This is an old revision of this page, as edited by Altg20April2nd (talk | contribs) at 08:11, 26 May 2015 (→Nightlighting and the moon). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 08:11, 26 May 2015 by Altg20April2nd (talk | contribs) (→Nightlighting and the moon)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff)See also: Menstruation and Menstruation (mammal)
The menstrual cycle is the cycle of natural changes that occurs in the uterus and ovary as an essential part of making sexual reproduction possible. Its timing is governed by endogenous (internal) biological cycles. The menstrual cycle is essential for the production of eggs, and for the preparation of the uterus for pregnancy. The cycle occurs only in fertile female humans and other female primates. In human females, the menstrual cycle occurs repeatedly between the age of menarche, when cycling begins, until menopause, when it ends.
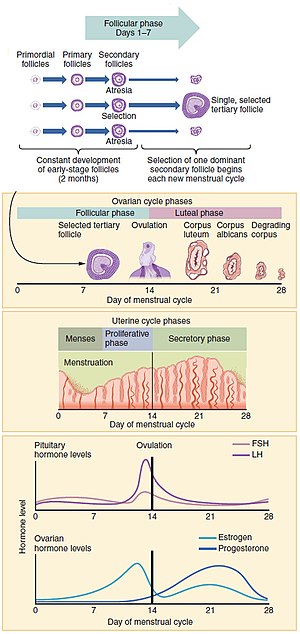
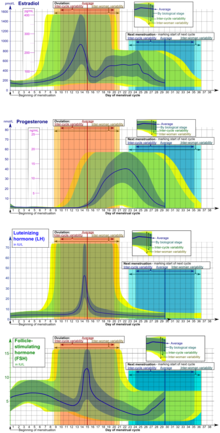
In humans, the length of a menstrual cycle varies greatly among women (ranging from 21 to 35 days), with 28 days designated as the average length. Each cycle can be divided into three phases based on events in the ovary (ovarian cycle) or in the uterus (uterine cycle). The ovarian cycle consists of the follicular phase, ovulation, and luteal phase whereas the uterine cycle is divided into menstruation, proliferative phase, and secretory phase. Both cycles are controlled by the endocrine system and the normal hormonal changes that occur can be interfered with using hormonal contraception to prevent reproduction.
By convention, the length of an individual menstrual cycle in days is counted starting with the first day of menstrual bleeding. Stimulated by gradually increasing amounts of estrogen in the follicular phase, discharges of blood (menses) flow then stop, and the lining of the uterus thickens. Follicles in the ovary begin developing under the influence of a complex interplay of hormones, and after several days one or occasionally two become dominant (non-dominant follicles atrophy and die). Approximately mid-cycle, 24–36 hours after the Luteinizing Hormone (LH) surges, the dominant follicle releases an ovum, or egg, in an event called ovulation. After ovulation, the egg only lives for 24 hours or less without fertilization while the remains of the dominant follicle in the ovary become a corpus luteum; this body has a primary function of producing large amounts of progesterone. Under the influence of progesterone, the endometrium (uterine lining) changes to prepare for potential implantation of an embryo to establish a pregnancy. If implantation does not occur within approximately two weeks, the corpus luteum will involute, causing sharp drops in levels of both progesterone and estrogen. The hormone drop causes the uterus to shed its lining and egg in a process termed menstruation.
In the menstrual cycle, changes occur in the female reproductive system as well as in other bodily systems (which can lead to breast tenderness or mood changes, for example). A woman's first menstruation is termed menarche, and occurs typically around age 12-13. The end of a woman's reproductive phase of life is called the menopause, and this commonly occurs somewhere between the ages of 45 and 55.
Overview
The average age of menarche in humans is 12–13 years, but it is considered normal for it to occur anywhere between ages 8 and 16. The average age of menarche is about 12.5 years in the United States, 12.72 in Canada, 12.9 in the UK and 13.06 ± 0.10 years in Iceland. Factors such as heredity, diet and overall health can accelerate or delay menarche. The cessation of menstrual cycles at the end of a woman's reproductive period is termed menopause. The average age of menopause in women is 52 years, with anywhere between 45 and 55 being common. Menopause before age 45 is considered premature in industrialised countries. Like the age of menarche, the age of menopause is largely a result of cultural and biological factors; however, illnesses, certain surgeries, or medical treatments may cause menopause to occur earlier than it might have otherwise.
The length of a woman's menstrual cycle typically varies somewhat, with some shorter cycles and some longer cycles. A woman who experiences variations of less than eight days between her longest cycles and shortest cycles is considered to have regular menstrual cycles. It is unusual for a woman to experience cycle length variations of less than four days. Length variation between eight and 20 days is considered as moderately irregular cycles. Variation of 21 days or more between a woman's shortest and longest cycle lengths is considered very irregular.
In a number of countries, mainly in Asia, legislation or corporate practice has introduced formal menstrual leave to provide women with either paid or unpaid leave of absence from their employment while they are menstruating. The practice is controversial.
Cycles and phases

The menstrual cycle can be described by the ovarian or uterine cycle. The ovarian cycle describes changes that occur in the follicles of the ovary whereas the uterine cycle describes changes in the endometrial lining of the uterus. Both cycles can be divided into three phases. The ovarian cycle consists of the follicular phase, ovulation, and the luteal phase whereas the uterine cycle consists of menstruation, proliferative phase, and secretory phase.
Ovarian cycle
Follicular phase
Main article: Follicular phaseThe follicular phase is the first part of the ovarian cycle. During this phase, the ovarian follicles mature and get ready to release an egg. The latter part of this phase overlaps with the proliferative phase of the uterine cycle.
Through the influence of a rise in follicle stimulating hormone (FSH) during the first days of the cycle, a few ovarian follicles are stimulated. These follicles, which were present at birth and have been developing for the better part of a year in a process known as folliculogenesis, compete with each other for dominance. Under the influence of several hormones, all but one of these follicles will stop growing, while one dominant follicle in the ovary will continue to maturity. The follicle that reaches maturity is called a tertiary, or Graafian, follicle, and it contains the ovum.
Ovulation
Main article: Ovulation
Ovulation is the second phase of the ovarian cycle in which a mature egg is released from the ovarian follicles into the oviduct. During the follicular phase, estradiol suppresses production of luteinizing hormone (LH) from the anterior pituitary gland. When the egg has nearly matured, levels of estradiol reach a threshold above which this effect is reversed and estrogen stimulates the production of a large amount of LH. This process, known as the LH surge, starts around day 12 of the average cycle and may last 48 hours.
The exact mechanism of these opposite responses of LH levels to estradiol is not well understood. In animals, a Gonadotropin-releasing hormone (GnRH) surge has been shown to precede the LH surge, suggesting that estrogen's main effect is on the hypothalamus, which controls GnRH secretion. This may be enabled by the presence of two different estrogen receptors in the hypothalamus: estrogen receptor alpha, which is responsible for the negative feedback estradiol-LH loop, and estrogen receptor beta, which is responsible for the positive estradiol-LH relationship. However in humans it has been shown that high levels of estradiol can provoke abrupt increases in LH, even when GnRH levels and pulse frequencies are held constant, suggesting that estrogen acts directly on the pituitary to provoke the LH surge.
The release of LH matures the egg and weakens the wall of the follicle in the ovary, causing the fully developed follicle to release its secondary oocyte. The secondary oocyte promptly matures into an ootid and then becomes a mature ovum. The mature ovum has a diameter of about 0.2 mm.
Which of the two ovaries—left or right—ovulates appears essentially random; no known left and right co-ordination exists. Occasionally, both ovaries will release an egg; if both eggs are fertilized, the result is fraternal twins.
After being released from the ovary, the egg is swept into the fallopian tube by the fimbria, which is a fringe of tissue at the end of each fallopian tube. After about a day, an unfertilized egg will disintegrate or dissolve in the fallopian tube.
Fertilization by a spermatozoon, when it occurs, usually takes place in the ampulla, the widest section of the fallopian tubes. A fertilized egg immediately begins the process of embryogenesis, or development. The developing embryo takes about three days to reach the uterus and another three days to implant into the endometrium. It has usually reached the blastocyst stage at the time of implantation.
In some women, ovulation features a characteristic pain called mittelschmerz (German term meaning middle pain). The sudden change in hormones at the time of ovulation sometimes also causes light mid-cycle blood flow.
Luteal phase
Main article: Luteal phaseThe luteal phase is the final phase of the ovarian cycle and it corresponds to the secretory phase of the uterine cycle. During the luteal phase, the pituitary hormones FSH and LH cause the remaining parts of the dominant follicle to transform into the corpus luteum, which produces progesterone. The increased progesterone in the adrenals starts to induce the production of estrogen. The hormones produced by the corpus luteum also suppress production of the FSH and LH that the corpus luteum needs to maintain itself. Consequently, the level of FSH and LH fall quickly over time, and the corpus luteum subsequently atrophies. Falling levels of progesterone trigger menstruation and the beginning of the next cycle. From the time of ovulation until progesterone withdrawal has caused menstruation to begin, the process typically takes about two weeks, with 14 days considered normal. For an individual woman, the follicular phase often varies in length from cycle to cycle; by contrast, the length of her luteal phase will be fairly consistent from cycle to cycle.
The loss of the corpus luteum is prevented by fertilization of the egg. The syncytiotrophoblast, which is the outer layer of the resulting embryo-containing structure (the blastocyst) and later also becomes the outer layer of the placenta, produces human chorionic gonadotropin (hCG), which is very similar to LH and which preserves the corpus luteum. The corpus luteum can then continue to secrete progesterone to maintain the new pregnancy. Most pregnancy tests look for the presence of hCG.
Uterine cycle
Menstruation
Main article: MenstruationMenstruation (also called menstrual bleeding, menses, catamenia or a period) is the first phase of the uterine cycle. The flow of menses normally serves as a sign that a woman has not become pregnant. (However, this cannot be taken as certainty, as a number of factors can cause bleeding during pregnancy; some factors are specific to early pregnancy, and some can cause heavy flow.)
Eumenorrhea denotes normal, regular menstruation that lasts for a few days (usually 3 to 5 days, but anywhere from 2 to 7 days is considered normal). The average blood loss during menstruation is 35 milliliters with 10–80 ml considered normal. Women who experience Menorrhagia are more susceptible to iron deficiency than the average person. An enzyme called plasmin inhibits clotting in the menstrual fluid.
Painful cramping in the abdomen, back, or upper thighs is common during the first few days of menstruation. Severe uterine pain during menstruation is known as dysmenorrhea, and it is most common among adolescents and younger women (affecting about 67.2% of adolescent females). When menstruation begins, symptoms of premenstrual syndrome (PMS) such as breast tenderness and irritability generally decrease. Many sanitary products are marketed to women for use during their menstruation.
Proliferative phase
The proliferative phase is the second phase of the uterine cycle when estrogen causes the lining of the uterus to grow, or proliferate, during this time. As they mature, the ovarian follicles secrete increasing amounts of estradiol, and estrogen. The estrogens initiate the formation of a new layer of endometrium in the uterus, histologically identified as the proliferative endometrium. The estrogen also stimulates crypts in the cervix to produce fertile cervical mucus, which may be noticed by women practicing fertility awareness.
Secretory phase
The secretory phase is the final phase of the uterine cycle and it corresponds to the luteal phase of the ovarian cycle. During the secretory phase, the corpus luteum produces progesterone, which plays a vital role in making the endometrium receptive to implantation of the blastocyst and supportive of the early pregnancy, by increasing blood flow and uterine secretions and reducing the contractility of the smooth muscle in the uterus; it also has the side effect of raising the woman's basal body temperature.
Length
The average menstrual cycle lasts 28 days. The variability of menstrual cycle lengths is highest for women under 25 years of age and is lowest, that is, most regular, for ages 35 to 39. Subsequently, the variability increases slightly for women aged 40 to 44. Usually, length variation between eight and 20 days in a woman is considered as moderately irregular menstrual cycles. Variation of 21 days or more is considered very irregular.
As measured on women undergoing in vitro fertilization, a longer menstrual cycle length is associated with higher pregnancy and delivery rates, even after age adjustment. Delivery rates after IVF have been estimated to be almost doubled for women with a menstrual cycle length of more than 34 days compared with women with a menstrual cycle length shorter than 26 days. A longer menstrual cycle length is also significantly associated with better ovarian response to gonadotropin stimulation and embryo quality.
The luteal phase of the menstrual cycle is about the same length in most individuals (mean 14/13 days, SD 1.41 days) whereas the follicular phase tends to show much more variability (log-normally distributed with 95% of individuals having follicular phases between 10.3 and 16.3 days). The follicular phase also seems to get significantly shorter with age (geometric mean 14.2 days in women aged 18–24 vs. 10.4 days in women aged 40–44).
Fertile window
Main article: Fertility testingThe most fertile period (the time with the highest likelihood of pregnancy resulting from sexual intercourse) covers the time from some 5 days before until 1 to 2 days after ovulation. In a 28‑day cycle with a 14‑day luteal phase, this corresponds to the second and the beginning of the third week. A variety of methods have been developed to help individual women estimate the relatively fertile and the relatively infertile days in the cycle; these systems are called fertility awareness.
Fertility awareness methods that rely on cycle length records alone are called calendar-based methods. Methods that require observation of one or more of the three primary fertility signs (basal body temperature, cervical mucus, and cervical position) are known as symptoms-based methods. Urine test kits are available that detect the LH surge that occurs 24 to 36 hours before ovulation; these are known as ovulation predictor kits (OPKs). Computerized devices, such as Lady-Comp, that interpret basal body temperatures, urinary test results, or changes in saliva are called fertility monitors.
A woman's fertility is also affected by her age. As a woman's total egg supply is formed in fetal life, to be ovulated decades later, it has been suggested that this long lifetime may make the chromatin of eggs more vulnerable to division problems, breakage, and mutation than the chromatin of sperm, which are produced continuously during a man's reproductive life. However, despite this hypothesis, a similar paternal age effect has also been observed.
Effect on other systems
Some women with neurological conditions experience increased activity of their conditions at about the same time during each menstrual cycle. For example, drops in estrogen levels have been known to trigger migraines, especially when the woman who suffers migraines is also taking the birth control pill. Many women with epilepsy have more seizures in a pattern linked to the menstrual cycle; this is called "catamenial epilepsy". Different patterns seem to exist (such as seizures coinciding with the time of menstruation, or coinciding with the time of ovulation), and the frequency with which they occur has not been firmly established. Using one particular definition, one group of scientists found that around one-third of women with intractable partial epilepsy has catamenial epilepsy. An effect of hormones has been proposed, in which progesterone declines and estrogen increases would trigger seizures. Recently, studies have shown that high doses of estrogen can cause or worsen seizures, whereas high doses of progesterone can act like an antiepileptic drug. Studies by medical journals have found that women experiencing menses are 1.68 times more likely to commit suicide.
Mice have been used as an experimental system to investigate possible mechanisms by which levels of sex steroid hormones might regulate nervous system function. During the part of the mouse estrous cycle when progesterone is highest, the level of nerve-cell GABA receptor subtype delta was high. Since these GABA receptors are inhibitory, nerve cells with more delta receptors are less likely to fire than cells with lower numbers of delta receptors. During the part of the mouse estrous cycle when estrogen levels are higher than progesterone levels, the number of delta receptors decrease, increasing nerve cell activity, in turn increasing anxiety and seizure susceptibility.
Estrogen levels may affect thyroid behavior. For example, during the luteal phase (when estrogen levels are lower), the velocity of blood flow in the thyroid is lower than during the follicular phase (when estrogen levels are higher).
Among women living closely together, it was once thought that the onsets of menstruation tend to synchronize. This effect was first described in 1971, and possibly explained by the action of pheromones in 1998. Subsequent research has called this hypothesis into question.
Research indicates that women have a significantly higher likelihood of anterior cruciate ligament injuries in the pre-ovulatory stage, than post-ovulatory stage.
Mood and behavior
The different phases of the menstrual cycle correlate with women’s moods. In some cases, hormones released during the menstrual cycle can cause behavioral changes in females; mild to severe mood changes can occur. The menstrual cycle phase and ovarian hormones may contribute to increased empathy in women. The natural shift of hormone levels during the different phases of the menstrual cycle has been studied in conjunction with test scores. When completing empathy exercises, women in the follicular stage of their menstrual cycle performed better than women in their midluteal phase. A significant correlation between progesterone levels and the ability to accurately recognize emotion was found. Performances on emotion recognition tasks were better when women had lower progesterone levels. Women in the follicular stage showed higher emotion recognition accuracy than their midluteal phase counterparts. Women were found to react more to negative stimuli when in midluteal stage over the women in the follicular stage, perhaps indicating more reactivity to social stress during that menstrual cycle phase. Overall, it has been found that women in the follicular phase demonstrated better performance in tasks that contain empathetic traits.
Fear response in women during two different points in the menstrual cycle has been examined. When oestrogen is highest in the preovulatory stage, women are significantly better at identifying expressions of fear than women who were menstruating, which is when oestrogen levels are lowest. The women were equally able to identify happy faces, demonstrating that the fear response was a more powerful response. To summarize, menstrual cycle phase and the oestrogen levels correlates with women’s fear processing.
However, the examination of daily moods in women with measuring ovarian hormones may indicate a less powerful connection. In comparison to levels of stress or physical health, the ovarian hormones had less of an impact on overall mood. This indicates that while changes of ovarian hormones may influence mood, on a day-to-day level it does not influence mood more than other stressors do.
Cycle abnormalities and disorders
Main article: Menstrual disorderInfrequent or irregular ovulation is called oligoovulation. The absence of ovulation is called anovulation. Normal menstrual flow can occur without ovulation preceding it: an anovulatory cycle. In some cycles, follicular development may start but not be completed; nevertheless, estrogens will be formed and stimulate the uterine lining. Anovulatory flow resulting from a very thick endometrium caused by prolonged, continued high estrogen levels is called estrogen breakthrough bleeding. Anovulatory bleeding triggered by a sudden drop in estrogen levels is called changes. Anovulatory cycles commonly occur before menopause (perimenopause) and in women with polycystic ovary syndrome.
Very little flow (less than 10 ml) is called hypomenorrhea. Regular cycles with intervals of 21 days or fewer are polymenorrhea; frequent but irregular menstruation is known as metrorrhagia. Sudden heavy flows or amounts greater than 80 ml are termed menorrhagia. Heavy menstruation that occurs frequently and irregularly is menometrorrhagia. The term for cycles with intervals exceeding 35 days is oligomenorrhea. Amenorrhea refers to more than three to six months without menses (while not being pregnant) during a woman's reproductive years.
George Preti, an organic chemist at the Monell Chemical Senses Center in Philadelphia and Winnefred Cutler of the University of Pennsylvania's psychology department, discovered that women with irregular menstrual cycles became regular when exposed to male underarm extracts. They hypothesized that the only explanation was that underarms contain pheromones, as there was no other explanation for the effects, which mirrored how pheromones affect other mammals.
Ovulation suppression
Hormonal contraception
Main article: Hormonal contraception
While some forms of birth control do not affect the menstrual cycle, hormonal contraceptives work by disrupting it. Progestogen negative feedback decreases the pulse frequency of gonadotropin-releasing hormone (GnRH) release by the hypothalamus, which decreases the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) by the anterior pituitary. Decreased levels of FSH inhibit follicular development, preventing an increase in estradiol levels. Progestogen negative feedback and the lack of estrogen positive feedback on LH release prevent a mid-cycle LH surge. Inhibition of follicular development and the absence of a LH surge prevent ovulation.
The degree of ovulation suppression in progestogen-only contraceptives depends on the progestogen activity and dose. Low dose progestogen-only contraceptives—traditional progestogen only pills, subdermal implants Norplant and Jadelle, and intrauterine system Mirena—inhibit ovulation in about 50% of cycles and rely mainly on other effects, such as thickening of cervical mucus, for their contraceptive effectiveness. Intermediate dose progestogen-only contraceptives—the progestogen-only pill Cerazette and the subdermal implant Nexplanon—allow some follicular development but more consistently inhibit ovulation in 97–99% of cycles. The same cervical mucus changes occur as with very low-dose progestogens. High-dose, progestogen-only contraceptives—the injectables Depo-Provera and Noristerat—completely inhibit follicular development and ovulation.
Combined hormonal contraceptives include both an estrogen and a progestogen. Estrogen negative feedback on the anterior pituitary greatly decreases the release of FSH, which makes combined hormonal contraceptives more effective at inhibiting follicular development and preventing ovulation. Estrogen also reduces the incidence of irregular breakthrough bleeding. Several combined hormonal contraceptives—the pill, NuvaRing, and the contraceptive patch—are usually used in a way that causes regular withdrawal bleeding. In a normal cycle, menstruation occurs when estrogen and progesterone levels drop rapidly. Temporarily discontinuing use of combined hormonal contraceptives (a placebo week, not using patch or ring for a week) has a similar effect of causing the uterine lining to shed. If withdrawal bleeding is not desired, combined hormonal contraceptives may be taken continuously, although this increases the risk of breakthrough bleeding.
Lactational amenorrhea
Main article: Lactational amenorrhea methodBreastfeeding causes negative feedback to occur on pulse secretion of gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH). Depending on the strength of the negative feedback, breastfeeding women may experience complete suppression of follicular development, follicular development but no ovulation, or normal menstrual cycles may resume. Suppression of ovulation is more likely when suckling occurs more frequently. The production of prolactin in response to suckling is important to maintaining lactational amenorrhea. On average, women who are fully breastfeeding whose infants suckle frequently experience a return of menstruation at fourteen and a half months postpartum. There is a wide range of response among individual breastfeeding women, however, with some experiencing return of menstruation at two months and others remaining amenorrheic for up to 42 months postpartum.
Etymological and cultural associations
Menstruation and the moon
See also: Culture and menstruation and Lunar effectThe word "menstruation" is etymologically related to "moon". The terms "menstruation" and "menses" are derived from the Latin mensis (month), which in turn relates to the Greek mene (moon) and to the roots of the English words month and moon.
To many, such cultural associations appear persuasive in view of the fact that the human menstrual quite closely approximates the moon’s 29.5-day synodic cycle, unlike chimpanzees (~36 days) or bonobos (~40 days). Statistical information from hunter gatherers is lacking, but where large-scale western studies focus on women’s peak reproductive years – removing outlier values – the cycle length gravitates around 29.1-29.5 days, while the figure for women in their thirties shortens toward 28 days. In no extant human population has statistically significant lunar phase-locking been demonstrated. Turning to the evolutionary past, however, a possible adaptive basis for the biological capacity would be reproductive levelling: among primates, synchronising to any natural clock makes it difficult for an alpha male to monopolise fertile sex with multiple females This would be consistent with the striking gender egalitarianism of non-storage hunter-gatherer societies. A further deep-time evolutionary pressure may have been lions’ habit of eating people on moonless nights:
Nocturnal carnivores are widely believed to have played an important role in human evolution, driving the need for nighttime shelter, the control of fire and our innate fear of darkness. We performed an extensive analysis of predatory behavior across the lunar cycle on the largest dataset of lion attacks ever assembled and found that African lions are as sensitive to moonlight when hunting humans as when hunting herbivores and that lions are most dangerous to humans when the moon is faint or below the horizon.
— C. Packer, A. Swanson, D. Ikanda, and H. Kushnir (2011), "Fear of Darkness, the Full Moon and the Nocturnal Ecology of African Lions.", PLoS ONE, 6 (7): e22285, doi:10.1371/journal.pone.0022285{{citation}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link)
For some 3 - 4 million years, bipedal hominins in the East African Rift valley were evolving in potential conflict and competition with fearsome carnivores including sabre-toothed cats equipped with excellent night-vision. Using the largest data set ever recorded – 1,000 lion attacks on humans across Tanzania between 1988 and 2009 – Craig Packer and his colleagues showed that there is a peak of attacks by lions upon humans during the evening dark hours following full moon. According to Packer, this may help explain why so many myths and superstitions attribute fearsome dangers and nightmarish potencies to the moon.
While not all archaeologists accept that lunar periodicity was ever relevant to human evolution, those favouring the idea include Curtis Marean, who heads excavations at the important Middle Stone Age site of Pinnacle Point, South Africa. Marean argues that anatomically modern humans around 165,000 years ago – when inland regions of the continent were dry, arid and uninhabitable – became restricted to small populations clustered around coastal refugia, reliant on marine resources including shellfish whose safe harvesting at spring low tides presupposed careful tracking of lunar phase. Against this background, if Marean is right, humans who ignored or misread the moon might frequently have been drowned.
With gradual offshore platforms during spring low tides, substantial areas of the intertidal zone are revealed, and these are the most productive and safest shellfish collecting times... Foragers should schedule visits to coastal residential sites at times during the lunar month when spring tides are present and then move slightly inland during neaps to broaden the size of the exploitable terrestrial area.
— Marean, C. 2010. Pinnacle Point Cave 13B (Western Cape Province, South Africa) in context: The Cape Floral kingdom, shellfish, and modern human origins. Journal of Human Evolution 59: 425e-443 .
When early Pleistocene hominids in Africa were attempting to survive by robbing big cats of their kills, according to some evolutionary scientists, it may have been adaptive to restrict overnight journeys – including sexual liaisons – to times when there was a moon in the sky. Some authors believe that, historically, women in traditional societies without nightlighting ovulated with the full moon and menstruated with the new moon, and one author documents the controversial attempts to use the association to improve the rhythm method of regulating conception.
Some studies in both humans and other animals have found that artificial light at night does influence the menstrual cycle in humans and the estrus cycle in mice (cycles are more regular in the absence of artificial light at night). It has also been suggested that bright light exposure in the morning promotes more regular cycles.
A meta-analysis of studies from 1996 showed no correlation between the human menstrual cycle and the lunar cycle. Dogon villagers did not have electric lighting and spent most nights outdoors, talking and sleeping; so they were apparently an ideal population for detecting a lunar influence; none was found. Other scholars counter, however, that the Dogon — unlike ancestral African hunter-gatherer populations — are polygamous, meaning that reproductive synchrony would not be expected on theoretical grounds.
References
- ^ Silverthorn, Dee Unglaub (2013). Human Physiology: An Integrated Approach (6th ed.). Glenview, IL: Pearson Education, Inc. pp. 850–890. ISBN 0-321-75007-1.
- Sherwood, Laurelee (2013). Human Physiology: From Cells to Systems (8th ed.). Belmont, CA: Cengage. pp. 735–794. ISBN 1-111-57743-9.
- Widmaier, Eric P.; Raff, Hershel; Strang, Kevin T. (2010). Vander's Human Physiology: The Mechanism of Body Function (12th ed.). New York, NY: McGrawHill. pp. 555–631. ISBN 0-077-35001-4.
- Klump KL, Keel PK, Racine SE, Burt SA, Burt AS, Neale M, Sisk CL, Boker S, Hu JY (February 2013). "The interactive effects of estrogen and progesterone on changes in emotional eating across the menstrual cycle". J Abnorm Psychol. 122 (1): 131–7. doi:10.1037/a0029524. PMID 22889242.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Anderson SE, Dallal GE, Must A (April 2003). "Relative weight and race influence average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart". Pediatrics. 111 (4 Pt 1): 844–50. doi:10.1542/peds.111.4.844. PMID 12671122.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Al-Sahab B, Ardern CI, Hamadeh MJ, Tamim H (2010). "Age at menarche in Canada: results from the National Longitudinal Survey of Children & Youth". BMC Public Health. 10: 736. doi:10.1186/1471-2458-10-736. PMC 3001737. PMID 21110899.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Hamilton-Fairley, Diana (2004) . Lecture notes on obstetrics and gynaecology (pdf) (2nd ed.). Blackwell. p. 29. ISBN 1-4051-2066-5.
- Macgússon TE (May 1978). "Age at menarche in Iceland". Am. J. Phys. Anthropol. 48 (4): 511–4. doi:10.1002/ajpa.1330480410. PMID 655271.
- "At what age does a girl get her first period?". National Women's Health Information Center. Retrieved 20 November 2011.
- "Clinical topic - Menopause". NHS. Retrieved 2 November 2009.
- Beyene, Yewoubdar (1989). From Menarche to Menopause: Reproductive Lives of Peasant Women in Two Cultures. Albany, NY: State University of New York Press. ISBN 0-88706-866-9.
- Shuman, Tracy (February 2006). "Your Guide to Menopause". WebMD. Retrieved 16 December 2006.
- ^ Kippley, John; Kippley, Sheila (1996). The Art of Natural Family Planning (4th ed.). Cincinnati: The Couple to Couple League. p. 92. ISBN 978-0-926412-13-2.
- Maila Ager (18 August 2008). "Mandatory menstruation leave measure filed in House". Inquirer.net. Retrieved 16 June 2011.
- Owoseje, Toyin (31 July 2013). "Menstruation Leave: Russian Lawmaker Proposes Paid Days Off For Women Employees on Period". International Business Times. Retrieved 3 January 2014.
- Iuliano, Sarah. "Menstrual leave: delightful or discriminatory?". 5 August 2013. Lip Magazine. Retrieved 3 January 2014.
- Price, Catherine (11 October 2006). "Should women get paid menstruation leave?". Salon. Retrieved 3 January 2014.
- ^ Losos, Jonathan B.; Raven, Peter H.; Johnson, George B.; Singer, Susan R. (2002). Biology. New York: McGraw-Hill. pp. 1207–09. ISBN 0-07-303120-8.
- Ovulation Test at Duke Fertility Center. Retrieved 2 July 2011
- "Ovulation Calendar". Pregnology.
- ^ Comprehensive gynecology. St. Louis: Elsevier Mosby. 2013. ISBN 978-0-323-06986-1. Retrieved 5 April 2012.
{{cite book}}: Unknown parameter|authors=ignored (help) - Hu L, Gustofson RL, Feng H, Leung PK, Mores N, Krsmanovic LZ, Catt KJ (October 2008). "Converse regulatory functions of estrogen receptor-alpha and -beta subtypes expressed in hypothalamic gonadotropin-releasing hormone neurons". Mol. Endocrinol. 22 (10): 2250–9. doi:10.1210/me.2008-0192. PMC 2582533. PMID 18701637.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Gray, Henry David (2000). "The Ovum". Anatomy of the human body. Philadelphia: Bartleby.com. ISBN 1-58734-102-6.
{{cite book}}:|access-date=requires|url=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Ecochard R, Gougeon A (April 2000). "Side of ovulation and cycle characteristics in normally fertile women". Hum. Reprod. 15 (4): 752–5. doi:10.1093/humrep/15.4.752. PMID 10739814.
- "Multiple Pregnancy: Twins or More - Topic Overview". WebMD Medical Reference from Healthwise. 24 July 2007. Retrieved 5 October 2008.
- ^ John M Goldenring (1 February 2007). "All About Menstruation". WebMD. Retrieved 5 October 2008.
- Weschler (2002), p.65
- Weschler (2002), p.47
- Greenfield, Marjorie (17 September 2001). "Subchorionic Hematoma in Early Pregnancy". Ask Our Experts. DrSpock.com. Archived from the original on 15 September 2008. Retrieved 21 September 2008.
- Anderson-Berry, Ann L; Terence Zach (10 December 2007). "Vanishing Twin Syndrome". Emedicine.com. WebMD. Retrieved 21 September 2008.
- Ko, Patrick; Young Yoon (23 August 2007). "Placenta Previa". Emedicine.com. WebMD. Retrieved 21 September 2008.
- "Menstruation and the Menstrual Cycle". Womenshealth.gov. April 2007. Archived from the original on 24 October 2008.
- David L Healy (24 November 2004). "Menorrhagia Heavy Periods - Current Issues". Monash University. ABN 12 377 614 012.
- Harvey LJ, Armah CN, Dainty JR, Foxall RJ, John Lewis D, Langford NJ, Fairweather-Tait SJ (October 2005). "Impact of menstrual blood loss and diet on iron deficiency among women in the UK". Br. J. Nutr. 94 (4): 557–64. doi:10.1079/BJN20051493. PMID 16197581.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Shiraishi M (August 1962). "Studies on identification of menstrual blood stain by fibrin-plate method. I. A study on the incoagulability of menstrual blood". Acta Med Okayama. 16: 192–200. PMID 13977381.
- Sharma P, Malhotra C, Taneja DK, Saha R (February 2008). "Problems related to menstruation amongst adolescent girls". Indian J Pediatr. 75 (2): 125–9. doi:10.1007/s12098-008-0018-5. PMID 18334791.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Weschler, Toni (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. pp. 359–361. ISBN 0-06-093764-5.
- Lombardi, Julian (1998). Comparative Vertebrate Reproduction. Springer. p. 184. ISBN 9780792383369.
- ^ Weschler (2002), pp.361-2
- ^ Chiazze L, Brayer FT, Macisco JJ, Parker MP, Duffy BJ (February 1968). "The length and variability of the human menstrual cycle". JAMA. 203 (6): 377–80. doi:10.1001/jama.1968.03140060001001. PMID 5694118.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Brodin T, Bergh T, Berglund L, Hadziosmanovic N, Holte J (2008). "Menstrual cycle length is an age-independent marker of female fertility: Results from 6271 treatment cycles of in vitro fertilization". Fertility and Sterility. 90 (5): 1656–1661. doi:10.1016/j.fertnstert.2007.09.036. PMID 18155201.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lenton EA, Landgren BM, Sexton L (July 1984). "Normal variation in the length of the luteal phase of the menstrual cycle: identification of the short luteal phase". Br J Obstet Gynaecol. 91 (7): 685–9. doi:10.1111/j.1471-0528.1984.tb04831.x. PMID 6743610.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lenton EA, Landgren BM, Sexton L, Harper R (July 1984). "Normal variation in the length of the follicular phase of the menstrual cycle: effect of chronological age". Br J Obstet Gynaecol. 91 (7): 681–4. doi:10.1111/j.1471-0528.1984.tb04830.x. PMID 6743609.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Weschler (2002), pp.242,374
- ^ "Medical Eligibility Criteria for Contraceptive Use:Fertility awareness-based methods". Third edition. World Health Organization. 2004. Retrieved 29 April 2008.
{{cite journal}}: Cite journal requires|journal=(help) - Weschler (2002), p.52
- MedlinePlus Encyclopedia: LH urine test (home test)
- Leridon H (July 2004). "Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment". Hum. Reprod. 19 (7): 1548–53. doi:10.1093/humrep/deh304. PMID 15205397.
- Krock, Lexi (October 2001). "Fertility Throughout Life". 18 Ways to Make a Baby. NOVA Online. Retrieved 24 December 2006. Haines, Cynthiac (January 2006). "Your Guide to the Female Reproductive System". The Cleveland Clinic Women's Health Center. WebMD. Retrieved 24 December 2006.
- "Migraine and Estrogen Officially Linked". The Daily Headache. Retrieved 19 October 2012.
- ^ Herzog AG (March 2008). "Catamenial epilepsy: definition, prevalence pathophysiology and treatment". Seizure. 17 (2): 151–9. doi:10.1016/j.seizure.2007.11.014. PMID 18164632.
- Herzog AG, Harden CL, Liporace J, Pennell P, Schomer DL, Sperling M, Fowler K, Nikolov B, Shuman S, Newman M (September 2004). "Frequency of catamenial seizure exacerbation in women with localization-related epilepsy". Annals of Neurology. 56 (3): 431–4. doi:10.1002/ana.20214. PMID 15349872.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Herzog AG, Klein P, Ransil BJ (October 1997). "Three patterns of catamenial epilepsy". Epilepsia. 38 (10): 1082–8. doi:10.1111/j.1528-1157.1997.tb01197.x. PMID 9579954.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Scharfman HE, MacLusky NJ (September 2006). "The influence of gonadal hormones on neuronal excitability, seizures, and epilepsy in the female". Epilepsia. 47 (9): 1423–40. doi:10.1111/j.1528-1167.2006.00672.x. PMC 1924802. PMID 16981857.
- "Menstrual cycle". epilepsy.com. Retrieved 19 October 2012.
- Baca-García E, Diaz-Sastre C, Ceverino A, Saiz-Ruiz J, Diaz FJ, de Leon J (2003). "Association between the menses and suicide attempts: a replication study". Psychosom Med. 65 (2): 237–44. doi:10.1097/01.PSY.0000058375.50240.F6. PMID 12651991.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Maguire JL, Stell BM, Rafizadeh M, Mody I (June 2005). "Ovarian cycle-linked changes in GABA(A) receptors mediating tonic inhibition alter seizure susceptibility and anxiety". Nat. Neurosci. 8 (6): 797–804. doi:10.1038/nn1469. PMID 15895085.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Doufas AG, Mastorakos G (2000). "The hypothalamic-pituitary-thyroid axis and the female reproductive system". Annals of the New York Academy of Sciences. 900: 65–76. doi:10.1111/j.1749-6632.2000.tb06217.x. PMID 10818393.
- Krejza J, Nowacka A, Szylak A, Bilello M, Melhem LY (July 2004). "Variability of thyroid blood flow Doppler parameters in healthy women". Ultrasound Med Biol. 30 (7): 867–76. doi:10.1016/j.ultrasmedbio.2004.05.008. PMID 15313319.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Stern K, McClintock MK (March 1998). "Regulation of ovulation by human pheromones". Nature. 392 (6672): 177–9. doi:10.1038/32408. PMID 9515961.
- Adams, Cecil (20 December 2002). "Does menstrual synchrony really exist?". The Straight Dope. The Chicago Reader. Retrieved 10 January 2007.
- Renstrom P, Ljungqvist A, Arendt E, Beynnon B, Fukubayashi T, Garrett W, Georgoulis T, Hewett TE, Johnson R, Krosshaug T, Mandelbaum B, Micheli L, Myklebust G, Roos E, Roos H, Schamasch P, Shultz S, Werner S, Wojtys E, Engebretsen L (June 2008). "Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement". Br J Sports Med. 42 (6): 394–412. doi:10.1136/bjsm.2008.048934. PMC 3920910. PMID 18539658.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Schmidt PJ, Nieman LK, Danaceau MA, Adams LF, Rubinow DR (January 1998). "Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome". N. Engl. J. Med. 338 (4): 209–16. doi:10.1056/NEJM199801223380401. PMID 9435325.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Derntl B, Hack RL, Kryspin-Exner I, Habel U (January 2013). "Association of menstrual cycle phase with the core components of empathy". Horm Behav. 63 (1): 97–104. doi:10.1016/j.yhbeh.2012.10.009. PMC 3549494. PMID 23098806.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Schwartz DH, Romans SE, Meiyappan S, De Souza MJ, Einstein G (September 2012). "The role of ovarian steroid hormones in mood". Horm Behav. 62 (4): 448–54. doi:10.1016/j.yhbeh.2012.08.001. PMID 22902271.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Pearson R, Lewis MB (March 2005). "Fear recognition across the menstrual cycle". Horm Behav. 47 (3): 267–71. doi:10.1016/j.yhbeh.2004.11.003. PMID 15708754.
- Galan, Nicole (16 April 2008). "Oligoovulation". about.com. Retrieved 12 October 2008.
- Weschler (2002), p.107
- Anovulation at eMedicine
- ^ Menstruation Disorders at eMedicine
- ^ Oriel KA, Schrager S (October 1999). "Abnormal uterine bleeding". Am Fam Physician. 60 (5): 1371–80, discussion 1381–2. PMID 10524483.
- ^ Delude, Cathryn M. (2 September 2003). "Looking for love potion number nine". Boston Globe.
- ^ Trussell, James (2007). "Contraceptive Efficacy". In Hatcher, Robert A.; et al. (eds.). Contraceptive Technology (19th rev. ed.). New York: Ardent Media. ISBN 0-9664902-0-7.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Speroff, Leon; Darney, Philip D. (2005). "Oral Contraception". A Clinical Guide for Contraception (4th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 21–138. ISBN 0-7817-6488-2.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Brunton, Laurence L.; Lazo, John S.; Parker, Keith, eds. (2005). Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. pp. 1541–71. ISBN 0-07-142280-3.
- ^ Glasier, Anna (2006). "Contraception". In DeGroot, Leslie J.; Jameson, J. Larry (eds.) (ed.). Endocrinology (5th ed.). Philadelphia: Elsevier Saunders. pp. 3000–1. ISBN 0-7216-0376-9.
{{cite book}}:|editor=has generic name (help)CS1 maint: multiple names: editors list (link) - McNeilly AS (2001). "Lactational control of reproduction". Reprod. Fertil. Dev. 13 (7–8): 583–90. doi:10.1071/RD01056. PMID 11999309.
- Kippley, John; Sheila Kippley (1996). The Art of Natural Family Planning (4th ed.). Cincinnati, OH: The Couple to Couple League. p. 347. ISBN 0-926412-13-2.
- Stallings JF, Worthman CM, Panter-Brick C, Coates RJ (February 1996). "Prolactin response to suckling and maintenance of postpartum amenorrhea among intensively breastfeeding Nepali women". Endocr. Res. 22 (1): 1–28. doi:10.3109/07435809609030495. PMID 8690004.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Breastfeeding: Does It Really Space Babies?". The Couple to Couple League International. Internet Archive. 17 January 2008. Archived from the original on 17 January 2008. Retrieved 21 September 2008., which cites:
- Kippley SK, Kippley JF (November–December 1972). "The relation between breastfeeding and amenorrhea". Journal of obstetric, gynecologic, and neonatal nursing. 1 (4): 15–21. doi:10.1111/j.1552-6909.1972.tb00558.x. PMID 4485271.
- Sheila Kippley (November–December 1986 and January–February 1987). "Breastfeeding survey results similar to 1971 study". The CCL News. 13 (3): 10.
{{cite journal}}: Check date values in:|date=(help) and 13(4): 5.
- ^ Allen, Kevin (2007). The Reluctant Hypothesis: A History of Discourse Surrounding the Lunar Phase Method of Regulating Conception. Lacuna Press. p. 239. ISBN 978-0-9510974-2-7.
- Martin, R. D. 1992. Female cycles in relation to paternity in primate societies. In R. D. Martin, A. F. Dixson and E. J. Wickings (eds), Paternity in Primates. Genetic tests and theories. Basel: Karger, pp. 238-74.
- Martin, R. D. 2007. The evolution of human reproduction: a primatological perspective. Am J Phys Anthropol. Suppl 45:59-84.
- Saltzman, W., S. D. Tardif and J. N. Rutherford, 2010. Hormones and Reproductive Cycles in Primates. Chapter 13 in D. O. Norris and K. H. Lopez (eds), Hormones and Reproduction of Vertebrates, Vol. 5, Mammals. London: Academic Press.
- Treloar, A. E., R. E. Boynton, B. G. Behn and B. W. Brown 1967. Variation of the human menstrual cycle through reproductive life. International Journal of Fertility 12: 77-126.
- Harlow, S. D., Lin X and Ho, M. J. 2000. Analysis of menstrual diary data across the reproductive life span: applicability of the bipartite model approach and the importance of within-woman variance. J Clin Epidemiol. 53(7):722-33.
- Turke, P. W. 1984. Effects of ovulatory concealment and synchrony on protohominid mating systems and parental roles. Ethology and Sociobiology 5: 33-44.
- Turke, P. W. 1988. Concealed ovulation, menstrual synchrony and paternal investment. in E. Filsinger (ed.), Biosocial Perspectives on the Family. Newbury Park, CA: Sage, pp. 119-136.
- Ostner, J, C. L. Nunn and O. Schülke 2008. Female reproductive synchrony predicts skewed paternity across primates. Behavioral Ecology 19(6): 1150-1158.
- Carnes L. M., Nunn C. L., Lewis R. J. 2011. Effects of the Distribution of Female Primates on the Number of Males. PLoS ONE 6(5): e19853. doi:10.1371/journal.pone.0019853
- Power, C., Sommer, V., Watts, I., (2013). The Seasonality Thermostat: Female reproductive synchrony and male behaviour in monkeys, Neanderthals and modern humans. PaleoAnthropology 2013: 33−60. doi:10.4207/PA.2013.ART79
- M. Dyble, G. D. Salali, N. Chaudhary, A. Page, D. Smith, J. Thompson, L. Vinicius, R. Mace, A. B. Migliano. Sex equality can explain the unique social structure of hunter-gatherer bands. Science, 2015 DOI: 10.1126/science.aaa5139
- Packer, C., A. Swanson, D. Ikanda and H. Kushnir 2011. Fear of Darkness, the Full Moon and the Nocturnal Ecology of African Lions. PLoS ONE 6(7): e22285. Doi10.1371/journal.pone.0022285.
- C. Packer, A. Swanson, D. Ikanda, and H. Kushnir (2011). Fear of Darkness, the Full Moon and the Nocturnal Ecology of African Lions. PLoS ONE 6(7): e22285. doi:10.1371/journal.pone.0022285
- Curtis Marean (2010). Pinnacle Point Cave 13B (Western Cape Province, South Africa) in context: The Cape Floral kingdom, shellfish, and modern human origins. Journal of Human Evolution 59: 425e443
- Blumenschine, R. J. 1986. Early Hominid Scavenging Opportunities: Implications of Carcass Availability in the Serengeti and Ngorongoro Ecosystems. Oxford: British Archaeological Reports, International Series 283.
- O’Connell, J. F., K. Hawkes, K. D. Lupo and N. Blurton Jones 2002. Male strategies and Plio-Pleistocene archaeology. Journal of Human Evolution 43, 831–872
- Shipman, P. 2011. The Animal Connection. A new perspective on what makes us human. New York & London: Norton.
- Packer, C., A. Swanson, D. Ikanda and H. Kushnir 2011. Fear of Darkness, the Full Moon and the Nocturnal Ecology of African Lions. PLoS ONE 6(7): e22285. Doi10.1371/journal.pone.0022285
- Cohen, Sari (February–March 2005). "Melatonin, menstruation, and the moon". Townsend Letter for Doctors and Patients. Retrieved 21 September 2008.
"The Human Symbolic Revolution: A Darwinian Account" (PDF). Cambridge Archaeological Journal. 5 (1): 75–114. 1995. doi:10.1017/S0959774300001190. Retrieved 13 December 2006.{{cite journal}}: Unknown parameter|authors=ignored (help)
Lacey, Louise (1975). Lunaception: a feminine odyssey into fertility and contraception. New York: Coward, McCann & Geoghegan. ISBN 0-698-10674-1. - Singer, Katie. "Fertility Awareness, Food, and Night-Lighting". Wise Traditions in Food, Farming and the Healing Arts, Spring 2004. See section on Night-Lighting.
- Harder, Ben (28 August 2004). "Bright nights kindle cancers in mice". Science News. 166 (9): 141. doi:10.1002/scin.5591660912.
- Danilenko KV, Samoilova EA (2007). "Stimulatory Effect of Morning Bright Light on Reproductive Hormones and Ovulation: Results of a Controlled Crossover Trial". PLoS clinical trials. 2 (2): e7. doi:10.1371/journal.pctr.0020007. PMC 1851732. PMID 17290302.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - As cited by Adams, Cecil, "What's the link between the moon and menstruation?" (accessed 6 June 2006):
Abell, George O.; Barry Singer (1983). Science and the Paranormal: Probing the Existence of the Supernatural. Scribner Book Company. ISBN 0-684-17820-6. - Cutler WB (August 1980). "Lunar and menstrual phase locking". Am. J. Obstet. Gynecol. 137 (7): 834–9. PMID 7405975.
- Friedmann E (June 1981). "Menstrual and lunar cycles". Am. J. Obstet. Gynecol. 140 (3): 350. PMID 7246643.
- Law SP (1986). "The regulation of menstrual cycle and its relationship to the moon". Acta Obstet Gynecol Scand. 65 (1): 45–8. doi:10.3109/00016348609158228. PMID 3716780.
- Zimecki M (2006). "The lunar cycle: effects on human and animal behavior and physiology". Postepy Hig Med Dosw (Online). 60: 1–7. PMID 16407788.
- Kelly, Ivan; Rotton, James; Culver, Roger; Simpson, Audric (1986). "The Moon Was Full and Nothing Happened: A Review of Studies on the Moon and Human Behavior". Skeptical Inquirer. 10 (2): 129–43.. Reprinted in The Hundredth Monkey - and other paradigms of the paranormal, edited by Kendrick Frazier, Prometheus Books. Revised and updated in The Outer Edge: Classic Investigations of the Paranormal, edited by Joe Nickell, Barry Karr, and Tom Genoni, 1996, CSICOP.
- Strassmann B. I. (1997). "The biology of menstruation in Homo sapiens: total lifetime menses, fecundity, and nonsynchrony in a natural fertility population". Current Anthropology. 38: 123–9. doi:10.1086/204592. JSTOR 2744446.
- Power, C., V. Sommer, and I. Watts (2013) The Seasonality Thermostat: Female Reproductive Synchrony and Male Behavior in Monkeys, Neanderthals, and Modern Humans. PaleoAnthropology 2013:33-60
External links
| Menstrual cycle | |||||
|---|---|---|---|---|---|
| Events and phases | |||||
| Life stages | |||||
| Tracking |
| ||||
| Suppression | |||||
| Disorders | |||||
| Related events | |||||
| Mental health | |||||
| Hygiene | |||||
| In culture and religion | |||||