| Revision as of 12:49, 20 May 2009 editRich Farmbrough (talk | contribs)Edit filter managers, Autopatrolled, Extended confirmed users, File movers, Pending changes reviewers, Rollbackers, Template editors1,726,089 editsm clean up- spelling "et al." and gen fixes using AWB← Previous edit | Revision as of 06:07, 19 June 2009 edit undo98.212.223.174 (talk) Added mention of use of AFM to determine a-beta aggregation state. I love you, John Darrow.Next edit → | ||
| Line 57: | Line 57: | ||
| Imaging compounds, notable Pittsburgh Compound-B, (BTA-1, a ]), can selectively bind to amyloid beta in vitro and in vivo. This technique, combined with ] imaging, has been used to image areas of plaque deposits in Alzheimer's patients. | Imaging compounds, notable Pittsburgh Compound-B, (BTA-1, a ]), can selectively bind to amyloid beta in vitro and in vivo. This technique, combined with ] imaging, has been used to image areas of plaque deposits in Alzheimer's patients. | ||
| ], which can visualize nanoscale molecular surfaces, can be used to determine the aggregation state of Amyloid beta in vitro.<ref name="pmid12499373">{{cite journal |author=Stine WB, Dahlgren KN, Krafft GA, LaDu MJ |title=In vitro characterization of conditions for amyloid-beta peptide oligomerization and fibrillogenesis |journal=J. Biol. Chem. |volume=278 |issue=13 |pages=11612-22 |year=2003 |month=March |pmid=12499373 |doi=10.1074/jbc.M210207200}}</ref> | |||
| ==External links== | ==External links== | ||
| * {{OMIM|104300}} | * {{OMIM|104300}} | ||
Revision as of 06:07, 19 June 2009
| amyloid beta (A4) precursor protein (peptidase nexin-II, Alzheimer disease) | |||||||
|---|---|---|---|---|---|---|---|
 Processing of the amyloid precursor protein Processing of the amyloid precursor protein | |||||||
| Identifiers | |||||||
| Symbol | APP | ||||||
| Alt. symbols | AD1 | ||||||
| NCBI gene | 351 | ||||||
| HGNC | 620 | ||||||
| OMIM | 104760 | ||||||
| RefSeq | NM_000484 | ||||||
| UniProt | P05067 | ||||||
| Other data | |||||||
| Locus | Chr. 21 q21.2 | ||||||
| |||||||
Amyloid beta (Aβ or Abeta) is a peptide of 39–43 amino acids that appear to be the main constituent of amyloid plaques in the brains of Alzheimer's disease patients. Similar plaques appear in some variants of Lewy body dementia and in inclusion body myositis, a muscle disease. Aβ also forms aggregates coating cerebral blood vessels in cerebral amyloid angiopathy. These plaques are composed of a tangle of regularly ordered fibrillar aggregates called amyloid fibers, a protein fold shared by other peptides such as prions associated with protein misfolding diseases. Research on laboratory rats suggest that the two-molecule, soluble form of the peptide is a causative agent in the development of Alzheimer's and that the two-molecule form is the smallest synaptotoxic species of soluble amyloid beta oligomer
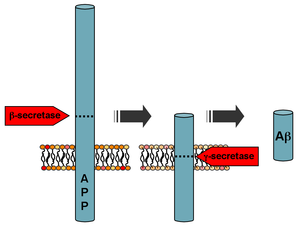
Formation
Aβ is formed after sequential cleavage of the amyloid precursor protein, a transmembrane glycoprotein of undetermined function. APP can be processed by α-, β- and γ-secretases; Aβ protein is generated by successive action of the β and γ secretases. The γ secretase, which produces the C-terminal end of the Aβ peptide, cleaves within the transmembrane region of APP and can generate a number of isoforms of 39-43 amino acid residues in length. The most common isoforms are Aβ40 and Aβ42; the shorter form is typically produced by cleavage that occurs in the endoplasmic reticulum, while the longer form is produced by cleavage in the trans-Golgi network. The Aβ40 form is the more common of the two, but Aβ42 is the more fibrillogenic and is thus associated with disease states. Mutations in APP associated with early-onset Alzheimer's have been noted to increase the relative production of Aβ42, and thus one suggested avenue of Alzheimer's therapy involves modulating the activity of β and γ secretases to produce mainly Aβ40.
Genetics
Autosomal-dominant mutations in APP cause hereditary early-onset Alzheimer's disease, likely as a result of altered proteolytic processing. Increases in either total Aβ levels or the relative concentration of both Aβ40 and Aβ42 (where the former is more concentrated in cerebrovascular plaques and the latter in neuritic plaques) have been implicated in the pathogenesis of both familial and sporadic Alzheimer's disease. Due to its more hydrophobic nature, the Aβ42 is the most amyloidogenic form of the peptide. However the central sequence KLVFFAE is known to form amyloid on its own, and probably forms the core of the fibril.
The "amyloid hypothesis", that the plaques are responsible for the pathology of Alzheimer's disease, is accepted by the majority of researchers but is by no means conclusively established. Intra-cellular deposits of tau protein are also seen in the disease, and may also be implicated. The oligomers that form on the amyloid pathway, rather than the mature fibrils, may be the cytotoxic species.
Intervention strategies
Researchers in Alzheimer's disease have identified five strategies as possible interventions against amyloid:
- β-Secretase inhibitors. These work to block the first cleavage of APP outside of the cell.
- γ-Secretase inhibitors (e. g. Semagacestat). These work to block the second cleavage of APP in the cell membrane and would then stop the subsequent formation of Aβ and its toxic fragments.
- Selective Aβ42 lowering agents (e. g. Tarenflurbil). These modulate γ-secretase to reduce Aβ42 production in favor of other (shorter) Aβ versions.
- Immunotherapies. These stimulate the host immune system to recognize and attack Aβ or provide antibodies that either prevent plaque deposition or enhance clearance of plaques.
- Anti-aggregation agents.These prevent Aβ fragments from aggregating or clear aggregates once they are formed.
There is some indication that supplementation of the hormone melatonin may be effective against amyloid.
Measuring amyloid beta
There are many different ways to measure Amyloid beta. One highly sensitive method is ELISA which is an immuno-sandwich assay which utilizes a pair of antibodies that recognize Amyloid beta.
Imaging compounds, notable Pittsburgh Compound-B, (BTA-1, a thioflavin), can selectively bind to amyloid beta in vitro and in vivo. This technique, combined with PET imaging, has been used to image areas of plaque deposits in Alzheimer's patients.
Atomic force microscopy, which can visualize nanoscale molecular surfaces, can be used to determine the aggregation state of Amyloid beta in vitro.
External links
References
- Scmid, Randolf (2008). "New clue to Alzheimer's found" ( – ). Yahoo News.
{{cite journal}}: External link in|format=|month=ignored (help) - Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, Brett FM, Farrell MA, Rowan MJ, Lemere CA, Regan CM, Walsh DM, Sabatini BL, Selkoe DJ (2008). "Amyloid-protein dimers isolated directly from Alzheimer's brains impair synaptic plasticity and memory". Nature Medicine. 14 (June 22, 2008 online): 837. doi:10.1038/nm1782. PMID 18568035.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hartmann T, Bieger SC, Brühl B; et al. (1997). "Distinct sites of intracellular production for Alzheimer's disease Aβ40/42 amyloid peptides". Nat. Med. 3 (9): 1016–20. doi:10.1038/nm0997-1016. PMID 9288729.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Yin YI, Bassit B, Zhu L, Yang X, Wang C, Li YM (2007). "γ-Secretase Substrate Concentration Modulates the Aβ42/Aβ40 Ratio: Implications for Alzheimer's disease". J. Biol. Chem. 282 (32): 23639–44. doi:10.1074/jbc.M704601200. PMID 17556361.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Lue LF, Kuo YM, Roher AE; et al. (1999). "Soluble amyloid beta peptide concentration as a predictor of synaptic change in Alzheimer's disease". Am. J. Pathol. 155 (3): 853–62. PMC 1866907. PMID 10487842.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Kayed R, Head E, Thompson JL; et al. (2003). "Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis". Science (journal). 300 (5618): 486–9. doi:10.1126/science.1079469. PMID 12702875.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Citron M (2004). "Strategies for disease modification in Alzheimer's disease". Nat. Rev. Neurosci. 5 (9): 677–85. doi:10.1038/nrn1495. PMID 15322526.
-
Lashuel HA, Hartley DM, Balakhaneh D, Aggarwal A, Teichberg S, Callaway DJE (2002). "New class of inhibitors of amyloid-beta fibril formation. Implications for the mechanism of pathogenesis in [[Alzheimer's disease]]". J Biol Chem. 277 (45): 42881–42890. doi:10.1074/jbc.M206593200. PMID 12167652.
{{cite journal}}: URL–wikilink conflict (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Michael H. Parker, Robert Chen, Kelly A. Conway, Daniel H. S. Lee; Chi Luoi, Robert E. Boyd, Samuel O. Nortey, Tina M. Ross, Malcolm K. Scott, Allen B. Reitz (2002). "Synthesis of (+)-5,8-Dihydroxy-3R-methyl-2R-(dipropylamino)-1,2,3,4-tetrahydro-naphthalene: An Inhibitor of β-Amyloid1-42 Aggregation". Bioorg. Med. Chem. 10 (11): 3565–3569. doi:10.1016/S0968-0896(02)00251-1. PMID 12213471.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lahiri DK, Chen DM, Lahiri P, Bondy S, Greig NH (2005). "Amyloid, cholinesterase, melatonin, and metals and their roles in aging and neurodegenerative diseases". Ann. N. Y. Acad. Sci. 1056: 430–49. doi:10.1196/annals.1352.008. PMID 16387707.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Wang XC, Zhang YC, Chatterjie N, Grundke-Iqbal I, Iqbal K, Wang JZ (2008). "Effect of melatonin and Melatonylvalpromide on beta-amyloid and neurofilaments in N2a cells". Neurochem. Res. 33 (6): 1138–44. doi:10.1007/s11064-007-9563-y. PMID 18231852.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Stine WB, Dahlgren KN, Krafft GA, LaDu MJ (2003). "In vitro characterization of conditions for amyloid-beta peptide oligomerization and fibrillogenesis". J. Biol. Chem. 278 (13): 11612–22. doi:10.1074/jbc.M210207200. PMID 12499373.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link)
| Amyloidosis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Common amyloid forming proteins | |||||||||||
| Systemic amyloidosis | |||||||||||
| Organ-limited amyloidosis |
| ||||||||||