
The 1993 Four Corners hantavirus outbreak was a disease outbreak caused by a hantavirus that occurred in the Four Corners region of the US states in Arizona, Colorado, and New Mexico. The outbreak marked the discovery of hantaviruses in the Western Hemisphere that could cause disease and revealed the existence of a novel type of disease caused by hantaviruses: hantavirus pulmonary syndrome (HPS). Hantaviruses that cause disease in humans are native to rodents and, prior to the outbreak, were known to exist in Asia and Europe, but previously were only associated with a different disease called hemorrhagic fever with renal syndrome (HFRS).
The outbreak began in May 1993 after the death of a young Navajo couple within days of each other due to sudden respiratory failure. Medical investigators quickly found other cases with the same symptoms: an initial phase of fever, muscle pain, and variable respiratory symptoms such as coughing, followed by acute respiratory distress. The outbreak reached a peak in July. From May to August, 23 cases had been confirmed in the Four Corners, most of which resulted in death. A thorough investigation into the cause of the outbreak discovered a new hantavirus as the agent responsible. This new virus was named the Sin Nombre virus and its natural reservoir was identified as the Eastern deer mouse (Peromyscus maniculatus). During the outbreak, the Navajo people experienced significant prejudice and discrimination since most cases were among the Navajo.
The 1991–1992 El Niño indirectly caused the outbreak by producing a warmer-than-usual winter and increased rainfall in the spring. This increased the amount of vegetation available for rodents for food and shelter, which in turn led to a 10-fold increase in the rodent population in the Four Corners region in one year, thereby making human-rodent interactions more likely to happen. According to Navajo oral tradition, outbreaks occurred in 1918, 1933, and 1934, all of which were preceded by the same environmental conditions that occurred prior to the 1993 outbreak. A similar increase in cases occurred in 1998.
Since the 1993 outbreak, other hantaviruses that cause HPS have been found in the US and throughout the Americas. Sin Nombre virus remains the most common cause of HPS in North America. Although the disease was feared by many to be contagious during the 1993 outbreak, human-to-human transmission of the Sin Nombre virus has never been observed. Infection remains rare—about 10–50 cases of HPS occur each year in the US, most in spring and early summer and mainly in southwestern states. Infections usually occur at home or in the workplace when inhaling aerosols that contain rodent saliva or excretions. While treatment has improved, HPS still has a case fatality rate of around 40%.
Background
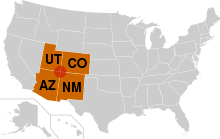
The Four Corners region is the name given to the area where the borders of the US states of Arizona (AZ), Colorado (CO), New Mexico (NM), and Utah (UT) all meet each other. Most of the Four Corners region belongs to Native American nations on reservations, the largest of which is the Navajo Nation, followed by the Hopi, Ute, and Zuni. The area is part of the Colorado Plateau and is characterized by arid, rolling plains with sedimentary rocky features such as mesas, buttes, and canyons. The region is rural: Farmington, New Mexico, the largest city in the region, has a population of around 44,000. The Navajo Nation, which takes up a large portion of the region, has a population of around 165,000 (2020), with a population density of around 6 people per square mile.
Hantaviruses are a family of viruses in the family Hantaviridae. Hantaviruses known to cause disease in humans are all native to rodents and assigned to the genus Orthohantavirus. In general, each species of hantavirus is transmitted primarily by one rodent species. Prior to the 1993 Four Corners outbreak, Old World hantaviruses were known to cause hemorrhagic fever with renal syndrome (HFRS) and a milder form of it called nephropathia epidemica (NE), which had mainly been observed in Asia and Europe. In the Americas, New World hantaviruses that had been identified were not known to infect or cause illness in humans. The 1993 outbreak would mark the first time that a disease caused by New World hantaviruses was identified in the Americas.
Initial cases
On the morning of Friday, May 14, 1993, a 19 year-old Navajo man was riding in the back of a car with his family from Crownpoint, NM to Gallup, NM when he became severely short of breath. They stopped their car at a convenience store in Thoreau, NM, about 30 miles east of Gallup, and contacted emergency services. By the time help had arrived, he had already collapsed due to respiratory failure. An ambulance crew performed CPR as he was taken to the Gallup Indian Medical Center, where he was diagnosed with fluid buildup in the lungs (pulmonary edema), but even with emergency treatment he died. The man had previously visited an outpatient clinic a few days prior due to fever, headache, cough, and muscle pain, which were treated. The death of the young man, a competitive marathon runner, due to sudden respiratory failure confused medical staff.
Because the man's death was highly unusual, it was reported to the New Mexico Office of the Medical Investigator (OMI). The only officer on duty that day was investigator Richard Malone. He had previously investigated a similar death of a 30 year-old Navajo woman a few weeks earlier at the same medical facility. The woman's death, tentatively listed as acute respiratory distress syndrome (ARDS), was investigated in postmortem examination by University of New Mexico pathologist Patricia McFeeley. The woman's lungs were twice as heavy as usual and filled with the clear, yellowish liquid of blood plasma. Tests came back negative for all known diseases that could have caused it. After speaking to Malone, McFeeley performed an autopsy on the man once permission was obtained from the man's family.
Continuing to investigate the cause of the disease, Malone spoke to the family of the deceased man. They told him that they were on their way to the funeral for the man's 21 year-old fiancée and mother of his infant child. She had died just five days earlier at a clinic in Crownpoint with the same symptoms as her fiancé. Since Crownpoint is in the Navajo reservation, the clinic there was not required to report her death to the New Mexico OMI. After contacting McFeeley again and updating her on the situation, Malone convinced the family to have her body examined. McFeeley called the state health department in Santa Fe to report a possible outbreak of an unknown and deadly respiratory illness. The autopsies of the couple conducted by McFeeley showed only severe pulmonary edema with no explanation for the cause of illness.
The investigation expands
Malone then contacted Bruce Tempest, the then medical director at Gallup Indian Medical Center. Tempest recalled having spoken to two physicians who had cared for young, previously healthy tribal members who died suddenly from an unknown respiratory illness. Malone and Tempest agreed that the situation required further action, so they started looking for more cases. Several suspicious cases from prior months were uncovered, including one from November the previous year, and on May 17 they notified the New Mexico Department of Health of their concerns. State officials then sent a letter describing the illness and situation to clinicians in the Four Corners states and asked for any similar cases to be reported to them immediately, which was effective in identifying several more potential cases.
After learning of the situation, the press reported on May 27th that an unexplained illness was killing tribe members in the Four Corners region, causing panic in the public. Navajo and Hopi people were ostracized from the rest of society and politicians were pressured to act. On May 28, NM state officials contacted the Centers for Disease Control and Prevention (CDC) to ask for assistance. Within hours, a team of investigators was assembled. Jay Butler, an epidemiologist at the Epidemic Intelligence Service (EIS) at the CDC, was made the leader and assisted by two EIS officers, Ronald Moolenar and Jeffrey Duchin. Less than 24 hours later, they had arrived to the campus of the University of Mexico and were joined by other professionals to form a team that included people from the CDC, the state health departments of NM, CO, and UT, the Indian Health Service, the Navajo Nation, and the University of New Mexico.
The task force agreed to evaluate any patient in the area from January 1st, 1993 onward who had imaging showing evidence of unexplained excess substances in both lungs (bilateral infiltrate) with low levels of oxygen in the blood (hypoxemia) as well as any case with unexplained pulmonary edema. More than 30 suspected cases were found and various causes were considered. Plague, tularemia, and anthrax, among other diseases, were eliminated due to lack of evidence. The team considered the new disease to either be a new, aggressive form of influenza, an environmental toxin, or a previously unrecognized pathogen.
Hantavirus suspected
On Tuesday, June 1, fifteen members of the CDC team began on-site reviews of medical records, interviewed patient families and control families, inspected homes and workplaces, and obtained samples from suspected cases. After testing at a local laboratory continually yielded no positive results, samples were flown to the CDC in Atlanta, Georgia for immediate analysis. By Friday, June 4, scientists of the Special Pathogens Branch of the CDC had tested IgM antibodies from nine patients with a panel of 25 different virus samples. Antibodies from all 9 patients showed reactivity to three species of hantavirus and none of the other 22 viruses: Hantaan virus, Puumala virus, and Seoul virus. Shortly thereafter, the samples were shown to be reactive to Prospect Hill virus, a hantavirus known to infect voles in Maryland but which had never been isolated from human tissue or associated with human disease.
Some members of the team had experience and knowledge of HFRS, known to be caused by hantaviruses in Asia and Europe. The disease, transmitted to humans from rodents, is characterized by a significant increase in vascular permeability of endothelial cells, mainly in the kidneys, with massive loss of intravascular fluid in the kidneys and surrounding area. The loss of fluid is so severe that the density of blood cells in blood increases due to the loss of liquid (hemoconcentration). Hemoconcentration was observed in several cases and combined with the CDC's findings, a hantavirus was suspected of causing the outbreak.
Suspecting a hantavirus required a substantial leap of thought at the time. Identified hantaviruses in the Western Hemisphere were only known to infect rodents, and no instances of human disease had been described. There were also no known hemorrhagic fevers endemic to North America, and none of the victims had travelled abroad before falling ill. Furthermore, the disease had little renal involvement. The main symptom was respiratory failure in all cases. Nonetheless, an unknown hantavirus that specifically targeted pulmonary capillary endothelial cells was suspected by some members of the investigative team. Acting on this information, the CDC dispatched a rat trapping team to New Mexico on June 7th, who proceeded to capture around 1,700 rodents from June to mid-August at patient and control sites. The most commonly captured rodent was the eastern deer mouse (Peromyscus maniculatus).
Identification of virus and host

At the same time as the rat trapping operation, scientists at the CDC's Special Pathogens Branch worked to identify the new hantavirus. On June 10, reverse transcription polymerase chain reaction (RT-PCR) was used to obtain an RNA sequence from one segment of the virus's genome. The Viral Pathology Laboratory identified hantaviral antigens in the endothelium of the pulmonary capillary bed and other tissues. On June 16, the same team identified an identical viral base pair sequence and prevalence of hantavirus antibody in eastern deer mouse specimens captured in the residence of an initial case, which conclusively identified the virus and its natural reservoir. By late June, testing had shown that about 30% of trapped eastern deer mice and a small number of other rodents were carrying the hantavirus.
Due to difficulties in culturing the virus, it wasn't until November 1993 that teams from the CDC and the US Army Medical Research Institute of Infectious Diseases at Fort Detrick in Frederick, Maryland were able to culture the virus. Initially, the CDC proposed to name the virus the Muerto Canyon virus after a location in the Navajo Reservation. The Navajo strongly opposed any further association with the virus because of the prejudice against them the virus had caused, and the Navajo Nation Council voted unanimously to request the CDC to find an alternative name. Ultimately, the virus was named the Sin Nombre virus, Spanish for the virus with no name.
The Hantavirus Study Group found eighteen people who had either serologic or PCR evidence of infection, most of them young adults. Physical examination of these people showed fever, rapid and shallow breathing (tachypnea), an abnormally fast heart rate (tachycardia), and low blood pressure (hypotension). Severe pulmonary edema was near-ubiquitous. Other symptoms included low oxygen levels in the blood (hypoxemia), higher than normal white blood cell count in the blood (leukocytosis) hemoconcentration, abnormally low platelet levels in the blood (thrombocytopenia), and increased time needed for the liver to produce prothrombin and for blood to clot. The Hantavirus Study Group's findings were published in the April 7, 1994 edition of the New England Journal of Medicine, in which they described the newly defined disease hantavirus pulmonary syndrome.
Course of outbreak
In the weeks following the discovery of the outbreak, a dozen more cases occurred, mostly among the Navajo. The death rate remained high, even for those who made it to the hospital faster than the early victims did. In one case, a person felt fine in the morning but was dead by the end of the day. By late May, the outbreak became more alarming. Two family members of the deceased couple had fallen ill with respiratory illness. On May 22, a medical technician who had assisted McFeeley became ill with fever and muscle aches. The outbreak continued to worsen and reached a peak in July. From May to August, 23 cases of hantavirus had been confirmed in the Four Corners region. 30 cases nationwide had been confirmed, of which 20 resulted in death.
The antiviral drug ribavirin was made available for treatment on June 4 and intravenous ribavirin stocks were provided to health care facilities in the Four Corners region. Intravenous administration of ribavirin had shown some efficacy in treating infections of Hantaan virus, another hantavirus, when provided early in infection, so it was tested experimentally on suspected cases during the outbreak. A toll-free telephone hotline was created by the government to provide updated information about unexplained respiratory illness and to receive calls about suspected hantavirus cases throughout the country. By October, 60 cases of hantaviral disease had been reported nationwide, about half in the Four Corners region. The rest were from California, Texas, Louisiana, Idaho, Nevada, the Dakotas, and Montana. Around 40 of these cases had been confirmed by laboratory, with 25 deaths.
Through December 31, 48 cases were confirmed nationwide, with 27 deaths (56%). Death rates were similar cross age, sex, and race, though most of the infected were male. Of the 33 cases to occur in AZ, CO, and NM in 1993, 25 occurred during the height of the outbreak from April to July and of those 33 people, 17 died (52%). Symptoms of affected persons during the outbreak started with a prodromal phase of fever, muscle pain, and variable respiratory symptoms such as coughing, followed by acute respiratory distress. Other early symptoms reported were headache and gastrointestinal symptoms including abdominal pain, nausea, and vomiting. Hemoconcentration was reported in most cases, as was thrombocytopenia. In all reviewed cases, pulmonary edema developed within two days of hospitalization and during hospitalization, fever, hypoxia, and hypotension occurred.
Social impact
National media flooded the local community with reporters, taking pictures of funerals, printing deceased people's names, and trying to interview victims' families with no respect for the traditional four-day mourning period in Navajo culture. Health officials also failed to respect mourning practices as they continuously probed for information on recent deaths. Residents began posting anti-media signs, and resentment became so severe that some people refused to cooperate with medical investigators. Before the disease's transmission method was confirmed, there was widespread fear of Navajo spreading the disease. This sparked discrimination and racism against the Navajo—some restaurants refused to serve Navajo while in others staff would wear gloves when serving Navajo. The high case fatality rate of the disease only intensified people's fears.
Peterson Zah, the president of the Navajo Nation at the time, was a vocal critic of the sensationalist news coverage of the outbreak and the stigmatization of his community. He said, "The story of Hanta Virus is a perfect example of an intercultural setting and the friction that lies just beneath the surface, and which explodes when unknowing outsiders trample on age-old customs. Deaths and the unknown nature of the illness served only to reinforce stereotypes … the view of Indians as second-class citizens was further supported." Once the disease's connection to rodents was made, many viewed the Navajo as dirty. Some members of the Navajo Nation expressed skepticism toward the government's explanation, instead blaming the outbreak on toxic waste.
Within a month of the outbreak's discovery, it became clear that the disease was not restricted to Navajo or the Four Corners. White and Hispanic victims began to appear in eastern New Mexico and eastern Texas, nowhere near the Four Corners. The popular press by this point had moved on to other news and left the Navajo with the stigma the news had created. Various names for the disease entered public discourse such as Navajo Flu, Navajo Illness, and Four Corners Illness. The CDC's initial proposed name for the virus, Muerto Canyon virus, was problematic given the location's connection to a past Spanish atrocity. After successful pushback from the Navajo, the CDC adopted the name Sin Nombre virus for the newly discovered virus.
Cause of outbreak

A question for the scientific community at the time was why the outbreak occurred. A group of biologists from the University of New Mexico studying the deer mouse population in the Four Corners region during that time period noted that the deer mouse population experienced a 10-fold increase in population from May 1992 to May 1993. Working with environmental scientists, it was demonstrated that the conditions of the 1991–1992 El Niño caused a relatively warm winter and rainy spring. This produced a relative abundance of springtime vegetation in the Four Corners region, which had previously experienced drought for a few years. This provided more shelter and food for local animals, which led to explosive growth in the deer mouse population, thereby increasing the number of interactions between humans and deer mice. The species of deer mouse that carries the Sin Nombre virus, in particular, is more likely to enter human dwellings than other deer mice species.
It is believed that other cases of hantavirus had been occurring regularly but which had simply been diagnosed as ARDS, which is often used as a way to classify unexplainable respiratory failure. Additionally, genetic analysis of the Sin Nombre virus has indicated that it has been indigenous in its natural reservoir since long before the outbreak. The Navajo viewed mice in the home as a source of bad luck and disease, and their oral tradition spoke of past outbreaks in 1918, 1933, and 1934, which they attributed to "disharmony", which leads to excess. Every year that the disease struck had excess rain and snowfall, which led to increased rodent food supply and in turn increased rodent populations and increased human-rodent interactions. Serum samples collected in 1991 and 1992 as part of the Navajo Health and Nutrition Survey were tested and showed that three out of 270 had antibodies to hantavirus, indicative of past infection. The case of a 38 year-old man in Utah in 1959 is the earliest case of HPS to be confirmed by a laboratory.
Aftermath
Following the outbreak, other hantaviruses responsible for HPS were found in the US, including the Bayou virus, Black Creek Canal virus, and New York virus, each associated with an individual rodent species. HPS has since been discovered throughout the Americas, making it a pan-hemispheric disease. Just like in 1993, high precipitation following a severe El Niño in 1998 led to an increase in hantavirus cases in affected areas. Based on environmental models of El Niño oscillations, it is possible to predict when future spikes in hantavirus cases will occur. Winter severity and cone crop productivity especially are predictive of the following year's deer mouse population—harsher winters result in a smaller deer mouse population.
Sin Nombre virus remains the most common cause of HPS in North America. In its rodent host, it causes a chronic and seemingly asymptomatic infection. Sin Nombre virus is primarily associated with one species of deer mouse, and other hantaviruses discovered in North America follow the same pattern, each with their own natural reservoir. In the US, most HPS cases occur in rural areas in southwestern states and almost all infections are contracted by inhalation of aerosols containing rodent excretions at home or in the workplace. About 10–50 cases of HPS occur each year in the US, most in spring and early summer, for a total of around 850 cases from 1993 to 2023 in 39 states. Human-to-human transmission of the Sin Nombre virus has never been recorded, not even among health care workers exposed to infected people and tissues.
Infection is rare but still carries a high case fatality rate of around 40%. Treatment has improved significantly since the outbreak, through means such as extracorporeal membrane oxygenation (ECMO) and preemptively preparing for ECMO upon hospital arrival for anyone suspected of hantavirus infection. The Sin Nombre virus, however, occasionally shows up at unexpected locations. In 2012, a small outbreak occurred at Yosemite National Park in California and claimed the lives of three tourists out of ten infected. No vaccines exist to protect against Sin Nombre virus infection, so the main way to prevent infection is to avoid or minimize contact with mice that carry the virus.
Notes
- No cases were identified in Utah in 1993, the only Four Corners state to not record any cases.
References
- ^ "Geologic Tour of the Colorado Plateau". New Mexico Bureau of Geology & Mineral Resources. New Mexico Institute of Mining and Technology. Retrieved January 4, 2025.
- ^ "Four Corners Region". Southwest Telehealth Resource Center. Retrieved January 4, 2025.
- Klauk E (May 22, 2006). "Physiography of the Navajo Nation". Impacts of Resource Development on American Indian Lands. Carleton College. Retrieved January 4, 2025.
- "About Farmington and the Four Corners". Visit Farmington. Farmington Convention & Visitors Bureau. Retrieved January 4, 2025.
- Navajo Epidemiology Center (July 2024). "Navajo Nation Population Profile U.S. Census 2020" (pdf). Navajo Nation. Retrieved January 4, 2025.
- ^ Chen R, Gong H, Wang X, Sun M, Ji Y, Tan S, Chen J, Shao J, Liao M (August 8, 2023). "Zoonotic Hantaviridae with Global Public Health Significance". Viruses. 15 (8): 1705. doi:10.3390/v15081705. PMC 10459939. PMID 37632047.
- ^ Kuhn JH, Schmaljohn CS (February 28, 2023). "A Brief History of Bunyaviral Family Hantaviridae". Diseases. 11 (1): 38. doi:10.3390/diseases11010038. PMC 10047430. PMID 36975587.
- ^ Van Hook CJ (November 2018). "Hantavirus Pulmonary Syndrome—The 25th Anniversary of the Four Corners Outbreak". Emerg Infect Dis. 24 (11): 2056–2060. doi:10.3201/eid2411.180381. PMC 6199996.
- Centers for Disease Control and Prevention (June 11, 1993). "Outbreak of acute illness--southwestern United States, 1993". MMWR Morb Mortal Wkly Rep. 42 (22): 421–424. PMID 8502213.
- ^ Grady D (May 21, 2019). "Death at the Corners". Discover Magazine. Retrieved January 4, 2025.
- ^ "Tracking a Mystery Disease: The Detailed Story of Hantavirus Pulmonary Syndrome (HPS)". Retrieved January 4, 2025.
- ^ Jacob AT, Ziegler BM, Farha SM, Vivian LR, Zilinski CA, Armstrong AR, Burdette AJ, Beachboard DC, Stobart CC (November 9, 2023). "Sin Nombre Virus and the Emergence of Other Hantaviruses: A Review of the Biology, Ecology, and Disease of a Zoonotic Pathogen". Biology (Basel). 12 (11): 1143. doi:10.3390/biology12111413. PMC 10669331. PMID 37998012.
- ^ Borowski S (January 13, 2013). "The virus that rocked the Four Corners reemerges". American Association For The Advancement of Science. Retrieved January 4, 2025.
- ^ Radcliffe C (June 30, 2021). "The Tragedy of Names". Yale J Biol Med. 94 (2): 375–378. PMC 8223546. PMID 34211356.
- ^ Centers for Disease Control and Prevention (January 28, 1994). "Update: hantavirus pulmonary syndrome--United States, 1993". MMWR Morb Mortal Wkly Rep. 43 (3): 45–48. PMID 8283965.
- Centers for Disease Control and Prevention (CDC) (August 13, 1993). "Update: hantavirus disease--United States, 1993". MMWR Morb Mortal Wkly Rep. 42 (31): 612–614. PMID 8336693.
- ^ Centers for Disease Control and Prevention (June 18, 1993). "Update: outbreak of hantavirus infection--southwestern United States, 1993". MMWR Morb Mortal Wkly Rep. 42 (23): 441–443. PMID 8502218.
- Tappero JW, Khan AS, Pinner RW, Wenger JD, Graber JM, Armstrong LR, Holman RC, Ksiazek TG, Khabbaz RF (February 7, 1996). "Utility of emergency, telephone-based national surveillance for Hantavirus pulmonary syndrome. Hantavirus Task Force". JAMA. 275 (5): 398–400. PMID 8569020.
- ^ "Reported Cases of Hantavirus Disease". Centers for Disease Control and Prevention (CDC). June 26, 2024. Retrieved January 4, 2025.
- Centers for Disease Control and Prevention (October 29, 1993). "Update: hantavirus pulmonary syndrome--United States, 1993". MMWR Morb Mortal Wkly Rep. 42 (42): 816–820. PMID 8413161.
- ^ Pressley, Sue Ann (June 18, 1993). "NAVAJOS PROTEST RESPONSE TO MYSTERY FLU OUTBREAK". The Washington Post. Retrieved January 4, 2025.
- ^ Fimrite P (September 23, 2012). "Hantavirus outbreak puzzles experts". SFGATE. Retrieved January 4, 2025.
- ^ MacDonald J (March 14, 2018). "Solving a Medical Mystery With Oral Traditions". JSTOR Daily. Retrieved January 4, 2025.
- Mather K, Gorman A (September 10, 2012). "Doctors still trying to diagnose mysteries of hantavirus". Los Angeles Times. Retrieved January 4, 2025.
- Warner BM, Dowhanik S, Audet J, Grolla A, Dick D, Strong JE, Kobasa D, Lindsay LR, Kobinger G, Feldmann H, Artsob H, Drebot MA, Safronetz D (December 2020). "Hantavirus Cardiopulmonary Syndrome in Canada". Emerg Infect Dis. 26 (12): 3020–3024. doi:10.3201/eid2612.202808. PMC 7706972. PMID 33219792.
External links
- CDC's Hantavirus Technical Information Index page
- Viralzone: Hantavirus
- Virus Pathogen Database and Analysis Resource (ViPR): Hantaviridae