| Revision as of 03:04, 26 December 2011 editDavidruben (talk | contribs)Extended confirmed users18,994 edits →Medications: NICE document does not suggest renin inhibitors - a class of drug not used in any significant level in UK nor GTN,remove this as unrepresentative of real usage.← Previous edit | Revision as of 03:06, 26 December 2011 edit undoDavidruben (talk | contribs)Extended confirmed users18,994 editsm →Classification: into template form , then for ref botNext edit → | ||
| Line 74: | Line 74: | ||
| ] is an excessively high elevation in blood pressure during ].<ref name="pmid3583204">{{cite journal |author=Jetté M, Landry F, Blümchen G |title=Exercise hypertension in healthy normotensive subjects. Implications, evaluation and interpretation |journal=] |volume=12 |issue=2 |pages=110–8 |year=1987 |month=April |pmid=3583204 |doi= |url= }}</ref><ref name="pmid2953661">{{cite journal |author=Pickering TG |title=Pathophysiology of exercise hypertension |journal=] |volume=12 |issue=2 |pages=119–24 |year=1987 |month=April |pmid=2953661 |doi= |url= }}</ref><ref name="pmid3583205">{{cite journal |author=Rost R, Heck H |title= |language=German |journal=] |volume=12 |issue=2 |pages=125–33 |year=1987 |month=April |pmid=3583205 |doi= |url= }}</ref> The range considered normal for systolic values during exercise is between 200 and 230 mm Hg.<ref name="pmid3583208">{{cite journal |author=Klaus D |title= |language=German |journal=] |volume=12 |issue=2 |pages=146–55 |year=1987 |month=April |pmid=3583208 |doi= |url= }}</ref> Exercise hypertension may indicate that an individual is at risk for developing hypertension at rest.<ref name="pmid3583205" /><ref name="pmid3583208"/> | ] is an excessively high elevation in blood pressure during ].<ref name="pmid3583204">{{cite journal |author=Jetté M, Landry F, Blümchen G |title=Exercise hypertension in healthy normotensive subjects. Implications, evaluation and interpretation |journal=] |volume=12 |issue=2 |pages=110–8 |year=1987 |month=April |pmid=3583204 |doi= |url= }}</ref><ref name="pmid2953661">{{cite journal |author=Pickering TG |title=Pathophysiology of exercise hypertension |journal=] |volume=12 |issue=2 |pages=119–24 |year=1987 |month=April |pmid=2953661 |doi= |url= }}</ref><ref name="pmid3583205">{{cite journal |author=Rost R, Heck H |title= |language=German |journal=] |volume=12 |issue=2 |pages=125–33 |year=1987 |month=April |pmid=3583205 |doi= |url= }}</ref> The range considered normal for systolic values during exercise is between 200 and 230 mm Hg.<ref name="pmid3583208">{{cite journal |author=Klaus D |title= |language=German |journal=] |volume=12 |issue=2 |pages=146–55 |year=1987 |month=April |pmid=3583208 |doi= |url= }}</ref> Exercise hypertension may indicate that an individual is at risk for developing hypertension at rest.<ref name="pmid3583205" /><ref name="pmid3583208"/> | ||
| Orthostatic Hypertension is an abnormal increase in blood pressure when a person stands up. Orthostatic hypertension can precede or coexist with essential hypertension and may also coexist with other disorders such as ]. <ref> http://www.nature.com/nrneph/journal/v2/n8/full/ncpneph0228.html </ref> In a population based study, ] was found to exist in 1% of the population. <ref> |
Orthostatic Hypertension is an abnormal increase in blood pressure when a person stands up. Orthostatic hypertension can precede or coexist with essential hypertension and may also coexist with other disorders such as ]. <ref> http://www.nature.com/nrneph/journal/v2/n8/full/ncpneph0228.html </ref> In a population based study, ] was found to exist in 1% of the population. <ref>{{cite journal pmid=18712045}}</ref> | ||
| ==Signs and symptoms== | ==Signs and symptoms== | ||
Revision as of 03:06, 26 December 2011
This article is about arterial hypertension. For other forms of hypertension, see Hypertension (disambiguation). Medical condition| Hypertension | |
|---|---|
| Specialty | Family medicine, hypertensiology |
Hypertension (HTN) or high blood pressure, sometimes arterial hypertension, is a chronic medical condition in which the blood pressure in the arteries is elevated. This requires the heart is having to work harder than normal to circulate blood through the blood vessels. Blood pressure involves two measurements, systolic and diastolic, which depend on whether the heart muscle is contracting (systole) or relaxed (diastole) between beats. Normal blood pressure is at or below 120/80 mmHg. High blood pressure is said to be present if it is persistently above 140/90 mmHg.
Hypertension is classified as either primary (essential) hypertension or secondary hypertension; about 90–95% of cases are categorized as "primary hypertension" which means high blood pressure with no obvious underlying medical cause. The remaining 5–10% of cases (secondary hypertension) are caused by other conditions that affect the kidneys, arteries, heart or endocrine system.
Persistent hypertension is a major risk factor for stroke, myocardial infarction (heart attacks), heart failure and aneurysms of the arteries (e.g. aortic aneurysm), and is a leading cause of chronic kidney disease. Even moderate elevation of arterial blood pressure is associated with a shortened life expectancy. Dietary and lifestyle changes can improve blood pressure control and decrease the risk of associated health complications, although drug treatment is often necessary in patients for whom lifestyle changes prove ineffective or insufficient.
Classification

| Classification | Systolic pressure | Diastolic pressure | ||
|---|---|---|---|---|
| mmHg | kPa | mmHg | kPa | |
| Normal | 90–119 | 12–15.9 | 60–79 | 8.0–10.5 |
| Prehypertension | 120–139 | 16.0–18.5 | 80–89 | 10.7–11.9 |
| Stage 1 | 140–159 | 18.7–21.2 | 90–99 | 12.0–13.2 |
| Stage 2 | ≥160 | ≥21.3 | ≥100 | ≥13.3 |
| Isolated systolic hypertension |
≥140 | ≥18.7 | <90 | <12.0 |
| Source: American Heart Association (2003). | ||||
Blood pressure is usually classified based on the systolic and diastolic blood pressures. Systolic blood pressure is the blood pressure in vessels during a heart beat. Diastolic blood pressure is the pressure between heartbeats. A systolic or the diastolic blood pressure measurement higher than the accepted normal values for the age of the individual is classified as prehypertension or hypertension.
Hypertension has several sub-classifications, including hypertension stage I, hypertension stage II, and isolated systolic hypertension. Isolated systolic hypertension refers to elevated systolic pressure with normal diastolic pressure and is common in the elderly. These classifications are made after averaging a patient's resting blood pressure readings taken on two or more office visits. Individuals older than 40 years are classified as having hypertension if their blood pressure is consistently at least 140 mmHg systolic or 90 mmHg diastolic on clinic readings; alternatvely 135 mmHg systolic or 85 mmHg diastolic on 24-hour ambulatory or home monitoring. Patients with blood pressures higher than 130/80 mmHg with concomitant presence of diabetes mellitus or kidney disease require further treatment.
Hypertension is also classified as resistant if medications do not reduce blood pressure to normal levels.
Exercise hypertension is an excessively high elevation in blood pressure during exercise. The range considered normal for systolic values during exercise is between 200 and 230 mm Hg. Exercise hypertension may indicate that an individual is at risk for developing hypertension at rest.
Orthostatic Hypertension is an abnormal increase in blood pressure when a person stands up. Orthostatic hypertension can precede or coexist with essential hypertension and may also coexist with other disorders such as dysautonomia. In a population based study, orthostatic hypertension was found to exist in 1% of the population.
Signs and symptoms
Mild to moderate essential hypertension is usually asymptomatic.
Accelerated hypertension
Accelerated hypertension is associated with headache, drowsiness, confusion, vision disorders, nausea, and vomiting. These symptoms are collectively called hypertensive encephalopathy. Hypertensive encephalopathy is caused by severe small blood vessel congestion and brain swelling, which is reversible if blood pressure is lowered.
Secondary hypertension
Main article: Secondary hypertensionSome additional signs and symptoms suggest that the hypertension is caused by disorders in hormone regulation. Hypertension combined with obesity distributed on the trunk of the body, accumulated fat on the back of the neck ('buffalo hump'), wide purple marks on the abdomen (abdominal striae), or the recent onset of diabetes suggests that an individual has a hormone disorder known as Cushing's syndrome. Hypertension caused by other hormone disorders such as hyperthyroidism, hypothyroidism, or growth hormone excess will be accompanied by additional symptoms specific to these disorders. For example, hyperthyrodism can cause weight loss, tremors, heart rate abnormalities, reddening of the palms, and increased sweating. Signs and symptoms associated with growth hormone excess include coarsening of facial features, protrusion of the lower jaw, enlargement of the tongue, excessive hair growth, darkening of the skin color, and excessive sweating.. Other hormone disorders like hyperaldosteronism may cause less specific symptoms such as numbness, excessive urination, excessive sweating, electrolyte imbalances and dehydration, and elevated blood alkalinity. and also cause mental pressure.
In pregnancy
Hypertension in pregnant women is one symptom of pre-eclampsia. Pre-eclampsia can progress to a life-threatening condition called eclampsia, which is the development of protein in the urine, generalized swelling, and severe seizures. Other symptoms indicating that brain function is becoming impaired may precede these seizures such as nausea, vomiting, headaches, and vision loss.
In addition, the systemic vascular resistance and blood pressure decrease during pregnancy. The body must compensate by increasing cardiac output and blood volume to provide sufficient circulation in the utero-placental arterial bed.
In children
Some signs and symptoms are especially important in newborns and infants such as failure to thrive, seizures, irritability, lack of energy, and difficulty breathing. In children, hypertension can cause headache, fatigue, blurred vision, nosebleeds, and facial paralysis.
Even with the above clinical symptoms, the true incidence of pediatric hypertension is not known. In adults, hypertension has been defined due to the adverse effects caused by hypertension. However, in children, similar studies have not been performed thoroughly to link any adverse effects with the increase in blood pressure. Therefore, the prevalence of pediatric hypertension remains unknown due to the lack of scientific knowledge.
Cause
Essential hypertension
Main article: Essential hypertensionEssential hypertension is the most prevalent hypertension type, affecting 90–95% of hypertensive patients. Although no direct cause has been identified, there are many factors such as sedentary lifestyle, smoking, stress, obesity (particularly visceral obesity, where the excess weight is concentrated around the waist as opposed to the hips) (more than 85% of cases occur in those with a body mass index greater than 25), salt (sodium) sensitivity, alcohol intake, and vitamin D deficiency that increase the risk of developing hypertension. Risk also increases with aging, some inherited genetic mutations, and having a family history of hypertension. An elevated level of renin, a hormone secreted by the kidney, is another risk factor, as is sympathetic nervous system overactivity. Insulin resistance, which is a component of syndrome X (or the metabolic syndrome), is also thought to contribute to hypertension. Recent studies have implicated low birth weight as a risk factor for adult essential hypertension.
Secondary hypertension
Main article: Secondary hypertensionSecondary hypertension by definition results from an identifiable cause. This type is important to recognize since it's treated differently to essential hypertension, by treating the underlying cause of the elevated blood pressure. Hypertension results in the compromise or imbalance of the pathophysiological mechanisms, such as the hormone-regulating endocrine system, that regulate blood plasma volume and heart function. Many conditions cause hypertension. Some are common, well-recognized secondary causes such as renovascular hypertension and Cushing's syndrome, which is a condition where the adrenal glands overproduce the hormone cortisol. Hypertension is also caused by other conditions that cause hormone changes, such as hyperthyroidism, hypothyroidism, and certain tumors of the adrenal medulla (e.g., pheochromocytoma). Other common causes of secondary hypertension include kidney disease, obesity/metabolic disorder, pre-eclampsia during pregnancy, the congenital defect known as coarctation of the aorta, and certain prescription and illegal drugs.
Pathophysiology
Main article: Pathophysiology of hypertension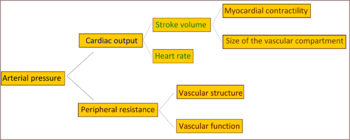
Most of the mechanisms associated with secondary hypertension are generally fully understood. However, those associated with essential (primary) hypertension are far less understood. What is known is that cardiac output is raised early in the disease course, with total peripheral resistance (TPR) normal; over time cardiac output drops to normal levels but TPR is increased. Three theories have been proposed to explain this:
- Inability of the kidneys to excrete sodium, resulting in natriuretic factors such as Atrial Natriuretic Factor being secreted to promote salt excretion with the side effect of raising total peripheral resistance.
- An overactive Renin-angiotensin system leads to vasoconstriction and retention of sodium and water. The increase in blood volume plus vasoconstriction leads to hypertension.
- An overactive sympathetic nervous system, leading to increased stress responses.
It is also known that hypertension is highly heritable and polygenic (caused by more than one gene) and a few candidate genes have been postulated in the etiology of this condition.
Recently, work related to the association between essential hypertension and sustained endothelial damage has gained popularity among hypertension scientists. It remains unclear, however, whether endothelial changes precede the development of hypertension or whether such changes are mainly due to longstanding elevated blood pressures.
Diagnosis
Hypertension is generally diagnosed on the basis of a persistently high blood pressure. Traditionally, this requires three separate sphygmomanometer measurements at one monthly intervals. Initial assessment of the hypertensive patient should include a complete history and physical examination. Exceptionally, if the elevation is extreme, or if symptoms of organ damage are present, then a diagnosis may be made and treatment started immediately. With the availability of 24-hour ambulatory blood pressure monitors and home blood pressure machines, the importance of not wrongly diangosing those who have white coat hypertension has lead to a change in protocol advice in the United Kingdom, with best practice of now following up a single raised clinic reading with ambulatory measurement, or less ideally with home blood pressure monitring over the course of 7 days.
Once the diagnosis of hypertension has been made, physicians will attempt to identify the underlying cause based on risk factors and other symptoms, if present. Secondary hypertension is more common in preadolescent children, with most cases caused by renal disease. Primary or essential hypertension is more common in adolescents and has multiple risk factors, including obesity and a family history of hypertension. Laboratory tests can also be performed to identify possible causes of secondary hypertension, and to determine whether hypertension has caused damage to the heart, eyes, and kidneys. Additional tests for diabetes and high cholesterol levels are usually performed because these conditions are additional risk factors for the development of heart disease and require treatment. Typical tests are classified as follows:
| System | Tests |
|---|---|
| Renal | Microscopic urinalysis, proteinuria, serum BUN (blood urea nitrogen) and/or creatinine |
| Endocrine | Serum sodium, potassium, calcium, TSH (thyroid-stimulating hormone). |
| Metabolic | Fasting blood glucose, total cholesterol, HDL and LDL cholesterol, triglycerides |
| Other | Hematocrit, electrocardiogram, and chest radiograph |
| Sources: Harrison's principles of internal medicine others | |
Creatinine (renal function) testing is done to assess the presence of kidney disease, which can be either the cause or the result of hypertension. In addition, creatinine testing provides a baseline measurement of kidney function that can be used to monitor for side effects of certain antihypertensive drugs on kidney function. Additionally, testing of urine samples for protein is used as a secondary indicator of kidney disease. Glucose testing is done to determine if diabetes mellitus is present. Electrocardiogram (EKG/ECG) testing is done to check for evidence that the heart is under strain from high blood pressure. It may also show whether there is thickening of the heart muscle (left ventricular hypertrophy) or whether the heart has experienced a prior minor disturbance such as a silent heart attack. A chest X-ray may be performed to look for signs of heart enlargement or damage to heart tissue.
Prevention
The degree to which hypertension can be prevented depends on a number of features including current blood pressure level, sodium/potassium balance, detection and omission of environmental toxins, changes in end/target organs (retina, kidney, heart, among others), risk factors for cardiovascular diseases and the age at diagnosis of prehypertension or at risk for hypertension. A prolonged assessment that involves repeated blood pressure measurements provides the most accurate blood pressure level assessment. Following this, lifestyle changes are recommended to lower blood pressure, before the initiation of prescription drug therapy. According to the British Hypertension Society, the process of managing prehypertension includes lifestyle changes such as the following:
- Weight reduction and regular aerobic exercise (e.g., walking): Regular exercise improves blood flow and helps to reduce the resting heart rate and blood pressure.
- Reduce dietary sugar
- Reduce sodium (salt) in the body by disuse of condiment sodium and the adoption of a high potassium diet which rids the renal system of excess sodium. Many people use potassium chloride salt substitute to reduce their salt intake.
- Additional dietary changes beneficial to reducing blood pressure include the DASH diet (as demonstrated by the Dietary Approaches to Stop Hypertension study) which is rich in fruits and vegetables and low-fat or fat-free dairy products
- Discontinuing tobacco use and alcohol consumption has been shown to lower blood pressure. The exact mechanisms are not fully understood, but blood pressure (especially systolic) always transiently increases following alcohol or nicotine consumption. Abstaining from cigarette smoking reduces the risks of stroke and heart attack associated with hypertension.
- Vasodilators such as niacin
- Limiting alcohol intake to less than two standard drinks per day can reduce systolic blood pressure by 2–4 mmHg.
- Reducing stress
- Increasing omega 3 fatty acids can help lower hypertension. Fish oil is shown to lower blood pressure in hypertensive individuals. The fish oil may increase sodium and water excretion.
- Caffeine raises blood pressure
- Theobromine lowers blood pressure, through its actions as both a vasodilator and a diuretic
Treatment
Lifestyle modifications
The first line of treatment for hypertension is identical to the recommended preventive lifestyle changes and includes: dietary changes physical exercise, and weight loss. These have all been shown to significantly reduce blood pressure in people with hypertension. If hypertension is high enough to justify immediate use of medications, lifestyle changes are still recommended in conjunction with medication. Drug prescription should take into account the patient's absolute cardiovascular risk (including risk of myocardial infarction and stroke) as well as blood pressure readings, in order to gain a more accurate picture of the patient's cardiovascular profile. Different programs aimed to reduce psychological stress such as biofeedback, relaxation or meditation are advertised to reduce hypertension. However, in general claims of efficacy are not supported by scientific studies, which have been in general of low quality.
Regarding dietary changes, a low sodium diet is beneficial. A long term (more than 4 weeks) low sodium diet in Caucasians is effective in reducing blood pressure, both in people with hypertension and in people with normal blood pressure. Also, the DASH diet (Dietary Approaches to Stop Hypertension) is a diet promoted by the National Heart, Lung, and Blood Institute (part of the NIH, a United States government organization) to control hypertension. A major feature of the plan is limiting intake of sodium, and it also generally encourages the consumption of nuts, whole grains, fish, poultry, fruits and vegetables while lowering the consumption of red meats, sweets, and sugar. It is also "rich in potassium, magnesium, and calcium, as well as protein".
Medications
Several classes of medications, collectively referred to as antihypertensive drugs, are currently available for treating hypertension. Reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischaemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. The aim of treatment should be to reduce blood pressure to <140/90 mmHg for most individuals, and lower for individuals with diabetes or kidney disease (some medical professionals recommend keeping levels below 120/80 mmHg). If the blood pressure goal is not met, a change in treatment should be made as therapeutic inertia is a clear impediment to blood pressure control. Comorbidity also plays a role in determining target blood pressure, with lower BP targets applying to patients with end-organ damage or proteinuria.
Often multiple medications are needed to be combined to achieve the goal blood pressure. Guidelines on the choice of first line agent and how to best to step up treatment with multiple agents for various subgroups of patients have changed over time and differ between countries.
In the UK low dose thiazide-based diuretic were previously thought the best first line agent, but latest guidelines emphasise calcium channel blockers (CCB) in preference for patients over the age of 55 years or if of African or Caribbean family origin, with angiotensin converting enzyme inhibitors (ACE-I) used first line for younger patients. Preferred dual therapy is generally CCB with an ACE-I, and triple therapy with addition of a thiazide-like diuretic. If a fourth agent is needed then additional diuretics of spironolactone or a higher-dose of a thiazide-like diuretics. Additional agents that may be considered are alpha blockers or beta blockers. Angiotensin II receptor antagonists are suggested as preferable to ACE-I for black people of African or Caribbean family origin, and are an alternative for patients who are unable to tolerate ACE-I. Beta-blockers may be also be considered first line in younger people, and women of child-bearing potential.
Combination tablets
Tablets containing fixed combinations of two classes of drugs are available and whilst convenient for the patient, may be best reserved for patients who have been established on the individual components.
Some examples of common combined prescription drug include:
- A fixed combination of an ACE inhibitor and a calcium channel blocker. One example of this is the combination of perindopril and amlodipine, the efficacy of which has been demonstrated in individuals with glucose intolerance or metabolic syndrome.
- A fixed combination of a diuretic and an angiotensin blocker - ARB.
Combinations of an ACE-inhibitor or angiotensin II–receptor antagonist, a diuretic and an NSAID (including selective COX-2 inhibitors and non-prescribed drugs such as ibuprofen) should be avoided whenever possible due to a high documented risk of acute renal failure. The combination is known colloquially as a "triple whammy" in the Australian health industry.
In the elderly
Treating moderate to severe high blood pressure decreases death rates in those under 80 years of age. In those over 80 years old there was a decrease in morbidity but no decrease in mortality. The recommended BP goal is advised as <140/90 mm Hg with thiazide diuretics being the first line medication in America, but in the revised UK guidelines calcium-channel blockers are advocated with targets of clinic readings <150/90, or <145/85 on ambulatory or home blood pressure monitoring.
Resistant
Guidelines for treating resistant hypertension have been published in the UK and US.
Complications
Main article: Complications of hypertension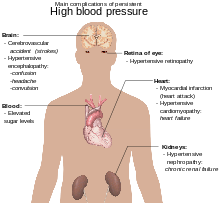
Hypertension is the most important risk factor for death in industrialized countries. It increases hardening of the arteries thus predisposes individuals to heart disease, peripheral vascular disease, and strokes. Types of heart disease that may occur include: myocardial infarction, heart failure, and left ventricular hypertrophy Other complications include:
- Hypertensive retinopathy
- Hypertensive nephropathy
- If blood pressure is very high hypertensive encephalopathy may result.
- Silent stroke is a type of stroke (infarct) that does not have any outward symptoms (asymptomatic), and the patient is typically unaware they have suffered a stroke. Despite not causing identifiable symptoms a silent stroke still causes damage to the brain, and places the patient at increased risk for a major stroke in the future. Hypertension is the major treatable risk factor associated with silent stokes.
Epidemiology
In the year 2000 it is estimated that nearly one billion people or ~26% of the adult population had hypertension worldwide. It was common in both developed (333 million ) and undeveloped (639 million) countries. However rates vary markedly in different regions with rates as low as 3.4% (men) and 6.8% (women) in rural India and as high as 68.9% (men) and 72.5% (women) in Poland.
In 1995 it is estimated that 43 million people in the United States had hypertension or were taking antihypertensive medication, almost 24% of the adult population. The prevalence of hypertension in the United States is increasing and reached 29% in 2004. It is more common in blacks and native Americans and less in whites and Mexican Americans, rates increase with age, and is greater in the southeastern United States. Hypertension is more prevalent in men (though menopause tends to decrease this difference) and those of low socioeconomic status.
Over 90–95% of adult hypertension is essential hypertension. One of the most common causes of secondary hypertension is primary aldosteronism. The incidence of exercise hypertension is reported to range from 1–10%.
In children
The prevalence of high blood pressure in the young is increasing. Most childhood hypertension, particularly in preadolescents, is secondary to an underlying disorder. Kidney disease is the most common (60–70%) cause of hypertension in children. Adolescents usually have primary or essential hypertension, which accounts for 85–95% of cases.
History
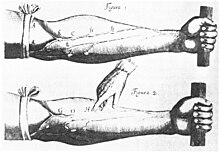
Some cite the writings of Sushruta in the 6th century BC as being the first mention of symptoms like those of hypertension. Others propose even earlier descriptions dating as far as 2600 BCE. Main treatment for what was called the "hard pulse disease" consisted in reducing the quantity of blood in a subject by the sectioning of veins or the application of leeches. Well known individuals such as The Yellow Emperor of China, Cornelius Celsus, Galen, and Hipocrates advocated such treatments.
Our modern understanding of hypertension began with the work of physician William Harvey (1578–1657), who was the first to describe correctly the systemic circulation of blood being pumped around the body by the heart in his book "De motu cordis". The basis for measuring blood pressure were established by Stephen Hales in 1733. Initial descriptions of hypertension as a disease came among others from Thomas Young in 1808 and specially Richard Bright in 1836. The first ever elevated blood pressure in a patient without kidney disease was reported by Frederick Mahomed (1849–1884). It was not until 1904 that sodium restriction was advocated while a rice diet was popularized around 1940.
Studies in the 1920s demonstrated the public health impact of untreated high blood pressure; treatment options were limited at the time, and deaths from malignant hypertension and its complications were common. A prominent victim of severe hypertension leading to cerebral hemorrhage was Franklin D. Roosevelt (1882–1945). The Framingham Heart Study added to the epidemiological understanding of hypertension and its relationship with coronary artery disease. The National Institutes of Health also sponsored other population studies, which additionally showed that African Americans had a higher burden of hypertension and its complications. Before pharmacological treatment for hypertension became possible, three treatment modalities were used, all with numerous side-effects: strict sodium restriction, sympathectomy (surgical ablation of parts of the sympathetic nervous system), and pyrogen therapy (injection of substances that caused a fever, indirectly reducing blood pressure).
The first chemical for hypertension, sodium thiocyanate, was used in 1900 but had many side effects and was unpopular. Several other agents were developed after the Second World War, the most popular and reasonably effective of which were tetramethylammonium chloride and its derivative hexamethonium, hydralazine and reserpine (derived from the medicinal plant Rauwolfia serpentina). A randomized controlled trial sponsored by the Veterans Administration using these drugs had to be stopped early because those not receiving treatment were developing more complications and it was deemed unethical to withhold treatment from them. These studies prompted public health campaigns to increase public awareness of hypertension and the advice to get blood pressure measured and treated. These measures appear to have contributed at least in part of the observed 50% fall in stroke and ischemic heart disease between 1972 and 1994.
A major breakthrough was achieved with the discovery of the first well-tolerated orally available agents. The first was chlorothiazide, the first thiazide and developed from the antibiotic sulfanilamide, which became available in 1958; it increased salt excretion while preventing fluid accumulation. In 1975, the Lasker Special Public Health Award was awarded to the team that developed chlorothiazide. The British physician James W. Black developed beta blockers in the early 1960s; these were initially used for angina, but turned out to lower blood pressure. Black received the 1976 Lasker Award and in 1988 the Nobel Prize in Physiology or Medicine for his discovery. The next class of antihypertensives to be discovered was that of the calcium channel blockers. The first member was verapamil, a derivative of papaverine that was initially thought to be a beta blocker and used for angina, but then turned out to have a different mode of action and was shown to lower blood pressure. ACE inhibitors were developed through rational drug design; the renin-angiotensin system was known to play an important role in blood pressure regulation, and snake venom from Bothrops jararaca could lower blood pressure through inhibition of ACE. In 1977 captopril, an orally active agent, was described; this led to the development of a number of other ACE inhibitors.
Society and culture
Economics
The National Heart, Lung, and Blood Institute (NHLBI) estimated in 2002 that hypertension cost the United States $47.2 billion.
High blood pressure is the most common chronic medical problem prompting visits to primary health care providers, yet it is estimated that only 34% of the 50 million American adults with hypertension have their blood pressure controlled to a level of <140/90 mm Hg. Thus, about two thirds of Americans with hypertension are at increased risk for heart disease. The medical, economic, and human costs of untreated and inadequately controlled high blood pressure are enormous. Adequate management of hypertension can be hampered by inadequacies in the diagnosis, treatment, and/or control of high blood pressure. Health care providers face many obstacles to achieving blood pressure control from their patients, including resistance to taking multiple medications to reach blood pressure goals. Patients also face the challenges of adhering to medicine schedules and making lifestyle changes. Nonetheless, the achievement of blood pressure goals is possible, and most importantly, lowering blood pressure significantly reduces the risk of death due to heart disease, the development of other debilitating conditions, and the cost associated with advanced medical care.,
Awareness

The World Health Organization attributes hypertension, or high blood pressure, as the leading cause of cardiovascular mortality. The World Hypertension League (WHL), an umbrella organization of 85 national hypertension societies and leagues, recognized that more than 50% of the hypertensive population worldwide are unaware of their condition. To address this problem, the WHL initiated a global awareness campaign on hypertension in 2005 and dedicated May 17 of each year as World Hypertension Day (WHD). Over the past three years, more national societies have been engaging in WHD and have been innovative in their activities to get the message to the public. In 2007, there was record participation from 47 member countries of the WHL. During the week of WHD, all these countries – in partnership with their local governments, professional societies, nongovernmental organizations and private industries – promoted hypertension awareness among the public through several media and public rallies. Using mass media such as Internet and television, the message reached more than 250 million people. As the momentum picks up year after year, the WHL is confident that almost all the estimated 1.5 billion people affected by elevated blood pressure can be reached.
References
- ^ Carretero OA, Oparil S (2000). "Essential hypertension. Part I: definition and etiology". Circulation. 101 (3): 329–35. doi:10.1161/01.CIR.101.3.329. PMID 10645931.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Chobanian AV; Bakris GL; Black HR; et al. (2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension. 42 (6): 1206–52. doi:10.1161/01.HYP.0000107251.49515.c2. PMID 14656957.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - "High blood pressure - NHS". National Health Service (NHS).
- ^ National Clinical Guidence Centre (August 2011). "7 Diagnosis of Hypertension, 7.5 Link from evidence to recommendations". Hypertension (NICE CG 127) (PDF). National Institute for Health and Clinical Excellence. p. 102. Retrieved 2011-12-22.
- Jetté M, Landry F, Blümchen G (1987). "Exercise hypertension in healthy normotensive subjects. Implications, evaluation and interpretation". Herz. 12 (2): 110–8. PMID 3583204.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Pickering TG (1987). "Pathophysiology of exercise hypertension". Herz. 12 (2): 119–24. PMID 2953661.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rost R, Heck H (1987). "". Herz (in German). 12 (2): 125–33. PMID 3583205.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Klaus D (1987). "". Herz (in German). 12 (2): 146–55. PMID 3583208.
{{cite journal}}: Unknown parameter|month=ignored (help) - http://www.nature.com/nrneph/journal/v2/n8/full/ncpneph0228.html
- Template:Cite journal pmid=18712045
- Pitts SR, Adams RP (1998). "Emergency department hypertension and regression to the mean". Annals of Emergency Medicine. 31 (2): 214–8. doi:10.1016/S0196-0644(98)70309-9. PMID 9472183.
{{cite journal}}: Unknown parameter|month=ignored (help) - Papadakis, Maxine A.; McPhee, Stephen J. (2008). Current Medical Diagnosis and Treatment 2009 (Current Medical Diagnosis and Treatment). McGraw-Hill Professional. ISBN 0-07-159124-9.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Lee, Stephanie L (April 26, 2010). "Hyperthyroidism". eMedicine Endocrinology. Medscape. Retrieved 2009-06-16.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Khandwala, Hasnain M (February 13, 2009). "Acromegaly". eMedicine Endocrinology. Medscape. Retrieved 2009-06-16.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin:no Clinical Dermatology (10th ed.). 56.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Chrousos, George P (March 4, 2009). "Hyperaldosteronism". eMedicine Pediatrics: General Medicine. Medscape. Retrieved 2009-06-16.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Gibson, Paul (July 30, 2009). "Hypertension and Pregnancy". eMedicine Obstetrics and Gynecology. Medscape. Retrieved 2009-06-16.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - Fabry, IG; Richart, T; Chengz, X; Van Bortel, LM; Staessen, JA (2010). "Diagnosis and treatment of hypertensive disorders during pregnancy". Acta clinica Belgica. 65 (4): 229–36. PMID 20954460.
- ^ Rodriguez-Cruz, Edwin (April 6, 2010). "Hypertension". eMedicine Pediatrics: Cardiac Disease and Critical Care Medicine. Medscape. Retrieved 2009-06-16.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - http://emedicine.medscape.com/article/889877-overview
- Kyrou I, Chrousos GP, Tsigos C (2006). "Stress, visceral obesity, and metabolic complications". Annals of the New York Academy of Sciences. 1083: 77–110. doi:10.1196/annals.1367.008. PMID 17148735.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Wofford MR, Hall JE (2004). "Pathophysiology and treatment of obesity hypertension". Current Pharmaceutical Design. 10 (29): 3621–37. doi:10.2174/1381612043382855. PMID 15579059.
- Haslam DW, James WP (2005). "Obesity". Lancet. 366 (9492): 1197–209. doi:10.1016/S0140-6736(05)67483-1. PMID 16198769.
- Lackland DT, Egan BM (2007). "Dietary salt restriction and blood pressure in clinical trials". Curr. Hypertens. Rep. 9 (4): 314–9. doi:10.1007/s11906-007-0057-8. PMID 17686383.
{{cite journal}}: Unknown parameter|month=ignored (help) - Djoussé L, Mukamal KJ (2009). "Alcohol consumption and risk of hypertension: does the type of beverage or drinking pattern matter?". Revista Española De Cardiología. 62 (6): 603–5. doi:10.1016/S1885-5857(09)72223-6. PMID 19480755.
{{cite journal}}: Unknown parameter|month=ignored (help) - Tuohimaa P (2009). "Vitamin D and aging". The Journal of Steroid Biochemistry and Molecular Biology. 114 (1–2): 78–84. doi:10.1016/j.jsbmb.2008.12.020. PMID 19444937.
{{cite journal}}: Unknown parameter|month=ignored (help) - Lee JH, O'Keefe JH, Bell D, Hensrud DD, Holick MF (2008). "Vitamin D deficiency an important, common, and easily treatable cardiovascular risk factor?". J. Am. Coll. Cardiol. 52 (24): 1949–56. doi:10.1016/j.jacc.2008.08.050. PMID 19055985.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Kosugi T, Nakagawa T, Kamath D, Johnson RJ (2009). "Uric acid and hypertension: an age-related relationship?". J Hum Hypertens. 23 (2): 75–6. doi:10.1038/jhh.2008.110. PMID 18754017.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Dickson ME, Sigmund CD (2006). "Genetic basis of hypertension: revisiting angiotensinogen". Hypertension. 48 (1): 14–20. doi:10.1161/01.HYP.0000227932.13687.60. PMID 16754793.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Luma GB, Spiotta RT (2006). "Hypertension in children and adolescents". Am Fam Physician. 73 (9): 1558–68. PMID 16719248.
{{cite journal}}: Unknown parameter|month=ignored (help) Cite error: The named reference "pmid16719248" was defined multiple times with different content (see the help page). - ^ Segura J, Ruilope LM (2007). "Obesity, essential hypertension and renin-angiotensin system". Public Health Nutrition. 10 (10A): 1151–5. doi:10.1017/S136898000700064X. PMID 17903324.
{{cite journal}}: Unknown parameter|month=ignored (help) - Rahmouni K, Correia ML, Haynes WG, Mark AL (2005). "Obesity-associated hypertension: new insights into mechanisms". Hypertension. 45 (1): 9–14. doi:10.1161/01.HYP.0000151325.83008.b4. PMID 15583075.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Sorof J, Daniels S (2002). "Obesity hypertension in children: a problem of epidemic proportions". Hypertension. 40 (4): 441–7. doi:10.1161/01.HYP.0000032940.33466.12. PMID 12364344. Retrieved 2009-06-03.
{{cite journal}}: Unknown parameter|month=ignored (help) - Uchiyama M (2008). "". Nippon Rinsho (in Japanese). 66 (8): 1477–80. PMID 18700545.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Dodt C, Wellhöner JP, Schütt M, Sayk F (2009). "". Der Internist (in German). 50 (1): 36–41. doi:10.1007/s00108-008-2197-6. PMID 19096817.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Pimenta E, Oparil S (2009). "Role of aliskiren in cardio-renal protection and use in hypertensives with multiple risk factors". Vascular Health and Risk Management. 5 (1): 453–63. PMC 2686262. PMID 19475781.
- Takahashi H (2008). "". Nippon Rinsho. Japanese Journal of Clinical Medicine (in Japanese). 66 (8): 1495–502. PMID 18700548.
{{cite journal}}: Unknown parameter|month=ignored (help) - Sagnella GA, Swift PA (2006). "The Renal Epithelial Sodium Channel: Genetic Heterogeneity and Implications for the Treatment of High Blood Pressure". Current Pharmaceutical Design. 12 (14): 2221–34. doi:10.2174/138161206777585157. PMID 16787251.
{{cite journal}}: Unknown parameter|month=ignored (help) - North of England Hypertension Guideline Development Group (1st August 2004). "Frequency of measurements". Essential hypertension (NICE CG18). National Institute for Health and Clinical Excellence. p. 53. Retrieved 2011-12-22.
{{cite book}}: Check date values in:|date=(help) - Loscalzo, Joseph; Fauci, Anthony S.; Braunwald, Eugene; Dennis L. Kasper; Hauser, Stephen L; Longo, Dan L. (2008). Harrison's principles of internal medicine. McGraw-Hill Medical. ISBN 0-07-147691-1.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Padwal RS; Hemmelgarn BR; Khan NA; et al. (2009). "The 2009 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". The Canadian Journal of Cardiology. 25 (5): 279–86. doi:10.1016/S0828-282X(09)70491-X. PMC 2707176. PMID 19417858.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ Mulatero P; Bertello C; Verhovez A; et al. (2009). "Differential diagnosis of primary aldosteronism subtypes". Current Hypertension Reports. 11 (3): 217–23. doi:10.1007/s11906-009-0038-1. PMID 19442332.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Padwal RJ; Hemmelgarn BR; Khan NA; et al. (2008). "The 2008 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". The Canadian Journal of Cardiology. 24 (6): 455–63. doi:10.1016/S0828-282X(08)70619-6. PMC 2643189. PMID 18548142.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Padwal RS; Hemmelgarn BR; McAlister FA; et al. (2007). "The 2007 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". The Canadian Journal of Cardiology. 23 (7): 529–38. doi:10.1016/S0828-282X(07)70797-3. PMC 2650756. PMID 17534459.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Hemmelgarn BR; McAlister FA; Grover S; et al. (2006). "The 2006 Canadian Hypertension Education Program recommendations for the management of hypertension: Part I – Blood pressure measurement, diagnosis and assessment of risk". The Canadian Journal of Cardiology. 22 (7): 573–81. doi:10.1016/S0828-282X(06)70279-3. PMC 2560864. PMID 16755312.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Hemmelgarn BR; McAllister FA; Myers MG; et al. (2005). "The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: part 1- blood pressure measurement, diagnosis and assessment of risk". The Canadian Journal of Cardiology. 21 (8): 645–56. PMID 16003448.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Elley CR, Arroll B (2002). "Review: aerobic exercise reduces systolic and diastolic blood pressure in adults". ACP J. Club. 137 (3): 109. PMID 12418849.
- Mohan S, Campbell NR, Willis K (2009). "Effective population-wide public health interventions to promote sodium reduction". CMAJ. 181 (9): 605–9. doi:10.1503/cmaj.090361. PMC 2764755. PMID 19752102.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "NPS Prescribing Practice Review 52: Treating hypertension". NPS Medicines Wise. September 1, 2010. Retrieved November 5, 2010.
- Morris MC, Sacks F, Rosner B (1993). "Does Fish oil lower blood pressure?". Journal of Human Hypertension (88): 523–533.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Siebenhofer, A (2011 Sep 7). Siebenhofer, Andrea (ed.). "Long-term effects of weight-reducing diets in hypertensive patients". Cochrane database of systematic reviews (Online). 9: CD008274. doi:10.1002/14651858.CD008274.pub2. PMID 21901719.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Blumenthal JA; Babyak MA; Hinderliter A; et al. (2010). "Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study". Arch. Intern. Med. 170 (2): 126–35. doi:10.1001/archinternmed.2009.470. PMID 20101007.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ Nelson, Mark. "Drug treatment of elevated blood pressure". Australian Prescriber (33): 108–112. Retrieved August 11, 2010.
- Greenhalgh J, Dickson R, Dundar Y (2009). "The effects of biofeedback for the treatment of essential hypertension: a systematic review". Health Technol Assess. 13 (46): 1–104. doi:10.3310/hta13460. PMID 19822104.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Rainforth MV, Schneider RH, Nidich SI, Gaylord-King C, Salerno JW, Anderson JW (2007). "Stress Reduction Programs in Patients with Elevated Blood Pressure: A Systematic Review and Meta-analysis". Curr. Hypertens. Rep. 9 (6): 520–8. doi:10.1007/s11906-007-0094-3. PMC 2268875. PMID 18350109.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Ospina MB; Bond K; Karkhaneh M; et al. (2007). "Meditation practices for health: state of the research". Evid Rep Technol Assess (Full Rep) (155): 1–263. PMID 17764203.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - He FJ, MacGregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No.: CD004937. DOI: 10.1002/14651858.CD004937.
- "Your Guide To Lowering Your Blood Pressure With DASH" (PDF). Retrieved 2009-06-08.
- Law M, Wald N, Morris J (2003). "Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy" (PDF). Health Technol Assess. 7 (31): 1–94. PMID 14604498.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Shaw, Gina (2009-03-07). "Prehypertension: Early-stage High Blood Pressure". WebMD. Retrieved 2009-07-03.
- Eni C. Okonofua; Kit N. Simpson; Ammar Jesri; Shakaib U. Rehman; Valerie L. Durkalski; Brent M. Egan (January 23, 2006). "Therapeutic Inertia Is an Impediment to Achieving the Healthy People 2010 Blood Pressure Control Goals". Hypertension. 47 (2006, 47:345): 345–51. doi:10.1161/01.HYP.0000200702.76436.4b. PMID 16432045. Retrieved 2009-11-22.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Wright JM, Musini VM (2009). Wright, James M (ed.). "First-line drugs for hypertension". Cochrane Database Syst Rev (3): CD001841. doi:10.1002/14651858.CD001841.pub2. PMID 19588327.
- ^ National Institute Clinical Excellence (August 2011). "1.5 Initiating and monitoring antihypertensive drug treatment, including blood pressure targets". GC127 Hypertension: Clinical management of primary hypertension in adults. Retrieved 2011-12-23.
- "2.5.5.1 Angiotensin-converting enzyme inhibitors". British National Formulary. Vol. No. 62. September 2011.
{{cite book}}:|access-date=requires|url=(help);|volume=has extra text (help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - Widimský J (2009). "". Vnitr̆ní Lékar̆ství (in Czech). 55 (2): 123–30. PMID 19348394.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Musini VM, Tejani AM, Bassett K, Wright JM (2009). Musini, Vijaya M (ed.). "Pharmacotherapy for hypertension in the elderly". Cochrane Database Syst Rev (4): CD000028. doi:10.1002/14651858.CD000028.pub2. PMID 19821263.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - http://content.onlinejacc.org/cgi/reprint/j.jacc.2011.01.008v1.pdf ACCF/AHA 2011 Expert Consensus Document on Hypertension in the Elderly
- "CG34 Hypertension - quick reference guide" (PDF). National Institute for Health and Clinical Excellence. 28 June 2006. Retrieved 2009-03-04.
- Calhoun DA; Jones D; Textor S; et al. (2008). "Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research". Hypertension. 51 (6): 1403–19. doi:10.1161/HYPERTENSIONAHA.108.189141. PMID 18391085.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Novo S, Lunetta M, Evola S, Novo G (2009). "Role of ARBs in the blood hypertension therapy and prevention of cardiovascular events". Current Drug Targets. 10 (1): 20–5. doi:10.2174/138945009787122897. PMID 19149532.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Riccioni G (2009). "The effect of antihypertensive drugs on carotid intima media thickness: an up-to-date review". Current Medicinal Chemistry. 16 (8): 988–96. doi:10.2174/092986709787581923. PMID 19275607.
- Agabiti-Rosei E (2008). "From macro- to microcirculation: benefits in hypertension and diabetes". Journal of Hypertension. 26 Suppl 3: S15–21. doi:10.1097/01.hjh.0000334602.71005.52. PMID 18815511.
{{cite journal}}: Unknown parameter|month=ignored (help) - Singer DR, Kite A (2008). "Management of hypertension in peripheral arterial disease: does the choice of drugs matter?". European Journal of Vascular and Endovascular Surgery. 35 (6): 701–8. doi:10.1016/j.ejvs.2008.01.007. PMID 18375152.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ White WB (2009). "Defining the problem of treating the patient with hypertension and arthritis pain". The American Journal of Medicine. 122 (5 Suppl): S3–9. doi:10.1016/j.amjmed.2009.03.002. PMID 19393824.
{{cite journal}}: Unknown parameter|month=ignored (help) - Pedrinelli R, Dell'Omo G, Talini E, Canale ML, Di Bello V (2009). "Systemic hypertension and the right-sided cardiovascular system: a review of the available evidence". Journal of Cardiovascular Medicine (Hagerstown, Md.). 10 (2): 115–21. doi:10.2459/JCM.0b013e32831da941. PMID 19377378.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Giacchetti G, Turchi F, Boscaro M, Ronconi V (2009). "Management of primary aldosteronism: its complications and their outcomes after treatment". Current Vascular Pharmacology. 7 (2): 244–49. doi:10.2174/157016109787455716. PMID 19356005.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Rodríguez NA, Zurutuza A (2008). "[Ophthalmological manifestations of arterial hypertension]". Anales Del Sistema Sanitario De Navarra (in Spanish; Castilian). 31 Suppl 3: 13–22. PMID 19169291. Retrieved 2009-06-21.
{{cite journal}}: CS1 maint: unrecognized language (link) - Zeng C, Villar VA, Yu P, Zhou L, Jose PA (2009). "Reactive oxygen species and dopamine receptor function in essential hypertension". Clinical and Experimental Hypertension. 31 (2): 156–78. doi:10.1080/10641960802621283. PMID 19330604.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Chen X, Wen W, Anstey KJ, Sachdev PS (2009). "Prevalence, incidence, and risk factors of lacunar infarcts in a community sample". Neurology. 73 (4): 266–72. doi:10.1212/WNL.0b013e3181aa52ea. PMID 19636046.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J (2005). "Global burden of hypertension: analysis of worldwide data". Lancet. 365 (9455): 217–23. doi:10.1016/S0140-6736(05)17741-1. PMID 15652604.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Kearney PM, Whelton M, Reynolds K, Whelton PK, He J (2004). "Worldwide prevalence of hypertension: a systematic review". J. Hypertens. 22 (1): 11–9. PMID 15106785.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Burt VL; Whelton P; Roccella EJ; et al. (1995). "Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988-1991". Hypertension. 25 (3): 305–13. PMID 7875754. Retrieved 2009-06-05.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ Burt VL; Cutler JA; Higgins M; et al. (1995). "Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991". Hypertension. 26 (1): 60–9. PMID 7607734. Retrieved 2009-06-05.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S (2007). "Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004". Journal of the American Geriatrics Society. 55 (7): 1056–65. doi:10.1111/j.1532-5415.2007.01215.x. PMID 17608879.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Falkner B (2009). "Hypertension in children and adolescents: epidemiology and natural history". Pediatr. Nephrol. 25 (7): 1219–24. doi:10.1007/s00467-009-1200-3. PMC 2874036. PMID 19421783.
{{cite journal}}: Unknown parameter|month=ignored (help) - GREGORY B. LUMA, M.D., and ROSEANN T. SPIOTTA, M.D., Jamaica Hospital Medical Center (2006). "Hypertension in Children and Adolescents". Hypertension in Children and Adolescents. American Academy of Family Physician. Retrieved 2007-07-24.
{{cite web}}: CS1 maint: multiple names: authors list (link) - Dwivedi, Girish & Dwivedi, Shridhar (2007). History of Medicine: Sushruta – the Clinician – Teacher par Excellence. National Informatics Centre (Government of India).
- ^ Esunge PM (1991). "From blood pressure to hypertension: the history of research". J R Soc Med. 84 (10): 621. PMC 1295564. PMID 1744849.
{{cite journal}}: Unknown parameter|month=ignored (help) - J.D. Swales., ed. (1995). Manual of hypertension. Oxford: Blackwell Science. pp. xiii. ISBN 0-86542-861-1.
- ^ Dustan HP, Roccella EJ, Garrison HH (1996). "Controlling hypertension. A research success story". Arch. Intern. Med. 156 (17): 1926–35. doi:10.1001/archinte.156.17.1926. PMID 8823146.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Novello FC, Sprague JM (1957). "Benzothiadiazine dioxides as novel diuretics". J Am Chem Soc. 79 (8): 2028. doi:10.1021/ja01565a079.
- Black JW, Crowther AF, Shanks RG, Smith LH, Dornhorst AC (1964). "A new adrenergic betareceptor antagonist". Lancet. 1 (7342): 1080–1. doi:10.1016/S0140-6736(64)91275-9. PMID 14132613.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Ondetti MA, Rubin B, Cushman DW (1977). "Design of specific inhibitors of angiotensin-converting enzyme: new class of orally active antihypertensive agents". Science. 196 (4288): 441–4. doi:10.1126/science.191908. PMID 191908.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "What is Hypertension? - WrongDiagnosis.com".
- Elliott, William J. (2003). "The Economic Impact of Hypertension". The Journal of Clinical Hypertension. 5 (3): 3–13. doi:10.1111/j.1524-6175.2003.02463.x. PMID 12826765.
- Alcocer L, Cueto L (2008). "Hypertension, a health economics perspective". Therapeutic Advances in Cardiovascular Disease. 2 (3): 147–55. doi:10.1177/1753944708090572. PMID 19124418. Retrieved 2009-06-20.
{{cite journal}}: Unknown parameter|month=ignored (help) - William J. Elliott (2003). "The Economic Impact of Hypertension". The Journal of Clinical Hypertension. 5 (4): 3–13. doi:10.1111/j.1524-6175.2003.02463.x. PMID 12826765.
{{cite journal}}: Unknown parameter|month=ignored (help) - Coca A (2008). "Economic benefits of treating high-risk hypertension with angiotensin II receptor antagonists (blockers)". Clinical Drug Investigation. 28 (4): 211–20. doi:10.2165/00044011-200828040-00002. PMID 18345711.
- Chockalingam A (2007). "Impact of World Hypertension Day". The Canadian Journal of Cardiology. 23 (7): 517–9. doi:10.1016/S0828-282X(07)70795-X. PMC 2650754. PMID 17534457.
{{cite journal}}: Unknown parameter|month=ignored (help) - Chockalingam A (2008). "World Hypertension Day and global awareness". The Canadian Journal of Cardiology. 24 (6): 441–4. doi:10.1016/S0828-282X(08)70617-2. PMC 2643187. PMID 18548140.
{{cite journal}}: Unknown parameter|month=ignored (help)
External links
- The Framingham Heart Study
- Video showing how to measure blood pressure
- Template:Dmoz
- High Blood Pressure from the Heart and Stroke Foundation of Canada
- A guide to lowering high blood pressure from the National Heart, Lung, and Blood Institute
- High Blood Pressure (from the American Heart Association)
- Pulmonary Hypertension from Cleveland Clinic Online Medical Reference
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure
| Cardiovascular disease (vessels) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Arteries, arterioles and capillaries | |||||||||
| Veins |
| ||||||||
| Arteries or veins | |||||||||
| Blood pressure |
| ||||||||