This is an old revision of this page, as edited by CheMoBot (talk | contribs) at 04:31, 22 August 2011 (Updating {{drugbox}} (no changed fields - updated 'ChemSpiderID_Ref', 'DrugBank_Ref', 'UNII_Ref', 'ChEMBL_Ref', 'ChEBI_Ref', 'KEGG_Ref', 'StdInChI_Ref', 'StdInChIKey_Ref', 'ChEBI_Ref') per [[Misplaced Pages:WikiProject Chemicals/Chembox validation|Chem/Dru). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 04:31, 22 August 2011 by CheMoBot (talk | contribs) (Updating {{drugbox}} (no changed fields - updated 'ChemSpiderID_Ref', 'DrugBank_Ref', 'UNII_Ref', 'ChEMBL_Ref', 'ChEBI_Ref', 'KEGG_Ref', 'StdInChI_Ref', 'StdInChIKey_Ref', 'ChEBI_Ref') per [[Misplaced Pages:WikiProject Chemicals/Chembox validation|Chem/Dru)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff)| This article needs attention from an expert in Medicine. Please add a reason or a talk parameter to this template to explain the issue with the article. WikiProject Medicine may be able to help recruit an expert. (July 2009) |
| Vaccine description | |
|---|---|
| Target | Measles |
| Vaccine type | Attenuated |
| Clinical data | |
| ATC code | |
| (verify) | |
Measles vaccine is a highly effective vaccine used against measles. The measles-mumps-rubella-varicella combo (MMRV vaccine) vaccine has been available since 2005. The most common side effect is a fever, which occurs in about 5%-15% of patients.
Effectiveness
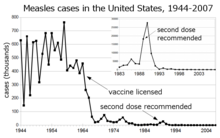
Before the widespread use of a vaccine against measles, its incidence was so high that infection with measles was felt to be "as inevitable as death and taxes." Today, the incidence of measles has fallen to less than 1% of people under the age of 30 in countries with routine childhood vaccination. In the United States, reported cases of measles fell from hundreds of thousands to tens of thousands per year following introduction of the vaccine in 1963 (see chart at right). Increasing uptake of the vaccine following outbreaks in 1971 and 1977 brought this down to thousands of cases per year in the 1980s. An outbreak of almost 30,000 cases in 1990 led to a renewed push for vaccination and the addition of a second vaccine to the recommended schedule. Fewer than 200 cases have been reported each year since 1997, and the disease is no longer considered endemic in the United States.
The benefit of measles vaccination in preventing illness, disability, and death has been well documented. The first 20 years of licensed measles vaccination in the U.S. prevented an estimated 52 million cases of the disease, 17,400 cases of mental retardation, and 5,200 deaths. During 1999–2004, a strategy led by the World Health Organization and UNICEF led to improvements in measles vaccination coverage that averted an estimated 1.4 million measles deaths worldwide. The vaccine for measles has led to the near-complete elimination of the disease in the United States and other developed countries. It was introduced in 1963. These impressive reductions in death and long-range after-effectiveness were initially achieved with a live virus version of the vaccine that itself caused side effects, although these are far fewer and less serious than the sickness and death caused by measles itself. While preventing many deaths and serious illnesses, the live virus version of the vaccine did cause side effects in a small percentage of recipients, ranging from rashes to, rarely, convulsions.
Measles is endemic worldwide. Although it was declared eliminated from the U.S. in 2000, high rates of vaccination and good communication with persons who refuse vaccination are needed to prevent outbreaks and sustain the elimination of measles in the U.S. Of the 66 cases of measles reported in the U.S. in 2005, slightly over half were attributable to one unvaccinated individual who acquired measles during a visit to Romania. This individual returned to a community with many unvaccinated children. The resulting outbreak infected 34 people, mostly children and virtually all unvaccinated; 9% were hospitalized, and the cost of containing the outbreak was estimated at $167,685. A major epidemic was averted due to high rates of vaccination in the surrounding communities.
History
As a fellow at Children's Hospital Boston, Dr. Thomas C. Peebles worked with Dr. John Franklin Enders, known as "The Father of Modern vaccines", who earned the Nobel Prize in 1954 for his research on cultivating the polio virus that led to the development of a vaccination for the disease. Switching to study measles, Peebles was sent to a school where an outbreak of the disease was under way and was able to isolate the virus from some of the blood samples and throat swabs he had taken from students. Even after Enders had taken him off the study team, Peebles was able to cultivate the virus and show that the disease could be passed on to monkeys inoculated with the material he had collected. Enders was able to use the cultivated virus to develop a measles vaccine in 1963 based on the material isolated by Peebles. In the late 1950s and early 1960s, nearly twice as many children died from measles as from polio. The vaccine Enders developed was based on the Edmonston strain of attenuated live measles virus, which was named for the student from which Peebles had taken the culture that led to the virus' cultivation.
Dr. Maurice Hilleman of Merck & Co., a pioneer in the development of vaccinations, developed the MMR vaccine in 1971, which treats measles, mumps and rubella in a single shot followed by a booster. One form is called "Attenuvax" with more than 40 peptide sequences. The measles component of the MMR vaccine uses Attenuvax, which is grown in a chick embryo cell culture using the Enders' attenuated Edmonston strain.
See also
References
- Ruigrok RW, Gerlier D (2007). "Structure of the measles virus H glycoprotein sheds light on an efficient vaccine". Proc. Natl. Acad. Sci. U.S.A. 104 (52): 20639–40. doi:10.1073/pnas.0709995105. PMC 2409202. PMID 18087048.
{{cite journal}}: Unknown parameter|month=ignored (help) - http://www.vaccineinformation.org/measles/qandavax.asp
- Babbott FL Jr, Gordon JE (1954). "Modern measles". Am J Med Sci. 228 (3): 334–61. PMID 13197385.
- Centers for Disease Control and Prevention Summary of notifable diseases—United States, 1993 Published October 21, 1994 for Morbidity and Mortality Weekly Report 1993; 42 (No. 53)
- Centers for Disease Control and Prevention Summary of notifable diseases—United States, 2007 Published July 9, 2009 for Morbidity and Mortality Weekly Report 2007; 56 (No. 53)
- Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases. Atkinson W, Wolfe S, Hamborsky J, McIntyre L, eds. 11th ed. Washington DC: Public Health Foundation, 2009
- Bloch AB, Orenstein WA, Stetler HC; et al. (1985). "Health impact of measles vaccination in the United States". Pediatrics. 76 (4): 524–32. PMID 3931045.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Centers for Disease Control and Prevention (CDC) (2006). "Progress in reducing global measles deaths, 1999–2004". MMWR Morb Mortal Wkly Rep. 55 (9): 247–9. PMID 16528234.
- ^ Martin, Douglas. "Dr. Thomas C. Peebles, Who Identified Measles Virus, Dies at 89", The New York Times, August 4, 2010. Accessed August 4, 2010.
- Hayden GF (1979). "Measles vaccine failure. A survey of causes and means of prevention". Clin Pediatr (Phila). 18 (3): 155–6, 161–3, 167. doi:10.1177/000992287901800308. PMID 371890.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Collins, Huntly. "The Man Who Saved Your Life - Maurice R. Hilleman - Developer of Vaccines for Mumps and Pandemic Flu: Maurice Hilleman's Vaccines Prevent Millions of Deaths Every Year", copy of article from The Philadelphia Inquirer, August 30, 1999. Accessed August 4, 2010.
- ^ Parker AA, Staggs W, Dayan GH; et al. (2006). "Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States". N Engl J Med. 355 (5): 447–55. doi:10.1056/NEJMoa060775. PMID 16885548.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Centers for Disease Control and Prevention (CDC) (2006). "Measles—United States, 2005". MMWR Morb Mortal Wkly Rep. 55 (50): 1348–51. PMID 17183226.
- Staff. "Work by Enders Brings Measles Vaccine License", The Hartford Courant, March 22, 1963. Accessed August 4, 2010. "A strain of measles virus isolated in 1954 by Dr. Thomas C. Peebles, instructor in pediatrics at Harvard, and Enders, formed the basis for the development of the present vaccine".
- Staff. "The Measles Vaccine", The New York Times, March 28, 1963. Accessed August 4, 2010.
- Hilleman, Maurice R. "Past, Present, and Future of Measles, Mumps, and Rubella Virus Vaccines", Pediatrics (journal), Vol. 90 No. 1 July 1992, pp. 149-153. Accessed August 4, 2010.
- Sullivan, Patricia (2005-04-13). "Maurice R. Hilleman Dies; Created Vaccines (washingtonpost.com)". The Washington Post. Retrieved 2009-07-21.
- Ovsyannikova IG, Johnson KL, Naylor S, Poland GA (2005). "Identification of HLA-DRB1-bound self-peptides following measles virus infection". J. Immunol. Methods. 297 (1–2): 153–67. doi:10.1016/j.jim.2004.12.020. PMID 15777939.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
| Artificial induction of immunity / Immunization: Vaccines, Vaccination, Infection, Inoculation (J07) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Development | |||||||||||
| Classes | |||||||||||
| Administration | |||||||||||
| Vaccines |
| ||||||||||
| Inventors/ researchers | |||||||||||
| Controversy | |||||||||||
| Related | |||||||||||
| |||||||||||