This is an old revision of this page, as edited by CFCF (talk | contribs) at 15:32, 12 November 2013 (image from NIH). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 15:32, 12 November 2013 by CFCF (talk | contribs) (image from NIH)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff)Template:Infobox disease doubleimage Chronic obstructive pulmonary disease (COPD), also known as chronic obstructive lung disease (COLD), chronic obstructive airway disease (COAD), chronic airflow limitation (CAL), and chronic obstructive respiratory disease (CORD), is a lung disease defined by persistently poor airflow as a result of breakdown of lung tissue (known as emphysema) and dysfunction of the small airways. It typically worsens over time. Primary symptoms include: shortness of breath, cough, and sputum production.
COPD is most commonly caused by tobacco smoke, with a number of other factors playing a less common role. This triggers an inflammatory response in the lung. COPD is often defined based on low airflow on lung function tests. In contrast to asthma, this limitation is rarely reversible and usually gets worse over time.
Management involves quitting smoking, vaccinations, rehabilitation, and often inhaled bronchodilators. Some people may benefit from long-term oxygen therapy or lung transplantation.
Worldwide, COPD ranked as the fourth leading cause of death, killing over 3 million people in 2011. Mortality is expected to increase due to an increase in smoking rates and an aging population in many countries. COPD is the third leading cause of death in the U.S., and the economic burden of COPD in the U.S. in 2007 was $42.6 billion in health care costs and lost productivity.
Signs and symptoms

Problems playing this file? See media help.
The most common symptoms of COPD are sputum production, shortness of breath and a productive cough.
Cough
A chronic cough is usually the first symptom to occur. When it exists for more than three months a year for more than two years without another explanation, there is by definition chronic bronchitis. This condition can occur before COPD fully develops. The amount of sputum produced can change over hours to days. In some cases the cough may not be present or only occur occasionally and may not be productive. Some people with COPD write it off as simply a "smoker's cough". Sputum may be swallowed or spat out, depending often on social and cultural factors. Vigorous coughing may lead to rib fractures or a brief loss of consciousness. Those with COPD often have a history of "common colds" that last a long time.
Shortness of breath
Shortness of breath is often the symptom that bothers people the most. It is commonly described as: "my breathing requires effort," "I feel out of breath," or "I can't get enough air in". Different terms,however, may be used in different cultures. Typically the shortness of breath is of a prolonged duration, worsens over time, and is worse with exercise. In the advanced stages it occurs during rest and may be always present. It is a source of both anxiety and a poor quality of life in those with COPD.
Other
Those with obstructed airflow may have wheezing or decreased sounds of air entry with poor air entry typically representing a greater severity of disease. Crackles may also occur. It may also take longer to breathe out than breathing in. Chest tightness may occur but is not common and may represent another problem. A barrel chest, while a classific finding, is also not a frequent finding. In those with severe disease tiredness and weight loss become common.
Advanced COPD may lead to cor pulmonale, a strain on the heart due to the extra work required to pump blood through the lungs. It is also the most common cause of the condition. Symptoms that indicate the presence of cor pulmonale include swelling of the ankles. Finger nail clubbing is not specific to COPD and should prompt investigations for an underlying lung cancer. Many people with COPD breathe through pursed lips and this action can improve shortness of breath in some.
Exacerbation
An exacerbation is defined as increased shortness of breath, increased sputum production, a change in the color of the sputum from clear to green or yellow, or an increase in cough in someone with COPD. This may present with signs of increased work of breathing such as: fast breathing, a fast heart rate, sweating, active use of muscles in the neck, a bluish tinge to the skin, and confusion if in a severe exacerbation.
Co-existing conditions
COPD often occurs along with a number of other conditions due in part to common risk factors. These conditions include: ischemic heart disease, hypertension, diabetes mellitus, muscle wasting, osteoporosis, lung cancer, anxiety disorder and / or major depressive disorder.
Bronchial hyperresponsiveness, is a characteristic of asthma and refers to the increased sensitivity of the airways in response to an inhaled constrictor agonist. Many people with COPD also have this tendency. In COPD, the presence of bronchial hyperresponsiveness predicts a worse course of the disease.
Cause
The primary cause of COPD is tobacco smoke; with occupational exposures and pollution from indoor fires being a significant cause in some countries. Typically these exposures must occur over several decades before symptoms develop. Genetics also affects the risk.
Smoking
The primary risk factor for COPD globally is tobacco smoking. Other types of smoke are also a risk including: marijuana, cigar, second hand and water pipe smoke. In the United States, 80 to 90% of cases of COPD are due to smoking. Exposure to cigarette smoke is measured in pack-years, the average number of packages of cigarettes smoked daily multiplied by the number of years of smoking. The likelihood of developing COPD increases with age and cumulative smoke exposure, and almost all lifelong smokers will develop COPD, provided that smoking-related, extrapulmonary diseases (cardiovascular, diabetes, cancer) do not claim their lives beforehand.
Air pollution
In many developing countries, indoor air pollution from cooking fire smoke (often using biomass fuels such as wood and animal dung) is a common cause of COPD, especially in women. This is a common method of cooking and heating for nearly three billion people globally.
People who live in large cities have a higher rate of COPD compared to people who live in rural areas. While urban air pollution may be a contributing factor to exacerbations, its likely overall role in causing COPD is believed to be small.
Occupational exposures
Intense and prolonged exposure to workplace dusts found in coal mining, gold mining, and the cotton textile industry and chemicals such as cadmium, isocyanates, and fumes from welding have been implicated in the development of airflow obstruction, even in nonsmokers. Workers who smoke and are exposed to these particles and gases are even more likely to develop COPD. Intense silica dust exposure causes silicosis, a restrictive lung disease distinct from COPD; however, less intense silica dust exposures have been linked to a COPD-like condition. The effect of occupational pollutants on the lungs appears substantially less important than the effect of cigarette smoking. In the United States it is the cause of about 20% of cases overall and 30% of those in never-smokers. The rates are believed to be higher in the developing world.
Genetics
Genetics play a role in the development of COPD. It is more common among relatives of those with COPD who smoke than unrelated smokers.
An inherited genetic condition, alpha 1-antitrypsin deficiency is responsible for about 2% of cases.
Other
A number of other factors are less well linked to COPD. The risk is greater in those who are poor however it is not clear if this is due to poverty itself or other factors associated with poverty such as air pollution and nutrition. There is tentative evidence that those with asthma and airway hyperreactivity are at increased risk. Birth factors such as low birth weight may also play a role as do a number of infectious diseases including HIV/AIDS and tuberculosis.
Acute exacerbations
An acute exacerbation of COPD is a sudden worsening of symptoms (shortness of breath, quantity and color of phlegm). It may be triggered by an infection or by environmental pollutants. Typically, infections cause 75% or more of the exacerbations; bacteria in 25% of cases, viruses in 25%, and both in 25%. Airway inflammation is increased during the exacerbation, resulting in increased hyperinflation, reduced expiratory air flow and worsening of gas transfer. This can also lead to hypoventilation and eventually hypoxia, insufficient tissue perfusion, and then cell necrosis. Pulmonary emboli can also worsen symptoms in those with COPD.
Pathophysiology

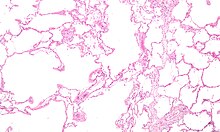
COPD is a type of obstructive lung disease in which a chronic incompletely reversible airflow limit exists. This airflow limitation is due to breakdown of lung tissue (known as emphysema) and small airway disease known as obstructive bronchiolitis. The amount of these two factors vary between people. It develops in response to a more pronounced and chronic inflammatory response to inhaled irritants. Cigarette smoke stimulates polymorphonuclear leukocytes (PHN) to release serene elastase and inactivated elastase inhibitor alpha-antitrypsine. This lets serene elastase destroy elastic tissue of lungs and produce emphysema.
Other processes causing lung damage are:
- Oxidative stress produced by the high concentrations of free radicals in tobacco smoke
- Cytokine release due to inflammation as the body responds to irritant particles such as tobacco smoke in the airway
- Tobacco smoke and free radicals impair the activity of antiprotease enzymes such as alpha 1-antitrypsin, allowing protease enzymes to damage the lung
Narrowing of the airways reduces the airflow rate to and from the air sacs (alveoli) and limits effectiveness of the lungs. In COPD, the greatest reduction in air flow occurs when breathing out (during expiration) because the pressure in the chest tends to compress rather than expand the airways. In theory, air flow could be increased by breathing more forcefully, increasing the pressure in the chest during expiration. In COPD, there is often a limit to how much this can actually increase air flow, a situation known as expiratory flow limitation.
If the rate of airflow is too low, a person with COPD may not be able to completely finish breathing out (expiration) before he or she needs to take another breath. This is particularly common during exercise, when breathing must be faster. A little of the air of the previous breath remains within the lungs when the next breath is started, resulting in an increase in the volume of air in the lungs, a process called dynamic hyperinflation.
Dynamic hyperinflation is closely linked to shortness of breath in COPD. It is less comfortable to breathe with hyperinflation because it takes more effort to move the lungs and chest wall when they are already stretched by hyperinflation.
Another factor contributing to shortness of breath in COPD is the loss of the surface area available for the exchange of oxygen and carbon dioxide with emphysema. This reduces the rate of transfer of these gases between the body and the atmosphere and can lead to low oxygen and high carbon dioxide levels in the body. A person with emphysema may have to breathe faster or more deeply to compensate, which can be difficult to do if there is also flow limitation or hyperinflation.
Some people with advanced COPD do manage to breathe fast to compensate, but usually have shortness of breath as a result. Others, who may be less short of breath, tolerate low oxygen and high carbon dioxide levels in their bodies, but this can eventually lead to headaches, drowsiness and heart failure.
Advanced COPD can lead to complications beyond the lungs, such as weight loss (cachexia), pulmonary hypertension and right-sided heart failure (cor pulmonale). Osteoporosis, heart disease, muscle wasting and depression are all more common in people with COPD.
Diagnosis
The diagnosis of COPD should be considered in anyone over the age of 35 to 40 who has shortness of breath, a chronic cough, sputum production, or frequent winter colds and a history of exposure to risk factors for the disease. Spirometry is then used to confirm the diagnosis; with an FEV1/FVC ratio of less than 0.7 following the use of a bronchodilator being diagnostic.
Spirometry
| Severity | FEV1 % predicted |
|---|---|
| Mild (GOLD 1) | ≥80 |
| Moderate (GOLD 2) | 50–79 |
| Severe (GOLD 3) | 30–49 |
| Very severe (GOLD 4) | <30 or chronic respiratory failure |
Spirometry measures the forced expiratory volume in one second (FEV1), which is the greatest volume of air that can be breathed out in the first second of a breath. Spirometry also measures the forced vital capacity (FVC), which is the greatest volume of air that can be breathed out in a whole large breath. Normally, at least 70% of the FVC comes out in the first second, giving a FEV1/FVC ratio of greater than 70%. A ratio of less than this defines a person as having COPD per the GOLD criteria. The NICE criteria additionally require a FEV1 of less than 80% of predicted.
According to the ERS criteria, it is FEV1% predicted that defines when a person has COPD, that is, when FEV1% predicted is < 88% for men, or < 89% for women. Evidence for using spirometry among those without symptoms in an effort to diagnose the condition earlier is of uncertain effect and therefore as of 2013 not recommended. A peak expiratory flow is not sufficient for the diagnosis.
Other tests

A chest x-ray and complete blood count may be useful to exclude other conditions at the time of diagnosis. The classic signs of COPD on chest X-ray are over expanded lung, a flattened diaphragm, increased retrosternal airspace, and bulla while it can help exclude other lung diseases, such as pneumonia, pulmonary edema or a pneumothorax. Complete pulmonary function tests with measurements of lung volumes and gas transfer may also show hyperinflation and can discriminate between COPD with emphysema and COPD without emphysema. A high-resolution computed tomography scan of the chest may show the distribution of emphysema throughout the lungs and can also be useful to exclude other lung diseases.
An analysis of arterial blood is used to determine the need for oxygen. Testing is recommended in those with an FEV1 less than 35%, those with a peripheral oxygen saturation of less than 92% and those with congestive heart failure. In areas of the world were alpha-1 antitrypsin deficiency is common, people with COPD should be tested for it.
-
 Axial CT image of the lung of a person with end-stage bullus emphysema.
Axial CT image of the lung of a person with end-stage bullus emphysema.
-
A lateral chest x-ray of a person with emphysema. Note the barrel chest and flat diaphragm.
-
Lung bulla as seen on CXR in a person with severe COPD
-
 A severe case of bullous emphysema
A severe case of bullous emphysema
Severity
| Grade | Activity affected |
|---|---|
| 1 | Only strenuous activity |
| 2 | Vigorous walking |
| 3 | With normal walking |
| 4 | After a few minutes of walking |
| 5 | With changing clothing |
Spirometry can help to determine the severity of COPD. The FEV1 (measured after bronchodilator medication) is expressed as a percentage of a predicted "normal" value based on a person's age, gender, height and weight.
There are a number of methods to determine how much COPD is affecting a given individual. This depends partly on the severity of shortness of breath and exercise limitation. These and other factors can be combined with spirometry results to obtain a COPD severity score.
COPD Assessment Test (CAT) is a patient-completed questionnaire that assesses the impact of COPD (cough, sputum, dysnea, chest tighteness) on health status. The range of CAT scores is from 0–40. Higher the score, more the severity of the disease. The GOLD guidelines suggest dividing people into four categories based on current symptoms (assessed using the modified medical research council questionnaire or the CAT Score).
Types
It is unclear if different types of COPD exist. While previously divided into emphysema and chronic bronchitis; emphysema is only a description of pathological lung changes rather than a disease in itself and is simply a descriptor of symptoms that may or may not occur with COPD.
Emphysema is an enlargement of the air spaces distal to the terminal bronchioles, with destruction of their walls. People with emphysema have historically been known as "Pink Puffers", due to their pink complexion.
Chronic bronchitis is defined in clinical terms as a cough with sputum production on most days for 3 months of a year, for 2 consecutive years. People with advanced COPD that have primarily chronic bronchitis were commonly referred to as "Blue Bloaters" because of the bluish color of the skin and lips (cyanosis) along with hypoxia and fluid retention.
Differential diagnosis
COPD may need to be differentiated from congestive heart failure which often has jugular venous distension or pedal edema. If only one leg is swollen a deep vein thrombosis or pulmonary embolism should be considered. In those with poor air entry on one side versus both sides, pneumonia or pneumothorax may be the cause of shortness of breath. Many people with COPD mistakenly think they have asthma. The distinction between asthma and COPD however cannot be made via spirometry. Tuberculosis may also present with a chronic cough and should be considered in locations where it is common. Less common conditions which may present similarly include: bronchopulmonary dysplasia and obliterative bronchiolitis.
Prevention
Annual influenza vaccinations and pneumococcal vaccinations may be beneficial.
Smoking cessation
Preventing people from starting smoking is a key aspect of prevention of COPD. The policies of governments, public health agencies and antismoking organizations can reduce smoking rates by encouraging stopping smoking and discouraging people from starting. These policies are important strategies in the prevention of COPD.
In those who smoke, smoking cessation is one of the most important factors in slowing down the progression of COPD. Once COPD has been diagnosed, stopping smoking slows down the rate of progression of the disease and is the only measure that has been shown to do so. Even at a late stage of the disease, it can reduce the rate of deterioration in lung function and delay the onset of disability and death.
Smoking cessation starts with the decision to stop smoking, leading to an attempt at quitting. Often several attempts are required before long-term smoking cessation is achieved. Attempts over 5 years lead to success in nearly 40% of people.
Some smokers can achieve long-term smoking cessation through willpower alone. However, smoking is highly addictive, and many smokers need further support to quit. The chance of stopping smoking is improved through social support, engagement in a smoking cessation program and the use of medications such as nicotine replacement therapy, bupropion or varenicline.
Occupational health
Measures can be taken to reduce the likelihood that workers in at-risk industries—such as coal mining, construction and stonemasonry—will develop COPD. Examples of these measures include: education of workers and management about the risks, promoting smoking cessation, surveillance of workers for early signs of COPD, use of personal dust monitors, use of respirators, and dust control. Dust control can be achieved by improving ventilation, using water sprays and by using mining techniques that minimize dust generation. If a worker develops COPD, further lung damage can be reduced by avoiding ongoing dust exposure, for example by changing the work role.
Air pollution
Air quality can be improved by pollution reduction efforts, which should lead to health gains for people with COPD. A person who has COPD may experience fewer symptoms if they stay indoors on days when air quality is poor.
Management
There is no known cure for COPD; however, it is both preventable and treatable. The major goals of management are to reduce risk factors, manage stable COPD, prevent and treat acute exacerbations and manage associated illnesses. The only measures that have been shown to reduce mortality is smoking cessation and supplemental oxygen. Stopping smoking decreases the risk of death by 18%. Other recommendations include: influenza vaccination once a year, pneumococcal vaccinations once every 5 years, and reduction in exposure to environmental air pollution. Palliative care at the end of life may be useful, with morphine improving the feelings of shortness of breath. Additionally noninvasive ventilation may provide comfort.
Exercise
Pulmonary rehabilitation is a program of exercise, disease management and counselling coordinated to benefit the individual. Pulmonary rehabilitation appears to improve over all quality of life, the ability to exercise, and mortality in those who have had a recent exacerbation. It has also been shown to improve the sense of control a patient has over their disease as well as their emotions. Breathing exercises in and of themselves appear to have a limited role.
Being either underweight or overweight can affect the symptoms, degree of disability and prognosis of COPD. People with COPD who are underweight can improve their breathing muscle strength by increasing their calorie intake. When combined with regular exercise or a pulmonary rehabilitation programme, this can lead to improvements in COPD symptoms. Supplemental nutrition may be useful in those who are malnourished.
Bronchodilators
Inhaled bronchodilators are the primary medications used and result in a small overall benefit. There are two major types, β2 agonists and anticholinergics and they exist in long-acting and short-acting forms. They reduce shortness of breath, wheeze and exercise limitation, resulting in an improved quality of life. It is unclear if they change the progression of the underlying disease.
In those with mild disease short acting agents on an as needed basis are recommended. In those with more severe disease long acting agents and if not sufficient inhaled corticosteroids are recommended. With respect to long acting agents; it is unclear if tiotropium or long acting beta agonists (LABAs) are better and it may be worth trying each and continuing the one that worked best. Both types of agent reduce the risk of acute worsenings by 15-25%. While using both at the same time may offer a benefit, this benefit if any is of questionable significance.
There are several β2 agonists available including salbutamol (Ventolin) and terbutaline. They provide rapid relief of symptoms. Long acting β2 agonists such as salmeterol and formoterol are used as maintenance therapy and lead to improved airflow, exercise capacity, and quality of life. Long term use appears safe in COPD. Adverse effects include: shakiness and heart palpitations. When used with steroids they increase the risk of pneumonia.
There are two main anticholinergics used in COPD, ipratropium and tiotropium. Ipratropium is a short-acting agent while tiotropium is long-acting. Tiotropium is associated with a decrease in exacerbations and improved quality of life, and tiotropium provides those benefits better than ipratropium. While overall the two formulations of tiotroprium do not appear to affect mortality, the dry powder form may decrease and the mist form may increase mortality. Anticholinergics can cause dry mouth and urinary tract symptoms. They are also associated with increased risk of heart disease and stroke.
Corticosteroids
Corticosteroids are usually used in inhaled form but may also be used as tablets to treat and prevent acute exacerbations. While inhaled corticosteroids (ICS) have not shown benefit for people with mild COPD, they decrease acute exacerbations in those with either moderate or severe disease. When used in combination with a LABA they decrease mortality more than either ICS or LABA alone. By themselves they have no effect on overall one-year mortality and are associated with increased rates of pneumonia. It is unclear if they affect the progression of the disease.
Other medication
Long term antibiotics specifically macrolides such as azithromycin reduce the frequency of exacerbations in those who have two or more a year. Methylxanthines such as theophylline generally causes more harm than benefit and thus are usually not recommended. It may be used as a second line agent in those not controlled by other measures.
Oxygen
Supplemental oxygen in those with low oxygen levels (a partial pressure of oxygen of less than 50 mmHg) decreases the risk of heart failure and death if used 15 hours per day. It may also improve peoples ability to exercise. In those with normal or mildly low oxygen levels, oxygen supplementation may improve shortness of breath. High concentrations of oxygen can lead to increased levels of carbon dioxide in some people with severe COPD. Smoking while on oxygen is a safety risk.
Surgery
For those with very severe disease surgery is sometimes helpful and may include lung transplantation or lung volume reduction surgery. Lung volume reduction surgery involves removing the parts of the lung most damaged by emphysema allowing the remaining, relatively good lung to expand and work better. Lung transplantation is sometimes performed for severe COPD, particularly in younger individuals.
Acute exacerbation
Acute exacerbations are typically treated by increases the usage of short acting bronchodilators. If this is not sufficient then oral corticosteroids may be useful. In those with a severe exacerbation antibiotics improve outcomes. There is no clear evidence for those with less severe cases. Non-invasive positive pressure ventilation in those with high CO2 levels decreases the probability of death or needing intubation. Additionally theophylline may have a role in those who do not respond to other measures.
Prognosis
COPD usually gets gradually worse over time and can ultimately result in death. It is estimated that 3% of all disability is related to COPD. The proportion of disability from COPD globally has decreased from 1990 to 2010 due to improved indoor air quality primarily in Asia. The overall number of years lived with disability from COPD; however, has increased. Results of spirometry is a good predictor of the future progress of the disease.
The rate at which it gets worse varies with factors that predict a poor prognosis including: severe airflow obstruction, little ability to exercise, shortness of breath, significantly underweight or overweight, congestive heart failure, continued smoking, and frequent acute exacerbations. Prognosis in COPD can be estimated using the Bode index. This scoring system uses FEV1, body-mass index, 6-minute walk distance, and the modified MRC dyspnea scale to estimate outcomes in COPD.
Epidemiology

Globally as of 2010, COPD affected approximately 329 million people (4.8% of the population) and is slightly more common in men than women. This is as compared to 64 million being affected in 2004. This number is expected to continue increasing as risk factors remain common and the population is getting older. The number of deaths from COPD has decreased slightly from 3.1 million to 2.9 million from 1990 to 2010. Overall it is the 4th leading cause of death. In some countries while mortality has decreased in males it has increased in female.
Rates are higher in older people with it occurs in 34-200 out of 1000 older than 65 years depending on the population looked at. In the developing world the rates of COPD have increased significantly between the 1970s and the 2000s due in part to increasing rates of cigarette smoking in these regions of the world. In the developed world some countries have seen increased rates, some have remained stable and some have seen a lessening of COPD.
In England, an estimated 0.84 of 50 million people have a diagnosis of COPD; translating into approximately one person in 59 receiving a diagnosis of COPD at some point in their lives. In the most socioeconomically deprived parts of the country, one in 32 people were diagnosed with COPD, compared with one in 98 in the most affluent areas. In the United States approximately 6.3% of the adult population, totaling approximately 15 million people, have been diagnosed with COPD. Possibly 25 million people have COPD if undiagnosed cases are included. There were approximately 729,000 inpatient stays at U.S. hospitals for COPD in 2011.
History
The term "emphysema" is derived from the Greek ἐμφυσᾶν emphysan meaning "inflate" -itself composed of ἐν en, meaning "in", and φυσᾶν physan, meaning "breath, blast".
COPD has probably always existed but has been called by different names in the past. Bonet, in 1679, described a condition of "voluminous lungs". Giovanni Morgagni, in 1769, described 19 cases where the lungs were "turgid" particularly from air. The first description and illustration of the enlarged airspaces in emphysema was provided by Ruysh in 1721. Matthew Baillie illustrated an emphysematous lung in 1789 and described the destructive character of the condition. Badham used the word "catarrh" to describe the cough and mucus hypersecretion of chronic bronchitis in 1814. He recognised that chronic bronchitis was a disabling disorder.
René Laennec, the physician who invented the stethoscope, used the term "emphysema" in his book A Treatise on the Diseases of the Chest and of Mediate Auscultation (1837) to describe lungs that did not collapse when he opened the chest during an autopsy. He noted that they did not collapse as usual because they were full of air and the airways were filled with mucus.
In 1842, John Hutchinson invented the spirometer, which allowed the measurement of vital capacity of the lungs. However, his spirometer could only measure volume, not airflow. Tiffeneau in 1947 and Gaensler in 1950 and 1951 described the principles of measuring airflow.
The terms chronic bronchitis and emphysema were formally defined at the CIBA guest symposium of physicians in 1959. The term COPD was first used by William Briscoe in 1965 and has gradually overtaken other terms to become established today as the preferred name for this disease.
Society and culture
See also: COPD Awareness MonthIt is a challenge for many health systems to ensure appropriate identification, diagnosis and care for people with COPD; Britain's Department of Health has identified this as a major issue for the National Health Service and has introduced a specific strategy for COPD to tackle these problems.
Economics
In Europe, COPD represents 3% of health care spending. In the United States, costs of the disease are estimated at $50 billion, most of which is due to exacerbation. COPD was among the most expensive conditions seen in U.S. hospitals in 2011, with an aggregated cost of about $5.7 billion.
Research
Infliximab has been tested in COPD but there was no evidence of benefit with the possibility of harm. Roflumilast shows promise in decreasing the rate of exacerbations but does not appear to change quality of life. A number of new long acting agents are under development.
Other animals
Chronic obstructive pulmonary disease in horses also known as recurrent airway obstruction is an inflammatory disease of the airways due to an allergic reaction to straw containing fungus.
References
- ^ Vestbo, Jorgen (2013). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (PDF). Global Initiative for Chronic Obstructive Lung Disease. p. Chapter 1.
- ^ Decramer M, Janssens W, Miravitlles M (2012). "Chronic obstructive pulmonary disease". Lancet. 379 (9823): 1341–51. doi:10.1016/S0140-6736(11)60968-9. PMID 22314182.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Rabe KF; Hurd S; Anzueto A; et al. (2007). "Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: GOLD Executive Summary". Am. J. Respir. Crit. Care Med. 176 (6): 532–55. doi:10.1164/rccm.200703-456SO. PMID 17507545.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1186/1465-9921-8-89, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1186/1465-9921-8-89instead. - "The 10 leading causes of death in the world, 2000 and 2011". World Health Organization. July 2013. Fact sheet No 310.
- Mathers CD, Loncar D (2006). "Projections of Global Mortality and Burden of Disease from 2002 to 2030". PLoS Med. 3 (11): e442. doi:10.1371/journal.pmed.0030442. PMC 1664601. PMID 17132052.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - "COPD (Chronic Obstructive Pulmonary Disease)". Educational Campaigns. National Heart, Lung, and Blood Institute, U.S. Department of Health & Human Services. 2012-02-15. Retrieved 2013-07-23.
"2007 NHLBI Morbidity and Mortality Chart Book" (PDF). Retrieved 2008-06-06. - ^ Vestbo, Jorgen (2013). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (PDF). Global Initiative for Chronic Obstructive Lung Disease. p. Chapter 2.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 101: Chronic Obstructive Pulmonary Disease. London, June 2010.
- Mahler DA (2006). "Mechanisms and measurement of dyspnea in chronic obstructive pulmonary disease". Proceedings of the American Thoracic Society. 3 (3): 234–8. doi:10.1513/pats.200509-103SF. PMID 16636091.
- "What Are the Signs and Symptoms of COPD?". U.S. National Heart Lung and Blood Institute. 8 June 2012.
- ^ MedlinePlus Encyclopedia: Chronic obstructive pulmonary disease
- ^ Gruber, Phillip (2008). "The Acute Presentation of Chronic Obstructive Pulmonary Disease In the Emergency Department: A Challenging Oxymoron". Emergency Medicine Practice. 10 (11).
{{cite journal}}: Unknown parameter|month=ignored (help) - Carol, T. Fundamentals of nursing: The art and science of nursing care. ISBN 9780781793834
- ^ Weitzenblum, E (2009). "Cor pulmonale". Chronic respiratory disease. 6 (3): 177–85. doi:10.1177/1479972309104664. PMID 19643833.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Mandell, editors, James K. Stoller, Franklin A. Michota, Jr., Brian F. (2009). The Cleveland Clinic Foundation intensive review of internal medicine (5th ed. ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 419. ISBN 9780781790796.
{{cite book}}:|edition=has extra text (help);|first=has generic name (help)CS1 maint: multiple names: authors list (link) - Morrison, Nathan E. Goldstein, R. Sean. Evidence-based practice of palliative medicine. Philadelphia: Elsevier/Saunders. p. 124. ISBN 9781437737967.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ Holland, AE (2012 October 17). Holland, Anne E (ed.). "Breathing exercises for chronic obstructive pulmonary disease". The Cochrane database of systematic reviews. 10: CD008250. doi:10.1002/14651858.CD008250.pub2. PMID 23076942.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Loscalzo, Joseph; Fauci, Anthony S.; Braunwald, Eugene; Dennis L. Kasper; Hauser, Stephen L; Longo, Dan L. (2008). Harrison's Principles of Internal Medicine (17th ed.). McGraw-Hill Professional. ISBN 0-07-146633-9.
{{cite book}}: CS1 maint: multiple names: authors list (link) - "— COPD causes". Medicinenet.com. 2013-05-13. Retrieved 2013-07-23.
- Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD (2009). "COPD prevalence is increased in lung cancer, independent of age, sex and smoking history". Eur. Respir. J. 34 (2): 380–6. doi:10.1183/09031936.00144208. PMID 19196816.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Definition of pack year". NCI Dictionary of Cancer Terms.
- Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1016/S0140-6736(06)68516-4, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1016/S0140-6736(06)68516-4instead. - Kennedy SM, Chambers R, Du W, Dimich-Ward H (2007). "Environmental and occupational exposures: do they affect chronic obstructive pulmonary disease differently in women and men?". Proceedings of the American Thoracic Society. 4 (8): 692–4. doi:10.1513/pats.200707-094SD. PMID 18073405.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM (2006). "Global burden of COPD: systematic review and meta-analysis". Eur. Respir. J. 28 (3): 523–32. doi:10.1183/09031936.06.00124605. PMID 16611654.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Devereux, G (2006 May 13). "ABC of chronic obstructive pulmonary disease. Definition, epidemiology, and risk factors". BMJ (Clinical research ed.). 332 (7550): 1142–4. doi:10.1136/bmj.332.7550.1142. PMC 1459603. PMID 16690673.
{{cite journal}}: Check date values in:|date=(help) - Hnizdo E, Vallyathan V (2003). "Chronic obstructive pulmonary disease due to occupational exposure to silica dust: a review of epidemiological and pathological evidence". Occup Environ Med. 60 (4): 237–43. doi:10.1136/oem.60.4.237. PMC 1740506. PMID 12660371.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Calverley PM, Koulouris NG (2005). "Flow limitation and dynamic hyperinflation: key concepts in modern respiratory physiology". Eur Respir J. 25 (1): 186–199. doi:10.1183/09031936.04.00113204. PMID 15640341.
- O'Donnell DE (2006). "Hyperinflation, Dyspnea, and Exercise Intolerance in Chronic Obstructive Pulmonary Disease". The Proceedings of the American Thoracic Society. 3 (2): 180–4. doi:10.1513/pats.200508-093DO. PMID 16565429.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 101: Chronic Obstructive Pulmonary Disease. London, June 2010.
- ^ Torres M, Moayedi S (2007). "Evaluation of the acutely dyspneic elderly patient". Clin. Geriatr. Med. 23 (2): 307–25, vi. doi:10.1016/j.cger.2007.01.007. PMID 17462519.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Celli BR; Cote CG; Marin JM; et al. (2004). "The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease". N. Engl. J. Med. 350 (10): 1005–12. doi:10.1056/NEJMoa021322. PMID 14999112.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - "COPD Assessment Test (CAT) Questionnaire" (PDF). Retrieved 2013-07-23.
- ^ "COPD Assessment Test (CAT)". American Thoracic Society (ATS). Retrieved 15 June 2013.
- "The Global Initiative for Chronic Obstructive Lung Disease (GOLD)". Retrieved 15 June 2013.
- ^ Longmore, J. M.; Murray Longmore; Wilkinson, Ian; Supraj R. Rajagopalan (2004). Oxford handbook of clinical medicine. Oxford : Oxford University Press. pp. 188–9. ISBN 0-19-852558-3.
{{cite book}}: CS1 maint: multiple names: authors list (link) - "Pink Puffer - definition of Pink Puffer in the Medical dictionary - by the Free Online Medical Dictionary, Thesaurus and Encyclopedia". Medical-dictionary.thefreedictionary.com. Retrieved 2013-07-23.
- Chung C, Delaney J, Hodgins R (2008). "Respirology". In Somogyi, Ron; Colman, Rebecca (ed.). The Toronto notes 2008: a comprehensive medical reference and review for the Medical Council of Canada Qualifying Exam — Part 1 and the United States Medical Licensing Exam — Step 2. Toronto: Toronto Notes for Medical Students. p. R9. ISBN 0-9685928-8-0.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Vestbo, Jorgen (2013). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (PDF). Global Initiative for Chronic Obstructive Lung Disease. p. xiii-xv.
- ^ "World Health Organization Tobacco Free Initiative — Policy recommendations for smoking cessation and treatment of tobacco dependence". Retrieved 28 July 2008.
- ^ Drummond MB, Dasenbrook EC, Pitz MW, Murphy DJ, Fan E (2008). "Inhaled corticosteroids in patients with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis". JAMA. 300 (20): 2407–16. doi:10.1001/jama.2008.717. PMID 19033591.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Kumar P, Clark M (2005). Clinical Medicine (6th ed.). Elsevier Saunders. pp. 900–1. ISBN 0-7020-2763-4.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 23457163, please use {{cite journal}} with
|pmid=23457163instead. - "Why is smoking addictive?". NHS Choices.
- Kissell, Fred N. (June 2003). "Handbook for Dust Control in Mining" (PDF). U.S. Department of Health and Human Services. Information Circular 9465.
- Wet cutting Health and Safety Executive (UK Government). Accessed March 20, 2012.
- ^ Carlucci A, Guerrieri A, Nava S (2012). "Palliative care in COPD patients: is it only an end-of-life issue?". Eur Respir Rev. 21 (126): 347–54. doi:10.1183/09059180.00001512. PMID 23204123.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "COPD — Treatment". U.S. National Heart Lung and Blood Institute. Retrieved 2013-07-23.
- Puhan MA, Gimeno-Santos E, Scharplatz M, Troosters T, Walters EH, Steurer J (2011). Puhan, Milo A (ed.). "Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev (10): CD005305. doi:10.1002/14651858.CD005305.pub3. PMID 21975749.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lacasse Y; Brosseau L; Milne S; et al. (2002). Lacasse, Yves (ed.). "Pulmonary rehabilitation for chronic obstructive pulmonary disease". Cochrane database of systematic reviews (Online) (3): CD003793. doi:10.1002/14651858.CD003793. PMID 12137716.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - Ferreira IM, Brooks D, White J, Goldstein R (2012). Ferreira, Ivone M (ed.). "Nutritional supplementation for stable chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 12: CD000998. doi:10.1002/14651858.CD000998.pub3. PMID 23235577.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - van Dijk, WD (2013 Mar-Apr). "Megatrials for bronchodilators in chronic obstructive pulmonary disease (COPD) treatment: time to reflect". Journal of the American Board of Family Medicine : JABFM. 26 (2): 221–4. doi:10.3122/jabfm.2013.02.110342. PMID 23471939.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Liesker JJ, Wijkstra PJ, Ten Hacken NH, Koëter GH, Postma DS, Kerstjens HA (2002). "A systematic review of the effects of bronchodilators on exercise capacity in patients with COPD". Chest. 121 (2): 597–608. doi:10.1378/chest.121.2.597. PMID 11834677.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Chong, J (2012 Sep 12). Chong, Jimmy (ed.). "Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease". Cochrane database of systematic reviews (Online). 9: CD009157. doi:10.1002/14651858.CD009157.pub2. PMID 22972134.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Karner, C (2012 Apr 18). Karner, Charlotta (ed.). "Long-acting beta(2)-agonist in addition to tiotropium versus either tiotropium or long-acting beta(2)-agonist alone for chronic obstructive pulmonary disease". The Cochrane database of systematic reviews. 4: CD008989. doi:10.1002/14651858.CD008989.pub2. PMID 22513969.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Calverley PM; Anderson JA; Celli B; et al. (2007). "Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease". N. Engl. J. Med. 356 (8): 775–89. doi:10.1056/NEJMoa063070. PMID 17314337.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - Decramer, ML (2013). "The safety of long-acting β2-agonists in the treatment of stable chronic obstructive pulmonary disease". International journal of chronic obstructive pulmonary disease. 8: 53–64. doi:10.2147/COPD.S39018. PMID 23378756.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Karner, C (2012 Jul 11). Karner, Charlotta (ed.). "Tiotropium versus placebo for chronic obstructive pulmonary disease". Cochrane database of systematic reviews (Online). 7: CD009285. doi:10.1002/14651858.CD009285.pub2. PMID 22786525.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Cheyne L, Irvin-Sellers MJ, White J (2013 Sep 16). Cheyne, Leanne (ed.). "Tiotropium versus ipratropium bromide for chronic obstructive pulmonary disease". Cochrane Database of Systematic Reviews (9): CD009552. doi:10.1002/14651858.CD009552.pub2.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: multiple names: authors list (link) - Singh, S (2008 Sep 24). "Inhaled anticholinergics and risk of major adverse cardiovascular events in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis". JAMA: the Journal of the American Medical Association. 300 (12): 1439–50. doi:10.1001/jama.300.12.1439. PMID 18812535.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Singh, S (2013 Jan). "Pro-arrhythmic and pro-ischaemic effects of inhaled anticholinergic medications". Thorax. 68 (1): 114–6. doi:10.1136/thoraxjnl-2011-201275. PMID 22764216.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Gartlehner G, Hansen RA, Carson SS, Lohr KN (2006). "Efficacy and Safety of Inhaled Corticosteroids in Patients With COPD: A Systematic Review and Meta-Analysis of Health Outcomes". Ann Fam Med. 4 (3): 253–62. doi:10.1370/afm.517. PMC 1479432. PMID 16735528.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Shafazand, S (2013 Jun 18). "Review: Inhaled medications vary substantively in their effects on mortality in COPD". Annals of internal medicine. 158 (12): JC2. doi:10.7326/0003-4819-158-12-201306180-02002. PMID 23778926.
{{cite journal}}: Check date values in:|date=(help) - Mammen, MJ (2012). "Macrolide therapy for the prevention of acute exacerbations in chronic obstructive pulmonary disease". Polskie Archiwum Medycyny Wewnetrznej. 122 (1–2): 54–9. PMID 22353707.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - Barr RG, Rowe BH, Camargo CA (2003). Barr, R Graham (ed.). "Methylxanthines for exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev (2): CD002168. doi:10.1002/14651858.CD002168. PMID 12804425.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - COPD Working, Group (2012). "Long-term oxygen therapy for patients with chronic obstructive pulmonary disease (COPD): an evidence-based analysis". Ontario health technology assessment series. 12 (7): 1–64. PMC 3384376. PMID 23074435.
{{cite journal}}:|first=has generic name (help) - Bradley, JM (2005 Oct 19). Bradley, Judy M (ed.). "Short-term ambulatory oxygen for chronic obstructive pulmonary disease". The Cochrane database of systematic reviews (4): CD004356. doi:10.1002/14651858.CD004356.pub3. PMID 16235359.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - Uronis, H (2011 Jun 15). Abernethy, Amy (ed.). "Symptomatic oxygen for non-hypoxaemic chronic obstructive pulmonary disease". The Cochrane database of systematic reviews (6): CD006429. doi:10.1002/14651858.CD006429.pub2. PMID 21678356.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA (2012). Vollenweider, Daniela J (ed.). "Antibiotics for exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev. 12: CD010257. doi:10.1002/14651858.CD010257. PMID 23235687.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Murray, CJ (2012 Dec 15). "Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2197–223. doi:10.1016/S0140-6736(12)61689-4. PMID 23245608.
{{cite journal}}: Check date values in:|date=(help) - ^ Vos, T (2012 Dec 15). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
{{cite journal}}: Check date values in:|date=(help) - "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov. 11, 2009.
{{cite web}}: Check date values in:|accessdate=(help) - "Chronic obstructive pulmonary disease (COPD) Fact sheet N°315". WHO. November 2012.
- Lozano, R (2012 Dec 15). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604.
{{cite journal}}: Check date values in:|date=(help) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22927753, please use {{cite journal}} with
|pmid=22927753instead. - Simpson CR, Hippisley-Cox J, Sheikh A (2010). "Trends in the epidemiology of chronic obstructive pulmonary disease in England: a national study of 51 804 patients". Brit J Gen Pract. 60 (576): 483–8. doi:10.3399/bjgp10X514729. PMC 2894402. PMID 20594429.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 23169314, please use {{cite journal}} with
|pmid=23169314instead. - "Morbidity & Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases" (PDF). National Heart, Lung, and Blood Institute.
- Torio CM, Andrews RM. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. HCUP Statistical Brief #160. Agency for Healthcare Research and Quality, Rockville, MD. August 2013.
- emphysema at dictionary.com
- ^ Petty TL (2006). "The history of COPD". Int J Chron Obstruct Pulmon Dis. 1 (1): 3–14. doi:10.2147/copd.2006.1.1.3. PMC 2706597. PMID 18046898.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Wright, Joanne L.; Churg, Andrew (2008). "History of pathologic descriptions of COPD". In Fishman, Alfred; Elias, Jack; Fishman, Jay (eds.). Fishman's Pulmonary Diseases and Disorders (PDF) (4th ed.). McGraw Hill Professional. pp. 693–705. ISBN 978-0-07-164109-8.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - Fishman AP (2005). "One hundred years of chronic obstructive pulmonary disease". Am. J. Respir. Crit. Care Med. 171 (9): 941–8. doi:10.1164/rccm.200412-1685OE. PMID 15849329.
{{cite journal}}: Unknown parameter|month=ignored (help) - "NHS Outcomes Framework". 20 Dec 2010. Retrieved 18 Oct 2011.
- "An outcomes strategy for people with chronic obstructive pulmonary disease (COPD) and asthma in England". 18 July 2011. Retrieved 18 Oct 2011.
- Torio CM, Andrews RM. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. HCUP Statistical Brief #160. Agency for Healthcare Research and Quality, Rockville, MD. August 2013.
- Rennard SI; Fogarty C; Kelsen S; et al. (2007). "The safety and efficacy of infliximab in moderate to severe chronic obstructive pulmonary disease". Am. J. Respir. Crit. Care Med. 175 (9): 926–34. doi:10.1164/rccm.200607-995OC. PMID 17290043.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - Marinkovic, D (2007). "Cellular basis of chronic obstructive pulmonary disease in horses". International review of cytology. International Review of Cytology. 257: 213–47. doi:10.1016/S0074-7696(07)57006-3. ISBN 978-0-12-373701-4. PMID 17280899.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)
External links
- Template:Dmoz
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) clinical practive guidelines (2013)
- National Institute for Health and Clinical Excellence. Clinical guideline 101: Chronic Obstructive Pulmonary Disease. London, June 2010.
| Diseases of the respiratory system | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Upper RT (including URTIs, common cold) |
| ||||||||||||||||||||||
| Lower RT/ lung disease (including LRTIs) |
| ||||||||||||||||||||||
| Pleural cavity/ mediastinum |
| ||||||||||||||||||||||
| Other/general | |||||||||||||||||||||||
Template:Link FA Template:Link GA
Categories: