This is an old revision of this page, as edited by CheMoBot (talk | contribs) at 00:15, 12 November 2011 (Updating {{drugbox}} (no changed fields - added verified revid - updated 'ChemSpiderID_Ref', 'CAS_number_Ref') per Chem/Drugbox validation (report errors or bugs)). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 00:15, 12 November 2011 by CheMoBot (talk | contribs) (Updating {{drugbox}} (no changed fields - added verified revid - updated 'ChemSpiderID_Ref', 'CAS_number_Ref') per Chem/Drugbox validation (report errors or bugs))(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff) Pharmaceutical compound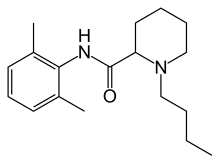 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration | parenteral, topical |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | n/a |
| Metabolism | hepatic |
| Elimination half-life | 3.5 hours (adults) 8.1 hours (neonates) |
| Excretion | Renal, 4–10% |
| Identifiers | |
IUPAC name
| |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.048.993 |
| Chemical and physical data | |
| Formula | C18H28N2O |
| Molar mass | 288.43 g/mol g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Bupivacaine (rINN) (/bjuːˈpɪvəkeɪn/) is a local anaesthetic drug belonging to the amino amide group. AstraZeneca commonly markets it under various trade names, including Marcain, Marcaine, Sensorcaine and Vivacaine.
Indications
Bupivacaine is indicated for local anaesthesia including infiltration, nerve block, epidural, and intrathecal anaesthesia. Bupivacaine often is administered by epidural injection before total hip arthroplasty. It also is commonly injected to surgical wound sites to reduce pain for up to 20 hours after the surgery. Sometimes, bupivacaine is co-administered with epinephrine to prolong the duration of its action, fentanyl for epidural analgesia, or glucose.
Contraindications
Bupivacaine is contraindicated for IV regional anaesthesia (IVRA) because of potential risk of tourniquet failure and systemic absorption of the drug.
Adverse effects
Compared to other local anaesthetic, bupivacaine is markedly cardiotoxic. However, adverse drug reactions (ADRs) are rare when it is administered correctly. Most ADRs relate to administration technique (resulting in systemic exposure) or pharmacological effects of anesthesia, however allergic reactions can rarely occur.
Systemic exposure to excessive quantities of bupivacaine mainly result in central nervous system (CNS) and cardiovascular effects – CNS effects usually occur at lower blood plasma concentrations and additional cardiovascular effects present at higher concentrations, though cardiovascular collapse may also occur with low concentrations. CNS effects may include CNS excitation (nervousness, tingling around the mouth, tinnitus, tremor, dizziness, blurred vision, seizures) followed by depression (drowsiness, loss of consciousness, respiratory depression and apnea). Cardiovascular effects include hypotension, bradycardia, arrhythmias, and/or cardiac arrest – some of which may be due to hypoxemia secondary to respiratory depression.
Bupivacaine has caused several deaths when the epidural anaesthetic has been administered intravenously accidentally.
Treatment of overdose: lipid rescue
Further information: ]There is animal evidence that Intralipid, a commonly available intravenous lipid emulsion, can be effective in treating severe cardiotoxicity secondary to local anaesthetic overdose, and human case reports of successful use in this way. Schemes to publicise this use more widely have been published.
Mechanism of action
Bupivacaine binds to the intracellular portion of sodium channels and blocks sodium influx into nerve cells, which prevents depolarization. Since pain transmitting nerve fibres tend to be thinner and either unmyelinated or lightly myelinated, the agent can diffuse more readily into them than into thicker and more heavily myelinated nerve fibres like touch, proprioception, etc. (Myelin is non-polar / lipophilic).It should be noted, however, that bupivacaine also blocks specific potassium channels, an effect contributing to resting membrane potential depolarization.
Developments
Levobupivacaine is the (S)-(–)-enantiomer of bupivacaine, with a longer duration of action and produces less vasodilation. Durect Corporation is developing a biodegradable controlled-release drug delivery system for post surgery. It is currently in Phase II.
References
- "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- ABS-CBN Interactive: Filipino nurse dies in UK due to wrong use of anaesthetic
- Weinberg, GL; VadeBoncouer, T; Ramaraju, GA; Garcia-Amaro, MF; Cwik, MJ. (1998). "Pretreatment or resuscitation with a lipid infusion shifts the dose-response to bupivacaine-induced asystole in rats". Anesthesiology. 88 (4): 1071–5. doi:10.1097/00000542-199804000-00028. PMID 9579517.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help) - Weinberg, G; Ripper, R; Feinstein, DL; Hoffman, W. (2003). "Lipid emulsion infusion rescues dogs from bupivacaine-induced cardiac toxicity". Regional Anesthesia and Pain Medicine. 28 (3): 198–202. doi:10.1053/rapm.2003.50041. PMID 12772136.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help) - Rosenblatt, MA; Abel, M; Fischer, GW; Itzkovich, CJ; Eisenkraft, JB (2006). "Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest". Anesthesiology. 105 (1): 217–8. doi:10.1097/00000542-200607000-00033. PMID 16810015.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Litz, RJ; Popp, M; Stehr, S N; Koch, T. (2006). "Successful resuscitation of a patient with ropivacaine-induced asystole after axillary plexus block using lipid infusion". Anaesthesia. 61 (8): 800–1. doi:10.1111/j.1365-2044.2006.04740.x. PMID 16867094.
- Picard, J; Meek, T (2006). "Lipid emulsion to treat overdose of local anaesthetic: the gift of the glob". Anaesthesia. 61 (2): 107–9. doi:10.1111/j.1365-2044.2005.04494.x. PMID 16430560.
{{cite journal}}: Cite has empty unknown parameter:|author-name-separator=(help); Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help)
External links
| Local anesthetics (primarily sodium channel blockers) (N01B) | |||||||
|---|---|---|---|---|---|---|---|
| Esters by acid |
| ||||||
| Amides | |||||||
| Combinations | |||||||
| |||||||