| Primary mediastinal large B-cell lymphoma | |
|---|---|
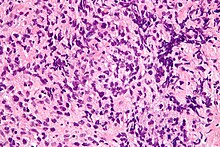 | |
| Micrograph of a primary mediastinal large B-cell lymphoma. H&E stain. | |
| Specialty | Hematology and oncology |
Primary mediastinal B-cell lymphoma, abbreviated PMBL or PMBCL, is a rare type of lymphoma that forms in the mediastinum (the space in between the lungs) and predominantly affects young adults.
While it had previously been considered a subtype of diffuse large B-cell lymphoma;, the World Health Organization no longer classifies it as such, based on distinct clinicopathologic and molecular features.
Pathophysiology
PMLBCL arises from a putative thymic peripheral B cell. It has several distinctive biological features. Molecular analysis shows that PMLBCL is distinct from other types of diffuse large B-cell lymphomas (DLBCL). MAL gene expression is seen in 70%, unlike other diffuse large B-cell lymphomas. Gene expression profiling shows considerable variance from other DLBCLs and similarity to Hodgkin disease.
PMLBCL is CD20 positive, expresses pan-B markers including CD79a, and has clonal immunoglobulin gene rearrangements and mRNA but paradoxically does not express cytoplasmic or cell surface immunoglobulin.
Clinically, PMLBCL is unusual in several respects. Despite 80% PMLBCL being stage I or II, the presenting anterior mediastinal mass is often over 10 cm and is locally invasive of lung, chest wall, pleura, and pericardium. At initial presentation, PMLBCL is usually confined to mediastinum, but its bulk, rather than additional adenopathy, can sometimes be palpated at the low neck. Increased LDH is seen in approximately 75%, but unlike other large cell lymphomas, no increase in beta-2 microglobulin is seen even when bulky which may relate to defective major histocompatibility complex expression.
Diagnosis
Diagnosis requires a biopsy, so that the exact type of tissue can be determined by examination under a microscope. PMBCL is a distinct type of lymphoma that shares some features with both diffuse large B-cell lymphoma, and nodular sclerosing Hodgkin lymphoma (NSHL). Tumors that are even more closely related to NSHL than typical for PMBCL are called gray zone lymphoma.
Treatment
Multiagent chemotherapy is recommended, but the preferred regimen is controversial, as is consolidative radiotherapy.
Treatment commonly begins with either R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisolone) or DA-EPOCH-R (dose-adjusted etoposide, prednisolone, vincristine, cyclophosphamide, doxorubicin, rituximab). Other, more intense, regimens may be more effective. PD-1 and PD-L1 inhibitors can be used.
Radiation therapy may be added, especially if chemotherapy does not seem sufficient on its own. Radiation may cause other health problems later, such as breast cancer, and there is some debate about the best approach to it.
FDG-PET scanning is not as useful for predicting treatment success in PMBCL as it is in other lymphomas.
Prognosis
Most people with PMBCL are successfully treated and survive for many years. However, if the initial treatment is unsuccessful, or if it returns, the long-term prognosis is worse. Relapses generally appear within 12 to 18 months after the completion of treatment.
Epidemiology
This lymphoma is most commonly seen in women between the age of 20 and 40.
See also
References
- Johnson PW, Davies AJ (2008). "Primary mediastinal B-cell lymphoma". Hematology. American Society of Hematology. Education Program. 2008: 349–58. doi:10.1182/asheducation-2008.1.349. PMID 19074109.
- Coso D, Rey J, Bouabdallah R (February 2010). "". Revue de Pneumologie Clinique. 66 (1): 32–5. doi:10.1016/j.pneumo.2009.12.007. PMID 20207294.
- ^ Yu, Yating; Dong, Xifeng; Tu, Meifeng; Wang, Huaquan (November 2021). "Primary mediastinal large B cell lymphoma". Thoracic Cancer. 12 (21): 2831–2837. doi:10.1111/1759-7714.14155. PMC 8563158.
- "Types of Non-Hodgkin Lymphoma". www.cancer.org. Retrieved 2017-09-28.
- "Primary mediastinal large B-cell lymphoma". ashpublications.org/blood/article/140/9/955/476814/Primary-mediastinal-large-B-cell-lymphoma.
- ^ Armitage, JO; Mauch PM; Harris NL; et al. (2010). "Chapter 21". Non-Hodgkin Lymphomas (2nd ed.). Lippincott Williams & Wilkins. ISBN 9780781791168.
- ^ Martelli M, Di Rocco A, Russo E, et al. (2015). "Primary mediastinal lymphoma: diagnosis and treatment options". Expert Rev Hematol. 8 (2): 173–86. doi:10.1586/17474086.2015.994604. hdl:11573/780924. PMID 25537750. S2CID 23040185.
- ^ Jaffe, ES; Harris NL; Vardiman JW; Campo E; Arber DA (2011). Hematopathology (1st ed.). Elsevier Saunders. ISBN 9780721600406.
- Sweetenham, J. Lymphomas (Emerging Cancer Therapeutics V3 I2). Demos. November 2, 2012. ISBN 9781936287789
- ^ Dunleavy K, Wilson WH (January 2015). "Primary mediastinal B-cell lymphoma and mediastinal gray zone lymphoma: do they require a unique therapeutic approach?". Blood. 125 (1): 33–9. doi:10.1182/blood-2014-05-575092. PMC 4281829. PMID 25499450.
- "Non-Hodgkin's Lymphoma" (PDF). Archived from the original (PDF) on May 14, 2005.
- Faris JE, LaCasce AS (2009). "Primary mediastinal large B-cell lymphoma". Clin Adv Hematol Oncol. 7 (2): 125–33. PMID 19367254.
- Dabrowska-Iwanicka A, Walewski JA (2014). "Primary mediastinal large B-cell lymphoma". Curr Hematol Malig Rep. 9 (3): 273–83. doi:10.1007/s11899-014-0219-0. PMC 4180024. PMID 24952250.
- ^ Lees C, Keane C, Gandhi MK, Gunawardana J (February 2019). "Biology and therapy of primary mediastinal B-cell lymphoma: current status and future directions". British Journal of Haematology. 185 (1): 25–41. doi:10.1111/bjh.15778. PMC 6594147. PMID 30740662.
External links
| Classification | D |
|---|---|
| External resources |
| Leukaemias, lymphomas and related disease | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
| Cutaneous lymphoid hyperplasia | |||||||||||||||||||||||||||||||||||||||||||||
| General | |||||||||||||||||||||||||||||||||||||||||||||