| Revision as of 06:42, 24 July 2007 editNaomiAmethyst (talk | contribs)Edit filter managers, Extended confirmed users, Rollbackers, Template editors6,269 edits Undid revision 146710293 by 210.4.37.47 (talk) Vandalism← Previous edit | Latest revision as of 07:59, 6 January 2025 edit undoOAbot (talk | contribs)Bots441,761 editsm Open access bot: doi, hdl updated in citation with #oabot. | ||
| Line 1: | Line 1: | ||
| {{short description|Inflammatory disease involving buildup of lesions in the walls of arteries}} | |||
| {{DiseaseDisorder infobox | | |||
| {{distinguish|Arteriosclerosis}} | |||
| Name = Atherosclerosis | | |||
| {{For|the journal|Atherosclerosis (journal)}} | |||
| Image = Endo dysfunction Athero.PNG | | |||
| {{Infobox medical condition (new) | |||
| Caption = Changes in endothelial dysfunction in atherosclerosis (note text comments about geometry error) | | |||
| | name = Atherosclerosis | |||
| DiseasesDB = 1039 | | |||
| | synonyms = Arteriosclerotic vascular disease (ASVD) | |||
| ICD10 = {{ICD10|I|70||i|70}} | | |||
| | image = Atherosclerosis timeline - endothelial dysfunction.svg | |||
| ICD9 = {{ICD9|440}} | | |||
| | caption = The progression of atherosclerosis (narrowing exaggerated) | |||
| MedlinePlus = | | |||
| | field = ], ] | |||
| eMedicineSubj = med | | |||
| | symptoms = None<ref name=NIH2016Sym/> | |||
| eMedicineTopic = 182 | | |||
| | complications = ], ], ], ]<ref name=NIH2016Sym/> | |||
| | onset = Youth (worsens with age)<ref name=NIH2016Cau/> | |||
| | duration = | |||
| | causes = Accumulation of saturated fats, smoking, high blood pressure, and diabetes | |||
| | risks = ], ], ], ], family history, unhealthy diet (notably ]), chronic ] deficiency<ref>{{Cite web|title= New Concept of Heart Disease Posits Vitamin C Deficiency as Culprit |url= https://www.dicardiology.com/article/new-concept-heart-disease-posits-vitamin-c-deficiency-culprit |access-date=2022-02-06|website=DAIC (Diagnostic and Interventional Cardiology) |date= 27 April 2015 |language=en}}</ref><ref name=NIH2016Risk/> | |||
| | diagnosis = | |||
| | differential = | |||
| | prevention = ], exercise, not smoking, maintaining a normal weight<ref name=NIH2016Pre/> | |||
| | treatment = | |||
| | medication = ]s, ], ]<ref name=NIH2016Tx/> | |||
| | prognosis = | |||
| | frequency = ≈100% (>65 years old)<ref name=AR2013/> | |||
| | deaths = | |||
| }} | }} | ||
| <!-- Definition and symptoms --> | |||
| '''Atherosclerosis''' is a ] affecting ] ]s. It is a chronic inflammatory response in the walls of arteries, in large part to the deposition of lipoproteins (plasma proteins that carry cholesterol and triglycerides). It is commonly referred to as a "hardening" or "furring" of the arteries. It is caused by the formation of multiple ] within the arteries. | |||
| '''Atherosclerosis'''{{efn|Also '''arteriosclerotic vascular disease''' ('''ASVD''')}} is a pattern of the disease ],<ref>{{Cite web|title=Arteriosclerosis / atherosclerosis - Symptoms and causes|url=https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569|access-date=2021-05-06|website=Mayo Clinic|language=en}}</ref> characterized by development of abnormalities called ]s in walls of ]. This is a chronic inflammatory disease involving many different cell types and driven by elevated levels of cholesterol in the blood.<ref name=cas>{{Cite journal |last1=Scipione |first1=Corey A. |last2=Hyduk |first2=Sharon J. |last3=Polenz |first3=Chanele K. |last4=Cybulsky |first4=Myron I. |date=December 2023 |title=Unveiling the Hidden Landscape of Arterial Diseases at Single-Cell Resolution |url=https://linkinghub.elsevier.com/retrieve/pii/S0828282X2301663X |journal=Canadian Journal of Cardiology |language=en |volume=39 |issue=12 |pages=1781–1794 |doi=10.1016/j.cjca.2023.09.009|pmid=37716639 }}</ref> These lesions may lead to narrowing of the arterial walls due to buildup of ]s.<ref name=NIH2016Def>{{cite web|title=What Is Atherosclerosis? - NHLBI, NIH|url=https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis|website=www.nhlbi.nih.gov|access-date=6 November 2017|language=en|date=22 June 2016}}</ref><ref>{{Cite journal |last1=Tsukahara |first1=Tamotsu |last2=Tsukahara |first2=Ryoko |last3=Haniu |first3=Hisao |last4=Matsuda |first4=Yoshikazu |last5=Murakami-Murofushi |first5=Kimiko |date=2015-09-05 |title=Cyclic phosphatidic acid inhibits the secretion of vascular endothelial growth factor from diabetic human coronary artery endothelial cells through peroxisome proliferator-activated receptor gamma |journal=Molecular and Cellular Endocrinology |language=en |volume=412 |pages=320–329 |doi=10.1016/j.mce.2015.05.021 |pmid=26007326 |hdl=10069/35888 |hdl-access=free }}</ref> At the onset there are usually no symptoms, but if they develop, symptoms generally begin around middle age.<ref name=NIH2016Sym>{{cite web|title=What Are the Signs and Symptoms of Atherosclerosis? - NHLBI, NIH|url=https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/signs|website=www.nhlbi.nih.gov|access-date=5 November 2017|language=en|date=22 June 2016}}</ref> In severe cases, it can result in ], ], ], or ]s, depending on which body part(s) the affected arteries are located in the body.<ref name=NIH2016Sym/> | |||
| <!-- Cause and diagnosis --> | |||
| ], the ''']''' is divided into three distinct components: | |||
| The exact cause of atherosclerosis is unknown and is proposed to be multifactorial.<ref name=NIH2016Sym/> Risk factors include ], elevated levels of ]s,<ref>{{cite journal | vauthors = Lind L | title = Circulating markers of inflammation and atherosclerosis | journal = Atherosclerosis | volume = 169 | issue = 2 | pages = 203–214 | date = August 2003 | pmid = 12921971 | doi = 10.1016/s0021-9150(03)00012-1 }}</ref> ], ], ] (both active and ]), ], genetic factors, family history, lifestyle habits, and an unhealthy diet.<ref name=NIH2016Risk>{{cite web | title = Who Is at Risk for Atherosclerosis? | url = https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/atrisk |website=www.nhlbi.nih.gov|access-date=5 November 2017|language=en|date=22 June 2016 }}</ref> ] is made up of fat, ], immune cells, ], and other substances found in the ].<ref name=NIH2016Def/><ref name="cas"/> The narrowing of ] limits the flow of oxygen-rich blood to parts of the body.<ref name=NIH2016Def/> Diagnosis is based upon a physical exam, ], and ], among others.<ref name=NIH2016Diag>{{cite web|title=How Is Atherosclerosis Diagnosed? - NHLBI, NIH|url=https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/diagnosis|website=www.nhlbi.nih.gov|access-date=6 November 2017|language=en|date=22 June 2016}}</ref> | |||
| # The '']'' ("lump of porridge", from ''Athera'', ] in Greek,) is the nodular accumulation of a soft, flaky, yellowish material at the center of large plaques, composed of ]s nearest the ] of the artery. | |||
| # Underlying areas of ] crystals. | |||
| # Calcification at the outer base of older/more advanced lesions. | |||
| <!-- Prevention and treatment --> | |||
| The following terms are similar, yet distinct, in both spelling and meaning, and can be easily confused: arteriosclerosis, arteriolosclerosis and atherosclerosis. '''Arteriosclerosis''' is a general term describing any hardening (and loss of elasticity) of medium or large arteries (in Greek, "Arterio" meaning artery and "sclerosis" meaning hardening), '''arteriolosclerosis''' is arteriosclerosis mainly affecting the ]s (small arteries), '''atherosclerosis''' is a hardening of an artery specifically due to an atheromatous plaque. Therefore, atherosclerosis is a form of arteriosclerosis. | |||
| Prevention guidelines include eating a ], exercising, not smoking, and maintaining normal body weight.<ref name=NIH2016Pre>{{cite web|title=How Can Atherosclerosis Be Prevented or Delayed? - NHLBI, NIH|url=https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/prevention|website=www.nhlbi.nih.gov|access-date=6 November 2017|language=en|date=22 June 2016}}</ref> Treatment of established atherosclerotic disease may include medications to lower ] such as ]s, ], and anticoagulant therapies to reduce the risk of blood clot formation.<ref name=NIH2016Tx/> As the disease state progresses more invasive strategies are applied such as ], ], or ].<ref name=NIH2016Tx>{{cite web|title=How Is Atherosclerosis Treated? - NHLBI, NIH|url=https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/treatment|website=www.nhlbi.nih.gov|access-date=6 November 2017|language=en|date=22 June 2016}}</ref> Genetic factors are also strongly implicated in the disease process; it is unlikely to be entirely based on lifestyle choices.<ref>{{cite book |last1=Information (US) |first1=National Center for Biotechnology |title=Genes and Disease |date=1998 |publisher=National Center for Biotechnology Information (US) |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK22171/ |chapter=Atherosclerosis }}</ref> | |||
| <!-- Epidemiology --> | |||
| '''Arteriosclerosis''' ("hardening of the artery") results from a deposition of tough, rigid ] inside the vessel wall and around the atheroma. This increases the stiffness, decreases the elasticity of the artery wall. '''Arteriolosclerosis''' (hardening of small arteries, the ]s) is the result of collagen deposition, but also muscle wall thickening and deposition of protein ("hyaline"). | |||
| Atherosclerosis generally starts when a person is young and worsens with age. Females are 78% at higher risk level than men<ref name=NIH2016Cau>{{cite web|title=What Causes Atherosclerosis? - NHLBI, NIH|url=https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/causes|website=www.nhlbi.nih.gov|access-date=6 November 2017|language=en|date=22 June 2016}}</ref> Almost all people are affected to some degree by the age of 65.<ref name=AR2013>{{cite book| vauthors = Aronow WS, Fleg JL, Rich MW |title=Tresch and Aronow's Cardiovascular Disease in the Elderly, Fifth Edition|date=2013|publisher=CRC Press|isbn=978-1-84214-544-9 |pages=171|url=https://books.google.com/books?id=OrbNBQAAQBAJ&pg=PA171|language=en}}</ref> It is the number one ] and ] in ].<ref>{{cite journal | vauthors = Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro AL, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V | display-authors = 6 | title = Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study | journal = Journal of the American College of Cardiology | volume = 76 | issue = 25 | pages = 2982–3021 | date = December 2020 | pmid = 33309175 | pmc = 7755038 | doi = 10.1016/j.jacc.2020.11.010 }}</ref><ref>{{cite journal | vauthors = Song P, Fang Z, Wang H, Cai Y, Rahimi K, Zhu Y, Fowkes FG, Fowkes FJ, Rudan I | display-authors = 6 | title = Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study | language = English | journal = The Lancet. Global Health | volume = 8 | issue = 5 | pages = e721–e729 | date = May 2020 | pmid = 32353319 | doi = 10.1016/S2214-109X(20)30117-0 | doi-access = free | hdl = 10044/1/78967 | hdl-access = free }}</ref><ref>{{cite book| vauthors = Topol EJ, Califf RM |title=Textbook of Cardiovascular Medicine|date=2007|publisher=Lippincott Williams & Wilkins|isbn=978-0-7817-7012-5 |pages=2|url=https://books.google.com/books?id=35zSLWyEWbcC&pg=PA2|language=en}}</ref> Though it was first described in 1575,<ref name="Al2008">{{cite book |doi=10.1007/978-1-84628-810-4 |title=Chlamydia Atherosclerosis Lesion |date=2007 |isbn=978-1-84628-809-8 |first1=Allan |last1=Shor |page=8 }}</ref> there is evidence suggesting that this disease state is genetically inherent in the broader human population, with its origins tracing back to genetic mutations that may have occurred more than two million years ago during the evolution of hominin ancestors of modern human beings.<ref>{{cite news |title=Evolutionary gene loss may help explain why only humans are prone to heart attacks |url=https://www.sciencedaily.com/releases/2019/07/190723182255.htm |work=ScienceDaily |publisher=University of California - San Diego |date=23 July 2019 }}</ref> | |||
| {{TOC limit|3}} | |||
| ==Signs and symptoms== | |||
| ], sometimes even ] (formation of complete bone tissue) occurs within the deepest and oldest layers of the ] vessel wall. | |||
| Atherosclerosis is typically ] for decades because the arteries enlarge at all plaque locations, thus there is no effect on blood flow.<ref name="Ross1993">{{cite journal | vauthors = Ross R | title = The pathogenesis of atherosclerosis: a perspective for the 1990s | journal = Nature | volume = 362 | issue = 6423 | pages = 801–9 | date = April 1993 | pmid = 8479518 | doi = 10.1038/362801a0 | bibcode = 1993Natur.362..801R }}</ref> Even most ] do not produce symptoms until enough narrowing or closure of an artery, due to ], occurs. Signs and symptoms only occur after severe narrowing or closure impedes blood flow to different organs enough to induce symptoms.<ref>Atherosclerosis. Harvard Health Publications Harvard Health Publications. Health Topics A – Z, (2011)</ref> Most of the time, patients realize that they have the disease only when they experience other ] such as ] or ]. These symptoms, however, still vary depending on which artery or organ is affected.<ref name="nhlbi.nih.gov">{{cite web | title = Atherosclerosis | publisher = National Heart, Lung and Blood Institute | url = http://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/signs.html | year = 2011 }}</ref> | |||
| Early atherosclerotic processes likely begin in childhood. Fibrous and gelatinous lesions have been observed in the ] of children.<ref name="Velican & Velican 1979">{{cite journal | vauthors = Velican D, Velican C | title = Study of fibrous plaques occurring in the coronary arteries of children | journal = Atherosclerosis | volume = 33 | issue = 2 | pages = 201–205 | date = June 1979 | pmid = 475879 | doi = 10.1016/0021-9150(79)90117-5 }}</ref> ]s have been observed in the coronary arteries of juveniles.<ref name="Velican & Velican 1979" /> While ] is more prevalent in men than women, atherosclerosis of the ] and strokes equally affect both sexes.<ref name="pmid5697685">{{cite journal | vauthors = Flora GC, Baker AB, Loewenson RB, Klassen AC | title = A comparative study of cerebral atherosclerosis in males and females | journal = Circulation | volume = 38 | issue = 5 | pages = 859–69 | date = November 1968 | pmid = 5697685 | doi = 10.1161/01.CIR.38.5.859| doi-access = free }}</ref> | |||
| Atherosclerosis causes two main problems. First, the ], though long compensated for by artery enlargement, eventually lead to plaque ruptures and ''stenosis'' (narrowing) of the artery and, therefore, an insufficient blood supply to the organ it feeds. Alternatively, if the compensating artery enlargement process is excessive, then a net ] results. | |||
| ] in the coronary arteries, which are responsible for bringing oxygenated blood to the heart, can produce symptoms such as chest pain of ] and shortness of breath, sweating, ], dizziness or lightheadedness, breathlessness or ].<ref name="nhlbi.nih.gov"/> Abnormal heart rhythms called ]s—the heart beating either too slowly or too quickly—are another consequence of ].<ref name="heartandstroke.com">Arrhythmia. Heart and Stroke Foundation. {{cite web |url=http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.3484057/ |title=Heart disease - Arrhythmia - Heart and Stroke Foundation of Canada |access-date=2014-01-31 |url-status=dead |archive-url=https://web.archive.org/web/20140203120532/http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.3484057/ |archive-date=2014-02-03 }} (2011)</ref> | |||
| These complications are chronic, slowly progressing and cumulative. Most commonly, soft plaque suddenly ''ruptures'' (see ]), causing the formation of a thrombus that will rapidly slow or stop blood flow, e.g. 5 minutes, leading to death of the tissues fed by the artery. This catastrophic event is called an '']''. One of the most common recognized scenarios is called ] of a ] causing ] (a heart attack). Another common scenario in very advanced disease is '']'' from insufficient blood supply to the legs, typically due to a combination of both stenosis and aneurysmal segments narrowed with ]. Since atherosclerosis is a body wide process, similar events also occur in the arteries to the brain, intestines, kidneys, legs, etc. | |||
| ] supply blood to the brain and neck.<ref name="heartandstroke.com"/> Marked narrowing of the carotid arteries can present with symptoms such as a feeling of weakness; being unable to think straight; difficulty speaking; dizziness; difficulty in walking or standing up straight; blurred vision; numbness of the face, arms and legs; severe headache; and loss of consciousness. These symptoms are also related to stroke (death of brain cells). Stroke is caused by marked narrowing or closure of arteries going to the brain; lack of adequate blood supply leads to the death of the cells of the affected tissue.<ref>{{cite journal |last1=Sims |first1=Neil R. |last2=Muyderman |first2=Hakan |title=Mitochondria, oxidative metabolism and cell death in stroke |journal=Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease |date=January 2010 |volume=1802 |issue=1 |pages=80–91 |doi=10.1016/j.bbadis.2009.09.003 |pmid=19751827 }}</ref> | |||
| ==Symptoms== | |||
| Atherosclerosis typically begins in early adolescence, and is usually found in most major ], yet is asymptomatic and not detected by most diagnostic methods during life. Autopsies of healthy young men who died during the Korean and Vietnam Wars showed evidence of the disease. It most commonly becomes seriously symptomatic when interfering with the ] supplying the ] or ] supplying the ], and is considered the most important underlying cause of ], ]s, various ]s including ] and most ]s in general. Atheroma in arm or more often leg arteries and producing decreased blood flow is called ] (PAOD). | |||
| ], which supply blood to the legs, arms, and pelvis, also experience marked narrowing due to plaque rupture and clots. Symptoms of the narrowing are pain and numbness within the arms or legs. Another significant location for plaque formation is the ], which supply blood to the kidneys. Plaque occurrence and accumulation lead to decreased kidney blood flow and ], which, like in all other areas, is typically asymptomatic until late stages.<ref name="nhlbi.nih.gov"/> | |||
| According to United States data for the year 2004, for about 65% of men and 47% of women, the first ] of atherosclerotic ] is ] or ] (death within one hour of onset of the symptom). | |||
| In 2004, US data indicated that in ~66% of men and ~47% of women, the first symptom of atherosclerotic cardiovascular disease was a ] or ] (defined as death within one hour of onset of the symptom).<ref>{{cite book |doi=10.1007/978-0-387-78665-0_51 |chapter=Atherosclerotic Burden and Mortality |title=Handbook of Disease Burdens and Quality of Life Measures |date=2010 |last1=Roquer |first1=J. |last2=Ois |first2=Angel |pages=899–918 |isbn=978-0-387-78664-3 }}</ref> | |||
| Most artery flow disrupting events occur at locations with less than 50% ] narrowing (~20% ] is average. trial, the ] photographs on page 8, as examples for a more accurate understanding.] The relative geometry error within the illustration is common to many older illustrations, an error slowly being more commonly recognized within the last decade. | |||
| Case studies have included ] of U.S. soldiers killed in ] and the ]. A much-cited report involved the autopsies of 300 U.S. soldiers killed in Korea. Although the average age of the men was 22.1 years, 77.3 percent had "gross evidence of coronary arteriosclerosis".<ref name=Enos>{{cite journal |vauthors=Enos WF, Holmes RH, Beyer J |title= Coronary disease among United States soldiers killed in action in Korea: Preliminary Report |journal= JAMA |volume=152 |issue=12 |pages= 1090–93 |year=1953 |doi=10.1001/jama.1953.03690120006002 |pmid= 13052433 }} The average age was calculated from the ages of 200 of the soldiers. No age was recorded in nearly 100 of the men.</ref> | |||
| ]ing, traditionally the most commonly performed non-invasive testing method for blood flow limitations generally only detects ] narrowing of ~75% or greater, although some physicians advocate that nuclear stress methods can detect as little as 50%. | |||
| ==Risk factors== | |||
| ==Atherogenesis==<!-- This section is linked from ] --> | |||
| {{See also|Lipoprotein|Lipoprotein (a)}} | |||
| ''Atherogenesis'' is the developmental process of atheromatous plaques. It is characterized by a remodeling of ] involving the concomitant accumulation of fatty substances called plaques. One recent theory suggests that for unknown reasons, ] such as ] or ] begin to attack the ] of the artery lumen in cardiac muscle. The ensuing ] leads to formation of ''atheromatous plaques'' in the arterial intima, a region of the vessel wall located between the ] and the ] and ]. The bulk of these lesions are made of excess fat, ], and ]. The plaques initially grow without producing any narrowing, ], of the artery opening, called the lumen. | |||
| ] | |||
| The atherosclerotic process is not well understood.{{update inline|date=November 2024}} Atherosclerosis is associated with inflammatory processes in the ] of the vessel wall associated with retained ] (LDL) particles.<ref name="li-2016">{{cite journal | vauthors = Li X, Fang P, Li Y, Kuo YM, Andrews AJ, Nanayakkara G, Johnson C, Fu H, Shan H, Du F, Hoffman NE, Yu D, Eguchi S, Madesh M, Koch WJ, Sun J, Jiang X, Wang H, Yang X | title = Mitochondrial Reactive Oxygen Species Mediate Lysophosphatidylcholine-Induced Endothelial Cell Activation | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 36 | issue = 6 | pages = 1090–100 | date = June 2016 | pmid = 27127201 | pmc = 4882253 | doi = 10.1161/ATVBAHA.115.306964 }}</ref><ref name="botts-2021">{{cite journal | vauthors = Botts SR, Fish JE, Howe KL | title = Dysfunctional Vascular Endothelium as a Driver of Atherosclerosis: Emerging Insights Into Pathogenesis and Treatment | journal = Frontiers in Pharmacology | volume = 12 | pages = 787541 | date = December 2021 | pmid = 35002720 | pmc = 8727904 | doi = 10.3389/fphar.2021.787541 | doi-access = free }}</ref> This retention may be a cause, an effect, or both, of the underlying inflammatory process.<ref>{{cite journal | vauthors = Williams KJ, Tabas I | title = The response-to-retention hypothesis of early atherogenesis | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 15 | issue = 5 | pages = 551–61 | date = May 1995 | pmid = 7749869 | pmc = 2924812 | doi = 10.1161/01.ATV.15.5.551 }}</ref> | |||
| ===Cellular=== | |||
| The first step of atherogenesis is the development of ]s, small subendothelial deposits of lipid. The exact cause for this process is unknown, and fatty streaks may appear and disappear. | |||
| The presence of the plaque induces the ] of the blood vessel to stretch, compensating for the additional bulk. The endothelial lining then thickens, increasing the separation between the plaque and lumen. The thickening somewhat offsets the narrowing caused by the growth of the plaque, but moreover, it causes the wall to stiffen and become less compliant to stretching with each heartbeat.<ref>{{cite journal | vauthors = Aviram M, Fuhrman B | title = LDL oxidation by arterial wall macrophages depends on the oxidative status in the lipoprotein and in the cells: role of prooxidants vs. antioxidants | journal = Molecular and Cellular Biochemistry | volume = 188 | issue = 1–2 | pages = 149–59 | date = November 1998 | pmid = 9823020 | doi = 10.1023/A:1006841011201 }}</ref> | |||
| LDL in blood plasma poses a risk for ] when it invades the ] and becomes ]d. A complex set of biochemical reactions regulates the oxidation of LDL, chiefly stimulated by presence of ] in the ] or blood vessel lining. | |||
| === Modifiable === | |||
| The initial damage to the blood vessel wall results in a "call for help," an ] response. ]s (a type of ]) enter the artery wall from the bloodstream, with platelets adhering to the area of insult. This may be promoted by ] induction of factors such as ], which recruit circulating monocytes. The ]s differentiate into ]s, which ingest ]d ], slowly turning into large "foam cells" – so-described because of their changed appearance resulting from the numerous internal cytoplasmic ]s and resulting high ] content. Under the microscope, the lesion now appears as a fatty streak. Foam cells eventually die, and further propagate the inflammatory process. | |||
| * ]<ref name=nhlbi.nih>{{Cite web|url=https://www.nhlbi.nih.gov/health/health-topics/topics/atherosclerosis/atrisk|title = Atherosclerosis | NHLBI, NIH| date=24 March 2022 }}</ref> | |||
| There is also smooth muscle proliferation and migration from tunica media to intima responding to cytokines secreted by damaged endothelial cells. This would cause the formation of a fibrous capsule covering the fatty streak. | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref name="pmid26004263">{{cite journal | vauthors = Campbell LA, Rosenfeld ME | title = Infection and Atherosclerosis Development | journal = Arch Med Res | volume = 46 | issue = 5 | pages = 339–50 | date = July 2015 | pmid = 26004263 | pmc = 4524506 | doi = 10.1016/j.arcmed.2015.05.006 }}</ref> | |||
| * ]<ref>{{cite journal | vauthors = Sinha A, Feinstein MJ | title = Coronary Artery Disease Manifestations in HIV: What, How, and Why | journal = The Canadian Journal of Cardiology | volume = 35 | issue = 3 | pages = 270–279 | date = March 2019 | pmid = 30825949 | doi = 10.1016/j.cjca.2018.11.029 | pmc = 9532012 }}</ref> | |||
| === Nonmodifiable === | |||
| * ] descent<ref>{{cite journal | vauthors = Enas EA, Kuruvila A, Khanna P, Pitchumoni CS, Mohan V | title = Benefits & risks of statin therapy for primary prevention of cardiovascular disease in Asian Indians - a population with the highest risk of premature coronary artery disease & diabetes | journal = The Indian Journal of Medical Research | volume = 138 | issue = 4 | pages = 461–91 | date = October 2013 | pmid = 24434254 | pmc = 3868060 }}</ref><ref name="Indian Heart">Indian Heart Association Why South Asians Facts Web. 30 April 2015. http://indianheartassociation.org/why-indians-why-south-asians/overview/</ref> | |||
| * ]<ref name=nhlbi.nih/><ref>{{cite journal | vauthors = Tyrrell DJ, Blin MB, Song J, Wood SC, Zhang M, Beard DA, Goldstein DR | title = Age-Associated Mitochondrial Dysfunction Accelerates Atherogenesis | journal = Circulation Research | volume = 126 | issue = 3 | pages = 298–314 | date = January 2020 | pmid = 31818196 | pmc = 7006722 | doi = 10.1161/CIRCRESAHA.119.315644 }}</ref> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * Family history<ref name=nhlbi.nih/> | |||
| * Coronary anatomy and branch pattern<ref>{{cite journal | vauthors = Velican C, Velican D | title = Differences in the pattern of atherosclerotic involvement between non-branched regions and adjacent branching points of human coronary arteries | journal = Atherosclerosis | volume = 54 | issue = 3 | pages = 333–342 | date = March 1985 | pmid = 3994786 | doi = 10.1016/0021-9150(85)90126-1 }}</ref> | |||
| === Lesser or uncertain === | |||
| * ]<ref>{{cite journal | vauthors = Borissoff JI, Spronk HM, Heeneman S, ten Cate H | title = Is thrombin a key player in the 'coagulation-atherogenesis' maze? | journal = Cardiovascular Research | volume = 82 | issue = 3 | pages = 392–403 | date = June 2009 | pmid = 19228706 | doi = 10.1093/cvr/cvp066 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Borissoff JI, Heeneman S, Kilinç E, Kassák P, Van Oerle R, Winckers K, Govers-Riemslag JW, Hamulyák K, Hackeng TM, Daemen MJ, ten Cate H, Spronk HM | title = Early atherosclerosis exhibits an enhanced procoagulant state | journal = Circulation | volume = 122 | issue = 8 | pages = 821–30 | date = August 2010 | pmid = 20697022 | doi = 10.1161/CIRCULATIONAHA.109.907121 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Borissoff JI, Spronk HM, ten Cate H | title = The hemostatic system as a modulator of atherosclerosis | journal = The New England Journal of Medicine | volume = 364 | issue = 18 | pages = 1746–60 | date = May 2011 | pmid = 21542745 | doi = 10.1056/NEJMra1011670 }}</ref> | |||
| * ]<ref name=nhlbi.nih/><ref>{{Cite book|last = Food and nutrition board, institute of medicine of the national academies | title = Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) | publisher = National Academies Press | year = 2005 | pages = 481–484 | doi = 10.17226/10490 | isbn = 978-0-309-08525-0 | url = http://www.nap.edu/openbook.php?record_id=10490&pages=481}}</ref> | |||
| * Excessive ]s<ref name=nhlbi.nih/><ref>{{cite journal | vauthors = Mozaffarian D, Rimm EB, Herrington DM | title = Dietary fats, carbohydrate, and progression of coronary atherosclerosis in postmenopausal women | journal = The American Journal of Clinical Nutrition | volume = 80 | issue = 5 | pages = 1175–84 | date = November 2004 | pmid = 15531663 | pmc = 1270002 | doi = 10.1093/ajcn/80.5.1175 }}</ref> | |||
| * Elevated ]<ref name=nhlbi.nih/> | |||
| * ]<ref name=Bhatt>{{cite journal | vauthors = Bhatt DL, Topol EJ | title = Need to test the arterial inflammation hypothesis | journal = Circulation | volume = 106 | issue = 1 | pages = 136–40 | date = July 2002 | pmid = 12093783 | doi = 10.1161/01.CIR.0000021112.29409.A2 | doi-access = free }}</ref> | |||
| * ]<ref name=Hyperinsulinaemia>{{cite journal | vauthors = Griffin M, Frazer A, Johnson A, Collins P, Owens D, Tomkin GH | title = Cellular cholesterol synthesis--the relationship to post-prandial glucose and insulin following weight loss | journal = Atherosclerosis | volume = 138 | issue = 2 | pages = 313–8 | date = June 1998 | pmid = 9690914 | doi = 10.1016/S0021-9150(98)00036-7 }}</ref> | |||
| * ]<ref>{{cite journal | vauthors = King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS | title = Short sleep duration and incident coronary artery calcification | journal = JAMA | volume = 300 | issue = 24 | pages = 2859–66 | date = December 2008 | pmid = 19109114 | pmc = 2661105 | doi = 10.1001/jama.2008.867 }}</ref> | |||
| * ]<ref name="Provost2015">{{cite journal | vauthors = Provost EB, Madhloum N, Int Panis L, De Boever P, Nawrot TS | title = Carotid intima-media thickness, a marker of subclinical atherosclerosis, and particulate air pollution exposure: the meta-analytical evidence | journal = PLOS ONE | volume = 10 | issue = 5 | pages = e0127014 | date = 2015 | pmid = 25970426 | pmc = 4430520 | doi = 10.1371/journal.pone.0127014 | bibcode = 2015PLoSO..1027014P | doi-access = free }}</ref><ref name=PLoSMed42313>{{cite journal | vauthors = Adar SD, Sheppard L, Vedal S, Polak JF, Sampson PD, Diez Roux AV, Budoff M, Jacobs DR, Barr RG, Watson K, Kaufman JD | title = Fine particulate air pollution and the progression of carotid intima-medial thickness: a prospective cohort study from the multi-ethnic study of atherosclerosis and air pollution | journal = PLOS Medicine | volume = 10 | issue = 4 | pages = e1001430 | date = April 23, 2013 | pmid = 23637576 | pmc = 3637008 | doi = 10.1371/journal.pmed.1001430 | quote = This early analysis from MESA suggests that higher long-term PM2.5 concentrations are associated with increased IMT progression and that greater reductions in PM2.5 are related to slower IMT progression. | doi-access = free }}</ref> | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref>{{cite journal | vauthors = Wang CH, Jeng JS, Yip PK, Chen CL, Hsu LI, Hsueh YM, Chiou HY, Wu MM, Chen CJ | display-authors = 6 | title = Biological gradient between long-term arsenic exposure and carotid atherosclerosis | journal = Circulation | volume = 105 | issue = 15 | pages = 1804–1809 | date = April 2002 | pmid = 11956123 | doi = 10.1161/01.cir.0000015862.64816.b2 | doi-access = free }}</ref> | |||
| * ]<ref name=nhlbi.nih/>{{failed verification|date=July 2023}} | |||
| * ]<ref name=nhlbi.nih/> | |||
| * ]<ref>{{cite journal |last1=Sadovsky |first1=Richard |title=Treating Hypothyroidism Reduces Atherosclerosis Risk |journal=American Family Physician |volume=69 |issue=3 |date=February 2004 |pages=656–657 |id={{ProQuest|234284553}} |url=https://www.aafp.org/afp/2004/0201/p656.html }}</ref> | |||
| * ]<ref>{{cite journal | vauthors = Bale BF, Doneen AL, Vigerust DJ | title = High-risk periodontal pathogens contribute to the pathogenesis of atherosclerosis | journal = Postgraduate Medical Journal | volume = 93 | issue = 1098 | pages = 215–220 | date = April 2017 | pmid = 27899684 | pmc = 5520251 | doi = 10.1136/postgradmedj-2016-134279 }}</ref> | |||
| === Dietary === | |||
| The relation between dietary fat and atherosclerosis is controversial. The ], in its ], promotes a diet of about 64% ]s from total calories. The ], the ], and the ] make similar recommendations. In contrast, Prof ] (Harvard School of Public Health, ] of the second ]) recommends much higher levels of fat, especially of ] and ].<ref name="titleFood Pyramids: Nutrition Source, Harvard School of Public Health">{{cite web|url=http://www.hsph.harvard.edu/nutritionsource/pyramids.html |title=Food Pyramids: Nutrition Source, Harvard School of Public Health |access-date=2007-11-25 |archive-url=https://web.archive.org/web/20071226085222/http://www.hsph.harvard.edu/nutritionsource/pyramids.html |archive-date=26 December 2007 |url-status=dead }}</ref> These dietary recommendations reach a consensus, though, against consumption of ]s.{{citation needed|date=December 2020}} | |||
| The role of eating oxidized fats (]) in humans is not clear. | |||
| Rabbits fed rancid fats develop atherosclerosis faster.<ref>{{cite journal | vauthors = Staprãns I, Rapp JH, Pan XM, Hardman DA, Feingold KR | title = Oxidized lipids in the diet accelerate the development of fatty streaks in cholesterol-fed rabbits | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 16 | issue = 4 | pages = 533–8 | date = April 1996 | pmid = 8624775 | doi = 10.1161/01.atv.16.4.533 }}</ref> Rats fed ]-containing oils experienced marked disruptions to their ] systems, and accumulated significant amounts of ] ] in their blood, livers and kidneys.<ref name=SongJH>{{cite journal | vauthors = Song JH, Fujimoto K, Miyazawa T | title = Polyunsaturated (n-3) fatty acids susceptible to peroxidation are increased in plasma and tissue lipids of rats fed docosahexaenoic acid-containing oils | journal = The Journal of Nutrition | volume = 130 | issue = 12 | pages = 3028–33 | date = December 2000 | pmid = 11110863 | doi = 10.1093/jn/130.12.3028 | doi-access = free }}</ref> | |||
| Rabbits fed atherogenic diets containing various oils were found to undergo the most oxidative susceptibility of ] via polyunsaturated oils.<ref name=YapSC>{{cite journal | vauthors = Yap SC, Choo YM, Hew NF, Yap SF, Khor HT, Ong AS, Goh SH | title = Oxidative susceptibility of low density lipoprotein from rabbits fed atherogenic diets containing coconut, palm, or soybean oils | journal = Lipids | volume = 30 | issue = 12 | pages = 1145–50 | date = December 1995 | pmid = 8614305 | doi = 10.1007/BF02536616 }}</ref> In another study, rabbits fed heated soybean oil "grossly induced atherosclerosis and marked liver damage were histologically and clinically demonstrated."<ref name=Greco>{{cite journal | vauthors = Greco AV, Mingrone G | title = Serum and biliary lipid pattern in rabbits feeding a diet enriched with unsaturated fatty acids | journal = Experimental Pathology | volume = 40 | issue = 1 | pages = 19–33 | year = 1990 | pmid = 2279534 | doi = 10.1016/S0232-1513(11)80281-1 }}</ref> However, ] claims that it is not dietary cholesterol, but ]s, or oxidized cholesterols, from fried foods and smoking, that are the culprit.<ref>{{cite web|url=http://medicalxpress.com/news/2013-08-scientist-orthodoxy-heart-disease.html|title=Scientist, 98, challenges orthodoxy on causes of heart disease|work=medicalxpress.com}}</ref> | |||
| Rancid fats and oils taste very unpleasant in even small amounts, so people avoid eating them.<ref name=pmid16249011>{{cite journal | vauthors = Mattes RD | title = Fat taste and lipid metabolism in humans | journal = Physiology & Behavior | volume = 86 | issue = 5 | pages = 691–7 | date = December 2005 | pmid = 16249011 | doi = 10.1016/j.physbeh.2005.08.058 | quote = The rancid odor of an oxidized fat is readily detectable }}</ref> | |||
| It is very difficult to measure or estimate the actual human consumption of these substances.<ref name=pmid12589185>{{cite journal | vauthors = Dobarganes C, Márquez-Ruiz G | title = Oxidized fats in foods | journal = Current Opinion in Clinical Nutrition and Metabolic Care | volume = 6 | issue = 2 | pages = 157–163 | date = March 2003 | pmid = 12589185 | doi = 10.1097/00075197-200303000-00004 }}</ref> Highly unsaturated ] rich oils such as fish oil, when being sold in pill form, can hide the taste of oxidized or rancid fat that might be present. In the US, the health food industry's dietary supplements are self-regulated and outside of FDA regulations.<ref>{{cite web |url= https://www.fda.gov/Food/DietarySupplements/default.htm |title=Dietary Supplements |website=] |date=4 February 2020}}</ref> To protect unsaturated fats from oxidation, it is best to keep them cool and in oxygen-free environments.<ref>{{cite journal | vauthors = Khan-Merchant N, Penumetcha M, Meilhac O, Parthasarathy S | title = Oxidized fatty acids promote atherosclerosis only in the presence of dietary cholesterol in low-density lipoprotein receptor knockout mice | journal = The Journal of Nutrition | volume = 132 | issue = 11 | pages = 3256–3262 | date = November 2002 | pmid = 12421837 | doi = 10.1093/jn/132.11.3256 | doi-access = free | author-link4 = Sampath Parthasarathy }}</ref> | |||
| == Pathophysiology ==<!-- This section is linked ] --> | |||
| Atherogenesis is the developmental process of ]. It is characterized by a remodeling of arteries leading to subendothelial accumulation of fatty substances called plaques. The buildup of an atheromatous plaque is a slow process, developed over several years through a complex series of cellular events occurring within the arterial wall and in response to several local vascular circulating factors. One recent hypothesis suggests that, for unknown reasons, ], such as ] or ], begin to attack the ] of the artery lumen in ]. The ensuing ] leads to the formation of atheromatous plaques in the arterial ], a region of the vessel wall located between the ] and the ]. Chronic inflammation within the arterial wall, driven by immune cells like macrophages, accelerates atherosclerotic plaque instability by promoting collagen breakdown and thinning the fibrous cap, which increases the likelihood of rupture and thrombosis.<ref>{{cite book |last1=Shahjehan |first1=Rai Dilawar |last2=Sharma |first2=Sanjeev |last3=Bhutta |first3=Beenish S. |title=StatPearls |date=2024 |publisher=StatPearls Publishing |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK564304/ |chapter=Coronary Artery Disease |pmid=33231974 }}</ref> The bulk of these lesions is made of excess fat, ], and ]. At first, as the plaques grow, only ] occurs without narrowing. ] is a late event, which may never occur and is often the result of repeated plaque rupture and healing responses, not just the atherosclerotic process.<ref>{{cite web |url= https://www.lecturio.com/concepts/atherosclerosis/ | title= Atherosclerosis | |||
| | website= The Lecturio Medical Concept Library |access-date= 2 July 2021}}</ref> Autopsy studies have shown that the prevalence of coronary artery atherosclerosis in males from the United States, with an average age of 22.1 years old, who died in war, ranges from 45% to 77.3%.<ref>{{cite journal |last1=Joseph |first1=Abraham |last2=Ackerman |first2=Douglas |last3=Talley |first3=J.David |last4=Johnstone |first4=John |last5=Kupersmith |first5=Joel |title=Manifestations of coronary atherosclerosis in young trauma victims—An autopsy study |journal=Journal of the American College of Cardiology |date=August 1993 |volume=22 |issue=2 |pages=459–467 |doi=10.1016/0735-1097(93)90050-B |pmid=8335815 }}</ref> | |||
| === Cellular === | |||
| ] of an ] that supplies the ] showing significant atherosclerosis and marked ] narrowing. Tissue has been stained using ].]] | |||
| Early atherogenesis is characterized by the adherence of blood circulating ] (a type of ]) to the vascular bed lining, the ], then by their migration to the sub-endothelial space, and further activation into monocyte-derived ]s.<ref name=cas/><ref>{{cite journal | vauthors = Schwartz CJ, Valente AJ, Sprague EA, Kelley JL, Cayatte AJ, Mowery J | title = Atherosclerosis. Potential targets for stabilization and regression | journal = Circulation | volume = 86 | issue = 6 Suppl | pages = III117–23 | date = December 1992 | pmid = 1424045 }}</ref> The primary documented driver of this process is oxidized lipoprotein particles within the wall, beneath the ] cells, though upper normal or elevated concentrations of ] also plays a major role and not all factors are fully understood. ]s may appear and disappear.{{citation needed|date=December 2020}} | |||
| ] (LDL) particles in blood plasma invade the ] and become oxidized, creating risk of ]. A complex set of biochemical reactions regulates the oxidation of ], involving enzymes (such as ]) and ]s in the endothelium.<ref name=Endotext2000>{{cite journal | vauthors = Linton MF, Yancey PG, Davies SS, Jerome WG, Linton EF, Song WL, etal | title = The Role of Lipids and Lipoproteins in Atherosclerosis | journal = Endotext | date = 2000 | pmid = 26844337 | id = {{NCBIBook2|NBK343489}} }}</ref> | |||
| Initial damage to the endothelium results in an inflammatory response. Monocytes enter the artery wall from the bloodstream, with ]s adhering to the area of insult. This may be promoted by ] induction of factors such as ], which recruits circulating monocytes, and ], which is selectively required for the differentiation of monocytes to macrophages. The monocytes differentiate into ]s, which proliferate locally,<ref>{{cite journal | vauthors = Robbins CS, Hilgendorf I, Weber GF, Theurl I, Iwamoto Y, Figueiredo JL, Gorbatov R, Sukhova GK, Gerhardt LM, Smyth D, Zavitz CC, Shikatani EA, Parsons M, van Rooijen N, Lin HY, Husain M, Libby P, Nahrendorf M, Weissleder R, Swirski FK | title = Local proliferation dominates lesional macrophage accumulation in atherosclerosis | journal = Nature Medicine | volume = 19 | issue = 9 | pages = 1166–72 | date = September 2013 | pmid = 23933982 | pmc = 3769444 | doi = 10.1038/nm.3258 }}</ref> ingest oxidized LDL, slowly turning into large "]s" – so-called because of their changed appearance resulting from the numerous internal cytoplasmic ] and resulting high ] content. Under the microscope, the lesion now appears as a fatty streak. Foam cells eventually die and further propagate the inflammatory process.{{citation needed|date=December 2020}} | |||
| In addition to these cellular activities, there is also ] proliferation and migration from the ] into the ] in response to ]s secreted by damaged endothelial cells. This causes the formation of a fibrous capsule covering the fatty streak. Intact endothelium can prevent this smooth muscle proliferation by releasing ].{{citation needed|date=December 2020}} | |||
| ===Calcification and lipids=== | ===Calcification and lipids=== | ||
| ] forms among ] cells of the surrounding muscular layer, specifically in the muscle cells adjacent to atheromas and on the surface of atheroma plaques and tissue.<ref>{{cite journal | vauthors = Miller JD | title = Cardiovascular calcification: Orbicular origins | journal = Nature Materials | volume = 12 | issue = 6 | pages = 476–478 | date = June 2013 | pmid = 23695741 | doi = 10.1038/nmat3663 | bibcode = 2013NatMa..12..476M }}</ref> In time, as cells die, this leads to extracellular calcium deposits between the muscular wall and outer portion of the atheromatous plaques. With the atheromatous plaque interfering with the regulation of calcium deposition, it accumulates and crystallizes. A similar form of intramural calcification, presenting the picture of an early phase of arteriosclerosis, appears to be induced by many drugs that have an antiproliferative mechanism of action (] 2008).{{citation needed|date=April 2021}} | |||
| Cholesterol is delivered into the vessel wall by cholesterol-containing ] (LDL) particles. To attract and stimulate macrophages, the cholesterol must be released from the LDL particles and oxidized, a key step in the ongoing inflammatory process. The process is worsened if |
Cholesterol is delivered into the vessel wall by cholesterol-containing ] (LDL) particles. To attract and stimulate macrophages, the cholesterol must be released from the LDL particles and oxidized, a key step in the ongoing inflammatory process. The process is worsened if it is insufficient ] (HDL), the lipoprotein particle that removes cholesterol from tissues and carries it back to the liver.<ref name=Endotext2000/> | ||
| The foam |
The ]s and ]s encourage the migration and proliferation of ] cells, which in turn ingest lipids, become replaced by ], and transform into foam cells themselves. A protective fibrous cap normally forms between the fatty deposits and the artery lining (the ]).{{citation needed|date=December 2020}} | ||
| These capped fatty deposits (now called |
These capped fatty deposits (now called 'atheromas') produce enzymes that cause the artery to enlarge over time. As long as the artery enlarges sufficiently to compensate for the extra thickness of the atheroma, then no narrowing ("]") of the opening ("lumen") occurs. The artery expands with an egg-shaped cross-section, still with a circular opening. If the enlargement is beyond proportion to the atheroma thickness, then an ] is created.<ref name=Glagov>{{cite journal | vauthors = Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ | title = Compensatory enlargement of human atherosclerotic coronary arteries | journal = The New England Journal of Medicine | volume = 316 | issue = 22 | pages = 1371–5 | date = May 1987 | pmid = 3574413 | doi = 10.1056/NEJM198705283162204 }}</ref> | ||
| ===Visible features=== | ===Visible features=== | ||
| ]. ] specimen.]] | ]. ] specimen.]] | ||
| Although arteries are not typically studied microscopically, two plaque types can be distinguished |
Although arteries are not typically studied microscopically, two plaque types can be distinguished:<ref>{{cite web |url=http://www.pathologyatlas.ro/coronary-atherosclerosis-fibrous-plaque.php |title=Coronary atherosclerosis — the fibrous plaque with calcification |publisher=www.pathologyatlas.ro |access-date=2010-03-25 }}</ref> | ||
| # ''The fibro-lipid (fibro-fatty) plaque'' is characterized by an accumulation of lipid-laden cells underneath the intima of the arteries, typically without narrowing the lumen due to compensatory expansion of the bounding muscular layer of the artery wall. Beneath the endothelium there is a "fibrous cap" covering the atheromatous "core" of the plaque. The core consists of lipid-laden cells (macrophages and smooth muscle cells) with elevated tissue cholesterol and cholesterol ester content, fibrin, proteoglycans, collagen, elastin and cellular debris. In advanced plaques, the central core of the plaque usually contains extracellular cholesterol deposits (released from dead cells), which form areas of cholesterol crystals with empty, needle-like clefts. At the periphery of the plaque are younger "foamy" cells and capillaries. These plaques usually produce the most damage to the individual when they rupture. | |||
| # ''The fibrous plaque'' is also localized under the intima, within the wall of the artery resulting in thickening and expansion of the wall and, sometimes, spotty localized narrowing of the lumen with some atrophy of the muscular layer. The fibrous plaque contains collagen fibres (eosinophilic), precipitates of calcium (hematoxylinophilic) and, rarely, lipid-laden cells. | |||
| # The fibro-lipid (fibro-fatty) plaque is characterized by an accumulation of lipid-laden cells underneath the ] of the arteries, typically without narrowing the lumen due to compensatory expansion of the bounding muscular layer of the artery wall. Beneath the endothelium, there is a "fibrous cap" covering the atheromatous "core" of the plaque. The core consists of lipid-laden cells (macrophages and smooth muscle cells) with elevated tissue cholesterol and ] content, ], ]s, ], ], and cellular debris. In advanced plaques, the central core of the plaque usually contains extracellular cholesterol deposits (released from dead cells), which form areas of cholesterol crystals with empty, needle-like clefts. At the periphery of the plaque are younger "foamy" cells and capillaries. These plaques usually produce the most damage to the individual when they rupture. Cholesterol crystals may also play a role.<ref>{{cite journal | vauthors = Janoudi A, Shamoun FE, Kalavakunta JK, Abela GS | title = Cholesterol crystal-induced arterial inflammation and destabilization of atherosclerotic plaque | journal = European Heart Journal | volume = 37 | issue = 25 | pages = 1959–67 | date = July 2016 | pmid = 26705388 | doi = 10.1093/eurheartj/ehv653 | doi-access = free }}</ref> | |||
| In effect, the muscular portion of the artery wall forms small ]s just large enough to hold the ] that are present. The muscular portion of artery walls usually remain strong, even after they have remodeled to compensate for the ]tous plaques. | |||
| # The fibrous plaque is also localized under the intima, within the arterial wall resulting in thickening and expansion of the wall and, sometimes, spotty localized narrowing of the lumen with some atrophy of the muscular layer. The fibrous plaque contains collagen fibers (]), precipitates of calcium (hematoxylinophilic), and rarely, lipid-laden cells.{{citation needed|date=December 2020}} | |||
| In effect, the muscular portion of the artery wall forms small ]s just large enough to hold the ] that are present. The muscular portion of artery walls usually remains strong, even after they have been remodeled to compensate for the atheromatous plaques.{{citation needed|date=December 2020}} | |||
| However, ]s within the vessel wall are soft and fragile with little elasticity. Arteries constantly expand and contract with each heartbeat, i.e., the pulse. In addition, the calcification deposits between the outer portion of the atheroma and the muscular wall, as they progress, lead to a loss of elasticity and stiffening of the artery as a whole. | |||
| However, atheromas within the vessel wall are soft and fragile with little elasticity. Arteries constantly expand and contract with each heartbeat, i.e., the pulse. In addition, the calcification deposits between the outer portion of the atheroma and the muscular wall, as they progress, lead to a loss of elasticity and stiffening of the artery as a whole.{{citation needed|date=December 2020}} | |||
| The calcification deposits, after they have become sufficiently advanced, are partially visible on coronary artery ] or ] (EBT) as rings of increased radiographic density, forming halos around the outer edges of the atheromatous plaques, within the artery wall. On CT, >130 units on the ] {some argue for 90 units) has been the radiographic density usually accepted as clearly representing tissue calcification within arteries. These deposits demonstrate unequivocal evidence of the disease, relatively advanced, even though the lumen of the artery is often still normal by angiographic or ]. | |||
| The calcification deposits,<ref>{{cite book | vauthors = Maton A, Hopkins RL, McLaughlin CW, Johnson S, Warner MQ, LaHart D, Wright JD | display-authors = 6 | title = Human Biology and Health | publisher = Prentice Hall | year = 1993 | location = Englewood Cliffs, NJ | isbn = 978-0-13-981176-0 | oclc = 32308337 | url-access = registration | url = https://archive.org/details/humanbiologyheal00scho }}</ref> after they have become sufficiently advanced, are partially visible on coronary artery ] or ] (EBT) as rings of increased radiographic density, forming halos around the outer edges of the atheromatous plaques, within the artery wall. On CT, >130 units on the ] (some argue for 90 units) has been the radiographic density usually accepted as clearly representing tissue calcification within arteries. These deposits demonstrate unequivocal evidence of the disease, relatively advanced, even though the lumen of the artery is often still normal by angiography.{{citation needed|date=December 2020}} | |||
| ===Rupture and stenosis=== | ===Rupture and stenosis=== | ||
| ] | |||
| Although the disease process tends to be slowly progressive over decades, it usually remains asymptomatic until an atheroma obstructs the bloodstream in the artery. This is typically by rupture of an atheroma, clotting and fibrous organization of the clot within the lumen, covering the rupture but also producing ], or over time and after repeated ruptures, resulting in a persistent, usually localized stenosis. Stenoses can be slowly progressive, while plaque rupture is a sudden event that occurs specifically in atheromas with thinner/weaker fibrous caps that have become "unstable". | |||
| Although the disease process tends to be slowly progressive over decades, it usually remains asymptomatic until an atheroma ], which leads to immediate blood clotting at the site of the atheroma ulcer. This triggers a cascade of events that leads to clot enlargement, which may quickly obstruct blood flow. A complete blockage leads to ischemia of the myocardial (heart) muscle and damage. This process is the ] or "heart attack".<ref name="What Are the Signs and Symptoms of">{{cite web|title=What Are the Signs and Symptoms of Coronary Heart Disease?|url=http://www.nhlbi.nih.gov/health/health-topics/topics/cad/signs|website=www.nhlbi.nih.gov|access-date=2 July 2021|date=September 29, 2014|url-status=dead|archive-url=https://web.archive.org/web/20150224034615/http://www.nhlbi.nih.gov/health/health-topics/topics/cad/signs|archive-date=24 February 2015}}</ref> | |||
| If the heart attack is not fatal, fibrous organization of the clot within the lumen ensues, covering the rupture but also producing ] or closure of the lumen, or over time and after repeated ruptures, resulting in a persistent, usually localized stenosis or blockage of the artery lumen. Stenoses can be slowly progressive, whereas plaque ulceration is a sudden event that occurs specifically in atheromas with thinner/weaker fibrous caps that have become "unstable".<ref name="What Are the Signs and Symptoms of"/> | |||
| Repeated plaque ruptures, ones not resulting in total lumen closure, combined with the clot patch over the rupture and healing response to stabilize the clot, is the process that produces most stenoses over time. The stenotic areas tend to become more stable, despite increased flow velocities at these narrowings. Most major blood-flow-stopping events occur at large plaques, which, prior to their rupture, produced very little if any stenosis. | |||
| Repeated plaque ruptures, ones not resulting in total lumen closure, combined with the clot patch over the rupture and healing response to stabilize the clot is the process that produces most stenoses over time. The stenotic areas often become more stable despite increased flow velocities at these narrowings. Most major blood-flow-stopping events occur at large plaques, which, before their rupture, produced little if any stenosis.{{citation needed|date=December 2020}} | |||
| From clinical trials, 20% is the average stenosis at plaques that subsequently rupture with resulting complete artery closure. Most severe clinical events do not occur at plaques that produce high-grade stenosis. From clinical trials, only 14% of heart attacks occur from artery closure at plaques producing a 75% or greater stenosis prior to the vessel closing. | |||
| From clinical trials, 20% is the average stenosis at plaques that subsequently rupture with resulting complete artery closure. Most severe clinical events do not occur at plaques that produce high-grade stenosis. From clinical trials, only 14% of heart attacks occur from artery closure at plaques producing a 75% or greater stenosis before the vessel closing.{{Citation needed|date=August 2010}} | |||
| If the fibrous cap separating a soft atheroma from the bloodstream within the artery ruptures, tissue fragments are exposed and released, and blood enters the atheroma within the wall and sometimes results in a sudden expansion of the atheroma size. Tissue fragments are very clot-promoting, containing ] and ]; they activate ]s and activate the ]. The result is the formation of a ] (blood clot) overlying the atheroma, which obstructs blood flow acutely. With the obstruction of blood flow, downstream tissues are starved of ] and nutrients. If this is the ] (heart muscle), ] (cardiac chest pain) or ] (heart attack) develops. | |||
| If the fibrous cap separating a soft atheroma from the bloodstream within the artery ruptures, tissue fragments are exposed and released. These tissue fragments are very clot-promoting, containing ] and ]; they activate ]s and activate the ]. The result is the formation of a ] (blood clot) overlying the atheroma, which obstructs blood flow acutely. With the obstruction of blood flow, downstream tissues are starved of ] and nutrients. If this is the ] (heart muscle) ] (cardiac chest pain) or ] (heart attack) develops.{{citation needed|date=December 2020}} | |||
| ==Diagnosis of plaque-related disease== | |||
| ] | |||
| Areas of severe narrowing, ], detectable by angiography, and to a lesser extent "]" have long been the focus of human diagnostic techniques for ], in general. However, these methods focus on detecting only severe ], not the underlying atherosclerosis disease. As demonstrated by human clinical studies, most severe events occur in locations with heavy plaque, yet little or no lumen ] present before debilitating events suddenly occur. Plaque rupture can lead to artery lumen occlusion within seconds to minutes, and potential permanent debility and sometimes sudden death. | |||
| ===Accelerated growth of plaques=== | |||
| Greater than 75% lumen ] used to be considered by cardiologists as the hallmark of clinically significant disease because it is typically only at this severity of narrowing of the larger heart arteries that recurring episodes of ] and detectable abnormalities by ]ing methods are seen. However, clinical trials have shown that only about 14% of clinically-debilitating events occur at locations with this, or greater severity of ]. The majority of events occur due to atheroma plaque rupture at areas without ] sufficient enough to produce any ] or ] abnormalities. Thus, since the later-1990s, greater attention is being focused on the "vulnerable plaque." | |||
| The distribution of atherosclerotic plaques in a part of arterial endothelium is inhomogeneous. The multiple and focal development of atherosclerotic changes is similar to that in the development of ] in the brain and age spots on the skin. Misrepair-accumulation aging theory suggests that misrepair mechanisms<ref>{{cite journal | vauthors = Wang J, Michelitsch T, Wunderlin A, Mahadeva R |title=Aging as a consequence of misrepair -- A novel theory of aging |journal=Nature Precedings |date=6 April 2009 |doi=10.1038/npre.2009.2988.2 |arxiv=0904.0575 }}</ref><ref>{{cite arXiv |title= Aging as a process of accumulation of Misrepairs | vauthors = Wang-Michelitsch J, Michelitsch T |class= q-bio.TO |year=2015 | eprint = 1503.07163 }}</ref> play an important role in the focal development of atherosclerosis.<ref>{{cite arXiv |title= Misrepair mechanism in the development of atherosclerotic plaques | vauthors = Wang-Michelitsch J, Michelitsch TM |class= q-bio.TO |year=2015 | eprint = 1505.01289 }}</ref> The development of a plaque is a result of the repair of the injured endothelium. Because of the infusion of lipids into the sub-endothelium, the repair has to end up with altered remodeling of the local endothelium. This is the manifestation of a misrepair. This altered remodeling increases the susceptibility of the local endothelium to damage and reduces its repair efficiency. Consequently, this part of endothelium has an increased risk of being injured and improperly repaired. Thus, the accumulation of misrepairs of endothelium is focalized and self-accelerating. In this way, the growth of a plaque is also self-accelerating. Within a part of the arterial wall, the oldest plaque is always the biggest and is the most dangerous one to cause blockage of a local artery.{{citation needed|date=December 2020}} | |||
| ===Components=== | |||
| Though any artery in the body can be involved, usually only severe ] or obstruction of some arteries, those that supply more critically-important organs are recognized. Obstruction of arteries supplying the heart muscle result in a ]. Obstruction of arteries supplying the brain result in a ]. These events are life-changing, and often result in irreversible loss of function because lost heart muscle and brain cells do not grow back to any significant extent, typically less than 2%. | |||
| The plaque is divided into three distinct components: | |||
| # The ] ("lump of gruel", {{ety|gre|''ἀθήρα'' (athera)|]}}), which is the nodular accumulation of a soft, flaky, yellowish material at the center of large plaques, composed of macrophages nearest the ] of the artery{{citation needed|date=December 2020}} | |||
| # Underlying areas of cholesterol crystals{{citation needed|date=December 2020}} | |||
| # Calcification at the outer base of older or more advanced ]. Atherosclerotic lesions, or atherosclerotic plaques, are separated into two broad categories: Stable and unstable (also called vulnerable).<ref>{{cite journal | vauthors = Ross R | title = Atherosclerosis--an inflammatory disease | journal = The New England Journal of Medicine | volume = 340 | issue = 2 | pages = 115–26 | date = January 1999 | pmid = 9887164 | doi = 10.1056/NEJM199901143400207 }}</ref> The pathobiology of atherosclerotic lesions is very complicated, but generally, stable atherosclerotic plaques, which tend to be asymptomatic, are rich in ] and ]. On the other hand, unstable plaques are rich in macrophages and ]s, and the extracellular matrix separating the lesion from the arterial lumen (also known as the ]) is usually weak and prone to rupture.<ref>{{cite journal | vauthors = Finn AV, Nakano M, Narula J, Kolodgie FD, Virmani R | title = Concept of vulnerable/unstable plaque | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 30 | issue = 7 | pages = 1282–92 | date = July 2010 | pmid = 20554950 | doi = 10.1161/ATVBAHA.108.179739 | doi-access = free }}</ref> Ruptures of the fibrous cap expose thrombogenic material, such as ],<ref>{{cite journal | vauthors = Didangelos A, Simper D, Monaco C, Mayr M | title = Proteomics of acute coronary syndromes | journal = Current Atherosclerosis Reports | volume = 11 | issue = 3 | pages = 188–95 | date = May 2009 | pmid = 19361350 | doi = 10.1007/s11883-009-0030-x }}</ref> to the circulation and eventually induce ] formation in the lumen. Upon formation, intraluminal thrombi can occlude arteries outright (e.g., coronary occlusion), but more often they detach, move into the circulation, and eventually occlude smaller downstream branches causing ].{{citation needed|date=December 2020}} | |||
| Apart from thromboembolism, chronically expanding atherosclerotic lesions can cause complete closure of the lumen. Chronically expanding lesions are often asymptomatic until the lumen ] is so severe (usually over 80%) that blood supply to downstream tissue(s) is insufficient, resulting in ]. These complications of advanced atherosclerosis are chronic, slowly progressive, and cumulative. Most commonly, soft plaque suddenly ruptures (see ]), causing the formation of a thrombus that will rapidly slow or stop blood flow, leading to the death of the tissues fed by the artery in approximately five minutes. This event is called an ].{{citation needed|date=December 2020}} | |||
| Over the last couple of decades, methods other than angiography and stress-testing have been increasingly developed as ways to better detect atherosclerotic disease before it becomes symptomatic. These have included both (a) anatomic detection methods and (b) physiologic measurement methods. | |||
| ==Diagnosis== | |||
| Examples of anatomic methods include: (1) coronary calcium scoring by CT, (2) carotid IMT (intimal medial thickness) measurement by ultrasound, and (3) IVUS. | |||
| ] of atherosclerosis of the abdominal aorta. Woman of 70 years old with hypertension and dyslipidemia.]] | |||
| ] and ] stain)]] | |||
| Areas of severe narrowing, ], detectable by ], and to a lesser extent "]" have long been the focus of human diagnostic techniques for ], in general. However, these methods focus on detecting only severe narrowing, not the underlying atherosclerosis disease.<ref name=CR118-4>{{cite journal | vauthors = Tarkin JM, Dweck MR, Evans NR, Takx RA, Brown AJ, Tawakol A, Fayad ZA, Rudd JH | display-authors = 6 | title = Imaging Atherosclerosis | journal = Circulation Research | volume = 118 | issue = 4 | pages = 750–769 | date = February 2016 | pmid = 26892971 | pmc = 4756468 | doi = 10.1161/CIRCRESAHA.115.306247 }}</ref> As demonstrated by human clinical studies, most severe events occur in locations with heavy plaque, yet little or no lumen narrowing present before debilitating events suddenly occur. Plaque rupture can lead to artery lumen occlusion within seconds to minutes, potential permanent debility, and sometimes sudden death.{{citation needed|date=December 2020}} | |||
| Examples of physiologic methods include: (1) lipoprotein subclass analysis, (2) HbA1c, (3) hs-CRP, and (4) homocysteine. | |||
| Plaques that have ruptured are called complicated lesions. The ] of the lesion breaks, usually at the shoulder of the fibrous cap that separates the lesion from the arterial lumen, where the exposed thrombogenic components of the plaque, mainly ], will trigger ] formation. The thrombus then travels downstream to other blood vessels, where the blood clot may partially or completely block blood flow. If the blood flow is completely blocked, cell deaths occur due to the lack of ] supply to ] cells, resulting in ].<ref>{{cite journal | vauthors = Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW | display-authors = 6 | title = A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association | journal = Circulation | volume = 92 | issue = 5 | pages = 1355–1374 | date = September 1995 | pmid = 7648691 | doi = 10.1161/01.CIR.92.5.1355 | doi-access = free | author-link4 = Valentín Fuster }}</ref> The narrowing or obstruction of blood flow can occur in any artery within the body. Obstruction of arteries supplying the heart muscle results in a ], while the obstruction of arteries supplying the brain results in an ischaemic ].{{citation needed|date=December 2020}} | |||
| The example of the metabolic syndrome combines both anatomic (abdominal girth) and physiologic (blood pressure, elevated blood glucose) methods. | |||
| ] | |||
| Advantages of these two approaches: The anatomic methods directly measure some aspect of the actual atherosclerotic disease process itself, thus offer potential for earlier detection, including before symptoms start, disease staging and tracking of disease progression. The physiologic methods are often less expensive and safer and changing them for the better may slow disease progression, in some cases with marked improvement. | |||
| Lumen ] that is greater than 75% was considered the hallmark of clinically significant disease in the past because recurring episodes of ] and abnormalities in ] are only detectable at that particular severity of stenosis. However, clinical trials have shown that only about 14% of clinically debilitating events occur at sites with more than 75% stenosis. Most cardiovascular events that involve sudden rupture of the atheroma plaque do not display any evident luminal narrowing. Thus, greater attention has been focused on "vulnerable plaque" from the late 1990s onwards.<ref name=MaseriFuster>{{cite journal | vauthors = Maseri A, Fuster V | title = Is there a vulnerable plaque? | journal = ] | volume = 107 | issue = 16 | pages = 2068–71 | date = April 2003 | pmid = 12719286 | doi = 10.1161/01.CIR.0000070585.48035.D1 | doi-access = free }}</ref> | |||
| Disadvantages of these two approaches: The anatomic methods are generally more expensive and several are invasive, such as IVUS. The physiologic methods do not quantify the current state of the disease or directly track progression. For both, clinicians and third party payers have been slow to accept the usefulness of these newer approaches. | |||
| Besides the traditional diagnostic methods such as ] and stress-testing, other detection techniques have been developed in the past decades for earlier detection of atherosclerotic disease. Some of the detection approaches include anatomical detection and physiologic measurement.{{citation needed|date=December 2020}} | |||
| ==Physiologic factors that increase risk== | |||
| Various anatomic, physiological & behavioral risk factors for atherosclerosis are known. These can be divided into various categories: congenital ''vs'' acquired, modifiable or not, classical or non-classical. The points labelled '+' in the following list form the core components of "]": | |||
| Examples of anatomical detection methods include coronary calcium scoring by ], carotid IMT (]) measurement by ultrasound, and intravascular imaging techniques, such as ] (IVUS), and ] (OCT),<ref>{{Cite journal |last1=Tearney |first1=Guillermo J. |last2=Regar |first2=Evelyn |last3=Akasaka |first3=Takashi |last4=Adriaenssens |first4=Tom |last5=Barlis |first5=Peter |last6=Bezerra |first6=Hiram G. |last7=Bouma |first7=Brett |last8=Bruining |first8=Nico |last9=Cho |first9=Jin-man |last10=Chowdhary |first10=Saqib |last11=Costa |first11=Marco A. |last12=de Silva |first12=Ranil |last13=Dijkstra |first13=Jouke |last14=Di Mario |first14=Carlo |last15=Dudeck |first15=Darius |date=2012-03-20 |title=Consensus Standards for Acquisition, Measurement, and Reporting of Intravascular Optical Coherence Tomography Studies: A Report From the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation |journal=Journal of the American College of Cardiology |volume=59 |issue=12 |pages=1058–1072 |doi=10.1016/j.jacc.2011.09.079 |pmid=22421299 }}</ref><ref>{{cite journal |last1=Pereira |first1=Vitor M. |last2=Lylyk |first2=Pedro |last3=Cancelliere |first3=Nicole |last4=Lylyk |first4=Pedro N. |last5=Lylyk |first5=Ivan |last6=Anagnostakou |first6=Vania |last7=Bleise |first7=Carlos |last8=Nishi |first8=Hidehisa |last9=Epshtein |first9=Mark |last10=King |first10=Robert M. |last11=Shazeeb |first11=Mohammed Salman |last12=Puri |first12=Ajit S. |last13=Liang |first13=Conrad W. |last14=Hanel |first14=Ricardo A. |last15=Spears |first15=Julian |last16=Marotta |first16=Thomas R. |last17=Lopes |first17=Demetrius K. |last18=Gounis |first18=Matthew J. |last19=Ughi |first19=Giovanni J. |title=Volumetric microscopy of cerebral arteries with a miniaturized optical coherence tomography imaging probe |journal=Science Translational Medicine |date=15 May 2024 |volume=16 |issue=747 |pages=eadl4497 |doi=10.1126/scitranslmed.adl4497 |pmid=38748771 }}</ref> allowing direct visualization of atherosclerotic plaques. | |||
| * ] | |||
| * ] sex | |||
| Other methods include blood measurements, e.g., lipoprotein subclass analysis, ], ], and ].{{citation needed|date=December 2020}} | |||
| * Having ] or ] (IGT) + | |||
| * ] (unhealthy patterns of serum proteins carrying fats & ]): + | |||
| Both anatomic and physiologic methods allow early detection before symptoms show up, disease staging, and tracking of disease progression. | |||
| ** High serum concentration of ] (LDL, "bad if elevated concentrations and small"), ] (a variant of LDL), and / or ] (VLDL) particles, i.e. "lipoprotein subclass analysis" | |||
| ** Low serum concentration of functioning ] (HDL "protective if large and high enough" particles), i.e. "lipoprotein subclass analysis" | |||
| In recent years, developments in ] techniques such as PET and SPECT have provided non-invasive ways of estimating the severity of atherosclerotic plaques.<ref name="CR118-4" /> | |||
| * ] | |||
| * Having ] ] + | |||
| ==Prevention== | |||
| * Being ] (in particular ], also referred to as ''abdominal'' or ''male-type'' obesity) + | |||
| Up to 90% of cardiovascular disease may be preventable if established risk factors are avoided.<ref name="McGillMcMahan2008">{{cite journal | vauthors = McGill HC, McMahan CA, Gidding SS | title = Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study | journal = Circulation | volume = 117 | issue = 9 | pages = 1216–27 | date = March 2008 | pmid = 18316498 | doi = 10.1161/CIRCULATIONAHA.107.717033 | doi-access = free }}</ref><ref>{{cite journal | vauthors = McNeal CJ, Dajani T, Wilson D, Cassidy-Bushrow AE, Dickerson JB, Ory M | title = Hypercholesterolemia in youth: opportunities and obstacles to prevent premature atherosclerotic cardiovascular disease | journal = Current Atherosclerosis Reports | volume = 12 | issue = 1 | pages = 20–8 | date = January 2010 | pmid = 20425267 | doi = 10.1007/s11883-009-0072-0 }}</ref> Medical management of atherosclerosis first involves modification to risk factors–for example, via ] and diet restrictions. Prevention is generally by eating a healthy diet, exercising, not smoking, and maintaining a normal weight.<ref name=NIH2016Pre/> | |||
| * A ] | |||
| * Having close relatives who have had some complication of atherosclerosis (eg. ] or ]) | |||
| ===Diet=== | |||
| * Elevated serum levels of ] | |||
| Changes in diet may help prevent the development of atherosclerosis. Tentative evidence suggests that a diet containing ]s has no effect on or decreases the risk of ].<ref>{{cite journal | vauthors = Rice BH | title = Dairy and Cardiovascular Disease: A Review of Recent Observational Research | journal = Current Nutrition Reports | volume = 3 | issue = 2 | pages = 130–138 | date = 2014 | pmid = 24818071 | pmc = 4006120 | doi = 10.1007/s13668-014-0076-4 }}</ref><ref>{{cite journal | vauthors = Kratz M, Baars T, Guyenet S | title = The relationship between high-fat dairy consumption and obesity, cardiovascular, and metabolic disease | journal = European Journal of Nutrition | volume = 52 | issue = 1 | pages = 1–24 | date = February 2013 | pmid = 22810464 | doi = 10.1007/s00394-012-0418-1 }}</ref> | |||
| * Elevated serum levels of ] (also responsible for gout) | |||
| * Elevated serum ] concentrations + | |||
| A diet high in fruits and vegetables decreases the risk of cardiovascular disease and death.<ref>{{cite journal | vauthors = Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB | title = Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies | journal = BMJ | volume = 349 | pages = g4490 | date = July 2014 | pmid = 25073782 | pmc = 4115152 | doi = 10.1136/bmj.g4490 }}</ref> Evidence suggests that the ] may improve cardiovascular results.<ref>{{cite journal |last1=Walker |first1=Christopher |last2=Reamy |first2=Brian V |title=Diets for Cardiovascular Disease Prevention: What Is the Evidence? |journal=American Family Physician |volume=79 |issue=7 |date=April 2009 |pages=571–578 |id={{ProQuest|234120649}} |pmid=19378874 |url=https://www.aafp.org/link_out?pmid=19378874 }}</ref> There is also evidence that a Mediterranean diet may be better than a ] in bringing about long-term changes to cardiovascular risk factors (e.g., lower ] and ]).<ref>{{cite journal | vauthors = Nordmann AJ, Suter-Zimmermann K, Bucher HC, Shai I, Tuttle KR, Estruch R, Briel M | title = Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors | journal = The American Journal of Medicine | volume = 124 | issue = 9 | pages = 841–51.e2 | date = September 2011 | pmid = 21854893 | doi = 10.1016/j.amjmed.2011.04.024 }}</ref> A 2024 review highlighted that bioactive compounds found in Mediterranean diet components (such as olive, grape, garlic, rosemary, and saffron) exhibit properties that may contribute to cardiovascular health and atherosclerosis prevention.<ref name="FBio-2024">{{cite journal |last1=Anguera-Tejedor |first1=Mateu |last2=Garrido |first2=Gabino |last3=Garrido-Suárez |first3=Bárbara B. |last4=Ardiles-Rivera |first4=Alejandro |last5=Bistué-Rovira |first5=Àngel |last6=Jiménez-Altayó |first6=Francesc |last7=Delgado-Hernández |first7=René |title=Exploring the therapeutic potential of bioactive compounds from selected plant extracts of Mediterranean diet constituents for cardiovascular diseases: A review of mechanisms of action, clinical evidence, and adverse effects |journal=Food Bioscience |date=December 2024 |volume=62 |pages=105487 |doi=10.1016/j.fbio.2024.105487 }}</ref> | |||
| * Chronic systemic ] as reflected by upper normal WBC concentrations, elevated ] and many other blood chemistry markers, most only research level at present, not clinically done.<ref name=Bhatt> ''Need to Test the Arterial Inflammation Hypothesis'', 2002, referenced on 4/1/06 </ref> | |||
| * ] or symptoms of ] | |||
| ===Exercise=== | |||
| * ] (a slow-acting ]) | |||
| A controlled exercise program combats atherosclerosis by improving the circulation and functionality of the vessels. Exercise is also used to manage weight in patients who are obese, lower blood pressure, and decrease cholesterol. Often lifestyle modification is combined with medication therapy. For example, ]s help to lower cholesterol. Antiplatelet medications like ] help to prevent clots, and a variety of ] medications are routinely used to control blood pressure. If the combined efforts of risk factor modification and medication therapy are not sufficient to control symptoms or fight imminent threats of ischemic events, a physician may resort to interventional or surgical procedures to correct the obstruction.<ref>{{cite book |chapter= Cardiovascular, Circulatory, and Hematologic Function |pages=730–1047 |chapter-url= https://books.google.com/books?id=SB_-CRXvZPYC&pg=PA730 | veditors = Paul P, Williams B |title=Brunner & Suddarth's Textbook of Canadian Medical-surgical Nursing |date=2009 |publisher=Lippincott Williams & Wilkins |isbn=978-0-7817-9989-8 }}</ref> | |||
| * High intake of trans-fats and saturated fats in diet | |||
| ==Treatment== | ==Treatment== | ||
| Treatment of established disease may include medications to lower cholesterol such as ]s, ], or medications that decrease clotting, such as ].<ref name=NIH2016Tx/> Many procedures may also be carried out such as ], ], or ].<ref name=NIH2016Tx/> | |||
| If atherosclerosis leads to symptoms, some symptoms such as ] can be treated. Non-pharmaceutical means are usually the first method of treatment, such as cessation of smoking and practicing regular exercise. If these methods do not work, medicines are usually the next step in treating cardiovascular diseases, and with improvements, have increasingly become the most effective method over the long term. However, medicines are criticized for their expense, patented control and occasional undesired effects. | |||
| Medical treatments often focus on alleviating symptoms. However, measures that focus on decreasing underlying atherosclerosis—as opposed to simply treating symptoms—are more effective.<ref name="Fonarow, G 2003">{{cite journal | vauthors = Fonarow G | year = 2003 | title = Aggressive treatment of atherosclerosis: The time is now | journal = Cleve. Clin. J. Med. | volume = 70 | issue = 5| pages = 431–434 | doi=10.3949/ccjm.70.5.431| doi-broken-date = 4 December 2024 | pmid = 12785316 }}</ref> Non-pharmaceutical means are usually the first method of treatment, such as stopping smoking and practicing regular exercise.<ref>{{cite journal | vauthors = Ambrose JA, Barua RS | title = The pathophysiology of cigarette smoking and cardiovascular disease: an update | journal = Journal of the American College of Cardiology | volume = 43 | issue = 10 | pages = 1731–7 | date = May 2004 | pmid = 15145091 | doi = 10.1016/j.jacc.2003.12.047 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Pigozzi F, Rizzo M, Fagnani F, Parisi A, Spataro A, Casasco M, Borrione P | title = Endothelial (dys)function: the target of physical exercise for prevention and treatment of cardiovascular disease | journal = The Journal of Sports Medicine and Physical Fitness | volume = 51 | issue = 2 | pages = 260–267 | date = June 2011 | pmid = 21681161 | url = http://www.minervamedica.it/index2.t?show=R40Y2011N02A0260 }}</ref> If these methods do not work, medicines are usually the next step in treating cardiovascular diseases and, with improvements, have increasingly become the most effective method over the long term.<ref>{{Cite journal |last1=Gupta |first1=Keshav Kumar |last2=Ali |first2=Shair |last3=Sanghera |first3=Ranjodh Singh |date=June 2019 |title=Pharmacological Options in Atherosclerosis: A Review of the Existing Evidence |journal=Cardiology and Therapy |volume=8 |issue=1 |pages=5–20 |doi=10.1007/s40119-018-0123-0 |pmc=6525235 |pmid=30543029}}</ref> | |||
| ], upper normal and especially elevated blood sugar, i.e. ], high blood pressure, ], stopping smoking, taking ]s (anti-clotting agents) which target clotting factors, taking omega 3 oils from fatty fish or plant oils such as flax or canola oils, exercising and losing weight are the usual focus of treatments which have proved to be helpful in clinical trials. The target serum cholesterol level is ideally equal or less than 4mmol/L (160 mg/dL) and triglycerides equal or less than 2mmol/L 180 (mg/dL). | |||
| The key to the more effective approaches is to combine different treatment strategies.<ref>{{cite journal | vauthors = Koh KK, Han SH, Oh PC, Shin EK, Quon MJ | title = Combination therapy for treatment or prevention of atherosclerosis: focus on the lipid-RAAS interaction | journal = Atherosclerosis | volume = 209 | issue = 2 | pages = 307–13 | date = April 2010 | pmid = 19800624 | pmc = 2962413 | doi = 10.1016/j.atherosclerosis.2009.09.007 }}</ref> In addition, for those approaches, such as lipoprotein transport behaviors, which have been shown to produce the most success, adopting more aggressive combination treatment strategies taken daily and indefinitely has generally produced better results, both before and especially after people are symptomatic.<ref name="Fonarow, G 2003"/> | |||
| In general, the group of medications referred to as statins has seen popularity yet they are not approved in most jurisdictions for treating atherosclerosis. They have relatively few short-term undesirable side-effects and have shown some effect in reducing atherosclerotic disease 'events' in some but not all studies such as . | |||
| ===Statins=== | |||
| The newest statin, ], has been the first to demonstrate regression of atherosclerotic plaque within the ] by ] evaluation,<ref name=Nissen "JAMA">, "Effect of Very High-Intensity Statin Therapy on Regression of Coronary Atherosclerosis".</ref> see the ''Effect of Very High-Intensity Statin Therapy'' reference below. The study was not set up to demonstrate clinical benefit or harm. However, for most people, changing their physiologic behaviors, from the usual high risk to greatly reduced risk, requires a combination of several compounds, taken on a daily basis and indefinitely. More and more human treatment trials have been done and are ongoing which demonstrate improved outcome for those people using more complex and effective treatment regimens which change physiologic behaviour patterns to more closely resemble those humans exhibit in childhood at a time before ] begin forming. | |||
| ] medications are widely prescribed for treating atherosclerosis. They have shown benefit in reducing cardiovascular disease and mortality in those with ] with few side effects.<ref>{{cite journal |last1=Taylor |first1=Fiona |last2=Huffman |first2=Mark D |last3=Macedo |first3=Ana Filipa |last4=Moore |first4=Theresa HM |last5=Burke |first5=Margaret |last6=Davey Smith |first6=George |last7=Ward |first7=Kirsten |last8=Ebrahim |first8=Shah |last9=Gay |first9=Hawkins C |title=Statins for the primary prevention of cardiovascular disease |journal=Cochrane Database of Systematic Reviews |date=31 January 2013 |volume=2021 |issue=9 |pages=CD004816 |doi=10.1002/14651858.CD004816.pub5 |pmid=23440795 |pmc=6481400 }}</ref> Secondary prevention therapy, which includes high-intensity statins and aspirin, is recommended by multi-society guidelines for all patients with a history of ASCVD (atherosclerotic cardiovascular disease) to prevent the recurrence of coronary artery disease, ischemic stroke, or peripheral arterial disease.<ref>{{cite journal | vauthors = Virani SS, Smith SC, Stone NJ, Grundy SM | title = Secondary Prevention for Atherosclerotic Cardiovascular Disease: Comparing Recent US and European Guidelines on Dyslipidemia | journal = Circulation | volume = 141 | issue = 14 | pages = 1121–1123 | date = April 2020 | pmid = 32250694 | doi = 10.1161/CIRCULATIONAHA.119.044282 | doi-access = free }}</ref><ref>{{cite journal |last1=Grundy |first1=Scott M. |last2=Stone |first2=Neil J. |last3=Bailey |first3=Alison L. |last4=Beam |first4=Craig |last5=Birtcher |first5=Kim K. |last6=Blumenthal |first6=Roger S. |last7=Braun |first7=Lynne T. |last8=de Ferranti |first8=Sarah |last9=Faiella-Tommasino |first9=Joseph |last10=Forman |first10=Daniel E. |last11=Goldberg |first11=Ronald |last12=Heidenreich |first12=Paul A. |last13=Hlatky |first13=Mark A. |last14=Jones |first14=Daniel W. |last15=Lloyd-Jones |first15=Donald |last16=Lopez-Pajares |first16=Nuria |last17=Ndumele |first17=Chiadi E. |last18=Orringer |first18=Carl E. |last19=Peralta |first19=Carmen A. |last20=Saseen |first20=Joseph J. |last21=Smith |first21=Sidney C. |last22=Sperling |first22=Laurence |last23=Virani |first23=Salim S. |last24=Yeboah |first24=Joseph |title=2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol |journal=Journal of the American College of Cardiology |date=June 2019 |volume=73 |issue=24 |pages=e285–e350 |doi=10.1016/j.jacc.2018.11.003 |pmid=30423393 |hdl=20.500.12749/1738 |hdl-access=free }}</ref> However, prescription of and adherence to these guideline-concordant therapies is lacking, particularly among young patients and women.<ref>{{cite journal | vauthors = Nanna MG, Wang TY, Xiang Q, Goldberg AC, Robinson JG, Roger VL, Virani SS, Wilson PW, Louie MJ, Koren A, Li Z, Peterson ED, Navar AM | display-authors = 6 | title = Sex Differences in the Use of Statins in Community Practice | journal = Circulation: Cardiovascular Quality and Outcomes | volume = 12 | issue = 8 | pages = e005562 | date = August 2019 | pmid = 31416347 | pmc = 6903404 | doi = 10.1161/CIRCOUTCOMES.118.005562 }}</ref><ref>{{cite journal | vauthors = Lee MT, Mahtta D, Ramsey DJ, Liu J, Misra A, Nasir K, Samad Z, Itchhaporia D, Khan SU, Schofield RS, Ballantyne CM, Petersen LA, Virani SS | display-authors = 6 | title = Sex-Related Disparities in Cardiovascular Health Care Among Patients With Premature Atherosclerotic Cardiovascular Disease | journal = JAMA Cardiology | volume = 6 | issue = 7 | pages = 782–790 | date = July 2021 | pmid = 33881448 | pmc = 8060887 | doi = 10.1001/jamacardio.2021.0683 }}</ref> | |||
| ]s work by inhibiting HMG-CoA (hydroxymethylglutaryl-coenzyme A) reductase, a hepatic rate-limiting enzyme in cholesterol's biochemical production pathway. Inhibiting this rate-limiting enzyme reduces the body's ability to produce as much cholesterol endogenously, thereby reducing the level of LDL-cholesterol in the blood. This reduced endogenous cholesterol production triggers the body to then pull cholesterol from other cellular sources, enhancing serum HDL-cholesterol.{{citation needed|date=January 2021}} These data are primarily in middle-aged men and the conclusions are less clear for women and people over the age of 70.<ref>{{cite journal | vauthors = Vos E, Rose CP | title = Questioning the benefits of statins | journal = CMAJ | volume = 173 | issue = 10 | pages = 1207; author reply 1210 | date = November 2005 | pmid = 16275976 | pmc = 1277053 | doi = 10.1503/cmaj.1050120 }}</ref> | |||
| Lowering ], a genetic variant of LDL, can be achieved with large daily doses of vitamin B3, niacin. Niacin also tends to shift LDL particle distribution to larger particle size and improve HDL functioning. Work on increasing HDL particle concentration and function, beyond the niacin effect, perhaps even more important, is slowly advancing. Combinations of ]s, ], intestinal cholesterol absorption inhibiting supplements (] and others, and to a much lesser extent ]s have been the most successful in changing ] patterns and but, in the case of inhibitors and fibrates without improving clinical outcomes in secondary prevention. In primary prevention, cholesterol lowering agents have not reduced the mortality rates, for example the AFCAPS/TexCAPS and EXCEL trials and the 2 main trials with atorvastatin, Lipitor, as in the ASCOT and SPARCL studies. Dietary changes to achieve benefit have been more controversial, generally far less effective and less widely adhered to with success. | |||
| ===Surgery=== | |||
| Evidence has increased that people with ], despite not having clinically detectable atherosclotic disease, have more severe debility from atherosclerotic events over time than even non-diabetics who have already suffered atherosclerotic events. Thus ] has been upgraded to be viewed as an advanced atherosclerotic disease equivalent. | |||
| When atherosclerosis has become severe and caused irreversible ], such as ] in the case of ], surgery may be indicated. ] can re-establish flow around the diseased segment of the artery, and ] with or without ]ing can reopen narrowed arteries and improve blood flow. ] without manipulation of the ascending aorta has demonstrated reduced rates of postoperative stroke and mortality compared to traditional on-pump coronary revascularization.<ref>{{cite journal | vauthors = Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, Thourani V, Lamy A, Taggart DP, Puskas JD, Vallely MP | title = Coronary Artery Bypass Grafting With and Without Manipulation of the Ascending Aorta: A Network Meta-Analysis | journal = Journal of the American College of Cardiology | volume = 69 | issue = 8 | pages = 924–936 | date = February 2017 | pmid = 28231944 | doi = 10.1016/j.jacc.2016.11.071 | doi-access = free }}</ref> | |||
| ===Other=== | |||
| Lowering ] levels, including within the normal range and dietary supplements of Omega 3 oils, especially those from the muscle of some deep salt water living fish species, also have clinical evidence of significant protective effects as confirmed by 6 ] ] ] human clinical trials. | |||
| There is evidence that some ]s, particularly ], which inhibit clot formation by interfering with ] metabolism, may promote arterial calcification in the long term despite reducing clot formation in the short term.<ref>{{cite journal | vauthors = Vlasschaert C, Goss CJ, Pilkey NG, McKeown S, Holden RM | title = Vitamin K Supplementation for the Prevention of Cardiovascular Disease: Where Is the Evidence? A Systematic Review of Controlled Trials | journal = Nutrients | volume = 12 | issue = 10 | pages = 2909 | date = September 2020 | pmid = 32977548 | pmc = 7598164 | doi = 10.3390/nu12102909 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Price PA, Faus SA, Williamson MK | title = Warfarin-induced artery calcification is accelerated by growth and vitamin D | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 20 | issue = 2 | pages = 317–327 | date = February 2000 | pmid = 10669626 | doi = 10.1161/01.ATV.20.2.317 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Geleijnse JM, Vermeer C, Grobbee DE, Schurgers LJ, Knapen MH, van der Meer IM, Hofman A, Witteman JC | display-authors = 6 | title = Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam Study | journal = The Journal of Nutrition | volume = 134 | issue = 11 | pages = 3100–3105 | date = November 2004 | pmid = 15514282 | doi = 10.1093/jn/134.11.3100 | doi-access = free | hdl = 1765/10366 | hdl-access = free }}</ref><ref>{{cite web |url=http://lpi.oregonstate.edu/infocenter/vitamins/vitaminK/ |title=Vitamin K |publisher=Linus Pauling Institute at Oregon State University |access-date=2010-03-25 | archive-url= https://web.archive.org/web/20100407093811/http://lpi.oregonstate.edu/infocenter/vitamins/vitaminK/| archive-date= 7 April 2010 | url-status= live}}</ref>{{excessive citations inline|date=October 2021}} Also, small molecules such as ] and ] have shown vasculoprotective effects to reduce risk of atherosclerosis.<ref name="pmid25411835">{{cite journal | vauthors = Kong BS, Cho YH, Lee EJ | title = G protein-coupled estrogen receptor-1 is involved in the protective effect of protocatechuic aldehyde against endothelial dysfunction | journal = PLOS ONE | volume = 9 | issue = 11 | pages = e113242 | date = 2014 | pmid = 25411835 | pmc = 4239058 | doi = 10.1371/journal.pone.0113242 | doi-access = free | bibcode = 2014PLoSO...9k3242K }}</ref><ref name="pmid27002821">{{cite journal | vauthors = Kong BS, Im SJ, Lee YJ, Cho YH, Do YR, Byun JW, Ku CR, Lee EJ | display-authors = 6 | title = Vasculoprotective Effects of 3-Hydroxybenzaldehyde against VSMCs Proliferation and ECs Inflammation | journal = PLOS ONE | volume = 11 | issue = 3 | pages = e0149394 | date = 2016 | pmid = 27002821 | pmc = 4803227 | doi = 10.1371/journal.pone.0149394 | doi-access = free | bibcode = 2016PLoSO..1149394K }}</ref> | |||
| ==Epidemiology== | |||
| Aerobic exercise, weight loss, and dietary changes can also help, but are generally much less effective and often more problematic for many to achieve and continue long term.{{Fact|date=June 2007}} | |||
| Cardiovascular disease, which is predominantly the clinical manifestation of atherosclerosis, is one of the leading causes of death worldwide.<ref>{{Cite web|url=https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death|title=The top 10 causes of death|website=www.who.int|language=en|access-date=2020-01-26}}</ref> | |||
| Almost all children older than age 10 in ] have ] fatty streaks, with ] fatty streaks beginning in ].<ref name="Robbins">Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; & Mitchell, Richard N. (2007). ''Robbins Basic Pathology'' (8th ed.). Saunders Elsevier. pp. 348-351 {{ISBN|978-1-4160-2973-1}}</ref><ref>{{Cite journal |last1=Strong |first1=J. P. |last2=McGill |first2=H. C. |date=1969-05-06 |title=The pediatric aspects of atherosclerosis |journal=Journal of Atherosclerosis Research |language=en |volume=9 |issue=3 |pages=251–265 |doi=10.1016/S0368-1319(69)80020-7 |pmid=5346899 }}</ref><ref>{{Cite journal |last1=Zieske |first1=Arthur W. |last2=Malcom |first2=Gray T. |last3=Strong |first3=Jack P. |date=January 2002 |title=Natural history and risk factors of atherosclerosis in children and youth: The PDAY study |journal=Pediatric Pathology & Molecular Medicine |volume=21 |issue=2 |pages=213–237 |doi=10.1080/pdp.21.2.213.237 |pmid=11942537 }}</ref> | |||
| Medical treatments often focus predominantly on the symptoms. However, over time, the treatments which focus on decreasing the underlying atherosclerosis processes, as opposed to simply treating the symptoms resulting from the atherosclerosis, have been shown by clinical trials to be more effective. | |||
| In 1953, a study was published that examined the results of 300 autopsies performed on U.S. soldiers who had died in the ]. Despite the average age of the soldiers being just 22 years old, 77% of them had visible signs of coronary atherosclerosis. This study showed that heart disease could affect people at a younger age and was not just a problem for older individuals.<ref>{{cite journal |last1=Enos |first1=William F. |title=CORONARY DISEASE AMONG UNITED STATES SOLDIERS KILLED IN ACTION IN KOREA: PRELIMINARY REPORT |journal=Journal of the American Medical Association |date=18 July 1953 |volume=152 |issue=12 |pages=1090–1093 |doi=10.1001/jama.1953.03690120006002 |pmid=13052433 }}</ref><ref>{{Cite web |title=Stopping Heart Disease in Childhood |url=https://nutritionfacts.org/2014/07/15/stopping-heart-disease-in-childhood/ |access-date=2022-12-08 |website=NutritionFacts.org |date=15 July 2014 |language=en-US}}</ref><ref>{{cite book |last1=Wilson |first1=Don P. |title=Endotext |date=2000 |publisher=MDText.com, Inc. |chapter-url=http://www.ncbi.nlm.nih.gov/books/NBK395576/ |chapter=Is Atherosclerosis a Pediatric Disease? |pmid=27809437 }}</ref> | |||
| Other physical treatments, helpful in the short term, include minimally invasive ] procedures to physically expand narrowed arteries and major invasive surgery, such as ], to create additional blood supply connections which go around the more severely narrowed areas. | |||
| In 1992, a report showed that microscopic fatty streaks were seen in the ] in over 50% of children aged 10–14 and 8% had even more advanced lesions with more accumulations of extracellular lipid.<ref>{{cite journal |last1=Strong |first1=Jack P. |last2=Malcom |first2=Gray T. |last3=Newman |first3=William P. |last4=Oalmann |first4=Margaret C. |title=Early Lesions of Atherosclerosis in Childhood and Youth: Natural History and Risk Factors |journal=Journal of the American College of Nutrition |date=June 1992 |volume=11 |issue=sup1 |pages=51S–54S |doi=10.1080/07315724.1992.10737984 |pmid=1619200 }}</ref> | |||
| High dose supplements of vitamin E or C, with the goal of improving ] protection, have failed to produce any beneficial trends in human, double blind, clinical research trials. However, these trials have consistently used lower doses than those claimed to be effective and have ignored the short half life of high intakes of ] in the body. | |||
| A 2005 report of a study done between 1985 and 1995 found that around 87% of aortas and 30% of coronary arteries in the age group 5–14 years had fatty streaks which increased with age.<ref>{{cite journal |last1=Mendis |first1=Shanthi |last2=Nordet |first2=P. |last3=Fernandez-Britto |first3=J.E. |last4=Sternby |first4=N. |title=Atherosclerosis in children and young adults: An overview of the World Health Organization and International Society and Federation of Cardiology study on Pathobiological Determinants of Atherosclerosis in Youth study (1985–1995) |journal=Global Heart |date=March 2005 |volume=1 |issue=1 |pages=3 |doi=10.1016/j.precon.2005.02.010 |doi-access=free }}</ref> | |||
| On the other hand, the ]s, and some other medications have been shown to have ] effects, possibly part of their basis for some of their therapeutic success in reducing cardiac 'events'. | |||
| == Etymology == | |||
| The success of statin drugs in clinical trials is based on some reductions in mortality rates, however never in women or people over the age of 70 . For example, in 4S, the first large placebo controlled, randomized clinical trial of a statin in people with advanced disease who had already suffered a heart attack, the overall mortality rate reduction for those taking the statin, vs. placebo, was 30%. For the subgroup of people in the trial who had Diabetes Mellitus, the mortality rate reduction between statin and placebo was 54%. 4S was a 5.4 year trial which started in 1989 and was published in 1995 after completion. There were 3 more dead women at trial's end on statin than in the group on placebo drug. The trial, mentioned above and in reference 3, has been the first to show actual disease volume regression (see page 8 of the paper which shows cross-sectional areas of the total heart artery wall at start and 2 years of rosuvastatin 40 mg/day treatment); however, its design was not able to "prove" the mortality reduction issue since it has no placebo group. | |||
| The following terms are similar, yet distinct, in both spelling and meaning, and can be easily confused: ], ], and atherosclerosis. ''Arteriosclerosis'' is a general term describing any hardening (and loss of elasticity) of medium or large arteries ({{ety|gre|''ἀρτηρία'' (artēria)|artery||''σκλήρωσις'' (])|hardening}}); ''arteriolosclerosis'' is any hardening (and loss of elasticity) of ]s (small arteries); ''atherosclerosis'' is a hardening of an artery specifically due to an ] ({{ety|grc| ''ἀθήρα'' (athḗra)|gruel}}). The term ''atherogenic'' is used for substances or processes that cause the formation of ].<ref>{{cite web | title = Atherogenic | url = https://www.merriam-webster.com/dictionary/atherogenic | work = Merriam-Webster Dictionary }}</ref> | |||
| ==Economics== | |||
| In summary, the key to the more effective approaches has been better understanding of the widespread and insidious nature of the disease and to combine multiple different treatment strategies, not rely on just one or a few approaches. Additionally, for those approaches, such as lipoprotein transport behaviors, which have been shown to produce the most success, adopting more aggressive combination treatment strategies has generally produced better results, both before and especially after people are symptomatic. However, treating asymptomatic people remains controversial in the medical community. | |||
| In 2011, coronary atherosclerosis was one of the top ten most expensive conditions seen during inpatient hospitalizations in the US, with aggregate inpatient hospital costs of $10.4 billion.<ref>{{cite journal |vauthors=Pfuntner A, Wier LM, Steiner C | title = Costs for Hospital Stays in the United States, 2011. | journal =HCUP Statistical Brief |issue=168 | publisher = Agency for Healthcare Research and Quality | location = Rockville, MD | date = December 2013 | pmid = 24455786 | url = http://hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.jsp }}</ref> | |||
| == Research == | |||
| Patients at risk for atherosclerosis-related diseases are increasingly being treated ] with low-dose ] and a ]. The high incidence of cardiovascular disease led Wald and Law<ref name="Polypill">Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80%. '']'' 2003;326:1419. PMID.</ref> to propose a '']'', a once-daily pill containing these two types of drugs in addition to an ], ] and ] and ]. They maintain that high uptake by the general population by such a ''Polypill'' would reduce cardiovascular mortality by 80%. It must be emphasized however that this is purely theoretical, as the Polypill has never been tested in a clinical trial. | |||
| ===Lipids=== | |||
| An indication of the role of ] (HDL) on atherosclerosis has been with the rare ] human genetic variant of this ] protein. A small short-term trial using bacterial synthesized human ] HDL in people with unstable angina produced a fairly dramatic reduction in measured coronary plaque volume in only six weeks vs. the usual increase in plaque volume in those randomized to placebo. The trial was published in '']'' in early 2006.{{Citation needed|date=February 2018}} Ongoing work starting in the 1990s may lead to human clinical trials—probably by about 2008.{{update inline|date=June 2014}} These may use synthesized Apo-A1 Milano HDL directly, or they may use gene-transfer methods to pass the ability to synthesize the Apo-A1 Milano HDLipoprotein.{{Citation needed|date=February 2018}} | |||
| Methods to increase HDL particle concentrations, which in some animal studies largely reverses and removes atheromas, are being developed and researched.{{Citation needed|date=February 2018}} However, increasing HDL by any means is not necessarily helpful. For example, the drug ] is the most effective agent currently known for raising HDL (by up to 60%). However, in clinical trials, it also raised deaths by 60%. All studies regarding this drug were halted in December 2006.<ref>{{cite journal | vauthors = Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, Lopez-Sendon J, Mosca L, Tardif JC, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer B | title = Effects of torcetrapib in patients at high risk for coronary events | journal = The New England Journal of Medicine | volume = 357 | issue = 21 | pages = 2109–22 | date = November 2007 | pmid = 17984165 | doi = 10.1056/NEJMoa0706628 | doi-access = free }}</ref> | |||
| == Recent research == | |||
| Methods to increase ] (HDL) particle concentrations, which in some animal studies largely reverses and remove atheromas, are being developed and researched. ] has HDL raising effects (by 10 - 30%) and showed clinical trial benefit in the Coronary Drug Project, however, the drug ] most effectively raising HDL (by 60%) also raised deaths by 60% and all studies regarding this drug were halted in December 2006. | |||
| The actions of ]s drive atherosclerotic plaque progression. | |||
| An indication of the role of HDL on atherosclerosis has been with the rare Apo-A1 Milano human genetic variant of this HDL protein. Ongoing work starting in the 1990s may lead to human clinical trials probably by about 2008, on using either synthesized Apo-A1 Milano HDL directly or by gene-transfer methods to pass the ability to synthesize the Apo-A1 Milano HDL protein. | |||
| ''Immunomodulation of atherosclerosis'' is the term for techniques that modulate immune system function to suppress this macrophage action.<ref name=Nilsson>{{cite journal | vauthors = Nilsson J, Hansson GK, Shah PK | title = Immunomodulation of atherosclerosis: implications for vaccine development | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 25 | issue = 1 | pages = 18–28 | date = January 2005 | pmid = 15514204 | doi = 10.1161/01.ATV.0000149142.42590.a2 | doi-access = free }}</ref> | |||
| Involvement of ] chain reaction in atherogenesis<ref>{{cite journal | vauthors = Spiteller G | title = The relation of lipid peroxidation processes with atherogenesis: a new theory on atherogenesis | journal = Molecular Nutrition & Food Research | volume = 49 | issue = 11 | pages = 999–1013 | date = November 2005 | pmid = 16270286 | doi = 10.1002/mnfr.200500055 }}</ref> triggered research on the protective role of the heavy isotope (]) ]s (D-PUFAs) that are less prone to oxidation than ordinary PUFAs (H-PUFAs). PUFAs are ] – they are involved in metabolism in that very form as they are consumed with food. In ], that are a model for human-like lipoprotein metabolism, adding D-PUFAs to diet indeed reduced body weight gain, improved cholesterol handling and reduced atherosclerotic damage to the aorta.<ref>{{cite journal | vauthors = Berbée JF, Mol IM, Milne GL, Pollock E, Hoeke G, Lütjohann D, Monaco C, Rensen PC, van der Ploeg LH, Shchepinov MS | title = Deuterium-reinforced polyunsaturated fatty acids protect against atherosclerosis by lowering lipid peroxidation and hypercholesterolemia | journal = Atherosclerosis | volume = 264 | pages = 100–107 | date = September 2017 | pmid = 28655430 | doi = 10.1016/j.atherosclerosis.2017.06.916 | url = https://ora.ox.ac.uk/objects/uuid:378458c5-65e0-4891-bb60-cc458455b81b }}</ref><ref>{{cite journal | vauthors = Tsikas D | title = Combating atherosclerosis with heavy PUFAs: Deuteron not proton is the first | journal = Atherosclerosis | volume = 264 | pages = 79–82 | date = September 2017 | pmid = 28756876 | doi = 10.1016/j.atherosclerosis.2017.07.018 }}</ref> | |||
| The ASTEROID trial used a high-dose of a powerful statin, ], and found plaque (intima + media volume) reduction; see the ''Effect of Very High-Intensity Statin Therapy'' reference below. No attempt has yet been made to compare this drug with placebo regarding clinical benefit. | |||
| ===miRNA=== | |||
| Since about 2002, progress in understanding and developing techniques for modulating immune system function so as to significantly suppress the action of macrophages to drive atherosclerotic plaque progression are being developed with considerable success in reducing plaque development in both mice and rabbits. Plans for human trials, hoped for by about 2008, are in progress. Generally these techniques are termed immunomodulation of atherosclerosis. | |||
| ]s (miRNAs) have complementary sequences in the ] and ] of target mRNAs of protein-coding genes, and cause mRNA cleavage or repression of translational machinery. In diseased vascular vessels, miRNAs are dysregulated and highly expressed. ] is found in cardiovascular diseases.<ref name="ReferenceA">{{cite journal | vauthors = Chen WJ, Yin K, Zhao GJ, Fu YC, Tang CK | title = The magic and mystery of microRNA-27 in atherosclerosis | journal = Atherosclerosis | volume = 222 | issue = 2 | pages = 314–23 | date = June 2012 | pmid = 22307089 | doi = 10.1016/j.atherosclerosis.2012.01.020 }}</ref> It is involved in atherosclerotic initiation and progression including ], ] and ], cell type progression and proliferation, and ] differentiation. It was found in rodents that the inhibition of ] will raise HDL-C levels and the expression of miR-33 is down-regulated in humans with atherosclerotic plaques.<ref name="pmid22488426">{{cite journal | vauthors = Sacco J, Adeli K | title = MicroRNAs: emerging roles in lipid and lipoprotein metabolism | journal = Current Opinion in Lipidology | volume = 23 | issue = 3 | pages = 220–5 | date = June 2012 | pmid = 22488426 | doi = 10.1097/MOL.0b013e3283534c9f }}</ref><ref name="pmid21356514">{{cite journal | vauthors = Bommer GT, MacDougald OA | title = Regulation of lipid homeostasis by the bifunctional SREBF2-miR33a locus | journal = Cell Metabolism | volume = 13 | issue = 3 | pages = 241–7 | date = March 2011 | pmid = 21356514 | pmc = 3062104 | doi = 10.1016/j.cmet.2011.02.004 }}</ref><ref name="pmid21646721">{{cite journal | vauthors = Rayner KJ, Sheedy FJ, Esau CC, Hussain FN, Temel RE, Parathath S, van Gils JM, Rayner AJ, Chang AN, Suarez Y, Fernandez-Hernando C, Fisher EA, Moore KJ | title = Antagonism of miR-33 in mice promotes reverse cholesterol transport and regression of atherosclerosis | journal = The Journal of Clinical Investigation | volume = 121 | issue = 7 | pages = 2921–31 | date = July 2011 | pmid = 21646721 | pmc = 3223840 | doi = 10.1172/JCI57275 }}</ref> | |||
| miR-33a and miR-33b are located on ] 16 of human sterol regulatory element-binding protein 2 (]) gene on ] and intron 17 of ] gene on chromosome 17.<ref name="pmid22395363">{{cite journal | vauthors = Iwakiri Y | title = A role of miR-33 for cell cycle progression and cell proliferation | journal = Cell Cycle | volume = 11 | issue = 6 | pages = 1057–8 | date = March 2012 | pmid = 22395363 | doi = 10.4161/cc.11.6.19744 | doi-access = free }}</ref> miR-33a/b regulates cholesterol/lipid homeostasis by binding in the ] of genes involved in cholesterol transport such as ] (ABC) transporters and enhance or represses its expression. Studies have shown that ] mediates cholesterol transport from peripheral tissues to Apolipoprotein-1. It is also important in the reverse cholesterol transport pathway, where cholesterol is delivered from peripheral tissue to the liver, where it can be excreted into ] or converted to ]s before excretion.<ref name="ReferenceA"/> Therefore, ABCA1 prevents cholesterol accumulation in macrophages. By enhancing miR-33 function, the level of ABCA1 is decreased, leading to decreased cellular cholesterol efflux to apoA-1. On the other hand, by inhibiting miR-33 function, the level of ABCA1 is increased and increases the cholesterol efflux to ]. Suppression of miR-33 will lead to less cellular cholesterol and higher plasma HDL level through the regulation of ABCA1 expression.<ref name="pmid16728652">{{cite journal | vauthors = Singaraja RR, Stahmer B, Brundert M, Merkel M, Heeren J, Bissada N, Kang M, Timmins JM, Ramakrishnan R, Parks JS, Hayden MR, Rinninger F | title = Hepatic ATP-binding cassette transporter A1 is a key molecule in high-density lipoprotein cholesteryl ester metabolism in mice | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 26 | issue = 8 | pages = 1821–7 | date = August 2006 | pmid = 16728652 | doi = 10.1161/01.ATV.0000229219.13757.a2 | doi-access = free }}</ref> | |||
| Genetic expression and control mechanism research, including (a) the PPAR ] known to be important in blood sugar and variants of lipoprotein production and function and (b) of the multiple variants of the proteins which form the lipoprotein transport particles, is progressing. | |||
| The sugar, ], removed cholesterol that had built up in the arteries of mice fed a high-fat diet.<ref>{{cite journal | vauthors = Zimmer S, Grebe A, Bakke SS, Bode N, Halvorsen B, Ulas T, Skjelland M, De Nardo D, Labzin LI, Kerksiek A, Hempel C, Heneka MT, Hawxhurst V, Fitzgerald ML, Trebicka J, Björkhem I, Gustafsson JÅ, Westerterp M, Tall AR, Wright SD, Espevik T, Schultze JL, Nickenig G, Lütjohann D, Latz E | title = Cyclodextrin promotes atherosclerosis regression via macrophage reprogramming | journal = Science Translational Medicine | volume = 8 | issue = 333 | pages = 333ra50 | date = April 2016 | pmid = 27053774 | pmc = 4878149 | doi = 10.1126/scitranslmed.aad6100 }} | |||
| Some controversial research has suggested a link between atherosclerosis and the presence of several different ] in the arteries, e.g. ], though trials of current antibiotic treatments known to be usually effective in suppressing growth or killing these bacteria have not been successful in improving outcomes. | |||
| * {{lay source |template=cite news|vauthors = Hesman Saey T|url= https://www.sciencenews.org/article/sugar-can-melt-away-cholesterol|title = A sugar can melt away cholesterol|date = April 8, 2016|website = Science News.org }}</ref> | |||
| ===DNA damage=== | |||
| The immunomodulation approaches mentioned above, because they deal with innate responses of the host to promote atherosclerosis, have far greater prospects for success. | |||
| ] is the most important risk factor for cardiovascular problems. The causative basis by which aging mediates its impact, independently of other recognized risk factors, remains to be determined. Evidence has been reviewed for a key role of ] in vascular aging.<ref name="pmid23953979">{{cite journal | vauthors = Wu H, Roks AJ | title = Genomic instability and vascular aging: a focus on nucleotide excision repair | journal = Trends in Cardiovascular Medicine | volume = 24 | issue = 2 | pages = 61–8 | date = February 2014 | pmid = 23953979 | doi = 10.1016/j.tcm.2013.06.005 }}</ref><ref name="pmid27213333">{{cite journal | vauthors = Bautista-Niño PK, Portilla-Fernandez E, Vaughan DE, Danser AH, Roks AJ | title = DNA Damage: A Main Determinant of Vascular Aging | journal = International Journal of Molecular Sciences | volume = 17 | issue = 5 | pages = 748 | date = May 2016 | pmid = 27213333 | pmc = 4881569 | doi = 10.3390/ijms17050748 | doi-access = free }}</ref><ref name="pmid28347738">{{cite journal | vauthors = Shah AV, Bennett MR | title = DNA damage-dependent mechanisms of ageing and disease in the macro- and microvasculature | journal = European Journal of Pharmacology | volume = 816 | pages = 116–128 | date = December 2017 | pmid = 28347738 | doi = 10.1016/j.ejphar.2017.03.050 | url = https://www.repository.cam.ac.uk/handle/1810/264776 }}</ref> | |||
| ], a common type of oxidative damage in ], is found to accumulate in plaque ] cells, ]s and ],<ref name="pmid12186795">{{cite journal | vauthors = Martinet W, Knaapen MW, De Meyer GR, Herman AG, Kockx MM | title = Elevated levels of oxidative DNA damage and DNA repair enzymes in human atherosclerotic plaques | journal = Circulation | volume = 106 | issue = 8 | pages = 927–32 | date = August 2002 | pmid = 12186795 | doi = 10.1161/01.cir.0000026393.47805.21 | doi-access = free }}</ref> thus linking DNA damage to plaque formation. DNA strand breaks also increased in atherosclerotic plaques.<ref name="pmid12186795" /> ] (WS) is a premature aging condition in humans.<ref name="pmid24334614">{{cite journal | vauthors = Ishida T, Ishida M, Tashiro S, Yoshizumi M, Kihara Y | title = Role of DNA damage in cardiovascular disease | journal = Circulation Journal | volume = 78 | issue = 1 | pages = 42–50 | year = 2014 | pmid = 24334614 | doi = 10.1253/circj.CJ-13-1194| doi-access = free }}</ref> WS is caused by a genetic defect in a ] that is employed in several ]. WS patients develop a considerable burden of atherosclerotic plaques in their ] and ]: calcification of the aortic valve is also frequently observed.<ref name="pmid27213333" /> These findings link excessive unrepaired DNA damage to premature aging and early atherosclerotic plaque development (see ]).{{citation needed|date=December 2020}} | |||
| ===Microorganisms=== | |||
| ==References== | |||
| The ] – all the ]s in the body, can contribute to atherosclerosis in many ways: modulation of the ], changes in ], processing of nutrients and production of certain metabolites that can get into blood circulation.<ref name="nature.com">{{cite journal | vauthors = Barrington WT, Lusis AJ | title = Atherosclerosis: Association between the gut microbiome and atherosclerosis | journal = Nature Reviews. Cardiology | volume = 14 | issue = 12 | pages = 699–700 | date = December 2017 | pmid = 29099096 | pmc = 5815826 | doi = 10.1038/nrcardio.2017.169 }}</ref> One such metabolite, produced by ], is ] (TMAO). Its levels have been associated with atherosclerosis in human studies and animal research suggests that may be a causal relation. An association between the bacterial genes encoding trimethylamine lyases — the ]s involved in TMAO generation — and atherosclerosis has been noted.<ref name="pmid29018189">{{cite journal | vauthors = Jie Z, Xia H, Zhong SL, Feng Q, Li S, Liang S, Zhong H, Liu Z, Gao Y, Zhao H, Zhang D, Su Z, Fang Z, Lan Z, Li J, Xiao L, Li J, Li R, Li X, Li F, Ren H, Huang Y, Peng Y, Li G, Wen B, Dong B, Chen JY, Geng QS, Zhang ZW, Yang H, Wang J, Wang J, Zhang X, Madsen L, Brix S, Ning G, Xu X, Liu X, Hou Y, Jia H, He K, Kristiansen K | display-authors = 6 | title = The gut microbiome in atherosclerotic cardiovascular disease | journal = Nature Communications | volume = 8 | issue = 1 | pages = 845 | date = October 2017 | pmid = 29018189 | pmc = 5635030 | doi = 10.1038/s41467-017-00900-1 | bibcode = 2017NatCo...8..845J }}</ref><ref name="nature.com"/> | |||
| <references />5. Stevens, Karen M.J. Douglas, Athanasios N. Saratzis and George D. Kitas Inflammation and atherosclerosis in rheumatoid arthritis Robert J. Expert Rev. Mol. Med. Vol. 7, Issue 7 | |||
| === Vascular smooth muscle cells === | |||
| 6. Mol, A 2002 _The Body Multiple: Ontology in medical practice_ London: Duke University Press | |||
| ] play a key role in atherogenesis and were historically considered to be beneficial for plaque stability by forming a protective fibrous cap and synthesizing strength-giving ] components.<ref name="Harman & Jørgensen 2019">{{cite journal | vauthors = Harman JL, Jørgensen HF | title = The role of smooth muscle cells in plaque stability: Therapeutic targeting potential | journal = British Journal of Pharmacology | volume = 176 | issue = 19 | pages = 3741–3753 | date = October 2019 | pmid = 31254285 | pmc = 6780045 | doi = 10.1111/bph.14779 }}</ref><ref>{{cite journal | vauthors = Bennett MR, Sinha S, Owens GK | title = Vascular Smooth Muscle Cells in Atherosclerosis | journal = Circulation Research | volume = 118 | issue = 4 | pages = 692–702 | date = February 2016 | pmid = 26892967 | pmc = 4762053 | doi = 10.1161/CIRCRESAHA.115.306361 }}</ref> However, in addition to the fibrous cap, vascular smooth muscle cells also give rise to many of the cell types found within the plaque core and can modulate their phenotype to both promote and reduce plaque stability.<ref name="Harman & Jørgensen 2019" /><ref>{{cite journal | vauthors = Gomez D, Shankman LS, Nguyen AT, Owens GK | title = Detection of histone modifications at specific gene loci in single cells in histological sections | journal = Nature Methods | volume = 10 | issue = 2 | pages = 171–177 | date = February 2013 | pmid = 23314172 | pmc = 3560316 | doi = 10.1038/nmeth.2332 }}</ref><ref name="auto">{{cite journal | vauthors = Wang Y, Dubland JA, Allahverdian S, Asonye E, Sahin B, Jaw JE, Sin DD, Seidman MA, Leeper NJ, Francis GA | display-authors = 6 | title = Smooth Muscle Cells Contribute the Majority of Foam Cells in ApoE (Apolipoprotein E)-Deficient Mouse Atherosclerosis | journal = Arteriosclerosis, Thrombosis, and Vascular Biology | volume = 39 | issue = 5 | pages = 876–887 | date = May 2019 | pmid = 30786740 | pmc = 6482082 | doi = 10.1161/ATVBAHA.119.312434 }}</ref><ref name="Chappell 1313–1323">{{cite journal | vauthors = Chappell J, Harman JL, Narasimhan VM, Yu H, Foote K, Simons BD, Bennett MR, Jørgensen HF | display-authors = 6 | title = Extensive Proliferation of a Subset of Differentiated, yet Plastic, Medial Vascular Smooth Muscle Cells Contributes to Neointimal Formation in Mouse Injury and Atherosclerosis Models | journal = Circulation Research | volume = 119 | issue = 12 | pages = 1313–1323 | date = December 2016 | pmid = 27682618 | pmc = 5149073 | doi = 10.1161/CIRCRESAHA.116.309799 }}</ref> Vascular smooth muscle cells exhibit pronounced plasticity within atherosclerotic plaque and can modify their gene expression profile to resemble various other cell types, including ]s, ]s, ]s and osteochondrocytes.<ref>{{cite journal | vauthors = Durham AL, Speer MY, Scatena M, Giachelli CM, Shanahan CM | title = Role of smooth muscle cells in vascular calcification: implications in atherosclerosis and arterial stiffness | journal = Cardiovascular Research | volume = 114 | issue = 4 | pages = 590–600 | date = March 2018 | pmid = 29514202 | pmc = 5852633 | doi = 10.1093/cvr/cvy010 }}</ref><ref>{{cite journal | vauthors = Basatemur GL, Jørgensen HF, Clarke MC, Bennett MR, Mallat Z | title = Vascular smooth muscle cells in atherosclerosis | journal = Nature Reviews. Cardiology | volume = 16 | issue = 12 | pages = 727–744 | date = December 2019 | pmid = 31243391 | doi = 10.1038/s41569-019-0227-9 | url = https://www.repository.cam.ac.uk/handle/1810/294564 }}</ref><ref name="Harman & Jørgensen 2019"/> Importantly, genetic lineage-tracing experiments have unequivocally shown that 40-90% of plaque-resident cells are vascular smooth muscle cell-derived,<ref name="auto"/><ref name="Chappell 1313–1323"/> therefore, it is important to research the role of vascular smooth muscle cells in atherosclerosis to identify new therapeutic targets. | |||
| == |
== Notes == | ||
| {{notelist}} | |||
| * | |||
| * | |||
| == |
== References == | ||
| {{reflist}} | |||
| *] | |||
| *] | |||
| == External links == | |||
| *] | |||
| {{commons category|Atherosclerosis}} | |||
| *] | |||
| * {{wikiquote-inline}} | |||
| *] | |||
| * pathophysiology-stages and types | |||
| *] | |||
| {{Medical condition classification and resources | |||
| *] | |||
| | DiseasesDB = 1039 | |||
| *] | |||
| | ICD10 = {{ICD10|I25.0}},{{ICD10|I25.1}},{{ICD10|I70}} | |||
| *] | |||
| | ICD9 = {{ICD9|440}}, {{ICD9|414.0}} | |||
| | MedlinePlus = 000171 | |||
| | eMedicineSubj = med | |||
| | eMedicineTopic = 182 | |||
| | MeshID = D050197 | |||
| | Scholia = Q12252367 | |||
| }} | |||
| {{Vascular diseases}} | |||
| {{Authority control}} | |||
| {{Circulatory system pathology}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 07:59, 6 January 2025
Inflammatory disease involving buildup of lesions in the walls of arteries Not to be confused with Arteriosclerosis. For the journal, see Atherosclerosis (journal). Medical condition| Atherosclerosis | |
|---|---|
| Other names | Arteriosclerotic vascular disease (ASVD) |
 | |
| The progression of atherosclerosis (narrowing exaggerated) | |
| Specialty | Cardiology, angiology |
| Symptoms | None |
| Complications | Coronary artery disease, stroke, peripheral artery disease, kidney problems |
| Usual onset | Youth (worsens with age) |
| Causes | Accumulation of saturated fats, smoking, high blood pressure, and diabetes |
| Risk factors | High blood pressure, diabetes, smoking, obesity, family history, unhealthy diet (notably trans fat), chronic Vitamin C deficiency |
| Prevention | Healthy diet, exercise, not smoking, maintaining a normal weight |
| Medication | Statins, blood pressure medication, aspirin |
| Frequency | ≈100% (>65 years old) |
Atherosclerosis is a pattern of the disease arteriosclerosis, characterized by development of abnormalities called lesions in walls of arteries. This is a chronic inflammatory disease involving many different cell types and driven by elevated levels of cholesterol in the blood. These lesions may lead to narrowing of the arterial walls due to buildup of atheromatous plaques. At the onset there are usually no symptoms, but if they develop, symptoms generally begin around middle age. In severe cases, it can result in coronary artery disease, stroke, peripheral artery disease, or kidney disorders, depending on which body part(s) the affected arteries are located in the body.
The exact cause of atherosclerosis is unknown and is proposed to be multifactorial. Risk factors include abnormal cholesterol levels, elevated levels of inflammatory biomarkers, high blood pressure, diabetes, smoking (both active and passive smoking), obesity, genetic factors, family history, lifestyle habits, and an unhealthy diet. Plaque is made up of fat, cholesterol, immune cells, calcium, and other substances found in the blood. The narrowing of arteries limits the flow of oxygen-rich blood to parts of the body. Diagnosis is based upon a physical exam, electrocardiogram, and exercise stress test, among others.
Prevention guidelines include eating a healthy diet, exercising, not smoking, and maintaining normal body weight. Treatment of established atherosclerotic disease may include medications to lower cholesterol such as statins, blood pressure medication, and anticoagulant therapies to reduce the risk of blood clot formation. As the disease state progresses more invasive strategies are applied such as percutaneous coronary intervention, coronary artery bypass graft, or carotid endarterectomy. Genetic factors are also strongly implicated in the disease process; it is unlikely to be entirely based on lifestyle choices.
Atherosclerosis generally starts when a person is young and worsens with age. Females are 78% at higher risk level than men Almost all people are affected to some degree by the age of 65. It is the number one cause of death and disability in developed countries. Though it was first described in 1575, there is evidence suggesting that this disease state is genetically inherent in the broader human population, with its origins tracing back to genetic mutations that may have occurred more than two million years ago during the evolution of hominin ancestors of modern human beings.
Signs and symptoms
Atherosclerosis is typically asymptomatic for decades because the arteries enlarge at all plaque locations, thus there is no effect on blood flow. Even most plaque ruptures do not produce symptoms until enough narrowing or closure of an artery, due to clots, occurs. Signs and symptoms only occur after severe narrowing or closure impedes blood flow to different organs enough to induce symptoms. Most of the time, patients realize that they have the disease only when they experience other cardiovascular disorders such as stroke or heart attack. These symptoms, however, still vary depending on which artery or organ is affected.
Early atherosclerotic processes likely begin in childhood. Fibrous and gelatinous lesions have been observed in the coronary arteries of children. Fatty streaks have been observed in the coronary arteries of juveniles. While coronary artery disease is more prevalent in men than women, atherosclerosis of the cerebral arteries and strokes equally affect both sexes.
Marked narrowing in the coronary arteries, which are responsible for bringing oxygenated blood to the heart, can produce symptoms such as chest pain of angina and shortness of breath, sweating, nausea, dizziness or lightheadedness, breathlessness or palpitations. Abnormal heart rhythms called arrhythmias—the heart beating either too slowly or too quickly—are another consequence of ischemia.
Carotid arteries supply blood to the brain and neck. Marked narrowing of the carotid arteries can present with symptoms such as a feeling of weakness; being unable to think straight; difficulty speaking; dizziness; difficulty in walking or standing up straight; blurred vision; numbness of the face, arms and legs; severe headache; and loss of consciousness. These symptoms are also related to stroke (death of brain cells). Stroke is caused by marked narrowing or closure of arteries going to the brain; lack of adequate blood supply leads to the death of the cells of the affected tissue.
Peripheral arteries, which supply blood to the legs, arms, and pelvis, also experience marked narrowing due to plaque rupture and clots. Symptoms of the narrowing are pain and numbness within the arms or legs. Another significant location for plaque formation is the renal arteries, which supply blood to the kidneys. Plaque occurrence and accumulation lead to decreased kidney blood flow and chronic kidney disease, which, like in all other areas, is typically asymptomatic until late stages.
In 2004, US data indicated that in ~66% of men and ~47% of women, the first symptom of atherosclerotic cardiovascular disease was a heart attack or sudden cardiac death (defined as death within one hour of onset of the symptom).
Case studies have included autopsies of U.S. soldiers killed in World War II and the Korean War. A much-cited report involved the autopsies of 300 U.S. soldiers killed in Korea. Although the average age of the men was 22.1 years, 77.3 percent had "gross evidence of coronary arteriosclerosis".
Risk factors
See also: Lipoprotein and Lipoprotein (a)
The atherosclerotic process is not well understood. Atherosclerosis is associated with inflammatory processes in the endothelial cells of the vessel wall associated with retained low-density lipoprotein (LDL) particles. This retention may be a cause, an effect, or both, of the underlying inflammatory process.
The presence of the plaque induces the muscle cells of the blood vessel to stretch, compensating for the additional bulk. The endothelial lining then thickens, increasing the separation between the plaque and lumen. The thickening somewhat offsets the narrowing caused by the growth of the plaque, but moreover, it causes the wall to stiffen and become less compliant to stretching with each heartbeat.
Modifiable
- Western pattern diet
- Abdominal obesity
- Insulin resistance
- Diabetes
- Dyslipidemia
- Hypertension
- Trans fat
- Tobacco smoking
- Bacterial infections
- HIV/AIDS
Nonmodifiable
- South Asian descent
- Advanced age
- Genetic abnormalities
- Family history
- Coronary anatomy and branch pattern
Lesser or uncertain
- Thrombophilia
- Saturated fat
- Excessive carbohydrates
- Elevated triglycerides
- Systemic inflammation
- Hyperinsulinemia
- Sleep deprivation
- Air pollution
- Sedentary lifestyle
- Arsenic poisoning
- Alcohol
- Chronic stress
- Hypothyroidism
- Periodontal disease
Dietary
The relation between dietary fat and atherosclerosis is controversial. The USDA, in its food pyramid, promotes a diet of about 64% carbohydrates from total calories. The American Heart Association, the American Diabetes Association, and the National Cholesterol Education Program make similar recommendations. In contrast, Prof Walter Willett (Harvard School of Public Health, PI of the second Nurses' Health Study) recommends much higher levels of fat, especially of monounsaturated and polyunsaturated fat. These dietary recommendations reach a consensus, though, against consumption of trans fats.
The role of eating oxidized fats (rancid fats) in humans is not clear. Rabbits fed rancid fats develop atherosclerosis faster. Rats fed DHA-containing oils experienced marked disruptions to their antioxidant systems, and accumulated significant amounts of phospholipid hydroperoxide in their blood, livers and kidneys.
Rabbits fed atherogenic diets containing various oils were found to undergo the most oxidative susceptibility of LDL via polyunsaturated oils. In another study, rabbits fed heated soybean oil "grossly induced atherosclerosis and marked liver damage were histologically and clinically demonstrated." However, Fred Kummerow claims that it is not dietary cholesterol, but oxysterols, or oxidized cholesterols, from fried foods and smoking, that are the culprit.
Rancid fats and oils taste very unpleasant in even small amounts, so people avoid eating them. It is very difficult to measure or estimate the actual human consumption of these substances. Highly unsaturated omega-3 rich oils such as fish oil, when being sold in pill form, can hide the taste of oxidized or rancid fat that might be present. In the US, the health food industry's dietary supplements are self-regulated and outside of FDA regulations. To protect unsaturated fats from oxidation, it is best to keep them cool and in oxygen-free environments.
Pathophysiology
Atherogenesis is the developmental process of atheromatous plaques. It is characterized by a remodeling of arteries leading to subendothelial accumulation of fatty substances called plaques. The buildup of an atheromatous plaque is a slow process, developed over several years through a complex series of cellular events occurring within the arterial wall and in response to several local vascular circulating factors. One recent hypothesis suggests that, for unknown reasons, leukocytes, such as monocytes or basophils, begin to attack the endothelium of the artery lumen in cardiac muscle. The ensuing inflammation leads to the formation of atheromatous plaques in the arterial tunica intima, a region of the vessel wall located between the endothelium and the tunica media. Chronic inflammation within the arterial wall, driven by immune cells like macrophages, accelerates atherosclerotic plaque instability by promoting collagen breakdown and thinning the fibrous cap, which increases the likelihood of rupture and thrombosis. The bulk of these lesions is made of excess fat, collagen, and elastin. At first, as the plaques grow, only wall thickening occurs without narrowing. Stenosis is a late event, which may never occur and is often the result of repeated plaque rupture and healing responses, not just the atherosclerotic process. Autopsy studies have shown that the prevalence of coronary artery atherosclerosis in males from the United States, with an average age of 22.1 years old, who died in war, ranges from 45% to 77.3%.
Cellular
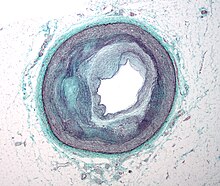
Early atherogenesis is characterized by the adherence of blood circulating monocytes (a type of white blood cell) to the vascular bed lining, the endothelium, then by their migration to the sub-endothelial space, and further activation into monocyte-derived macrophages. The primary documented driver of this process is oxidized lipoprotein particles within the wall, beneath the endothelial cells, though upper normal or elevated concentrations of blood glucose also plays a major role and not all factors are fully understood. Fatty streaks may appear and disappear.
Low-density lipoprotein (LDL) particles in blood plasma invade the endothelium and become oxidized, creating risk of cardiovascular disease. A complex set of biochemical reactions regulates the oxidation of LDL, involving enzymes (such as Lp-LpA2) and free radicals in the endothelium.
Initial damage to the endothelium results in an inflammatory response. Monocytes enter the artery wall from the bloodstream, with platelets adhering to the area of insult. This may be promoted by redox signaling induction of factors such as VCAM-1, which recruits circulating monocytes, and M-CSF, which is selectively required for the differentiation of monocytes to macrophages. The monocytes differentiate into macrophages, which proliferate locally, ingest oxidized LDL, slowly turning into large "foam cells" – so-called because of their changed appearance resulting from the numerous internal cytoplasmic vesicles and resulting high lipid content. Under the microscope, the lesion now appears as a fatty streak. Foam cells eventually die and further propagate the inflammatory process.
In addition to these cellular activities, there is also smooth muscle proliferation and migration from the tunica media into the intima in response to cytokines secreted by damaged endothelial cells. This causes the formation of a fibrous capsule covering the fatty streak. Intact endothelium can prevent this smooth muscle proliferation by releasing nitric oxide.
Calcification and lipids
Calcification forms among vascular smooth muscle cells of the surrounding muscular layer, specifically in the muscle cells adjacent to atheromas and on the surface of atheroma plaques and tissue. In time, as cells die, this leads to extracellular calcium deposits between the muscular wall and outer portion of the atheromatous plaques. With the atheromatous plaque interfering with the regulation of calcium deposition, it accumulates and crystallizes. A similar form of intramural calcification, presenting the picture of an early phase of arteriosclerosis, appears to be induced by many drugs that have an antiproliferative mechanism of action (Rainer Liedtke 2008).
Cholesterol is delivered into the vessel wall by cholesterol-containing low-density lipoprotein (LDL) particles. To attract and stimulate macrophages, the cholesterol must be released from the LDL particles and oxidized, a key step in the ongoing inflammatory process. The process is worsened if it is insufficient high-density lipoprotein (HDL), the lipoprotein particle that removes cholesterol from tissues and carries it back to the liver.
The foam cells and platelets encourage the migration and proliferation of smooth muscle cells, which in turn ingest lipids, become replaced by collagen, and transform into foam cells themselves. A protective fibrous cap normally forms between the fatty deposits and the artery lining (the intima).
These capped fatty deposits (now called 'atheromas') produce enzymes that cause the artery to enlarge over time. As long as the artery enlarges sufficiently to compensate for the extra thickness of the atheroma, then no narrowing ("stenosis") of the opening ("lumen") occurs. The artery expands with an egg-shaped cross-section, still with a circular opening. If the enlargement is beyond proportion to the atheroma thickness, then an aneurysm is created.
Visible features

Although arteries are not typically studied microscopically, two plaque types can be distinguished:
- The fibro-lipid (fibro-fatty) plaque is characterized by an accumulation of lipid-laden cells underneath the intima of the arteries, typically without narrowing the lumen due to compensatory expansion of the bounding muscular layer of the artery wall. Beneath the endothelium, there is a "fibrous cap" covering the atheromatous "core" of the plaque. The core consists of lipid-laden cells (macrophages and smooth muscle cells) with elevated tissue cholesterol and cholesterol ester content, fibrin, proteoglycans, collagen, elastin, and cellular debris. In advanced plaques, the central core of the plaque usually contains extracellular cholesterol deposits (released from dead cells), which form areas of cholesterol crystals with empty, needle-like clefts. At the periphery of the plaque are younger "foamy" cells and capillaries. These plaques usually produce the most damage to the individual when they rupture. Cholesterol crystals may also play a role.
- The fibrous plaque is also localized under the intima, within the arterial wall resulting in thickening and expansion of the wall and, sometimes, spotty localized narrowing of the lumen with some atrophy of the muscular layer. The fibrous plaque contains collagen fibers (eosinophilic), precipitates of calcium (hematoxylinophilic), and rarely, lipid-laden cells.
In effect, the muscular portion of the artery wall forms small aneurysms just large enough to hold the atheroma that are present. The muscular portion of artery walls usually remains strong, even after they have been remodeled to compensate for the atheromatous plaques.
However, atheromas within the vessel wall are soft and fragile with little elasticity. Arteries constantly expand and contract with each heartbeat, i.e., the pulse. In addition, the calcification deposits between the outer portion of the atheroma and the muscular wall, as they progress, lead to a loss of elasticity and stiffening of the artery as a whole.
The calcification deposits, after they have become sufficiently advanced, are partially visible on coronary artery computed tomography or electron beam tomography (EBT) as rings of increased radiographic density, forming halos around the outer edges of the atheromatous plaques, within the artery wall. On CT, >130 units on the Hounsfield scale (some argue for 90 units) has been the radiographic density usually accepted as clearly representing tissue calcification within arteries. These deposits demonstrate unequivocal evidence of the disease, relatively advanced, even though the lumen of the artery is often still normal by angiography.
Rupture and stenosis

Although the disease process tends to be slowly progressive over decades, it usually remains asymptomatic until an atheroma ulcerates, which leads to immediate blood clotting at the site of the atheroma ulcer. This triggers a cascade of events that leads to clot enlargement, which may quickly obstruct blood flow. A complete blockage leads to ischemia of the myocardial (heart) muscle and damage. This process is the myocardial infarction or "heart attack".
If the heart attack is not fatal, fibrous organization of the clot within the lumen ensues, covering the rupture but also producing stenosis or closure of the lumen, or over time and after repeated ruptures, resulting in a persistent, usually localized stenosis or blockage of the artery lumen. Stenoses can be slowly progressive, whereas plaque ulceration is a sudden event that occurs specifically in atheromas with thinner/weaker fibrous caps that have become "unstable".
Repeated plaque ruptures, ones not resulting in total lumen closure, combined with the clot patch over the rupture and healing response to stabilize the clot is the process that produces most stenoses over time. The stenotic areas often become more stable despite increased flow velocities at these narrowings. Most major blood-flow-stopping events occur at large plaques, which, before their rupture, produced little if any stenosis.
From clinical trials, 20% is the average stenosis at plaques that subsequently rupture with resulting complete artery closure. Most severe clinical events do not occur at plaques that produce high-grade stenosis. From clinical trials, only 14% of heart attacks occur from artery closure at plaques producing a 75% or greater stenosis before the vessel closing.
If the fibrous cap separating a soft atheroma from the bloodstream within the artery ruptures, tissue fragments are exposed and released. These tissue fragments are very clot-promoting, containing collagen and tissue factor; they activate platelets and activate the system of coagulation. The result is the formation of a thrombus (blood clot) overlying the atheroma, which obstructs blood flow acutely. With the obstruction of blood flow, downstream tissues are starved of oxygen and nutrients. If this is the myocardium (heart muscle) angina (cardiac chest pain) or myocardial infarction (heart attack) develops.
Accelerated growth of plaques
The distribution of atherosclerotic plaques in a part of arterial endothelium is inhomogeneous. The multiple and focal development of atherosclerotic changes is similar to that in the development of amyloid plaques in the brain and age spots on the skin. Misrepair-accumulation aging theory suggests that misrepair mechanisms play an important role in the focal development of atherosclerosis. The development of a plaque is a result of the repair of the injured endothelium. Because of the infusion of lipids into the sub-endothelium, the repair has to end up with altered remodeling of the local endothelium. This is the manifestation of a misrepair. This altered remodeling increases the susceptibility of the local endothelium to damage and reduces its repair efficiency. Consequently, this part of endothelium has an increased risk of being injured and improperly repaired. Thus, the accumulation of misrepairs of endothelium is focalized and self-accelerating. In this way, the growth of a plaque is also self-accelerating. Within a part of the arterial wall, the oldest plaque is always the biggest and is the most dangerous one to cause blockage of a local artery.
Components
The plaque is divided into three distinct components:
- The atheroma ("lump of gruel", from Greek ἀθήρα (athera) 'gruel'), which is the nodular accumulation of a soft, flaky, yellowish material at the center of large plaques, composed of macrophages nearest the lumen of the artery
- Underlying areas of cholesterol crystals
- Calcification at the outer base of older or more advanced lesions. Atherosclerotic lesions, or atherosclerotic plaques, are separated into two broad categories: Stable and unstable (also called vulnerable). The pathobiology of atherosclerotic lesions is very complicated, but generally, stable atherosclerotic plaques, which tend to be asymptomatic, are rich in extracellular matrix and smooth muscle cells. On the other hand, unstable plaques are rich in macrophages and foam cells, and the extracellular matrix separating the lesion from the arterial lumen (also known as the fibrous cap) is usually weak and prone to rupture. Ruptures of the fibrous cap expose thrombogenic material, such as collagen, to the circulation and eventually induce thrombus formation in the lumen. Upon formation, intraluminal thrombi can occlude arteries outright (e.g., coronary occlusion), but more often they detach, move into the circulation, and eventually occlude smaller downstream branches causing thromboembolism.
Apart from thromboembolism, chronically expanding atherosclerotic lesions can cause complete closure of the lumen. Chronically expanding lesions are often asymptomatic until the lumen stenosis is so severe (usually over 80%) that blood supply to downstream tissue(s) is insufficient, resulting in ischemia. These complications of advanced atherosclerosis are chronic, slowly progressive, and cumulative. Most commonly, soft plaque suddenly ruptures (see vulnerable plaque), causing the formation of a thrombus that will rapidly slow or stop blood flow, leading to the death of the tissues fed by the artery in approximately five minutes. This event is called an infarction.
Diagnosis


Areas of severe narrowing, stenosis, detectable by angiography, and to a lesser extent "stress testing" have long been the focus of human diagnostic techniques for cardiovascular disease, in general. However, these methods focus on detecting only severe narrowing, not the underlying atherosclerosis disease. As demonstrated by human clinical studies, most severe events occur in locations with heavy plaque, yet little or no lumen narrowing present before debilitating events suddenly occur. Plaque rupture can lead to artery lumen occlusion within seconds to minutes, potential permanent debility, and sometimes sudden death.
Plaques that have ruptured are called complicated lesions. The extracellular matrix of the lesion breaks, usually at the shoulder of the fibrous cap that separates the lesion from the arterial lumen, where the exposed thrombogenic components of the plaque, mainly collagen, will trigger thrombus formation. The thrombus then travels downstream to other blood vessels, where the blood clot may partially or completely block blood flow. If the blood flow is completely blocked, cell deaths occur due to the lack of oxygen supply to nearby cells, resulting in necrosis. The narrowing or obstruction of blood flow can occur in any artery within the body. Obstruction of arteries supplying the heart muscle results in a heart attack, while the obstruction of arteries supplying the brain results in an ischaemic stroke.

Lumen stenosis that is greater than 75% was considered the hallmark of clinically significant disease in the past because recurring episodes of angina and abnormalities in stress tests are only detectable at that particular severity of stenosis. However, clinical trials have shown that only about 14% of clinically debilitating events occur at sites with more than 75% stenosis. Most cardiovascular events that involve sudden rupture of the atheroma plaque do not display any evident luminal narrowing. Thus, greater attention has been focused on "vulnerable plaque" from the late 1990s onwards.
Besides the traditional diagnostic methods such as angiography and stress-testing, other detection techniques have been developed in the past decades for earlier detection of atherosclerotic disease. Some of the detection approaches include anatomical detection and physiologic measurement.
Examples of anatomical detection methods include coronary calcium scoring by CT, carotid IMT (intimal media thickness) measurement by ultrasound, and intravascular imaging techniques, such as intravascular ultrasound (IVUS), and intravascular optical coherence tomography (OCT), allowing direct visualization of atherosclerotic plaques.
Other methods include blood measurements, e.g., lipoprotein subclass analysis, HbA1c, hs-CRP, and homocysteine.
Both anatomic and physiologic methods allow early detection before symptoms show up, disease staging, and tracking of disease progression.
In recent years, developments in nuclear imaging techniques such as PET and SPECT have provided non-invasive ways of estimating the severity of atherosclerotic plaques.
Prevention
Up to 90% of cardiovascular disease may be preventable if established risk factors are avoided. Medical management of atherosclerosis first involves modification to risk factors–for example, via smoking cessation and diet restrictions. Prevention is generally by eating a healthy diet, exercising, not smoking, and maintaining a normal weight.
Diet
Changes in diet may help prevent the development of atherosclerosis. Tentative evidence suggests that a diet containing dairy products has no effect on or decreases the risk of cardiovascular disease.
A diet high in fruits and vegetables decreases the risk of cardiovascular disease and death. Evidence suggests that the Mediterranean diet may improve cardiovascular results. There is also evidence that a Mediterranean diet may be better than a low-fat diet in bringing about long-term changes to cardiovascular risk factors (e.g., lower cholesterol level and blood pressure). A 2024 review highlighted that bioactive compounds found in Mediterranean diet components (such as olive, grape, garlic, rosemary, and saffron) exhibit properties that may contribute to cardiovascular health and atherosclerosis prevention.
Exercise
A controlled exercise program combats atherosclerosis by improving the circulation and functionality of the vessels. Exercise is also used to manage weight in patients who are obese, lower blood pressure, and decrease cholesterol. Often lifestyle modification is combined with medication therapy. For example, statins help to lower cholesterol. Antiplatelet medications like aspirin help to prevent clots, and a variety of antihypertensive medications are routinely used to control blood pressure. If the combined efforts of risk factor modification and medication therapy are not sufficient to control symptoms or fight imminent threats of ischemic events, a physician may resort to interventional or surgical procedures to correct the obstruction.
Treatment
Treatment of established disease may include medications to lower cholesterol such as statins, blood pressure medication, or medications that decrease clotting, such as aspirin. Many procedures may also be carried out such as percutaneous coronary intervention, coronary artery bypass graft, or carotid endarterectomy.
Medical treatments often focus on alleviating symptoms. However, measures that focus on decreasing underlying atherosclerosis—as opposed to simply treating symptoms—are more effective. Non-pharmaceutical means are usually the first method of treatment, such as stopping smoking and practicing regular exercise. If these methods do not work, medicines are usually the next step in treating cardiovascular diseases and, with improvements, have increasingly become the most effective method over the long term.
The key to the more effective approaches is to combine different treatment strategies. In addition, for those approaches, such as lipoprotein transport behaviors, which have been shown to produce the most success, adopting more aggressive combination treatment strategies taken daily and indefinitely has generally produced better results, both before and especially after people are symptomatic.
Statins
Statin medications are widely prescribed for treating atherosclerosis. They have shown benefit in reducing cardiovascular disease and mortality in those with high cholesterol with few side effects. Secondary prevention therapy, which includes high-intensity statins and aspirin, is recommended by multi-society guidelines for all patients with a history of ASCVD (atherosclerotic cardiovascular disease) to prevent the recurrence of coronary artery disease, ischemic stroke, or peripheral arterial disease. However, prescription of and adherence to these guideline-concordant therapies is lacking, particularly among young patients and women.
Statins work by inhibiting HMG-CoA (hydroxymethylglutaryl-coenzyme A) reductase, a hepatic rate-limiting enzyme in cholesterol's biochemical production pathway. Inhibiting this rate-limiting enzyme reduces the body's ability to produce as much cholesterol endogenously, thereby reducing the level of LDL-cholesterol in the blood. This reduced endogenous cholesterol production triggers the body to then pull cholesterol from other cellular sources, enhancing serum HDL-cholesterol. These data are primarily in middle-aged men and the conclusions are less clear for women and people over the age of 70.
Surgery
When atherosclerosis has become severe and caused irreversible ischemia, such as tissue loss in the case of peripheral artery disease, surgery may be indicated. Vascular bypass surgery can re-establish flow around the diseased segment of the artery, and angioplasty with or without stenting can reopen narrowed arteries and improve blood flow. Coronary artery bypass grafting without manipulation of the ascending aorta has demonstrated reduced rates of postoperative stroke and mortality compared to traditional on-pump coronary revascularization.
Other
There is evidence that some anticoagulants, particularly warfarin, which inhibit clot formation by interfering with Vitamin K metabolism, may promote arterial calcification in the long term despite reducing clot formation in the short term. Also, small molecules such as 3-hydroxybenzaldehyde and protocatechuic aldehyde have shown vasculoprotective effects to reduce risk of atherosclerosis.
Epidemiology
Cardiovascular disease, which is predominantly the clinical manifestation of atherosclerosis, is one of the leading causes of death worldwide.
Almost all children older than age 10 in developed countries have aortic fatty streaks, with coronary fatty streaks beginning in adolescence.
In 1953, a study was published that examined the results of 300 autopsies performed on U.S. soldiers who had died in the Korean War. Despite the average age of the soldiers being just 22 years old, 77% of them had visible signs of coronary atherosclerosis. This study showed that heart disease could affect people at a younger age and was not just a problem for older individuals.
In 1992, a report showed that microscopic fatty streaks were seen in the left anterior descending artery in over 50% of children aged 10–14 and 8% had even more advanced lesions with more accumulations of extracellular lipid.
A 2005 report of a study done between 1985 and 1995 found that around 87% of aortas and 30% of coronary arteries in the age group 5–14 years had fatty streaks which increased with age.
Etymology
The following terms are similar, yet distinct, in both spelling and meaning, and can be easily confused: arteriosclerosis, arteriolosclerosis, and atherosclerosis. Arteriosclerosis is a general term describing any hardening (and loss of elasticity) of medium or large arteries (from Greek ἀρτηρία (artēria) 'artery' and σκλήρωσις (sklerosis) 'hardening'); arteriolosclerosis is any hardening (and loss of elasticity) of arterioles (small arteries); atherosclerosis is a hardening of an artery specifically due to an atheromatous plaque (from Ancient Greek ἀθήρα (athḗra) 'gruel'). The term atherogenic is used for substances or processes that cause the formation of atheroma.
Economics
In 2011, coronary atherosclerosis was one of the top ten most expensive conditions seen during inpatient hospitalizations in the US, with aggregate inpatient hospital costs of $10.4 billion.
Research
Lipids
An indication of the role of high-density lipoprotein (HDL) on atherosclerosis has been with the rare Apo-A1 Milano human genetic variant of this HDL protein. A small short-term trial using bacterial synthesized human Apo-A1 Milano HDL in people with unstable angina produced a fairly dramatic reduction in measured coronary plaque volume in only six weeks vs. the usual increase in plaque volume in those randomized to placebo. The trial was published in JAMA in early 2006. Ongoing work starting in the 1990s may lead to human clinical trials—probably by about 2008. These may use synthesized Apo-A1 Milano HDL directly, or they may use gene-transfer methods to pass the ability to synthesize the Apo-A1 Milano HDLipoprotein.
Methods to increase HDL particle concentrations, which in some animal studies largely reverses and removes atheromas, are being developed and researched. However, increasing HDL by any means is not necessarily helpful. For example, the drug torcetrapib is the most effective agent currently known for raising HDL (by up to 60%). However, in clinical trials, it also raised deaths by 60%. All studies regarding this drug were halted in December 2006.
The actions of macrophages drive atherosclerotic plaque progression. Immunomodulation of atherosclerosis is the term for techniques that modulate immune system function to suppress this macrophage action.
Involvement of lipid peroxidation chain reaction in atherogenesis triggered research on the protective role of the heavy isotope (deuterated) polyunsaturated fatty acids (D-PUFAs) that are less prone to oxidation than ordinary PUFAs (H-PUFAs). PUFAs are essential nutrients – they are involved in metabolism in that very form as they are consumed with food. In transgenic mice, that are a model for human-like lipoprotein metabolism, adding D-PUFAs to diet indeed reduced body weight gain, improved cholesterol handling and reduced atherosclerotic damage to the aorta.
miRNA
MicroRNAs (miRNAs) have complementary sequences in the 3' UTR and 5' UTR of target mRNAs of protein-coding genes, and cause mRNA cleavage or repression of translational machinery. In diseased vascular vessels, miRNAs are dysregulated and highly expressed. miR-33 is found in cardiovascular diseases. It is involved in atherosclerotic initiation and progression including lipid metabolism, insulin signaling and glucose homeostatis, cell type progression and proliferation, and myeloid cell differentiation. It was found in rodents that the inhibition of miR-33 will raise HDL-C levels and the expression of miR-33 is down-regulated in humans with atherosclerotic plaques.
miR-33a and miR-33b are located on intron 16 of human sterol regulatory element-binding protein 2 (SREBP2) gene on chromosome 22 and intron 17 of SREBP1 gene on chromosome 17. miR-33a/b regulates cholesterol/lipid homeostasis by binding in the 3'UTRs of genes involved in cholesterol transport such as ATP binding cassette (ABC) transporters and enhance or represses its expression. Studies have shown that ABCA1 mediates cholesterol transport from peripheral tissues to Apolipoprotein-1. It is also important in the reverse cholesterol transport pathway, where cholesterol is delivered from peripheral tissue to the liver, where it can be excreted into bile or converted to bile acids before excretion. Therefore, ABCA1 prevents cholesterol accumulation in macrophages. By enhancing miR-33 function, the level of ABCA1 is decreased, leading to decreased cellular cholesterol efflux to apoA-1. On the other hand, by inhibiting miR-33 function, the level of ABCA1 is increased and increases the cholesterol efflux to apoA-1. Suppression of miR-33 will lead to less cellular cholesterol and higher plasma HDL level through the regulation of ABCA1 expression.
The sugar, cyclodextrin, removed cholesterol that had built up in the arteries of mice fed a high-fat diet.
DNA damage
Aging is the most important risk factor for cardiovascular problems. The causative basis by which aging mediates its impact, independently of other recognized risk factors, remains to be determined. Evidence has been reviewed for a key role of DNA damage in vascular aging. 8-oxoG, a common type of oxidative damage in DNA, is found to accumulate in plaque vascular smooth muscle cells, macrophages and endothelial cells, thus linking DNA damage to plaque formation. DNA strand breaks also increased in atherosclerotic plaques. Werner syndrome (WS) is a premature aging condition in humans. WS is caused by a genetic defect in a RecQ helicase that is employed in several repair processes that remove damages from DNA. WS patients develop a considerable burden of atherosclerotic plaques in their coronary arteries and aorta: calcification of the aortic valve is also frequently observed. These findings link excessive unrepaired DNA damage to premature aging and early atherosclerotic plaque development (see DNA damage theory of aging).
Microorganisms
The microbiota – all the microorganisms in the body, can contribute to atherosclerosis in many ways: modulation of the immune system, changes in metabolism, processing of nutrients and production of certain metabolites that can get into blood circulation. One such metabolite, produced by gut bacteria, is trimethylamine N-oxide (TMAO). Its levels have been associated with atherosclerosis in human studies and animal research suggests that may be a causal relation. An association between the bacterial genes encoding trimethylamine lyases — the enzymes involved in TMAO generation — and atherosclerosis has been noted.
Vascular smooth muscle cells
Vascular smooth muscle cells play a key role in atherogenesis and were historically considered to be beneficial for plaque stability by forming a protective fibrous cap and synthesizing strength-giving extracellular matrix components. However, in addition to the fibrous cap, vascular smooth muscle cells also give rise to many of the cell types found within the plaque core and can modulate their phenotype to both promote and reduce plaque stability. Vascular smooth muscle cells exhibit pronounced plasticity within atherosclerotic plaque and can modify their gene expression profile to resemble various other cell types, including macrophages, myofibroblasts, mesenchymal stem cells and osteochondrocytes. Importantly, genetic lineage-tracing experiments have unequivocally shown that 40-90% of plaque-resident cells are vascular smooth muscle cell-derived, therefore, it is important to research the role of vascular smooth muscle cells in atherosclerosis to identify new therapeutic targets.
Notes
- Also arteriosclerotic vascular disease (ASVD)
References
- ^ "What Are the Signs and Symptoms of Atherosclerosis? - NHLBI, NIH". www.nhlbi.nih.gov. 22 June 2016. Retrieved 5 November 2017.
- ^ "What Causes Atherosclerosis? - NHLBI, NIH". www.nhlbi.nih.gov. 22 June 2016. Retrieved 6 November 2017.
- "New Concept of Heart Disease Posits Vitamin C Deficiency as Culprit". DAIC (Diagnostic and Interventional Cardiology). 27 April 2015. Retrieved 2022-02-06.
- ^ "Who Is at Risk for Atherosclerosis?". www.nhlbi.nih.gov. 22 June 2016. Retrieved 5 November 2017.
- ^ "How Can Atherosclerosis Be Prevented or Delayed? - NHLBI, NIH". www.nhlbi.nih.gov. 22 June 2016. Retrieved 6 November 2017.
- ^ "How Is Atherosclerosis Treated? - NHLBI, NIH". www.nhlbi.nih.gov. 22 June 2016. Retrieved 6 November 2017.
- ^ Aronow WS, Fleg JL, Rich MW (2013). Tresch and Aronow's Cardiovascular Disease in the Elderly, Fifth Edition. CRC Press. p. 171. ISBN 978-1-84214-544-9.
- "Arteriosclerosis / atherosclerosis - Symptoms and causes". Mayo Clinic. Retrieved 2021-05-06.
- ^ Scipione, Corey A.; Hyduk, Sharon J.; Polenz, Chanele K.; Cybulsky, Myron I. (December 2023). "Unveiling the Hidden Landscape of Arterial Diseases at Single-Cell Resolution". Canadian Journal of Cardiology. 39 (12): 1781–1794. doi:10.1016/j.cjca.2023.09.009. PMID 37716639.
- ^ "What Is Atherosclerosis? - NHLBI, NIH". www.nhlbi.nih.gov. 22 June 2016. Retrieved 6 November 2017.
- Tsukahara, Tamotsu; Tsukahara, Ryoko; Haniu, Hisao; Matsuda, Yoshikazu; Murakami-Murofushi, Kimiko (2015-09-05). "Cyclic phosphatidic acid inhibits the secretion of vascular endothelial growth factor from diabetic human coronary artery endothelial cells through peroxisome proliferator-activated receptor gamma". Molecular and Cellular Endocrinology. 412: 320–329. doi:10.1016/j.mce.2015.05.021. hdl:10069/35888. PMID 26007326.
- Lind L (August 2003). "Circulating markers of inflammation and atherosclerosis". Atherosclerosis. 169 (2): 203–214. doi:10.1016/s0021-9150(03)00012-1. PMID 12921971.
- "How Is Atherosclerosis Diagnosed? - NHLBI, NIH". www.nhlbi.nih.gov. 22 June 2016. Retrieved 6 November 2017.
- Information (US), National Center for Biotechnology (1998). "Atherosclerosis". Genes and Disease . National Center for Biotechnology Information (US).
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. (December 2020). "Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study". Journal of the American College of Cardiology. 76 (25): 2982–3021. doi:10.1016/j.jacc.2020.11.010. PMC 7755038. PMID 33309175.
- Song P, Fang Z, Wang H, Cai Y, Rahimi K, Zhu Y, et al. (May 2020). "Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study". The Lancet. Global Health. 8 (5): e721 – e729. doi:10.1016/S2214-109X(20)30117-0. hdl:10044/1/78967. PMID 32353319.
- Topol EJ, Califf RM (2007). Textbook of Cardiovascular Medicine. Lippincott Williams & Wilkins. p. 2. ISBN 978-0-7817-7012-5.
- Shor, Allan (2007). Chlamydia Atherosclerosis Lesion. p. 8. doi:10.1007/978-1-84628-810-4. ISBN 978-1-84628-809-8.
- "Evolutionary gene loss may help explain why only humans are prone to heart attacks". ScienceDaily. University of California - San Diego. 23 July 2019.
- Ross R (April 1993). "The pathogenesis of atherosclerosis: a perspective for the 1990s". Nature. 362 (6423): 801–9. Bibcode:1993Natur.362..801R. doi:10.1038/362801a0. PMID 8479518.
- Atherosclerosis. Harvard Health Publications Harvard Health Publications. Health Topics A – Z, (2011)
- ^ "Atherosclerosis". National Heart, Lung and Blood Institute. 2011.
- ^ Velican D, Velican C (June 1979). "Study of fibrous plaques occurring in the coronary arteries of children". Atherosclerosis. 33 (2): 201–205. doi:10.1016/0021-9150(79)90117-5. PMID 475879.
- Flora GC, Baker AB, Loewenson RB, Klassen AC (November 1968). "A comparative study of cerebral atherosclerosis in males and females". Circulation. 38 (5): 859–69. doi:10.1161/01.CIR.38.5.859. PMID 5697685.
- ^ Arrhythmia. Heart and Stroke Foundation. "Heart disease - Arrhythmia - Heart and Stroke Foundation of Canada". Archived from the original on 2014-02-03. Retrieved 2014-01-31. (2011)
- Sims, Neil R.; Muyderman, Hakan (January 2010). "Mitochondria, oxidative metabolism and cell death in stroke". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1802 (1): 80–91. doi:10.1016/j.bbadis.2009.09.003. PMID 19751827.
- Roquer, J.; Ois, Angel (2010). "Atherosclerotic Burden and Mortality". Handbook of Disease Burdens and Quality of Life Measures. pp. 899–918. doi:10.1007/978-0-387-78665-0_51. ISBN 978-0-387-78664-3.
- Enos WF, Holmes RH, Beyer J (1953). "Coronary disease among United States soldiers killed in action in Korea: Preliminary Report". JAMA. 152 (12): 1090–93. doi:10.1001/jama.1953.03690120006002. PMID 13052433. The average age was calculated from the ages of 200 of the soldiers. No age was recorded in nearly 100 of the men.
- Li X, Fang P, Li Y, Kuo YM, Andrews AJ, Nanayakkara G, Johnson C, Fu H, Shan H, Du F, Hoffman NE, Yu D, Eguchi S, Madesh M, Koch WJ, Sun J, Jiang X, Wang H, Yang X (June 2016). "Mitochondrial Reactive Oxygen Species Mediate Lysophosphatidylcholine-Induced Endothelial Cell Activation". Arteriosclerosis, Thrombosis, and Vascular Biology. 36 (6): 1090–100. doi:10.1161/ATVBAHA.115.306964. PMC 4882253. PMID 27127201.
- Botts SR, Fish JE, Howe KL (December 2021). "Dysfunctional Vascular Endothelium as a Driver of Atherosclerosis: Emerging Insights Into Pathogenesis and Treatment". Frontiers in Pharmacology. 12: 787541. doi:10.3389/fphar.2021.787541. PMC 8727904. PMID 35002720.
- Williams KJ, Tabas I (May 1995). "The response-to-retention hypothesis of early atherogenesis". Arteriosclerosis, Thrombosis, and Vascular Biology. 15 (5): 551–61. doi:10.1161/01.ATV.15.5.551. PMC 2924812. PMID 7749869.
- Aviram M, Fuhrman B (November 1998). "LDL oxidation by arterial wall macrophages depends on the oxidative status in the lipoprotein and in the cells: role of prooxidants vs. antioxidants". Molecular and Cellular Biochemistry. 188 (1–2): 149–59. doi:10.1023/A:1006841011201. PMID 9823020.
- ^ "Atherosclerosis | NHLBI, NIH". 24 March 2022.
- Campbell LA, Rosenfeld ME (July 2015). "Infection and Atherosclerosis Development". Arch Med Res. 46 (5): 339–50. doi:10.1016/j.arcmed.2015.05.006. PMC 4524506. PMID 26004263.
- Sinha A, Feinstein MJ (March 2019). "Coronary Artery Disease Manifestations in HIV: What, How, and Why". The Canadian Journal of Cardiology. 35 (3): 270–279. doi:10.1016/j.cjca.2018.11.029. PMC 9532012. PMID 30825949.
- Enas EA, Kuruvila A, Khanna P, Pitchumoni CS, Mohan V (October 2013). "Benefits & risks of statin therapy for primary prevention of cardiovascular disease in Asian Indians - a population with the highest risk of premature coronary artery disease & diabetes". The Indian Journal of Medical Research. 138 (4): 461–91. PMC 3868060. PMID 24434254.
- Indian Heart Association Why South Asians Facts Web. 30 April 2015. http://indianheartassociation.org/why-indians-why-south-asians/overview/
- Tyrrell DJ, Blin MB, Song J, Wood SC, Zhang M, Beard DA, Goldstein DR (January 2020). "Age-Associated Mitochondrial Dysfunction Accelerates Atherogenesis". Circulation Research. 126 (3): 298–314. doi:10.1161/CIRCRESAHA.119.315644. PMC 7006722. PMID 31818196.
- Velican C, Velican D (March 1985). "Differences in the pattern of atherosclerotic involvement between non-branched regions and adjacent branching points of human coronary arteries". Atherosclerosis. 54 (3): 333–342. doi:10.1016/0021-9150(85)90126-1. PMID 3994786.
- Borissoff JI, Spronk HM, Heeneman S, ten Cate H (June 2009). "Is thrombin a key player in the 'coagulation-atherogenesis' maze?". Cardiovascular Research. 82 (3): 392–403. doi:10.1093/cvr/cvp066. PMID 19228706.
- Borissoff JI, Heeneman S, Kilinç E, Kassák P, Van Oerle R, Winckers K, Govers-Riemslag JW, Hamulyák K, Hackeng TM, Daemen MJ, ten Cate H, Spronk HM (August 2010). "Early atherosclerosis exhibits an enhanced procoagulant state". Circulation. 122 (8): 821–30. doi:10.1161/CIRCULATIONAHA.109.907121. PMID 20697022.
- Borissoff JI, Spronk HM, ten Cate H (May 2011). "The hemostatic system as a modulator of atherosclerosis". The New England Journal of Medicine. 364 (18): 1746–60. doi:10.1056/NEJMra1011670. PMID 21542745.
- Food and nutrition board, institute of medicine of the national academies (2005). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academies Press. pp. 481–484. doi:10.17226/10490. ISBN 978-0-309-08525-0.
- Mozaffarian D, Rimm EB, Herrington DM (November 2004). "Dietary fats, carbohydrate, and progression of coronary atherosclerosis in postmenopausal women". The American Journal of Clinical Nutrition. 80 (5): 1175–84. doi:10.1093/ajcn/80.5.1175. PMC 1270002. PMID 15531663.
- Bhatt DL, Topol EJ (July 2002). "Need to test the arterial inflammation hypothesis". Circulation. 106 (1): 136–40. doi:10.1161/01.CIR.0000021112.29409.A2. PMID 12093783.
- Griffin M, Frazer A, Johnson A, Collins P, Owens D, Tomkin GH (June 1998). "Cellular cholesterol synthesis--the relationship to post-prandial glucose and insulin following weight loss". Atherosclerosis. 138 (2): 313–8. doi:10.1016/S0021-9150(98)00036-7. PMID 9690914.
- King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS (December 2008). "Short sleep duration and incident coronary artery calcification". JAMA. 300 (24): 2859–66. doi:10.1001/jama.2008.867. PMC 2661105. PMID 19109114.
- Provost EB, Madhloum N, Int Panis L, De Boever P, Nawrot TS (2015). "Carotid intima-media thickness, a marker of subclinical atherosclerosis, and particulate air pollution exposure: the meta-analytical evidence". PLOS ONE. 10 (5): e0127014. Bibcode:2015PLoSO..1027014P. doi:10.1371/journal.pone.0127014. PMC 4430520. PMID 25970426.
- Adar SD, Sheppard L, Vedal S, Polak JF, Sampson PD, Diez Roux AV, Budoff M, Jacobs DR, Barr RG, Watson K, Kaufman JD (April 23, 2013). "Fine particulate air pollution and the progression of carotid intima-medial thickness: a prospective cohort study from the multi-ethnic study of atherosclerosis and air pollution". PLOS Medicine. 10 (4): e1001430. doi:10.1371/journal.pmed.1001430. PMC 3637008. PMID 23637576.
This early analysis from MESA suggests that higher long-term PM2.5 concentrations are associated with increased IMT progression and that greater reductions in PM2.5 are related to slower IMT progression.
- Wang CH, Jeng JS, Yip PK, Chen CL, Hsu LI, Hsueh YM, et al. (April 2002). "Biological gradient between long-term arsenic exposure and carotid atherosclerosis". Circulation. 105 (15): 1804–1809. doi:10.1161/01.cir.0000015862.64816.b2. PMID 11956123.
- Sadovsky, Richard (February 2004). "Treating Hypothyroidism Reduces Atherosclerosis Risk". American Family Physician. 69 (3): 656–657. ProQuest 234284553.
- Bale BF, Doneen AL, Vigerust DJ (April 2017). "High-risk periodontal pathogens contribute to the pathogenesis of atherosclerosis". Postgraduate Medical Journal. 93 (1098): 215–220. doi:10.1136/postgradmedj-2016-134279. PMC 5520251. PMID 27899684.
- "Food Pyramids: Nutrition Source, Harvard School of Public Health". Archived from the original on 26 December 2007. Retrieved 2007-11-25.
- Staprãns I, Rapp JH, Pan XM, Hardman DA, Feingold KR (April 1996). "Oxidized lipids in the diet accelerate the development of fatty streaks in cholesterol-fed rabbits". Arteriosclerosis, Thrombosis, and Vascular Biology. 16 (4): 533–8. doi:10.1161/01.atv.16.4.533. PMID 8624775.
- Song JH, Fujimoto K, Miyazawa T (December 2000). "Polyunsaturated (n-3) fatty acids susceptible to peroxidation are increased in plasma and tissue lipids of rats fed docosahexaenoic acid-containing oils". The Journal of Nutrition. 130 (12): 3028–33. doi:10.1093/jn/130.12.3028. PMID 11110863.
- Yap SC, Choo YM, Hew NF, Yap SF, Khor HT, Ong AS, Goh SH (December 1995). "Oxidative susceptibility of low density lipoprotein from rabbits fed atherogenic diets containing coconut, palm, or soybean oils". Lipids. 30 (12): 1145–50. doi:10.1007/BF02536616. PMID 8614305.
- Greco AV, Mingrone G (1990). "Serum and biliary lipid pattern in rabbits feeding a diet enriched with unsaturated fatty acids". Experimental Pathology. 40 (1): 19–33. doi:10.1016/S0232-1513(11)80281-1. PMID 2279534.
- "Scientist, 98, challenges orthodoxy on causes of heart disease". medicalxpress.com.
- Mattes RD (December 2005). "Fat taste and lipid metabolism in humans". Physiology & Behavior. 86 (5): 691–7. doi:10.1016/j.physbeh.2005.08.058. PMID 16249011.
The rancid odor of an oxidized fat is readily detectable
- Dobarganes C, Márquez-Ruiz G (March 2003). "Oxidized fats in foods". Current Opinion in Clinical Nutrition and Metabolic Care. 6 (2): 157–163. doi:10.1097/00075197-200303000-00004. PMID 12589185.
- "Dietary Supplements". Food and Drug Administration. 4 February 2020.
- Khan-Merchant N, Penumetcha M, Meilhac O, Parthasarathy S (November 2002). "Oxidized fatty acids promote atherosclerosis only in the presence of dietary cholesterol in low-density lipoprotein receptor knockout mice". The Journal of Nutrition. 132 (11): 3256–3262. doi:10.1093/jn/132.11.3256. PMID 12421837.
- Shahjehan, Rai Dilawar; Sharma, Sanjeev; Bhutta, Beenish S. (2024). "Coronary Artery Disease". StatPearls. StatPearls Publishing. PMID 33231974.
- "Atherosclerosis". The Lecturio Medical Concept Library. Retrieved 2 July 2021.
- Joseph, Abraham; Ackerman, Douglas; Talley, J.David; Johnstone, John; Kupersmith, Joel (August 1993). "Manifestations of coronary atherosclerosis in young trauma victims—An autopsy study". Journal of the American College of Cardiology. 22 (2): 459–467. doi:10.1016/0735-1097(93)90050-B. PMID 8335815.
- Schwartz CJ, Valente AJ, Sprague EA, Kelley JL, Cayatte AJ, Mowery J (December 1992). "Atherosclerosis. Potential targets for stabilization and regression". Circulation. 86 (6 Suppl): III117–23. PMID 1424045.
- ^ Linton MF, Yancey PG, Davies SS, Jerome WG, Linton EF, Song WL, et al. (2000). "The Role of Lipids and Lipoproteins in Atherosclerosis". Endotext. PMID 26844337. NBK343489.
- Robbins CS, Hilgendorf I, Weber GF, Theurl I, Iwamoto Y, Figueiredo JL, Gorbatov R, Sukhova GK, Gerhardt LM, Smyth D, Zavitz CC, Shikatani EA, Parsons M, van Rooijen N, Lin HY, Husain M, Libby P, Nahrendorf M, Weissleder R, Swirski FK (September 2013). "Local proliferation dominates lesional macrophage accumulation in atherosclerosis". Nature Medicine. 19 (9): 1166–72. doi:10.1038/nm.3258. PMC 3769444. PMID 23933982.
- Miller JD (June 2013). "Cardiovascular calcification: Orbicular origins". Nature Materials. 12 (6): 476–478. Bibcode:2013NatMa..12..476M. doi:10.1038/nmat3663. PMID 23695741.
- Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ (May 1987). "Compensatory enlargement of human atherosclerotic coronary arteries". The New England Journal of Medicine. 316 (22): 1371–5. doi:10.1056/NEJM198705283162204. PMID 3574413.
- "Coronary atherosclerosis — the fibrous plaque with calcification". www.pathologyatlas.ro. Retrieved 2010-03-25.
- Janoudi A, Shamoun FE, Kalavakunta JK, Abela GS (July 2016). "Cholesterol crystal-induced arterial inflammation and destabilization of atherosclerotic plaque". European Heart Journal. 37 (25): 1959–67. doi:10.1093/eurheartj/ehv653. PMID 26705388.
- Maton A, Hopkins RL, McLaughlin CW, Johnson S, Warner MQ, LaHart D, et al. (1993). Human Biology and Health. Englewood Cliffs, NJ: Prentice Hall. ISBN 978-0-13-981176-0. OCLC 32308337.
- ^ "What Are the Signs and Symptoms of Coronary Heart Disease?". www.nhlbi.nih.gov. September 29, 2014. Archived from the original on 24 February 2015. Retrieved 2 July 2021.
- Wang J, Michelitsch T, Wunderlin A, Mahadeva R (6 April 2009). "Aging as a consequence of misrepair -- A novel theory of aging". Nature Precedings. arXiv:0904.0575. doi:10.1038/npre.2009.2988.2.
- Wang-Michelitsch J, Michelitsch T (2015). "Aging as a process of accumulation of Misrepairs". arXiv:1503.07163 .
- Wang-Michelitsch J, Michelitsch TM (2015). "Misrepair mechanism in the development of atherosclerotic plaques". arXiv:1505.01289 .
- Ross R (January 1999). "Atherosclerosis--an inflammatory disease". The New England Journal of Medicine. 340 (2): 115–26. doi:10.1056/NEJM199901143400207. PMID 9887164.
- Finn AV, Nakano M, Narula J, Kolodgie FD, Virmani R (July 2010). "Concept of vulnerable/unstable plaque". Arteriosclerosis, Thrombosis, and Vascular Biology. 30 (7): 1282–92. doi:10.1161/ATVBAHA.108.179739. PMID 20554950.
- Didangelos A, Simper D, Monaco C, Mayr M (May 2009). "Proteomics of acute coronary syndromes". Current Atherosclerosis Reports. 11 (3): 188–95. doi:10.1007/s11883-009-0030-x. PMID 19361350.
- ^ Tarkin JM, Dweck MR, Evans NR, Takx RA, Brown AJ, Tawakol A, et al. (February 2016). "Imaging Atherosclerosis". Circulation Research. 118 (4): 750–769. doi:10.1161/CIRCRESAHA.115.306247. PMC 4756468. PMID 26892971.
- Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, et al. (September 1995). "A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association". Circulation. 92 (5): 1355–1374. doi:10.1161/01.CIR.92.5.1355. PMID 7648691.
- Maseri A, Fuster V (April 2003). "Is there a vulnerable plaque?". Circulation. 107 (16): 2068–71. doi:10.1161/01.CIR.0000070585.48035.D1. PMID 12719286.
- Tearney, Guillermo J.; Regar, Evelyn; Akasaka, Takashi; Adriaenssens, Tom; Barlis, Peter; Bezerra, Hiram G.; Bouma, Brett; Bruining, Nico; Cho, Jin-man; Chowdhary, Saqib; Costa, Marco A.; de Silva, Ranil; Dijkstra, Jouke; Di Mario, Carlo; Dudeck, Darius (2012-03-20). "Consensus Standards for Acquisition, Measurement, and Reporting of Intravascular Optical Coherence Tomography Studies: A Report From the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation". Journal of the American College of Cardiology. 59 (12): 1058–1072. doi:10.1016/j.jacc.2011.09.079. PMID 22421299.
- Pereira, Vitor M.; Lylyk, Pedro; Cancelliere, Nicole; Lylyk, Pedro N.; Lylyk, Ivan; Anagnostakou, Vania; Bleise, Carlos; Nishi, Hidehisa; Epshtein, Mark; King, Robert M.; Shazeeb, Mohammed Salman; Puri, Ajit S.; Liang, Conrad W.; Hanel, Ricardo A.; Spears, Julian; Marotta, Thomas R.; Lopes, Demetrius K.; Gounis, Matthew J.; Ughi, Giovanni J. (15 May 2024). "Volumetric microscopy of cerebral arteries with a miniaturized optical coherence tomography imaging probe". Science Translational Medicine. 16 (747): eadl4497. doi:10.1126/scitranslmed.adl4497. PMID 38748771.
- McGill HC, McMahan CA, Gidding SS (March 2008). "Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study". Circulation. 117 (9): 1216–27. doi:10.1161/CIRCULATIONAHA.107.717033. PMID 18316498.
- McNeal CJ, Dajani T, Wilson D, Cassidy-Bushrow AE, Dickerson JB, Ory M (January 2010). "Hypercholesterolemia in youth: opportunities and obstacles to prevent premature atherosclerotic cardiovascular disease". Current Atherosclerosis Reports. 12 (1): 20–8. doi:10.1007/s11883-009-0072-0. PMID 20425267.
- Rice BH (2014). "Dairy and Cardiovascular Disease: A Review of Recent Observational Research". Current Nutrition Reports. 3 (2): 130–138. doi:10.1007/s13668-014-0076-4. PMC 4006120. PMID 24818071.
- Kratz M, Baars T, Guyenet S (February 2013). "The relationship between high-fat dairy consumption and obesity, cardiovascular, and metabolic disease". European Journal of Nutrition. 52 (1): 1–24. doi:10.1007/s00394-012-0418-1. PMID 22810464.
- Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB (July 2014). "Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies". BMJ. 349: g4490. doi:10.1136/bmj.g4490. PMC 4115152. PMID 25073782.
- Walker, Christopher; Reamy, Brian V (April 2009). "Diets for Cardiovascular Disease Prevention: What Is the Evidence?". American Family Physician. 79 (7): 571–578. PMID 19378874. ProQuest 234120649.
- Nordmann AJ, Suter-Zimmermann K, Bucher HC, Shai I, Tuttle KR, Estruch R, Briel M (September 2011). "Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors". The American Journal of Medicine. 124 (9): 841–51.e2. doi:10.1016/j.amjmed.2011.04.024. PMID 21854893.
- Anguera-Tejedor, Mateu; Garrido, Gabino; Garrido-Suárez, Bárbara B.; Ardiles-Rivera, Alejandro; Bistué-Rovira, Àngel; Jiménez-Altayó, Francesc; Delgado-Hernández, René (December 2024). "Exploring the therapeutic potential of bioactive compounds from selected plant extracts of Mediterranean diet constituents for cardiovascular diseases: A review of mechanisms of action, clinical evidence, and adverse effects". Food Bioscience. 62: 105487. doi:10.1016/j.fbio.2024.105487.
- Paul P, Williams B, eds. (2009). "Cardiovascular, Circulatory, and Hematologic Function". Brunner & Suddarth's Textbook of Canadian Medical-surgical Nursing. Lippincott Williams & Wilkins. pp. 730–1047. ISBN 978-0-7817-9989-8.
- ^ Fonarow G (2003). "Aggressive treatment of atherosclerosis: The time is now". Cleve. Clin. J. Med. 70 (5): 431–434. doi:10.3949/ccjm.70.5.431 (inactive 4 December 2024). PMID 12785316.
{{cite journal}}: CS1 maint: DOI inactive as of December 2024 (link) - Ambrose JA, Barua RS (May 2004). "The pathophysiology of cigarette smoking and cardiovascular disease: an update". Journal of the American College of Cardiology. 43 (10): 1731–7. doi:10.1016/j.jacc.2003.12.047. PMID 15145091.
- Pigozzi F, Rizzo M, Fagnani F, Parisi A, Spataro A, Casasco M, Borrione P (June 2011). "Endothelial (dys)function: the target of physical exercise for prevention and treatment of cardiovascular disease". The Journal of Sports Medicine and Physical Fitness. 51 (2): 260–267. PMID 21681161.
- Gupta, Keshav Kumar; Ali, Shair; Sanghera, Ranjodh Singh (June 2019). "Pharmacological Options in Atherosclerosis: A Review of the Existing Evidence". Cardiology and Therapy. 8 (1): 5–20. doi:10.1007/s40119-018-0123-0. PMC 6525235. PMID 30543029.
- Koh KK, Han SH, Oh PC, Shin EK, Quon MJ (April 2010). "Combination therapy for treatment or prevention of atherosclerosis: focus on the lipid-RAAS interaction". Atherosclerosis. 209 (2): 307–13. doi:10.1016/j.atherosclerosis.2009.09.007. PMC 2962413. PMID 19800624.
- Taylor, Fiona; Huffman, Mark D; Macedo, Ana Filipa; Moore, Theresa HM; Burke, Margaret; Davey Smith, George; Ward, Kirsten; Ebrahim, Shah; Gay, Hawkins C (31 January 2013). "Statins for the primary prevention of cardiovascular disease". Cochrane Database of Systematic Reviews. 2021 (9): CD004816. doi:10.1002/14651858.CD004816.pub5. PMC 6481400. PMID 23440795.
- Virani SS, Smith SC, Stone NJ, Grundy SM (April 2020). "Secondary Prevention for Atherosclerotic Cardiovascular Disease: Comparing Recent US and European Guidelines on Dyslipidemia". Circulation. 141 (14): 1121–1123. doi:10.1161/CIRCULATIONAHA.119.044282. PMID 32250694.
- Grundy, Scott M.; Stone, Neil J.; Bailey, Alison L.; Beam, Craig; Birtcher, Kim K.; Blumenthal, Roger S.; Braun, Lynne T.; de Ferranti, Sarah; Faiella-Tommasino, Joseph; Forman, Daniel E.; Goldberg, Ronald; Heidenreich, Paul A.; Hlatky, Mark A.; Jones, Daniel W.; Lloyd-Jones, Donald; Lopez-Pajares, Nuria; Ndumele, Chiadi E.; Orringer, Carl E.; Peralta, Carmen A.; Saseen, Joseph J.; Smith, Sidney C.; Sperling, Laurence; Virani, Salim S.; Yeboah, Joseph (June 2019). "2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol". Journal of the American College of Cardiology. 73 (24): e285 – e350. doi:10.1016/j.jacc.2018.11.003. hdl:20.500.12749/1738. PMID 30423393.
- Nanna MG, Wang TY, Xiang Q, Goldberg AC, Robinson JG, Roger VL, et al. (August 2019). "Sex Differences in the Use of Statins in Community Practice". Circulation: Cardiovascular Quality and Outcomes. 12 (8): e005562. doi:10.1161/CIRCOUTCOMES.118.005562. PMC 6903404. PMID 31416347.
- Lee MT, Mahtta D, Ramsey DJ, Liu J, Misra A, Nasir K, et al. (July 2021). "Sex-Related Disparities in Cardiovascular Health Care Among Patients With Premature Atherosclerotic Cardiovascular Disease". JAMA Cardiology. 6 (7): 782–790. doi:10.1001/jamacardio.2021.0683. PMC 8060887. PMID 33881448.
- Vos E, Rose CP (November 2005). "Questioning the benefits of statins". CMAJ. 173 (10): 1207, author reply 1210. doi:10.1503/cmaj.1050120. PMC 1277053. PMID 16275976.
- Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, Thourani V, Lamy A, Taggart DP, Puskas JD, Vallely MP (February 2017). "Coronary Artery Bypass Grafting With and Without Manipulation of the Ascending Aorta: A Network Meta-Analysis". Journal of the American College of Cardiology. 69 (8): 924–936. doi:10.1016/j.jacc.2016.11.071. PMID 28231944.
- Vlasschaert C, Goss CJ, Pilkey NG, McKeown S, Holden RM (September 2020). "Vitamin K Supplementation for the Prevention of Cardiovascular Disease: Where Is the Evidence? A Systematic Review of Controlled Trials". Nutrients. 12 (10): 2909. doi:10.3390/nu12102909. PMC 7598164. PMID 32977548.
- Price PA, Faus SA, Williamson MK (February 2000). "Warfarin-induced artery calcification is accelerated by growth and vitamin D". Arteriosclerosis, Thrombosis, and Vascular Biology. 20 (2): 317–327. doi:10.1161/01.ATV.20.2.317. PMID 10669626.
- Geleijnse JM, Vermeer C, Grobbee DE, Schurgers LJ, Knapen MH, van der Meer IM, et al. (November 2004). "Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam Study". The Journal of Nutrition. 134 (11): 3100–3105. doi:10.1093/jn/134.11.3100. hdl:1765/10366. PMID 15514282.
- "Vitamin K". Linus Pauling Institute at Oregon State University. Archived from the original on 7 April 2010. Retrieved 2010-03-25.
- Kong BS, Cho YH, Lee EJ (2014). "G protein-coupled estrogen receptor-1 is involved in the protective effect of protocatechuic aldehyde against endothelial dysfunction". PLOS ONE. 9 (11): e113242. Bibcode:2014PLoSO...9k3242K. doi:10.1371/journal.pone.0113242. PMC 4239058. PMID 25411835.
- Kong BS, Im SJ, Lee YJ, Cho YH, Do YR, Byun JW, et al. (2016). "Vasculoprotective Effects of 3-Hydroxybenzaldehyde against VSMCs Proliferation and ECs Inflammation". PLOS ONE. 11 (3): e0149394. Bibcode:2016PLoSO..1149394K. doi:10.1371/journal.pone.0149394. PMC 4803227. PMID 27002821.
- "The top 10 causes of death". www.who.int. Retrieved 2020-01-26.
- Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; & Mitchell, Richard N. (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 348-351 ISBN 978-1-4160-2973-1
- Strong, J. P.; McGill, H. C. (1969-05-06). "The pediatric aspects of atherosclerosis". Journal of Atherosclerosis Research. 9 (3): 251–265. doi:10.1016/S0368-1319(69)80020-7. PMID 5346899.
- Zieske, Arthur W.; Malcom, Gray T.; Strong, Jack P. (January 2002). "Natural history and risk factors of atherosclerosis in children and youth: The PDAY study". Pediatric Pathology & Molecular Medicine. 21 (2): 213–237. doi:10.1080/pdp.21.2.213.237. PMID 11942537.
- Enos, William F. (18 July 1953). "CORONARY DISEASE AMONG UNITED STATES SOLDIERS KILLED IN ACTION IN KOREA: PRELIMINARY REPORT". Journal of the American Medical Association. 152 (12): 1090–1093. doi:10.1001/jama.1953.03690120006002. PMID 13052433.
- "Stopping Heart Disease in Childhood". NutritionFacts.org. 15 July 2014. Retrieved 2022-12-08.
- Wilson, Don P. (2000). "Is Atherosclerosis a Pediatric Disease?". Endotext. MDText.com, Inc. PMID 27809437.
- Strong, Jack P.; Malcom, Gray T.; Newman, William P.; Oalmann, Margaret C. (June 1992). "Early Lesions of Atherosclerosis in Childhood and Youth: Natural History and Risk Factors". Journal of the American College of Nutrition. 11 (sup1): 51S – 54S. doi:10.1080/07315724.1992.10737984. PMID 1619200.
- Mendis, Shanthi; Nordet, P.; Fernandez-Britto, J.E.; Sternby, N. (March 2005). "Atherosclerosis in children and young adults: An overview of the World Health Organization and International Society and Federation of Cardiology study on Pathobiological Determinants of Atherosclerosis in Youth study (1985–1995)". Global Heart. 1 (1): 3. doi:10.1016/j.precon.2005.02.010.
- "Atherogenic". Merriam-Webster Dictionary.
- Pfuntner A, Wier LM, Steiner C (December 2013). "Costs for Hospital Stays in the United States, 2011". HCUP Statistical Brief (168). Rockville, MD: Agency for Healthcare Research and Quality. PMID 24455786.
- Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, Lopez-Sendon J, Mosca L, Tardif JC, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer B (November 2007). "Effects of torcetrapib in patients at high risk for coronary events". The New England Journal of Medicine. 357 (21): 2109–22. doi:10.1056/NEJMoa0706628. PMID 17984165.
- Nilsson J, Hansson GK, Shah PK (January 2005). "Immunomodulation of atherosclerosis: implications for vaccine development". Arteriosclerosis, Thrombosis, and Vascular Biology. 25 (1): 18–28. doi:10.1161/01.ATV.0000149142.42590.a2. PMID 15514204.
- Spiteller G (November 2005). "The relation of lipid peroxidation processes with atherogenesis: a new theory on atherogenesis". Molecular Nutrition & Food Research. 49 (11): 999–1013. doi:10.1002/mnfr.200500055. PMID 16270286.
- Berbée JF, Mol IM, Milne GL, Pollock E, Hoeke G, Lütjohann D, Monaco C, Rensen PC, van der Ploeg LH, Shchepinov MS (September 2017). "Deuterium-reinforced polyunsaturated fatty acids protect against atherosclerosis by lowering lipid peroxidation and hypercholesterolemia". Atherosclerosis. 264: 100–107. doi:10.1016/j.atherosclerosis.2017.06.916. PMID 28655430.
- Tsikas D (September 2017). "Combating atherosclerosis with heavy PUFAs: Deuteron not proton is the first". Atherosclerosis. 264: 79–82. doi:10.1016/j.atherosclerosis.2017.07.018. PMID 28756876.
- ^ Chen WJ, Yin K, Zhao GJ, Fu YC, Tang CK (June 2012). "The magic and mystery of microRNA-27 in atherosclerosis". Atherosclerosis. 222 (2): 314–23. doi:10.1016/j.atherosclerosis.2012.01.020. PMID 22307089.
- Sacco J, Adeli K (June 2012). "MicroRNAs: emerging roles in lipid and lipoprotein metabolism". Current Opinion in Lipidology. 23 (3): 220–5. doi:10.1097/MOL.0b013e3283534c9f. PMID 22488426.
- Bommer GT, MacDougald OA (March 2011). "Regulation of lipid homeostasis by the bifunctional SREBF2-miR33a locus". Cell Metabolism. 13 (3): 241–7. doi:10.1016/j.cmet.2011.02.004. PMC 3062104. PMID 21356514.
- Rayner KJ, Sheedy FJ, Esau CC, Hussain FN, Temel RE, Parathath S, van Gils JM, Rayner AJ, Chang AN, Suarez Y, Fernandez-Hernando C, Fisher EA, Moore KJ (July 2011). "Antagonism of miR-33 in mice promotes reverse cholesterol transport and regression of atherosclerosis". The Journal of Clinical Investigation. 121 (7): 2921–31. doi:10.1172/JCI57275. PMC 3223840. PMID 21646721.
- Iwakiri Y (March 2012). "A role of miR-33 for cell cycle progression and cell proliferation". Cell Cycle. 11 (6): 1057–8. doi:10.4161/cc.11.6.19744. PMID 22395363.
- Singaraja RR, Stahmer B, Brundert M, Merkel M, Heeren J, Bissada N, Kang M, Timmins JM, Ramakrishnan R, Parks JS, Hayden MR, Rinninger F (August 2006). "Hepatic ATP-binding cassette transporter A1 is a key molecule in high-density lipoprotein cholesteryl ester metabolism in mice". Arteriosclerosis, Thrombosis, and Vascular Biology. 26 (8): 1821–7. doi:10.1161/01.ATV.0000229219.13757.a2. PMID 16728652.
- Zimmer S, Grebe A, Bakke SS, Bode N, Halvorsen B, Ulas T, Skjelland M, De Nardo D, Labzin LI, Kerksiek A, Hempel C, Heneka MT, Hawxhurst V, Fitzgerald ML, Trebicka J, Björkhem I, Gustafsson JÅ, Westerterp M, Tall AR, Wright SD, Espevik T, Schultze JL, Nickenig G, Lütjohann D, Latz E (April 2016). "Cyclodextrin promotes atherosclerosis regression via macrophage reprogramming". Science Translational Medicine. 8 (333): 333ra50. doi:10.1126/scitranslmed.aad6100. PMC 4878149. PMID 27053774.
- Lay summary in: Hesman Saey T (April 8, 2016). "A sugar can melt away cholesterol". Science News.org.
- Wu H, Roks AJ (February 2014). "Genomic instability and vascular aging: a focus on nucleotide excision repair". Trends in Cardiovascular Medicine. 24 (2): 61–8. doi:10.1016/j.tcm.2013.06.005. PMID 23953979.
- ^ Bautista-Niño PK, Portilla-Fernandez E, Vaughan DE, Danser AH, Roks AJ (May 2016). "DNA Damage: A Main Determinant of Vascular Aging". International Journal of Molecular Sciences. 17 (5): 748. doi:10.3390/ijms17050748. PMC 4881569. PMID 27213333.
- Shah AV, Bennett MR (December 2017). "DNA damage-dependent mechanisms of ageing and disease in the macro- and microvasculature". European Journal of Pharmacology. 816: 116–128. doi:10.1016/j.ejphar.2017.03.050. PMID 28347738.
- ^ Martinet W, Knaapen MW, De Meyer GR, Herman AG, Kockx MM (August 2002). "Elevated levels of oxidative DNA damage and DNA repair enzymes in human atherosclerotic plaques". Circulation. 106 (8): 927–32. doi:10.1161/01.cir.0000026393.47805.21. PMID 12186795.
- Ishida T, Ishida M, Tashiro S, Yoshizumi M, Kihara Y (2014). "Role of DNA damage in cardiovascular disease". Circulation Journal. 78 (1): 42–50. doi:10.1253/circj.CJ-13-1194. PMID 24334614.
- ^ Barrington WT, Lusis AJ (December 2017). "Atherosclerosis: Association between the gut microbiome and atherosclerosis". Nature Reviews. Cardiology. 14 (12): 699–700. doi:10.1038/nrcardio.2017.169. PMC 5815826. PMID 29099096.
- Jie Z, Xia H, Zhong SL, Feng Q, Li S, Liang S, et al. (October 2017). "The gut microbiome in atherosclerotic cardiovascular disease". Nature Communications. 8 (1): 845. Bibcode:2017NatCo...8..845J. doi:10.1038/s41467-017-00900-1. PMC 5635030. PMID 29018189.
- ^ Harman JL, Jørgensen HF (October 2019). "The role of smooth muscle cells in plaque stability: Therapeutic targeting potential". British Journal of Pharmacology. 176 (19): 3741–3753. doi:10.1111/bph.14779. PMC 6780045. PMID 31254285.
- Bennett MR, Sinha S, Owens GK (February 2016). "Vascular Smooth Muscle Cells in Atherosclerosis". Circulation Research. 118 (4): 692–702. doi:10.1161/CIRCRESAHA.115.306361. PMC 4762053. PMID 26892967.
- Gomez D, Shankman LS, Nguyen AT, Owens GK (February 2013). "Detection of histone modifications at specific gene loci in single cells in histological sections". Nature Methods. 10 (2): 171–177. doi:10.1038/nmeth.2332. PMC 3560316. PMID 23314172.
- ^ Wang Y, Dubland JA, Allahverdian S, Asonye E, Sahin B, Jaw JE, et al. (May 2019). "Smooth Muscle Cells Contribute the Majority of Foam Cells in ApoE (Apolipoprotein E)-Deficient Mouse Atherosclerosis". Arteriosclerosis, Thrombosis, and Vascular Biology. 39 (5): 876–887. doi:10.1161/ATVBAHA.119.312434. PMC 6482082. PMID 30786740.
- ^ Chappell J, Harman JL, Narasimhan VM, Yu H, Foote K, Simons BD, et al. (December 2016). "Extensive Proliferation of a Subset of Differentiated, yet Plastic, Medial Vascular Smooth Muscle Cells Contributes to Neointimal Formation in Mouse Injury and Atherosclerosis Models". Circulation Research. 119 (12): 1313–1323. doi:10.1161/CIRCRESAHA.116.309799. PMC 5149073. PMID 27682618.
- Durham AL, Speer MY, Scatena M, Giachelli CM, Shanahan CM (March 2018). "Role of smooth muscle cells in vascular calcification: implications in atherosclerosis and arterial stiffness". Cardiovascular Research. 114 (4): 590–600. doi:10.1093/cvr/cvy010. PMC 5852633. PMID 29514202.
- Basatemur GL, Jørgensen HF, Clarke MC, Bennett MR, Mallat Z (December 2019). "Vascular smooth muscle cells in atherosclerosis". Nature Reviews. Cardiology. 16 (12): 727–744. doi:10.1038/s41569-019-0227-9. PMID 31243391.
External links
 Quotations related to Atherosclerosis at Wikiquote
Quotations related to Atherosclerosis at Wikiquote- Atherosclerosis pathophysiology-stages and types
| Classification | D |
|---|---|
| External resources |
| Cardiovascular disease (vessels) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Arteries, arterioles and capillaries | |||||||||
| Veins |
| ||||||||
| Arteries or veins | |||||||||
| Blood pressure |
| ||||||||