| B-cell lymphoma | |
|---|---|
 | |
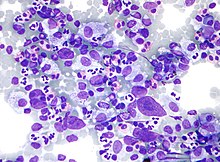
| Micrograph showing a large B cell lymphoma. Field stain. | |
| Specialty | Hematology, oncology |
The B-cell lymphomas are types of lymphoma affecting B cells. Lymphomas are "blood cancers" in the lymph nodes. They develop more frequently in older adults and in immunocompromised individuals.
B-cell lymphomas include both Hodgkin's lymphomas and most non-Hodgkin lymphomas. They are typically divided into low and high grade, typically corresponding to indolent (slow-growing) lymphomas and aggressive lymphomas, respectively. As a generalisation, indolent lymphomas respond to treatment and are kept under control (in remission) with long-term survival of many years, but are not cured. Aggressive lymphomas usually require intensive treatments, with some having a good prospect for a permanent cure.
Prognosis and treatment depends on the specific type of lymphoma as well as the stage and grade. Treatment includes radiation and chemotherapy. Early-stage indolent B-cell lymphomas can often be treated with radiation alone, with long-term non-recurrence. Early-stage aggressive disease is treated with chemotherapy and often radiation, with a 70–90% cure rate. Late-stage indolent lymphomas are sometimes left untreated and monitored until they progress. Late-stage aggressive disease is treated with chemotherapy, with cure rates of over 70%.
Types

There are numerous kinds of lymphomas involving B cells. The most commonly used classification system is the WHO classification, a convergence of more than one, older classification systems.
Common
Five account for nearly three out of four patients with non-Hodgkin lymphoma:
- Diffuse large B-cell lymphoma (DLBCL)
- Follicular lymphoma
- Marginal zone B-cell lymphoma (MZL) or mucosa-associated lymphatic tissue lymphoma (MALT)
- Small lymphocytic lymphoma (SLL, also known as chronic lymphocytic leukemia, CLL)
- Mantle cell lymphoma (MCL)
Rare
The remaining forms are much less common:
- DLBCL variants or sub-types of
- Primary mediastinal B-cell lymphoma
- T cell/histiocyte-rich large B-cell lymphoma
- Primary cutaneous diffuse large B-cell lymphoma, leg type (Primary cutaneous DLBCL, leg type)
- EBV positive diffuse large B-cell lymphoma of the elderly
- Diffuse large B-cell lymphoma associated with chronic inflammation
- Fibrin-associated diffuse large B-cell lymphoma
- Primary testicular diffuse large B-cell lymphoma
- Burkitt's lymphoma
- Lymphoplasmacytic lymphoma, which may manifest as Waldenström's macroglobulinemia
- Nodal marginal zone B cell lymphoma (NMZL)
- Splenic marginal zone lymphoma (SMZL)
- Intravascular lymphomas variants
- Primary effusion lymphoma
- Lymphomatoid granulomatosis
- Primary central nervous system lymphoma
- ALK+ large B-cell lymphoma
- Plasmablastic lymphoma
- Large B-cell lymphoma arising in HHV8-associated multicentric Castleman's disease
- B-cell lymphoma, unclassifiable with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma
- B-cell lymphoma, unclassifiable with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma
Other
Additionally, some researchers separate out lymphomas that appear to result from other immune system disorders, such as AIDS-related lymphoma.
Classic Hodgkin's lymphoma and nodular lymphocyte predominant Hodgkin's lymphoma are now considered forms of B-cell lymphoma.
Diagnosis
When a person appears to have a B-cell lymphoma, the main components of a workup (for determining the appropriate therapy and the person's prognosis) are:
- Establishing the precise subtype: Initially, an incisional or excisional biopsy is preferred. A core needle biopsy is discouraged except in case a lymph node is not easily accessible. Fine-needle aspiration is only acceptable in selected circumstances, in combination with immunohistochemistry and flow cytometry.
- Determining the extent of the disease (localized or advanced; nodal or extranodal)
- The person's general health status.
| Follicular lymphoma | Marginal zone B-cell lymphoma (MZL) or mucosa-associated lymphatic tissue (MALT) lymphoma | Small lymphocytic lymphoma (SLL) / chronic lymphocytic leukemia (CLL) | Mantle cell lymphoma (MCL) | |
|---|---|---|---|---|
| CD5 | - | - | + | + |
| CD10 | + | - | - | - |
| CD23 | - | - | + | - |
| Cyclin D1 | - | - | - | + |
Associated chromosomal translocations
Chromosomal translocations involving the immunoglobulin heavy locus is a classic cytogenetic abnormality for many B-cell lymphomas, including follicular lymphoma, mantle cell lymphoma and Burkitt's lymphoma. In these cases, the immunoglobulin heavy locus forms a fusion protein with another protein that has pro-proliferative or anti-apoptotic abilities. The enhancer element of the immunoglobulin heavy locus, which normally functions to make B cells produce massive production of antibodies, now induces massive transcription of the fusion protein, resulting in excessive pro-proliferative or anti-apoptotic effects on the B cells containing the fusion protein.
In Burkitt's lymphoma and mantle cell lymphoma, the other protein in the fusion is c-myc (on chromosome 8) and cyclin D1 (on chromosome 11), respectively, which gives the fusion protein pro-proliferative ability. In follicular lymphoma, the fused protein is Bcl-2 (on chromosome 18), which gives the fusion protein anti-apoptotic abilities.
See also
References
- ^ Merck Manual home edition, Non-Hodgkin Lymphomas
- Nguyen, Nghi; Khan, Mujahid; Shah, Muhammad (2017). "Primary B-cell lymphoma of the pelvic bone in a young patient: Imaging features of a rare case". Cancer Research Frontiers. 3 (1): 51–55. doi:10.17980/2017.51. ISSN 2328-5249.
- ^ "The Lymphomas" (PDF). The Leukemia & Lymphoma Society. May 2006. p. 12. Archived from the original (PDF) on 2008-07-06. Retrieved 2008-04-07.
- Mazen Sanoufa; Mohammad Sami Walid; Talat Parveen (2010). "B-Cell Lymphoma of the Thoracic Spine Presenting with Spinal Cord Pressure Syndrome". Journal of Clinical Medicine Research. 2 (1): 53–54. doi:10.4021/jocmr2010.02.258w. PMC 3299178. PMID 22457704.
- "HMDS: Hodgkin's Lymphoma". Archived from the original on 4 March 2009. Retrieved 2009-02-01.
- Mohammad Muhsin Chisti, Haresh Kumar, Sumeet K Yadav. "B-Cell Lymphoma Workup". Medscape.
{{cite web}}: CS1 maint: multiple names: authors list (link) Updated Jul 27, 2020 - Attanoos, Richard (2018). "Lymphoid Malignancies of the Pleura and Peritoneum". Practical Pathology of Serous Membranes. pp. 203–208. doi:10.1017/9781316402009.016. ISBN 9781316402009.
- Küppers, R; Dalla-Favera, R (10 September 2001). "Mechanisms of chromosomal translocations in B cell lymphomas" (PDF). Oncogene. 20 (40): 5580–94. doi:10.1038/sj.onc.1204640. PMID 11607811. S2CID 10776403.
- Li JY, Gaillard F, Moreau A, et al. (May 1999). "Detection of translocation t(11;14)(q13;q32) in mantle cell lymphoma by fluorescence in situ hybridization". Am. J. Pathol. 154 (5): 1449–52. doi:10.1016/S0002-9440(10)65399-0. PMC 1866594. PMID 10329598.
External links
| Classification | D |
|---|---|
| External resources |
| Leukaemias, lymphomas and related disease | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
| Cutaneous lymphoid hyperplasia | |||||||||||||||||||||||||||||||||||||||||||||
| General | |||||||||||||||||||||||||||||||||||||||||||||