"VVF" redirects here. For the health and nutrition charity formerly known as The Vegetarian and Vegan Foundation, see Viva! Health. Medical condition
| Vesicovaginal fistula | |
|---|---|
 | |
| Specialty | Gynaecology |
Vesicovaginal fistula (VVF) is a subtype of female urogenital fistula (UGF).
Presentation
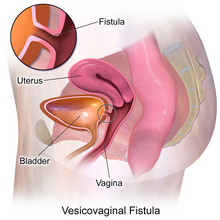
Vesicovaginal fistula, or VVF, is an abnormal fistulous tract extending between the bladder (vesica) and the vagina that allows the continuous involuntary discharge of urine into the vaginal vault.
In addition to the medical sequela from these fistulas, they often have a profound effect on the patient's emotional well-being.
Causes
It may be the result of a congenital birth condition such as VACTERL association. It is often caused by childbirth (in which case it is known as an obstetric fistula), when a prolonged labor presses the unborn child tightly against the pelvis, cutting off blood flow to the vesicovaginal wall. The affected tissue may necrotize (die), leaving a hole.
Vaginal fistulas can also result from particularly violent cases of rape, especially those involving multiple rapists and/or foreign objects. Some health centers in countries such as the Democratic Republic of Congo have begun to specialize in the surgical repair of vaginal fistulas. It can also be associated with hysterectomy, cancer operations, radiation therapy and cone biopsy.
Treatment
Vesicovaginal fistulae are typically repaired either transvaginally or laparoscopically, although patients who have had multiple transvaginal procedures sometimes attempt a final repair through a large abdominal incision, or laparotomy.
The laparoscopic (minimally invasive) approach to VVF repair has become more prevalent due to its greater visualization, higher success rate, and lower rate of complications.
Possible complications of surgical treatment
- Recurrent formation of the fistula
- Injury to ureter, bowel, or intestines
- Vaginal shortening
History
Before the 19th century, women who suffered from VVF were judged harshly and rejected by society. Throughout the 19th century, treatment for VVF was limited because the practice of gynecology was perceived as taboo. Doctors were almost entirely male at this time and looking at a nude female, even for medical purposes, was seen as divergent from 19th-century values.
One of the most famous gynecological surgeons of this time was Dr. J. Marion Sims, who developed a successful technique for treating VVF in the mid-1800s, for which he is hailed as a pioneer of gynecology.
Black enslaved women in the American South were particularly prone to VVF because they were denied proper nutrients and medical care. Sims performed on these women without anesthesia, which had not been introduced until after he started his experiments, and which in its infancy Sims hesitated to use. (Ether anesthesia was publicly demonstrated in Boston in 1846, a year after Sims began his experimentation.) Sims did not have a white female patient until he made ether available to them, although he publicly noted that he never resorted to using anesthetics because he believed that the pain did not justify the risks. A detailed case study of Sims even discusses the case of a white woman who underwent three operations, all without anesthesia. It was considered acceptable to operate on them without anesthetic because, Sims claimed, African-American women have a naturally higher pain tolerance.
The healing process of the VVF procedure is still arduous. To have a successful recovery from the surgery, it must be successful on the first attempt. Sims's operations on African-American enslaved women showcase the dangerous nature of the procedure. There still have not been clear instructions on how to properly recover from the procedure other than taking prescribed antibiotics.
See also
References
- Bhatia J (8 January 2010). "Rape epidemic fuels fistula cases in the Democratic Republic of Congo". Conversations for a Better World. Archived from the original on 28 August 2010.
- Nordland R (12 November 2006). "Congo: More Vicious Than Rape". Newsweek.
- Kochakarn W, Pummangura W (October 2007). "A new dimension in vesicovaginal fistula management: an 8-year experience at Ramathibodi hospital". Asian Journal of Surgery. 30 (4): 267–71. doi:10.1016/S1015-9584(08)60037-8. PMID 17962130.
- Miklos JR (20 October 2010). "Fistula Repair Overview". Bladder - Vaginal Fistula Surgeons. Retrieved 11 September 2013.
- Miklos JR, Sobolewski C, Lucente V (1999). "Laparoscopic management of recurrent vesicovaginal fistula" (PDF). International Urogynecology Journal and Pelvic Floor Dysfunction. 10 (2): 116–7. doi:10.1007/s001920050029. PMID 10384974. S2CID 21633111. Archived from the original (PDF) on 6 August 2013.
- Ojanuga D (March 1993). "The medical ethics of the 'father of gynaecology', Dr J Marion Sims". Journal of Medical Ethics. 19 (1): 28–31. doi:10.1136/jme.19.1.28. PMC 1376165. PMID 8459435.
- ^ Wall LL (June 2006). "The medical ethics of Dr J. Marion Sims: a fresh look at the historical record". Journal of Medical Ethics. 32 (6): 346–50. doi:10.1136/jme.2005.012559. PMC 2563360. PMID 16731734.
- Spettel S, White MD (June 2011). "The portrayal of J. Marion Sims' controversial surgical legacy". The Journal of Urology. 185 (6): 2424–7. doi:10.1016/j.juro.2011.01.077. PMID 21511295.
- ^ Stamatakos, M., Sargedi, C., Stasinou, T., & Kontzoglou, K. (2014). Vesicovaginal Fistula: Diagnosis and Management. The Indian Journal of Surgery, 76(2), 131–136. http://doi.org/10.1007/s12262-012-0787-y
External links
| Classification | D |
|---|---|
| External resources |
| Reproductive health |
| ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sexual health |
| ||||||||||||||||
| Non-reproductive health |
| ||||||||||||||||
| Sociocultural factors |
| ||||||||||||||||
| Politics, research and advocacy |
| ||||||||||||||||
| Women's health by country |
| ||||||||||||||||
| Female diseases of the pelvis and genitals | |||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Internal |
| ||||||||||||||||||||||||||||||||||||
| External |
| ||||||||||||||||||||||||||||||||||||
| Female genital mutilation | |||||||
|---|---|---|---|---|---|---|---|
| Health issues | |||||||
| By country | |||||||
| Writers/groups |
| ||||||
| Media |
| ||||||
| Legislation | |||||||
| Categories | |||||||