| Revision as of 11:13, 23 June 2015 editRichard Keatinge (talk | contribs)Extended confirmed users, Pending changes reviewers, Rollbackers16,937 edits removed extensive unreferenced comments, clarity in remainder← Previous edit | Revision as of 06:59, 24 June 2015 edit undoYobot (talk | contribs)Bots4,733,870 editsm WP:CHECKWIKI error fixes using AWB (11267)Next edit → | ||
| Line 1: | Line 1: | ||
| {{Refimprove|date=February 2009}} | {{Refimprove|date=February 2009}} | ||
| {{Infobox |
{{Infobox disease | | ||
| Name = Keratoacanthoma | | Name = Keratoacanthoma | | ||
| Image = Keratoacanthoma_2.jpg | | Image = Keratoacanthoma_2.jpg | | ||
| Line 18: | Line 18: | ||
| The defining characteristic of KA is that it is dome-shaped, symmetrical, surrounded by a smooth wall of inflamed skin, and capped with keratin scales and debris. It grows rapidly, reaching a large size within days or weeks, and if untreated for months will almost always starve itself of nourishment, necrose (die), slough, and heal with scarring. While some pathologists classify KA as a distinct entity and not a malignancy, some clinical and histological keratoacanthomas do progress to invasive and aggressive squamous cell cancers, therefore prompt and definitive treatment may be recommended.<ref>Ko CJ, Keratoacanthoma: facts and controversies. Clin Dermatol. 2010; 28(3):254–61 (ISSN: 1879-1131)</ref><ref>http://www.emedicine.com/derm/topic206.htm</ref> | The defining characteristic of KA is that it is dome-shaped, symmetrical, surrounded by a smooth wall of inflamed skin, and capped with keratin scales and debris. It grows rapidly, reaching a large size within days or weeks, and if untreated for months will almost always starve itself of nourishment, necrose (die), slough, and heal with scarring. While some pathologists classify KA as a distinct entity and not a malignancy, some clinical and histological keratoacanthomas do progress to invasive and aggressive squamous cell cancers, therefore prompt and definitive treatment may be recommended.<ref>Ko CJ, Keratoacanthoma: facts and controversies. Clin Dermatol. 2010; 28(3):254–61 (ISSN: 1879-1131)</ref><ref>http://www.emedicine.com/derm/topic206.htm</ref> | ||
| Under the microscope, keratoacanthoma very closely resembles squamous cell carcinoma. In order to differeniate between the two, almost the entire structure needs to be removed and examined. |
Under the microscope, keratoacanthoma very closely resembles squamous cell carcinoma. In order to differeniate between the two, almost the entire structure needs to be removed and examined. | ||
| == Classification == | == Classification == | ||
| Line 34: | Line 34: | ||
| == Diagnosis == | == Diagnosis == | ||
| Keratoacanthoma presents as a fleshy, elevated and nodular lesion with an irregular crater shape and a characteristic central hyperkeratotic core. Usually the patient will notice a rapidly growing dome-shaped tumor on sun-exposed skin.{{ |
Keratoacanthoma presents as a fleshy, elevated and nodular lesion with an irregular crater shape and a characteristic central hyperkeratotic core. Usually the patient will notice a rapidly growing dome-shaped tumor on sun-exposed skin.{{citation needed|date=October 2013}} | ||
| ] | ] | ||
| If the entire lesion is removed, the pathologist will probably be able to differentiate between keratoacanthoma and squamous cell carcinoma. If only part of the lesion is removed, confident diagnosis may be impossible. |
If the entire lesion is removed, the pathologist will probably be able to differentiate between keratoacanthoma and squamous cell carcinoma. If only part of the lesion is removed, confident diagnosis may be impossible. | ||
| == Treatment == | == Treatment == | ||
| Excision of the entire lesion, with adequate margin, will remove the lesion, allow full tissue diagnosis, and leave a planned surgical wound which can usually be repaired with a good cosmetic result. However, removing the entire lesion (especially on the face) may present difficult problems of plastic reconstruction. (On the nose and face, ] may allow for good margin control with minimal tissue removal, but many insurance companies require the correct diagnosis of a malignancy |
Excision of the entire lesion, with adequate margin, will remove the lesion, allow full tissue diagnosis, and leave a planned surgical wound which can usually be repaired with a good cosmetic result. However, removing the entire lesion (especially on the face) may present difficult problems of plastic reconstruction. (On the nose and face, ] may allow for good margin control with minimal tissue removal, but many insurance companies require the correct diagnosis of a malignancy ''before'' they are prepared to pay the extra costs of Mohs surgery.) Especially in more cosmetically-sensitive areas, and where the clinical diagnosis is reasonably certain, alternatives to surgery may include no treatment (awaiting spontaneous resolution).<ref>Keratoacanthoma. Désirée Ratner. 2004. http://www.medscape.com/viewarticle/467069 accessed 23 June 2015</ref> | ||
| On the trunk, arms, and legs, ] and ] often suffice to control keratoacanthomas until they regress. Other modalities of treatment include ] and ]; intralesional injection of ] or of ] have also been used.<refKeratoacanthoma. Désirée Ratner. 2004. http://www.medscape.com/viewarticle/467069 accessed 23 June 2015</ref> |
On the trunk, arms, and legs, ] and ] often suffice to control keratoacanthomas until they regress. Other modalities of treatment include ] and ]; intralesional injection of ] or of ] have also been used.<refKeratoacanthoma. Désirée Ratner. 2004. http://www.medscape.com/viewarticle/467069 accessed 23 June 2015</ref> | ||
| Recurrence after electrodesiccation and curettage is common, and usually can be identified and treated promptly with either further curettage or surgical excision. |
Recurrence after electrodesiccation and curettage is common, and usually can be identified and treated promptly with either further curettage or surgical excision. | ||
| == See also == | == See also == | ||
Revision as of 06:59, 24 June 2015
| This article needs additional citations for verification. Please help improve this article by adding citations to reliable sources. Unsourced material may be challenged and removed. Find sources: "Keratoacanthoma" – news · newspapers · books · scholar · JSTOR (February 2009) (Learn how and when to remove this message) |
| Keratoacanthoma | |
|---|---|
| Specialty | Oncology, dermatology |
Keratoacanthoma (KA) is a common low-grade (unlikely to metastasize or invade) skin tumour that is believed to originate from the neck of the hair follicle. Many pathologists consider it to be a form of squamous cell carcinoma (SCC). Pathologists may label KA as "well-differentiated squamous cell carcinoma, keratoacanthoma variant", because about 6% of keratoacanthomas manifest themselves as squamous cell carcinoma when left untreated. KA is commonly found on sun-exposed skin, and often is seen on the face, forearms and hands.
The defining characteristic of KA is that it is dome-shaped, symmetrical, surrounded by a smooth wall of inflamed skin, and capped with keratin scales and debris. It grows rapidly, reaching a large size within days or weeks, and if untreated for months will almost always starve itself of nourishment, necrose (die), slough, and heal with scarring. While some pathologists classify KA as a distinct entity and not a malignancy, some clinical and histological keratoacanthomas do progress to invasive and aggressive squamous cell cancers, therefore prompt and definitive treatment may be recommended.
Under the microscope, keratoacanthoma very closely resembles squamous cell carcinoma. In order to differeniate between the two, almost the entire structure needs to be removed and examined.
Classification
Keratoacanthomas (molluscum sebaceum) may be divided into the following types:
- Giant keratoacanthomas are a variant of keratoacanthoma, which may reach dimensions of several centimeters.
- Keratoacanthoma centrifugum marginatum is a cutaneous condition, a variant of keratoacanthomas, which is characterized by multiple tumors growing in a localized area.
- Multiple keratoacanthomas (also known as "Ferguson–Smith syndrome," "Ferguson-Smith type of multiple self-healing keratoacanthomas,") is a cutaneous condition, a variant of keratoacanthomas, which is characterized by the appearance of multiple, sometimes hundreds of keratoacanthomas.
- A solitary keratoacanthoma (also known as "Subungual keratoacanthoma") is a benign, but rapidly growing, locally aggressive tumor which sometimes occur in the nail apparatus.

- Generalized eruptive keratoacanthoma (also known as "Generalized eruptive keratoacanthoma of Grzybowski") is a cutaneous condition, a variant of keratoacanthomas, characterized by hundreds to thousands of tiny follicular keratotic papules over the entire body. Treatments are not successful for many patients with Generalized eruptive keratoacanthoma. Use of emollients and anti-itch medications can ease some symptoms. Improvement or complete resolutions of the condition has occurred with the application of the following medications: Acitretin, Isotretinoin, Fluorouracil, Methotrexate, Cyclophosphamide.
Cause
The tumors usually occur in older individuals. As with squamous cell cancer, it seems likely that ultraviolet light from the sun causes the development of KA. As with squamous cell cancer, sporadic cases have been found co-infected with the human papilloma virus (HPV).
Diagnosis
Keratoacanthoma presents as a fleshy, elevated and nodular lesion with an irregular crater shape and a characteristic central hyperkeratotic core. Usually the patient will notice a rapidly growing dome-shaped tumor on sun-exposed skin.
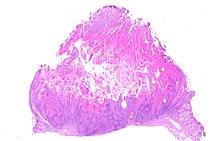
If the entire lesion is removed, the pathologist will probably be able to differentiate between keratoacanthoma and squamous cell carcinoma. If only part of the lesion is removed, confident diagnosis may be impossible.
Treatment
Excision of the entire lesion, with adequate margin, will remove the lesion, allow full tissue diagnosis, and leave a planned surgical wound which can usually be repaired with a good cosmetic result. However, removing the entire lesion (especially on the face) may present difficult problems of plastic reconstruction. (On the nose and face, Mohs surgery may allow for good margin control with minimal tissue removal, but many insurance companies require the correct diagnosis of a malignancy before they are prepared to pay the extra costs of Mohs surgery.) Especially in more cosmetically-sensitive areas, and where the clinical diagnosis is reasonably certain, alternatives to surgery may include no treatment (awaiting spontaneous resolution).
On the trunk, arms, and legs, electrodesiccation and curettage often suffice to control keratoacanthomas until they regress. Other modalities of treatment include cryosurgery and radiotherapy; intralesional injection of methotrexate or of 5-fluorouracil have also been used.<refKeratoacanthoma. Désirée Ratner. 2004. http://www.medscape.com/viewarticle/467069 accessed 23 June 2015</ref>
Recurrence after electrodesiccation and curettage is common, and usually can be identified and treated promptly with either further curettage or surgical excision.
See also
References
- Fisher, B.K., Elliot, G.B. Keratoacanthoma: Reflections on an Unusual Lesion. Can Med Assoc J. 1965 August 7; 93(6): 272–273.
- Kossard S; Tan KB; Choy C; Keratoacanthoma and infundibulocystic squamous cell carcinoma. Am J Dermatopathol. 2008; 30(2):127–34 (ISSN: 1533-0311)
- Weedon DD, et al. Squamous cell carcinoma arising in keratoacanthoma: a neglected phenomenon in the elderly. Am J Dermatopathol. 2010; 32(5):423–6
- Schwartz RA. The Keratoacanthoma: A Review. J Surg Oncol 1979; 12:305–17.
- Ko CJ, Keratoacanthoma: facts and controversies. Clin Dermatol. 2010; 28(3):254–61 (ISSN: 1879-1131)
- http://www.emedicine.com/derm/topic206.htm
- ^ Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- ^ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- Schwartz RA (February 2004). "Keratoacanthoma: a clinico-pathologic enigma". Dermatol Surg. 30 (2 Pt 2): 326–33, discussion 333. doi:10.1111/j.1524-4725.2004.30080.x. PMID 14871228.
- Niebuhr M, et al. Giant keratoacanthoma in an immunocompetent patient with detection of HPV 11. Hautarzt. 2009; 60(3):229–32 (ISSN: 1432-1173)
- Keratoacanthoma. Désirée Ratner. 2004. http://www.medscape.com/viewarticle/467069 accessed 23 June 2015
| Skin cancer of the epidermis | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tumor |
| ||||||||||||||||||
| Other |
| ||||||||||||||||||