746341">{{cite journal | vauthors = Dehhaghi M, Kazemi Shariat Panahi H, Holmes EC, Hudson BJ, Schloeffel R, Guillemin GJ | title = Human Tick-Borne Diseases in Australia | journal = Frontiers in Cellular and Infection Microbiology | volume = 9 | issue = | pages = 3 | year = 2019 | pmid = 30746341 | pmc = 6360175 | doi = 10.3389/fcimb.2019.00003 | doi-access = free }}</ref> While there have been reports of people acquiring Lyme disease in Australia, and even evidence of closely related ''Borrelia'' species in ticks,<ref name="pmid35502617">{{cite journal | vauthors = Gofton AW, Blasdell KR, Taylor C, Banks PB, Michie M, Roy-Dufresne E, Poldy J, Wang J, Dunn M, Tachedjian M, Smith I | title = Metatranscriptomic profiling reveals diverse tick-borne bacteria, protozoans and viruses in ticks and wildlife from Australia | journal = Transboundary and Emerging Diseases | volume = 69 | issue = 5 | pages = e2389–e2407 | date = September 2022 | pmid = 35502617 | pmc = 9790515 | doi = 10.1111/tbed.14581 }}</ref> the evidence linking these cases to local transmission is limited. Ongoing research on resolving potential ''Borrelia'' species to Debilitating Symptom Complexes Attributed to Ticks (DSCATT) in Australia are ongoing.<ref name="pmid36365042">{{cite journal | vauthors = Barbosa AD, Long M, Lee W, Austen JM, Cunneen M, Ratchford A, Burns B, Kumarasinghe P, Ben-Othman R, Kollmann TR, Stewart CR, Beaman M, Parry R, Hall R, Tabor A, O'Donovan J, Faddy HM, Collins M, Cheng AC, Stenos J, Graves S, Oskam CL, Ryan UM, Irwin PJ | title = The Troublesome Ticks Research Protocol: Developing a Comprehensive, Multidiscipline Research Plan for Investigating Human Tick-Associated Disease in Australia | journal = Pathogens | volume = 11 | issue = 11 | page = 1290 | date = November 2022 | pmid = 36365042 | pmc = 9694322 | doi = 10.3390/pathogens11111290 | doi-access = free }}</ref> | |||
| ===Europe=== | ===Europe=== | ||
| In Europe, Lyme disease is caused by infection with one or more pathogenic European genospecies of the spirochaete ''B. burgdorferi sensu lato'', mainly transmitted by the tick ''Ixodes ricinus''.<ref name="pmid21794218"/> Cases of ''B. burgdorferi sensu lato''-infected ticks are found predominantly in central Europe, particularly in ] and |
In Europe, Lyme disease is caused by infection with one or more pathogenic European genospecies of the spirochaete ''B. burgdorferi sensu lato'', mainly transmitted by the tick '']''.<ref name="pmid21794218"/> Cases of ''B. burgdorferi sensu lato''-infected ticks are found predominantly in central Europe, particularly in ] and Austria, but have been isolated in almost every country on the continent.<ref name="pmid16819127"/> The number of cases in southern Europe, such as Italy and Portugal, is much lower.<ref name="pmid17130658"/> Diagnosed cases in some Western countries, such as Iceland, are rising.<ref>{{cite journal | vauthors = Vandekerckhove O, De Buck E, Van Wijngaerden E | title = Lyme disease in Western Europe: an emerging problem? A systematic review | journal = Acta Clinica Belgica | volume = 76 | issue = 3 | pages = 244–252 | date = June 2021 | pmid = 31739768 | doi = 10.1080/17843286.2019.1694293 | s2cid = 208170787 }}</ref> Lyme disease is rare in Iceland. On average around 6 to 7 cases are diagnosed every year, primarily localised infections presenting as erythema migrans. None of the cases had a definitive Icelandic origin and the yearly number of cases has not been increasing.<ref>{{cite journal | vauthors = Vigfusson HB, Hardarson HS, Ludviksson BR, Gudlaugsson O | title = | journal = Laeknabladid | volume = 105 | issue = 2 | pages = 63–70 | date = February 2019 | pmid = 30713153 | doi = 10.17992/lbl.2019.02.215 | s2cid = 73424569 | doi-access = free }}</ref> | ||
| ====United Kingdom==== | ====United Kingdom==== | ||
| In the |
In the United Kingdom the number of laboratory-confirmed cases of Lyme disease has been rising steadily since voluntary reporting was introduced in 1986<ref name=hpaEpidemiology/> when 68 cases were recorded in the UK and Ireland combined.<ref name=Muhlemann_1987/> In the UK there were 23 confirmed cases in 1988 and 19 in 1990,<ref name=hansard1991/> but 973 in 2009<ref name=hpaEpidemiology /> and 953 in 2010.<ref name=hpa5-15/> Provisional figures for the first 3 quarters of 2011 show a 26% increase on the same period in 2010.<ref name=disease_action_2011/> | ||
| It is thought, however, that the actual number of cases is significantly higher than suggested by the above figures, with |
It is thought, however, that the actual number of cases is significantly higher than suggested by the above figures, with England's ] estimating that there are between 2,000 and 3,000 cases in England and Wales per year<ref name=hpa5-15 /> (with an average of around 15% of the infections acquired overseas<ref name=hpaEpidemiology />), while Dr Darrel Ho-Yen, Director of the Scottish Toxoplasma Reference Laboratory and National Lyme Disease Testing Service, believes that the number of confirmed cases should be multiplied by 10 "to take account of wrongly diagnosed cases, tests giving false results, sufferers who weren't tested, people who are infected but not showing symptoms, failures to notify and infected individuals who don't consult a doctor."<ref name=cassidy_2011/><ref name=danger_2009/> | ||
| Despite Lyme disease (Borrelia burgdorferi infection) being a ] in Scotland<ref name=scotland_2012/> since January 1990<ref name=hansard_1997/> which should therefore be reported on the basis of clinical suspicion, it is believed that many ] are unaware of the requirement.<ref name=fox_2010/> Mandatory reporting, limited to laboratory test results only, was introduced throughout the UK in October 2010, under the Health Protection (Notification) Regulations 2010.<ref name=hpaEpidemiology /> | Despite Lyme disease (''Borrelia burgdorferi'' infection) being a ] in Scotland<ref name=scotland_2012/> since January 1990<ref name=hansard_1997/> which should therefore be reported on the basis of clinical suspicion, it is believed that many ] are unaware of the requirement.<ref name=fox_2010/> Mandatory reporting, limited to laboratory test results only, was introduced throughout the UK in October 2010, under the Health Protection (Notification) Regulations 2010.<ref name=hpaEpidemiology /> | ||
| Although there is a greater |
Although there is a greater number of cases of Lyme disease in the ], ], ], the ], parts of ] and ], ]<ref name=hpa_2013/> and the West coast and islands of Scotland,<ref name=defra_2009/> infected ticks are widespread and can even be found in the parks of London.<ref name=hansard1991 /><ref name=tick_bite/> A 1989 report found that 25% of forestry workers in the New Forest were ], as were between 2% and 4–5% of the general local population of the area.<ref name="pmid8037992"/><ref name="pmid2563850"/> | ||
| Tests on pet dogs |
Tests on pet dogs carried out throughout the country in 2009 indicated that around 2.5% of ticks in the UK may be infected, considerably higher than previously thought.<ref name=Smith_2012/><ref name=bbc_dogs_2012/> It is speculated that ] may lead to an increase in tick activity in the future, as well as an increase in the amount of time that people spend in public parks, thus increasing the risk of infection.<ref name=londong_2008/> However no published research has proven this to be so. | ||
| ===North America=== | ===North America=== | ||
| Many studies in North America have examined ecological and environmental correlates of Lyme disease |
Many studies in North America have examined ecological and environmental correlates of the number of people affected by Lyme disease. A 2005 study using climate suitability modelling of ''I. scapularis'' projected that ] an overall 213% increase in suitable vector habitat by 2080, with northward expansions in Canada, increased suitability in the central U.S., and decreased suitable habitat and vector retraction in the southern U.S.<ref name=Brownstein_etal_2005>{{cite journal | vauthors = Brownstein JS, Holford TR, Fish D | title = Effect of Climate Change on Lyme Disease Risk in North America | journal = EcoHealth | volume = 2 | issue = 1 | pages = 38–46 | date = March 2005 | pmid = 19008966 | pmc = 2582486 | doi = 10.1007/s10393-004-0139-x }}</ref> A 2008 review of published studies concluded that the presence of forests or forested areas was the only variable that consistently elevated the risk of Lyme disease whereas other environmental variables showed little or no concordance between studies.<ref name=Killilea_etal_2008>{{cite journal | vauthors = Killilea ME, Swei A, Lane RS, Briggs CJ, Ostfeld RS | title = Spatial dynamics of lyme disease: a review | journal = EcoHealth | volume = 5 | issue = 2 | pages = 167–195 | date = June 2008 | pmid = 18787920 | doi = 10.1007/s10393-008-0171-3 | url = http://www.caryinstitute.org/sites/default/files/public/reprints/2008_Killilea_EcoHealth_Spatial_Dynamics.pdf | url-status = live | s2cid = 13545850 | citeseerx = 10.1.1.580.8928 | archive-url = https://web.archive.org/web/20150908101635/http://www.caryinstitute.org/sites/default/files/public/reprints/2008_Killilea_EcoHealth_Spatial_Dynamics.pdf | archive-date = 8 September 2015 }}</ref> The authors argued that the factors influencing tick density and human risk between sites are still poorly understood, and that future studies should be conducted over longer time periods, become more standardized across regions, and incorporate existing knowledge of regional Lyme ].<ref name=Killilea_etal_2008/> | ||
| ====Canada==== | ====Canada==== | ||
| The range of ticks able to carry Lyme disease has expanded from a limited area of Ontario to include areas of southern Quebec, Manitoba, northern Ontario, southern New Brunswick, southwest Nova Scotia and limited parts of Saskatchewan and Alberta, as well as British Columbia. Cases have been reported as far east as the island of Newfoundland.<ref name=canada_lyme_map/><ref name=min_ag_2012/><ref name=fact_sheet_2012/><ref name=Ogden_2009/> A model-based prediction by Leighton ''et al.'' (2012) suggests that the range of the ''I. scapularis'' tick will expand into Canada by 46 km/year over the next decade, with warming climatic temperatures as the main driver of increased speed of spread.<ref name=Leighton_2012/> | |||
| ====Mexico==== | ====Mexico==== | ||
| Line 250: | Line 321: | ||
| ====United States==== | ====United States==== | ||
| ] map showing the risk of Lyme disease in the United States, particularly its concentration in the ] and western ] |
] map showing the risk of Lyme disease in the United States, particularly its concentration in the ] and western ]]] | ||
| Lyme disease is the most common tick-borne disease in North America and Europe, and one of the fastest-growing infectious diseases in the United States. Of cases reported to the United States CDC, the ratio of Lyme disease infection is 7.9 cases for every 100,000 persons. In the ten states where Lyme disease is most common, the average was 31.6 cases for every 100,000 persons for the year 2005.<ref name=cdc_stats_2012/><ref name=mmwr_2007/><ref name=Bacon_2008/> | Lyme disease is the most common tick-borne disease in North America and Europe, and one of the fastest-growing infectious diseases in the United States. Of cases reported to the United States CDC, the ratio of Lyme disease infection is 7.9 cases for every 100,000 persons. In the ten states where Lyme disease is most common, the average was 31.6 cases for every 100,000 persons for the year 2005.<ref name=cdc_stats_2012/><ref name=mmwr_2007/><ref name=Bacon_2008/> | ||
| Although Lyme disease has been reported in all states |
Although Lyme disease has been reported in all states due to travel-associated infections, about 99% of all reported cases are confined to just five geographic areas (New England, Mid-Atlantic, East-North Central, South Atlantic, and West North-Central).<ref name=CDC-FAQ/><ref name=cdc_stats2/><ref name="nytimes.com"/> CDC implemented national surveillance of Lyme disease cases in 1991. Since then, reporting criteria has been modified multiple times.<ref name="cdc-surveillance">{{cite web |title=National Notifiable Diseases Surveillance System (NNDSS) - Lyme Disease |url=https://ndc.services.cdc.gov/conditions/lyme-disease/ |website=Centers for Disease Control and Prevention |access-date=11 January 2023 |date=7 September 2021}}</ref> The 2022 surveillance case definition classifies cases as confirmed, probable, and suspect.<ref name="cdc-surveillance-2022">{{cite web |title=Lyme Disease (Borrelia burgdorferi) 2022 Case Definition |url=https://ndc.services.cdc.gov/case-definitions/lyme-disease-2022/ |website=Centers for Disease Control and Prevention |access-date=11 January 2023 |date=12 August 2022}}</ref> The number of reported cases of the disease has been increasing, as are endemic regions in North America. | ||
| The CDC emphasizes that, while surveillance data has limitations, it is useful due to "uniformity, simplicity, and timeliness." While cases are under-reported in high-incidence areas, over-reporting is likely in low-incidence areas. Additionally, surveillance cases are reported by county of residence and not where an infection was necessarily contracted.<ref name="cdc-surveillance-faq">{{cite web |title=Lyme disease surveillance and available data |url=https://www.cdc.gov/lyme/stats/survfaq.html |website=Centers for Disease Control and Prevention |access-date=11 January 2023 |language=en-us |date=15 November 2022}}</ref><ref name=CDC-FAQ/> | |||
| Effective January 2008, the CDC gives equal weight to laboratory evidence from 1) a positive culture for ''B. burgdorferi''; 2) two-tier testing (] screening and ] confirming); or 3) single-tier ] (old infection) Western blot.<ref name=cdc_surveil_2008/> Previously, the CDC only included laboratory evidence based on (1) and (2) in their surveillance case definition. The case definition now includes the use of Western blot without prior ELISA screen.<ref name=cdc_surveil_2008/> | |||
| Several similar but apparently distinct conditions may exist, caused by various species or subspecies of ''Borrelia'' in North America. A regionally restricted condition that may be related to ''Borrelia'' infection is ] (STARI), also known as Masters disease. '']'', known commonly as the lone-star tick, is recognized as the primary vector for STARI. In some parts of the geographical distribution of STARI, Lyme disease is quite rare (e.g., Arkansas), so people in these regions experiencing Lyme-like symptoms—especially if they follow a bite from a lone-star tick—should consider STARI as a possibility. It is generally a milder condition than Lyme and typically responds well to antibiotic treatment.<ref>{{Cite web|url=https://www.cdc.gov/stari/disease/index.html|title=STARI or Lyme?|date=19 November 2018|website=Centers for Disease Control and Prevention|url-status=live|archive-url=https://web.archive.org/web/20191112160112/https://www.cdc.gov/stari/disease/index.html|archive-date=12 November 2019}}</ref> | |||
| The number of reported cases of the disease has been increasing, as are endemic regions in North America. For example, ''B. burgdorferi sensu lato'' was previously thought to be hindered in its ability to be maintained in an ] cycle in ], because it was assumed the large lizard population would dilute the prevalence of ''B. burgdorferi'' in local tick populations; this has since been brought into question, as some evidence has suggested lizards can become infected.<ref name="pmid17417956" /> | |||
| In recent years there have been 5 to 10 cases a year of a disease similar to Lyme occurring in Montana. It occurs primarily in pockets along the ] in central Montana. People have developed a red bull's-eye rash around a tick bite followed by weeks of fatigue and a fever.<ref name="nytimes.com"/> | |||
| Except for one study in Europe,<ref name="pmid16820453"/> much of the data implicating lizards is based on DNA detection of the spirochete and has not demonstrated lizards are able to infect ticks feeding upon them.<ref name="pmid17417956"/><ref name="pmid17626342"/><ref name="pmid17427701"/><ref name="pmid17326941"/> As some experiments suggest lizards are refractory to infection with ''Borrelia'', it appears likely their involvement in the enzootic cycle is more complex and species-specific.<ref name="pmid16995383"/> | |||
| ===South America=== | |||
| While ''B. burgdorferi'' is most associated with ticks hosted by ] and ], ''Borrelia afzelii'' is most frequently detected in rodent-feeding vector ticks, and ''Borrelia garinii'' and ''Borrelia valaisiana'' appear to be associated with birds. Both rodents and birds are competent reservoir hosts for ''B. burgdorferi sensu stricto''. The resistance of a genospecies of Lyme disease spirochetes to the bacteriolytic activities of the alternative complement pathway of various host species may determine its reservoir host association.{{citation needed|date=March 2013}} | |||
| In Brazil, Lyme disease is not considered endemic.<ref name="BYS-2024"/> A Lyme-like disease known as ] has been described, attributed to microorganisms that do not belong to the ''B. burgdorferi sensu lato'' complex and transmitted by ticks of the '']'' and '']'' genera.<ref name=Mantovani_2007/> The first reported case of BYS in Brazil was made in 1992 in ], São Paulo.<ref name=Yoshinari_1993/> A 2024 analysis concluded that evidence to connect BYS to ''Borrelia'' bacteria was lacking.<ref name="BYS-2024">{{cite journal |last1=Labruna |first1=Marcelo B. |last2=Faccini-Martínez |first2=Álvaro A. |last3=Muñoz-Leal |first3=Sebastián |last4=Szabó |first4=Matias P. J. |last5=Angerami |first5=Rodrigo N. |title=Lyme borreliosis in Brazil: a critical review on the Baggio–Yoshinari syndrome (Brazilian Lyme-like disease) |journal=Clinical Microbiology Reviews |date=4 November 2024 |pages=e0009724 |doi=10.1128/cmr.00097-24|pmid=39494872 }}</ref> | |||
| == Etymology == | |||
| Several similar but apparently distinct conditions may exist, caused by various species or subspecies of ''Borrelia'' in North America. A regionally restricted condition that may be related to ''Borrelia'' infection is ] (STARI), also known as Masters' disease. '']'', known commonly as the lone-star tick, is recognized as the primary vector for STARI. In some parts of the geographical distribution of STARI, Lyme disease is quite rare (e.g., Arkansas), so patients in these regions experiencing Lyme-like symptoms—especially if they follow a bite from a lone-star tick—should consider STARI as a possibility. It is generally a milder condition than Lyme and typically responds well to antibiotic treatment.{{citation needed|date=March 2013}} | |||
| Lyme disease was diagnosed as a separate condition for the first time in 1975 in ].<ref>{{cite book| vauthors = Murray P |title=The Widening Circle : A Lyme Disease Pioneer Tells Her Story|date=1006|publisher=St. Martin's Press|location=New York|isbn=978-0-312-14068-7}}</ref> | |||
| Although Montana is the only state that has not reported a confirmed case of Lyme disease, in recent years there have been 5 to 10 cases a year of a disease similar to Lyme. It occurs primarily in pockets along the ] in central Montana. People have developed a red bull's-eye rash around a tick bite followed by weeks of fatigue and a fever.<ref name="nytimes.com"/> | |||
| Lyme disease prevalence is comparable among males and females. A wide range of age groups is affected, though the number of cases is highest among 10–19-year-olds. For unknown reasons, Lyme disease is seven times more common among Asians.<ref name=vox_facts/> | |||
| ===South America=== | |||
| In ], tick-borne disease recognition and occurrence is rising. Ticks carrying ''B. burgdorferi sensu lato'', as well as canine and human tick-borne disease, have been reported widely in ], but the subspecies of ''Borrelia'' has not yet been defined.<ref name=Mantovani_2007/> The first reported case of Lyme disease in Brazil was made in 1993 in ].<ref name=Yoshinari_1993/> ''B. burgdorferi sensu stricto'' antigens in patients have been identified in ] and ].{{Citation needed|date=February 2012}} | |||
| ==History== | ==History== | ||
| The evolutionary history of ''Borrelia burgdorferi'' genetics has been the subject of recent studies. One study has found that prior to the ] that accompanied post colonial farm abandonment in ] and the wholesale migration into the ] that occurred during the early 19th century, Lyme disease was present for thousands of years in America and had spread along with its tick hosts from the Northeast to the Midwest.<ref name=Hoen_2009/> | |||
| The earliest known evidence of Lyme disease was found in ], a 5300 year old mummy in the ] near the Italian border.<ref>{{Cite journal |last=Wynne Parry |date=2012-02-28 |title=Iceman Mummy May Hold Earliest Evidence of Lyme Disease |url=https://www.livescience.com/18704-oldest-case-lyme-disease-spotted-iceman-mummy.html |journal=Live Science |language=en}}</ref> | |||
| John Josselyn, who visited New England in 1638 and again from 1663–1670, wrote "there be infinite numbers of tikes hanging upon the bushes in summer time that will cleave to man's garments and creep into his breeches eating themselves in a short time into the very flesh of a man. I have seen the stockins of those that have gone through the woods covered with them."<ref name=Josselyn_1670/> | |||
| The evolutionary history of ''Borrelia burgdorferi'' genetics has been examined by scientists. One study has found that prior to the ] that accompanied post-colonial farm abandonment in ] and the wholesale migration into the ] that occurred during the early 19th century, Lyme disease had been present for thousands of years in America and had spread along with its tick hosts from the Northeast to the Midwest.<ref name=Hoen_2009/> | |||
| John Josselyn, who visited New England in 1638 and again from 1663 to 1670, wrote "there be infinite numbers of ticks hanging upon the bushes in summertime that will cleave to man's garments and creep into his breeches, eating themselves in a short time into the very flesh of a man. I have seen the stockings of those that have gone through the woods covered with them."<ref name=Josselyn_1670/> | |||
| This is also confirmed by the writings of ], a Swedish botanist who was sent to America by ], and who found the forests of New York "abound" with ticks when he visited in 1749. When Kalm's journey was retraced 100 years later, the forests were gone and the Lyme bacterium had probably become isolated to a few pockets along the northeast coast, Wisconsin, and Minnesota.<ref name=Drymon_2008/> | |||
| This is also confirmed by the writings of ], a Swedish botanist who was sent to America by ], and who found the forests of New York "abound" with ticks when he visited in 1749. When Kalm's journey was retraced 100 years later, the forests were gone and the Lyme bacterium had probably become isolated to a few pockets along the northeast coast, Wisconsin, and Minnesota.<ref name=Drymon_2008/> | |||
| Perhaps the first detailed description of what is now known as Lyme disease appeared in the writings of ] after a visit to the ] (Deer Island) off the west coast of Scotland in 1764.<ref name=summerton_1995/> He gives a good description both of the symptoms of Lyme disease (with "exquisite pain the interior parts of the limbs") and of the tick vector itself, which he describes as a "worm" with a body which is "of a reddish colour and of a compressed shape with a row of feet on each side" that "penetrates the skin". Many people from this area of Great Britain immigrated to North America between 1717 and the end of the 18th century. | |||
| Perhaps the first detailed description of what is now known as Lyme disease appeared in the writings of ] after a visit to the island of ] (Deer Island) off the west coast of Scotland in 1764.<ref name=summerton_1995/> He gives a good description both of the symptoms of Lyme disease (with "exquisite pain the interior parts of the limbs") and of the tick vector itself, which he describes as a "worm" with a body which is "of a reddish color and of a compressed shape with a row of feet on each side" that "penetrates the skin". Many people from this area of Great Britain emigrated to North America between 1717 and the end of the 18th century.<ref>{{Cite web |title=US Voyage New World |url=https://www.ulsterscotsagency.com/fs/doc/new_range_of_ulster-scots_booklets/US_Voyage_New_World_BK7_AW_3.pdf |access-date=May 1, 2024 |website=www.ulsterscotsagency.com}}</ref> | |||
| The examination of preserved museum specimens has found ''Borrelia'' DNA in an infected '']'' tick from Germany that dates back to 1884, and from an infected mouse from Cape Cod that died in 1894.<ref name=Drymon_2008/> The 2010 autopsy of ], a 5,300-year-old ], revealed the presence of the DNA sequence of ''Borrelia burgdorferi'' making him the earliest known human with Lyme disease.<ref name="ngautopsy"/> | The examination of preserved museum specimens has found ''Borrelia'' DNA in an infected '']'' tick from Germany that dates back to 1884, and from an infected mouse from Cape Cod that died in 1894.<ref name=Drymon_2008/> The 2010 autopsy of ], a 5,300-year-old ], revealed the presence of the DNA sequence of ''Borrelia burgdorferi'' making him the earliest known human with Lyme disease.<ref name="ngautopsy"/> | ||
| The early European studies of what is now known as Lyme disease described its skin manifestations. The first study dates to 1883 in ], Germany (now ], |
The early European studies of what is now known as Lyme disease described its skin manifestations. The first study dates to 1883 in ], Germany (now ], Poland), where physician Alfred Buchwald described a man who for 16 years had had a degenerative ] now known as ].<ref name="Afzelius1910"/> | ||
| ===20th century=== | |||
| At a 1909 research conference, Swedish dermatologist ] presented a study about an expanding, ring-like lesion he had observed in an older woman following the bite of a sheep tick. He named the lesion ''erythema migrans''.<ref name="Afzelius1910" /> The skin condition now known as ] was first described in 1911.<ref name=burckhardt_1911/> | At a 1909 research conference, Swedish dermatologist ] presented a study about an expanding, ring-like lesion he had observed in an older woman following the bite of a sheep tick. He named the lesion ''erythema migrans''.<ref name="Afzelius1910" /> The skin condition now known as ] was first described in 1911.<ref name=burckhardt_1911/> | ||
| The modern history of medical understanding of the disease, including its cause, diagnosis, and treatment, has been difficult.<ref name=Edlow_2003/> | |||
| Neurological problems following tick bites were recognized starting in the 1920s. French physicians Garin and Bujadoux described a farmer with a painful sensory ] accompanied by mild ] following a tick bite. A large, ring-shaped rash was also noted, although the doctors did not relate it to the meningoradiculitis. In 1930, the Swedish dermatologist Sven Hellerström was the first to propose EM and neurological symptoms following a tick bite were related.<ref name=hellerstrom_1930/> In the 1940s, German neurologist ] described several cases of chronic lymphocytic meningitis and polyradiculoneuritis, some of which were accompanied by erythematous skin lesions. | Neurological problems following tick bites were recognized starting in the 1920s. French physicians Garin and Bujadoux described a farmer with a painful sensory ] accompanied by mild ] following a tick bite. A large, ring-shaped rash was also noted, although the doctors did not relate it to the meningoradiculitis. In 1930, the Swedish dermatologist Sven Hellerström was the first to propose EM and neurological symptoms following a tick bite were related.<ref name=hellerstrom_1930/> In the 1940s, German neurologist ] described several cases of chronic lymphocytic meningitis and polyradiculoneuritis, some of which were accompanied by erythematous skin lesions. | ||
| Carl Lennhoff, who worked at the ] in Sweden, believed many skin conditions were caused by spirochetes. In 1948, he |
Carl Lennhoff, who worked at the ] in Sweden, believed many skin conditions were caused by spirochetes. In 1948, he published on his use of a special stain to microscopically observe what he believed were spirochetes in various types of skin lesions, including EM.<ref name=lenhoff_1948/> Although his conclusions were later shown to be erroneous, interest in the study of spirochetes was sparked.{{Citation needed|date=May 2024}} Starting in 1946, facilities in Sweden experimented with treating EM rashes with substances known to kill spirochetes.<ref name="hollstrom-1951">{{cite journal |last1=Hollström |first1=Einar |title=Successful treatment of erythema migrans Afzelius. |journal=Acta Dermato-venereologica |date=1951 |volume=31 |issue=2 |pages=235–43 |doi=10.2340/0001555531235243 |doi-broken-date=1 November 2024 |pmid=14829185 |url=https://www.medicaljournals.se/acta/content_files/files/pdf/31/2/31235243.pdf}}</ref> {{ill|Einar Hollström|sv}} reported that "penicillin was found to be the most effective."<ref name="hollstrom-1958">{{cite journal |last1=Hollström |first1=Einar |title=Penicillin Treatment of erythema chronicum migrans afzelius |journal=Acta Dermato-Venereologica |date=1958 |volume=38 |issue=5 |doi=10.2340/0001555538285289|doi-broken-date=1 November 2024 |url=https://www.medicaljournals.se/acta/content_files/files/pdf/38/5/38285289.pdf}}</ref> In 1949, Nils Thyresson, who also worked at the Karolinska Institute, was the first to treat ACA with penicillin.<ref name="pmid18140373"/> In the 1950s, the relationship among tick bite, lymphocytoma, EM and Bannwarth's syndrome was recognized throughout Europe leading to the widespread use of ] for treatment in Europe.<ref name=Bianchi_1950/><ref name=Paschoud_1954/> | ||
| In 1970 |
In 1970 a dermatologist in ] named Rudolph Scrimenti recognized an EM lesion in a person after recalling a paper by Hellerström that had been reprinted in an American science journal in 1950. This was the first documented case of EM in the United States. Based on the European literature, he treated the person with penicillin.<ref name=Scrimenti_1970/> | ||
| The full ] now known as Lyme disease was not recognized until a cluster of cases originally thought to be ] was identified in three towns in southeastern ] in 1975, including the towns ] and ], which gave the disease its popular name.<ref name= |
The full ] now known as Lyme disease was not recognized until a cluster of cases originally thought to be ] was identified in three towns in southeastern ] in 1975, including the towns ] and ], which gave the disease its popular name.<ref name=Borchers2015>{{cite journal | vauthors = Borchers AT, Keen CL, Huntley AC, Gershwin ME | title = Lyme disease: a rigorous review of diagnostic criteria and treatment | journal = Journal of Autoimmunity | volume = 57 | pages = 82–115 | date = February 2015 | pmid = 25451629 | doi = 10.1016/j.jaut.2014.09.004 }}</ref> This was investigated by physicians David Snydman and ] of the ], and by others from ], including ], who is credited as a co-discover of the disease.<ref name=hcourant>{{cite news| vauthors = Weir W |title=Lyme Disease Pioneer Stephen Malawista Dies|url=https://www.courant.com/2013/09/19/lyme-disease-pioneer-stephen-malawista-dies/|work=]|date=19 September 2013|access-date=14 October 2013|url-status=live|archive-url=https://web.archive.org/web/20131014173239/http://articles.courant.com/2013-09-19/health/hc-malawista-lyme-0920-20130919_1_lyme-disease-rheumatology-department-disease-control|archive-date=14 October 2013}}</ref> The recognition that the people in the United States had EM led to the recognition that "Lyme arthritis" was one manifestation of the same tick-borne condition known in Europe.<ref name=Sternbach/> | ||
| Before 1976, elements of ''B. burgdorferi sensu lato'' infection were called or known as tick-borne meningopolyneuritis, Garin-Bujadoux syndrome, Bannwarth syndrome, Afzelius' disease,<ref name="Bolognia"/> ] or sheep tick fever. Since 1976 the disease is most often referred to as Lyme disease,<ref name=Mast_1976/><ref name=Steere_1977/> Lyme borreliosis or simply borreliosis.{{ |
Before 1976, the elements of ''B. burgdorferi sensu lato'' infection were called or known as tick-borne meningopolyneuritis, Garin-Bujadoux syndrome, Bannwarth syndrome, Afzelius's disease,<ref name="Bolognia"/> ] or sheep tick fever. Since 1976 the disease is most often referred to as Lyme disease,<ref name=Mast_1976/><ref name=Steere_1977/> Lyme borreliosis or simply borreliosis.<ref>{{Cite web|url=https://www.ecdc.europa.eu/en/borreliosis/facts/factsheet|title=Factsheet about Borreliosis|website=European Centre for Disease Prevention and Control|date=17 June 2017 |language=en|access-date=30 January 2020|archive-url=https://web.archive.org/web/20190927011644/https://ecdc.europa.eu/en/borreliosis/facts/factsheet|archive-date=27 September 2019|url-status=live}}</ref><ref>{{Cite web|url=https://www.who.int/ith/diseases/lyme/en/|title=WHO {{!}} Lyme Borreliosis (Lyme disease)|website=WHO|access-date=30 January 2020|archive-url=https://web.archive.org/web/20191129114243/https://www.who.int/ith/diseases/lyme/en/|archive-date=29 November 2019|url-status=dead}}</ref> | ||
| In 1980, Steere, ''et al.'', began to test ] regimens in |
In 1980, Steere, ''et al.'', began to test ] regimens in adults with Lyme disease.<ref name=Steere_1983/> In the same year, New York State Health Dept. epidemiologist ] provided ], a researcher at the ], with collections of ''I. dammini'' from Shelter Island, New York, a known Lyme-endemic area as part of an ongoing investigation of Rocky Mountain spotted fever. In examining the ticks for rickettsiae, Burgdorfer noticed "poorly stained, rather long, irregularly coiled spirochetes." Further examination revealed spirochetes in 60% of the ticks. Burgdorfer credited his familiarity with the European literature for his realization that the spirochetes might be the "long-sought cause of ECM and Lyme disease." Benach supplied him with more ticks from Shelter Island and ] from people diagnosed with Lyme disease. University of Texas Health Science Center researcher Alan Barbour "offered his expertise to culture and immunochemically characterize the organism." Burgdorfer subsequently confirmed his discovery by isolating, from people with Lyme disease, spirochetes identical to those found in ticks.<ref name=Burgdorfer_1984/> In June 1982, he published his findings in ], and the spirochete was named ''Borrelia burgdorferi'' in his honor.<ref name=Burgdorfer_1982/> | ||
| After the identification of ''B. burgdorferi'' as the causative agent of Lyme disease, antibiotics were selected for testing, guided by ''in vitro'' antibiotic sensitivities, including ], ], ], intravenous and intramuscular penicillin and intravenous ].<ref name=Luft_1988/><ref name=Dattwyler_1990/> The mechanism of tick transmission was also the subject of much discussion. ''B. burgdorferi'' spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.<ref name=Ribeiro_1987/> | After the identification of ''B. burgdorferi'' as the causative agent of Lyme disease, antibiotics were selected for testing, guided by ''in vitro'' antibiotic sensitivities, including ], ], ], intravenous and intramuscular penicillin and intravenous ].<ref name=Luft_1988/><ref name=Dattwyler_1990/> The mechanism of tick transmission was also the subject of much discussion. ''B. burgdorferi'' spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.<ref name=Ribeiro_1987/> | ||
| ==Society, culture, and controversy== | |||
| Jonathan Edlow, Professor of Medicine at Harvard Medical School, quotes the late Ed Masters (discoverer of ], a Lyme-like illness) in his book ''Bull's-Eye'', on the history of Lyme disease. Edlow writes: | |||
| ===Landscape changes and urbanization=== | |||
| Urbanization and other ] factors can be implicated in the spread of Lyme disease to humans. In many areas, expansion of suburban neighborhoods has led to gradual deforestation of surrounding wooded areas and increased border contact between humans and tick-dense areas. Human expansion has also resulted in a reduction of predators that hunt deer as well as mice, chipmunks and other small rodents—the primary reservoirs for Lyme disease. As a consequence of increased human contact with host and ], the likelihood of transmission of the disease has greatly increased.<ref name="The ecology of infectious disease"/><ref name="Patz"/> Researchers are investigating possible links between ] and the spread of vector-borne diseases, including Lyme disease.<ref name="Khasnis"/> | |||
| ===The dilution effect=== | |||
| Given these habitat-host dynamics, in 2003 some researchers began to postulate whether the so called dilution effect could mitigate the spread of Lyme disease.<ref name="The ecology of infectious disease"/> The dilution effect is a hypothesis that predicts that an increase in host biodiversity will result in a decrease in the number of vectors infected with ''B. burgdorferi''.<ref name="The ecology of infectious disease"/> Scientific research has shown that nymphal infection prevalence (NIP) decreases as the number of host species increases, supporting the dilution effect.<ref name="The ecology of infectious disease"/> That said, there is no direct relationship between decreased NIP and decreased epidemiological risk, as this has yet to be proven.<ref name="The ecology of infectious disease"/> Additionally, as of 2018, the dilution effect is only supported in the Northeastern United States, and has been disproved in other parts of the world that also experience high Lyme disease incidence rates <ref>{{cite journal | vauthors = Ruyts SC, Landuyt D, Ampoorter E, Heylen D, Ehrmann S, Coipan EC, Matthysen E, Sprong H, Verheyen K | title = Low probability of a dilution effect for Lyme borreliosis in Belgian forests | journal = Ticks and Tick-Borne Diseases | volume = 9 | issue = 5 | pages = 1143–1152 | date = July 2018 | pmid = 29716838 | doi = 10.1016/j.ttbdis.2018.04.016 | publisher = Ticks and Tick-Borne Diseases. | s2cid = 13746169 }}</ref> | |||
| ===Chronic Lyme disease=== | |||
| {{quote|Masters points out that the "track record" of the "conventional wisdom" regarding Lyme disease is not very good: "First off, they said it was a new disease, which it wasn't. Then it was thought to be viral, but it isn't. Then it was thought that sero-negativity didn't exist, which it does. They thought it was easily treated by short courses of antibiotics, which sometimes it isn't. Then it was only the ''Ixodes dammini'' tick, which we now know is not even a separate valid tick species. If you look throughout the history, almost every time a major dogmatic statement has been made about what we 'know' about this disease, it was subsequently proven wrong or underwent major modifications."<ref name=Edlow_2003/>}} | |||
| {{main|Chronic Lyme disease}} | |||
| The term "chronic Lyme disease" is controversial and not recognized in the medical literature,<ref name="nejm-feder"/> and most medical authorities advise against long-term antibiotic treatment for Lyme disease.<ref name="idsa guideline"/><ref name="pmid17522387"/><ref name="nih-cld"/> Studies have shown that most people diagnosed with "chronic Lyme disease" either have no objective evidence of previous or current infection with '']'' or are people who should be classified as having post-treatment Lyme disease syndrome (PTLDS), which is defined as continuing or relapsing ] (such as fatigue, musculoskeletal pain, and cognitive complaints) in a person previously treated for Lyme disease.<ref name="Marques"/> | |||
| ==Society and culture== | |||
| ] and other ] factors can be implicated in the spread of Lyme disease to humans. In many areas, expansion of suburban neighborhoods has led to gradual deforestation of surrounding wooded areas and increased border contact between humans and tick-dense areas. Human expansion has also resulted in reduction of predators that hunt deer as well as mice, chipmunks and other small rodents—the primary reservoirs for Lyme disease. As a consequence of increased human contact with host and ], the likelihood of transmission of the disease has greatly increased.<ref name="LoGiudice"/><ref name="Patz"/> Researchers are investigating possible links between ] and the spread of vector-borne diseases, including Lyme disease.<ref name="Khasnis"/> | |||
| The 2008 documentary '']'' is known for promoting controversial and unrecognized theories about "chronic Lyme disease".<ref name="under-our-skin-sbm">{{cite web | vauthors = MacBeth B |title=A Review of Under Our Skin, A Cult Classic |url=https://sciencebasedmedicine.org/a-review-of-under-our-skin-a-cult-classic/ |website=Science-Based Medicine |access-date=10 September 2021 |date=8 April 2019}}</ref> | |||
| ==={{Anchor|CHRONIC}} Controversy over term "chronic Lyme disease" === | |||
| {{main|Lyme disease controversy}} | |||
| The term "chronic Lyme disease" is controversial and not recognized in the medical literature,<ref name="nejm-feder"/> and most medical authorities advise against long-term antibiotic treatment for Lyme disease.<ref name="idsa guideline"/><ref name="pmid17522387"/><ref name="nih-cld"/> Studies have shown that most patients diagnosed with “chronic Lyme disease” either have no objective evidence of previous or current infection with '']'' or are patients who should be classified as having post-treatment Lyme disease syndrome(PTLDS), which is defined as continuing or relapsing non-specific symptoms (such as fatigue, musculoskeletal pain, and cognitive complaints) in a patient previously treated for Lyme disease.<ref name="Marques"/> | |||
| ==Other animals== | ==Other animals== | ||
| === Dogs === | |||
| Prevention of Lyme disease is an important step in keeping dogs safe in endemic areas. Prevention education and a number of preventative measures are available. First, for dog owners who live near or who often frequent tick-infested areas, routine vaccinations of their dogs is an important step.<ref name=pmid20207198/> | |||
| Prevention of Lyme disease is an important step in keeping dogs safe in endemic areas. Prevention education and a number of preventive measures are available. First, for dog owners who live near or who often frequent tick-infested areas, routine vaccinations of their dogs is an important step.<ref name=pmid20207198/> | |||
| Another crucial preventive measure is the use of persistent acaricides, such as topical repellents or pesticides that contain triazapentadienes (]), phenylpyrazoles (]), or permethrin (]).<ref name=pmid20933139/> These acaricides target primarily the adult stages of Lyme-carrying ticks and reduce the number of reproductively active ticks in the environment.<ref name=pmid20207198/> Formulations of these ingredients are available in a variety of topical forms, including spot-ons, sprays, powders, impregnated collars, solutions, and shampoos.<ref name=pmid20933139/> | Another crucial preventive measure is the use of persistent acaricides, such as topical repellents or pesticides that contain triazapentadienes (]), phenylpyrazoles (]), or permethrin (]).<ref name=pmid20933139/> These acaricides target primarily the adult stages of Lyme-carrying ticks and reduce the number of reproductively active ticks in the environment.<ref name=pmid20207198/> Formulations of these ingredients are available in a variety of topical forms, including spot-ons, sprays, powders, impregnated collars, solutions, and shampoos.<ref name=pmid20933139/> | ||
| Line 321: | Line 396: | ||
| Examination of a dog for ticks after being in a tick-infested area is an important precautionary measure to take in the prevention of Lyme disease. Key spots to examine include the head, neck, and ears.<ref name=hahn/> | Examination of a dog for ticks after being in a tick-infested area is an important precautionary measure to take in the prevention of Lyme disease. Key spots to examine include the head, neck, and ears.<ref name=hahn/> | ||
| In dogs, a serious long-term prognosis may result in glomerular disease,<ref name=merck_2012/> which is a category of kidney damage that may cause chronic kidney disease.<ref name="Brooks, DVM"/> Dogs may also experience chronic joint disease if the disease is left untreated. However, the majority of cases of Lyme disease in dogs result in complete recovery with, and sometimes without, treatment with antibiotics.<ref name=staubinger/>{{Verify source|date=July 2013}} In rare cases, Lyme disease can be fatal to both humans and dogs.<ref name="fatal-cases"/> | |||
| == Notes == | |||
| {{Reflist|30em|refs= | |||
| === Cats === | |||
| <ref name=Baron>{{cite book | author = Johnson RC | chapter = Borrelia | title = Baron's Medical Microbiology |editors=Baron S, et al.| edition = 4th | publisher = Univ of Texas Medical Branch | year = 1996 | url = http://www.ncbi.nlm.nih.gov/books/bv.fcgi?&rid=mmed.section.1965 | isbn = 0-9631172-1-1 | pmid = 21413339 }}</ref> | |||
| Unlike dogs, it is very rare for a cat to be infected with Lyme disease. However, cats are nevertheless capable of being infected with ''] ,'' following a bite from an infected tick. Cats who are infected with Lyme Disease may show symptoms including but not limited to lameness, fatigue, or loss of appetite.<ref name="Merck Veterinary Manual">{{Cite web |last=Straubinger |first=Reinhard |year=2018 |title=Lyme Disease (Lyme Borreliosis) in Cats - Cat Owners |url=https://www.merckvetmanual.com/cat-owners/disorders-affecting-multiple-body-systems-of-cats/lyme-disease-lyme-borreliosis-in-cats |url-status=live |archive-url=https://web.archive.org/web/20210420102458/https://www.merckvetmanual.com/cat-owners/disorders-affecting-multiple-body-systems-of-cats/lyme-disease-lyme-borreliosis-in-cats |archive-date=2021-04-20 |access-date=2023-10-26 |website=Merck Veterinary Manual |language=en-US}}</ref> In two cases, the infected cats experienced cardiac irregularities similar to symptoms of Lyme in both dogs and humans.<ref name="Tørnqvist-Johnsen_2020">{{cite journal | vauthors = Tørnqvist-Johnsen C, Dickson SA, Rolph K, Palermo V, Hodgkiss-Geere H, Gilmore P, Gunn-Moore DA | title = First report of Lyme borreliosis leading to cardiac bradydysrhythmia in two cats | journal = JFMS Open Reports | volume = 6 | issue = 1 | pages = 2055116919898292 | date = 2020 | pmid = 31949917 | pmc = 6950542 | doi = 10.1177/2055116919898292 }}</ref> However, cats who are infected with Lyme disease are likely to be ], and show no noticeable signs of the disease.<ref name="Tørnqvist-Johnsen_2020" /><ref name="Merck Veterinary Manual" /> Cats with Lyme are often treated with antibiotics, much like other animals. In some cases, additional treatment or therapy may be required.<ref name="Merck Veterinary Manual" /> | |||
| <ref name="Afzelius1910">{{cite journal |doi=10.1007/BF01832773 |title=Verhandlungen der dermatologischen Gesellschaft zu Stockholm |year=1910 |last1=Marcus |first1=Karl |journal=Archiv für Dermatologie und Syphilis |volume=101 |issue=2–3 |pages=403–06}}</ref> | |||
| <ref name=burckhardt_1911>{{cite journal | author = Burckhardt JL | title = Zur Frage der Follikel- und Keimzentrenbildung in der Haut | journal = Frankfurter Zeitschrift fur Pathologie | language = German | year = 1911 | volume = 6 | pages = 352–59}}</ref> | |||
| === Horses === | |||
| <ref name=Bianchi_1950>{{cite journal |author=Bianchi GE |title=Die Penicillinbehandlung der Lymphozytome |trans_title=Penicillin therapy of lymphocytoma |language=German |journal=Dermatologica |volume=100 |issue=4-6 |pages=270–73 |year=1950 |pmid=15421023 |doi=10.1159/000257185}}</ref> | |||
| Lyme disease in horses is often challenging to diagnose because symptoms vary widely. Common acute symptoms include weight loss, fever, ], ], and other muscle and joint-related issues.<ref name=":02">{{Cite journal |last1=Parker |first1=J. L. |last2=White |first2=K. K. |date=1992 |title=Lyme borreliosis in cattle and horses: a review of the literature |url=https://pubmed.ncbi.nlm.nih.gov/1643876/ |journal=The Cornell Veterinarian |volume=82 |issue=3 |pages=253–274 |issn=0010-8901 |pmid=1643876}}</ref><ref name=":12">{{Cite journal |last1=Johnstone |first1=L. K. |last2=Engiles |first2=J. B. |last3=Aceto |first3=H. |last4=Buechner-Maxwell |first4=V. |last5=Divers |first5=T. |last6=Gardner |first6=R. |last7=Levine |first7=R. |last8=Scherrer |first8=N. |last9=Tewari |first9=D. |last10=Tomlinson |first10=J. |last11=Johnson |first11=A. L. |date=2016 |title=Retrospective Evaluation of Horses Diagnosed with Neuroborreliosis on Postmortem Examination: 16 Cases (2004-2015) |journal=Journal of Veterinary Internal Medicine |volume=30 |issue=4 |pages=1305–1312 |doi=10.1111/jvim.14369 |issn=1939-1676 |pmc=5094551 |pmid=27327172}}</ref><ref>{{Cite journal |last=Van der Kolk |first=J. H. |date=2016 |title=Lyme borreliosis in the horse: A mini-review |journal=Journal of Experimental Biology and Agricultural Sciences |volume=4 |issue=Spl-4-EHIDZ |pages=S196–S202 |doi=10.18006/2016.4(Spl-4-EHIDZ).S196.S202|s2cid=78836519 |doi-access=free }}</ref> Additional symptoms include muscle tenderness, swollen joints, ], and neck stiffness.<ref name=":2">{{Cite journal |last1=Burgess |first1=E. C. |last2=Gillette |first2=D. |last3=Pickett |first3=J. |date=1986 |title=Arthritis and panuveitis as manifestations of Borrelia burgdorferi infection in a Wisconsin pony |url=https://pubmed.ncbi.nlm.nih.gov/3793582/ |journal=Journal of the American Veterinary Medical Association |volume=189 |issue=10 |pages=1340–1342 |issn=0003-1488 |pmid=3793582}}</ref><ref name=":3">{{Cite journal |last1=Browning |first1=A. |last2=Carter |first2=S. D. |last3=Barnes |first3=A. |last4=May |first4=C. |last5=Bennett |first5=D. |date=1993 |title=Lameness associated with Borrelia burgdorferi infection in the horse |url=https://pubmed.ncbi.nlm.nih.gov/8337810/ |journal=The Veterinary Record |volume=132 |issue=24 |pages=610–611 |doi=10.1136/vr.132.24.610 |doi-broken-date=3 December 2024 |issn=0042-4900 |pmid=8337810}}</ref><ref>{{Cite journal |last1=Gall |first1=Y |last2=Pfister |first2=K |date=2006 |title=Survey on the subject of equine Lyme borreliosis |url=https://pubmed.ncbi.nlm.nih.gov/16524771/ |journal=International Journal of Medical Microbiology |volume=296 |issue=1 |pages=274–279 |doi=10.1016/j.ijmm.2006.01.004 |issn=1438-4221 |pmid=16524771}}</ref> Chronic symptoms of the disease typically include neurological manifestations, such as ], cranial neuritis, ], and ].<ref>{{Cite journal |last1=Burgess |first1=E. C. |last2=Mattison |first2=M. |date=1987 |title=Encephalitis associated with Borrelia burgdorferi infection in a horse |url=https://pubmed.ncbi.nlm.nih.gov/3692996/ |journal=Journal of the American Veterinary Medical Association |volume=191 |issue=11 |pages=1457–1458 |issn=0003-1488 |pmid=3692996}}</ref><ref name=":02" /><ref name=":4">{{Cite journal |last1=Hahn |first1=C. N. |last2=Mayhew |first2=I. G. |last3=Whitwell |first3=K. E. |last4=Smith |first4=K. C. |last5=Carey |first5=D. |last6=Carter |first6=S. D. |last7=Read |first7=R. A. |date=1996 |title=A possible case of Lyme borreliosis in a horse in the UK |url=https://pubmed.ncbi.nlm.nih.gov/8565961/ |journal=Equine Veterinary Journal |volume=28 |issue=1 |pages=84–88 |doi=10.1111/j.2042-3306.1996.tb01595.x |issn=0425-1644 |pmid=8565961}}</ref><ref>{{Cite journal |last1=James |first1=F. M. |last2=Engiles |first2=J. B. |last3=Beech |first3=J. |date=2010 |title=Meningitis, cranial neuritis, and radiculoneuritis associated with Borrelia burgdorferi infection in a horse |url=https://pubmed.ncbi.nlm.nih.gov/21073390/ |journal=Journal of the American Veterinary Medical Association |volume=237 |issue=10 |pages=1180–1185 |doi=10.2460/javma.237.10.1180 |issn=0003-1488 |pmid=21073390}}</ref> Furthermore, it is important to note that some horses do not slow clinical signs of Lyme disease.<ref name=":5">{{Cite journal |last1=Divers |first1=T. J. |last2=Gardner |first2=R. B. |last3=Madigan |first3=J. E. |last4=Witonsky |first4=S. G. |last5=Bertone |first5=J. J. |last6=Swinebroad |first6=E. L. |last7=Schutzer |first7=S. E. |last8=Johnson |first8=A. L. |date=2018 |title=Borrelia burgdorferi Infection and Lyme Disease in North American Horses: A Consensus Statement |journal=Journal of Veterinary Internal Medicine |volume=32 |issue=2 |pages=617–632 |doi=10.1111/jvim.15042 |issn=1939-1676 |pmc=5866975 |pmid=29469222}}</ref> | |||
| <ref name="Bolognia">{{cite book |author=Bolognia JL | coauthors = Jorizzo JL ; Rapini RP |title=Dermatology |publisher=Mosby |location=St. Louis |year=2007 |pages= |isbn=978-1-4160-2999-1 | edition = 2nd }}{{page needed|date=March 2013}}</ref> | |||
| <ref name="Cairns">{{cite journal |author=Cairns V, Godwin J |title=Post-Lyme borreliosis syndrome: a meta-analysis of reported symptoms |journal=Int J Epidemiol |volume=34 |issue=6 |pages=1340–45 |date=December 2005 |pmid=16040645 |doi=10.1093/ije/dyi129}}</ref> | |||
| There are three main testing strategies used to diagnose horses with Lyme disease. They include clinical evaluation, ], and ] (PCR) testing.<ref>{{Cite journal |last1=Cohen |first1=N. D. |last2=Heck |first2=F. C. |last3=Heim |first3=B. |last4=Flad |first4=D. M. |last5=Bosler |first5=E. M. |last6=Cohen |first6=D. |date=1992 |title=Seroprevalence of antibodies to Borrelia burgdorferi in a population of horses in central Texas |url=https://pubmed.ncbi.nlm.nih.gov/1429127/ |journal=Journal of the American Veterinary Medical Association |volume=201 |issue=7 |pages=1030–1034 |doi=10.2460/javma.1992.201.07.1030 |issn=0003-1488 |pmid=1429127}}</ref><ref>{{Cite journal |last1=Metcalf |first1=K. B. |last2=Lilley |first2=C. S. |last3=Revenaugh |first3=M. S. |last4=Glaser |first4=A. L. |last5=Metcalf |first5=E. S. |date=2008 |title=The prevalence of antibodies against Borrelia burgdorferi found in horses residing in the northwestern United States |url=https://www.researchgate.net/publication/248868949 |journal=Journal of Equine Veterinary Science |volume=28 |issue=10 |pages=587–589|doi=10.1016/j.jevs.2008.08.010 }}</ref><ref name=":12" /> Detection of ] against ''B. burgdorferi'' alone is not sufficient for a diagnosis of ] Lyme disease and unspecific testing for antibodies is not recommended.<ref>{{cite journal |vauthors=Gehlen H, Inerle K, Bartel A, Stöckle SD, Ulrich S, Briese B, Straubinger RK |date=June 2023 |title=Seroprevalence of ''Borrelia burgdorferi'' sensu lato and ''Anaplasma phagocytophilum'' Infections in German Horses |journal=Animals |volume=13 |issue=12 |pages=1984 |doi=10.3390/ani13121984 |pmc=10295046 |pmid=37370494 |doi-access=free}}</ref> | |||
| <ref name=Burgdorfer_1984>{{cite journal |author=Burgdorfer W |title=Discovery of the Lyme disease spirochete and its relation to tick vectors |journal=Yale J Biol Med |volume=57 |issue=4 |pages=515–20 |year=1984 |pmid=6516454 |pmc=2590008}}</ref> | |||
| <ref name=Burgdorfer_1982>{{cite journal |author=Burgdorfer W, Barbour AG, Hayes SF, Benach JL, Grunwaldt E, Davis JP |title=Lyme disease-a tick-borne spirochetosis? |journal=Science |volume=216 |issue=4552 |pages=1317–19 |date=June 1982 |pmid=7043737 |doi=10.1126/science.7043737|bibcode = 1982Sci...216.1317B }}</ref> | |||
| Typical treatment involves antibiotics such as ], ], ], or ].<ref>{{Cite journal |last1=Bryant |first1=J. E. |last2=Brown |first2=M. P. |last3=Gronwall |first3=R. R. |last4=Merritt |first4=K. A. |date=2000 |title=Study of intragastric administration of doxycycline: pharmacokinetics including body fluid, endometrial and minimum inhibitory concentrations |url=https://pubmed.ncbi.nlm.nih.gov/10836479/ |journal=Equine Veterinary Journal |volume=32 |issue=3 |pages=233–238 |doi=10.2746/042516400776563608 |issn=0425-1644 |pmid=10836479}}</ref><ref name=":6">{{Cite journal |last1=Chang |first1=Y. F. |last2=Ku |first2=Y. W. |last3=Chang |first3=C. F. |last4=Chang |first4=C. D. |last5=McDonough |first5=S. P. |last6=Divers |first6=T. |last7=Pough |first7=M. |last8=Torres |first8=A. |date=2005 |title=Antibiotic treatment of experimentally Borrelia burgdorferi-infected ponies |url=https://pubmed.ncbi.nlm.nih.gov/15863289/ |journal=Veterinary Microbiology |volume=107 |issue=3 |pages=285–294 |doi=10.1016/j.vetmic.2005.02.006 |issn=0378-1135 |pmid=15863289}}</ref><ref name=":5" /> In some cases, a combination of antibiotics may be administered. Doxycycline and minocycline are taken orally, while oxytetracycline and ceftriaxone are usually administered intravenously.<ref name=":6" /><ref>{{Cite journal |last1=Schnabel |first1=L. V. |last2=Papich |first2=M. G. |last3=Divers |first3=T. J. |last4=Altier |first4=C. |last5=Aprea |first5=M. S. |last6=McCarrel |first6=T. M. |last7=Fortier |first7=L. A. |date=2012 |title=Pharmacokinetics and distribution of minocycline in mature horses after oral administration of multiple doses and comparison with minimum inhibitory concentrations |url=https://pubmed.ncbi.nlm.nih.gov/21950341/ |journal=Equine Veterinary Journal |volume=44 |issue=4 |pages=453–458 |doi=10.1111/j.2042-3306.2011.00459.x |issn=2042-3306 |pmid=21950341}}</ref><ref name=":5" /> The duration and dosage of treatment vary widely among cases. In most cases, the infected horse is ].<ref name=":2" /><ref name=":3" /><ref name=":4" /><ref>{{Cite journal |last1=Sears |first1=K. P. |last2=Divers |first2=T. J. |last3=Neff |first3=R. T. |last4=Miller |first4=W. H. |last5=McDonough |first5=S. P. |date=2012 |title=A case of Borrelia-associated cutaneous pseudolymphoma in a horse |url=https://pubmed.ncbi.nlm.nih.gov/22029872/ |journal=Veterinary Dermatology |volume=23 |issue=2 |pages=153–156 |doi=10.1111/j.1365-3164.2011.01013.x |issn=1365-3164 |pmid=22029872}}</ref> Death of horses as a result of ''Borrelia burgdorferi'' infection remains unknown.<ref>{{Cite journal |last1=Divers |first1=T. J. |last2=Grice |first2=A. L. |last3=Mohammed |first3=H. O. |last4=Glaser |first4=A. L. |last5=Wagner |first5=B. |date=2012 |title=Changes in Borrelia burgdorferi ELISA antibody over time in both antibiotic treated and untreated horses |url=https://madbarn.com/research/changes-in-borrelia-burgdorferi-elisa-antibody-over-time-in-both-antibiotic-treated-and-untreated-horses/?srsltid=AfmBOoq2jh8z5HX8l73s1xRpdvZavBtCgGgM563QHerbYqGbzm7KNRmC |journal=Acta Veterinaria Hungarica |volume=60 |issue=4 |pages=421–429|doi=10.1556/avet.2012.036 }}</ref> | |||
| <ref name=aucott_2012>{{cite journal |author=Aucott JN, Crowder LA, Yedlin V, Kortte KB |title=Bull's-Eye and nontarget skin lesions of Lyme disease: an internet survey of identification of erythema migrans |journal=Dermatol Res Pract |volume=2012 |issue= |page=451727 |year=2012 |pmid=23133445 |pmc=3485866 |doi=10.1155/2012/451727}} (primary source)</ref> | |||
| <ref name="Bach">{{cite conference | author=Bach G | title=Recovery of Lyme spirochetes by PCR in semen samples of previously diagnosed Lyme disease patients | booktitle=14th International Scientific Conference on Lyme Disease | year=2001 | url=http://www.anapsid.org/lyme/bach.html}}</ref> | |||
| Currently, there is no approved Lyme disease vaccine for horses available.<ref name=":7">{{Cite journal |last1=Guarino |first1=C. |last2=Asbie |first2=S. |last3=Rohde |first3=J. |last4=Glaser |first4=A. |last5=Wagner |first5=B. |date=2017 |title=Vaccination of horses with Lyme vaccines for dogs induces short-lasting antibody responses |url=https://www.sciencedirect.com/science/article/pii/S0264410X17308496 |journal=Vaccine |volume=35 |issue=33 |pages=4140–4147 |doi=10.1016/j.vaccine.2017.06.052 |issn=0264-410X|doi-access=free }}</ref> However, a study demonstrated that ponies could be protected using an aluminum adjuvanted recombinant ] A (rOspA) vaccine.<ref>{{Cite journal |last1=Chang |first1=Y. F. |last2=Novosol |first2=V. |last3=McDonough |first3=S. P. |last4=Chang |first4=C. F. |last5=Jacobson |first5=R. H. |last6=Divers |first6=T. |last7=Quimby |first7=F. W. |last8=Shin |first8=S. |last9=Lein |first9=D. H. |date=1999 |title=Vaccination against Lyme Disease with recombinant Borrelia burgdorferi outer-surface protein A (rOspA) in horses |url=https://www.sciencedirect.com/science/article/pii/S0264410X99001875 |journal=Vaccine |volume=18 |issue=5 |pages=540–548 |doi=10.1016/S0264-410X(99)00187-5 |pmid=10519945 |issn=0264-410X|doi-access=free }}</ref> While horses have been administered a Lyme disease vaccine designed for dogs, it elicits only a short-lasting antibody response.<ref name=":7" /> Another study supports the use of commercial Lyme disease vaccines, showing that they do elicit an antibody response, which can be significantly enhanced when horses receive an additional booster vaccine.<ref>{{Cite journal |last1=Knödlseder |first1=J. M. |last2=Fell |first2=S. F. |last3=Straubinger |first3=R. K. |date=2019 |title=A study with a commercial vaccine against Lyme borreliosis in horses using two different vaccination schedules: Characterization of the humoral immune response |url=https://pubmed.ncbi.nlm.nih.gov/31635975/ |journal=Vaccine |volume=37 |issue=49 |pages=7207–7212|doi=10.1016/j.vaccine.2019.09.087 |pmid=31635975 }}</ref> | |||
| <ref name=Calcagni_2006>{{cite journal |author=Calcagni E, Elenkov I |title=Stress system activity, innate and T helper cytokines, and susceptibility to immune-related diseases |journal=Annals of the New York Academy of Sciences |volume=1069 |issue= |pages=62–76 |date=June 2006 |pmid=16855135 |doi=10.1196/annals.1351.006 |bibcode=2006NYASA1069...62C}}</ref> | |||
| <ref name=CDC-FAQ>{{cite web|url=http://www.cdc.gov/lyme/faq/index.html#sexually|work=CDC Lyme FAQ|publisher=Centers for Disease Control | title=CDC Lyme FAQ}}</ref> | |||
| == References == | |||
| <ref name=Bolz_2004>{{cite journal |author=Bolz DD, Weis JJ |title=Molecular mimicry to Borrelia burgdorferi: pathway to autoimmunity? |journal=Autoimmunity |volume=37 |issue=5 |pages=387–92 |date=August 2004 |pmid=15621562 |doi=10.1080/08916930410001713098}}</ref> | |||
| {{Reflist|refs= | |||
| <ref name="Brown">{{cite journal |author=Brown SL, Hansen SL, Langone JJ |title=Role of serology in the diagnosis of Lyme disease |journal=JAMA |volume=282 |issue=1 |pages=62–66 |date=July 1999 |pmid=10404913 |doi=10.1001/jama.282.1.62}}</ref> | |||
| <ref name="Afzelius1910">{{cite journal |doi=10.1007/BF01832773 |title=Verhandlungen der dermatologischen Gesellschaft zu Stockholm |year=1910 | vauthors = Marcus K |journal=Archiv für Dermatologie und Syphilis |volume=101 |issue=2–3 |pages=403–06|s2cid=46704791 }}</ref> | |||
| <ref name="cdc-diagnosis">{{cite web | publisher = ] (CDC) | url = http://www.cdc.gov/ncidod/dvbid/lyme/ld_humandisease_diagnosis.htm | title = Lyme disease diagnosis | date = October 7, 2008 | accessdate = July 6, 2009}}</ref> | |||
| <ref name=Burdash_1991>{{cite journal |author=Burdash N, Fernandes J |title=Lyme borreliosis: detecting the great imitator |journal=J Am Osteopath Assoc |volume=91 |issue=6 |pages=573–74, 577–8 |date=June 1991 |pmid=1874654}}</ref> | |||
| <ref name= |
<ref name=burckhardt_1911>{{cite journal | vauthors = Burckhardt JL | title = Zur Frage der Follikel- und Keimzentrenbildung in der Haut | journal = Frankf. Z. Pathol. | language = de | year = 1911 | volume = 6 | pages = 352–59}}</ref> | ||
| <ref name=chabria_2007>{{cite journal |author=Chabria SB, Lawrason J |title=Altered mental status, an unusual manifestation of early disseminated Lyme disease: A case report |journal=Journal of Medical Case Reports |volume=1 |issue= |page=62 |year=2007 |pmid=17688693 |pmc=1973078 |doi=10.1186/1752-1947-1-62}}</ref> | |||
| <ref name= |
<ref name=Bianchi_1950>{{cite journal | vauthors = Bianchi GE | title = | language = de | journal = Dermatologica | volume = 100 | issue = 4–6 | pages = 270–273 | year = 1950 | pmid = 15421023 | doi = 10.1159/000257185 | trans-title = Penicillin therapy of lymphocytoma }}</ref> | ||
| <ref name=Bacon_2008>{{cite journal |author=Bacon RM, Kugeler KJ, Mead PS |title=Surveillance for Lyme disease--United States, 1992–2006 |journal=MMWR Surveill Summ |volume=57 |issue=10 |pages=1–9 |date=October 2008 |pmid=18830214 |url=http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5710a1.htm}}</ref> | |||
| <ref name="Bolognia">{{cite book | vauthors = Bolognia JL, Jorizzo JL, Rapini RP |title=Dermatology |publisher=Mosby |location=St. Louis |year=2007 |isbn=978-1-4160-2999-1 | edition = 2nd }}{{page needed|date=March 2013}}</ref> | |||
| <ref name=Coyle_1995>{{cite journal |author=Coyle PK, Schutzer SE, Deng Z, et al. |title=Detection of Borrelia burgdorferi-specific antigen in antibody-negative cerebrospinal fluid in neurologic Lyme disease |journal=Neurology |volume=45 |issue=11 |pages=2010–15 |date=November 1995 |pmid=7501150 |doi=10.1212/WNL.45.11.2010}}</ref> | |||
| <ref name=bulletin_2013>http://www.ct.gov/caes/lib/caes/documents/publications/bulletins/b1010.pdf{{full|date=March 2013}}</ref> | |||
| <ref name=Burgdorfer_1984>{{cite journal | vauthors = Burgdorfer W | title = Discovery of the Lyme disease spirochete and its relation to tick vectors | journal = The Yale Journal of Biology and Medicine | volume = 57 | issue = 4 | pages = 515–520 | year = 1984 | pmid = 6516454 | pmc = 2590008 }}</ref> | |||
| <ref name=bbc_dogs_2012>{{cite news |url=http://www.bbc.co.uk/news/health-16706942 |title=Lyme disease risk from dogs 'higher than thought' |publisher=BBC News Online |date=24 January 2012}}</ref> | |||
| <ref name=Dattwyler_1990>{{cite journal |author=Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ |title=Amoxycillin plus probenecid versus doxycycline for treatment of erythema migrans borreliosis |journal=Lancet |volume=336 |issue=8728 |pages=1404–06 |date=December 1990 |pmid=1978873 |doi=10.1016/0140-6736(90)93103-V}}</ref> | |||
| <ref name=Burgdorfer_1982>{{cite journal | vauthors = Burgdorfer W, Barbour AG, Hayes SF, Benach JL, Grunwaldt E, Davis JP | title = Lyme disease-a tick-borne spirochetosis? | journal = Science | volume = 216 | issue = 4552 | pages = 1317–1319 | date = June 1982 | pmid = 7043737 | doi = 10.1126/science.7043737 | url = http://www.escholarship.org/uc/item/9vj3t37b | access-date = 4 September 2018 | url-status = live | type = Submitted manuscript | bibcode = 1982Sci...216.1317B | archive-url = https://web.archive.org/web/20200130170502/https://escholarship.org/uc/item/9vj3t37b | archive-date = 30 January 2020 }}</ref> | |||
| <ref name=de_1997>{{cite journal |author=de Mik EL, van Pelt W, Docters-van Leeuwen BD, van der Veen A, Schellekens JF, Borgdorff MW |title=The geographical distribution of tick bites and erythema migrans in general practice in The Netherlands |journal=Int J Epidemiol |volume=26 |issue=2 |pages=451–7 |date=April 1997 |pmid=9169184 |doi=10.1093/ije/26.2.451}}</ref> | |||
| <ref name="cautionary">{{cite journal |author=Nigrovic LE, Thompson KM |title=The Lyme vaccine: a cautionary tale |journal=Epidemiol. Infect. |volume=135 |issue=1 |pages=1–8 |date=January 2007 |pmid=16893489 |pmc=2870557 |doi=10.1017/S0950268806007096}}</ref> | |||
| <ref name=CDC-FAQ>{{cite web |title=CDC Lyme disease FAQ |url=https://www.cdc.gov/lyme/faq/index.html |website=Centers for Disease Control and Prevention |access-date=11 January 2023 |language=en-us |date=8 January 2021}}</ref> | |||
| <ref name=Bouattour_2004>{{cite journal |author=Bouattour A, Ghorbel A, Chabchoub A, Postic D |title=Situation de la borreuose de lyme au maghreb |trans_title=Lyme borreliosis situation in North Africa |language=French |journal=Arch Inst Pasteur Tunis |volume=81 |issue=1-4 |pages=13–20 |year=2004 |pmid=16929760}}</ref> | |||
| <ref name=Drymon_2008>{{cite book |last=Drymon |first=MM |year=2008 |title=Disguised as the devil: how Lyme disease created witches and changed history |pages=51–52 |isbn=978-0-615-20061-3}}</ref> | |||
| <ref name=Bolz_2004>{{cite journal | vauthors = Bolz DD, Weis JJ | title = Molecular mimicry to Borrelia burgdorferi: pathway to autoimmunity? | journal = Autoimmunity | volume = 37 | issue = 5 | pages = 387–392 | date = August 2004 | pmid = 15621562 | doi = 10.1080/08916930410001713098 | s2cid = 43045224 }}</ref> | |||
| <ref name="Brooks, DVM">{{cite web|last=Brooks, DVM|first=Wendy C |title=Lyme Disease|url=http://www.VeterinaryPartner.com/Content.plx?P=A&S=0&C=0&A=1588&EVetID=3001782|publisher=Veterinary Information Network|accessdate=10 February 2012}}</ref> | |||
| <ref name="Duffy">{{cite journal |first1=David Cameron |last1=Duffy |first2=Randall |last2=Downer |first3=Christie |last3=Brinkley |year=1992 |title=The effectiveness of helmeted guineafowl in the control of the deer tick, the vector of Lyme disease |journal=The Wilson Bulletin |volume=104 |issue=2 |pages=342–45 |jstor=4163159 |url=http://www.guineafowl.com/fritsfarm/guineas/ticks/tickstudy.pdf}}</ref> | |||
| <ref name="Brown">{{cite journal | vauthors = Brown SL, Hansen SL, Langone JJ | title = Role of serology in the diagnosis of Lyme disease | journal = JAMA | volume = 282 | issue = 1 | pages = 62–66 | date = July 1999 | pmid = 10404913 | doi = 10.1001/jama.282.1.62 }}</ref> | |||
| <ref name=disease_action_2011>{{cite web |url=http://www.lymediseaseaction.org.uk/latest-news/concern-about-rise-in-lyme-disease-cases/ |title=Concern about rise in Lyme disease cases |publisher=Lyme Disease Action |date=2011-12-15 |accessdate=2012-12-15}}</ref> | |||
| <ref name=Edlow_2003>{{cite book |first=Jonathan A |last=Edlow |year=2003 |title=Bull's-eye: unraveling the medical mystery of Lyme disease |publisher=Yale University Press |isbn=0-300-09867-7}}{{page needed|date=March 2013}}</ref> | |||
| <ref name="cdc-diagnosis">{{cite web | publisher = ] (CDC) | url = https://www.cdc.gov/ncidod/dvbid/lyme/ld_humandisease_diagnosis.htm | title = Lyme disease diagnosis | date = 7 October 2008 | access-date = 6 July 2009 | url-status=live | archive-url = https://web.archive.org/web/20090828074557/http://www.cdc.gov/ncidod/dvbid/LYME/ld_humandisease_diagnosis.htm | archive-date = 28 August 2009}}</ref> | |||
| <ref name=cassidy_2011>{{cite news |url=http://www.pressandjournal.co.uk/Article.aspx/2177018 |work=Press and Journal |title=Tayside revealed as a Lyme disease hotspot as cases soar |first=Frank |last=Cassidy |date=14 March 2011}}</ref> | |||
| <ref name=emed_ophth>{{EMedicine|article|1202521|Ophthalmic aspects of Lyme disease overview of Lyme disease}}</ref> | |||
| <ref name=Burdash_1991>{{cite journal | vauthors = Burdash N, Fernandes J | title = Lyme borreliosis: detecting the great imitator | journal = The Journal of the American Osteopathic Association | volume = 91 | issue = 6 | pages = 573–4, 577–8 | date = June 1991 | pmid = 1874654 | doi = 10.1515/jom-1991-910610 | s2cid = 245118295 | doi-access = free }}</ref> | |||
| <ref name=danger_2009>{{cite web |url=http://www.rcn.org.uk/development/communities/specialisms/travel_health/news_stories/lyme_disease_a_clear_and_present_danger |title=Lyme disease: A clear and present danger |publisher=RCN |date=2009-04-28 |accessdate=2012-12-15}}</ref> | |||
| <ref name=Elenkov_2005>{{cite journal |author=Elenkov IJ, Iezzoni DG, Daly A, Harris AG, Chrousos GP |title=Cytokine dysregulation, inflammation and well-being |journal=Neuroimmunomodulation |volume=12 |issue=5 |pages=255–69 |year=2005 |pmid=16166805 |doi=10.1159/000087104}}</ref> | |||
| <ref name= |
<ref name="Clark">{{cite journal | vauthors = Clark K | title = Borrelia species in host-seeking ticks and small mammals in northern Florida | journal = Journal of Clinical Microbiology | volume = 42 | issue = 11 | pages = 5076–5086 | date = November 2004 | pmid = 15528699 | pmc = 525154 | doi = 10.1128/JCM.42.11.5076-5086.2004 }}</ref> | ||
| <ref name=Bacon_2008>{{cite journal | vauthors = Bacon RM, Kugeler KJ, Mead PS | title = Surveillance for Lyme disease--United States, 1992-2006 | journal = Morbidity and Mortality Weekly Report. Surveillance Summaries | volume = 57 | issue = 10 | pages = 1–9 | date = October 2008 | pmid = 18830214 | url = https://www.cdc.gov/mmwr/preview/mmwrhtml/ss5710a1.htm | url-status = live | archive-url = https://web.archive.org/web/20121110131222/http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5710a1.htm | archive-date = 10 November 2012 }}</ref> | |||
| <ref name=Coyle_1995>{{cite journal | vauthors = Coyle PK, Schutzer SE, Deng Z, Krupp LB, Belman AL, Benach JL, Luft BJ | title = Detection of Borrelia burgdorferi-specific antigen in antibody-negative cerebrospinal fluid in neurologic Lyme disease | journal = Neurology | volume = 45 | issue = 11 | pages = 2010–2015 | date = November 1995 | pmid = 7501150 | doi = 10.1212/WNL.45.11.2010 | s2cid = 23797801 }}</ref> | |||
| <ref name=bbc_dogs_2012>{{Cite news |url=https://www.bbc.co.uk/news/health-16706942 |title=Lyme disease risk from dogs 'higher than thought' |journal=BBC News |date=24 January 2012 |url-status=live |archive-url=https://web.archive.org/web/20120131034350/http://www.bbc.co.uk/news/health-16706942 |archive-date=31 January 2012 | vauthors = Roberts M }}</ref> | |||
| <ref name=Dattwyler_1990>{{cite journal | vauthors = Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ | title = Amoxycillin plus probenecid versus doxycycline for treatment of erythema migrans borreliosis | journal = Lancet | volume = 336 | issue = 8728 | pages = 1404–1406 | date = December 1990 | pmid = 1978873 | doi = 10.1016/0140-6736(90)93103-V | s2cid = 7314488 }}</ref> | |||
| <ref name=de_1997>{{cite journal | vauthors = de Mik EL, van Pelt W, Docters-van Leeuwen BD, van der Veen A, Schellekens JF, Borgdorff MW | title = The geographical distribution of tick bites and erythema migrans in general practice in The Netherlands | journal = International Journal of Epidemiology | volume = 26 | issue = 2 | pages = 451–457 | date = April 1997 | pmid = 9169184 | doi = 10.1093/ije/26.2.451 | doi-access = free }}</ref> | |||
| <ref name="cautionary">{{cite journal | vauthors = Nigrovic LE, Thompson KM | title = The Lyme vaccine: a cautionary tale | journal = Epidemiology and Infection | volume = 135 | issue = 1 | pages = 1–8 | date = January 2007 | pmid = 16893489 | pmc = 2870557 | doi = 10.1017/S0950268806007096 }}</ref> | |||
| <ref name=Bouattour_2004>{{cite journal | vauthors = Bouattour A, Ghorbel A, Chabchoub A, Postic D | title = | language = fr | journal = Archives de l'Institut Pasteur de Tunis | volume = 81 | issue = 1–4 | pages = 13–20 | year = 2004 | pmid = 16929760 | trans-title = Lyme borreliosis situation in North Africa }}</ref> | |||
| <ref name=Drymon_2008>{{cite book | vauthors = Drymon MM |year=2008 |title=Disguised as the devil: how Lyme disease created witches and changed history |pages=51–52 |publisher=Wythe Avenue Press |isbn=978-0-615-20061-3}}</ref> | |||
| <ref name="Brooks, DVM">{{cite web| vauthors = Brooks WC |title=Lyme Disease|url=http://www.VeterinaryPartner.com/Content.plx?P=A&S=0&C=0&A=1588&EVetID=3001782|publisher=Veterinary Information Network|access-date=10 February 2012|archive-url=https://web.archive.org/web/20150404175140/http://www.veterinarypartner.com/Content.plx?P=A&S=0&C=0&A=1588&EVetID=3001782|archive-date=4 April 2015|url-status=live}}</ref> | |||
| <ref name=disease_action_2011>{{cite web |url=http://www.lymediseaseaction.org.uk/latest-news/concern-about-rise-in-lyme-disease-cases/ |title=Concern about rise in Lyme disease cases |publisher=Lyme Disease Action |date=15 December 2011 |access-date=15 December 2012 |url-status=live |archive-url=https://web.archive.org/web/20130619044643/http://www.lymediseaseaction.org.uk/latest-news/concern-about-rise-in-lyme-disease-cases/ |archive-date=19 June 2013 }}</ref> | |||
| <ref name=Edlow_2003>{{cite book | vauthors = Edlow JA |year=2003 |title=Bull's-eye: unraveling the medical mystery of Lyme disease |publisher=Yale University Press |isbn=978-0-300-09867-9 |url=https://archive.org/details/bullseye00jona }} page 191.</ref> | |||
| <ref name=cassidy_2011>{{cite news |url=http://www.pressandjournal.co.uk/Article.aspx/2177018 |work=Press and Journal |title=Tayside revealed as a Lyme disease hotspot as cases soar | vauthors = Cassidy F |date=14 March 2011 |url-status=live |archive-url=https://web.archive.org/web/20160311055843/http://pressandjournal.co.uk/article.aspx/2177018 |archive-date=11 March 2016 }}</ref> | |||
| <ref name=danger_2009>{{cite web |url=http://www.rcn.org.uk/development/communities/specialisms/travel_health/news_stories/lyme_disease_a_clear_and_present_danger |title=Lyme disease: A clear and present danger |publisher=RCN |date=28 April 2009 |access-date=15 December 2012 |url-status=live |archive-url=https://web.archive.org/web/20130329024552/http://www.rcn.org.uk/development/communities/specialisms/travel_health/news_stories/lyme_disease_a_clear_and_present_danger |archive-date=29 March 2013 }}</ref> | |||
| <ref name=cdc_stats_2012>{{cite web | url = https://www.cdc.gov/lyme/stats/chartstables/reportedcases_statelocality.html | author = CDC | title = Reported Lyme disease cases by state, 2000-2010 | date = 4 January 2012 | access-date = 29 April 2012 | publisher = ] (CDC) | url-status=live | archive-url = https://web.archive.org/web/20120504101019/http://www.cdc.gov/lyme/stats/chartstables/reportedcases_statelocality.html | archive-date = 4 May 2012}}</ref> | |||
| <ref name=cdc_stats2>{{cite web | url = https://www.cdc.gov/lyme/stats/index.html | title = Lyme Disease Data | archive-url = https://web.archive.org/web/20120430203213/http://www.cdc.gov/lyme/stats/index.html | archive-date=30 April 2012 | publisher = ] (CDC) }}</ref> | |||
| <ref name=Ercolini>{{cite journal | vauthors = Ercolini AM, Miller SD | title = The role of infections in autoimmune disease | journal = Clinical and Experimental Immunology | volume = 155 | issue = 1 | pages = 1–15 | date = January 2009 | pmid = 19076824 | pmc = 2665673 | doi = 10.1111/j.1365-2249.2008.03834.x }}</ref> | |||
| <ref name="Halperin2008">{{cite journal | vauthors = Halperin JJ | title = Nervous system Lyme disease | journal = Infectious Disease Clinics of North America | volume = 22 | issue = 2 | pages = 261–74, vi | date = June 2008 | pmid = 18452800 | doi = 10.1016/j.idc.2007.12.009 | s2cid = 10590435 }}</ref> | |||
| <ref name=hellerstrom_1930>{{cite journal | vauthors = Hellerström S | title = ''Erythema chronicum migrans Afzelii'' | journal = Acta Derm. Venerol. | language = de | year = 1930 | volume = 11 | pages = 315–21}}</ref> | |||
| <!-- <ref name=hess_1999>{{cite journal | vauthors = Hess A, Buchmann J, Zettl UK, Henschel S, Schlaefke D, Grau G, Benecke R | title = Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder | journal = Biological Psychiatry | volume = 45 | issue = 6 | pages = 795 | date = March 1999 | pmid = 10188012 | doi = 10.1016/S0006-3223(98)00277-7 | s2cid = 44486654 }}</ref> --> | |||
| <ref name=defra_2009>{{cite web |url=http://www.defra.gov.uk/publications/files/pb13571-zoonoses2009-110125.pdf |title=Zoonoses report UK 2009 |publisher=] |date=24 January 2011 |url-status=live |archive-url=https://web.archive.org/web/20121103141930/http://www.defra.gov.uk/publications/files/pb13571-zoonoses2009-110125.pdf |archive-date=3 November 2012 }}</ref> | |||
| <ref name=Hoen_2009>{{cite journal | vauthors = Hoen AG, Margos G, Bent SJ, Diuk-Wasser MA, Barbour A, Kurtenbach K, Fish D | title = Phylogeography of Borrelia burgdorferi in the eastern United States reflects multiple independent Lyme disease emergence events | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 106 | issue = 35 | pages = 15013–15018 | date = September 2009 | pmid = 19706476 | pmc = 2727481 | doi = 10.1073/pnas.0903810106 | doi-access = free | bibcode = 2009PNAS..10615013H | jstor = 40484546 }}<br />Lay summary: {{cite web | title = Lyme Bacterium, Once Nearly Eradicated In U.S., Rebounded With Forests | url = http://news.yale.edu/2009/08/10/lyme-bacterium-once-nearly-eradicated-us-rebounded-forests | date = 10 August 2009 | website = YaleNews }}</ref> | |||
| <ref name=hovius_2007>{{cite journal | vauthors = Hovius JW, van Dam AP, Fikrig E | title = Tick-host-pathogen interactions in Lyme borreliosis | journal = Trends in Parasitology | volume = 23 | issue = 9 | pages = 434–438 | date = September 2007 | pmid = 17656156 | doi = 10.1016/j.pt.2007.07.001 | url = https://pure.uva.nl/ws/files/816561/62941_thesis.pdf | access-date = 9 September 2019 | url-status = live | archive-url = https://web.archive.org/web/20190216101036/https://pure.uva.nl/ws/files/816561/62941_thesis.pdf | archive-date = 16 February 2019 }}</ref> | |||
| <ref name=Dsouli_2006>{{cite journal | vauthors = Dsouli N, Younsi-Kabachii H, Postic D, Nouira S, Gern L, Bouattour A | title = Reservoir role of lizard Psammodromus algirus in transmission cycle of Borrelia burgdorferi sensu lato (Spirochaetaceae) in Tunisia | journal = Journal of Medical Entomology | volume = 43 | issue = 4 | pages = 737–742 | date = July 2006 | pmid = 16892633 | doi = 10.1603/0022-2585(2006)432.0.CO;2 | doi-broken-date = 1 December 2024 | url = http://doc.rero.ch/record/294963/files/jmedent43-0737.pdf | access-date = 5 July 2019 | url-status = live | s2cid = 24774778 | archive-url = https://web.archive.org/web/20180719060758/http://doc.rero.ch/record/294963/files/jmedent43-0737.pdf | archive-date = 19 July 2018 }}</ref> | |||
| <ref name="Hofmann">{{cite journal | vauthors = Hofmann H | title = Lyme borreliosis--problems of serological diagnosis | journal = Infection | volume = 24 | issue = 6 | pages = 470–472 | year = 1996 | pmid = 9007597 | doi = 10.1007/BF01713052 | s2cid = 19701481 }}</ref> | |||
| <ref name="Hildenbrand2009">{{cite journal | vauthors = Hildenbrand P, Craven DE, Jones R, Nemeskal P | title = Lyme neuroborreliosis: manifestations of a rapidly emerging zoonosis | journal = AJNR. American Journal of Neuroradiology | volume = 30 | issue = 6 | pages = 1079–1087 | date = June 2009 | pmid = 19346313 | pmc = 7051319 | doi = 10.3174/ajnr.A1579 | doi-access = free }}</ref> | |||
| <ref name="idsa guideline">{{cite journal | vauthors = Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, Krause PJ, Bakken JS, Strle F, Stanek G, Bockenstedt L, Fish D, Dumler JS, Nadelman RB | title = The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America | journal = Clinical Infectious Diseases | volume = 43 | issue = 9 | pages = 1089–1134 | date = November 2006 | pmid = 17029130 | doi = 10.1086/508667 | first12 = D | doi-access = free }}</ref> | |||
| <ref name=Fallon_2003>{{cite journal |author=Fallon BA, Keilp J, Prohovnik I, Heertum RV, Mann JJ |title=Regional cerebral blood flow and cognitive deficits in chronic lyme disease |journal=J Neuropsychiatry Clin Neurosci |volume=15 |issue=3 |pages=326–32 |year=2003 |pmid=12928508 |doi=10.1176/appi.neuropsych.15.3.326}}</ref> | |||
| <ref name=cdc_stats_2012>{{cite web | url = http://www.cdc.gov/lyme/stats/chartstables/reportedcases_statelocality.html | author = CDC | title = Reported Lyme disease cases by state, 2000-2010 | date = January 4, 2012 | accessdate = April 29, 2012 | publisher = ] (CDC) }}</ref> | |||
| <ref name=fell_2000>{{cite journal |author=Fell E |title=An update on Lyme disease and other tick-borne illnesses |journal=Nurse Pract |volume=25 |issue=10 |pages=38–40, 43–44, 47–48 passim; quiz 56–57 |date=October 2000 |pmid=11068777 |doi=10.1097/00006205-200025100-00003}}</ref> | |||
| <ref name=cdc_stats2>. ] (CDC).</ref> | |||
| <ref name=Ercolini>{{cite journal |author=Ercolini AM, Miller SD |title=The role of infections in autoimmune disease |journal=Clin. Exp. Immunol. |volume=155 |issue=1 |pages=1–15 |date=January 2009 |pmid=19076824 |pmc=2665673 |doi=10.1111/j.1365-2249.2008.03834.x}}</ref> | |||
| <ref name="Engstrom">{{cite journal |author=Engstrom SM, Shoop E, Johnson RC |title=Immunoblot interpretation criteria for serodiagnosis of early Lyme disease |journal=J. Clin. Microbiol. |volume=33 |issue=2 |pages=419–27 |date=February 1995 |pmid=7714202 |pmc=227960 |url=http://jcm.asm.org/cgi/pmidlookup?view=long&pmid=7714202}}</ref> | |||
| <ref name=cdc_surveil_2008>{{cite web |url=http://www.cdc.gov/osels/ph_surveillance/nndss/casedef/lyme_disease_2008.htm |title=Lyme disease (Borrelia burgdorferi) 2008 case definition |publisher=] }}</ref> | |||
| <ref name=Gasse_1994>{{cite journal |author=Gasse T |title=Neopterin production and tryptophan degradation in acute Lyme neuroborreliosis versus late Lyme encephalopathy |journal=European Journal of Clinical Chemistry and Clinical Biochemistry |volume=32 |issue=9 |pages=685–689 |year=1994 |pmid=7865624 |author2=Murr C |author3=Meyersbach P |display-authors=3 |last4=Schmutzhard |first4=E |last5=Wachter |first5=H |last6=Fuchs |first6=D |doi=10.1515/cclm.1994.32.9.685}}</ref> | |||
| <ref name=cdc_surveil_current>{{cite web |url=http://www.cdc.gov/osels/ph_surveillance/nndss/casedef/lyme_disease_current.htm |title=Lyme disease (Borrelia burgdorferi) 2011 case definition |publisher=] }}</ref> | |||
| <ref name="Gossens">{{cite journal |author=Goossens HA, Nohlmans MK, van den Bogaard AE |title=Epstein-Barr virus and cytomegalovirus infections cause false-positive results in IgM two-test protocol for early Lyme borreliosis |journal=Infection |volume=27 |issue=3 |page=231 |year=1999 |pmid=10378140 |doi=10.1007/BF02561539}}</ref> | |||
| <ref name="Halperin2008">{{cite journal |author=Halperin JJ |title=Nervous system Lyme disease |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=2 |pages=261–74, vi |date=June 2008 |pmid=18452800 |doi=10.1016/j.idc.2007.12.009}}</ref> | |||
| <ref name=hellerstrom_1930>{{cite journal | author = Hellerström S | title = Erythema chronicum migrans Afzelii | journal = Archiv Dermatologie and Venereologie (Stockholm) | language = German | year = 1930 | volume = 11 | pages = 315–21}}</ref> | |||
| <ref name=hess_1999>{{cite journal |author=Hess A, Buchmann J, Zettl UK, et al. |title=Borrelia burgdorferi central nervous system infection presenting as an organic schizophrenialike disorder |journal=Biol. Psychiatry |volume=45 |issue=6 |page=795 |date=March 1999 |pmid=10188012 |doi=10.1016/S0006-3223(98)00277-7}}</ref> | |||
| <ref name=defra_2009>{{cite web|url=http://www.defra.gov.uk/publications/files/pb13571-zoonoses2009-110125.pdf |title=Zoonoses report UK 2009 |publisher=] |date=24 January 2011 }}</ref> | |||
| <ref name=Eisendle_2007>{{cite journal |author=Eisendle K, Grabner T, Zelger B |title=Focus floating microscopy: 'gold standard' for cutaneous borreliosis? |journal=Am. J. Clin. Pathol. |volume=127 |issue=2 |pages=213–22 |date=February 2007 |pmid=17210530 |doi=10.1309/3369XXFPEQUNEP5C}}</ref> | |||
| <ref name=Hoen_2009>{{cite journal |author=Hoen AG, Margos G, Bent SJ, et al. |title=Phylogeography of Borrelia burgdorferi in the eastern United States reflects multiple independent Lyme disease emergence events |journal=Proc. Natl. Acad. Sci. U.S.A. |volume=106 |issue=35 |pages=15013–18 |date=September 2009 |pmid=19706476 |pmc=2727481 |doi=10.1073/pnas.0903810106 |bibcode=2009PNAS..10615013H |jstor=40484546 |laysummary=http://news.yale.edu/2009/08/10/lyme-bacterium-once-nearly-eradicated-us-rebounded-forests |laysource=YaleNews |laydate=August 10, 2009}}</ref> | |||
| <ref name=hovius_2007>{{cite journal |author=Hovius JW, van Dam AP, Fikrig E |title=Tick-host-pathogen interactions in Lyme borreliosis |journal=Trends Parasitol. |volume=23 |issue=9 |pages=434–8 |date=September 2007 |pmid=17656156 |doi=10.1016/j.pt.2007.07.001}}</ref> | |||
| <ref name=Dsouli_2006>{{cite journal |author=Dsouli N, Younsi-Kabachii H, Postic D, Nouira S, Gern L, Bouattour A |title=Reservoir role of lizard Psammodromus algirus in transmission cycle of Borrelia burgdorferi sensu lato (Spirochaetaceae) in Tunisia |journal=J. Med. Entomol. |volume=43 |issue=4 |pages=737–42 |date=July 2006 |pmid=16892633 |doi=10.1603/0022-2585(2006)432.0.CO;2}}</ref> | |||
| <ref name="Hofmann">{{cite journal |author=Hofmann H |title=Lyme borreliosis--problems of serological diagnosis |journal=Infection |volume=24 |issue=6 |pages=470–72 |year=1996 |pmid=9007597 |doi=10.1007/BF01713052}}</ref> | |||
| <ref name="Earnhart 2007">{{cite journal |author=Earnhart CG, Marconi RT |title=An octavalent lyme disease vaccine induces antibodies that recognize all incorporated OspC type-specific sequences |journal=Hum Vaccin |volume=3 |issue=6 |pages=281–89 |year=2007 |pmid=17921702 |url=http://www.landesbioscience.com/journals/hv/abstract.php?id=4661}}</ref> | |||
| <ref name=Hu>{{cite web | author = Hu, Linden | chapter = Clinical Manifestations of Lyme Disease in Adults | title = UpToDate | publisher = UpToDate | year = 2009 | url = http://www.uptodate.com/contents/clinical-manifestations-of-lyme-disease-in-adults }}</ref> | |||
| <ref name="Hildenbrand2009">{{cite journal |author=Hildenbrand P, Craven DE, Jones R, Nemeskal P |title=Lyme neuroborreliosis: manifestations of a rapidly emerging zoonosis |journal=AJNR Am J Neuroradiol |volume=30 |issue=6 |pages=1079–87 |date=June 2009 |pmid=19346313 |doi=10.3174/ajnr.A1579}}</ref> | |||
| <ref name="idsa guideline">{{cite journal |author=Wormser GP |title=The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America |journal=Clin. Infect. Dis. |volume=43 |issue=9|pages=1089–1134 | url = http://cid.oxfordjournals.org/content/43/9/1089.full.pdf |date=November 2006 |pmid=17029130 |doi=10.1086/508667 |last12=Fish |first12=D|last13=Dumler |first13=JS |first14=RB |author2=Dattwyler RJ |author3=Shapiro ED |display-authors=3 |last4=Nadelman |first4=John J. |last5=Steere |first5=Allen C. |last6=Klempner |first6=Mark S. |last7=Krause |first7=Peter J. |last8=Bakken |first8=Johan S. |last9=Strle |first9=Franc}}</ref> | |||
| <ref name="fatal-cases">Fatal cases of Lyme disease reported in the medical literature include: | <ref name="fatal-cases">Fatal cases of Lyme disease reported in the medical literature include: | ||
| * {{cite journal | |
* {{cite journal | vauthors = Kirsch M, Ruben FL, Steere AC, Duray PH, Norden CW, Winkelstein A | title = Fatal adult respiratory distress syndrome in a patient with Lyme disease | journal = JAMA | volume = 259 | issue = 18 | pages = 2737–2739 | date = May 1988 | pmid = 3357244 | doi = 10.1001/jama.1988.03720180063034 }} | ||
| * {{cite journal | |
* {{cite journal | vauthors = Oksi J, Kalimo H, Marttila RJ, Marjamäki M, Sonninen P, Nikoskelainen J, Viljanen MK | title = Inflammatory brain changes in Lyme borreliosis. A report on three patients and review of literature | journal = Brain | volume = 119 | issue = Pt 6 | pages = 2143–2154 | date = December 1996 | pmid = 9010017 | doi = 10.1093/brain/119.6.2143 | doi-access = free }} | ||
| * {{cite journal | |
* {{cite journal | vauthors = Waniek C, Prohovnik I, Kaufman MA, Dwork AJ | title = Rapidly progressive frontal-type dementia associated with Lyme disease | journal = The Journal of Neuropsychiatry and Clinical Neurosciences | volume = 7 | issue = 3 | pages = 345–347 | year = 1995 | pmid = 7580195 | doi = 10.1176/jnp.7.3.345 }} | ||
| * {{cite journal | |
* {{cite journal | vauthors = Cary NR, Fox B, Wright DJ, Cutler SJ, Shapiro LM, Grace AA | title = Fatal Lyme carditis and endodermal heterotopia of the atrioventricular node | journal = Postgraduate Medical Journal | volume = 66 | issue = 772 | pages = 134–136 | date = February 1990 | pmid = 2349186 | pmc = 2429516 | doi = 10.1136/pgmj.66.772.134 }}</ref> | ||
| <ref name=IDSA_FAQ>{{cite web | url = http://www.idsociety.org/Lyme_Facts/ | title = Ten Facts You Should Know About Lyme Disease |publisher = ]|date = May 10, 2011| accessdate = June 18, 2013}}</ref> | |||
| <ref name=Fivaz_1989>{{cite journal |author=Fivaz BH, Petney TN |title=Lyme disease--a new disease in southern Africa? |journal=J S Afr Vet Assoc |volume=60 |issue=3 |pages=155–58 |date=September 1989 |pmid=2699499}}</ref> | |||
| <ref name="isbn0-07-159991-6">{{cite journal |author=Steere, AC |chapter= Lyme borreliosis| title=Harrison's principles of internal medicine| publisher=McGraw-Hill Medical |edition=17th |isbn=0-07-159991-6 |editor=Fauci A, et al. | year=2008}}</ref> | |||
| <ref name=fact_sheet_2012>{{cite web|url=http://www.phac-aspc.gc.ca/id-mi/lyme-fs-eng.php |title=Lyme Disease Fact Sheet |publisher=Phac-aspc.gc.ca |date=2012-07-04 |accessdate=2012-12-15}}</ref> | |||
| <ref name=Josselyn_1670>{{cite book |first=John |last=Josselyn |year=1670 |title=An Account of Two Voyages to New-England Made during the Years 1638, 1663 |url=http://www.americanjourneys.org/aj-107/}}page 92</ref> | |||
| <ref name=fox_2010> BADA-UK, Wendy Fox, 2010</ref> | |||
| <ref name=ilads>{{cite web |authorlink=Igenex, Inc. |title=What You Should Know About Lyme Disease |publisher=International Lyme and Associated Diseases Society |url=http://www.ilads.org/lyme_research/lyme_articles6.html |accessdate = October 10, 2010}}</ref> | |||
| <ref name=kirby_2004>{{cite book |last=Stafford |first=Kirby C.| title = Tick Management Handbook | url = http://www.ct.gov/caes/lib/caes/documents/special_features/TickHandbook.pdf | year = 2004 | publisher = Connecticut Agricultural Experiment Station and Connecticut Department of Public Health | page =46 | accessdate = 2007-08-21}}</ref> | |||
| <ref name=JAMA_2007>{{cite journal |author=Zeller JL, Burke AE, Glass RM |title=JAMA patient page. Lyme disease |journal=JAMA |volume=297 |issue=23 |page=2664 |date=June 2007 |pmid=17579234 |doi=10.1001/jama.297.23.2664}}</ref> | |||
| <ref name=Ledin_2005>{{cite journal |author=Ledin KE, Zeidner NS, Ribeiro JM, et al. |title=Borreliacidal activity of saliva of the tick Amblyomma americanum |journal=Med. Vet. Entomol. |volume=19 |issue=1 |pages=90–5 |date=March 2005 |pmid=15752182 |doi=10.1111/j.0269-283X.2005.00546.x}}</ref> | |||
| <ref name=hahn>{{cite web|last=Hahn|first=Jeffrey|title=Ticks and Their Control|url=http://www.extension.umn.edu/distribution/horticulture/DD1013.html|publisher=Regents of the University of Minnesota}}</ref> | |||
| <ref name=lenhoff_1948>{{cite journal | author = Lenhoff C | title =Spirochetes in aetiologically obscure diseases | journal = Acta Derm. Venereol. | year = 1948 | volume = 28 | pages = 295–324}}</ref> | |||
| <ref name="Lakos2010">{{cite journal |author=Lakos A, Solymosi N |title=Maternal Lyme borreliosis and pregnancy outcome |journal=Int. J. Infect. Dis. |volume=14 |issue=6 |pages=e494–98 |date=June 2010 |pmid=19926325 |doi=10.1016/j.ijid.2009.07.019}}</ref> | |||
| <ref name=hansard1991> ] 1991-11-11</ref> | |||
| <ref name=Lindgren_2001>{{cite journal |author=Lindgren E, Gustafson R |title=Tick-borne encephalitis in Sweden and climate change |journal=Lancet |volume=358 |issue=9275 |pages=16–8 |date=July 2001 |pmid=11454371 |doi=10.1016/S0140-6736(00)05250-8}}</ref> | |||
| <ref name=hansard_1997> ], 1997-02-03</ref> | |||
| <ref name=Luft_1988>{{cite journal |author=Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ |title=New chemotherapeutic approaches in the treatment of Lyme borreliosis |journal=Annals of the New York Academy of Sciences |volume=539 |issue= |pages=352–61 |year=1988 |pmid=3056203 |doi=10.1111/j.1749-6632.1988.tb31869.x |bibcode=1988NYASA.539..352L}}</ref> | |||
| <ref name=Helmy_2000>{{cite journal |author=Helmy N |title=Seasonal abundance of Ornithodoros (O.) savignyi and prevalence of infection with Borrelia spirochetes in Egypt |journal=J Egypt Soc Parasitol |volume=30 |issue=2 |pages=607–19 |date=August 2000 |pmid=10946521}}</ref> | |||
| <ref name="Lymedisease">{{EMedicine|article|330178|Lyme disease'''}}</ref> | |||
| <ref name=Higgins_2004>{{cite journal |author=Higgins R |title=Emerging or re-emerging bacterial zoonotic diseases: bartonellosis, leptospirosis, Lyme borreliosis, plague |journal=Rev. - Off. Int. Epizoot. |volume=23 |issue=2 |pages=569–81 |date=August 2004 |pmid=15702720}}</ref> | |||
| <ref name="Magnarelli">{{cite journal |author=Magnarelli LA, Anderson JF |title=Ticks and biting insects infected with the etiologic agent of Lyme disease, Borrelia burgdorferi |journal=J. Clin. Microbiol. |volume=26 |issue=8 |pages=1482–6 |date=August 1988 |pmid=3170711 |pmc=266646}}</ref> | |||
| <ref name=hpaEpidemiology>{{cite web|url=http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/LymeDisease/EpidemiologicalData/lymLymeepidemiology/ |title=Epidemiology of Lyme borreliosis in the UK |publisher=HPA |accessdate=2012-12-15}}</ref> | |||
| <ref name="Luger">{{cite journal |author=Luger SW |title=Lyme disease transmitted by a biting fly |journal=N. Engl. J. Med. |volume=322 |issue=24 |page=1752 |date=June 1990 |pmid=2342543 |doi=10.1056/NEJM199006143222415}}</ref> | |||
| <ref name=hpa5-15>{{cite press release |title=Tick Lyme disease off your holiday list |publisher=Health Protection Agency |date=14 April 2011 |url=http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1296685255812 |accessdate=March 29, 2013}}</ref> | |||
| <ref name="LTBDRC">{{cite web | url = http://columbia-lyme.org/patients/ld_chronic.html | title = Why is Chronic Lyme Disease Chronic? | accessdate = 2011-02-26 | publisher = ]}}</ref> | |||
| <ref name=hpa_2009>{{cite web|url=http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1195733837876 |title=Lyme borreliosis in England and Wales: 2009 |publisher=HPA |accessdate=2012-12-15}}</ref> | |||
| <ref name=Mast_1976>{{cite journal |author=Mast WE, Burrows WM |title=Erythema chronicum migrans and 'lyme arthritis' |journal=JAMA |volume=236 |issue=21 |page=2392 |date=November 1976 |pmid=989847 |doi=10.1001/jama.236.21.2392d}}</ref> | |||
| <ref name=Masters2008>{{cite journal |author=Masters EJ, Grigery CN, Masters RW |title=STARI, or Masters disease: Lone Star tick-vectored Lyme-like illness |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=2 |pages=361–76, viii |date=June 2008 |pmid=18452807 |doi=10.1016/j.idc.2007.12.010}}</ref> | |||
| <ref name=managing_deer_2007>{{cite book |title=Managing Urban Deer in Connecticut |chapter=Figure 2: Changes in deer density and cases of Lyme disease in Mumford Cove, Connecticut, 1996–2004 (CT DEP data) |page=4 |publisher=Connecticut Department of Environmental Protection - Wildlife Division |edition=2nd |date=June 2007 |url=http://www.ct.gov/deep/lib/deep/wildlife/pdf_files/game/urbandeer07.pdf}}</ref> | |||
| <ref name=Krause_2006>{{cite journal |author=Krause PJ, Foley DT, Burke GS, Christianson D, Closter L, Spielman A |title=Reinfection and relapse in early Lyme disease |journal=Am. J. Trop. Med. Hyg. |volume=75 |issue=6 |pages=1090–94 |date=December 2006 |pmid=17172372}}</ref> | |||
| <ref name=mullegger_2004>{{cite journal |author=Mullegger RR |title=Dermatological manifestations of Lyme borreliosis |journal=Eur J Dermatol |volume=14 |issue=5 |pages=296–309 |year=2004 |pmid=15358567 |url=http://www.jle.com/medline.md?issn=1167-1122&vol=14&iss=5&page=296}}</ref> | |||
| <ref name="Klempner">{{cite journal |author=Klempner MS, Hu LT, Evans J, et al. |title=Two controlled trials of antibiotic treatment in patients with persistent symptoms and a history of Lyme disease |journal=N. Engl. J. Med. |volume=345 |issue=2 |pages=85–92 |date=July 2001 |pmid=11450676 |doi=10.1056/NEJM200107123450202}}</ref> | |||
| <ref name=Jowi_2005>{{cite journal |author=Jowi JO, Gathua SN |title=Lyme disease: report of two cases |journal=East Afr Med J |volume=82 |issue=5 |pages=267–69 |date=May 2005 |pmid=16119758 |doi=10.4314/eamj.v82i5.9318}}</ref> | |||
| <ref name=merck_2012>{{cite web|title=Glomerular Disease|url=http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/130605.htm|publisher=The Merck Veterinary Manual.|accessdate=11 Feb 2012}}</ref> | |||
| <ref name="Khasnis">{{cite journal |author=Khasnis AA, Nettleman MD |title=Global warming and infectious disease |journal=Arch. Med. Res. |volume=36 |issue=6 |pages=689–96 |year=2005 |pmid=16216650 |doi=10.1016/j.arcmed.2005.03.041}}</ref> | |||
| <ref name=Li_1998>{{cite journal |author=Li M, Masuzawa T, Takada N, et al. |title=Lyme disease Borrelia species in northeastern China resemble those isolated from far eastern Russia and Japan |journal=Appl. Environ. Microbiol. |volume=64 |issue=7 |pages=2705–09 |date=July 1998 |pmid=9647853 |pmc=106449 |url=http://aem.asm.org/cgi/pmidlookup?view=long&pmid=9647853}}</ref> | |||
| <ref name=Muhlemann_1987>{{cite journal |author=Muhlemann MF, Wright DJ |title=Emerging pattern of Lyme disease in the United Kingdom and Irish Republic |journal=Lancet |volume=1 |issue=8527 |pages=260–62 |date=January 1987 |pmid=2880076 |doi=10.1016/S0140-6736(87)90074-2}}</ref> | |||
| <ref name=londong_2008> ], August 2008</ref> | |||
| <ref name=min_ag_2012>{{cite web|author=BC Ministry of Agriculture |url=http://www.agf.gov.bc.ca/cropprot/ticksbc.htm |title=Ticks and Humans in British Columbia |publisher=Agf.gov.bc.ca |accessdate=2012-12-15}}</ref> | |||
| <ref name=Leighton_2012>{{cite journal |doi=10.1111/j.1365-2664.2012.02112.x |title=Predicting the speed of tick invasion: An empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada |year=2012 |last1=Leighton |first1=Patrick A |last2=Koffi |first2=Jules K |last3=Pelcat |first3=Yann |last4=Lindsay |first4=L Robbin |last5=Ogden |first5=Nicholas H |journal=Journal of Applied Ecology |volume=49 |issue=2 |pages=457–64}}</ref> | |||
| <ref name=mmwr_2007>{{cite journal |author= |title=Lyme disease--United States, 2003–2005 |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=56 |issue=23 |pages=573–76 |date=June 2007 |pmid=17568368 |url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5623a1.htm}}</ref> | |||
| <ref name=Mantovani_2007>{{cite journal |author=Mantovani E, Costa IP, Gauditano G, Bonoldi VL, Higuchi ML, Yoshinari NH |title=Description of Lyme disease-like syndrome in Brazil. Is it a new tick borne disease or Lyme disease variation? |journal=Braz. J. Med. Biol. Res. |volume=40 |issue=4 |pages=443–56 |date=April 2007 |pmid=17401487 |doi=10.1590/S0100-879X2006005000082}}</ref> | |||
| <ref name="LoGiudice">{{cite journal |author=LoGiudice K, Ostfeld RS, Schmidt KA, Keesing F |title=The ecology of infectious disease: effects of host diversity and community composition on Lyme disease risk |journal=Proc. Natl. Acad. Sci. U.S.A. |volume=100 |issue=2 |pages=567–71 |date=January 2003 |pmid=12525705 |pmc=141036 |doi=10.1073/pnas.0233733100 |bibcode=2003PNAS..100..567L}}</ref> | |||
| <ref name="Marques">{{cite journal | url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2430045/ |title=Chronic Lyme Disease: An appraisal | author=Marques, Adriana | journal=Infect Dis Clin North Am |date=June 2008 | volume=22 | issue=2 | pages=341–60 | doi=10.1016/j.idc.2007.12.011 | pmc=2430045}}</ref> | |||
| < |
<ref name=Fivaz_1989>{{cite journal | vauthors = Fivaz BH, Petney TN | title = Lyme disease--a new disease in southern Africa? | journal = Journal of the South African Veterinary Association | volume = 60 | issue = 3 | pages = 155–158 | date = September 1989 | pmid = 2699499 }}</ref> | ||
| <ref name=fact_sheet_2012>{{cite web |url=http://www.phac-aspc.gc.ca/id-mi/lyme-fs-eng.php |title=Lyme Disease Fact Sheet |publisher=Phac-aspc.gc.ca |date=4 July 2012 |access-date=15 December 2012 |url-status=live |archive-url=https://web.archive.org/web/20121227120507/http://www.phac-aspc.gc.ca/id-mi/lyme-fs-eng.php |archive-date=27 December 2012 }}</ref> | |||
| <ref name=Josselyn_1670>{{cite book | vauthors = Josselyn J |year=1670 |title=An Account of Two Voyages to New-England Made during the Years 1638, 1663 |url=http://www.americanjourneys.org/aj-107/ |url-status=live |archive-url=https://web.archive.org/web/20130625005205/http://www.americanjourneys.org/aj-107/ |archive-date=25 June 2013 }}page 92</ref> | |||
| <ref name="ngautopsy">{{cite news | first = Stephen S | last = Hall | url = http://ngm.nationalgeographic.com/2011/11/iceman-autopsy/hall-text | title = Iceman Autopsy | date = November 2011 | accessdate = October 17, 2011 | publisher= ] }}</ref> | |||
| <ref name=Paschoud_1954>{{cite journal |author=Paschoud JM |title=Lymphocytom nach Zeckenbiss |trans_title=Lymphocytoma after tick bite |language=German |journal=Dermatologica |volume=108 |issue=4-6 |pages=435–37 |year=1954 |pmid=13190934}}</ref> | |||
| <ref name=Papanicolaou_1998>{{cite journal |author=Papanicolaou DA, Wilder RL, Manolagas SC, Chrousos GP |title=The pathophysiologic roles of interleukin-6 in human disease |journal=Annals of Internal Medicine |volume=128 |issue=2 |pages=127–37 |date=January 1998 |pmid=9441573 |url=http://www.annals.org/article.aspx?volume=128&page=127}}</ref> | |||
| <ref name=Oldstone_1998>{{cite journal |author=Oldstone MB |title=Molecular mimicry and immune-mediated diseases |journal=FASEB J. |volume=12 |issue=13 |pages=1255–65 |date=October 1998 |pmid=9761770 |url=http://www.fasebj.org/content/12/13/1255.full.pdf }}</ref> | |||
| <ref name=Pachner_1989>{{cite journal |author=Pachner AR |title=Neurologic manifestations of Lyme disease, the new "great imitator" |journal=Rev. Infect. Dis. |volume=11 Suppl 6 |issue= |pages=S1482–1486 |year=1989 |pmid=2682960 |doi=10.1093/clinids/11.Supplement_6.S1482}}</ref> | |||
| <ref name="Perkins">{{cite journal |author=Perkins SE, Cattadori IM, Tagliapietra V, Rizzoli AP, Hudson PJ |title=Localized deer absence leads to tick amplification |journal=Ecology |volume=87 |issue=8 |pages=1981–86 |date=August 2006 |pmid=16937637 |doi=10.1890/0012-9658(2006)872.0.CO;2}}</ref> | |||
| <ref name="piesman2002">{{cite journal |author=Piesman J, Dolan MC |title=Protection against lyme disease spirochete transmission provided by prompt removal of nymphal Ixodes scapularis (Acari: Ixodidae) |journal=J. Med. Entomol. |volume=39 |issue=3 |pages=509–12 |date=May 2002 |pmid=12061448 |doi=10.1603/0022-2585-39.3.509}}</ref> | |||
| <ref name=Ogden_2009>{{cite journal |author=Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H |title=The emergence of Lyme disease in Canada |journal=CMAJ |volume=180 |issue=12 |pages=1221–24 |date=June 2009 |pmid=19506281 |pmc=2691438 |doi=10.1503/cmaj.080148}}</ref> | |||
| <ref name="nytimes.com">{{Cite news|last=Robbins|first=Jim|date=May 20, 2003|title=Montana Lab Tries to Identify Tick-Borne Disease|publisher=The New York Times|url=http://www.nytimes.com/2003/05/20/health/montana-lab-tries-to-identify-tick-borne-disease.html}}</ref> | |||
| <ref name="Patz">{{cite journal |author=Patz JA, Daszak P, Tabor GM, et al. |title=Unhealthy landscapes: Policy recommendations on land use change and infectious disease emergence |journal=Environ. Health Perspect. |volume=112 |issue=10 |pages=1092–98 |date=July 2004 |pmid=15238283 |pmc=1247383 |doi=10.1289/ehp.6877}}</ref> | |||
| <ref name="nejm-feder">{{cite journal | title = A Critical Appraisal of "Chronic Lyme Disease" | journal = ] | volume = 357 | issue = 14 | pages = 1422–30 | url = http://www.nejm.org/doi/full/10.1056/NEJMra072023 |date=October 2007 | pmid = 17914043 | doi = 10.1056/NEJMra072023 | last1 = Feder | first1 = HM | last2 = Johnson | first2 = BJB | last3 = O'Connell | first3 = S | display-authors = 3 | last4 = Shapiro | first4 = ED | last5 = Steere | first5 = AC | last6 = Wormser | first6 = GP | author7 = Ad Hoc International Lyme Disease Group | last8 = Agger | first8 = WA | last9 = Artsob | first9 = H | format = PDF }}</ref> | |||
| <ref name="nih-cld">{{cite web | publisher = ] | title = "Chronic Lyme Disease" Fact Sheet | url =http://www.niaid.nih.gov/topics/lymedisease/understanding/pages/chronic.aspx | date = April 17, 2009}}</ref> | |||
| <ref name=fox_2010>{{cite web | url = http://www.cieh-cymruwales.org/uploadedFiles/core/calendar/Tick_Borne_Disease_Risk_and_Reality_Wendy_Fox.pdf | title = Tick-Borne Disease, Risk and Realit | archive-url = https://web.archive.org/web/20121120152942/http://www.cieh-cymruwales.org/uploadedFiles/core/calendar/Tick_Borne_Disease_Risk_and_Reality_Wendy_Fox.pdf | archive-date=20 November 2012 | work = BADA-UK | vauthors = Fox W | date = 2010 }}</ref> | |||
| <!--ref name=Piesman_1991>{{cite journal |author=Piesman J, Stone BF |title=Vector competence of the Australian paralysis tick, Ixodes holocyclus, for the Lyme disease spirochete Borrelia burgdorferi |journal=Int. J. Parasitol. |volume=21 |issue=1 |pages=109–11 |date=February 1991 |pmid=2040556 |doi=10.1016/0020-7519(91)90127-S}}</ref--> | |||
| <ref name=kirby_2004>{{cite book | vauthors = Stafford KC | title = Tick Management Handbook | url = http://www.ct.gov/caes/lib/caes/documents/special_features/TickHandbook.pdf | year = 2004 | publisher = Connecticut Agricultural Experiment Station and Connecticut Department of Public Health | page = 46 | access-date = 21 August 2007 | url-status=live | archive-url = https://web.archive.org/web/20071025220415/http://www.ct.gov/caes/lib/caes/documents/special_features/TickHandbook.pdf | archive-date = 25 October 2007}}</ref> | |||
| <ref name="pmid12905137">{{cite journal |author=Steere AC, Sikand VK, Schoen RT, Nowakowski J |title=Asymptomatic infection with Borrelia burgdorferi |journal=Clin. Infect. Dis. |volume=37 |issue=4 |pages=528–32 |date=August 2003 |pmid=12905137 |doi=10.1086/376914}} (primary source)</ref> | |||
| <ref name="pmid11900494">{{cite journal |author=Smith RP, Schoen RT, Rahn DW, et al. |title=Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans |journal=Annals of Internal Medicine |volume=136 |issue=6 |pages=421–28 |date=March 2002 |pmid=11900494 |url=http://www.annals.org/article.aspx?volume=136&page=421 |doi=10.7326/0003-4819-136-6-200203190-00005}} (primary source)</ref> | |||
| <ref name="pmid14987414">{{cite journal |author=Auwaerter PG, Aucott J, Dumler JS |title=Lyme borreliosis (Lyme disease): molecular and cellular pathobiology and prospects for prevention, diagnosis and treatment |journal=Expert Rev Mol Med |volume=6 |issue=2 |pages=1–22 |date=January 2004 |pmid=14987414 |doi=10.1017/S1462399404007276}}</ref> | |||
| <ref name="pmid12543291">{{cite journal |author=Steere AC, Dhar A, Hernandez J, et al. |title=Systemic symptoms without erythema migrans as the presenting picture of early Lyme disease |journal=Am. J. Med. |volume=114 |issue=1 |pages=58–62 |date=January 2003 |pmid=12543291 |doi=10.1016/S0002-9343(02)01440-7}} (primary source)</ref> | |||
| <ref name=pmid15117014>{{cite journal |author=Lo Re V, Occi JL, MacGregor RR |title=Identifying the vector of Lyme disease |journal=Am Fam Physician |volume=69 |issue=8 |pages=1935–37 |date=April 2004 |pmid=15117014 |url=http://www.aafp.org/link_out?pmid=15117014}}</ref> | |||
| <ref name="pmid15085185">{{cite journal |author=Steere AC, Coburn J, Glickstein L |title=The emergence of Lyme disease |journal=J. Clin. Invest. |volume=113 |issue=8 |pages=1093–101 |date=April 2004 |pmid=15085185 |pmc=385417 |doi=10.1172/JCI21681}}</ref> | |||
| <ref name=pmid11450660>{{cite journal |author=Steere AC |title=Lyme disease |journal=N. Engl. J. Med. |volume=345 |issue=2 |pages=115–25 |date=July 2001 |pmid=11450660 |doi=10.1056/NEJM200107123450207}}</ref> | |||
| <ref name="pmid15709249">{{cite journal |author=Eisen L, Eisen RJ, Lane RS |title=The roles of birds, lizards, and rodents as hosts for the western black-legged tick Ixodes pacificus |journal=J. Vector Ecol. |volume=29 |issue=2 |pages=295–308 |date=December 2004 |pmid=15709249}}</ref> | |||
| <ref name="pmid16995383">{{cite journal |author=Lane RS, Mun J, Eisen L, Eisen RJ |title=Refractoriness of the western fence lizard (Sceloporus occidentalis) to the Lyme disease group spirochete Borrelia bissettii |journal=J. Parasitol. |volume=92 |issue=4 |pages=691–96 |date=August 2006 |pmid=16995383 |doi=10.1645/GE-738R1.1}}</ref> | |||
| <ref name=pmid17041141>{{cite journal |author=Swanson SJ, Neitzel D, Reed KD, Belongia EA |title=Coinfections acquired from ixodes ticks |journal=Clin. Microbiol. Rev. |volume=19 |issue=4 |pages=708–27 |date=October 2006 |pmid=17041141 |pmc=1592693 |doi=10.1128/CMR.00011-06}}</ref> | |||
| <ref name="pmid16807416">{{cite journal |author=Wormser GP |title=Clinical practice. Early Lyme disease |journal=N. Engl. J. Med. |volume=354 |issue=26 |pages=2794–801 |date=June 2006 |pmid=16807416 |doi=10.1056/NEJMcp061181}}</ref> | |||
| <ref name="pmid17509489">{{cite journal |author=Pachner AR, Steiner I |title=Lyme neuroborreliosis: infection, immunity, and inflammation |journal=Lancet Neurol |volume=6 |issue=6 |pages=544–52 |date=June 2007 |pmid=17509489 |doi=10.1016/S1474-4422(07)70128-X}}</ref> | |||
| <ref name="pmid16698304">{{cite journal |author=Fikrig E, Narasimhan S |title=Borrelia burgdorferi--traveling incognito? |journal=Microbes Infect. |volume=8 |issue=5 |pages=1390–9 |date=April 2006 |pmid=16698304 |doi=10.1016/j.micinf.2005.12.022}}</ref> | |||
| <ref name="pmid17404293">{{cite journal |author=Xu Q, Seemanapalli SV, Reif KE, Brown CR, Liang FT |title=Increasing the recruitment of neutrophils to the site of infection dramatically attenuates Borrelia burgdorferi infectivity |journal=Journal of Immunology |volume=178 |issue=8 |pages=5109–15 |date=April 2007 |pmid=17404293 |url=http://www.jimmunol.org/cgi/pmidlookup?view=long&pmid=17404293 |doi=10.4049/jimmunol.178.8.5109}}</ref> | |||
| <ref name="pmid17600717">{{cite journal |author=Cabello FC, Godfrey HP, Newman SA |title=Hidden in plain sight: Borrelia burgdorferi and the extracellular matrix |journal=Trends Microbiol. |volume=15 |issue=8 |pages=350–54 |date=August 2007 |pmid=17600717 |doi=10.1016/j.tim.2007.06.003}}</ref> | |||
| <ref name="pmid18140373">{{cite journal |author=Thyresson N |title=The penicillin treatment of acrodermatitis atrophicans chronica (Herxheimer) |journal=Acta Derm. Venereol. |volume=29 |issue=6 |pages=572–621 |year=1949 |pmid=18140373}}</ref> | |||
| <ref name="pmid11438915">{{cite journal |author=Molloy PJ, Persing DH, Berardi VP |title=False-positive results of PCR testing for Lyme disease |journal=Clin. Infect. Dis. |volume=33 |issue=3 |pages=412–13 |date=August 2001 |pmid=11438915 |doi=10.1086/321911}}</ref> | |||
| <ref name="pmid18452799">{{cite journal |author=Dandache P, Nadelman RB |title=Erythema migrans |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=2 |pages=235–60, vi |date=June 2008 |pmid=18452799 |doi=10.1016/j.idc.2007.12.012}}</ref> | |||
| <ref name="pmid18452805">{{cite journal |author=Stanek G, Strle F |title=Lyme disease: European perspective |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=2 |pages=327–39, vii |date=June 2008 |pmid=18452805 |doi=10.1016/j.idc.2008.01.001}}</ref> | |||
| <ref name="pmid12938230">{{cite journal |author=Ramesh G, Alvarez AL, Roberts ED, et al. |title=Pathogenesis of Lyme neuroborreliosis: Borrelia burgdorferi lipoproteins induce both proliferation and apoptosis in rhesus monkey astrocytes |journal=Eur. Journal of Immunology |volume=33 |issue=9 |pages=2539–50 |date=September 2003 |pmid=12938230 |doi=10.1002/eji.200323872}}</ref> | |||
| <ref name="pmid18452802">{{cite journal |author=Puius YA, Kalish RA |title=Lyme arthritis: pathogenesis, clinical presentation, and management |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=2 |pages=289–300, vi–vii |date=June 2008 |pmid=18452802 |doi=10.1016/j.idc.2007.12.014}}</ref> | |||
| <ref name="pmid11929056">{{cite journal |author=Staub D, Debrunner M, Amsler L, Steffen R |title=Effectiveness of a repellent containing DEET and EBAAP for preventing tick bites |journal=Wilderness Environ Med |volume=13 |issue=1 |pages=12–20 |year=2002 |pmid=11929056 |doi=10.1580/1080-6032(2002)0132.0.CO;2}}</ref> | |||
| <ref name="pmid19562015">{{cite journal |author=Nau R, Christen HJ, Eiffert H |title=Lyme disease--current state of knowledge |journal=Dtsch Arztebl Int |volume=106 |issue=5 |pages=72–81; quiz 82, I |date=January 2009 |pmid=19562015 |pmc=2695290 |doi=10.3238/arztebl.2009.0072}}</ref> | |||
| <ref name="pmid1531156">{{cite journal |author=Halperin JJ, Heyes MP |title=Neuroactive kynurenines in Lyme borreliosis |journal=Neurology |volume=42 |issue=1 |pages=43–50 |date=January 1992 |pmid=1531156 |doi=10.1212/WNL.42.1.43}}</ref> | |||
| <ref name="pmid18454594">{{cite journal |author=Schneider BS, Schriefer ME, Dietrich G, Dolan MC, Morshed MG, Zeidner NS |title=Borrelia bissettii isolates induce pathology in a murine model of disease |journal=Vector-Borne and Zoonotic Diseases |volume=8 |issue=5 |pages=623–33 |date=October 2008 |pmid=18454594 |doi=10.1089/vbz.2007.0251}}</ref> | |||
| <ref name="pmid16020686">{{cite journal |author=Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser GP |title=Diagnosis of lyme borreliosis |journal=Clin. Microbiol. Rev. |volume=18 |issue=3 |pages=484–509 |date=July 2005 |pmid=16020686 |pmc=1195970 |doi=10.1128/CMR.18.3.484-509.2005}}</ref> | |||
| <ref name="pmid23319969">{{cite journal |title=Lyme disease: review |author=Biesiada G, Czepiel J, Leśniak MR, Garlicki A, Mach T |journal=Arch Med Sci. |date=Dec 20, 2012 |volume=8 |issue=6 |pages=978–82.|doi=10.5114/aoms.2012.30948|pmid=23319969 |pmc=3542482}}</ref> | |||
| <ref name="pmid15623946">{{cite journal |author=Masuzawa T |title=Terrestrial distribution of the Lyme borreliosis agent Borrelia burgdorferi sensu lato in East Asia |journal=Jpn. J. Infect. Dis. |volume=57 |issue=6 |pages=229–35 |date=December 2004 |pmid=15623946 |url=http://www0.nih.go.jp/JJID/57/229.html}}</ref> | |||
| <ref name="pmid18650352">{{cite journal |author=Rudenko N, Golovchenko M, Mokrácek A, et al. |title=Detection of Borrelia bissettii in cardiac valve tissue of a patient with endocarditis and aortic valve stenosis in the Czech Republic |journal=J. Clin. Microbiol. |volume=46 |issue=10 |pages=3540–3 |date=October 2008 |pmid=18650352 |pmc=2566110 |doi=10.1128/JCM.01032-08}}</ref> | |||
| <ref name=pmid18452798>{{cite journal |author=Tilly K, Rosa PA, Stewart PE |title=Biology of infection with Borrelia burgdorferi |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=2 |pages=217–34, v |date=June 2008 |pmid=18452798 |pmc=2440571 |doi=10.1016/j.idc.2007.12.013}}</ref> | |||
| <ref name="pmid23091571">{{cite journal |author=von Baehr V, Doebis C, Volk HD, von Baehr R |title=The lymphocyte transformation test for borrelia detects active lyme borreliosis and verifies effective antibiotic treatment. |journal=Open Neurol J. |volume=6 |issue=2 |pages=104–12 |date=October 2012 |pmid=23091571 |doi=10.2174/1874205X01206010104}}</ref> | |||
| <ref name="pmid9556169">{{cite journal |author=Fahrer H, Sauvain MJ, Zhioua E, Van Hoecke C, Gern LE |title=Longterm survey (7 years) in a population at risk for Lyme borreliosis: what happens to the seropositive individuals? |journal=Eur. J. Epidemiol. |volume=14 |issue=2 |pages=117–23 |date=February 1998 |pmid=9556169 |doi=10.1023/A:1007404620701}} (primary source)</ref> | |||
| <ref name="pmid16819127">{{cite journal |author=Smith R, Takkinen J |title=Lyme borreliosis: Europe-wide coordinated surveillance and action needed? |journal=Euro Surveill. |volume=11 |issue=6 |pages=E060622.1 |year=2006 |pmid=16819127 |url=http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=2977}}</ref> | |||
| <ref name="pmid9452402">{{cite journal |author=Varde S, Beckley J, Schwartz I |title=Prevalence of tick-borne pathogens in Ixodes scapularis in a rural New Jersey County |journal=Emerging Infect. Dis. |volume=4 |issue=1 |pages=97–99 |year=1998 |pmid=9452402 |pmc=2627663 |doi=10.3201/eid0401.980113}}</ref> | |||
| <ref name="pmid17130658">{{cite journal |author=Lopes de Carvalho I, Núncio MS |title=Laboratory diagnosis of Lyme borreliosis at the Portuguese National Institute of Health (1990–2004) |journal=Euro Surveill. |volume=11 |issue=10 |pages=257–60 |year=2006 |pmid=17130658 |url=http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=650}}</ref> | |||
| <ref name="pmid9215633">{{cite journal |author=Coleman JL, Gebbia JA, Piesman J, Degen JL, Bugge TH, Benach JL |title=Plasminogen is required for efficient dissemination of B. burgdorferi in ticks and for enhancement of spirochetemia in mice |journal=Cell |volume=89 |issue=7 |pages=1111–9 |date=June 1997 |pmid=9215633 |doi=10.1016/S0092-8674(00)80298-6}}</ref> | |||
| <ref name="pmid16820453">{{cite journal |author=Richter D, Matuschka FR |title=Perpetuation of the Lyme disease spirochete Borrelia lusitaniae by lizards |journal=Appl. Environ. Microbiol. |volume=72 |issue=7 |pages=4627–32 |date=July 2006 |pmid=16820453 |pmc=1489336 |doi=10.1128/AEM.00285-06}}</ref> | |||
| <ref name=Ribeiro_1987>{{cite journal |author=Ribeiro JM, Mather TN, Piesman J, Spielman A |title=Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae) |journal=J. Med. Entomol. |volume=24 |issue=2 |pages=201–05 |date=March 1987 |pmid=3585913}}</ref> | |||
| <ref name="pmid17417956">{{cite journal |author=Swanson KI, Norris DE |title=Detection of Borrelia burgdorferi DNA in lizards from Southern Maryland |journal=Vector-Borne and Zoonotic Diseases |volume=7 |issue=1 |pages=42–49 |year=2007 |pmid=17417956 |doi=10.1089/vbz.2006.0548}}</ref> | |||
| <ref name="pmid18097481">{{cite journal |author=Rupprecht TA, Koedel U, Fingerle V, Pfister HW |title=The pathogenesis of lyme neuroborreliosis: from infection to inflammation |journal=Mol. Med. |volume=14 |issue=3-4 |pages=205–12 |year=2008 |pmid=18097481 |pmc=2148032 |doi=10.2119/2007-00091.Rupprecht |doi_brokendate=March 30, 2013 |url=http://molmed.org/journal/articles/3/1398}}</ref> | |||
| <ref name="pmid17326941">{{cite journal |author=Majláthová V, Majláth I, Derdáková M, Víchová B, Pet'ko B |title=Borrelia lusitaniae and green lizards (Lacerta viridis), Karst Region, Slovakia |journal=Emerging Infect. Dis. |volume=12 |issue=12 |pages=1895–901 |date=December 2006 |pmid=17326941 |pmc=3291370 |doi=10.3201/eid1212.060784}}</ref> | |||
| <ref name="Samuels DS; Radolf, JD editors 2010">{{cite book |editor1= Samuels DS|editor2=Radolf, JD | year=2010 |title=Borrelia: Molecular Biology, Host Interaction and Pathogenesis | publisher=Caister Academic Press | isbn= 978-1-904455-58-5}}</ref> | |||
| <ref name="pmid17427701">{{cite journal |author=Amore G, Tomassone L, Grego E, et al. |title=Borrelia lusitaniae in immature Ixodes ricinus (Acari: Ixodidae) feeding on common wall lizards in Tuscany, central Italy |journal=J. Med. Entomol. |volume=44 |issue=2 |pages=303–07 |date=March 2007 |pmid=17427701 |doi=10.1603/0022-2585(2007)442.0.CO;2}}</ref> | |||
| <ref name=samuels_2010>{{cite book |editor1= Samuels DS|editor2=Radolf, JD| year=2010 |title=Borrelia: Molecular Biology, Host Interaction and Pathogenesis | publisher=Caister Academic Press | isbn= 978-1-904455-58-5 | chapter=Chapter 6, Structure, Function and Biogenesis of the ''Borrelia'' Cell Envelope}}</ref> | |||
| <ref name="pmid17522387">{{cite journal |author=Halperin JJ, Shapiro ED, Logigian E, et al. |title=Practice parameter: treatment of nervous system Lyme disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology |journal=Neurology |volume=69 |issue=1 |pages=91–102 |date=July 2007 |pmid=17522387 |doi=10.1212/01.wnl.0000265517.66976.28}}</ref> | |||
| <ref name=Scrimenti_1970>{{cite journal |author=Scrimenti RJ |title=Erythema chronicum migrans |journal=Arch Dermatol |volume=102 |issue=1 |pages=104–05 |date=July 1970 |pmid=5497158 |doi=10.1001/archderm.102.1.104}}</ref> | |||
| <ref name="pmid17626342">{{cite journal |author=Giery ST, Ostfeld RS |title=The role of lizards in the ecology of Lyme disease in two endemic zones of the northeastern United States |journal=J. Parasitol. |volume=93 |issue=3 |pages=511–17 |date=June 2007 |pmid=17626342 |doi=10.1645/GE-1053R1.1}}</ref> | |||
| <ref name=Sherris>{{cite book | editor = Ryan KJ; Ray CG | title = Sherris Medical Microbiology | edition = 4th | pages = 434–37 | publisher = McGraw Hill | year = 2004 | isbn = 0-8385-8529-9}}</ref> | |||
| <ref name=Rasley_2002>{{cite journal |author=Rasley A, Anguita J, Marriott I |title=Borrelia burgdorferi induces inflammatory mediator production by murine microglia |journal=J. Neuroimmunol. |volume=130 |issue=1-2 |pages=22–31 |date=September 2002 |pmid=12225885 |doi=10.1016/S0165-5728(02)00187-X}}</ref> | |||
| <ref name=Shadick>{{cite journal |author=Shadick NA, Phillips CB, Sangha O, et al. |title=Musculoskeletal and neurologic outcomes in patients with previously treated Lyme disease |journal=Annals of Internal Medicine |volume=131 |issue=12 |pages=919–26 |date=December 1999 |pmid=10610642 |url=http://www.annals.org/article.aspx?volume=131&page=919 |doi=10.7326/0003-4819-131-12-199912210-00003}}</ref> | |||
| <ref name=Raveche_2005>{{cite journal |author=Raveche ES |title=Evidence of Borrelia autoimmunity-induced component of Lyme carditis and arthritis |journal=J. Clin. Microbiol. |volume=43 |issue=2 |pages=850–56 |date=February 2005 |pmid=15695691 |pmc=548028 |doi=10.1128/JCM.43.2.850-856.2005 |author2=Schutzer SE |author3=Fernandes H |display-authors=3 |last4=Bateman |first4=H. |last5=McCarthy |first5=B. A. |last6=Nickell |first6=S. P. |last7=Cunningham |first7=M. W.}}</ref> | |||
| <ref name=seltzer_2000>{{cite journal |author=Seltzer EG, Gerber MA, Cartter ML, Freudigman K, Shapiro ED |title=Long-term outcomes of persons with Lyme disease |journal=JAMA |volume=283 |issue=5 |pages=609–16 |date=February 2000 |pmid=10665700 |doi=10.1001/jama.283.5.609}}</ref> | |||
| <ref name="pmid8272083">{{cite journal |author=Nocton JJ, Dressler F, Rutledge BJ, Rys PN, Persing DH, Steere AC |title=Detection of Borrelia burgdorferi DNA by polymerase chain reaction in synovial fluid from patients with Lyme arthritis |journal=N. Engl. J. Med. |volume=330 |issue=4 |pages=229–34 |date=January 1994 |pmid=8272083 |doi=10.1056/NEJM199401273300401}}</ref> | |||
| <ref name=Stanek2011>{{cite journal | author = Stanek G, Reiter M | year = 2011 | title = The expanding Lyme Borrelia complex - clinical significance of genomic species | url = | journal = Clin Microbiol Infect | volume = 17 | issue = 4| pages = 487–93 | doi = 10.1111/j.1469-0691.2011.03492.x | pmid = 21414082 }}</ref> | |||
| <ref name=pmid20207198>{{cite journal |author=Little SE, Heise SR, Blagburn BL, Callister SM, Mead PS |title=Lyme borreliosis in dogs and humans in the USA |journal=Trends Parasitol. |volume=26 |issue=4 |pages=213–18 |date=April 2010 |pmid=20207198 |doi=10.1016/j.pt.2010.01.006}}</ref> | |||
| <ref name="Schmidt">{{cite journal |author=Schmidt BL, Aberer E, Stockenhuber C, Klade H, Breier F, Luger A |title=Detection of Borrelia burgdorferi DNA by polymerase chain reaction in the urine and breast milk of patients with Lyme borreliosis |journal=Diagn. Microbiol. Infect. Dis. |volume=21 |issue=3 |pages=121–28 |date=March 1995 |pmid=7648832 |doi=10.1016/0732-8893(95)00027-8}}</ref> | |||
| <ref name=pmid20933139>{{cite journal |author=Krupka I, Straubinger RK |title=Lyme borreliosis in dogs and cats: background, diagnosis, treatment and prevention of infections with Borrelia burgdorferi sensu stricto |journal=Vet. Clin. North Am. Small Anim. Pract. |volume=40 |issue=6 |pages=1103–19 |date=November 2010 |pmid=20933139 |doi=10.1016/j.cvsm.2010.07.011}}</ref> | |||
| <ref name=Steere_1977>{{cite journal |author=Steere AC |title=Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three connecticut communities |journal=Arthritis Rheum. |volume=20 |issue=1 |pages=7–17 |year=1977 |pmid=836338 |doi=10.1002/art.1780200102 |author2=Malawista SE |author3=Snydman DR |display-authors=3 |last4=Shope |first4=Robert E. |last5=Andiman |first5=Warren A. |last6=Ross |first6=Martin R. |last7=Steele |first7=Francis M.}}</ref> | |||
| <ref name="pmid21794218">{{cite journal |author=Rizzoli A, Hauffe H, Carpi G, Vourc HG, Neteler M, Rosa R |title=Lyme borreliosis in Europe |journal=Euro Surveill. |volume=16 |issue=27 |pages= |year=2011 |pmid=21794218 |url=http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19906}}</ref> | |||
| <ref name=Steere_1983>{{cite journal |author=Steere AC, Hutchinson GJ, Rahn DW, et al. |title=Treatment of the early manifestations of Lyme disease |journal=Annals of Internal Medicine |volume=99 |issue=1 |pages=22–26 |date=July 1983 |pmid=6407378}}</ref> | |||
| <ref name="pmid2563850">{{cite journal |author=Guy EC, Bateman DE, Martyn CN, Heckels JE, Lawton NF |title=Lyme disease: prevalence and clinical importance of Borrelia burgdorferi specific IgG in forestry workers |journal=Lancet |volume=1 |issue=8636 |pages=484–86 |date=March 1989 |pmid=2563850 |doi=10.1016/S0140-6736(89)91377-9}}</ref> | |||
| <ref name=Steere_2006>{{cite journal |author=Steere AC |title=Lyme borreliosis in 2005, 30 years after initial observations in Lyme Connecticut |journal=Wien. Klin. Wochenschr. |volume=118 |issue=21-22 |pages=625–33 |date=November 2006 |pmid=17160599 |doi=10.1007/s00508-006-0687-x}}</ref> | |||
| <ref name="pmid8037992">{{cite journal |author=Haywood GA, O'Connell S, Gray HH |title=Lyme carditis: a United Kingdom perspective |journal=Br Heart J |volume=70 |issue=1 |pages=15–16 |date=July 1993 |pmid=8037992 |pmc=1025222 |doi=10.1136/hrt.70.1.15}}</ref> | |||
| <ref name=Sternbach>{{cite journal |author=Sternbach G, Dibble CL |title=Willy Burgdorfer: Lyme disease |journal=J Emerg Med |volume=14 |issue=5 |pages=631–34 |year=1996 |pmid=8933327 |doi=10.1016/S0736-4679(96)00143-6}}</ref> | |||
| <ref name="Rand">{{cite journal |author=Rand PW, Lubelczyk C, Holman MS, Lacombe EH, Smith RP |title=Abundance of Ixodes scapularis (Acari: Ixodidae) after the complete removal of deer from an isolated offshore island, endemic for Lyme Disease |journal=J. Med. Entomol. |volume=41 |issue=4 |pages=779–84 |date=July 2004 |pmid=15311475 |doi=10.1603/0022-2585-41.4.779}}</ref> | |||
| <ref name=summerton_1995>{{cite journal |doi=10.1136/bmj.311.7018.1478 |title=Lyme disease in the eighteenth century |year=1995 |author=Summerton N |journal=BMJ |volume=311 |issue=7018 |page=1478}}</ref> | |||
| <ref name=Poland_2001>{{cite journal |author=Poland GA, Jacobson RM |title=The prevention of Lyme disease with vaccine |journal=Vaccine |volume=19 |issue=17-19 |pages=2303–08 |date=March 2001 |pmid=11257352 |doi=10.1016/S0264-410X(00)00520-X}}</ref> | |||
| <ref name="pmid15085185"/> | |||
| <ref name=Pozsgay_2007>{{cite journal |author=Pozsgay V, Kubler-Kielb J |title=Synthesis of an experimental glycolipoprotein vaccine against Lyme disease |journal=Carbohydr. Res. |volume=342 |issue=3-4 |pages=621–26 |date=February 2007 |pmid=17182019 |pmc=2709212 |doi=10.1016/j.carres.2006.11.014}}</ref> | |||
| <ref name=Sun_2003>{{cite journal |author=Sun Y, Xu R |title=Ability of Ixodes persulcatus, Haemaphysalis concinna and Dermacentor silvarum ticks to acquire and transstadially transmit Borrelia garinii |journal=Exp. Appl. Acarol. |volume=31 |issue=1-2 |pages=151–60 |year=2003 |pmid=14756409 |doi=10.1023/B:APPA.0000005119.30172.43}}</ref> | |||
| <ref name=rowe_199>{{cite news | url = http://www.nytimes.com/1999/06/13/nyregion/lukewarm-response-to-new-lyme-vaccine.html | title = Lukewarm Response To New Lyme Vaccine | first = Claudia |last = Rowe | work = ] | date = June 13, 1999 | accessdate = July 11, 2008}}</ref> | |||
| <ref name=Steere_2003>{{cite web | author = Steere AC | title = Lyme Disease: Questions and Answers |publisher = Massachusetts General Hospital / Harvard Medical School | url = http://www.mgh.harvard.edu/medicine/rheu/Q&ALYME.pdf |archiveurl=http://web.archive.org/web/20080307191326/http://www.mgh.harvard.edu/medicine/rheu/Q&ALYME.pdf | archivedate=2008-03-07 | date = 2003-02-01 | accessdate = 2009-04-01}}</ref> | |||
| <ref name=Singh>{{cite journal |author=Singh SK, Girschick HJ |title=Lyme borreliosis: from infection to autoimmunity |journal=Clin. Microbiol. Infect. |volume=10 |issue=7 |pages=598–614 |date=July 2004 |pmid=15214872 |doi=10.1111/j.1469-0691.2004.00895.x}}</ref> | |||
| <ref name="safe">{{cite journal |author= |title=When a vaccine is safe |journal=Nature |volume=439 |issue=7076 |page=509 |date=February 2006 |pmid=16452935 |doi=10.1038/439509a |bibcode=2006Natur.439Q.509.}}</ref> | |||
| <ref name=Ledin_2005>{{cite journal | vauthors = Ledin KE, Zeidner NS, Ribeiro JM, Biggerstaff BJ, Dolan MC, Dietrich G, Vredevoe L, Piesman J | title = Borreliacidal activity of saliva of the tick Amblyomma americanum | journal = Medical and Veterinary Entomology | volume = 19 | issue = 1 | pages = 90–95 | date = March 2005 | pmid = 15752182 | doi = 10.1111/j.0269-283X.2005.00546.x | s2cid = 270178 | url = https://zenodo.org/record/1230595 }}</ref> | |||
| <!-- unused ref | |||
| <ref name=Wang>{{cite journal |author=Wang G, van Dam AP, Schwartz I, Dankert J |title=Molecular typing of Borrelia burgdorferi sensu lato: taxonomic, epidemiological, and clinical implications |journal=Clin. Microbiol. Rev. |volume=12 |issue=4 |pages=633–53 |date=October 1999 |pmid=10515907 |pmc=88929 |url=http://cmr.asm.org/cgi/pmidlookup?view=long&pmid=10515907}}</ref> | |||
| --> | |||
| <ref name=hahn>{{cite web| vauthors = Hahn J |title=Ticks and Their Control|url=http://www.extension.umn.edu/distribution/horticulture/DD1013.html|publisher=Regents of the University of Minnesota|url-status=dead|archive-url=https://web.archive.org/web/20120225120056/http://www.extension.umn.edu/distribution/horticulture/DD1013.html|archive-date=25 February 2012|access-date=19 February 2012}}</ref> | |||
| <ref name="Sivak">{{cite journal |author=Sivak SL, Aguero-Rosenfeld ME, Nowakowski J, Nadelman RB, Wormser GP |title=Accuracy of IgM immunoblotting to confirm the clinical diagnosis of early Lyme disease |journal=Arch. Intern. Med. |volume=156 |issue=18 |pages=2105–09 |date=October 1996 |pmid=8862103 |doi=10.1001/archinte.156.18.2105}}</ref> | |||
| <ref name="Walsh2007">{{cite journal |author=Walsh CA, Mayer EW, Baxi LV |title=Lyme disease in pregnancy: case report and review of the literature |journal=Obstet Gynecol Surv |volume=62 |issue=1 |pages=41–50 |date=January 2007 |pmid=17176487 |doi=10.1097/01.ogx.0000251024.43400.9a}}</ref> | |||
| <ref name=lenhoff_1948>{{cite journal | vauthors = Lennhoff C | title = Spirochaetes in aetiologically obscure diseases | journal = Acta Dermato-Venereologica | volume = 28 | issue = 3 | pages = 295–324 | year = 1948 | pmid = 18891989 }}</ref> | |||
| <ref name=scotland_2012>{{cite web|url=http://www.scotland.gov.uk/Topics/Health/NHS-Scotland/publicact/Implementation/Timetable3333/Part2Guidance/Q/EditMode/on/ForceUpdate/on |title=Guidance on Part 2 - Notifiable Diseases, Notifiable Organisms and Health Risk States |publisher=Scotland.gov.uk |date=2012-09-10 |accessdate=2012-12-15}}</ref> | |||
| <ref name=Weinstein_2002>{{cite journal |author=Weinstein A, Britchkov M |title=Lyme arthritis and post-Lyme disease syndrome |journal=Current Opinion in Rheumatology |volume=14 |issue=4 |pages=383–87 |date=July 2002 |pmid=12118171 |doi=10.1097/00002281-200207000-00008}}</ref> | |||
| <ref name=" |
<ref name="Lakos2010">{{cite journal | vauthors = Lakos A, Solymosi N | title = Maternal Lyme borreliosis and pregnancy outcome | journal = International Journal of Infectious Diseases | volume = 14 | issue = 6 | pages = e494–e498 | date = June 2010 | pmid = 19926325 | doi = 10.1016/j.ijid.2009.07.019 | doi-access = free }}</ref> | ||
| <ref name="Wormser">{{cite journal | author=Wormser G | title=Prospective clinical evaluation of patients from missouri and New York with ''erythema migrans''-like skin lesions | journal=Clin Infect Dis | volume=41 | issue=7 | pages=958–65 | year=2005 | pmid= 16142659 | doi=10.1086/432935 | author-separator=, | author2=Masters E | author3=Nowakowski J | display-authors=3 | last4=McKenna | first4=D. | last5=Holmgren | first5=D. | last6=Ma | first6=K. | last7=Ihde | first7=L. | last8=Cavaliere | first8=L. F. | last9=Nadelman | first9=R. B.}}</ref> | |||
| <ref name=hansard1991>{{cite web | url = https://api.parliament.uk/historic-hansard/lords/1991/nov/11/lyme-disease | title = Lyme Disease | archive-url = https://web.archive.org/web/20130615185628/http://hansard.millbanksystems.com/lords/1991/nov/11/lyme-disease | archive-date=15 June 2013 | work = ] | url-status = live | date = 11 November 1991 }}</ref> | |||
| <ref name="Strasfeld">{{cite journal |author=Strasfeld L, Romanzi L, Seder RH, Berardi VP |title=False-positive serological test results for Lyme disease in a patient with acute herpes simplex virus type 2 infection |journal=Clin. Infect. Dis. |volume=41 |issue=12 |pages=1826–27 |date=December 2005 |pmid=16288417 |doi=10.1086/498319}}</ref> | |||
| <ref name=Wright_2006>{{cite journal |author=Wright CB, Sacco RL, Rundek T, Delman J, Rabbani L, Elkind M |title=Interleukin-6 is associated with cognitive function: the Northern Manhattan Study |journal=J Stroke Cerebrovasc Dis |volume=15 |issue=1 |pages=34–8 |year=2006 |pmid=16501663 |pmc=1382058 |doi=10.1016/j.jstrokecerebrovasdis.2005.08.009}}</ref> | |||
| <ref name= |
<ref name=Lindgren_2001>{{cite journal | vauthors = Lindgren E, Gustafson R | title = Tick-borne encephalitis in Sweden and climate change | journal = Lancet | volume = 358 | issue = 9275 | pages = 16–18 | date = July 2001 | pmid = 11454371 | doi = 10.1016/S0140-6736(00)05250-8 | s2cid = 336323 }}</ref> | ||
| <ref name=Smith_2012>{{cite journal |author=Smith FD, Ballantyne R, Morgan ER, Wall R |title=Estimating Lyme disease risk using pet dogs as sentinels |journal=Comp. Immunol. Microbiol. Infect. Dis. |volume=35 |issue=2 |pages=163–67 |date=March 2012 |pmid=22257866 |doi=10.1016/j.cimid.2011.12.009 |laysummary=http://www.bris.ac.uk/news/2012/8176.html |laysource=Bristol University |laydate=25 January 2012}}</ref> | |||
| <ref name=hansard_1997>{{cite web | url = https://api.parliament.uk/historic-hansard/written-answers/1997/feb/03/lyme-disease#S6CV0289P0_19970203_CWA_15 | title = Lyme Disease | archive-url = https://web.archive.org/web/20130615175146/http://hansard.millbanksystems.com/written_answers/1997/feb/03/lyme-disease | archive-date=15 June 2013 | work = ] | url-status = live | date = 3 February 1997 }}</ref> | |||
| <ref name=Zajkowska_2006>{{cite journal |author=Zajkowska J, Grygorczuk S, Kondrusik M, Pancewicz S, Hermanowska-Szpakowicz T |title= |language=Polish |journal=Przegl Epidemiol |volume=60 |issue=Suppl 1 |pages=167–70 |year=2006 |pmid=16909797}}</ref> | |||
| <ref name=staubinger>{{cite web|last=Staubinger, PhD|first=R.|title=Lyme Disease|url=http://siriusdog.com/lyme-disease-spirochete-ticks-dog.htm|publisher=Sirius Dog.|accessdate=10 Feb 2012}}{{Verify credibility|date=July 2013}}</ref> | |||
| <ref name= |
<ref name=Luft_1988>{{cite journal | vauthors = Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ | title = New chemotherapeutic approaches in the treatment of Lyme borreliosis | journal = Annals of the New York Academy of Sciences | volume = 539 | issue = 1 | pages = 352–361 | year = 1988 | pmid = 3056203 | doi = 10.1111/j.1749-6632.1988.tb31869.x | s2cid = 25939418 | bibcode = 1988NYASA.539..352L }}</ref> | ||
| <ref name="Steere 2006">{{cite journal |author=Steere AC, Angelis SM |title=Therapy for Lyme arthritis: strategies for the treatment of antibiotic-refractory arthritis |journal=Arthritis Rheum. |volume=54 |issue=10 |pages=3079–86 |date=October 2006 |pmid=17009226 |doi=10.1002/art.22131}}</ref> | |||
| <ref name= |
<ref name=Helmy_2000>{{cite journal | vauthors = Helmy N | title = Seasonal abundance of Ornithodoros (O.) savignyi and prevalence of infection with Borrelia spirochetes in Egypt | journal = Journal of the Egyptian Society of Parasitology | volume = 30 | issue = 2 | pages = 607–619 | date = August 2000 | pmid = 10946521 }}</ref> | ||
| <ref name="Lymedisease">{{EMedicine|article|330178|Lyme disease}}</ref> | |||
| <ref name=vaccine_2008>{{cite news | url = http://www.nytimes.com/2002/02/28/business/sole-lyme-vaccine-is-pulled-off-market.html | title = Sole Lyme Vaccine Is Pulled Off Market | work = ] | date = February 28, 2002 | accessdate = July 11, 2008}}</ref> | |||
| <ref name=wright_2012>{{cite journal |author=Wright WF, Riedel DJ, Talwani R, Gilliam BL |title=Diagnosis and management of Lyme disease |journal=Am Fam Physician |volume=85 |issue=11 |pages=1086–93 |date=June 2012 |pmid=22962880 |doi= |url=http://www.aafp.org/afp/2012/0601/p1086.html}}</ref> | |||
| <ref name= |
<ref name=Higgins_2004>{{cite journal | vauthors = Higgins R | title = Emerging or re-emerging bacterial zoonotic diseases: bartonellosis, leptospirosis, Lyme borreliosis, plague | journal = Revue Scientifique et Technique | volume = 23 | issue = 2 | pages = 569–581 | date = August 2004 | pmid = 15702720 | doi = 10.20506/rst.23.2.1503 | doi-access = free }}</ref> | ||
| <ref name=tick_bite> Tick Bite Prevention Week</ref> | |||
| <ref name=hpaEpidemiology>{{cite web |url=http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/LymeDisease/EpidemiologicalData/lymLymeepidemiology/ |title=Epidemiology of Lyme borreliosis in the UK |publisher=HPA |access-date=15 December 2012 |url-status=live |archive-url=https://web.archive.org/web/20130610054850/http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/LymeDisease/EpidemiologicalData/lymLymeepidemiology/ |archive-date=10 June 2013 }}</ref> | |||
| <ref name="cdc_dispatch_oct_2007">{{Citation | last=Gordillo-Pérez | first=Guadalupe | last2 =Torres | first2=Javier | last3=Solórzano-Santos | first3=Fortino | last4=de Martino | first4=Sylvie | last5=Lipsker | first5=Dan | last6=Velázquez | first6=Edmundo | title=Borrelia burgdorferi Infection and Cutaneous Lyme Disease, Mexico | journal=Emerg Infect Dis |date=Oct 2007 | url=http://wwwnc.cdc.gov/eid/article/13/10/06-0630.htm | doi=10.3201/eid1310.060630 }}</ref> | |||
| <ref name=vox_facts> Analysis of CDC data on VoxHealth. Retrieved on 2013-30-1</ref> | |||
| <ref name=hpa5-15>{{cite press release|title=Tick Lyme disease off your holiday list |publisher=Health Protection Agency |date=14 April 2011 |url=http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1296685255812 |access-date=29 March 2013 |archive-url=https://web.archive.org/web/20110428004436/http://www.hpa.org.uk/web/HPAweb%26HPAwebStandard/HPAweb_C/1296685255812 |archive-date=28 April 2011 |url-status=dead }}</ref> | |||
| <ref name=Yoshinari_1993>{{cite journal |author=Yoshinari NH, Oyafuso LK, Monteiro FG, et al. |title=Doença de Lyme: Relato de um caso observado no Brasil |trans_title=Lyme disease. Report of a case observed in Brazil |language=Portuguese |journal=Rev Hosp Clin Fac Med Sao Paulo |volume=48 |issue=4 |pages=170–74 |year=1993 |pmid=8284588}}</ref> | |||
| <ref name=hpa_2013>{{cite web |url=https://www.gov.uk/government/publications/lyme-borreliosis-epidemiology/lyme-borreliosis-epidemiology-and-surveillance |title=Lyme borreliosis epidemiology and surveillance: May 2013 |publisher=HPA |access-date=24 November 2015 |url-status=live |archive-url=https://web.archive.org/web/20151125115822/https://www.gov.uk/government/publications/lyme-borreliosis-epidemiology/lyme-borreliosis-epidemiology-and-surveillance |archive-date=25 November 2015 }}</ref> | |||
| <ref name=Mast_1976>{{cite journal | vauthors = Mast WE, Burrows WM | title = Erythema chronicum migrans and "lyme arthritis" | journal = JAMA | volume = 236 | issue = 21 | pages = 2392d–2392 | date = November 1976 | pmid = 989847 | doi = 10.1001/jama.236.21.2392d }}</ref> | |||
| <ref name=Masters2008>{{cite journal | vauthors = Masters EJ, Grigery CN, Masters RW | title = STARI, or Masters disease: Lone Star tick-vectored Lyme-like illness | journal = Infectious Disease Clinics of North America | volume = 22 | issue = 2 | pages = 361–76, viii | date = June 2008 | pmid = 18452807 | doi = 10.1016/j.idc.2007.12.010 }}</ref> | |||
| <ref name=managing_deer_2007>{{cite book |title=Managing Urban Deer in Connecticut |chapter=Figure 2: Changes in deer density and cases of Lyme disease in Mumford Cove, Connecticut, 1996–2004 (CT DEP data) |page=4 |publisher=Connecticut Department of Environmental Protection – Wildlife Division |edition=2nd |date=June 2007 |chapter-url=http://www.ct.gov/deep/lib/deep/wildlife/pdf_files/game/urbandeer07.pdf |url-status=live |archive-url=https://web.archive.org/web/20130602194618/http://www.ct.gov/deep/lib/deep/wildlife/pdf_files/game/urbandeer07.pdf |archive-date=2 June 2013 }}</ref> | |||
| <ref name=mullegger_2004>{{cite journal | vauthors = Mullegger RR | title = Dermatological manifestations of Lyme borreliosis | journal = European Journal of Dermatology | volume = 14 | issue = 5 | pages = 296–309 | year = 2004 | pmid = 15358567 | url = http://www.jle.com/medline.md?issn=1167-1122&vol=14&iss=5&page=296 }}</ref> | |||
| <ref name=Jowi_2005>{{cite journal | vauthors = Jowi JO, Gathua SN | title = Lyme disease: report of two cases | journal = East African Medical Journal | volume = 82 | issue = 5 | pages = 267–269 | date = May 2005 | pmid = 16119758 | doi = 10.4314/eamj.v82i5.9318 }}</ref> | |||
| <ref name=merck_2012>{{cite web|title=Glomerular Disease|url=http://www.merckvetmanual.com/pharmacology/systemic-pharmacotherapeutics-of-the-urinary-system/glomerular-disease|publisher=The Merck Veterinary Manual.|access-date=19 May 2017|url-status=live|archive-url=https://web.archive.org/web/20170626001610/http://www.merckvetmanual.com/pharmacology/systemic-pharmacotherapeutics-of-the-urinary-system/glomerular-disease|archive-date=26 June 2017}}</ref> | |||
| <ref name="Khasnis">{{cite journal | vauthors = Khasnis AA, Nettleman MD | title = Global warming and infectious disease | journal = Archives of Medical Research | volume = 36 | issue = 6 | pages = 689–696 | year = 2005 | pmid = 16216650 | doi = 10.1016/j.arcmed.2005.03.041 }}</ref> | |||
| <ref name=Li_1998>{{cite journal | vauthors = Li M, Masuzawa T, Takada N, Ishiguro F, Fujita H, Iwaki A, Wang H, Wang J, Kawabata M, Yanagihara Y | title = Lyme disease Borrelia species in northeastern China resemble those isolated from far eastern Russia and Japan | journal = Applied and Environmental Microbiology | volume = 64 | issue = 7 | pages = 2705–2709 | date = July 1998 | pmid = 9647853 | pmc = 106449 | doi = 10.1128/AEM.64.7.2705-2709.1998 | bibcode = 1998ApEnM..64.2705L }}</ref> | |||
| <ref name=Muhlemann_1987>{{cite journal | vauthors = Muhlemann MF, Wright DJ | title = Emerging pattern of Lyme disease in the United Kingdom and Irish Republic | journal = Lancet | volume = 1 | issue = 8527 | pages = 260–262 | date = January 1987 | pmid = 2880076 | doi = 10.1016/S0140-6736(87)90074-2 | s2cid = 25295954 }}</ref> | |||
| <ref name=londong_2008>{{cite web|url=http://legacy.london.gov.uk/mayor/publications/2008/docs/climate-change-adapt-strat.pdf|title= The London climate change adaptation strategy - Draft report|publisher=]|date= August 2008|archive-url=https://web.archive.org/web/20120817222243/http://legacy.london.gov.uk/mayor/publications/2008/docs/climate-change-adapt-strat.pdf|archive-date=17 August 2012}}</ref> | |||
| <ref name=min_ag_2012>{{cite web |author=BC Ministry of Agriculture |url=http://www.agf.gov.bc.ca/cropprot/ticksbc.htm |title=Ticks and Humans in British Columbia |publisher=Agf.gov.bc.ca |access-date=15 December 2012 |url-status=dead |archive-url=https://web.archive.org/web/20130103031719/http://www.agf.gov.bc.ca/cropprot/ticksbc.htm |archive-date=3 January 2013 }}</ref> | |||
| <ref name=Leighton_2012>{{cite journal | vauthors = Leighton PA, Koffi JK, Pelcat Y, Lindsay LR, Ogden NH |doi=10.1111/j.1365-2664.2012.02112.x |title=Predicting the speed of tick invasion: An empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada |year=2012 |journal=Journal of Applied Ecology |volume=49 |issue=2 |pages=457–64|bibcode=2012JApEc..49..457L |s2cid=16921155 |doi-access=free }}</ref> | |||
| <ref name=mmwr_2007>{{cite journal | title = Lyme disease--United States, 2003-2005 | journal = MMWR. Morbidity and Mortality Weekly Report | volume = 56 | issue = 23 | pages = 573–576 | date = June 2007 | pmid = 17568368 | url = https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5623a1.htm | url-status = live | archive-url = https://web.archive.org/web/20121119113810/http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5623a1.htm | archive-date = 19 November 2012 | author1 = Centers for Disease Control and Prevention (CDC) }}</ref> | |||
| <ref name=Mantovani_2007>{{cite journal | vauthors = Mantovani E, Costa IP, Gauditano G, Bonoldi VL, Higuchi ML, Yoshinari NH | title = Description of Lyme disease-like syndrome in Brazil. Is it a new tick borne disease or Lyme disease variation? | journal = Brazilian Journal of Medical and Biological Research = Revista Brasileira de Pesquisas Medicas e Biologicas | volume = 40 | issue = 4 | pages = 443–456 | date = April 2007 | pmid = 17401487 | doi = 10.1590/S0100-879X2006005000082 | doi-access = free }}</ref> | |||
| <ref name="The ecology of infectious disease">{{cite journal | vauthors = LoGiudice K, Ostfeld RS, Schmidt KA, Keesing F | title = The ecology of infectious disease: effects of host diversity and community composition on Lyme disease risk | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 100 | issue = 2 | pages = 567–571 | date = January 2003 | pmid = 12525705 | pmc = 141036 | doi = 10.1073/pnas.0233733100 | doi-access = free | bibcode = 2003PNAS..100..567L }}</ref> | |||
| <ref name="Marques">{{cite journal | vauthors = Marques A | title = Chronic Lyme disease: a review | journal = Infectious Disease Clinics of North America | volume = 22 | issue = 2 | pages = 341–60, vii–viii | date = June 2008 | pmid = 18452806 | pmc = 2430045 | doi = 10.1016/j.idc.2007.12.011 }}</ref> | |||
| <ref name="ngautopsy">{{cite magazine | vauthors = Hall SS | url = http://ngm.nationalgeographic.com/2011/11/iceman-autopsy/hall-text | title = Iceman Autopsy | date = November 2011 | access-date = 17 October 2011 | magazine = ] | url-status=dead | archive-url = https://web.archive.org/web/20111019172457/http://ngm.nationalgeographic.com/2011/11/iceman-autopsy/hall-text | archive-date = 19 October 2011}}</ref> | |||
| <ref name=Paschoud_1954>{{cite journal | vauthors = Paschoud JM | title = | language = de | journal = Dermatologica | volume = 108 | issue = 4–6 | pages = 435–437 | year = 1954 | pmid = 13190934 | trans-title = Lymphocytoma after tick bite }}</ref> | |||
| <ref name=Oldstone_1998>{{cite journal | vauthors = ] | title = Molecular mimicry and immune-mediated diseases | journal = FASEB Journal | volume = 12 | issue = 13 | pages = 1255–1265 | date = October 1998 | pmid = 9761770 | pmc = 7164021 | doi = 10.1096/fasebj.12.13.1255 | doi-access = free | s2cid = 16089636 }}</ref> | |||
| <ref name=Pachner_1989>{{cite journal | vauthors = Pachner AR | title = Neurologic manifestations of Lyme disease, the new "great imitator" | journal = Reviews of Infectious Diseases | volume = 11 | issue = Suppl 6 | pages = S1482–S1486 | year = 1989 | pmid = 2682960 | doi = 10.1093/clinids/11.Supplement_6.S1482 | s2cid = 3862308 }}</ref> | |||
| <!-- Not in use | |||
| <ref name="Perkins">{{cite journal | vauthors = Perkins SE, Cattadori IM, Tagliapietra V, Rizzoli AP, Hudson PJ | title = Localized deer absence leads to tick amplification | journal = Ecology | volume = 87 | issue = 8 | pages = 1981–6 | date = August 2006 | pmid = 16937637 | doi = 10.1890/0012-9658(2006)872.0.CO;2 | citeseerx = 10.1.1.218.7660 }}</ref> | |||
| Not in use--> | |||
| <ref name="piesman2002">{{cite journal | vauthors = Piesman J, Dolan MC | title = Protection against lyme disease spirochete transmission provided by prompt removal of nymphal Ixodes scapularis (Acari: Ixodidae) | journal = Journal of Medical Entomology | volume = 39 | issue = 3 | pages = 509–512 | date = May 2002 | pmid = 12061448 | doi = 10.1603/0022-2585-39.3.509 | s2cid = 39805040 | doi-access = free }}</ref> | |||
| <ref name=Ogden_2009>{{cite journal | vauthors = Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H | title = The emergence of Lyme disease in Canada | journal = CMAJ | volume = 180 | issue = 12 | pages = 1221–1224 | date = June 2009 | pmid = 19506281 | pmc = 2691438 | doi = 10.1503/cmaj.080148 }}</ref> | |||
| <ref name="nytimes.com">{{cite news | url=https://www.nytimes.com/2003/05/20/health/montana-lab-tries-to-identify-tick-borne-disease.html | title=Montana Lab Tries to Identify Tick-Borne Disease | date=20 May 2003 | vauthors = Robbins J | newspaper=The New York Times | url-status=live | archive-url=https://web.archive.org/web/20170903080910/http://www.nytimes.com/2003/05/20/health/montana-lab-tries-to-identify-tick-borne-disease.html | archive-date=3 September 2017}}</ref> | |||
| <ref name="Patz">{{cite journal | vauthors = Patz JA, Daszak P, Tabor GM, Aguirre AA, Pearl M, Epstein J, Wolfe ND, Kilpatrick AM, Foufopoulos J, Molyneux D, Bradley DJ | title = Unhealthy landscapes: Policy recommendations on land use change and infectious disease emergence | journal = Environmental Health Perspectives | volume = 112 | issue = 10 | pages = 1092–1098 | date = July 2004 | pmid = 15238283 | pmc = 1247383 | doi = 10.1289/ehp.6877 | bibcode = 2004EnvHP.112.1092P }}</ref> | |||
| <ref name="nejm-feder">{{cite journal | vauthors = Feder HM, Johnson BJ, O'Connell S, Shapiro ED, Steere AC, Wormser GP, Agger WA, Artsob H, Auwaerter P, Dumler JS, Bakken JS, Bockenstedt LK, Green J, Dattwyler RJ, Munoz J, Nadelman RB, Schwartz I, Draper T, McSweegan E, Halperin JJ, Klempner MS, Krause PJ, Mead P, Morshed M, Porwancher R, Radolf JD, Smith RP, Sood S, Weinstein A, Wong SJ, Zemel L | title = A critical appraisal of "chronic Lyme disease" | journal = The New England Journal of Medicine | volume = 357 | issue = 14 | pages = 1422–1430 | date = October 2007 | pmid = 17914043 | doi = 10.1056/NEJMra072023 | s2cid = 35285261 | others = Ad Hoc International Lyme Disease Group: Agger WA, Artsob H, Auwaerter P, Dumler JS, Bakken JS, Bockenstedt LK, Green J, Dattwyler RJ, Munoz J, Nadelman RB, Schwartz I, Draper T, McSweegan E, Halperin JJ, Klempner MS, Krause PJ, Mead P, Morshed M, Porwancher R, Radolf JD, Smith RP, Sood S, Weinstein A, Wong SJ, Zemel L }}</ref> | |||
| <ref name="nih-cld">{{cite web | publisher = ] | title = "Chronic Lyme Disease" Fact Sheet | date = 17 April 2009 | url = https://www.niaid.nih.gov/topics/lymedisease/understanding/pages/chronic.aspx | url-status=live | archive-date = 15 December 2012 | archive-url = https://archive.today/20121215073909/http://www.niaid.nih.gov/topics/lymedisease/understanding/pages/chronic.aspx}}</ref> | |||
| <ref name="pmid12905137">{{cite journal | vauthors = Steere AC, Sikand VK, Schoen RT, Nowakowski J | title = Asymptomatic infection with Borrelia burgdorferi | journal = Clinical Infectious Diseases | volume = 37 | issue = 4 | pages = 528–532 | date = August 2003 | pmid = 12905137 | doi = 10.1086/376914 | doi-access = free }} (primary source)</ref> | |||
| <ref name="pmid14987414">{{cite journal | vauthors = Auwaerter PG, Aucott J, Dumler JS | title = Lyme borreliosis (Lyme disease): molecular and cellular pathobiology and prospects for prevention, diagnosis and treatment | journal = Expert Reviews in Molecular Medicine | volume = 6 | issue = 2 | pages = 1–22 | date = January 2004 | pmid = 14987414 | doi = 10.1017/S1462399404007276 | s2cid = 24311718 }}</ref> | |||
| <ref name=pmid15117014>{{cite journal | vauthors = Lo Re V, Occi JL, MacGregor RR | title = Identifying the vector of Lyme disease | journal = American Family Physician | volume = 69 | issue = 8 | pages = 1935–1937 | date = April 2004 | pmid = 15117014 | url = http://www.aafp.org/link_out?pmid=15117014 }}</ref> | |||
| <ref name="pmid15085185">{{cite journal | vauthors = Steere AC, Coburn J, Glickstein L | title = The emergence of Lyme disease | journal = The Journal of Clinical Investigation | volume = 113 | issue = 8 | pages = 1093–1101 | date = April 2004 | pmid = 15085185 | pmc = 385417 | doi = 10.1172/JCI21681 }}</ref> | |||
| <ref name=pmid11450660>{{cite journal | vauthors = Steere AC | title = Lyme disease | journal = The New England Journal of Medicine | volume = 345 | issue = 2 | pages = 115–125 | date = July 2001 | pmid = 11450660 | doi = 10.1056/NEJM200107123450207 }}</ref> | |||
| <ref name="pmid15709249">{{cite journal | vauthors = Eisen L, Eisen RJ, Lane RS | title = The roles of birds, lizards, and rodents as hosts for the western black-legged tick Ixodes pacificus | journal = Journal of Vector Ecology | volume = 29 | issue = 2 | pages = 295–308 | date = December 2004 | pmid = 15709249 }}</ref> | |||
| <ref name="pmid16995383">{{cite journal | vauthors = Lane RS, Mun J, Eisen L, Eisen RJ | title = Refractoriness of the western fence lizard (Sceloporus occidentalis) to the Lyme disease group spirochete Borrelia bissettii | journal = The Journal of Parasitology | volume = 92 | issue = 4 | pages = 691–696 | date = August 2006 | pmid = 16995383 | doi = 10.1645/GE-738R1.1 | s2cid = 24200639 }}</ref> | |||
| <ref name=pmid17041141>{{cite journal | vauthors = Swanson SJ, Neitzel D, Reed KD, Belongia EA | title = Coinfections acquired from ixodes ticks | journal = Clinical Microbiology Reviews | volume = 19 | issue = 4 | pages = 708–727 | date = October 2006 | pmid = 17041141 | pmc = 1592693 | doi = 10.1128/CMR.00011-06 }}</ref> | |||
| <ref name="pmid17509489">{{cite journal | vauthors = Pachner AR, Steiner I | title = Lyme neuroborreliosis: infection, immunity, and inflammation | journal = The Lancet. Neurology | volume = 6 | issue = 6 | pages = 544–552 | date = June 2007 | pmid = 17509489 | doi = 10.1016/S1474-4422(07)70128-X | s2cid = 11600373 }}</ref> | |||
| <ref name="pmid16698304">{{cite journal | vauthors = Fikrig E, Narasimhan S | title = Borrelia burgdorferi--traveling incognito? | journal = Microbes and Infection | volume = 8 | issue = 5 | pages = 1390–1399 | date = April 2006 | pmid = 16698304 | doi = 10.1016/j.micinf.2005.12.022 | doi-access = free }}</ref> | |||
| <ref name="pmid17404293">{{cite journal | vauthors = Xu Q, Seemanapalli SV, Reif KE, Brown CR, Liang FT | title = Increasing the recruitment of neutrophils to the site of infection dramatically attenuates Borrelia burgdorferi infectivity | journal = Journal of Immunology | volume = 178 | issue = 8 | pages = 5109–5115 | date = April 2007 | pmid = 17404293 | doi = 10.4049/jimmunol.178.8.5109 | doi-access = free }}</ref> | |||
| <ref name="pmid17600717">{{cite journal | vauthors = Cabello FC, Godfrey HP, Newman SA | title = Hidden in plain sight: Borrelia burgdorferi and the extracellular matrix | journal = Trends in Microbiology | volume = 15 | issue = 8 | pages = 350–354 | date = August 2007 | pmid = 17600717 | doi = 10.1016/j.tim.2007.06.003 | url = https://touroscholar.touro.edu/nymc_fac_pubs/1685 | access-date = 5 July 2019 | url-status = live | archive-url = https://web.archive.org/web/20190707110727/https://touroscholar.touro.edu/nymc_fac_pubs/1685/ | archive-date = 7 July 2019 }}</ref> | |||
| <ref name="pmid18140373">{{cite journal | vauthors = Thyresson N | title = The penicillin treatment of acrodermatitis atrophicans chronica (Herxheimer) | journal = Acta Dermato-Venereologica | volume = 29 | issue = 6 | pages = 572–621 | year = 1949 | pmid = 18140373 }}</ref> | |||
| <ref name="pmid11438915">{{cite journal | vauthors = Molloy PJ, Persing DH, Berardi VP | title = False-positive results of PCR testing for Lyme disease | journal = Clinical Infectious Diseases | volume = 33 | issue = 3 | pages = 412–413 | date = August 2001 | pmid = 11438915 | doi = 10.1086/321911 | doi-access = free }}</ref> | |||
| <ref name="pmid18452805">{{cite journal | vauthors = Stanek G, Strle F | title = Lyme disease: European perspective | journal = Infectious Disease Clinics of North America | volume = 22 | issue = 2 | pages = 327–39, vii | date = June 2008 | pmid = 18452805 | doi = 10.1016/j.idc.2008.01.001 }}</ref> | |||
| <ref name="pmid18452802">{{cite journal | vauthors = Puius YA, Kalish RA | title = Lyme arthritis: pathogenesis, clinical presentation, and management | journal = Infectious Disease Clinics of North America | volume = 22 | issue = 2 | pages = 289–300, vi–vii | date = June 2008 | pmid = 18452802 | doi = 10.1016/j.idc.2007.12.014 }}</ref> | |||
| <ref name="pmid18454594">{{cite journal | vauthors = Schneider BS, Schriefer ME, Dietrich G, Dolan MC, Morshed MG, Zeidner NS | title = Borrelia bissettii isolates induce pathology in a murine model of disease | journal = Vector Borne and Zoonotic Diseases | volume = 8 | issue = 5 | pages = 623–633 | date = October 2008 | pmid = 18454594 | doi = 10.1089/vbz.2007.0251 | url = https://zenodo.org/record/1235289 | access-date = 29 January 2020 | url-status = live | archive-url = https://web.archive.org/web/20200129005244/https://zenodo.org/record/1235289 | archive-date = 29 January 2020 }}</ref> | |||
| <ref name="pmid16020686">{{cite journal | vauthors = Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser GP | title = Diagnosis of lyme borreliosis | journal = Clinical Microbiology Reviews | volume = 18 | issue = 3 | pages = 484–509 | date = July 2005 | pmid = 16020686 | pmc = 1195970 | doi = 10.1128/CMR.18.3.484-509.2005 }}</ref> | |||
| <ref name="pmid23319969">{{cite journal | vauthors = Biesiada G, Czepiel J, Leśniak MR, Garlicki A, Mach T | title = Lyme disease: review | journal = Archives of Medical Science | volume = 8 | issue = 6 | pages = 978–982 | date = December 2012 | pmid = 23319969 | pmc = 3542482 | doi = 10.5114/aoms.2012.30948 }}</ref> | |||
| <ref name="pmid15623946">{{cite journal | vauthors = Masuzawa T | title = Terrestrial distribution of the Lyme borreliosis agent Borrelia burgdorferi sensu lato in East Asia | journal = Japanese Journal of Infectious Diseases | volume = 57 | issue = 6 | pages = 229–235 | date = December 2004 | doi = 10.7883/yoken.JJID.2004.229 | pmid = 15623946 | url = http://www0.nih.go.jp/JJID/57/229.html | url-status = live | archive-url = https://web.archive.org/web/20130122210956/http://www0.nih.go.jp/JJID/57/229.html | archive-date = 22 January 2013 }}</ref> | |||
| <ref name="pmid18650352">{{cite journal | vauthors = Rudenko N, Golovchenko M, Mokrácek A, Piskunová N, Ruzek D, Mallatová N, Grubhoffer L | title = Detection of Borrelia bissettii in cardiac valve tissue of a patient with endocarditis and aortic valve stenosis in the Czech Republic | journal = Journal of Clinical Microbiology | volume = 46 | issue = 10 | pages = 3540–3543 | date = October 2008 | pmid = 18650352 | pmc = 2566110 | doi = 10.1128/JCM.01032-08 }}</ref> | |||
| <ref name=pmid18452798>{{cite journal | vauthors = Tilly K, Rosa PA, Stewart PE | title = Biology of infection with Borrelia burgdorferi | journal = Infectious Disease Clinics of North America | volume = 22 | issue = 2 | pages = 217–34, v | date = June 2008 | pmid = 18452798 | pmc = 2440571 | doi = 10.1016/j.idc.2007.12.013 }}</ref> | |||
| <ref name="pmid16819127">{{cite journal | vauthors = Smith R, Takkinen J | title = Lyme borreliosis: Europe-wide coordinated surveillance and action needed? | journal = Euro Surveillance | volume = 11 | issue = 6 | pages = E060622.1 | date = June 2006 | pmid = 16819127 | doi = 10.2807/esw.11.25.02977-en | doi-access = free }}</ref> | |||
| <ref name="pmid17130658">{{cite journal | vauthors = Lopes de Carvalho I, Núncio MS | title = Laboratory diagnosis of Lyme borreliosis at the Portuguese National Institute of Health (1990-2004) | journal = Euro Surveillance | volume = 11 | issue = 10 | pages = 257–260 | year = 2006 | pmid = 17130658 | url = http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=650 | url-status = live | archive-url = https://web.archive.org/web/20120617082119/http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=650 | archive-date = 17 June 2012 }}</ref> | |||
| <ref name="pmid9215633">{{cite journal | vauthors = Coleman JL, Gebbia JA, Piesman J, Degen JL, Bugge TH, Benach JL | title = Plasminogen is required for efficient dissemination of B. burgdorferi in ticks and for enhancement of spirochetemia in mice | journal = Cell | volume = 89 | issue = 7 | pages = 1111–1119 | date = June 1997 | pmid = 9215633 | doi = 10.1016/S0092-8674(00)80298-6 | s2cid = 18750257 | doi-access = free }}</ref> | |||
| <ref name="pmid16820453">{{cite journal | vauthors = Richter D, Matuschka FR | title = Perpetuation of the Lyme disease spirochete Borrelia lusitaniae by lizards | journal = Applied and Environmental Microbiology | volume = 72 | issue = 7 | pages = 4627–4632 | date = July 2006 | pmid = 16820453 | pmc = 1489336 | doi = 10.1128/AEM.00285-06 | bibcode = 2006ApEnM..72.4627R }}</ref> | |||
| <ref name=Ribeiro_1987>{{cite journal | vauthors = Ribeiro JM, Mather TN, Piesman J, Spielman A | title = Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae) | journal = Journal of Medical Entomology | volume = 24 | issue = 2 | pages = 201–205 | date = March 1987 | pmid = 3585913 | doi = 10.1093/jmedent/24.2.201 }}</ref> | |||
| <ref name="pmid17417956">{{cite journal | vauthors = Swanson KI, Norris DE | title = Detection of Borrelia burgdorferi DNA in lizards from Southern Maryland | journal = Vector Borne and Zoonotic Diseases | volume = 7 | issue = 1 | pages = 42–49 | year = 2007 | pmid = 17417956 | pmc = 4128253 | doi = 10.1089/vbz.2006.0548 }}</ref> | |||
| <ref name="pmid18097481">{{cite journal | vauthors = Rupprecht TA, Koedel U, Fingerle V, Pfister HW | title = The pathogenesis of lyme neuroborreliosis: from infection to inflammation | journal = Molecular Medicine | volume = 14 | issue = 3–4 | pages = 205–212 | year = 2008 | pmid = 18097481 | pmc = 2148032 | doi = 10.2119/2007-00091.Rupprecht | url = http://molmed.org/journal/articles/3/1398 | url-status = live | archive-url = https://web.archive.org/web/20150403135500/http://molmed.org/journal/articles/3/1398 | archive-date = 3 April 2015 }}</ref> | |||
| <ref name="pmid17326941">{{cite journal | vauthors = Majláthová V, Majláth I, Derdáková M, Víchová B, Pet'ko B | title = Borrelia lusitaniae and green lizards (Lacerta viridis), Karst Region, Slovakia | journal = Emerging Infectious Diseases | volume = 12 | issue = 12 | pages = 1895–1901 | date = December 2006 | pmid = 17326941 | pmc = 3291370 | doi = 10.3201/eid1212.060784 }}</ref> | |||
| <ref name="pmid17427701">{{cite journal | vauthors = Amore G, Tomassone L, Grego E, Ragagli C, Bertolotti L, Nebbia P, Rosati S, Mannelli A | title = Borrelia lusitaniae in immature Ixodes ricinus (Acari: Ixodidae) feeding on common wall lizards in Tuscany, central Italy | journal = Journal of Medical Entomology | volume = 44 | issue = 2 | pages = 303–307 | date = March 2007 | pmid = 17427701 | doi = 10.1603/0022-2585(2007)442.0.CO;2 | doi-broken-date = 1 December 2024 | s2cid = 18882042 }}</ref> | |||
| <!-- <ref name=samuels_2010>{{cite book | veditors =Samuels DS, Radolf JD | year=2010 |title=Borrelia: Molecular Biology, Host Interaction and Pathogenesis | publisher=Caister Academic Press | isbn= 978-1-904455-58-5 | chapter=Chapter 6, Structure, Function and Biogenesis of the ''Borrelia'' Cell Envelope}}</ref> --> | |||
| <ref name="pmid17522387">{{cite journal | vauthors = Halperin JJ, Shapiro ED, Logigian E, Belman AL, Dotevall L, Wormser GP, Krupp L, Gronseth G, Bever CT | title = Practice parameter: treatment of nervous system Lyme disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology | journal = Neurology | volume = 69 | issue = 1 | pages = 91–102 | date = July 2007 | pmid = 17522387 | doi = 10.1212/01.wnl.0000265517.66976.28 | doi-access = free }}</ref> | |||
| <ref name=Scrimenti_1970>{{cite journal | vauthors = Scrimenti RJ | title = Erythema chronicum migrans | journal = Archives of Dermatology | volume = 102 | issue = 1 | pages = 104–105 | date = July 1970 | pmid = 5497158 | doi = 10.1001/archderm.102.1.104 }}</ref> | |||
| <ref name="pmid17626342">{{cite journal | vauthors = Giery ST, Ostfeld RS | title = The role of lizards in the ecology of Lyme disease in two endemic zones of the northeastern United States | journal = The Journal of Parasitology | volume = 93 | issue = 3 | pages = 511–517 | date = June 2007 | pmid = 17626342 | doi = 10.1645/GE-1053R1.1 | s2cid = 42617030 }}</ref> | |||
| <ref name=Sherris>{{cite book | veditors = Ryan KJ, Ray CG | title = Sherris Medical Microbiology | url = https://archive.org/details/sherrismedicalmi00ryan | url-access = limited | edition = 4th | pages = –37 | publisher = McGraw Hill | year = 2004 | isbn = 978-0-8385-8529-0}}</ref> | |||
| <ref name=Shadick>{{cite journal | vauthors = Shadick NA, Phillips CB, Sangha O, Logigian EL, Kaplan RF, Wright EA, Fossel AH, Fossel K, Berardi V, Lew RA, Liang MH | title = Musculoskeletal and neurologic outcomes in patients with previously treated Lyme disease | journal = Annals of Internal Medicine | volume = 131 | issue = 12 | pages = 919–926 | date = December 1999 | pmid = 10610642 | doi = 10.7326/0003-4819-131-12-199912210-00003 | s2cid = 20746489 }}</ref> | |||
| <ref name=Raveche_2005>{{cite journal | vauthors = Raveche ES, Schutzer SE, Fernandes H, Bateman H, McCarthy BA, Nickell SP, Cunningham MW | title = Evidence of Borrelia autoimmunity-induced component of Lyme carditis and arthritis | journal = Journal of Clinical Microbiology | volume = 43 | issue = 2 | pages = 850–856 | date = February 2005 | pmid = 15695691 | pmc = 548028 | doi = 10.1128/JCM.43.2.850-856.2005 }}</ref> | |||
| <ref name=seltzer_2000>{{cite journal | vauthors = Seltzer EG, Gerber MA, Cartter ML, Freudigman K, Shapiro ED | title = Long-term outcomes of persons with Lyme disease | journal = JAMA | volume = 283 | issue = 5 | pages = 609–616 | date = February 2000 | pmid = 10665700 | doi = 10.1001/jama.283.5.609 | doi-access = free }}</ref> | |||
| <ref name="pmid8272083">{{cite journal | vauthors = Nocton JJ, Dressler F, Rutledge BJ, Rys PN, Persing DH, Steere AC | title = Detection of Borrelia burgdorferi DNA by polymerase chain reaction in synovial fluid from patients with Lyme arthritis | journal = The New England Journal of Medicine | volume = 330 | issue = 4 | pages = 229–234 | date = January 1994 | pmid = 8272083 | doi = 10.1056/NEJM199401273300401 | doi-access = free }}</ref> | |||
| <ref name=Stanek2011>{{cite journal | vauthors = Stanek G, Reiter M | title = The expanding Lyme Borrelia complex--clinical significance of genomic species? | journal = Clinical Microbiology and Infection | volume = 17 | issue = 4 | pages = 487–493 | date = April 2011 | pmid = 21414082 | doi = 10.1111/j.1469-0691.2011.03492.x | doi-access = free }}</ref> | |||
| <ref name=pmid20207198>{{cite journal | vauthors = Little SE, Heise SR, Blagburn BL, Callister SM, Mead PS | title = Lyme borreliosis in dogs and humans in the USA | journal = Trends in Parasitology | volume = 26 | issue = 4 | pages = 213–218 | date = April 2010 | pmid = 20207198 | doi = 10.1016/j.pt.2010.01.006 }}</ref> | |||
| <ref name=pmid20933139>{{cite journal | vauthors = Krupka I, Straubinger RK | title = Lyme borreliosis in dogs and cats: background, diagnosis, treatment and prevention of infections with Borrelia burgdorferi sensu stricto | journal = The Veterinary Clinics of North America. Small Animal Practice | volume = 40 | issue = 6 | pages = 1103–1119 | date = November 2010 | pmid = 20933139 | doi = 10.1016/j.cvsm.2010.07.011 }}</ref> | |||
| <ref name=Steere_1977>{{cite journal | vauthors = Steere AC, Malawista SE, Snydman DR, Shope RE, Andiman WA, Ross MR, Steele FM | title = Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three Connecticut communities | journal = Arthritis and Rheumatism | volume = 20 | issue = 1 | pages = 7–17 | year = 1977 | pmid = 836338 | doi = 10.1002/art.1780200102 | s2cid = 43397837 }}</ref> | |||
| <ref name="pmid21794218">{{cite journal | vauthors = Rizzoli A, Hauffe H, Carpi G, Vourc'h IG, Neteler M, Rosa R | title = Lyme borreliosis in Europe | journal = Euro Surveillance | volume = 16 | issue = 27 | date = July 2011 | pmid = 21794218 | url = http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19906 | url-status = live | archive-url = https://web.archive.org/web/20110709084836/http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19906 | archive-date = 9 July 2011 }}</ref> | |||
| <ref name=Steere_1983>{{cite journal | vauthors = Steere AC, Hutchinson GJ, Rahn DW, Sigal LH, Craft JE, DeSanna ET, Malawista SE | title = Treatment of the early manifestations of Lyme disease | journal = Annals of Internal Medicine | volume = 99 | issue = 1 | pages = 22–26 | date = July 1983 | pmid = 6407378 | doi = 10.7326/0003-4819-99-1-22 }}</ref> | |||
| <ref name="pmid2563850">{{cite journal | vauthors = Guy EC, Bateman DE, Martyn CN, Heckels JE, Lawton NF | title = Lyme disease: prevalence and clinical importance of Borrelia burgdorferi specific IgG in forestry workers | journal = Lancet | volume = 1 | issue = 8636 | pages = 484–486 | date = March 1989 | pmid = 2563850 | doi = 10.1016/S0140-6736(89)91377-9 | s2cid = 39557628 }}</ref> | |||
| <ref name="pmid8037992">{{cite journal | vauthors = Haywood GA, O'Connell S, Gray HH | title = Lyme carditis: a United Kingdom perspective | journal = British Heart Journal | volume = 70 | issue = 1 | pages = 15–16 | date = July 1993 | pmid = 8037992 | pmc = 1025222 | doi = 10.1136/hrt.70.1.15 }}</ref> | |||
| <ref name=Sternbach>{{cite journal | vauthors = Sternbach G, Dibble CL | title = Willy Burgdorfer: Lyme disease | journal = The Journal of Emergency Medicine | volume = 14 | issue = 5 | pages = 631–634 | year = 1996 | pmid = 8933327 | doi = 10.1016/S0736-4679(96)00143-6 | doi-access = free }}</ref> | |||
| <ref name="Rand">{{cite journal | vauthors = Rand PW, Lubelczyk C, Holman MS, Lacombe EH, Smith RP | title = Abundance of Ixodes scapularis (Acari: Ixodidae) after the complete removal of deer from an isolated offshore island, endemic for Lyme Disease | journal = Journal of Medical Entomology | volume = 41 | issue = 4 | pages = 779–784 | date = July 2004 | pmid = 15311475 | doi = 10.1603/0022-2585-41.4.779 | s2cid = 5853201 }}</ref> | |||
| <ref name=summerton_1995>{{cite journal |doi=10.1136/bmj.311.7018.1478 |title=Lyme disease in the eighteenth century |year=1995 | vauthors = Summerton N |journal=BMJ |volume=311 |issue=7018 |page=1478|s2cid=70661702 }}</ref> | |||
| <ref name=Poland_2001>{{cite journal | vauthors = Poland GA, Jacobson RM | title = The prevention of Lyme disease with vaccine | journal = Vaccine | volume = 19 | issue = 17–19 | pages = 2303–2308 | date = March 2001 | pmid = 11257352 | doi = 10.1016/S0264-410X(00)00520-X }}</ref> | |||
| <ref name=Sun_2003>{{cite journal | vauthors = Sun Y, Xu R | title = Ability of Ixodes persulcatus, Haemaphysalis concinna and Dermacentor silvarum ticks to acquire and transstadially transmit Borrelia garinii | journal = Experimental and Applied Acarology | volume = 31 | issue = 1–2 | pages = 151–160 | year = 2003 | pmid = 14756409 | doi = 10.1023/B:APPA.0000005119.30172.43 | s2cid = 19214181 }}</ref> | |||
| <ref name=rowe_199>{{cite news | url = https://www.nytimes.com/1999/06/13/nyregion/lukewarm-response-to-new-lyme-vaccine.html | title = Lukewarm Response To New Lyme Vaccine | vauthors = Rowe C | work = ] | date = 13 June 1999 | access-date = 11 July 2008 | url-status=live | archive-url = https://web.archive.org/web/20120210123556/http://www.nytimes.com/1999/06/13/nyregion/lukewarm-response-to-new-lyme-vaccine.html | archive-date = 10 February 2012}}</ref> | |||
| <ref name=Singh>{{cite journal | vauthors = Singh SK, Girschick HJ | title = Lyme borreliosis: from infection to autoimmunity | journal = Clinical Microbiology and Infection | volume = 10 | issue = 7 | pages = 598–614 | date = July 2004 | pmid = 15214872 | doi = 10.1111/j.1469-0691.2004.00895.x | doi-access = free }}</ref> | |||
| <ref name="safe">{{cite journal | vauthors = | title = When a vaccine is safe | journal = Nature | volume = 439 | issue = 7076 | pages = 509 | date = February 2006 | pmid = 16452935 | doi = 10.1038/439509a | doi-access = free | bibcode = 2006Natur.439Q.509. }}</ref> | |||
| <ref name="Walsh2007">{{cite journal | vauthors = Walsh CA, Mayer EW, Baxi LV | title = Lyme disease in pregnancy: case report and review of the literature | journal = Obstetrical & Gynecological Survey | volume = 62 | issue = 1 | pages = 41–50 | date = January 2007 | pmid = 17176487 | doi = 10.1097/01.ogx.0000251024.43400.9a | s2cid = 31929160 }}</ref> | |||
| <ref name=scotland_2012>{{cite web|url=http://www.scotland.gov.uk/Topics/Health/NHS-Scotland/publicact/Implementation/Timetable3333/Part2Guidance/Q/EditMode/on/ForceUpdate/on |title=Guidance on Part 2 – Notifiable Diseases, Notifiable Organisms and Health Risk States |publisher=Scotland.gov.uk |date=10 September 2012 |access-date=15 December 2012}}</ref> | |||
| <ref name=Weinstein_2002>{{cite journal | vauthors = Weinstein A, Britchkov M | title = Lyme arthritis and post-Lyme disease syndrome | journal = Current Opinion in Rheumatology | volume = 14 | issue = 4 | pages = 383–387 | date = July 2002 | pmid = 12118171 | doi = 10.1097/00002281-200207000-00008 }}</ref> | |||
| <ref name="Wormser">{{cite journal | vauthors = Wormser GP, Masters E, Nowakowski J, McKenna D, Holmgren D, Ma K, Ihde L, Cavaliere LF, Nadelman RB | title = Prospective clinical evaluation of patients from Missouri and New York with erythema migrans-like skin lesions | journal = Clinical Infectious Diseases | volume = 41 | issue = 7 | pages = 958–965 | date = October 2005 | pmid = 16142659 | doi = 10.1086/432935 | doi-access = free }}</ref> | |||
| <ref name=Wilske_2005>{{cite journal | vauthors = Wilske B | title = Epidemiology and diagnosis of Lyme borreliosis | journal = Annals of Medicine | volume = 37 | issue = 8 | pages = 568–579 | year = 2005 | pmid = 16338759 | doi = 10.1080/07853890500431934 | s2cid = 30818459 | doi-access = free }}</ref> | |||
| <ref name=Smith_2012>{{cite journal | vauthors = Smith FD, Ballantyne R, Morgan ER, Wall R | title = Estimating Lyme disease risk using pet dogs as sentinels | journal = Comparative Immunology, Microbiology and Infectious Diseases | volume = 35 | issue = 2 | pages = 163–167 | date = March 2012 | pmid = 22257866 | doi = 10.1016/j.cimid.2011.12.009 }}<br />Lay summary: {{cite press release | url = http://www.bris.ac.uk/news/2012/8176.html | date = 25 January 2012 | title = Survey of pet dogs indicates Lyme disease risk much greater than previous estimates suggest | publisher = University of Bristol }}</ref> | |||
| <ref name=staubinger>{{cite web| vauthors = Staubinger R |title=Lyme Disease|url=http://siriusdog.com/lyme-disease-spirochete-ticks-dog.htm|publisher=Sirius Dog.|access-date=10 February 2012|url-status=live|archive-url=https://web.archive.org/web/20120623204423/http://siriusdog.com/lyme-disease-spirochete-ticks-dog.htm|archive-date=23 June 2012|date=31 May 2000}}</ref>{{Unreliable source?|date=July 2013}} | |||
| <ref name="uphill">{{cite journal | vauthors = Abbott A | title = Lyme disease: uphill struggle | journal = Nature | volume = 439 | issue = 7076 | pages = 524–525 | date = February 2006 | pmid = 16452949 | doi = 10.1038/439524a | s2cid = 4315588 | doi-access = free }}</ref> | |||
| <ref name=vaccine_2008>{{cite news | url = https://www.nytimes.com/2002/02/28/business/sole-lyme-vaccine-is-pulled-off-market.html | title = Sole Lyme Vaccine Is Pulled Off Market | work = ] | date = 28 February 2002 | access-date = 11 July 2008 | url-status=live | archive-url = https://web.archive.org/web/20100830044423/http://www.nytimes.com/2002/02/28/business/sole-lyme-vaccine-is-pulled-off-market.html | archive-date = 30 August 2010}}</ref> | |||
| <ref name=wright_2012>{{cite journal | vauthors = Wright WF, Riedel DJ, Talwani R, Gilliam BL | title = Diagnosis and management of Lyme disease | journal = American Family Physician | volume = 85 | issue = 11 | pages = 1086–1093 | date = June 2012 | pmid = 22962880 | url = http://www.aafp.org/afp/2012/0601/p1086.html | url-status = live | archive-url = https://web.archive.org/web/20130927081243/http://www.aafp.org/afp/2012/0601/p1086.html | archive-date = 27 September 2013 }}</ref> | |||
| <ref name=Walder_2006>{{cite journal | vauthors = Walder G, Lkhamsuren E, Shagdar A, Bataa J, Batmunkh T, Orth D, Heinz FX, Danichova GA, Khasnatinov MA, Würzner R, Dierich MP | title = Serological evidence for tick-borne encephalitis, borreliosis, and human granulocytic anaplasmosis in Mongolia | journal = International Journal of Medical Microbiology | volume = 296 | issue = Suppl 40 | pages = 69–75 | date = May 2006 | pmid = 16524782 | doi = 10.1016/j.ijmm.2006.01.031 }}</ref> | |||
| <ref name=tick_bite>{{cite web | url = http://www.tickbitepreventionweek.org/overview.html | title = Overview Tick Bite Prevention Week | archive-url = https://web.archive.org/web/20120410220509/http://www.tickbitepreventionweek.org/overview.html | archive-date=10 April 2012 }}</ref> | |||
| <ref name="cdc_dispatch_oct_2007">{{cite journal | vauthors = Gordillo-Pérez G, Torres J, Solórzano-Santos F, de Martino S, Lipsker D, Velázquez E, Ramon G, Onofre M, Jaulhac B | title = Borrelia burgdorferi infection and cutaneous Lyme disease, Mexico | journal = Emerging Infectious Diseases | volume = 13 | issue = 10 | pages = 1556–1558 | date = October 2007 | pmid = 18258006 | pmc = 2851501 | doi = 10.3201/eid1310.060630 }}</ref> | |||
| <ref name=Yoshinari_1993>{{cite journal | vauthors = Yoshinari NH, Oyafuso LK, Monteiro FG, de Barros PJ, da Cruz FC, Ferreira LG, Bonasser F, Baggio D, Cossermelli W | title = | language = pt | journal = Revista do Hospital das Clinicas | volume = 48 | issue = 4 | pages = 170–174 | year = 1993 | pmid = 8284588 | trans-title = Lyme disease. Report of a case observed in Brazil }}</ref> | |||
| }} | }} | ||
| {{CDC|article=Post-Treatment Lyme Disease Syndrome|url=https://www.cdc.gov/lyme/postLDS/index.html}} | |||
| ==Further reading== | |||
| *{{cite book |author= Jonathan A. Edlow |year= 2004 |title= Bull's Eye: Unraveling the Medical Mystery of Lyme Disease |publisher= ] |edition= 2nd |isbn= 0300103700}} | |||
| *{{cite book |author= Richard Ostfeld |year= 2012 |title= Lyme Disease: The Ecology of a Complex System |publisher= ] |location= New York |isbn= 0199928479}} | |||
| *{{cite book |author= Pamela Weintraub |year= 2008 |title= Cure Unknown: Inside the Lyme Disease Epidemic |publisher= ] |isbn= 9780312378127}} | |||
| == Further reading == | |||
| ==External links== | |||
| <!-- Currently in ascending chronological order; an observation, not a personal preference. --> | |||
| * {{dmoz|/Health/Conditions_and_Diseases/Infectious_Diseases/Spirochetal/Lyme_Disease/Organizations/|Lyme disease organizations}} | |||
| {{refbegin}} | |||
| * : from the ] (CDC) | |||
| * {{cite book | vauthors = Ostfeld R |year= 2012 |title= Lyme Disease: The Ecology of a Complex System |publisher= ] |location= New York |isbn= 978-0-19-992847-7}} | |||
| * : from the ] | |||
| * {{cite book | vauthors = Barbour AG |title=Lyme disease: why it's spreading, how it makes you sick, and what to do about it |date=2015 |location=Baltimore | publisher = Johns Hopkins University Press |isbn=978-1-4214-1721-9}} | |||
| * ''The Merck Manual'' | |||
| * {{cite book | veditors = Halperin JJ |title=Lyme disease: an evidence-based approach |date=2018 |publisher=CABI |location=Wallingford, Oxfordshire, UK |isbn=978-1-78639-207-7 |edition=2nd}} | |||
| * - Lab Tests Online | |||
| * {{cite book | veditors = Radolf JD, Samuels DS |title=Lyme disease and relapsing fever spirochetes: genomics, molecular biology, host interactions and disease pathogenesis |date=2021 |publisher=Caister |location=Poole, UK |isbn=978-1-913652-61-6 |url=https://www.caister.com/lyme}} | |||
| * - Laboratory of Medical Zoology at the University of Massachusetts, Amherst | |||
| * {{cite web | vauthors = Oaklander M |date=June 17, 2021 |title=We Used to Have a Lyme Disease Vaccine. Are We Ready to Bring One Back? |url=https://time.com/6073576/lyme-disease-vaccine/ |magazine=]}} | |||
| * | |||
| {{refend}} | |||
| == External links == | |||
| {{Commons category|Borreliosis}} | |||
| * | |||
| * – Suggested Reporting Language, Interpretation and Guidance Regarding Lyme Disease Serologic Test Results | |||
| * | |||
| * | |||
| {{Medical condition classification and resources | |||
| | DiseasesDB = 1531 | |||
| | ICD10 = {{ICD10|A|69|2|a|65}} | |||
| | ICD9 = {{ICD9|088.81}} | |||
| | MedlinePlus = 001319 | |||
| | eMedicine_mult = {{eMedicine2|article|330178|330178}}<br />{{eMedicine2|article|965922|965922}}<br />{{eMedicine2|article|786767|786767}} | |||
| | MeshID = D008193 | |||
| | Scholia = Q201989 | |||
| |ICD10CM={{ICD10CM|A69.2}}|ICD11={{ICD11|1C1G}}}} | |||
| {{Tick-borne diseases}} | {{Tick-borne diseases}} | ||
| {{Gram-negative non-proteobacterial diseases}} | {{Gram-negative non-proteobacterial diseases}} | ||
| {{Bacterial cutaneous infections}} | |||
| {{Arthritis in children}} | |||
| {{Vaccines}} | |||
| {{Authority control}} | |||
| {{DEFAULTSORT:Lyme Disease}} | {{DEFAULTSORT:Lyme Disease}} | ||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | ] | ||
| {{Link GA|pl}} | |||
| {{Link FA|sl}} | |||
Latest revision as of 16:31, 23 December 2024
Infectious disease caused by Borrelia bacteria, spread by ticksNot to be confused with phytophotodermatitis, also known as "lime disease".
Medical condition
| Lyme disease | |
|---|---|
| Other names | Lyme borreliosis |
 | |
| An adult deer tick (most cases of Lyme are caused by nymphal rather than adult ticks) | |
| Specialty | Infectious disease |
| Symptoms | Expanding area of redness at the site of a tick bite, fever, headache, tiredness |
| Complications | Facial nerve paralysis, arthritis, meningitis-like symptoms, Heart rhythm irregularities |
| Usual onset | A week after a bite |
| Causes | Borrelia spread by ticks |
| Diagnostic method | Based on symptoms, tick exposure, blood tests |
| Prevention | Prevention of tick bites (clothing the limbs, DEET), doxycycline |
| Medication | Doxycycline, amoxicillin, ceftriaxone, cefuroxime |
| Frequency | ~476k/year in U.S. (a likely overestimate), 200k/year in Europe |
Lyme disease, also known as Lyme borreliosis, is a tick-borne disease caused by species of Borrelia bacteria, transmitted by blood-feeding ticks in the genus Ixodes. The most common sign of infection is an expanding red rash, known as erythema migrans (EM), which appears at the site of the tick bite about a week afterwards. The rash is typically neither itchy nor painful. Approximately 70–80% of infected people develop a rash. Early diagnosis can be difficult. Other early symptoms may include fever, headaches and tiredness. If untreated, symptoms may include loss of the ability to move one or both sides of the face, joint pains, severe headaches with neck stiffness or heart palpitations. Months to years later, repeated episodes of joint pain and swelling may occur. Occasionally, shooting pains or tingling in the arms and legs may develop.
Lyme disease is transmitted to humans by the bites of infected ticks of the genus Ixodes. In the United States, ticks of concern are usually of the Ixodes scapularis type. According to the Centers for Disease Control and Prevention, "In most cases, a tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted. If you remove a tick quickly (within 24 hours), you can greatly reduce your chances of getting Lyme disease." In Europe, Ixodes ricinus ticks may spread the bacteria more quickly. In North America, the bacterial species Borrelia burgdorferi and B. mayonii cause Lyme disease. In Europe and Asia, Borrelia afzelii, Borrelia garinii, B. spielmanii and four other species also cause the disease. The disease does not appear to be transmissible between people, by other animals nor through food. Diagnosis is based on a combination of symptoms, history of tick exposure and possibly testing for specific antibodies in the blood. Blood tests are often falsely negative in the early stages of the disease. Testing of individual ticks is not typically useful.
Prevention includes efforts to prevent tick bites by wearing clothing to cover the arms and legs and using DEET or picaridin-based insect repellents. Using pesticides to reduce tick numbers may also be effective. Ticks can be removed using tweezers. If the removed tick is full of blood a single dose of doxycycline may be used to prevent the development of infection but is not generally recommended since the development of infection is rare. If an infection develops, a number of antibiotics are effective, including doxycycline, amoxicillin and cefuroxime. Standard treatment usually lasts for two or three weeks. Some people develop a fever and muscle and joint pains from treatment, which may last for one or two days. In those who develop persistent symptoms, long-term antibiotic therapy has not been found to be useful.
Lyme disease is the most common disease spread by ticks in the Northern Hemisphere. Infections are most common in the spring and early summer. Lyme disease was diagnosed as a separate condition for the first time in 1975 in Lyme, Connecticut. It was originally mistaken for juvenile rheumatoid arthritis. The bacterium involved was first described in 1981 by Willy Burgdorfer. People with persistent symptoms after appropriate treatments are said to have Post-Treatment Lyme Disease Syndrome (PTLDS). PTLDS is different from chronic Lyme disease, a term no longer supported by scientists and used in different ways by different groups. Some healthcare providers claim that chronic Lyme is caused by persistent infection, but this is not believed to be true because no evidence of persistent infection can be found after standard treatment.
As of 2023, clinical trials of proposed human vaccines for Lyme disease were being carried out, but no vaccine was available. A vaccine, LYMERix, was produced, but discontinued in 2002 due to insufficient demand. There are several vaccines for the prevention of Lyme disease in dogs.
Signs and symptoms
Lyme disease can produce a broad range of symptoms.
-
 20% of Lyme rashes in the United States show a "bull's eye" or "target-like" appearance.
20% of Lyme rashes in the United States show a "bull's eye" or "target-like" appearance.
-
 Erythema migrans ("migrating redness") on a woman's neck. Rashes from non-Lyme causes may look similar.
Erythema migrans ("migrating redness") on a woman's neck. Rashes from non-Lyme causes may look similar.
The incubation period is usually one to two weeks, but can be much shorter (days) or much longer (months to years). Lyme symptoms most often occur from the month of May to September in the Northern Hemisphere because the nymphal stage of the tick is responsible for most cases.
Early localized infection
80% of Lyme infections begin with a rash of some sort at the site of a tick bite, often near skin folds such as the armpit, groin, back of the knee, or the trunk under clothing straps, or in children's hair, ears, or neck. Most people who get infected do not remember seeing a tick or a bite. The rash appears typically one or two weeks (range 3–32 days) after the bite and expands 2–3 cm per day up to a diameter of 5–70 cm (median is 16 cm).
The rash is usually circular or oval, red or bluish, and may have an elevated or darker center. This rash is termed an Erythema Migrans (EM) which translates as "Migrating Redness." In about 79% of cases in Europe, this rash gradually clears from the center toward the edges possibly forming a "bull's eye" or "target-like" pattern, but this clearing only happens in 19% of cases in endemic areas of the United States. The rash may feel warm, usually is not itchy, is rarely tender or painful, and takes up to four weeks to resolve if untreated.
The Lyme rash is often accompanied by symptoms of a flu-like illness, including fatigue, headache, body aches, fever, and chills . These symptoms may also appear without a rash or linger after the rash has disappeared. Lyme can progress to later stages without a rash or these symptoms.
People with high fever for more than two days or whose other symptoms of viral-like illness do not improve despite antibiotic treatment for Lyme disease, or who have abnormally low levels of white or red cells or platelets in the blood, should be investigated for possible coinfection with other tick-borne diseases such as ehrlichiosis and babesiosis.
Not everyone with Lyme disease has all the symptoms, and many of these symptoms can also occur with other diseases.
Asymptomatic infection exists, but occurs in less than 7% of infected individuals in the United States. Asymptomatic infection may be much more common among those infected in Europe.
Early disseminated infection
Within days to weeks after the onset of local infection, the Borrelia bacteria may spread through the lymphatic system or bloodstream. In 10–20% of untreated cases, EM rashes develop at sites across the body that bear no relation to the original tick bite. Transient muscle pains and joint pains are also common.
In about 10–15% of untreated people, Lyme causes neurological problems known as neuroborreliosis. Early neuroborreliosis typically appears 4–6 weeks (range 1–12 weeks) after the tick bite and involves some combination of lymphocytic meningitis, cranial neuritis, radiculopathy, and/or mononeuritis multiplex. Lymphocytic meningitis causes characteristic changes in the cerebrospinal fluid (CSF) and may be accompanied for several weeks by variable headache and, less commonly, usually mild meningitis signs such as inability to flex the neck fully and intolerance to bright lights but typically no or only very low fever. After several months neuroborreliosis can also present otolaryngological symptoms. Up to 76.5% of them present as tinnitus, the most common symptom. Vertigo and dizziness (53.7%) and hearing loss (16.7%) were the next most common symptoms. In children, partial loss of vision may also occur. Cranial neuritis is an inflammation of cranial nerves. When due to Lyme, it most typically causes facial palsy, impairing blinking, smiling, and chewing on one or both sides of the face. It may also cause intermittent double vision. Lyme radiculopathy is an inflammation of spinal nerve roots that often causes pain and less often weakness, numbness, or altered sensation in the areas of the body served by nerves connected to the affected roots, e.g. limb(s) or part(s) of trunk. The pain is often described as unlike any other previously felt, excruciating, migrating, worse at night, rarely symmetrical, and often accompanied by extreme sleep disturbance. Mononeuritis multiplex is an inflammation causing similar symptoms in one or more unrelated peripheral nerves. Rarely, early neuroborreliosis may involve inflammation of the brain or spinal cord, with symptoms such as confusion, abnormal gait, ocular movements, or speech, impaired movement, impaired motor planning, or shaking.
In North America, facial palsy is the typical early neuroborreliosis presentation, occurring in 5–10% of untreated people, in about 75% of cases accompanied by lymphocytic meningitis. Lyme radiculopathy is reported half as frequently, but many cases may be unrecognized. In European adults, the most common presentation is a combination of lymphocytic meningitis and radiculopathy known as Bannwarth syndrome, accompanied in 36-89% of cases by facial palsy. In this syndrome, radicular pain tends to start in the same body region as the initial erythema migrans rash, if there was one, and precedes possible facial palsy and other impaired movement. In extreme cases, permanent impairment of motor or sensory function of the lower limbs may occur. In European children, the most common manifestations are facial palsy (in 55%), other cranial neuritis, and lymphocytic meningitis (in 27%).
In about 4–10% of untreated cases in the United States and 0.3–4% of untreated cases in Europe, typically between June and December, about one month (range 4 days to 7 months) after the tick bite, the infection may cause heart complications known as Lyme carditis. Symptoms may include heart palpitations (in 69% of people), dizziness, fainting, shortness of breath, and chest pain. Other symptoms of Lyme disease may also be present, such as EM rash, joint aches, facial palsy, headaches, or radicular pain. In some people, however, carditis may be the first manifestation of Lyme disease. Lyme carditis in 19–87% of people adversely impacts the heart's electrical conduction system, causing atrioventricular block that often manifests as heart rhythms that alternate within minutes between abnormally slow and abnormally fast. In 10–15% of people, Lyme causes myocardial complications such as cardiomegaly, left ventricular dysfunction, or congestive heart failure.
Another skin condition, found in Europe but not in North America, is borrelial lymphocytoma, a purplish lump that develops on the ear lobe, nipple, or scrotum.
Late disseminated infection

Lyme arthritis occurs in up to 60% of untreated people, typically starting about six months after infection. It usually affects only one or a few joints, often a knee or possibly the hip, other large joints, or the temporomandibular joint. Usually, large joint effusion and swelling occur, but only mild or moderate pain. Without treatment, swelling and pain typically resolve over time, but periodically return. Baker's cysts may form and rupture.
In early US studies of Lyme disease, a rare peripheral neuropathy was described that included numbness, tingling, or burning starting at the feet or hands and over time possibly moving up the limbs. In a later analysis that discovered poor documentation of this manifestation, experts wondered if it exists at all in the US or is merely very rare.
A neurologic syndrome called Lyme encephalopathy is associated with subtle memory and cognitive difficulties, insomnia, a general sense of feeling unwell, and changes in personality. Lyme encephalopathy is controversial in the US and has not been reported in Europe. Problems such as depression and fibromyalgia are as common in people with Lyme disease as in the general population. There is no compelling evidence that Lyme disease causes psychiatric disorders, behavioral disorders (e.g. ADHD), or developmental disorders (e.g. autism).
Acrodermatitis chronica atrophicans is a chronic skin disorder observed primarily in Europe among the elderly. It begins as a reddish-blue patch of discolored skin, often on the backs of the hands or feet. The lesion slowly atrophies over several weeks or months, with the skin becoming first thin and wrinkled and then, if untreated, completely dry and hairless. It is also associated with peripheral neuropathy.
Cause
Main article: Lyme disease microbiology Further information: Weather and climate effects on Lyme disease exposure
Lyme disease is caused by spirochetes, gram-negative bacteria from the genus Borrelia. Spirochetes are surrounded by peptidoglycan and flagella. The Lyme-related Borrelia species are collectively known as Borrelia burgdorferi sensu lato, and show a great deal of genetic diversity.
B. burgdorferi sensu lato is a species complex made up of 20 accepted and three proposed genospecies. Eight species are known to cause Lyme disease: B. mayonii (found in North America), B. burgdorferi sensu stricto (found in North America and Europe), B. afzelii, B. garinii, B. spielmanii, and B. lusitaniae (all found in Eurasia). Some studies have also proposed that B. valaisiana may sometimes infect humans, but this species does not seem to be an important cause of disease.
Tick life cycle
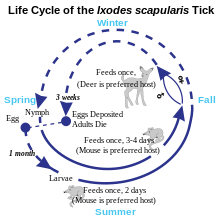

Three stages occur in the life cycle of a tick - larva, nymph, and adult. During the nymph stage, ticks most frequently transmit Lyme disease and are usually most active in late spring and early summer in regions where the climate is mild. During the adult stage, Lyme disease transmission is less common because adult ticks are less likely to bite humans and tend to be larger in size, so can be easily seen and removed.
Transmission
Lyme disease is classified as a zoonosis, as it is transmitted to humans from a natural reservoir among small mammals and birds by ticks that feed on both sets of hosts. Hard-bodied ticks of the genus Ixodes are the vectors of Lyme disease (also the vector for Babesia). Most infections are caused by ticks in the nymphal stage, because they are very small, thus may feed for long periods of time undetected. Nymphal ticks are generally the size of a poppy seed and sometimes with a dark head and a translucent body. Or, the nymphal ticks can be darker. The younger larval ticks are very rarely infected. Although deer are the preferred hosts of adult deer ticks, and tick populations are much lower in the absence of deer, ticks generally do not acquire Borrelia from deer, instead they obtain them from infected small mammals such as the white-footed mouse, and occasionally birds. Areas where Lyme is common are expanding.
Within the tick midgut, the Borrelia's outer surface protein A (OspA) binds to the tick receptor for OspA, known as TROSPA. When the tick feeds, the Borrelia downregulates OspA and upregulates OspC, another surface protein. After the bacteria migrate from the midgut to the salivary glands, OspC binds to Salp15, a tick salivary protein that appears to have immunosuppressive effects that enhance infection. Successful infection of the mammalian host depends on bacterial expression of OspC.
Tick bites often go unnoticed because of the small size of the tick in its nymphal stage, as well as tick secretions that prevent the host from feeling any itch or pain from the bite. However, transmission is quite rare, with only about 1.2 to 1.4 percent of recognized tick bites resulting in Lyme disease.
While B. burgdorferi is most associated with ticks hosted by white-tailed deer and white-footed mice, Borrelia afzelii is most frequently detected in rodent-feeding vector ticks, and Borrelia garinii and Borrelia valaisiana appear to be associated with birds. Both rodents and birds are competent reservoir hosts for B. burgdorferi sensu stricto. The resistance of a genospecies of Lyme disease spirochetes to the bacteriolytic activities of the alternative complement pathway of various host species may determine its reservoir host association.
Budding research has suggested that B. burgdorferi sensu lato may also be able to form enzootic cycle among lizard populations; this was previously assumed not to be possible in major areas containing populations of lizards, such as California. Except for one study in Europe, much of the data implicating lizards is based on DNA detection of the spirochete and has not demonstrated that lizards are able to infect ticks feeding upon them. As some experiments suggest lizards are refractory to infection with Borrelia, it appears likely their involvement in the enzootic cycle is more complex and species-specific.

In Europe, the main vector is Ixodes ricinus, which is also called the sheep tick or castor bean tick. In China, Ixodes persulcatus (the taiga tick) is probably the most important vector. In North America, the black-legged tick or deer tick (Ixodes scapularis) is the main vector on the East Coast.
The lone star tick (Amblyomma americanum), which is found throughout the Southeastern United States as far west as Texas, is unlikely to transmit the Lyme disease spirochetes, though it may be implicated in a related syndrome called southern tick-associated rash illness, which resembles a mild form of Lyme disease.
On the West Coast of the United States, the main vector is the western black-legged tick (Ixodes pacificus). The tendency of this tick species to feed predominantly on host species such as the Western Fence Lizard that are resistant to Borrelia infection appears to diminish transmission of Lyme disease in the West.
Transmission can occur across the placenta during pregnancy and as with a number of other spirochetal diseases, adverse pregnancy outcomes are possible with untreated infection; prompt treatment with antibiotics reduces or eliminates this risk.
There is no scientific evidence to support Lyme disease transmission via blood transfusion, sexual contact, or breast milk.
Tick-borne co-infections
Main article: Tick-borne diseaseTicks that transmit B. burgdorferi to humans can also carry and transmit several other microbes, such as Babesia microti and Anaplasma phagocytophilum, which cause the diseases babesiosis and human granulocytic anaplasmosis (HGA), respectively. Among people with early Lyme disease, depending on their location, 2–12% will also have HGA and 2–10% will have babesiosis. Ticks in certain regions also transmit viruses that cause tick-borne encephalitis and Powassan virus disease. Co-infections of Lyme disease may not require additional treatment, since they may resolve on their own or—as in the case of HGA—can be treated with the doxycycline prescribed for Lyme. Persistent fever or compatible anomalous laboratory findings may be indicative of a co-infection.
Pathophysiology
B. burgdorferi can spread throughout the body during the course of the disease, and has been found in the skin, heart, joints, peripheral nervous system, and central nervous system. B. Burgdorferi does not produce toxins. Therefore, many of the signs and symptoms of Lyme disease are a consequence of the immune response to spirochete in those tissues.
B. burgdorferi is injected into the skin by the bite of an infected Ixodes tick. Tick saliva, which accompanies the spirochete into the skin during the feeding process, contains substances that disrupt the immune response at the site of the bite. This provides a protective environment where the spirochete can establish infection. The spirochetes multiply and migrate outward within the dermis. The host inflammatory response to the bacteria in the skin causes the characteristic circular EM lesion. Neutrophils, however, which are necessary to eliminate the spirochetes from the skin, fail to appear in necessary numbers in the developing EM lesion because tick saliva inhibits neutrophil function. This allows the bacteria to survive and eventually spread throughout the body.
Days to weeks following the tick bite, the spirochetes spread via the bloodstream to joints, heart, nervous system, and distant skin sites, where their presence gives rise to the variety of symptoms of the disseminated disease. The spread of B. burgdorferi is aided by the attachment of the host protease plasmin to the surface of the spirochete.
If untreated, the bacteria may persist in the body for months or even years, despite the production of B. burgdorferi antibodies by the immune system. The spirochetes may avoid the immune response by decreasing expression of surface proteins that are targeted by antibodies, antigenic variation of the VlsE surface protein, inactivating key immune components such as complement, and hiding in the extracellular matrix, which may interfere with the function of immune factors.
Immunological studies
Exposure to the Borrelia bacterium during Lyme disease possibly causes a long-lived and damaging inflammatory response, a form of pathogen-induced autoimmune disease. The production of this reaction might be due to a form of molecular mimicry, where Borrelia avoids being killed by the immune system by resembling normal parts of the body's tissues.
Chronic symptoms from an autoimmune reaction could explain why some symptoms persist even after the spirochetes have been eliminated from the body. This hypothesis may explain why chronic arthritis persists after antibiotic therapy, similar to rheumatic fever, but its wider application is controversial.
Diagnosis
Lyme disease is diagnosed based on symptoms, objective physical findings (such as erythema migrans (EM) rash, facial palsy, or arthritis), history of possible exposure to infected ticks, and possibly laboratory tests. People with symptoms of early Lyme disease should have a total body skin examination for EM rashes and asked whether EM-type rashes had manifested within the last 1–2 months. Presence of an EM rash and recent tick exposure (i.e., being outdoors in a likely tick habitat where Lyme is common, within 30 days of the appearance of the rash) are sufficient for Lyme diagnosis; no laboratory confirmation is needed or recommended. Most people who get infected do not remember a tick or a bite, and the EM rash need not look like a bull's eye (most EM rashes in the U.S. do not) or be accompanied by any other symptoms. In the U.S., Lyme is most common in the New England and Mid-Atlantic states and parts of Wisconsin and Minnesota, but it is expanding into other areas. Several bordering areas of Canada also have high Lyme risk.
In the absence of an EM rash or history of tick exposure, Lyme diagnosis depends on laboratory confirmation. The bacteria that cause Lyme disease are difficult to observe directly in body tissues and also difficult and too time-consuming to grow in the laboratory. The most widely used tests look instead for presence of antibodies against those bacteria in the blood. A positive antibody test result does not by itself prove active infection but can confirm an infection that is suspected because of symptoms, objective findings, and history of tick exposure in a person. Because as many as 5–20% of the normal population have antibodies against Lyme, people without history and symptoms suggestive of Lyme disease should not be tested for Lyme antibodies: a positive result would likely be false, possibly causing unnecessary treatment.
In some cases, when history, signs, and symptoms are strongly suggestive of early disseminated Lyme disease, empiric treatment may be started and reevaluated as laboratory test results become available.
Laboratory testing
Tests for antibodies in the blood by ELISA and Western blot is the most widely used method for Lyme diagnosis. A two-tiered protocol is recommended by the Centers for Disease Control and Prevention (CDC): the sensitive ELISA test is performed first, and if it is positive or equivocal, then the more specific Western blot is run. The immune system takes some time to produce antibodies in quantity. After Lyme infection onset, antibodies of types IgM and IgG usually can first be detected respectively at 2–4 weeks and 4–6 weeks, and peak at 6–8 weeks. When an EM rash first appears, detectable antibodies may not be present. Therefore, it is recommended that testing not be performed and diagnosis be based on the presence of the EM rash. Up to 30 days after suspected Lyme infection onset, infection can be confirmed by detection of IgM or IgG antibodies; after that, it is recommended that only IgG antibodies be considered. A positive IgM and negative IgG test result after the first month of infection is generally indicative of a false-positive result. The number of IgM antibodies usually collapses 4–6 months after infection, while IgG antibodies can remain detectable for years.
Other tests may be used in neuroborreliosis cases. In Europe, neuroborreliosis is usually caused by Borrelia garinii and almost always involves lymphocytic pleocytosis, i.e. the densities of lymphocytes (infection-fighting cells) and protein in the cerebrospinal fluid (CSF) typically rise to characteristically abnormal levels, while glucose level remains normal. Additionally, the immune system produces antibodies against Lyme inside the intrathecal space, which contains the CSF. Demonstration by lumbar puncture and CSF analysis of pleocytosis and intrathecal antibody production are required for definite diagnosis of neuroborreliosis in Europe (except in cases of peripheral neuropathy associated with acrodermatitis chronica atrophicans, which usually is caused by Borrelia afzelii and confirmed by blood antibody tests). In North America, neuroborreliosis is caused by Borrelia burgdorferi and may not be accompanied by the same CSF signs; they confirm a diagnosis of central nervous system (CNS) neuroborreliosis if positive, but do not exclude it if negative. American guidelines consider CSF analysis optional when symptoms appear to be confined to the peripheral nervous system (PNS), e.g. facial palsy without overt meningitis symptoms. Unlike blood and intrathecal antibody tests, CSF pleocytosis tests revert to normal after infection ends and therefore can be used as objective markers of treatment success and inform decisions on whether to retreat. In infection involving the PNS, electromyography and nerve conduction studies can be used to monitor objectively the response to treatment.
In Lyme carditis, electrocardiograms are used to evidence heart conduction abnormalities, while echocardiography may show myocardial dysfunction. Biopsy and confirmation of Borrelia cells in myocardial tissue may be used in specific cases but are usually not done because of risk of the procedure.
Polymerase chain reaction (PCR) tests for Lyme disease have also been developed to detect the genetic material (DNA) of the Lyme disease spirochete. Culture or PCR are the current means for detecting the presence of the organism, as serologic studies only test for antibodies of Borrelia. PCR has the advantage of being much faster than culture. However, PCR tests are susceptible to false positive results, e.g. by detection of debris of dead Borrelia cells or specimen contamination. Even when properly performed, PCR often shows false-negative results because few Borrelia cells can be found in blood and cerebrospinal fluid (CSF) during infection. Hence, PCR tests are recommended only in special cases, e.g. diagnosis of Lyme arthritis, because it is a highly sensitive way of detecting ospA DNA in synovial fluid. Although sensitivity of PCR in CSF is low, its use may be considered when intrathecal antibody production test results are suspected of being falsely negative, e.g. in very early (< 6 weeks) neuroborreliosis or in immunosuppressed people.
Several other forms of laboratory testing for Lyme disease are available, some of which have not been adequately validated. OspA antigens, shed by live Borrelia bacteria into urine, are a promising technique being studied. The use of nanotrap particles for their detection is being looked at and the OspA has been linked to active symptoms of Lyme. High titers of either immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies to Borrelia antigens indicate disease, but lower titers can be misleading, because the IgM antibodies may remain after the initial infection, and IgG antibodies may remain for years.
The CDC does not recommend urine antigen tests, PCR tests on urine, immunofluorescent staining for cell-wall-deficient forms of B. burgdorferi, and lymphocyte transformation tests.
Imaging
Neuroimaging is controversial in whether it provides specific patterns unique to neuroborreliosis, but may aid in differential diagnosis and in understanding the pathophysiology of the disease. Though controversial, some evidence shows certain neuroimaging tests can provide data that are helpful in the diagnosis of a person. Magnetic resonance imaging (MRI) and single-photon emission computed tomography (SPECT) are two of the tests that can identify abnormalities in the brain of a person affected with this disease. Neuroimaging findings in an MRI include lesions in the periventricular white matter, as well as enlarged ventricles and cortical atrophy. The findings are considered somewhat unexceptional because the lesions have been found to be reversible following antibiotic treatment. Images produced using SPECT show numerous areas where an insufficient amount of blood is being delivered to the cortex and subcortical white matter. However, SPECT images are known to be nonspecific because they show a heterogeneous pattern in the imaging. The abnormalities seen in the SPECT images are very similar to those seen in people with cerebral vasculitis and Creutzfeldt–Jakob disease, which makes them questionable.
Differential diagnosis
Community clinics have been reported to misdiagnose 23–28% of Erythema migrans (EM) rashes and 83% of other objective manifestations of early Lyme disease. EM rashes are often misdiagnosed as spider bites, cellulitis, or shingles. Many misdiagnoses are credited to the widespread misconception that EM rashes should look like a bull's eye. Actually, the key distinguishing features of the EM rash are the speed and extent to which it expands, respectively up to 2–3 cm/day and a diameter of at least 5 cm, and in 50% of cases more than 16 cm. The rash expands away from its center, which may or may not look different or be separated by ring-like clearing from the rest of the rash. Compared to EM rashes, spider bites are more common in the limbs, tend to be more painful and itchy or become swollen, and some may cause necrosis (sinking dark blue patch of dead skin). Cellulitis most commonly develops around a wound or ulcer, is rarely circular, and is more likely to become swollen and tender. EM rashes often appear at sites that are unusual for cellulitis, such as the armpit, groin, abdomen, or back of knee. Like Lyme, shingles often begins with headache, fever, and fatigue, which are followed by pain or numbness. However, unlike Lyme, in shingles these symptoms are usually followed by appearance of rashes composed of multiple small blisters along with a nerve's dermatome, and shingles can also be confirmed by quick laboratory tests.
Facial palsy caused by Lyme disease (LDFP) is often misdiagnosed as Bell's palsy. Although Bell's palsy is the most common type of one-sided facial palsy (about 70% of cases), LDFP can account for about 25% of cases of facial palsy in areas where Lyme disease is common. Compared to LDFP, Bell's palsy much less frequently affects both sides of the face. Even though LDFP and Bell's palsy have similar symptoms and evolve similarly if untreated, corticosteroid treatment is beneficial for Bell's Palsy, while being detrimental for LDFP. Recent history of exposure to a likely tick habitat during warmer months, EM rash, viral-like symptoms such as headache and fever, and/or palsy in both sides of the face should be evaluated for the likelihood of LDFP; if it is more than minimal, empiric therapy with antibiotics should be initiated, without corticosteroids, and reevaluated upon completion of laboratory tests for Lyme disease.
Unlike viral meningitis, Lyme lymphocytic meningitis tends to not cause fever, last longer, and recur. Lymphocytic meningitis is also characterized by possibly co-occurring with EM rash, facial palsy, or partial vision obstruction and having much lower percentage of polymorphonuclear leukocytes in CSF.
Lyme radiculopathy affecting the limbs is often misdiagnosed as a radiculopathy caused by nerve root compression, such as sciatica. Although most cases of radiculopathy are compressive and resolve with conservative treatment (e.g., rest) within 4–6 weeks, guidelines for managing radiculopathy recommend first evaluating risks of other possible causes that, although less frequent, require immediate diagnosis and treatment, including infections such as Lyme and shingles. A history of outdoor activities in likely tick habitats in the last 3 months possibly followed by a rash or viral-like symptoms, and current headache, other symptoms of lymphocytic meningitis, or facial palsy would lead to suspicion of Lyme disease and recommendation of serological and lumbar puncture tests for confirmation.
Lyme radiculopathy affecting the trunk can be misdiagnosed as myriad other conditions, such as diverticulitis and acute coronary syndrome. Diagnosis of late-stage Lyme disease is often complicated by a multifaceted appearance and nonspecific symptoms, prompting one reviewer to call Lyme the new "great imitator". As all people with later-stage infection will have a positive antibody test, simple blood tests can exclude Lyme disease as a possible cause of a person's symptoms.
Prevention
Tick bites may be prevented by avoiding or reducing time in likely tick habitats and taking precautions while in and when getting out of one.
Most Lyme human infections are caused by Ixodes nymph bites between April and September. Ticks prefer moist, shaded locations in woodlands, shrubs, tall grasses and leaf litter or wood piles. Tick densities tend to be highest in woodlands, followed by unmaintained edges between woods and lawns (about half as high), ornamental plants and perennial groundcover (about a quarter), and lawns (about 30 times less). Ixodes larvae and nymphs tend to be abundant also where mice nest, such as stone walls and wood logs. Ixodes larvae and nymphs typically wait for potential hosts ("quest") on leaves or grasses close to the ground with forelegs outstretched; when a host brushes against its limbs, the tick rapidly clings and climbs on the host looking for a skin location to bite. In Northeastern United States, 69% of tick bites are estimated to happen in residences, 11% in schools or camps, 9% in parks or recreational areas, 4% at work, 3% while hunting, and 4% in other areas. Activities associated with tick bites around residences include yard work, brush clearing, gardening, playing in the yard, and letting dogs or cats that roam outside in woody or grassy areas into the house. In parks, tick bites often happen while hiking or camping. Walking on a mown lawn or center of a trail without touching adjacent vegetation is less risky than crawling or sitting on a log or stone wall. Pets should not be allowed to roam freely in likely tick habitats.
As a precaution, CDC recommends soaking or spraying clothes, shoes, and camping gear such as tents, backpacks and sleeping bags with 0.5% permethrin solution and hanging them to dry before use. Permethrin is odorless and safe for humans but highly toxic to ticks. After crawling on permethrin-treated fabric for as few as 10–20 seconds, tick nymphs become irritated and fall off or die. Permethrin-treated closed-toed shoes and socks reduce by 74 times the number of bites from nymphs that make first contact with a shoe of a person also wearing treated shorts (because nymphs usually quest near the ground, this is a typical contact scenario). Better protection can be achieved by tucking permethrin-treated trousers (pants) into treated socks and a treated long-sleeve shirt into the trousers so as to minimize gaps through which a tick might reach the wearer's skin. Light-colored clothing may make it easier to see ticks and remove them before they bite. Military and outdoor workers' uniforms treated with permethrin have been found to reduce the number of bite cases by 80–95%. Permethrin protection lasts several weeks of wear and washings in customer-treated items and up to 70 washings for factory-treated items. Permethrin should not be used on human skin, underwear or cats.
The EPA recommends several tick repellents for use on exposed skin, including DEET, picaridin, IR3535 (a derivative of amino acid beta-alanine), oil of lemon eucalyptus (OLE, a natural compound) and OLE's active ingredient para-menthane-diol (PMD). Unlike permethrin, repellents repel but do not kill ticks, protect for only several hours after application, and may be washed off by sweat or water. The most popular repellent is DEET in the U.S. and picaridin in Europe. Unlike DEET, picaridin is odorless and is less likely to irritate the skin or harm fabric or plastics. Repellents with higher concentration may last longer but are not more effective; against ticks, 20% picaridin may work for 8 hours vs. 55–98.11% DEET for 5–6 hours or 30–40% OLE for 6 hours. Repellents should not be used under clothes, on eyes, mouth, wounds or cuts, or on babies younger than 2 months (3 years for OLE or PMD). If sunscreen is used, repellent should be applied on top of it. Repellents should not be sprayed directly on a face, but should instead be sprayed on a hand and then rubbed on the face.
After coming indoors, clothes, gear and pets should be checked for ticks. Clothes can be put into a hot dryer for 10 minutes to kill ticks (just washing or warm dryer are not enough). Showering as soon as possible, looking for ticks over the entire body, and removing them reduce risk of infection. Unfed tick nymphs are the size of a poppy seed, but a day or two after biting and attaching themselves to a person, they look like a small blood blister. The following areas should be checked especially carefully: armpits, between legs, back of knee, bellybutton, trunk, and in children ears, neck and hair.
Tick removal

Attached ticks should be removed promptly. Risk of infection increases with time of attachment, but in North America risk of Lyme disease is small if the tick is removed within 36 hours. CDC recommends inserting a fine-tipped tweezer between the skin and the tick, grasping very firmly, and pulling the closed tweezer straight away from the skin without twisting, jerking, squeezing or crushing the tick. After tick removal, any tick parts remaining in the skin should be removed with a clean tweezer, if possible. The wound and hands should then be cleaned with alcohol or soap and water. The tick may be disposed by placing it in a container with alcohol, sealed bag, tape or flushed down the toilet. The bitten person should write down where and when the bite happened so that this can be informed to a doctor if the person gets a rash or flu-like symptoms in the following several weeks. CDC recommends not using fingers, nail polish, petroleum jelly or heat on the tick to try to remove it.
In Australia, where the Australian paralysis tick is prevalent, the Australasian Society of Clinical Immunology and Allergy recommends not using tweezers to remove ticks, because if the person is allergic, anaphylaxis could result. Instead, a product should be sprayed on the tick to cause it to freeze and then drop off. Another method consists in using about 20 cm of dental floss or fishing line for slowly tying an overhand knot between the skin and the tick and then pulling it away from the skin.
Preventive antibiotics
The risk of infectious transmission increases with the duration of tick attachment. It requires between 36 and 48 hours of attachment for the bacteria that causes Lyme to travel from within the tick into its saliva. If a deer tick that is sufficiently likely to be carrying Borrelia is found attached to a person and removed, and if the tick has been attached for 36 hours or is engorged, a single dose of doxycycline administered within the 72 hours after removal may reduce the risk of Lyme disease. It is not generally recommended for all people bitten, as development of infection is rare: about 50 bitten people would have to be treated this way to prevent one case of erythema migrans (i.e. the typical rash found in about 70–80% of people infected).
Garden landscaping
Several landscaping practices may reduce the risk of tick bites in residential yards. These include keeping lawns mown, removing leaf litter and weeds and avoiding the use of ground cover. A 3-ft-wide rock or woodchip barrier is recommended to separate lawns from wood piles, woodlands, stone walls and shrubs. Without vegetation on the barrier, ticks will tend not to cross it; acaricides may also be sprayed on it to kill ticks. A sun-exposed tick-safe zone at least 9 ft from the barrier should concentrate human activity on the yard, including any patios, playgrounds and gardening. Materials such as wood decking, concrete, bricks, gravel or woodchips used on the ground under patios and playgrounds would discourage ticks there. An 8-ft-high fence may be added to keep deer away from the tick-safe zone.
Occupational exposure
Outdoor workers are at risk of Lyme disease if they work at sites with infected ticks. This includes construction, landscaping, forestry, brush clearing, land surveying, farming, railroad work, oil field work, utility line work, park or wildlife management. U.S. workers in the northeastern and north-central states are at highest risk of exposure to infected ticks. Ticks may also transmit other tick-borne diseases to workers in these and other regions of the country. Worksites with woods, bushes, high grass or leaf litter are likely to have more ticks. Outdoor workers should be most careful to protect themselves in the late spring and summer when young ticks are most active.
Host animals
Ticks can feed upon the blood of a wide array of possible host species, including lizards, birds, mice, cats, dogs, deer, cattle and humans. The extent to which a tick can feed, reproduce, and spread will depend on the type and availability of its hosts. Whether it will spread disease is also affected by its available hosts. Some species, such as lizards, are referred to as "dilution hosts" because they don't tend to support Lyme disease pathogens and so decrease the likelihood that the disease will be passed on by ticks feeding on them. White-tailed deer are both a food source and a "reproductive host", where ticks tend to mate. The white-footed mouse is a reservoir host in which the pathogen for Lyme disease can survive. Availability of hosts can have significant impacts on the transmission of Lyme disease. A greater diversity of hosts, or of those that don't support the pathogen, tends to decrease the likelihood that the disease will be transmitted.
In the United States, one approach to reducing the incidence of Lyme and other deer tick-borne diseases has been to greatly reduce the deer population on which the adult ticks depend for feeding and reproduction. Lyme disease cases fell following deer eradication on an island, Monhegan, Maine, and following deer control in Mumford Cove, Connecticut. Advocates have suggested reducing the deer population to levels of 8 to 10 deer per square mile, compared to levels of 60 or more deer per square mile in the areas of the country with the highest Lyme disease rates. While these studies have found these effects, other studies have found opposite effects. A study done in Massachusetts removed deer and did not see a significant decrease in tick abundance afterwards. Another study done in New Jersey removed deer and also did not see a reduction in the number of questing ticks and determined that deer culling is an unlikely way to effectively control tick populations. One study summarized the results of multiple studies all looking at deer reduction controlling tick populations and determined that deer control can't be used as a standalone reduction for Lyme disease. It also claims that since most of the studies looking at this are not good representatives of areas with high human Lyme disease risk. There is varying information on whether or not the removal of deer is actually a way to control the Lyme disease epidemic. Removal of smaller mammals that are fed on by juveniles who are more actively acquiring and spreading the pathogen, would decrease Lyme disease risk the most.
Others have noted that while deer are reproductive hosts, they are not Borrelia burgdorferi reservoirs. This is because it was found that white-tailed deer blood actually kills the Borrelia burgdorferi bacteria. Researchers have suggested that smaller, less obviously visible Lyme reservoirs, like white-footed mice and Eastern chipmunks, may more strongly impact Lyme disease occurrence. Ecosystem studies in New York state suggest that white-footed mice thrive when forests are broken into smaller isolated chunks of woodland with fewer rodent predators. With more rodents harboring the disease, the odds increase that a tick will feed on a disease-harboring rodent and that someone will pick up a disease-carrying tick in their garden or walking in the woods. Data indicates that the smaller the wooded area, the more ticks it will contain and the likely they are to carry Lyme disease, supporting the idea that deforestation and habitat fragmentation affect ticks, hosts and disease transmission.
Tick-borne diseases are estimated to affect ~80 % of cattle worldwide. They also affect cats, dogs, and other pets. Routine veterinary control of ticks of domestic animals through the use of acaricides has been suggested as a way to reduce exposure of humans to ticks. However, chemical control with acaricides is now criticized on a number of grounds. Ticks appear to develop resistance to acaricides; acaricides are costly; and there are concerns over their toxicity and the potential for chemical residues to affect food and the environment.
In Europe, known reservoirs of Borrelia burgdorferi were 9 small mammals, 7 medium-sized mammals and 16 species of birds (including passerines, sea-birds and pheasants). These animals seem to transmit spirochetes to ticks and thus participate in the natural circulation of B. burgdorferi in Europe. The house mouse is also suspected as well as other species of small rodents, particularly in Eastern Europe and Russia. "The reservoir species that contain the most pathogens are the European roe deer Capreolus capreolus; "it does not appear to serve as a major reservoir of B. burgdorferi" thought Jaenson & al. (1992) (incompetent host for B. burgdorferi and TBE virus) but it is important for feeding the ticks, as red deer and wild boars (Sus scrofa), in which one Rickettsia and three Borrelia species were identified", with high risks of coinfection in roe deer. Nevertheless, in the 2000s, in roe deer in Europe "two species of Rickettsia and two species of Borrelia were identified".
Vaccination
As of 2023 no human vaccines for Lyme disease were available. The only human vaccine to advance to market was LYMErix, which was available from 1998, but discontinued in 2002. The vaccine candidate VLA15 was scheduled to start a phase 3 trial in the third quarter of 2022, with other research ongoing. Multiple vaccines are available for the prevention of Lyme disease in dogs.
LYMErix
The vaccine LYMErix was available from 1998 to 2002. The recombinant vaccine against Lyme disease, based on the outer surface protein A (OspA) of B. burgdorferi with aluminum hydroxide as adjuvant, was developed by SmithKline Beecham. In clinical trials involving more than 10,000 people, the vaccine was found to confer protective immunity to Lyme disease in 76% of adults after three doses with only mild or moderate and transient adverse effects. On 21 December 1998, the Food and Drug Administration (FDA) approved LYMErix on the basis of these trials for persons of ages 15 through 70.
Following approval of the vaccine, its entry into clinical practice was slow for a variety of reasons, including its cost, which was often not reimbursed by insurance companies. Subsequently, hundreds of vaccine recipients reported they had developed autoimmune and other side effects. Supported by some advocacy groups, a number of class-action lawsuits were filed against GlaxoSmithKline, alleging the vaccine had caused these health problems. These claims were investigated by the FDA and the Centers for Disease Control, which found no connection between the vaccine and the autoimmune complaints.
Despite the lack of evidence that the complaints were caused by the vaccine, sales plummeted and LYMErix was withdrawn from the U.S. market by GlaxoSmithKline in February 2002, in the setting of negative media coverage and fears of vaccine side effects. The fate of LYMErix was described in the medical literature as a "cautionary tale"; an editorial in Nature cited the withdrawal of LYMErix as an instance in which "unfounded public fears place pressures on vaccine developers that go beyond reasonable safety considerations." The original developer of the OspA vaccine at the Max Planck Institute told Nature: "This just shows how irrational the world can be ... There was no scientific justification for the first OspA vaccine LYMErix being pulled."
VLA15
The hexavalent (OspA) protein subunit-based vaccine candidate VLA15 was developed by Valneva. It was granted fast track designation by the U.S. Food and Drug Administration in July 2017. In April 2020 Pfizer paid $130 million for the rights to the vaccine, and the companies are developing it together, performing multiple phase 2 trials.
A phase 3 trial of VLA15 was scheduled for late 2022, recruiting volunteers at test sites located across the northeastern United States and in Europe. Participants were scheduled to receive an initial three-dose series of vaccines over the course of five to nine months, followed by a booster dose after twelve months, with both the initial series and the booster dose scheduled to be complete before the year's peak Lyme disease season.
Other research
An mRNA vaccine designed to cause a strong fast immune response to tick saliva allowed the immune system to detect and remove the ticks from test animals before they were able to transmit the infectious bacteria. The vaccine contains mRNAs for the body to build 19 proteins in tick saliva which, by enabling quick development of erythema (itchy redness) at the bite site, protects guinea pigs against Lyme disease. It also protected the test animals if the tick is not removed if only one tick, but not three, remain attached.
Canine vaccines
Canine vaccines have been formulated and approved for the prevention of Lyme disease in dogs. Currently, three Lyme disease vaccines are available. LymeVax, formulated by Fort Dodge Laboratories, contains intact dead spirochetes which expose the host to the organism. Galaxy Lyme, Intervet-Schering-Plough's vaccine, targets proteins OspC and OspA. The OspC antibodies kill any of the bacteria that have not been killed by the OspA antibodies. Canine Recombinant Lyme, formulated by Merial, generates antibodies against the OspA protein so a tick feeding on a vaccinated dog draws in blood full of anti-OspA antibodies, which kill the spirochetes in the tick's gut before they are transmitted to the dog.
Treatment
Antibiotics are the primary treatment. The specific approach to their use is dependent on the individual affected and the stage of the disease. For most people with early localized infection, oral administration of doxycycline is widely recommended as the first choice, as it is effective against not only Borrelia bacteria but also a variety of other illnesses carried by ticks. People taking doxycycline should avoid sun exposure because of higher risk of sunburns. Doxycycline is contraindicated in children younger than eight years of age and women who are pregnant or breastfeeding; alternatives to doxycycline are amoxicillin, cefuroxime axetil, and azithromycin. Azithromycin is recommended only in case of intolerance to the other antibiotics. The standard treatment for cellulitis, cephalexin, is not useful for Lyme disease. When it is unclear if a rash is caused by Lyme or cellulitis, the IDSA recommends treatment with cefuroxime or amoxicillin/clavulanic acid, as these are effective against both infections. Individuals with early disseminated or late Lyme infection may have symptomatic cardiac disease, Lyme arthritis, or neurologic symptoms like facial palsy, radiculopathy, meningitis, or peripheral neuropathy. Intravenous administration of ceftriaxone is recommended as the first choice in these cases; cefotaxime and doxycycline are available as alternatives.
Treatment regimens for Lyme disease range from 7–14 days in early localized disease, to 14–21 days in early disseminated disease to 14–28 days in late disseminated disease. Neurologic complications of Lyme disease may be treated with doxycycline as it can be taken by mouth and has a lower cost, although in North America evidence of efficacy is only indirect. In case of failure, guidelines recommend retreatment with injectable ceftriaxone. Several months after treatment for Lyme arthritis, if joint swelling persists or returns, a second round of antibiotics may be considered; intravenous antibiotics are preferred for retreatment in case of poor response to oral antibiotics. Outside of that, a prolonged antibiotic regimen lasting more than 28 days is not recommended as no evidence shows it to be effective. IgM and IgG antibody levels may be elevated for years even after successful treatment with antibiotics. As antibody levels are not indicative of treatment success, testing for them is not recommended.
Facial palsy may resolve without treatment: however, antibiotic treatment is recommended to stop other Lyme complications. Corticosteroids are not recommended when facial palsy is caused by Lyme disease. In those with facial palsy, frequent use of artificial tears while awake is recommended, along with ointment and a patch or taping the eye closed when sleeping.
About a third of people with Lyme carditis need a temporary pacemaker until their heart conduction abnormality resolves, and 21% need to be hospitalized. Lyme carditis should not be treated with corticosteroids.
People with Lyme arthritis should limit their level of physical activity to avoid damaging affected joints, and in case of limping should use crutches. Pain associated with Lyme disease may be treated with nonsteroidal anti-inflammatory drugs (NSAIDs). Corticosteroid joint injections are not recommended for Lyme arthritis that is being treated with antibiotics. People with Lyme arthritis treated with intravenous antibiotics or two months of oral antibiotics who continue to have joint swelling two months after treatment and have negative PCR test for Borrelia DNA in the synovial fluid are said to have post-antibiotic Lyme arthritis; this is more common after infection by certain Borrelia strains in people with certain genetic and immunologic characteristics. Post-antibiotic Lyme arthritis may be symptomatically treated with NSAIDs, disease-modifying antirheumatic drugs (DMARDs), arthroscopic synovectomy, or physical therapy.
People receiving treatment should be advised that reinfection is possible and how to prevent it.
Prognosis
Lyme disease's typical first sign, the erythema migrans (EM) rash, resolves within several weeks even without treatment. However, in untreated people, the infection often disseminates to the nervous system, heart or joints, possibly causing permanent damage to body tissues.
People who receive recommended antibiotic treatment within several days of appearance of an initial EM rash have the best prospects. Recovery may not be total or immediate. The percentage of people achieving full recovery in the United States increases from about 64–71% at end of treatment for EM rash to about 84–90% after 30 months; higher percentages are reported in Europe. Treatment failure, i.e. persistence of original or appearance of new signs of the disease, occurs only in a few people. Remaining people are considered cured but continue to experience subjective symptoms, e.g. joint or muscle pains or fatigue. These symptoms are usually mild and nondisabling.
People treated only after nervous system manifestations of the disease may end up with objective neurological deficits, in addition to subjective symptoms. In Europe, an average of 32–33 months after initial Lyme symptoms in people treated mostly with doxycycline 200 mg for 14–21 days, the percentage of people with lingering symptoms was much higher among those diagnosed with neuroborreliosis (50%) than among those with only an EM rash (16%). In another European study, 5 years after treatment for neuroborreliosis lingering symptoms were less common among children (15%) than adults (30%), and in the latter were less common among those treated within 30 days of the first symptom (16%) than among those treated later (39%); among those with lingering symptoms, 54% had daily activities restricted and 19% were on sick leave or incapacitated.
Some data suggest that about 90% of Lyme facial palsies treated with antibiotics recover fully a median of 24 days after appearing and most of the rest recover with only mild abnormality. However, in Europe 41% of people treated for facial palsy had other lingering symptoms at followup up to 6 months later, including 28% with numbness or altered sensation and 14% with fatigue or concentration problems. Palsies in both sides of the face are associated with worse and longer time to recovery. Historical data suggests that untreated people with facial palsies recover at nearly the same rate, but 88% subsequently have Lyme arthritis. Other research shows that synkinesis (involuntary movement of a facial muscle when another one is voluntarily moved) can become evident only 6–12 months after facial palsy appears to be resolved, as damaged nerves regrow and sometimes connect to incorrect muscles. Synkinesis is associated with corticosteroid use. In longer-term follow-up, 16–23% of Lyme facial palsies do not fully recover.
In Europe, about a quarter of people with Bannwarth syndrome (Lyme radiculopathy and lymphocytic meningitis) treated with intravenous ceftriaxone for 14 days an average of 30 days after first symptoms had to be retreated 3–6 months later because of unsatisfactory clinical response or continued objective markers of infection in cerebrospinal fluid; after 12 months, 64% recovered fully, 31% had nondisabling mild or infrequent symptoms that did not require regular use of analgesics, and 5% had symptoms that were disabling or required substantial use of analgesics. The most common lingering nondisabling symptoms were headache, fatigue, altered sensation, joint pains, memory disturbances, malaise, radicular pain, sleep disturbances, muscle pains, and concentration disturbances. Lingering disabling symptoms included facial palsy and other impaired movement.
Recovery from late neuroborreliosis tends to take longer and be less complete than from early neuroborreliosis, probably because of irreversible neurologic damage.
About half the people with Lyme carditis progress to complete heart block, but it usually resolves in a week. Other Lyme heart conduction abnormalities resolve typically within 6 weeks. About 94% of people have full recovery, but 5% need a permanent pacemaker and 1% end up with persistent heart block (the actual percentage may be higher because of unrecognized cases). Lyme myocardial complications usually are mild and self-limiting. However, in some cases Lyme carditis can be fatal.
Recommended antibiotic treatments are effective in about 90% of Lyme arthritis cases, although it can take several months for inflammation to resolve and a second round of antibiotics is often necessary. Antibiotic-refractory Lyme arthritis also eventually resolves, typically within 9–14 months (range 4 months – 4 years); DMARDs or synovectomy can accelerate recovery.
Reinfection is not uncommon. In a U.S. study, 6–11% of people treated for an EM rash had another EM rash within 30 months. The second rash typically is due to infection by a different Borrelia strain.
Post-treatment Lyme disease syndrome
Chronic symptoms like pain, fatigue, or cognitive impairment are experienced by 5–20% of people who contract Lyme disease, even after completing treatment. This is called Post-treatment Lyme disease syndrome, or PTLDS.
The cause is unknown. One hypothesis is that a persistent, difficult-to-detect infection remains. However, human and animal trials have not provided compelling evidence to support this hypothesis. Another hypothesis is that autoimmunity has been triggered by the infection. Auto–immune responses are known to occur following other infections, including Campylobacter (Guillain-Barré syndrome), Chlamydia (reactive arthritis), and strep throat (rheumatic heart disease). A third hypothesis is that debris from a previous infection could remain.
Another hypothesis is that symptoms are simply unrelated to a Lyme infection. Among 13 studies analyzing people who worried about Lyme disease, 47 to 80% had no evidence of Lyme infection while 15 to 55% (median 34%) were able to obtain other diagnoses.
There is no proven treatment for Post-treatment Lyme disease syndrome. While short-term antibiotics are effective in early Lyme disease, prolonged antibiotics are not. They have been shown ineffective in placebo-controlled trials and carry the risk of serious, sometimes deadly complications. Generally, treatment is symptomatic and is similar to the management of fibromyalgia or ME/CFS. PTLDS usually gets better over time, but recovery may take many months.
Epidemiology

Lyme disease occurs regularly in Northern Hemisphere temperate regions. An estimated 476,000 people a year are diagnosed and treated for the disease in the United States. This number is probably an overestimate due to overdiagnosis and overtreatment. Over 200,000 people a year are diagnosed and treated in Europe. There is a suggestion that tick populations and Lyme disease occurrence are increasing and spreading into new areas, owing in part to the warming temperatures of climate change. However, tick-borne disease systems are complex, and determining whether changes are due to climate change or other drivers can be difficult. Lyme disease effects are comparable among males and females. A wide range of age groups is affected, though the number of cases is highest among 10- to 19-year-olds.
Africa
In northern Africa, B. burgdorferi sensu lato has been identified in Morocco, Algeria, Egypt and Tunisia.
Lyme disease in sub-Saharan Africa is presently unknown, but evidence indicates it may occur in humans in this region. The abundance of hosts and tick vectors would favor the establishment of Lyme infection in Africa. In East Africa, two cases of Lyme disease have been reported in Kenya. According The Federation of Infectious Diseases Societies of Southern Africa, Lyme disease is not known to be endemic in either South Africa or Mozambique.
Asia
B. burgdorferi sensu lato-infested ticks are being found more frequently in Japan, as well as in northwest China, Nepal, Thailand and far eastern Russia. Borrelia has also been isolated in Mongolia.
Australia
Lyme disease is not considered endemic to Australia. While there have been reports of people acquiring Lyme disease in Australia, and even evidence of closely related Borrelia species in ticks, the evidence linking these cases to local transmission is limited. Ongoing research on resolving potential Borrelia species to Debilitating Symptom Complexes Attributed to Ticks (DSCATT) in Australia are ongoing.
Europe
In Europe, Lyme disease is caused by infection with one or more pathogenic European genospecies of the spirochaete B. burgdorferi sensu lato, mainly transmitted by the tick Ixodes ricinus. Cases of B. burgdorferi sensu lato-infected ticks are found predominantly in central Europe, particularly in Slovenia and Austria, but have been isolated in almost every country on the continent. The number of cases in southern Europe, such as Italy and Portugal, is much lower. Diagnosed cases in some Western countries, such as Iceland, are rising. Lyme disease is rare in Iceland. On average around 6 to 7 cases are diagnosed every year, primarily localised infections presenting as erythema migrans. None of the cases had a definitive Icelandic origin and the yearly number of cases has not been increasing.
United Kingdom
In the United Kingdom the number of laboratory-confirmed cases of Lyme disease has been rising steadily since voluntary reporting was introduced in 1986 when 68 cases were recorded in the UK and Ireland combined. In the UK there were 23 confirmed cases in 1988 and 19 in 1990, but 973 in 2009 and 953 in 2010. Provisional figures for the first 3 quarters of 2011 show a 26% increase on the same period in 2010.
It is thought, however, that the actual number of cases is significantly higher than suggested by the above figures, with England's Health Protection Agency estimating that there are between 2,000 and 3,000 cases in England and Wales per year (with an average of around 15% of the infections acquired overseas), while Dr Darrel Ho-Yen, Director of the Scottish Toxoplasma Reference Laboratory and National Lyme Disease Testing Service, believes that the number of confirmed cases should be multiplied by 10 "to take account of wrongly diagnosed cases, tests giving false results, sufferers who weren't tested, people who are infected but not showing symptoms, failures to notify and infected individuals who don't consult a doctor."
Despite Lyme disease (Borrelia burgdorferi infection) being a notifiable disease in Scotland since January 1990 which should therefore be reported on the basis of clinical suspicion, it is believed that many GPs are unaware of the requirement. Mandatory reporting, limited to laboratory test results only, was introduced throughout the UK in October 2010, under the Health Protection (Notification) Regulations 2010.
Although there is a greater number of cases of Lyme disease in the New Forest, Salisbury Plain, Exmoor, the South Downs, parts of Wiltshire and Berkshire, Thetford Forest and the West coast and islands of Scotland, infected ticks are widespread and can even be found in the parks of London. A 1989 report found that 25% of forestry workers in the New Forest were seropositive, as were between 2% and 4–5% of the general local population of the area.
Tests on pet dogs carried out throughout the country in 2009 indicated that around 2.5% of ticks in the UK may be infected, considerably higher than previously thought. It is speculated that global warming may lead to an increase in tick activity in the future, as well as an increase in the amount of time that people spend in public parks, thus increasing the risk of infection. However no published research has proven this to be so.
North America
Many studies in North America have examined ecological and environmental correlates of the number of people affected by Lyme disease. A 2005 study using climate suitability modelling of I. scapularis projected that climate change would cause an overall 213% increase in suitable vector habitat by 2080, with northward expansions in Canada, increased suitability in the central U.S., and decreased suitable habitat and vector retraction in the southern U.S. A 2008 review of published studies concluded that the presence of forests or forested areas was the only variable that consistently elevated the risk of Lyme disease whereas other environmental variables showed little or no concordance between studies. The authors argued that the factors influencing tick density and human risk between sites are still poorly understood, and that future studies should be conducted over longer time periods, become more standardized across regions, and incorporate existing knowledge of regional Lyme disease ecology.
Canada
The range of ticks able to carry Lyme disease has expanded from a limited area of Ontario to include areas of southern Quebec, Manitoba, northern Ontario, southern New Brunswick, southwest Nova Scotia and limited parts of Saskatchewan and Alberta, as well as British Columbia. Cases have been reported as far east as the island of Newfoundland. A model-based prediction by Leighton et al. (2012) suggests that the range of the I. scapularis tick will expand into Canada by 46 km/year over the next decade, with warming climatic temperatures as the main driver of increased speed of spread.
Mexico
A 2007 study suggests Borrelia burgdorferi infections are endemic to Mexico, from four cases reported between 1999 and 2000.
United States
Lyme disease is the most common tick-borne disease in North America and Europe, and one of the fastest-growing infectious diseases in the United States. Of cases reported to the United States CDC, the ratio of Lyme disease infection is 7.9 cases for every 100,000 persons. In the ten states where Lyme disease is most common, the average was 31.6 cases for every 100,000 persons for the year 2005.
Although Lyme disease has been reported in all states due to travel-associated infections, about 99% of all reported cases are confined to just five geographic areas (New England, Mid-Atlantic, East-North Central, South Atlantic, and West North-Central). CDC implemented national surveillance of Lyme disease cases in 1991. Since then, reporting criteria has been modified multiple times. The 2022 surveillance case definition classifies cases as confirmed, probable, and suspect. The number of reported cases of the disease has been increasing, as are endemic regions in North America.
The CDC emphasizes that, while surveillance data has limitations, it is useful due to "uniformity, simplicity, and timeliness." While cases are under-reported in high-incidence areas, over-reporting is likely in low-incidence areas. Additionally, surveillance cases are reported by county of residence and not where an infection was necessarily contracted.
Several similar but apparently distinct conditions may exist, caused by various species or subspecies of Borrelia in North America. A regionally restricted condition that may be related to Borrelia infection is southern tick-associated rash illness (STARI), also known as Masters disease. Amblyomma americanum, known commonly as the lone-star tick, is recognized as the primary vector for STARI. In some parts of the geographical distribution of STARI, Lyme disease is quite rare (e.g., Arkansas), so people in these regions experiencing Lyme-like symptoms—especially if they follow a bite from a lone-star tick—should consider STARI as a possibility. It is generally a milder condition than Lyme and typically responds well to antibiotic treatment.
In recent years there have been 5 to 10 cases a year of a disease similar to Lyme occurring in Montana. It occurs primarily in pockets along the Yellowstone River in central Montana. People have developed a red bull's-eye rash around a tick bite followed by weeks of fatigue and a fever.
South America
In Brazil, Lyme disease is not considered endemic. A Lyme-like disease known as Baggio–Yoshinari syndrome has been described, attributed to microorganisms that do not belong to the B. burgdorferi sensu lato complex and transmitted by ticks of the Amblyomma and Rhipicephalus genera. The first reported case of BYS in Brazil was made in 1992 in Cotia, São Paulo. A 2024 analysis concluded that evidence to connect BYS to Borrelia bacteria was lacking.
Etymology
Lyme disease was diagnosed as a separate condition for the first time in 1975 in Lyme, Connecticut.
History
The earliest known evidence of Lyme disease was found in Oetzi, a 5300 year old mummy in the Eastern Alps near the Italian border. The evolutionary history of Borrelia burgdorferi genetics has been examined by scientists. One study has found that prior to the reforestation that accompanied post-colonial farm abandonment in New England and the wholesale migration into the mid-west that occurred during the early 19th century, Lyme disease had been present for thousands of years in America and had spread along with its tick hosts from the Northeast to the Midwest.
John Josselyn, who visited New England in 1638 and again from 1663 to 1670, wrote "there be infinite numbers of ticks hanging upon the bushes in summertime that will cleave to man's garments and creep into his breeches, eating themselves in a short time into the very flesh of a man. I have seen the stockings of those that have gone through the woods covered with them."
This is also confirmed by the writings of Peter Kalm, a Swedish botanist who was sent to America by Linnaeus, and who found the forests of New York "abound" with ticks when he visited in 1749. When Kalm's journey was retraced 100 years later, the forests were gone and the Lyme bacterium had probably become isolated to a few pockets along the northeast coast, Wisconsin, and Minnesota.
Perhaps the first detailed description of what is now known as Lyme disease appeared in the writings of John Walker after a visit to the island of Jura (Deer Island) off the west coast of Scotland in 1764. He gives a good description both of the symptoms of Lyme disease (with "exquisite pain the interior parts of the limbs") and of the tick vector itself, which he describes as a "worm" with a body which is "of a reddish color and of a compressed shape with a row of feet on each side" that "penetrates the skin". Many people from this area of Great Britain emigrated to North America between 1717 and the end of the 18th century.
The examination of preserved museum specimens has found Borrelia DNA in an infected Ixodes ricinus tick from Germany that dates back to 1884, and from an infected mouse from Cape Cod that died in 1894. The 2010 autopsy of Ötzi the Iceman, a 5,300-year-old mummy, revealed the presence of the DNA sequence of Borrelia burgdorferi making him the earliest known human with Lyme disease.
The early European studies of what is now known as Lyme disease described its skin manifestations. The first study dates to 1883 in Breslau, Germany (now Wrocław, Poland), where physician Alfred Buchwald described a man who for 16 years had had a degenerative skin disorder now known as acrodermatitis chronica atrophicans.
At a 1909 research conference, Swedish dermatologist Arvid Afzelius presented a study about an expanding, ring-like lesion he had observed in an older woman following the bite of a sheep tick. He named the lesion erythema migrans. The skin condition now known as borrelial lymphocytoma was first described in 1911.
The modern history of medical understanding of the disease, including its cause, diagnosis, and treatment, has been difficult.
Neurological problems following tick bites were recognized starting in the 1920s. French physicians Garin and Bujadoux described a farmer with a painful sensory radiculitis accompanied by mild meningitis following a tick bite. A large, ring-shaped rash was also noted, although the doctors did not relate it to the meningoradiculitis. In 1930, the Swedish dermatologist Sven Hellerström was the first to propose EM and neurological symptoms following a tick bite were related. In the 1940s, German neurologist Alfred Bannwarth described several cases of chronic lymphocytic meningitis and polyradiculoneuritis, some of which were accompanied by erythematous skin lesions.
Carl Lennhoff, who worked at the Karolinska Institute in Sweden, believed many skin conditions were caused by spirochetes. In 1948, he published on his use of a special stain to microscopically observe what he believed were spirochetes in various types of skin lesions, including EM. Although his conclusions were later shown to be erroneous, interest in the study of spirochetes was sparked. Starting in 1946, facilities in Sweden experimented with treating EM rashes with substances known to kill spirochetes. Einar Hollström [sv] reported that "penicillin was found to be the most effective." In 1949, Nils Thyresson, who also worked at the Karolinska Institute, was the first to treat ACA with penicillin. In the 1950s, the relationship among tick bite, lymphocytoma, EM and Bannwarth's syndrome was recognized throughout Europe leading to the widespread use of penicillin for treatment in Europe.
In 1970 a dermatologist in Wisconsin named Rudolph Scrimenti recognized an EM lesion in a person after recalling a paper by Hellerström that had been reprinted in an American science journal in 1950. This was the first documented case of EM in the United States. Based on the European literature, he treated the person with penicillin.
The full syndrome now known as Lyme disease was not recognized until a cluster of cases originally thought to be juvenile rheumatoid arthritis was identified in three towns in southeastern Connecticut in 1975, including the towns Lyme and Old Lyme, which gave the disease its popular name. This was investigated by physicians David Snydman and Allen Steere of the Epidemic Intelligence Service, and by others from Yale University, including Stephen Malawista, who is credited as a co-discover of the disease. The recognition that the people in the United States had EM led to the recognition that "Lyme arthritis" was one manifestation of the same tick-borne condition known in Europe.
Before 1976, the elements of B. burgdorferi sensu lato infection were called or known as tick-borne meningopolyneuritis, Garin-Bujadoux syndrome, Bannwarth syndrome, Afzelius's disease, Montauk Knee or sheep tick fever. Since 1976 the disease is most often referred to as Lyme disease, Lyme borreliosis or simply borreliosis.
In 1980, Steere, et al., began to test antibiotic regimens in adults with Lyme disease. In the same year, New York State Health Dept. epidemiologist Jorge Benach provided Willy Burgdorfer, a researcher at the Rocky Mountain Biological Laboratory, with collections of I. dammini from Shelter Island, New York, a known Lyme-endemic area as part of an ongoing investigation of Rocky Mountain spotted fever. In examining the ticks for rickettsiae, Burgdorfer noticed "poorly stained, rather long, irregularly coiled spirochetes." Further examination revealed spirochetes in 60% of the ticks. Burgdorfer credited his familiarity with the European literature for his realization that the spirochetes might be the "long-sought cause of ECM and Lyme disease." Benach supplied him with more ticks from Shelter Island and sera from people diagnosed with Lyme disease. University of Texas Health Science Center researcher Alan Barbour "offered his expertise to culture and immunochemically characterize the organism." Burgdorfer subsequently confirmed his discovery by isolating, from people with Lyme disease, spirochetes identical to those found in ticks. In June 1982, he published his findings in Science, and the spirochete was named Borrelia burgdorferi in his honor.
After the identification of B. burgdorferi as the causative agent of Lyme disease, antibiotics were selected for testing, guided by in vitro antibiotic sensitivities, including tetracycline antibiotics, amoxicillin, cefuroxime axetil, intravenous and intramuscular penicillin and intravenous ceftriaxone. The mechanism of tick transmission was also the subject of much discussion. B. burgdorferi spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.
Society, culture, and controversy
Landscape changes and urbanization
Urbanization and other anthropogenic factors can be implicated in the spread of Lyme disease to humans. In many areas, expansion of suburban neighborhoods has led to gradual deforestation of surrounding wooded areas and increased border contact between humans and tick-dense areas. Human expansion has also resulted in a reduction of predators that hunt deer as well as mice, chipmunks and other small rodents—the primary reservoirs for Lyme disease. As a consequence of increased human contact with host and vector, the likelihood of transmission of the disease has greatly increased. Researchers are investigating possible links between global warming and the spread of vector-borne diseases, including Lyme disease.
The dilution effect
Given these habitat-host dynamics, in 2003 some researchers began to postulate whether the so called dilution effect could mitigate the spread of Lyme disease. The dilution effect is a hypothesis that predicts that an increase in host biodiversity will result in a decrease in the number of vectors infected with B. burgdorferi. Scientific research has shown that nymphal infection prevalence (NIP) decreases as the number of host species increases, supporting the dilution effect. That said, there is no direct relationship between decreased NIP and decreased epidemiological risk, as this has yet to be proven. Additionally, as of 2018, the dilution effect is only supported in the Northeastern United States, and has been disproved in other parts of the world that also experience high Lyme disease incidence rates
Chronic Lyme disease
Main article: Chronic Lyme diseaseThe term "chronic Lyme disease" is controversial and not recognized in the medical literature, and most medical authorities advise against long-term antibiotic treatment for Lyme disease. Studies have shown that most people diagnosed with "chronic Lyme disease" either have no objective evidence of previous or current infection with B. burgdorferi or are people who should be classified as having post-treatment Lyme disease syndrome (PTLDS), which is defined as continuing or relapsing non-specific symptoms (such as fatigue, musculoskeletal pain, and cognitive complaints) in a person previously treated for Lyme disease.
The 2008 documentary Under Our Skin is known for promoting controversial and unrecognized theories about "chronic Lyme disease".
Other animals
Dogs
Prevention of Lyme disease is an important step in keeping dogs safe in endemic areas. Prevention education and a number of preventive measures are available. First, for dog owners who live near or who often frequent tick-infested areas, routine vaccinations of their dogs is an important step.
Another crucial preventive measure is the use of persistent acaricides, such as topical repellents or pesticides that contain triazapentadienes (Amitraz), phenylpyrazoles (Fipronil), or permethrin (pyrethroids). These acaricides target primarily the adult stages of Lyme-carrying ticks and reduce the number of reproductively active ticks in the environment. Formulations of these ingredients are available in a variety of topical forms, including spot-ons, sprays, powders, impregnated collars, solutions, and shampoos.
Examination of a dog for ticks after being in a tick-infested area is an important precautionary measure to take in the prevention of Lyme disease. Key spots to examine include the head, neck, and ears.
In dogs, a serious long-term prognosis may result in glomerular disease, which is a category of kidney damage that may cause chronic kidney disease. Dogs may also experience chronic joint disease if the disease is left untreated. However, the majority of cases of Lyme disease in dogs result in complete recovery with, and sometimes without, treatment with antibiotics. In rare cases, Lyme disease can be fatal to both humans and dogs.
Cats
Unlike dogs, it is very rare for a cat to be infected with Lyme disease. However, cats are nevertheless capable of being infected with B. burgdorferi , following a bite from an infected tick. Cats who are infected with Lyme Disease may show symptoms including but not limited to lameness, fatigue, or loss of appetite. In two cases, the infected cats experienced cardiac irregularities similar to symptoms of Lyme in both dogs and humans. However, cats who are infected with Lyme disease are likely to be asymptomatic, and show no noticeable signs of the disease. Cats with Lyme are often treated with antibiotics, much like other animals. In some cases, additional treatment or therapy may be required.
Horses
Lyme disease in horses is often challenging to diagnose because symptoms vary widely. Common acute symptoms include weight loss, fever, lameness, ataxia, and other muscle and joint-related issues. Additional symptoms include muscle tenderness, swollen joints, arthritis, and neck stiffness. Chronic symptoms of the disease typically include neurological manifestations, such as meningitis, cranial neuritis, radiculoneuritis, and encephalitis. Furthermore, it is important to note that some horses do not slow clinical signs of Lyme disease.
There are three main testing strategies used to diagnose horses with Lyme disease. They include clinical evaluation, serological testing, and polymerase chain reaction (PCR) testing. Detection of specific antibodies against B. burgdorferi alone is not sufficient for a diagnosis of equine Lyme disease and unspecific testing for antibodies is not recommended.
Typical treatment involves antibiotics such as oxytetracycline, doxycycline, ceftriaxone, or minocycline. In some cases, a combination of antibiotics may be administered. Doxycycline and minocycline are taken orally, while oxytetracycline and ceftriaxone are usually administered intravenously. The duration and dosage of treatment vary widely among cases. In most cases, the infected horse is euthanized. Death of horses as a result of Borrelia burgdorferi infection remains unknown.
Currently, there is no approved Lyme disease vaccine for horses available. However, a study demonstrated that ponies could be protected using an aluminum adjuvanted recombinant outer-surface protein A (rOspA) vaccine. While horses have been administered a Lyme disease vaccine designed for dogs, it elicits only a short-lasting antibody response. Another study supports the use of commercial Lyme disease vaccines, showing that they do elicit an antibody response, which can be significantly enhanced when horses receive an additional booster vaccine.
References
- ^ "Signs and Symptoms of Lyme Disease". cdc.gov. 11 January 2013. Archived from the original on 16 January 2013. Retrieved 2 March 2015.
- "Clinical Care and Treatment of Neurologic Lyme Disease". Lyme Disease. 20 May 2024. Retrieved 27 May 2024.
- "Lyme disease - Symptoms and causes". Mayo Clinic. Retrieved 7 June 2022.
- ^ Shapiro ED (May 2014). "Clinical practice. Lyme disease" (PDF). The New England Journal of Medicine. 370 (18): 1724–1731. doi:10.1056/NEJMcp1314325. PMC 4487875. PMID 24785207. Archived from the original (PDF) on 21 August 2016. Retrieved 5 July 2016.
- ^ "Lyme Disease Diagnosis and Testing". cdc.gov. 10 January 2013. Archived from the original on 2 March 2015. Retrieved 2 March 2015.
- ^ "Lyme Disease Surveillance and Data". Centers for Disease Control and Prevention. 15 May 2024. Retrieved 16 August 2024.
- ^ Kugeler KJ, Schwartz AM, Delorey MJ, Mead PS, Hinckley AF (February 2021). "Estimating the Frequency of Lyme Disease Diagnoses, United States, 2010-2018". Emerging Infectious Diseases. 27 (2): 616–619. doi:10.3201/eid2702.202731. PMC 7853543. PMID 33496229.
- ^ Marques AR, Strle F, Wormser GP (August 2021). "Comparison of Lyme Disease in the United States and Europe". Emerging Infectious Diseases. 27 (8): 2017–2024. doi:10.3201/eid2708.204763. PMC 8314816. PMID 34286689.
- ^ Wenner M (11 June 2021). "Let's Do a Tick Check - These pervasive bloodsuckers can give you more than just Lyme disease. Here's how to protect yourself. (Interactive)". The New York Times. Retrieved 19 June 2021.
- ^ Wolcott KA, Margos G, Fingerle V, Becker NS (September 2021). "Host association of Borrelia burgdorferi sensu lato: A review". Ticks and Tick-Borne Diseases. 12 (5): 101766. doi:10.1016/j.ttbdis.2021.101766. PMID 34161868.
- Aucott J, Morrison C, Munoz B, Rowe PC, Schwarzwalder A, West SK (June 2009). "Diagnostic challenges of early Lyme disease: lessons from a community case series". BMC Infectious Diseases. 9: 79. doi:10.1186/1471-2334-9-79. PMC 2698836. PMID 19486523.
- Johnson RC (1996). "Borrelia". In Baron S, et al. (eds.). Baron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 978-0-9631172-1-2. PMID 21413339. Archived from the original on 7 February 2009.
- ^ "Lyme disease transmission". cdc.gov. 11 January 2013. Archived from the original on 3 March 2015. Retrieved 2 March 2015.
- ^ Steere AC, Strle F, Wormser GP, Hu LT, Branda JA, Hovius JW, et al. (December 2016). "Lyme borreliosis". Nature Reviews. Disease Primers. 2: 16090. doi:10.1038/nrdp.2016.90. PMC 5539539. PMID 27976670.
- "Lyme borreliosis" (PDF). ECDC. Archived (PDF) from the original on 29 September 2018. Retrieved 29 September 2018.
- ^ Pritt BS, Mead PS, Johnson DK, Neitzel DF, Respicio-Kingry LB, Davis JP, et al. (May 2016). "Identification of a novel pathogenic Borrelia species causing Lyme borreliosis with unusually high spirochaetaemia: a descriptive study". The Lancet. Infectious Diseases. 16 (5): 556–564. doi:10.1016/S1473-3099(15)00464-8. PMC 4975683. PMID 26856777.
- "Two-step Laboratory Testing Process". cdc.gov. 15 November 2011. Archived from the original on 12 March 2015. Retrieved 2 March 2015.
- "Testing of Ticks". cdc.gov. 4 June 2013. Archived from the original on 19 February 2015. Retrieved 2 March 2015.
Although some commercial groups offer testing, in general it is not recommended
- "Tick Removal". cdc.gov. 23 June 2014. Archived from the original on 10 March 2015. Retrieved 2 March 2015.
- ^ "Post-Treatment Lyme Disease Syndrome". cdc.gov. 1 December 2017. Archived from the original on 27 February 2015. Retrieved 20 June 2018.
- Regional Disease Vector Ecology Profile: Central Europe. DIANE Publishing. April 2001. p. 136. ISBN 978-1-4289-1143-7. Archived from the original on 8 September 2017.
- Williams C (2007). Infectious disease epidemiology : theory and practice (2nd ed.). Sudbury, Mass.: Jones and Bartlett Publishers. p. 447. ISBN 978-0-7637-2879-3. Archived from the original on 8 September 2017.
- "Willy Burgdorfer – obituary". Daily Telegraph. 1 December 2014. Archived from the original on 1 December 2014. Retrieved 1 December 2014.
- ^ CDC (11 June 2024). "Chronic Symptoms and Lyme Disease". Lyme Disease. Retrieved 27 July 2024.
- Baker PJ (November 2010). "Chronic Lyme disease: in defense of the scientific enterprise". FASEB Journal. 24 (11): 4175–4177. doi:10.1096/fj.10-167247. PMID 20631327. S2CID 36141950.
- Lantos PM (June 2015). "Chronic Lyme disease". Infectious Disease Clinics of North America. 29 (2): 325–340. doi:10.1016/j.idc.2015.02.006. PMC 4477530. PMID 25999227.
- ^ "Lyme disease vaccine". Centers for Disease Control and Prevention. 11 August 2022. Retrieved 13 November 2024.
- ^ Wright WF, Riedel DJ, Talwani R, Gilliam BL (June 2012). "Diagnosis and management of Lyme disease". American Family Physician. 85 (11): 1086–1093. PMID 22962880. Archived from the original on 27 September 2013.
- ^ "Lyme disease rashes and look-alikes". Lyme Disease. Centers for Disease Control and Prevention. 21 December 2018. Archived from the original on 2 April 2019. Retrieved 18 April 2019.
- ^ "Lyme disease: erythema migrans". Lyme disease NICE guideline . National Institute for Health and Care Excellence. Archived from the original on 9 May 2019. Retrieved 8 May 2019.
- Boyce RM, Pretsch P, Tyrlik K, Schulz A, Giandomenico DA, Barbarin AM, et al. (March 2024). "Delayed Diagnosis of Locally Acquired Lyme Disease, Central North Carolina, USA". Emerging Infectious Diseases. 30 (3): 564–567. doi:10.3201/eid3003.231302. PMC 10902532. PMID 38407256.
- ^ Tibbles CD, Edlow JA (June 2007). "Does this patient have erythema migrans?". JAMA. 297 (23): 2617–2627. doi:10.1001/jama.297.23.2617. PMID 17579230.
- Trayes KP, Savage K, Studdiford JS (1 September 2018). "Annular Lesions: Diagnosis and Treatment". American Family Physician. 98 (5): 283–291. PMID 30216021.
- ^ Lyme disease at eMedicine
- ^ Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, et al. (November 2006). "The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America". Clinical Infectious Diseases. 43 (9): 1089–1134. doi:10.1086/508667. PMID 17029130.
- "Lyme Disease". The Lecturio Medical Concept Library. Retrieved 9 July 2021.
- Steere AC, Sikand VK, Schoen RT, Nowakowski J (August 2003). "Asymptomatic infection with Borrelia burgdorferi". Clinical Infectious Diseases. 37 (4): 528–532. doi:10.1086/376914. PMID 12905137. (primary source)
- ^ Biesiada G, Czepiel J, Leśniak MR, Garlicki A, Mach T (December 2012). "Lyme disease: review". Archives of Medical Science. 8 (6): 978–982. doi:10.5114/aoms.2012.30948. PMC 3542482. PMID 23319969.
- ^ Halperin JJ (June 2008). "Nervous system Lyme disease". Infectious Disease Clinics of North America. 22 (2): 261–74, vi. doi:10.1016/j.idc.2007.12.009. PMID 18452800. S2CID 10590435.
- ^ Mygland A, Ljøstad U, Fingerle V, Rupprecht T, Schmutzhard E, Steiner I (January 2010). "EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis" (PDF). European Journal of Neurology. 17 (1): 8–16. doi:10.1111/j.1468-1331.2009.02862.x. PMID 19930447. S2CID 14166137. Archived (PDF) from the original on 8 August 2017. Retrieved 30 April 2019.
- ^ Pachner AR, Steere AC (July 1984). "Neurological findings of Lyme disease". The Yale Journal of Biology and Medicine. 57 (4): 481–483. PMC 2590042. PMID 6516450.
- Moscatello AL, Worden DL, Nadelman RB, Wormser G, Lucente F (June 1991). "Otolaryngologic aspects of Lyme disease". The Laryngoscope. 101 (6 Pt 1): 592–595. doi:10.1288/00005537-199106000-00004. PMID 2041438. S2CID 35345898.
- ^ Ogrinc K, Lusa L, Lotrič-Furlan S, Bogovič P, Stupica D, Cerar T, et al. (August 2016). "Course and Outcome of Early European Lyme Neuroborreliosis (Bannwarth Syndrome): Clinical and Laboratory Findings". Clinical Infectious Diseases. 63 (3): 346–353. doi:10.1093/cid/ciw299. PMID 27161773.
- ^ Garro A, Nigrovic LE (May 2018). "Managing Peripheral Facial Palsy". Annals of Emergency Medicine. 71 (5): 618–624. doi:10.1016/j.annemergmed.2017.08.039. PMID 29110887.
- ^ Halperin JJ (September 2010). "Nervous system Lyme disease". The Journal of the Royal College of Physicians of Edinburgh. 40 (3): 248–255. doi:10.4997/JRCPE.2010.314 (inactive 1 December 2024). PMID 21127770.
{{cite journal}}: CS1 maint: DOI inactive as of December 2024 (link) - ^ Fish AE, Pride YB, Pinto DS (June 2008). "Lyme carditis" (PDF). Infectious Disease Clinics of North America. 22 (2): 275–88, vi. doi:10.1016/j.idc.2007.12.008. PMID 18452801. Archived (PDF) from the original on 29 August 2017. Retrieved 9 May 2019.
- ^ Stanek G, Wormser GP, Gray J, Strle F (February 2012). "Lyme borreliosis". Lancet. 379 (9814): 461–473. doi:10.1016/S0140-6736(11)60103-7. PMID 21903253. S2CID 31461047.
- ^ Stanek G, Strle F (June 2008). "Lyme disease: European perspective". Infectious Disease Clinics of North America. 22 (2): 327–39, vii. doi:10.1016/j.idc.2008.01.001. PMID 18452805.
- Guardado KE, Sergent S (January 2022). "Pediatric unilateral knee swelling: a case report of a complicated differential diagnosis and often overlooked cause". Journal of Osteopathic Medicine. 122 (2): 105–109. doi:10.1515/jom-2020-0332. PMID 34989214. S2CID 245705028.
- Puius YA, Kalish RA (June 2008). "Lyme arthritis: pathogenesis, clinical presentation, and management". Infectious Disease Clinics of North America. 22 (2): 289–300, vi–vii. doi:10.1016/j.idc.2007.12.014. PMID 18452802.
- ^ Wormser GP, Strle F, Shapiro ED, Dattwyler RJ, Auwaerter PG (February 2017). "A critical appraisal of the mild axonal peripheral neuropathy of late neurologic Lyme disease". Diagnostic Microbiology and Infectious Disease. 87 (2): 163–167. doi:10.1016/j.diagmicrobio.2016.11.003. PMC 5924701. PMID 27914746.
- Bratton RL, Whiteside JW, Hovan MJ, Engle RL, Edwards FD (May 2008). "Diagnosis and treatment of Lyme disease". Mayo Clinic Proceedings. 83 (5): 566–571. doi:10.4065/83.5.566. PMID 18452688.
- Shadick NA, Phillips CB, Sangha O, Logigian EL, Kaplan RF, Wright EA, et al. (December 1999). "Musculoskeletal and neurologic outcomes in patients with previously treated Lyme disease". Annals of Internal Medicine. 131 (12): 919–926. doi:10.7326/0003-4819-131-12-199912210-00003. PMID 10610642. S2CID 20746489.
- Seltzer EG, Gerber MA, Cartter ML, Freudigman K, Shapiro ED (February 2000). "Long-term outcomes of persons with Lyme disease". JAMA. 283 (5): 609–616. doi:10.1001/jama.283.5.609. PMID 10665700.
- ^ Lantos PM, Rumbaugh J, Bockenstedt LK, Falck-Ytter YT, Aguero-Rosenfeld ME, Auwaerter PG, et al. (January 2021). "Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease". Clinical Infectious Diseases. 72 (1): e1 – e48. doi:10.1093/cid/ciaa1215. PMID 33417672.
- Mullegger RR (2004). "Dermatological manifestations of Lyme borreliosis". European Journal of Dermatology. 14 (5): 296–309. PMID 15358567.
- Winslow C, Coburn J (2019). "Recent discoveries and advancements in research on the Lyme disease spirochete Borrelia burgdorferi". F1000Res. 8: 763. doi:10.12688/f1000research.18379.1. PMC 6545822. PMID 31214329.
- Radolf JD, Samuels DS, eds. (2021). Lyme Disease and Relapsing Fever Spirochetes: Genomics, Molecular Biology, Host Interactions, and Disease Pathogenesis. Caister Academic Press. ISBN 978-1-913652-61-6.
- Cutler SJ, Ruzic-Sabljic E, Potkonjak A (February 2017). "Emerging borreliae - Expanding beyond Lyme borreliosis" (PDF). Molecular and Cellular Probes. 31: 22–27. doi:10.1016/j.mcp.2016.08.003. PMID 27523487.
- Stanek G, Reiter M (April 2011). "The expanding Lyme Borrelia complex--clinical significance of genomic species?". Clinical Microbiology and Infection. 17 (4): 487–493. doi:10.1111/j.1469-0691.2011.03492.x. PMID 21414082.
- Schneider BS, Schriefer ME, Dietrich G, Dolan MC, Morshed MG, Zeidner NS (October 2008). "Borrelia bissettii isolates induce pathology in a murine model of disease". Vector Borne and Zoonotic Diseases. 8 (5): 623–633. doi:10.1089/vbz.2007.0251. PMID 18454594. Archived from the original on 29 January 2020. Retrieved 29 January 2020.
- Rudenko N, Golovchenko M, Mokrácek A, Piskunová N, Ruzek D, Mallatová N, et al. (October 2008). "Detection of Borrelia bissettii in cardiac valve tissue of a patient with endocarditis and aortic valve stenosis in the Czech Republic". Journal of Clinical Microbiology. 46 (10): 3540–3543. doi:10.1128/JCM.01032-08. PMC 2566110. PMID 18650352.
- "UpToDate". www.uptodate.com. Retrieved 10 July 2021.
- ^ Tilly K, Rosa PA, Stewart PE (June 2008). "Biology of infection with Borrelia burgdorferi". Infectious Disease Clinics of North America. 22 (2): 217–34, v. doi:10.1016/j.idc.2007.12.013. PMC 2440571. PMID 18452798.
- ^ Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 434–37. ISBN 978-0-8385-8529-0.
- Smith-Fiola D, Hamilton GC (March 2005). "2005 Fact Sheet, Prevent Tick Bites: Prevent Lyme Disease" (PDF). Rutgers University, Rutgers Cooperative Research & Extension, New Jersey Agricultural Experiment Station. Archived from the original (PDF) on 26 June 2013.
- Scribner H (31 May 2019). "People are freaking out over the CDC's photo of a muffin with ticks in it". Deseret News. Utah. Archived from the original on 25 January 2020.
The U.S. CDC published a picture of a poppy seed muffin in which some of the "poppy seeds" were actually ticks
- ^ Lo Re V, Occi JL, MacGregor RR (April 2004). "Identifying the vector of Lyme disease". American Family Physician. 69 (8): 1935–1937. PMID 15117014.
- "Westport Weston Health District". 2004. Archived from the original on 29 September 2013. Retrieved 26 September 2013.
- ^ "Lyme Disease Data and surveillance". Lyme Disease. Centers for Disease Control and Prevention. 5 February 2019. Archived from the original on 13 April 2019. Retrieved 12 April 2019.
- Hovius JW, van Dam AP, Fikrig E (September 2007). "Tick-host-pathogen interactions in Lyme borreliosis" (PDF). Trends in Parasitology. 23 (9): 434–438. doi:10.1016/j.pt.2007.07.001. PMID 17656156. Archived (PDF) from the original on 16 February 2019. Retrieved 9 September 2019.
- ^ Steere AC, Coburn J, Glickstein L (April 2004). "The emergence of Lyme disease". The Journal of Clinical Investigation. 113 (8): 1093–1101. doi:10.1172/JCI21681. PMC 385417. PMID 15085185.
- Hu L (13 May 2019). "Patient education: What to do after a tick bite to prevent Lyme disease (Beyond the Basics)". www.uptodate.com. UpToDate. Archived from the original on 1 January 2020. Retrieved 30 January 2020.
- ^ Richter D, Matuschka FR (July 2006). "Perpetuation of the Lyme disease spirochete Borrelia lusitaniae by lizards". Applied and Environmental Microbiology. 72 (7): 4627–4632. Bibcode:2006ApEnM..72.4627R. doi:10.1128/AEM.00285-06. PMC 1489336. PMID 16820453.
- ^ Swanson KI, Norris DE (2007). "Detection of Borrelia burgdorferi DNA in lizards from Southern Maryland". Vector Borne and Zoonotic Diseases. 7 (1): 42–49. doi:10.1089/vbz.2006.0548. PMC 4128253. PMID 17417956.
- Giery ST, Ostfeld RS (June 2007). "The role of lizards in the ecology of Lyme disease in two endemic zones of the northeastern United States". The Journal of Parasitology. 93 (3): 511–517. doi:10.1645/GE-1053R1.1. PMID 17626342. S2CID 42617030.
- Amore G, Tomassone L, Grego E, Ragagli C, Bertolotti L, Nebbia P, et al. (March 2007). "Borrelia lusitaniae in immature Ixodes ricinus (Acari: Ixodidae) feeding on common wall lizards in Tuscany, central Italy". Journal of Medical Entomology. 44 (2): 303–307. doi:10.1603/0022-2585(2007)44[303:BLIIIR]2.0.CO;2 (inactive 1 December 2024). PMID 17427701. S2CID 18882042.
{{cite journal}}: CS1 maint: DOI inactive as of December 2024 (link) - Majláthová V, Majláth I, Derdáková M, Víchová B, Pet'ko B (December 2006). "Borrelia lusitaniae and green lizards (Lacerta viridis), Karst Region, Slovakia". Emerging Infectious Diseases. 12 (12): 1895–1901. doi:10.3201/eid1212.060784. PMC 3291370. PMID 17326941.
- ^ Lane RS, Mun J, Eisen L, Eisen RJ (August 2006). "Refractoriness of the western fence lizard (Sceloporus occidentalis) to the Lyme disease group spirochete Borrelia bissettii". The Journal of Parasitology. 92 (4): 691–696. doi:10.1645/GE-738R1.1. PMID 16995383. S2CID 24200639.
- de Mik EL, van Pelt W, Docters-van Leeuwen BD, van der Veen A, Schellekens JF, Borgdorff MW (April 1997). "The geographical distribution of tick bites and erythema migrans in general practice in The Netherlands". International Journal of Epidemiology. 26 (2): 451–457. doi:10.1093/ije/26.2.451. PMID 9169184.
- Sun Y, Xu R (2003). "Ability of Ixodes persulcatus, Haemaphysalis concinna and Dermacentor silvarum ticks to acquire and transstadially transmit Borrelia garinii". Experimental and Applied Acarology. 31 (1–2): 151–160. doi:10.1023/B:APPA.0000005119.30172.43. PMID 14756409. S2CID 19214181.
- Ledin KE, Zeidner NS, Ribeiro JM, Biggerstaff BJ, Dolan MC, Dietrich G, et al. (March 2005). "Borreliacidal activity of saliva of the tick Amblyomma americanum". Medical and Veterinary Entomology. 19 (1): 90–95. doi:10.1111/j.0269-283X.2005.00546.x. PMID 15752182. S2CID 270178.
- Masters EJ, Grigery CN, Masters RW (June 2008). "STARI, or Masters disease: Lone Star tick-vectored Lyme-like illness". Infectious Disease Clinics of North America. 22 (2): 361–76, viii. doi:10.1016/j.idc.2007.12.010. PMID 18452807.
- Clark K (November 2004). "Borrelia species in host-seeking ticks and small mammals in northern Florida". Journal of Clinical Microbiology. 42 (11): 5076–5086. doi:10.1128/JCM.42.11.5076-5086.2004. PMC 525154. PMID 15528699.
- Eisen L, Eisen RJ, Lane RS (December 2004). "The roles of birds, lizards, and rodents as hosts for the western black-legged tick Ixodes pacificus". Journal of Vector Ecology. 29 (2): 295–308. PMID 15709249.
- Walsh CA, Mayer EW, Baxi LV (January 2007). "Lyme disease in pregnancy: case report and review of the literature". Obstetrical & Gynecological Survey. 62 (1): 41–50. doi:10.1097/01.ogx.0000251024.43400.9a. PMID 17176487. S2CID 31929160.
- Dotters-Katz SK, Kuller J, Heine RP (September 2013). "Arthropod-borne bacterial diseases in pregnancy". Obstetrical & Gynecological Survey. 68 (9): 635–649. doi:10.1097/OGX.0b013e3182a5ed46. PMID 25102120. S2CID 26801402.
- Lakos A, Solymosi N (June 2010). "Maternal Lyme borreliosis and pregnancy outcome". International Journal of Infectious Diseases. 14 (6): e494 – e498. doi:10.1016/j.ijid.2009.07.019. PMID 19926325.
- Steere AC (August 1989). "Lyme disease". The New England Journal of Medicine. 321 (9): 586–596. doi:10.1056/NEJM198908313210906. PMID 2668764.
- ^ "CDC Lyme disease FAQ". Centers for Disease Control and Prevention. 8 January 2021. Retrieved 11 January 2023.
- Swanson SJ, Neitzel D, Reed KD, Belongia EA (October 2006). "Coinfections acquired from ixodes ticks". Clinical Microbiology Reviews. 19 (4): 708–727. doi:10.1128/CMR.00011-06. PMC 1592693. PMID 17041141.
- Lindgren E, Gustafson R (July 2001). "Tick-borne encephalitis in Sweden and climate change". Lancet. 358 (9275): 16–18. doi:10.1016/S0140-6736(00)05250-8. PMID 11454371. S2CID 336323.
- Pachner AR, Steiner I (June 2007). "Lyme neuroborreliosis: infection, immunity, and inflammation". The Lancet. Neurology. 6 (6): 544–552. doi:10.1016/S1474-4422(07)70128-X. PMID 17509489. S2CID 11600373.
- "Does Borrelia burgdorferi produce a neurotoxin ?". American Lyme Disease Foundation. Retrieved 30 July 2022.
- Auwaerter PG, Aucott J, Dumler JS (January 2004). "Lyme borreliosis (Lyme disease): molecular and cellular pathobiology and prospects for prevention, diagnosis and treatment". Expert Reviews in Molecular Medicine. 6 (2): 1–22. doi:10.1017/S1462399404007276. PMID 14987414. S2CID 24311718.
- Strnad M, Rudenko N, Rego RO (December 2023). "Pathogenicity and virulence of Borrelia burgdorferi". Virulence. 14 (1): 2265015. doi:10.1080/21505594.2023.2265015. PMC 10566445. PMID 37814488.
- Fikrig E, Narasimhan S (April 2006). "Borrelia burgdorferi--traveling incognito?". Microbes and Infection. 8 (5): 1390–1399. doi:10.1016/j.micinf.2005.12.022. PMID 16698304.
- Xu Q, Seemanapalli SV, Reif KE, Brown CR, Liang FT (April 2007). "Increasing the recruitment of neutrophils to the site of infection dramatically attenuates Borrelia burgdorferi infectivity". Journal of Immunology. 178 (8): 5109–5115. doi:10.4049/jimmunol.178.8.5109. PMID 17404293.
- Coleman JL, Gebbia JA, Piesman J, Degen JL, Bugge TH, Benach JL (June 1997). "Plasminogen is required for efficient dissemination of B. burgdorferi in ticks and for enhancement of spirochetemia in mice". Cell. 89 (7): 1111–1119. doi:10.1016/S0092-8674(00)80298-6. PMID 9215633. S2CID 18750257.
- Steere AC (July 2001). "Lyme disease". The New England Journal of Medicine. 345 (2): 115–125. doi:10.1056/NEJM200107123450207. PMID 11450660.
- Rupprecht TA, Koedel U, Fingerle V, Pfister HW (2008). "The pathogenesis of lyme neuroborreliosis: from infection to inflammation". Molecular Medicine. 14 (3–4): 205–212. doi:10.2119/2007-00091.Rupprecht. PMC 2148032. PMID 18097481. Archived from the original on 3 April 2015.
- Cabello FC, Godfrey HP, Newman SA (August 2007). "Hidden in plain sight: Borrelia burgdorferi and the extracellular matrix". Trends in Microbiology. 15 (8): 350–354. doi:10.1016/j.tim.2007.06.003. PMID 17600717. Archived from the original on 7 July 2019. Retrieved 5 July 2019.
- Ercolini AM, Miller SD (January 2009). "The role of infections in autoimmune disease". Clinical and Experimental Immunology. 155 (1): 1–15. doi:10.1111/j.1365-2249.2008.03834.x. PMC 2665673. PMID 19076824.
- Singh SK, Girschick HJ (July 2004). "Lyme borreliosis: from infection to autoimmunity". Clinical Microbiology and Infection. 10 (7): 598–614. doi:10.1111/j.1469-0691.2004.00895.x. PMID 15214872.
- Oldstone MB (October 1998). "Molecular mimicry and immune-mediated diseases". FASEB Journal. 12 (13): 1255–1265. doi:10.1096/fasebj.12.13.1255. PMC 7164021. PMID 9761770. S2CID 16089636.
- Raveche ES, Schutzer SE, Fernandes H, Bateman H, McCarthy BA, Nickell SP, et al. (February 2005). "Evidence of Borrelia autoimmunity-induced component of Lyme carditis and arthritis". Journal of Clinical Microbiology. 43 (2): 850–856. doi:10.1128/JCM.43.2.850-856.2005. PMC 548028. PMID 15695691.
- Weinstein A, Britchkov M (July 2002). "Lyme arthritis and post-Lyme disease syndrome". Current Opinion in Rheumatology. 14 (4): 383–387. doi:10.1097/00002281-200207000-00008. PMID 12118171.
- Bolz DD, Weis JJ (August 2004). "Molecular mimicry to Borrelia burgdorferi: pathway to autoimmunity?". Autoimmunity. 37 (5): 387–392. doi:10.1080/08916930410001713098. PMID 15621562. S2CID 43045224.
- Brown SL, Hansen SL, Langone JJ (July 1999). "Role of serology in the diagnosis of Lyme disease". JAMA. 282 (1): 62–66. doi:10.1001/jama.282.1.62. PMID 10404913.
- Hofmann H (1996). "Lyme borreliosis--problems of serological diagnosis". Infection. 24 (6): 470–472. doi:10.1007/BF01713052. PMID 9007597. S2CID 19701481.
- Wormser GP, Masters E, Nowakowski J, McKenna D, Holmgren D, Ma K, et al. (October 2005). "Prospective clinical evaluation of patients from Missouri and New York with erythema migrans-like skin lesions". Clinical Infectious Diseases. 41 (7): 958–965. doi:10.1086/432935. PMID 16142659.
- ^ "Lyme Disease risk areas map". Risk of Lyme disease to Canadians. Government of Canada. 27 January 2015. Archived from the original on 10 May 2019. Retrieved 8 May 2019.
- ^ Aucott J, Morrison C, Munoz B, Rowe PC, Schwarzwalder A, West SK (June 2009). "Diagnostic challenges of early Lyme disease: lessons from a community case series". BMC Infectious Diseases. 9 (79): 79. doi:10.1186/1471-2334-9-79. PMC 2698836. PMID 19486523.
- "Lyme disease diagnosis". Centers for Disease Control and Prevention (CDC). 7 October 2008. Archived from the original on 28 August 2009. Retrieved 6 July 2009.
- ^ "Lyme disease". NICE guideline . National Institute for Health and Care Excellence. 11 April 2018. Archived from the original on 11 May 2019. Retrieved 24 May 2019.
- Wilske B (2005). "Epidemiology and diagnosis of Lyme borreliosis". Annals of Medicine. 37 (8): 568–579. doi:10.1080/07853890500431934. PMID 16338759. S2CID 30818459.
- ^ DePietropaolo DL, Powers JH, Gill JM, Foy AJ (July 2005). "Diagnosis of lyme disease". American Family Physician. 72 (2): 297–304. doi:10.1093/cid/cir464. PMID 16050454.
- "Are serological tests of any value in the diagnosis of Lyme disease?". American Lyme Disease Foundation. Archived from the original on 19 December 2019. Retrieved 2 December 2019.
- Coyle PK, Schutzer SE, Deng Z, Krupp LB, Belman AL, Benach JL, et al. (November 1995). "Detection of Borrelia burgdorferi-specific antigen in antibody-negative cerebrospinal fluid in neurologic Lyme disease". Neurology. 45 (11): 2010–2015. doi:10.1212/WNL.45.11.2010. PMID 7501150. S2CID 23797801.
- ^ Halperin JJ, Shapiro ED, Logigian E, Belman AL, Dotevall L, Wormser GP, et al. (July 2007). "Practice parameter: treatment of nervous system Lyme disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 69 (1): 91–102. doi:10.1212/01.wnl.0000265517.66976.28. PMID 17522387.
- Molloy PJ, Persing DH, Berardi VP (August 2001). "False-positive results of PCR testing for Lyme disease". Clinical Infectious Diseases. 33 (3): 412–413. doi:10.1086/321911. PMID 11438915.
- ^ Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser GP (July 2005). "Diagnosis of lyme borreliosis". Clinical Microbiology Reviews. 18 (3): 484–509. doi:10.1128/CMR.18.3.484-509.2005. PMC 1195970. PMID 16020686.
- Nocton JJ, Dressler F, Rutledge BJ, Rys PN, Persing DH, Steere AC (January 1994). "Detection of Borrelia burgdorferi DNA by polymerase chain reaction in synovial fluid from patients with Lyme arthritis". The New England Journal of Medicine. 330 (4): 229–234. doi:10.1056/NEJM199401273300401. PMID 8272083.
- Hyde FW, Johnson RC, White TJ, Shelburne CE (January 1989). "Detection of antigens in urine of mice and humans infected with Borrelia burgdorferi, etiologic agent of Lyme disease". Journal of Clinical Microbiology. 27 (1): 58–61. doi:10.1128/JCM.27.1.58-61.1989. PMC 267232. PMID 2913036.
- Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, et al. (July 2014). "The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics". Pathogens and Disease. 71 (2): 164–176. doi:10.1111/2049-632X.12136. PMC 7108521. PMID 24449537.
- Shafagati N, Patanarut A, Luchini A, Lundberg L, Bailey C, Petricoin E, et al. (July 2014). "The use of Nanotrap particles for biodefense and emerging infectious disease diagnostics". Pathogens and Disease. 71 (2): 164–176. doi:10.1111/2049-632x.12136. PMC 7108521. PMID 24449537.
- Burdash N, Fernandes J (June 1991). "Lyme borreliosis: detecting the great imitator". The Journal of the American Osteopathic Association. 91 (6): 573–4, 577–8. doi:10.1515/jom-1991-910610. PMID 1874654. S2CID 245118295.
- Hildenbrand P, Craven DE, Jones R, Nemeskal P (June 2009). "Lyme neuroborreliosis: manifestations of a rapidly emerging zoonosis". AJNR. American Journal of Neuroradiology. 30 (6): 1079–1087. doi:10.3174/ajnr.A1579. PMC 7051319. PMID 19346313.
- Westervelt HJ, McCaffrey RJ (September 2002). "Neuropsychological functioning in chronic Lyme disease". Neuropsychology Review. 12 (3): 153–177. doi:10.1023/A:1020381913563. PMID 12428915. S2CID 2807397.
- Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, et al. (January 2007). "Recommendations for the management of herpes zoster". Clinical Infectious Diseases. 44 (Suppl 1): S1-26. doi:10.1086/510206. PMID 17143845. S2CID 10894629.
- Halperin JJ (May 2015). "Chronic Lyme disease: misconceptions and challenges for patient management". Infection and Drug Resistance. 8: 119–128. doi:10.2147/IDR.S66739. PMC 4440423. PMID 26028977.
- ^ Tarulli AW, Raynor EM (May 2007). "Lumbosacral radiculopathy" (PDF). Neurologic Clinics. 25 (2): 387–405. doi:10.1016/j.ncl.2007.01.008. PMID 17445735. S2CID 15518713. Archived from the original (PDF) on 20 February 2019.
- Pachner AR (1989). "Neurologic manifestations of Lyme disease, the new "great imitator"". Reviews of Infectious Diseases. 11 (Suppl 6): S1482 – S1486. doi:10.1093/clinids/11.Supplement_6.S1482. PMID 2682960. S2CID 3862308.
- Branda JA, Linskey K, Kim YA, Steere AC, Ferraro MJ (September 2011). "Two-tiered antibody testing for Lyme disease with use of 2 enzyme immunoassays, a whole-cell sonicate enzyme immunoassay followed by a VlsE C6 peptide enzyme immunoassay". Clinical Infectious Diseases. 53 (6): 541–547. doi:10.1093/cid/cir464. PMID 21865190.
- ^ "Preventing tick bites on people". Lyme Disease. Centers for Disease Control and Prevention. 8 March 2019. Archived from the original on 15 June 2019. Retrieved 21 May 2019.
- ^ "About ticks – preventative measures". Tick-borne diseases. Companion Vector-Borne Diseases. Archived from the original on 7 June 2019. Retrieved 21 May 2019.
- ^ Eisen L, Eisen RJ (September 2016). "Critical Evaluation of the Linkage Between Tick-Based Risk Measures and the Occurrence of Lyme Disease Cases". Journal of Medical Entomology. 53 (5): 1050–1062. doi:10.1093/jme/tjw092. PMC 5777907. PMID 27330093.
- "Host seeking". CVBD: Companion Vector-Borne Diseases. Archived from the original on 16 October 2016. Retrieved 8 December 2016.
- ^ "Tips to prevent tick bytes". Insect repellents. Environmental Protection Agency. 15 July 2013. Archived from the original on 15 April 2019. Retrieved 21 May 2019.
- ^ "Protection against Mosquitoes, Ticks, & Other Arthropods". Travelers' Health. Centers for Disease Control and Prevention. Archived from the original on 9 May 2019. Retrieved 21 May 2019.
- ^ Miller NJ, Rainone EE, Dyer MC, González ML, Mather TN (March 2011). "Tick bite protection with permethrin-treated summer-weight clothing". Journal of Medical Entomology. 48 (2): 327–333. doi:10.1603/me10158. PMID 21485369.
- ^ Eisen L, Rose D, Prose R, Breuner NE, Dolan MC, Thompson K, et al. (October 2017). "Bioassays to evaluate non-contact spatial repellency, contact irritancy, and acute toxicity of permethrin-treated clothing against nymphal Ixodes scapularis ticks". Ticks and Tick-Borne Diseases. 8 (6): 837–849. doi:10.1016/j.ttbdis.2017.06.010. PMC 5665650. PMID 28754599.
- Dymond NL, Swift IM (June 2008). "Permethrin toxicity in cats: a retrospective study of 20 cases". Australian Veterinary Journal. 86 (6): 219–223. doi:10.1111/j.1751-0813.2008.00298.x. PMID 18498556.
- ^ "Repellents: protection against mosquitoes, ticks and other arthropods". Insect repellents. Environmental Protection Agency. 9 July 2013. Archived from the original on 20 May 2019. Retrieved 21 May 2019.
- ^ Nguyen QD, Vu MN, Hebert AA (January 2023). "Insect repellents: An updated review for the clinician". Journal of the American Academy of Dermatology. 88 (1): 123–130. doi:10.1016/j.jaad.2018.10.053. PMID 30395919. S2CID 53246686.
- ^ Stafford KC (2007). "Tick management handbook (rev. ed.)" (PDF). Bulletins. Connecticut Agricultural Experiment Station. Archived (PDF) from the original on 3 April 2019. Retrieved 21 May 2019.
- Piesman J, Dolan MC (May 2002). "Protection against lyme disease spirochete transmission provided by prompt removal of nymphal Ixodes scapularis (Acari: Ixodidae)". Journal of Medical Entomology. 39 (3): 509–512. doi:10.1603/0022-2585-39.3.509. PMID 12061448. S2CID 39805040.
- ^ "Tick removal and testing". Lyme Disease. Centers for Disease Control and Prevention. 22 April 2019. Archived from the original on 23 November 2017. Retrieved 21 May 2019.
- ^ "Tick Allergy". 2014. Archived from the original on 14 May 2015. Retrieved 30 April 2015.
- Röggla G (2002). "Death of unknown origin in alpine medicine". Wilderness & Environmental Medicine. 13 (2): 181. doi:10.1580/1080-6032(2002)013[0181:ltte]2.0.co;2. PMID 12092975.
- Ghirga G, Ghirga P (September 2010). "Effective tick removal with a fishing line knot". Wilderness & Environmental Medicine. 21 (3): 270–271. doi:10.1016/j.wem.2010.04.005. PMID 20832708.
- ^ "Preventing tick bites in the yard". Lyme Disease. Centers for Disease Control and Prevention. 8 March 2019. Archived from the original on 15 June 2019. Retrieved 21 May 2019.
- "CDC – Lyme Disease – NIOSH Workplace Safety and Health Topic". www.cdc.gov. 3 August 2017. Archived from the original on 13 November 2015. Retrieved 3 November 2015.
- "Risks: Lyme Disease | NIOSH | CDC". www.cdc.gov. 14 November 2018. Archived from the original on 26 April 2019. Retrieved 26 April 2019.
- "Lyme disease". The Centers for Disease Control and Prevention. 12 October 2016. Archived from the original on 17 June 2017. Retrieved 22 June 2017.
 This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention.
- Levi T, Kilpatrick AM, Mangel M, Wilmers CC (3 July 2012). "Deer, predators, and the emergence of Lyme disease". Proceedings of the National Academy of Sciences. 109 (27): 10942–10947. Bibcode:2012PNAS..10910942L. doi:10.1073/pnas.1204536109. PMC 3390851. PMID 22711825.
- ^ Chrobak U (3 February 2022). "Lyme and other tick-borne diseases are on the rise. But why?". Knowable Magazine. doi:10.1146/knowable-020222-1. Retrieved 4 March 2022.
- Rand PW, Lubelczyk C, Holman MS, Lacombe EH, Smith RP (July 2004). "Abundance of Ixodes scapularis (Acari: Ixodidae) after the complete removal of deer from an isolated offshore island, endemic for Lyme Disease". Journal of Medical Entomology. 41 (4): 779–784. doi:10.1603/0022-2585-41.4.779. PMID 15311475. S2CID 5853201.
- "Figure 2: Changes in deer density and cases of Lyme disease in Mumford Cove, Connecticut, 1996–2004 (CT DEP data)" (PDF). Managing Urban Deer in Connecticut (2nd ed.). Connecticut Department of Environmental Protection – Wildlife Division. June 2007. p. 4. Archived (PDF) from the original on 2 June 2013.
- Stafford KC (2004). Tick Management Handbook (PDF). Connecticut Agricultural Experiment Station and Connecticut Department of Public Health. p. 46. Archived (PDF) from the original on 25 October 2007. Retrieved 21 August 2007.
- Wilson ML, Levine JF, Spielman A (1984). "Effect of deer reduction on abundance of the deer tick (Ixodes dammini)". Yale Journal of Biology and Medicine. 57 (4): 697–705. PMC 2589992. PMID 6516462.
- Jordan RA, Schulze TL, Jahn MB (1 September 2007). "Effects of Reduced Deer Density on the Abundance ofIxodes scapularis(Acari: Ixodidae) and Lyme Disease Incidence in a Northern New Jersey Endemic Area". Journal of Medical Entomology. 44 (5): 752–757. doi:10.1093/jmedent/44.5.752. ISSN 0022-2585. PMID 17915504.
- Kugeler KJ, Jordan RA, Schulze TL, Griffith KS, Mead PS (2016). "Will Culling White-Tailed Deer Prevent Lyme Disease?". Zoonoses and Public Health. 63 (5): 337–345. doi:10.1111/zph.12245. ISSN 1863-2378. PMC 4912954. PMID 26684932.
- Van Buskirk J, Ostfeld RS (1995). "Controlling Lyme Disease by Modifying the Density and Species Composition of Tick Hosts". Ecological Applications. 5 (4): 1133–1140. Bibcode:1995EcoAp...5.1133V. doi:10.2307/2269360. ISSN 1939-5582. JSTOR 2269360.
- Pearson P, Rich C, Feehan MJ, Ditchkoff SS, Rich SM (May 2023). "White-Tailed Deer Serum Kills the Lyme Disease Spirochete, Borrelia burgdorferi". Vector-Borne and Zoonotic Diseases. 23 (5): 303–305. doi:10.1089/vbz.2022.0095. ISSN 1530-3667. PMC 10178931. PMID 36944114.
- Rochlin I, Toledo A (June 2020). "Emerging tick-borne pathogens of public health importance: a mini-review". Journal of Medical Microbiology. 69 (6): 781–791. doi:10.1099/jmm.0.001206. PMC 7451033. PMID 32478654.
- Rajput ZI, Hu SH, Chen WJ, Arijo AG, Xiao CW (November 2006). "Importance of ticks and their chemical and immunological control in livestock". Journal of Zhejiang University. Science. B. 7 (11): 912–921. doi:10.1631/jzus.2006.B0912. PMC 1635821. PMID 17048307.
- ^ Gern L, Estrada-Peña A, Frandsen F, Gray JS, Jaenson TG, Jongejan F, et al. (March 1998). "European reservoir hosts of Borrelia burgdorferi sensu lato". Zentralblatt für Bakteriologie. 287 (3): 196–204. doi:10.1016/S0934-8840(98)80121-7. PMID 9580423.
- ^ Wodecka B, Rymaszewska A, Skotarczak B (April 2014). "Host and pathogen DNA identification in blood meals of nymphal Ixodes ricinus ticks from forest parks and rural forests of Poland". Experimental and Applied Acarology. 62 (4): 543–555. doi:10.1007/s10493-013-9763-x. PMC 3933768. PMID 24352572.
- Jaenson TG, Tälleklint L (September 1992). "Incompetence of roe deer as reservoirs of the Lyme borreliosis spirochete". Journal of Medical Entomology. 29 (5): 813–817. doi:10.1093/jmedent/29.5.813. PMID 1404260.
- Tälleklint L, Jaenson TG (November 1994). "Transmission of Borrelia burgdorferi s.l. from mammal reservoirs to the primary vector of Lyme borreliosis, Ixodes ricinus (Acari: Ixodidae), in Sweden". Journal of Medical Entomology. 31 (6): 880–886. doi:10.1093/jmedent/31.6.880. PMID 7815401.
- Overzier E, Pfister K, Herb I, Mahling M, Böck G, Silaghi C (June 2013). "Detection of tick-borne pathogens in roe deer (Capreolus capreolus), in questing ticks (Ixodes ricinus), and in ticks infesting roe deer in southern Germany". Ticks and Tick-Borne Diseases. 4 (4): 320–328. doi:10.1016/j.ttbdis.2013.01.004. PMID 23571115.
- ^ O'Bier NS, Hatke AL, Camire AC, Marconi RT (2021). "Human and Veterinary Vaccines for Lyme Disease". Current Issues in Molecular Biology. 42: 191–222. doi:10.21775/cimb.042.191. PMC 7946718. PMID 33289681.
- Poland GA, Jacobson RM (March 2001). "The prevention of Lyme disease with vaccine". Vaccine. 19 (17–19): 2303–2308. doi:10.1016/S0264-410X(00)00520-X. PMID 11257352.
- ^ Poland GA (February 2011). "Vaccines against Lyme disease: What happened and what lessons can we learn?". Clinical Infectious Diseases. 52 (Suppl 3): s253 – s258. doi:10.1093/cid/ciq116. PMID 21217172.
- Rowe C (13 June 1999). "Lukewarm Response To New Lyme Vaccine". The New York Times. Archived from the original on 10 February 2012. Retrieved 11 July 2008.
- ^ Abbott A (February 2006). "Lyme disease: uphill struggle". Nature. 439 (7076): 524–525. doi:10.1038/439524a. PMID 16452949. S2CID 4315588.
- "Sole Lyme Vaccine Is Pulled Off Market". The New York Times. 28 February 2002. Archived from the original on 30 August 2010. Retrieved 11 July 2008.
- ^ Nigrovic LE, Thompson KM (January 2007). "The Lyme vaccine: a cautionary tale". Epidemiology and Infection. 135 (1): 1–8. doi:10.1017/S0950268806007096. PMC 2870557. PMID 16893489.
- "When a vaccine is safe". Nature. 439 (7076): 509. February 2006. Bibcode:2006Natur.439Q.509.. doi:10.1038/439509a. PMID 16452935.
- Aronowitz RA (June 2012). "The rise and fall of the lyme disease vaccines: a cautionary tale for risk interventions in American medicine and public health". The Milbank Quarterly. 90 (2): 250–277. doi:10.1111/j.1468-0009.2012.00663.x. PMC 3460208. PMID 22709388.
- "Anti-vaxxers stopped the last Lyme disease vaccine. The FDA has just fast-tracked a new one". Newsweek. 25 July 2017. Archived from the original on 25 December 2017. Retrieved 25 December 2017.
- Brooks D (6 August 2018). "A Lyme vaccine for humans is getting closer, says French biotech firm". Concord Monitor. Retrieved 20 July 2021.
- Taylor NP (4 February 2022). "Pfizer's $130M Lyme disease vaccine advances to phase 3 after 3rd shot shown to increase antibodies". Fierce Biotech. Retrieved 5 June 2022.
- Neergaard L, Lum S (8 August 2022). "Major test of first possible Lyme vaccine in 20 years begins". Associated Press. Retrieved 11 August 2022.
- ^ "An Efficacy, Safety, Tolerability, Immunogenicity, and Lot-Consistency Clinical Trial of a 6-Valent OspA-Based Lyme Disease Vaccine (VLA15) (VALOR)". ClinicalTrials.gov. National Institute of Health. 28 July 2022. Retrieved 11 August 2022.
- Klein A (17 November 2021). "An mRNA vaccine that causes a red, itchy skin rash in response to bites by ticks may allow them to be removed before they transmit Lyme disease-causing bacteria". New Scientist.
- Hathaway B. "Novel Lyme vaccine shows promise". Yale University. Retrieved 13 December 2021.
Compared to non-immunized guinea pigs, vaccinated animals exposed to infected ticks quickly developed redness at the tick bite site. None of the immunized animals developed Lyme disease if ticks were removed when redness developed. In contrast, about half of the control group became infected with B. burgdorferi after tick removal. When a single infected tick was attached to immunized guinea pigs and not removed, none of vaccinated animals were infected compared to 60 percent of control animals. However, protection waned in immunized guinea pigs if three ticks remained attached to the animal. Ticks in immunized animals were unable to feed aggressively and dislodged more quickly than those on guinea pigs in the control group.
- Sajid A, Matias J, Arora G, Kurokawa C, DePonte K, Tang X, et al. (November 2021). "mRNA vaccination induces tick resistance and prevents transmission of the Lyme disease agent". Science Translational Medicine. 13 (620): eabj9827. doi:10.1126/scitranslmed.abj9827. PMID 34788080. S2CID 244375227.
- ^ Brooks WC. "Lyme Disease". Veterinary Information Network. Archived from the original on 4 April 2015. Retrieved 10 February 2012.
- Berende A, ter Hofstede HJ, Vos FJ, van Middendorp H, Vogelaar ML, Tromp M, et al. (March 2016). "Randomized Trial of Longer-Term Therapy for Symptoms Attributed to Lyme Disease". The New England Journal of Medicine. 374 (13): 1209–1220. doi:10.1056/NEJMoa1505425. PMID 27028911.
- Stephenson M (4 October 2012). "OTC Drops: Telling the Tears Apart". Review of Ophtalmology. Jobson Medical Information LLC. Archived from the original on 17 April 2019. Retrieved 16 April 2019.
- ^ Arvikar SL, Steere AC (June 2015). "Diagnosis and treatment of Lyme arthritis". Infectious Disease Clinics of North America. 29 (2): 269–280. doi:10.1016/j.idc.2015.02.004. PMC 4443866. PMID 25999223.
- ^ Wormser GP, Ramanathan R, Nowakowski J, McKenna D, Holmgren D, Visintainer P, et al. (May 2003). "Duration of antibiotic therapy for early Lyme disease. A randomized, double-blind, placebo-controlled trial". Annals of Internal Medicine. 138 (9): 697–704. doi:10.7326/0003-4819-138-9-200305060-00005. PMID 12729423. S2CID 3083800.
- Stupica D, Lusa L, Ruzić-Sabljić E, Cerar T, Strle F (August 2012). "Treatment of erythema migrans with doxycycline for 10 days versus 15 days". Clinical Infectious Diseases. 55 (3): 343–350. doi:10.1093/cid/cis402. PMID 22523260.
- ^ Dattwyler RJ, Luft BJ, Kunkel MJ, Finkel MF, Wormser GP, Rush TJ, et al. (July 1997). "Ceftriaxone compared with doxycycline for the treatment of acute disseminated Lyme disease". The New England Journal of Medicine. 337 (5): 289–294. doi:10.1056/NEJM199707313370501. PMID 9233865.
- Vrethem M, Hellblom L, Widlund M, Ahl M, Danielsson O, Ernerudh J, et al. (October 2002). "Chronic symptoms are common in patients with neuroborreliosis -- a questionnaire follow-up study". Acta Neurologica Scandinavica. 106 (4): 205–208. doi:10.1034/j.1600-0404.2002.01358.x. PMID 12225315. S2CID 42290158.
- Berglund J, Stjernberg L, Ornstein K, Tykesson-Joelsson K, Walter H (2002). "5-y Follow-up study of patients with neuroborreliosis". Scandinavian Journal of Infectious Diseases. 34 (6): 421–425. doi:10.1080/00365540110080421. PMID 12160168. S2CID 28306612.
- ^ Clark JR, Carlson RD, Sasaki CT, Pachner AR, Steere AC (November 1985). "Facial paralysis in Lyme disease". The Laryngoscope. 95 (11): 1341–1345. doi:10.1288/00005537-198511000-00009. PMID 4058212. S2CID 85021.
- ^ Dotevall L, Hagberg L (March 1999). "Successful oral doxycycline treatment of Lyme disease-associated facial palsy and meningitis". Clinical Infectious Diseases. 28 (3): 569–574. doi:10.1086/515145. PMID 10194080.
- Kalish RA, Kaplan RF, Taylor E, Jones-Woodward L, Workman K, Steere AC (February 2001). "Evaluation of study patients with Lyme disease, 10-20-year follow-up". The Journal of Infectious Diseases. 183 (3): 453–460. doi:10.1086/318082. PMID 11133377.
- ^ Jowett N, Gaudin RA, Banks CA, Hadlock TA (June 2017). "Steroid use in Lyme disease-associated facial palsy is associated with worse long-term outcomes". The Laryngoscope. 127 (6): 1451–1458. doi:10.1002/lary.26273. PMID 27598389. S2CID 25596860.
- Nadelman RB, Hanincová K, Mukherjee P, Liveris D, Nowakowski J, McKenna D, et al. (November 2012). "Differentiation of reinfection from relapse in recurrent Lyme disease". The New England Journal of Medicine. 367 (20): 1883–1890. doi:10.1056/NEJMoa1114362. PMC 3526003. PMID 23150958.
- Bai NA, Richardson CS (September 2023). "Posttreatment Lyme disease syndrome and myalgic encephalomyelitis/chronic fatigue syndrome: A systematic review and comparison of pathogenesis". Chronic Diseases and Translational Medicine. 9 (3): 183–190. doi:10.1002/cdt3.74. PMC 10497844. PMID 37711861.
- ^ Marques A (September 2022). "Persistent Symptoms After Treatment of Lyme Disease". Infectious Disease Clinics of North America. 36 (3): 621–638. doi:10.1016/j.idc.2022.04.004. PMC 9494579. PMID 36116839.
- ^ "Post-Treatment Lyme Disease Syndrome". CDC. 3 November 2016. Archived from the original on 17 June 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- "Post-treatment Lyme Disease as a Model for Persistent Symptoms in Lyme Disease", Frontiers in Medicine (Lausanne), Alison W Rebman, John N Aucott, PMCID: PMC7052487, Feb. 25, 2020.
- Higgins R (August 2004). "Emerging or re-emerging bacterial zoonotic diseases: bartonellosis, leptospirosis, Lyme borreliosis, plague". Revue Scientifique et Technique. 23 (2): 569–581. doi:10.20506/rst.23.2.1503. PMID 15702720.
- Berger S (2014). Lyme disease: Global Status 2014 Edition. GIDEON Informatics Inc. p. 7. ISBN 978-1-4988-0343-4. Archived from the original on 8 September 2017.
- Gilbert L (January 2021). "The Impacts of Climate Change on Ticks and Tick-Borne Disease Risk". Annual Review of Entomology. 66 (1): 373–388. doi:10.1146/annurev-ento-052720-094533. PMID 33417823. S2CID 231300522.
- Bouattour A, Ghorbel A, Chabchoub A, Postic D (2004). "" [Lyme borreliosis situation in North Africa]. Archives de l'Institut Pasteur de Tunis (in French). 81 (1–4): 13–20. PMID 16929760.
- Dsouli N, Younsi-Kabachii H, Postic D, Nouira S, Gern L, Bouattour A (July 2006). "Reservoir role of lizard Psammodromus algirus in transmission cycle of Borrelia burgdorferi sensu lato (Spirochaetaceae) in Tunisia" (PDF). Journal of Medical Entomology. 43 (4): 737–742. doi:10.1603/0022-2585(2006)43[737:RROLPA]2.0.CO;2 (inactive 1 December 2024). PMID 16892633. S2CID 24774778. Archived (PDF) from the original on 19 July 2018. Retrieved 5 July 2019.
{{cite journal}}: CS1 maint: DOI inactive as of December 2024 (link) - Helmy N (August 2000). "Seasonal abundance of Ornithodoros (O.) savignyi and prevalence of infection with Borrelia spirochetes in Egypt". Journal of the Egyptian Society of Parasitology. 30 (2): 607–619. PMID 10946521.
- Fivaz BH, Petney TN (September 1989). "Lyme disease--a new disease in southern Africa?". Journal of the South African Veterinary Association. 60 (3): 155–158. PMID 2699499.
- Jowi JO, Gathua SN (May 2005). "Lyme disease: report of two cases". East African Medical Journal. 82 (5): 267–269. doi:10.4314/eamj.v82i5.9318. PMID 16119758.
- "Case of the Month". Federation of Infectious Diseases Societies of Southern Africa (FIDSSA). December 2015. Retrieved 2 November 2023.
- Li M, Masuzawa T, Takada N, Ishiguro F, Fujita H, Iwaki A, et al. (July 1998). "Lyme disease Borrelia species in northeastern China resemble those isolated from far eastern Russia and Japan". Applied and Environmental Microbiology. 64 (7): 2705–2709. Bibcode:1998ApEnM..64.2705L. doi:10.1128/AEM.64.7.2705-2709.1998. PMC 106449. PMID 9647853.
- Masuzawa T (December 2004). "Terrestrial distribution of the Lyme borreliosis agent Borrelia burgdorferi sensu lato in East Asia". Japanese Journal of Infectious Diseases. 57 (6): 229–235. doi:10.7883/yoken.JJID.2004.229. PMID 15623946. Archived from the original on 22 January 2013.
- Walder G, Lkhamsuren E, Shagdar A, Bataa J, Batmunkh T, Orth D, et al. (May 2006). "Serological evidence for tick-borne encephalitis, borreliosis, and human granulocytic anaplasmosis in Mongolia". International Journal of Medical Microbiology. 296 (Suppl 40): 69–75. doi:10.1016/j.ijmm.2006.01.031. PMID 16524782.
- Dehhaghi M, Kazemi Shariat Panahi H, Holmes EC, Hudson BJ, Schloeffel R, Guillemin GJ (2019). "Human Tick-Borne Diseases in Australia". Frontiers in Cellular and Infection Microbiology. 9: 3. doi:10.3389/fcimb.2019.00003. PMC 6360175. PMID 30746341.
- Gofton AW, Blasdell KR, Taylor C, Banks PB, Michie M, Roy-Dufresne E, et al. (September 2022). "Metatranscriptomic profiling reveals diverse tick-borne bacteria, protozoans and viruses in ticks and wildlife from Australia". Transboundary and Emerging Diseases. 69 (5): e2389 – e2407. doi:10.1111/tbed.14581. PMC 9790515. PMID 35502617.
- Barbosa AD, Long M, Lee W, Austen JM, Cunneen M, Ratchford A, et al. (November 2022). "The Troublesome Ticks Research Protocol: Developing a Comprehensive, Multidiscipline Research Plan for Investigating Human Tick-Associated Disease in Australia". Pathogens. 11 (11): 1290. doi:10.3390/pathogens11111290. PMC 9694322. PMID 36365042.
- Rizzoli A, Hauffe H, Carpi G, Vourc'h IG, Neteler M, Rosa R (July 2011). "Lyme borreliosis in Europe". Euro Surveillance. 16 (27). PMID 21794218. Archived from the original on 9 July 2011.
- Smith R, Takkinen J (June 2006). "Lyme borreliosis: Europe-wide coordinated surveillance and action needed?". Euro Surveillance. 11 (6): E060622.1. doi:10.2807/esw.11.25.02977-en. PMID 16819127.
- Lopes de Carvalho I, Núncio MS (2006). "Laboratory diagnosis of Lyme borreliosis at the Portuguese National Institute of Health (1990-2004)". Euro Surveillance. 11 (10): 257–260. PMID 17130658. Archived from the original on 17 June 2012.
- Vandekerckhove O, De Buck E, Van Wijngaerden E (June 2021). "Lyme disease in Western Europe: an emerging problem? A systematic review". Acta Clinica Belgica. 76 (3): 244–252. doi:10.1080/17843286.2019.1694293. PMID 31739768. S2CID 208170787.
- Vigfusson HB, Hardarson HS, Ludviksson BR, Gudlaugsson O (February 2019). "[Lyme disease in Iceland - Epidemiology from 2011 to 2015]". Laeknabladid. 105 (2): 63–70. doi:10.17992/lbl.2019.02.215. PMID 30713153. S2CID 73424569.
- ^ "Epidemiology of Lyme borreliosis in the UK". HPA. Archived from the original on 10 June 2013. Retrieved 15 December 2012.
- Muhlemann MF, Wright DJ (January 1987). "Emerging pattern of Lyme disease in the United Kingdom and Irish Republic". Lancet. 1 (8527): 260–262. doi:10.1016/S0140-6736(87)90074-2. PMID 2880076. S2CID 25295954.
- ^ "Lyme Disease". Parliamentary Debates (Hansard). 11 November 1991. Archived from the original on 15 June 2013.
- ^ "Tick Lyme disease off your holiday list" (Press release). Health Protection Agency. 14 April 2011. Archived from the original on 28 April 2011. Retrieved 29 March 2013.
- "Concern about rise in Lyme disease cases". Lyme Disease Action. 15 December 2011. Archived from the original on 19 June 2013. Retrieved 15 December 2012.
- Cassidy F (14 March 2011). "Tayside revealed as a Lyme disease hotspot as cases soar". Press and Journal. Archived from the original on 11 March 2016.
- "Lyme disease: A clear and present danger". RCN. 28 April 2009. Archived from the original on 29 March 2013. Retrieved 15 December 2012.
- "Guidance on Part 2 – Notifiable Diseases, Notifiable Organisms and Health Risk States". Scotland.gov.uk. 10 September 2012. Retrieved 15 December 2012.
- "Lyme Disease". Parliamentary Debates (Hansard). 3 February 1997. Archived from the original on 15 June 2013.
- Fox W (2010). "Tick-Borne Disease, Risk and Realit" (PDF). BADA-UK. Archived from the original (PDF) on 20 November 2012.
- "Lyme borreliosis epidemiology and surveillance: May 2013". HPA. Archived from the original on 25 November 2015. Retrieved 24 November 2015.
- "Zoonoses report UK 2009" (PDF). DEFRA. 24 January 2011. Archived (PDF) from the original on 3 November 2012.
- "Overview Tick Bite Prevention Week". Archived from the original on 10 April 2012.
- Haywood GA, O'Connell S, Gray HH (July 1993). "Lyme carditis: a United Kingdom perspective". British Heart Journal. 70 (1): 15–16. doi:10.1136/hrt.70.1.15. PMC 1025222. PMID 8037992.
- Guy EC, Bateman DE, Martyn CN, Heckels JE, Lawton NF (March 1989). "Lyme disease: prevalence and clinical importance of Borrelia burgdorferi specific IgG in forestry workers". Lancet. 1 (8636): 484–486. doi:10.1016/S0140-6736(89)91377-9. PMID 2563850. S2CID 39557628.
- Smith FD, Ballantyne R, Morgan ER, Wall R (March 2012). "Estimating Lyme disease risk using pet dogs as sentinels". Comparative Immunology, Microbiology and Infectious Diseases. 35 (2): 163–167. doi:10.1016/j.cimid.2011.12.009. PMID 22257866.
Lay summary: "Survey of pet dogs indicates Lyme disease risk much greater than previous estimates suggest" (Press release). University of Bristol. 25 January 2012. - Roberts M (24 January 2012). "Lyme disease risk from dogs 'higher than thought'". BBC News. Archived from the original on 31 January 2012.
- "The London climate change adaptation strategy - Draft report" (PDF). Greater London Authority. August 2008. Archived from the original (PDF) on 17 August 2012.
- Brownstein JS, Holford TR, Fish D (March 2005). "Effect of Climate Change on Lyme Disease Risk in North America". EcoHealth. 2 (1): 38–46. doi:10.1007/s10393-004-0139-x. PMC 2582486. PMID 19008966.
- ^ Killilea ME, Swei A, Lane RS, Briggs CJ, Ostfeld RS (June 2008). "Spatial dynamics of lyme disease: a review" (PDF). EcoHealth. 5 (2): 167–195. CiteSeerX 10.1.1.580.8928. doi:10.1007/s10393-008-0171-3. PMID 18787920. S2CID 13545850. Archived (PDF) from the original on 8 September 2015.
- BC Ministry of Agriculture. "Ticks and Humans in British Columbia". Agf.gov.bc.ca. Archived from the original on 3 January 2013. Retrieved 15 December 2012.
- "Lyme Disease Fact Sheet". Phac-aspc.gc.ca. 4 July 2012. Archived from the original on 27 December 2012. Retrieved 15 December 2012.
- Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H (June 2009). "The emergence of Lyme disease in Canada". CMAJ. 180 (12): 1221–1224. doi:10.1503/cmaj.080148. PMC 2691438. PMID 19506281.
- Leighton PA, Koffi JK, Pelcat Y, Lindsay LR, Ogden NH (2012). "Predicting the speed of tick invasion: An empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada". Journal of Applied Ecology. 49 (2): 457–64. Bibcode:2012JApEc..49..457L. doi:10.1111/j.1365-2664.2012.02112.x. S2CID 16921155.
- Gordillo-Pérez G, Torres J, Solórzano-Santos F, de Martino S, Lipsker D, Velázquez E, et al. (October 2007). "Borrelia burgdorferi infection and cutaneous Lyme disease, Mexico". Emerging Infectious Diseases. 13 (10): 1556–1558. doi:10.3201/eid1310.060630. PMC 2851501. PMID 18258006.
- CDC (4 January 2012). "Reported Lyme disease cases by state, 2000-2010". Centers for Disease Control and Prevention (CDC). Archived from the original on 4 May 2012. Retrieved 29 April 2012.
- Centers for Disease Control and Prevention (CDC) (June 2007). "Lyme disease--United States, 2003-2005". MMWR. Morbidity and Mortality Weekly Report. 56 (23): 573–576. PMID 17568368. Archived from the original on 19 November 2012.
- Bacon RM, Kugeler KJ, Mead PS (October 2008). "Surveillance for Lyme disease--United States, 1992-2006". Morbidity and Mortality Weekly Report. Surveillance Summaries. 57 (10): 1–9. PMID 18830214. Archived from the original on 10 November 2012.
- "Lyme Disease Data". Centers for Disease Control and Prevention (CDC). Archived from the original on 30 April 2012.
- ^ Robbins J (20 May 2003). "Montana Lab Tries to Identify Tick-Borne Disease". The New York Times. Archived from the original on 3 September 2017.
- "National Notifiable Diseases Surveillance System (NNDSS) - Lyme Disease". Centers for Disease Control and Prevention. 7 September 2021. Retrieved 11 January 2023.
- "Lyme Disease (Borrelia burgdorferi) 2022 Case Definition". Centers for Disease Control and Prevention. 12 August 2022. Retrieved 11 January 2023.
- "Lyme disease surveillance and available data". Centers for Disease Control and Prevention. 15 November 2022. Retrieved 11 January 2023.
- "STARI or Lyme?". Centers for Disease Control and Prevention. 19 November 2018. Archived from the original on 12 November 2019.
- ^ Labruna MB, Faccini-Martínez ÁA, Muñoz-Leal S, Szabó MP, Angerami RN (4 November 2024). "Lyme borreliosis in Brazil: a critical review on the Baggio–Yoshinari syndrome (Brazilian Lyme-like disease)". Clinical Microbiology Reviews: e0009724. doi:10.1128/cmr.00097-24. PMID 39494872.
- Mantovani E, Costa IP, Gauditano G, Bonoldi VL, Higuchi ML, Yoshinari NH (April 2007). "Description of Lyme disease-like syndrome in Brazil. Is it a new tick borne disease or Lyme disease variation?". Brazilian Journal of Medical and Biological Research = Revista Brasileira de Pesquisas Medicas e Biologicas. 40 (4): 443–456. doi:10.1590/S0100-879X2006005000082. PMID 17401487.
- Yoshinari NH, Oyafuso LK, Monteiro FG, de Barros PJ, da Cruz FC, Ferreira LG, et al. (1993). "" [Lyme disease. Report of a case observed in Brazil]. Revista do Hospital das Clinicas (in Portuguese). 48 (4): 170–174. PMID 8284588.
- Murray P (1006). The Widening Circle : A Lyme Disease Pioneer Tells Her Story. New York: St. Martin's Press. ISBN 978-0-312-14068-7.
- Wynne Parry (28 February 2012). "Iceman Mummy May Hold Earliest Evidence of Lyme Disease". Live Science.
- Hoen AG, Margos G, Bent SJ, Diuk-Wasser MA, Barbour A, Kurtenbach K, et al. (September 2009). "Phylogeography of Borrelia burgdorferi in the eastern United States reflects multiple independent Lyme disease emergence events". Proceedings of the National Academy of Sciences of the United States of America. 106 (35): 15013–15018. Bibcode:2009PNAS..10615013H. doi:10.1073/pnas.0903810106. JSTOR 40484546. PMC 2727481. PMID 19706476.
Lay summary: "Lyme Bacterium, Once Nearly Eradicated In U.S., Rebounded With Forests". YaleNews. 10 August 2009. - Josselyn J (1670). An Account of Two Voyages to New-England Made during the Years 1638, 1663. Archived from the original on 25 June 2013.page 92
- ^ Drymon MM (2008). Disguised as the devil: how Lyme disease created witches and changed history. Wythe Avenue Press. pp. 51–52. ISBN 978-0-615-20061-3.
- Summerton N (1995). "Lyme disease in the eighteenth century". BMJ. 311 (7018): 1478. doi:10.1136/bmj.311.7018.1478. S2CID 70661702.
- "US Voyage New World" (PDF). www.ulsterscotsagency.com. Retrieved 1 May 2024.
- Hall SS (November 2011). "Iceman Autopsy". National Geographic. Archived from the original on 19 October 2011. Retrieved 17 October 2011.
- ^ Marcus K (1910). "Verhandlungen der dermatologischen Gesellschaft zu Stockholm". Archiv für Dermatologie und Syphilis. 101 (2–3): 403–06. doi:10.1007/BF01832773. S2CID 46704791.
- Burckhardt JL (1911). "Zur Frage der Follikel- und Keimzentrenbildung in der Haut". Frankf. Z. Pathol. (in German). 6: 352–59.
- Edlow JA (2003). Bull's-eye: unraveling the medical mystery of Lyme disease. Yale University Press. ISBN 978-0-300-09867-9. page 191.
- Hellerström S (1930). "Erythema chronicum migrans Afzelii". Acta Derm. Venerol. (in German). 11: 315–21.
- Lennhoff C (1948). "Spirochaetes in aetiologically obscure diseases". Acta Dermato-Venereologica. 28 (3): 295–324. PMID 18891989.
- Hollström E (1951). "Successful treatment of erythema migrans Afzelius" (PDF). Acta Dermato-venereologica. 31 (2): 235–43. doi:10.2340/0001555531235243 (inactive 1 November 2024). PMID 14829185.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - Hollström E (1958). "Penicillin Treatment of erythema chronicum migrans afzelius" (PDF). Acta Dermato-Venereologica. 38 (5). doi:10.2340/0001555538285289 (inactive 1 November 2024).
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - Thyresson N (1949). "The penicillin treatment of acrodermatitis atrophicans chronica (Herxheimer)". Acta Dermato-Venereologica. 29 (6): 572–621. PMID 18140373.
- Bianchi GE (1950). "" [Penicillin therapy of lymphocytoma]. Dermatologica (in German). 100 (4–6): 270–273. doi:10.1159/000257185. PMID 15421023.
- Paschoud JM (1954). "" [Lymphocytoma after tick bite]. Dermatologica (in German). 108 (4–6): 435–437. PMID 13190934.
- Scrimenti RJ (July 1970). "Erythema chronicum migrans". Archives of Dermatology. 102 (1): 104–105. doi:10.1001/archderm.102.1.104. PMID 5497158.
- Borchers AT, Keen CL, Huntley AC, Gershwin ME (February 2015). "Lyme disease: a rigorous review of diagnostic criteria and treatment". Journal of Autoimmunity. 57: 82–115. doi:10.1016/j.jaut.2014.09.004. PMID 25451629.
- Weir W (19 September 2013). "Lyme Disease Pioneer Stephen Malawista Dies". Hartford Courant. Archived from the original on 14 October 2013. Retrieved 14 October 2013.
- Sternbach G, Dibble CL (1996). "Willy Burgdorfer: Lyme disease". The Journal of Emergency Medicine. 14 (5): 631–634. doi:10.1016/S0736-4679(96)00143-6. PMID 8933327.
- Bolognia JL, Jorizzo JL, Rapini RP (2007). Dermatology (2nd ed.). St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- Mast WE, Burrows WM (November 1976). "Erythema chronicum migrans and "lyme arthritis"". JAMA. 236 (21): 2392d–2392. doi:10.1001/jama.236.21.2392d. PMID 989847.
- Steere AC, Malawista SE, Snydman DR, Shope RE, Andiman WA, Ross MR, et al. (1977). "Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three Connecticut communities". Arthritis and Rheumatism. 20 (1): 7–17. doi:10.1002/art.1780200102. PMID 836338. S2CID 43397837.
- "Factsheet about Borreliosis". European Centre for Disease Prevention and Control. 17 June 2017. Archived from the original on 27 September 2019. Retrieved 30 January 2020.
- "WHO | Lyme Borreliosis (Lyme disease)". WHO. Archived from the original on 29 November 2019. Retrieved 30 January 2020.
- Steere AC, Hutchinson GJ, Rahn DW, Sigal LH, Craft JE, DeSanna ET, et al. (July 1983). "Treatment of the early manifestations of Lyme disease". Annals of Internal Medicine. 99 (1): 22–26. doi:10.7326/0003-4819-99-1-22. PMID 6407378.
- Burgdorfer W (1984). "Discovery of the Lyme disease spirochete and its relation to tick vectors". The Yale Journal of Biology and Medicine. 57 (4): 515–520. PMC 2590008. PMID 6516454.
- Burgdorfer W, Barbour AG, Hayes SF, Benach JL, Grunwaldt E, Davis JP (June 1982). "Lyme disease-a tick-borne spirochetosis?". Science (Submitted manuscript). 216 (4552): 1317–1319. Bibcode:1982Sci...216.1317B. doi:10.1126/science.7043737. PMID 7043737. Archived from the original on 30 January 2020. Retrieved 4 September 2018.
- Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ (1988). "New chemotherapeutic approaches in the treatment of Lyme borreliosis". Annals of the New York Academy of Sciences. 539 (1): 352–361. Bibcode:1988NYASA.539..352L. doi:10.1111/j.1749-6632.1988.tb31869.x. PMID 3056203. S2CID 25939418.
- Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ (December 1990). "Amoxycillin plus probenecid versus doxycycline for treatment of erythema migrans borreliosis". Lancet. 336 (8728): 1404–1406. doi:10.1016/0140-6736(90)93103-V. PMID 1978873. S2CID 7314488.
- Ribeiro JM, Mather TN, Piesman J, Spielman A (March 1987). "Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae)". Journal of Medical Entomology. 24 (2): 201–205. doi:10.1093/jmedent/24.2.201. PMID 3585913.
- ^ LoGiudice K, Ostfeld RS, Schmidt KA, Keesing F (January 2003). "The ecology of infectious disease: effects of host diversity and community composition on Lyme disease risk". Proceedings of the National Academy of Sciences of the United States of America. 100 (2): 567–571. Bibcode:2003PNAS..100..567L. doi:10.1073/pnas.0233733100. PMC 141036. PMID 12525705.
- Patz JA, Daszak P, Tabor GM, Aguirre AA, Pearl M, Epstein J, et al. (July 2004). "Unhealthy landscapes: Policy recommendations on land use change and infectious disease emergence". Environmental Health Perspectives. 112 (10): 1092–1098. Bibcode:2004EnvHP.112.1092P. doi:10.1289/ehp.6877. PMC 1247383. PMID 15238283.
- Khasnis AA, Nettleman MD (2005). "Global warming and infectious disease". Archives of Medical Research. 36 (6): 689–696. doi:10.1016/j.arcmed.2005.03.041. PMID 16216650.
- Ruyts SC, Landuyt D, Ampoorter E, Heylen D, Ehrmann S, Coipan EC, et al. (July 2018). "Low probability of a dilution effect for Lyme borreliosis in Belgian forests". Ticks and Tick-Borne Diseases. 9 (5). Ticks and Tick-Borne Diseases.: 1143–1152. doi:10.1016/j.ttbdis.2018.04.016. PMID 29716838. S2CID 13746169.
- Feder HM, Johnson BJ, O'Connell S, Shapiro ED, Steere AC, Wormser GP, et al. (October 2007). "A critical appraisal of "chronic Lyme disease"". The New England Journal of Medicine. 357 (14). Ad Hoc International Lyme Disease Group: Agger WA, Artsob H, Auwaerter P, Dumler JS, Bakken JS, Bockenstedt LK, Green J, Dattwyler RJ, Munoz J, Nadelman RB, Schwartz I, Draper T, McSweegan E, Halperin JJ, Klempner MS, Krause PJ, Mead P, Morshed M, Porwancher R, Radolf JD, Smith RP, Sood S, Weinstein A, Wong SJ, Zemel L: 1422–1430. doi:10.1056/NEJMra072023. PMID 17914043. S2CID 35285261.
- ""Chronic Lyme Disease" Fact Sheet". National Institute of Allergy and Infectious Diseases. 17 April 2009. Archived from the original on 15 December 2012.
- Marques A (June 2008). "Chronic Lyme disease: a review". Infectious Disease Clinics of North America. 22 (2): 341–60, vii–viii. doi:10.1016/j.idc.2007.12.011. PMC 2430045. PMID 18452806.
- MacBeth B (8 April 2019). "A Review of Under Our Skin, A Cult Classic". Science-Based Medicine. Retrieved 10 September 2021.
- ^ Little SE, Heise SR, Blagburn BL, Callister SM, Mead PS (April 2010). "Lyme borreliosis in dogs and humans in the USA". Trends in Parasitology. 26 (4): 213–218. doi:10.1016/j.pt.2010.01.006. PMID 20207198.
- ^ Krupka I, Straubinger RK (November 2010). "Lyme borreliosis in dogs and cats: background, diagnosis, treatment and prevention of infections with Borrelia burgdorferi sensu stricto". The Veterinary Clinics of North America. Small Animal Practice. 40 (6): 1103–1119. doi:10.1016/j.cvsm.2010.07.011. PMID 20933139.
- Hahn J. "Ticks and Their Control". Regents of the University of Minnesota. Archived from the original on 25 February 2012. Retrieved 19 February 2012.
- "Glomerular Disease". The Merck Veterinary Manual. Archived from the original on 26 June 2017. Retrieved 19 May 2017.
- Staubinger R (31 May 2000). "Lyme Disease". Sirius Dog. Archived from the original on 23 June 2012. Retrieved 10 February 2012.
- Fatal cases of Lyme disease reported in the medical literature include:
- Kirsch M, Ruben FL, Steere AC, Duray PH, Norden CW, Winkelstein A (May 1988). "Fatal adult respiratory distress syndrome in a patient with Lyme disease". JAMA. 259 (18): 2737–2739. doi:10.1001/jama.1988.03720180063034. PMID 3357244.
- Oksi J, Kalimo H, Marttila RJ, Marjamäki M, Sonninen P, Nikoskelainen J, et al. (December 1996). "Inflammatory brain changes in Lyme borreliosis. A report on three patients and review of literature". Brain. 119 (Pt 6): 2143–2154. doi:10.1093/brain/119.6.2143. PMID 9010017.
- Waniek C, Prohovnik I, Kaufman MA, Dwork AJ (1995). "Rapidly progressive frontal-type dementia associated with Lyme disease". The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (3): 345–347. doi:10.1176/jnp.7.3.345. PMID 7580195.
- Cary NR, Fox B, Wright DJ, Cutler SJ, Shapiro LM, Grace AA (February 1990). "Fatal Lyme carditis and endodermal heterotopia of the atrioventricular node". Postgraduate Medical Journal. 66 (772): 134–136. doi:10.1136/pgmj.66.772.134. PMC 2429516. PMID 2349186.
- ^ Straubinger R (2018). "Lyme Disease (Lyme Borreliosis) in Cats - Cat Owners". Merck Veterinary Manual. Archived from the original on 20 April 2021. Retrieved 26 October 2023.
- ^ Tørnqvist-Johnsen C, Dickson SA, Rolph K, Palermo V, Hodgkiss-Geere H, Gilmore P, et al. (2020). "First report of Lyme borreliosis leading to cardiac bradydysrhythmia in two cats". JFMS Open Reports. 6 (1): 2055116919898292. doi:10.1177/2055116919898292. PMC 6950542. PMID 31949917.
- ^ Parker JL, White KK (1992). "Lyme borreliosis in cattle and horses: a review of the literature". The Cornell Veterinarian. 82 (3): 253–274. ISSN 0010-8901. PMID 1643876.
- ^ Johnstone LK, Engiles JB, Aceto H, Buechner-Maxwell V, Divers T, Gardner R, et al. (2016). "Retrospective Evaluation of Horses Diagnosed with Neuroborreliosis on Postmortem Examination: 16 Cases (2004-2015)". Journal of Veterinary Internal Medicine. 30 (4): 1305–1312. doi:10.1111/jvim.14369. ISSN 1939-1676. PMC 5094551. PMID 27327172.
- Van der Kolk JH (2016). "Lyme borreliosis in the horse: A mini-review". Journal of Experimental Biology and Agricultural Sciences. 4 (Spl-4-EHIDZ): S196 – S202. doi:10.18006/2016.4(Spl-4-EHIDZ).S196.S202. S2CID 78836519.
- ^ Burgess EC, Gillette D, Pickett J (1986). "Arthritis and panuveitis as manifestations of Borrelia burgdorferi infection in a Wisconsin pony". Journal of the American Veterinary Medical Association. 189 (10): 1340–1342. ISSN 0003-1488. PMID 3793582.
- ^ Browning A, Carter SD, Barnes A, May C, Bennett D (1993). "Lameness associated with Borrelia burgdorferi infection in the horse". The Veterinary Record. 132 (24): 610–611. doi:10.1136/vr.132.24.610 (inactive 3 December 2024). ISSN 0042-4900. PMID 8337810.
{{cite journal}}: CS1 maint: DOI inactive as of December 2024 (link) - Gall Y, Pfister K (2006). "Survey on the subject of equine Lyme borreliosis". International Journal of Medical Microbiology. 296 (1): 274–279. doi:10.1016/j.ijmm.2006.01.004. ISSN 1438-4221. PMID 16524771.
- Burgess EC, Mattison M (1987). "Encephalitis associated with Borrelia burgdorferi infection in a horse". Journal of the American Veterinary Medical Association. 191 (11): 1457–1458. ISSN 0003-1488. PMID 3692996.
- ^ Hahn CN, Mayhew IG, Whitwell KE, Smith KC, Carey D, Carter SD, et al. (1996). "A possible case of Lyme borreliosis in a horse in the UK". Equine Veterinary Journal. 28 (1): 84–88. doi:10.1111/j.2042-3306.1996.tb01595.x. ISSN 0425-1644. PMID 8565961.
- James FM, Engiles JB, Beech J (2010). "Meningitis, cranial neuritis, and radiculoneuritis associated with Borrelia burgdorferi infection in a horse". Journal of the American Veterinary Medical Association. 237 (10): 1180–1185. doi:10.2460/javma.237.10.1180. ISSN 0003-1488. PMID 21073390.
- ^ Divers TJ, Gardner RB, Madigan JE, Witonsky SG, Bertone JJ, Swinebroad EL, et al. (2018). "Borrelia burgdorferi Infection and Lyme Disease in North American Horses: A Consensus Statement". Journal of Veterinary Internal Medicine. 32 (2): 617–632. doi:10.1111/jvim.15042. ISSN 1939-1676. PMC 5866975. PMID 29469222.
- Cohen ND, Heck FC, Heim B, Flad DM, Bosler EM, Cohen D (1992). "Seroprevalence of antibodies to Borrelia burgdorferi in a population of horses in central Texas". Journal of the American Veterinary Medical Association. 201 (7): 1030–1034. doi:10.2460/javma.1992.201.07.1030. ISSN 0003-1488. PMID 1429127.
- Metcalf KB, Lilley CS, Revenaugh MS, Glaser AL, Metcalf ES (2008). "The prevalence of antibodies against Borrelia burgdorferi found in horses residing in the northwestern United States". Journal of Equine Veterinary Science. 28 (10): 587–589. doi:10.1016/j.jevs.2008.08.010.
- Gehlen H, Inerle K, Bartel A, Stöckle SD, Ulrich S, Briese B, et al. (June 2023). "Seroprevalence of Borrelia burgdorferi sensu lato and Anaplasma phagocytophilum Infections in German Horses". Animals. 13 (12): 1984. doi:10.3390/ani13121984. PMC 10295046. PMID 37370494.
- Bryant JE, Brown MP, Gronwall RR, Merritt KA (2000). "Study of intragastric administration of doxycycline: pharmacokinetics including body fluid, endometrial and minimum inhibitory concentrations". Equine Veterinary Journal. 32 (3): 233–238. doi:10.2746/042516400776563608. ISSN 0425-1644. PMID 10836479.
- ^ Chang YF, Ku YW, Chang CF, Chang CD, McDonough SP, Divers T, et al. (2005). "Antibiotic treatment of experimentally Borrelia burgdorferi-infected ponies". Veterinary Microbiology. 107 (3): 285–294. doi:10.1016/j.vetmic.2005.02.006. ISSN 0378-1135. PMID 15863289.
- Schnabel LV, Papich MG, Divers TJ, Altier C, Aprea MS, McCarrel TM, et al. (2012). "Pharmacokinetics and distribution of minocycline in mature horses after oral administration of multiple doses and comparison with minimum inhibitory concentrations". Equine Veterinary Journal. 44 (4): 453–458. doi:10.1111/j.2042-3306.2011.00459.x. ISSN 2042-3306. PMID 21950341.
- Sears KP, Divers TJ, Neff RT, Miller WH, McDonough SP (2012). "A case of Borrelia-associated cutaneous pseudolymphoma in a horse". Veterinary Dermatology. 23 (2): 153–156. doi:10.1111/j.1365-3164.2011.01013.x. ISSN 1365-3164. PMID 22029872.
- Divers TJ, Grice AL, Mohammed HO, Glaser AL, Wagner B (2012). "Changes in Borrelia burgdorferi ELISA antibody over time in both antibiotic treated and untreated horses". Acta Veterinaria Hungarica. 60 (4): 421–429. doi:10.1556/avet.2012.036.
- ^ Guarino C, Asbie S, Rohde J, Glaser A, Wagner B (2017). "Vaccination of horses with Lyme vaccines for dogs induces short-lasting antibody responses". Vaccine. 35 (33): 4140–4147. doi:10.1016/j.vaccine.2017.06.052. ISSN 0264-410X.
- Chang YF, Novosol V, McDonough SP, Chang CF, Jacobson RH, Divers T, et al. (1999). "Vaccination against Lyme Disease with recombinant Borrelia burgdorferi outer-surface protein A (rOspA) in horses". Vaccine. 18 (5): 540–548. doi:10.1016/S0264-410X(99)00187-5. ISSN 0264-410X. PMID 10519945.
- Knödlseder JM, Fell SF, Straubinger RK (2019). "A study with a commercial vaccine against Lyme borreliosis in horses using two different vaccination schedules: Characterization of the humoral immune response". Vaccine. 37 (49): 7207–7212. doi:10.1016/j.vaccine.2019.09.087. PMID 31635975.
![]() This article incorporates public domain material from Post-Treatment Lyme Disease Syndrome. Centers for Disease Control and Prevention.
This article incorporates public domain material from Post-Treatment Lyme Disease Syndrome. Centers for Disease Control and Prevention.
Further reading
- Ostfeld R (2012). Lyme Disease: The Ecology of a Complex System. New York: Oxford University Press. ISBN 978-0-19-992847-7.
- Barbour AG (2015). Lyme disease: why it's spreading, how it makes you sick, and what to do about it. Baltimore: Johns Hopkins University Press. ISBN 978-1-4214-1721-9.
- Halperin JJ, ed. (2018). Lyme disease: an evidence-based approach (2nd ed.). Wallingford, Oxfordshire, UK: CABI. ISBN 978-1-78639-207-7.
- Radolf JD, Samuels DS, eds. (2021). Lyme disease and relapsing fever spirochetes: genomics, molecular biology, host interactions and disease pathogenesis. Poole, UK: Caister. ISBN 978-1-913652-61-6.
- Oaklander M (17 June 2021). "We Used to Have a Lyme Disease Vaccine. Are We Ready to Bring One Back?". Time.
External links
- CDC - Lyme Disease
- Association for Public Health Laboratories guide – Suggested Reporting Language, Interpretation and Guidance Regarding Lyme Disease Serologic Test Results
- NIH – Lyme Disease
- NICE Guidelines – Lyme Disease
| Classification | D |
|---|---|
| External resources |
|
| Tick-borne diseases and infestations | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diseases |
| ||||||||||||||
| Infestations | |||||||||||||||
| Species and bites |
| ||||||||||||||
| Bacterial diseases due to gram negative non-proteobacteria (BV4) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Spirochaetota |
| ||||||||||
| Chlamydiota |
| ||||||||||
| Bacteroidota | |||||||||||
| Fusobacteriota | |||||||||||
| Artificial induction of immunity / Immunization: Vaccines, Vaccination, Infection, Inoculation (J07) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Development | |||||||||||
| Classes | |||||||||||
| Administration | |||||||||||
| Vaccines |
| ||||||||||
| Inventors/ researchers | |||||||||||
| Controversy | |||||||||||
| Related | |||||||||||
| |||||||||||