| Revision as of 23:18, 14 September 2012 editSemanticMantis (talk | contribs)Extended confirmed users9,386 editsm →History: minor update to dated info on generics, added update template for Jan.2013, also minor wording and wikilinking← Previous edit | Latest revision as of 01:25, 10 December 2024 edit undoCitation bot (talk | contribs)Bots5,430,507 edits Added bibcode. | Use this bot. Report bugs. | Suggested by Dominic3203 | Linked from User:Marbletan/sandbox | #UCB_webform_linked 898/2664 | ||
| (488 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{short description|Hypnotic medication}} | |||
| {{Drugbox | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| {{Infobox drug | |||
| | Watchedfields = changed | |||
| | verifiedrevid = 458773669 | | verifiedrevid = 458773669 | ||
| | IUPAC_name = (''RS'')-6-(5-chloropyridin-2-yl)-7-oxo-6,7-dihydro- |
| IUPAC_name = (''RS'')-6-(5-chloropyridin-2-yl)-7-oxo-6,7-dihydro-5''H''-pyrrolopyrazin-5-yl 4-methylpiperazine-1-carboxylate | ||
| | image = Zopiclone.svg | | image = Zopiclone structure.svg | ||
| | width = |
| width = 200 | ||
| | |
| image2 = Zopiclone-from-xtal-Mercury-3D-bs.png | ||
| | |
| width2 = 230 | ||
| <!-- Clinical data --> | |||
| | tradename = Imovane, Zimovane, Dopareel, others | |||
| <!--Clinical data--> | |||
| | tradename = Imovane, Zimovane | |||
| | Drugs.com = {{drugs.com|international|zopiclone}} | | Drugs.com = {{drugs.com|international|zopiclone}} | ||
| | pregnancy_AU = C | |||
| | pregnancy_US = C | | pregnancy_US = C | ||
| | |
| legal_AU = S4 | ||
| | legal_BR = B1 | |||
| | legal_BR_comment = <ref>{{Cite web |author=Anvisa |author-link=Brazilian Health Regulatory Agency |date=2023-03-31 |title=RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial |trans-title=Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control|url=https://www.in.gov.br/en/web/dou/-/resolucao-rdc-n-784-de-31-de-marco-de-2023-474904992 |url-status=live |archive-url=https://web.archive.org/web/20230803143925/https://www.in.gov.br/en/web/dou/-/resolucao-rdc-n-784-de-31-de-marco-de-2023-474904992 |archive-date=2023-08-03 |access-date=2023-08-16 |publisher=] |language=pt-BR |publication-date=2023-04-04}}</ref> | |||
| | legal_CA = Rx-only | |||
| | legal_UK = Class C | |||
| | legal_NZ = Class C | |||
| | legal_US = Schedule IV | | legal_US = Schedule IV | ||
| | legal_status = Rx-only | |||
| | routes_of_administration = Oral tablets, 3.75mg (UK), 5 or 7.5 mg | |||
| | routes_of_administration = Oral tablets, 3.75 mg or 7.5mg (<small>]</small>), 5 mg, 7.5 mg, or 10 mg (<small>]</small>) | |||
| <!--Pharmacokinetic data--> | <!-- Pharmacokinetic data --> | ||
| | bioavailability = 75–80%<ref name = "Assessment">{{cite web|title=Assessment of Zopiclone|url=https://www.who.int/medicines/areas/quality_safety/4.6ZopicloneCritReview.pdf|website=World Health Organization. Essential Medicines and Health Products |publisher=World Health Organization|year=2006|access-date=5 December 2015|page=9 (Section 5. Pharmacokinetics)}}</ref> | |||
| | bioavailability = 52-59% bound to plasma protein | |||
| | protein_bound = 52–59% | |||
| | metabolism = Various cytochrome P450 liver enzymes | |||
| | metabolism = ] through ] and ] | |||
| | elimination_half-life = ~6 hours <br>~9 hours for over 65 | |||
| | elimination_half-life = ~5 hours (3.5–6.5 hours) <br>~7–9 hours for 65+ years old | |||
| | excretion = Urine | |||
| | excretion = Urine (80%) | |||
| <!--Identifiers--> | <!-- Identifiers --> | ||
| | IUPHAR_ligand = 7430 | |||
| | CASNo_Ref = {{cascite|correct|CAS}} | |||
| | CAS_number_Ref = {{cascite|correct|??}} | | CAS_number_Ref = {{cascite|correct|??}} | ||
| | CAS_number = 43200-80-2 | | CAS_number = 43200-80-2 | ||
| Line 29: | Line 38: | ||
| | PubChem = 5735 | | PubChem = 5735 | ||
| | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | | DrugBank_Ref = {{drugbankcite|correct|drugbank}} | ||
| | DrugBank = DB01198 | |||
| | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | ||
| | ChemSpiderID = 5533 | | ChemSpiderID = 5533 | ||
| Line 40: | Line 49: | ||
| | ChEMBL_Ref = {{ebicite|correct|EBI}} | | ChEMBL_Ref = {{ebicite|correct|EBI}} | ||
| | ChEMBL = 135400 | | ChEMBL = 135400 | ||
| | PDB_ligand = ZPC | |||
| <!--Chemical data--> | <!-- Chemical data --> | ||
| | C=17 | H=17 | Cl=1 | N=6 | O=3 |
| C=17 | H=17 | Cl=1 | N=6 | O=3 | ||
| | molecular_weight = 388.808 g/mol | |||
| | smiles = O=C(OC3c1nccnc1C(=O)N3c2ncc(Cl)cc2)N4CCN(C)CC4 | | smiles = O=C(OC3c1nccnc1C(=O)N3c2ncc(Cl)cc2)N4CCN(C)CC4 | ||
| | InChI = 1/C17H17ClN6O3/c1-22-6-8-23(9-7-22)17(26)27-16-14-13(19-4-5-20-14)15(25)24(16)12-3-2-11(18)10-21-12/h2-5,10,16H,6-9H2,1H3 | |||
| | InChIKey = GBBSUAFBMRNDJC-UHFFFAOYAX | |||
| | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChI = 1S/C17H17ClN6O3/c1-22-6-8-23(9-7-22)17(26)27-16-14-13(19-4-5-20-14)15(25)24(16)12-3-2-11(18)10-21-12/h2-5,10,16H,6-9H2,1H3 | | StdInChI = 1S/C17H17ClN6O3/c1-22-6-8-23(9-7-22)17(26)27-16-14-13(19-4-5-20-14)15(25)24(16)12-3-2-11(18)10-21-12/h2-5,10,16H,6-9H2,1H3 | ||
| Line 52: | Line 59: | ||
| | StdInChIKey = GBBSUAFBMRNDJC-UHFFFAOYSA-N | | StdInChIKey = GBBSUAFBMRNDJC-UHFFFAOYSA-N | ||
| }} | }} | ||
| <!-- this ref was in the drugbox template for the US legal bit, but seems to have been braking the template. put here for safe keeping.<ref name="pmid15806735">{{cite journal |title=Schedules of controlled substances: placement of zopiclone into schedule IV. Final rule |journal=Fed Regist |volume=70 |issue=63 |pages=16935–16937 |date=April 2005 |pmid=15806735 |url=http://edocket.access.gpo.gov/2005/pdf/05-6703.pdf |author1= Drug Enforcement Administration, Department of Justice}}</ref> --> | |||
| '''Zopiclone''', sold under the brand name '''Imovane''' among others, is a ], specifically a ], used to treat ]. Zopiclone is molecularly distinct from benzodiazepine drugs and is classed as a ]. However, zopiclone increases the normal transmission of the ] ] (GABA) in the central nervous system, via modulating ] receptors similarly to the way ] drugs do inducing sedation but not with the anti-anxiety properties of the benzodiazepines. | |||
| <!-- this ref was in the drugbox template for the US legal bit, but seems to have been braking the template. put here for safe keeping.<ref name="pmid15806735">{{cite journal |author= |title=Schedules of controlled substances: placement of zopiclone into schedule IV. Final rule |journal=Fed Regist |volume=70 |issue=63 |pages=16935–7 |year=2005 |month=April |pmid=15806735 |doi= |url=http://edocket.access.gpo.gov/2005/pdf/05-6703.pdf |author1= Drug Enforcement Administration, Department of Justice}}</ref> --> | |||
| '''Zopiclone''' (brand name '''Imovane''' in Canada, Australia and '''Zimovane''' in the UK) is a ] ] (a ''cyclopyrrolone'', which increases the normal transmission of the signal substance GABA in the central nerve system, as benzodiazepines do, however in a rather different way) agent used in the treatment of ]. In the United States, zopiclone is not commercially available,<ref>http://www.drugs.com/cons/zopiclone.html</ref> although its active ], ], is sold under the name '''Lunesta''' (see ]). Zopiclone is a controlled substance in the ], ], ] and some ]an countries, and may be illegal to possess without a prescription. | |||
| Zopiclone is a ]. It works by causing a depression or tranquilization of the central nervous system. After prolonged use, the body can become accustomed to the effects of zopiclone. When the dose is then reduced or the drug is abruptly stopped, withdrawal symptoms may result. These can include a range of symptoms similar to those of ]. Although withdrawal symptoms from therapeutic doses of zopiclone and its isomers (i.e., ]) do not typically present with convulsions and are therefore not considered life-threatening, patients may experience such significant agitation or anxiety that they seek emergency medical attention. {{citation needed|date=July 2023}} | |||
| Zopiclone is known colloquially as a "]". Other Z-drugs include ] (Sonata) and ] (Ambien and AmbienCR) and were initially thought to be less addictive and/or habit-forming than benzodiazepines. However, this appraisal has shifted somewhat in the last few years as cases of addiction and habituation have been presented. It is recommended that zopiclone be taken on a short-term basis, usually a week or less<ref>http://www.nice.org.uk/nicemedia/pdf/TA077publicinfoenglish.pdf</ref>. Daily or continuous use of the drug is not usually advised.<ref>{{cite journal |pmid=2744064 |url= |year=1989 |month= |author=Van, Der, Kleijn, E |title=Effects of zopiclone and temazepam on sleep, behaviour and mood during the day |volume=36 |issue=3 |pages=247–51 |issn=0031-6970 |journal=European journal of clinical pharmacology |doi=10.1007/BF00558155 }}</ref> Zopiclone is a tranquillizer drug. It works by causing a depression or tranquilization of the Central Nervous System. As zopiclone is sedating it is marketed as a sleeping pill. After regular dampening down of the Central Nervous System the body becomes accustomed to functioning under the influence of zopiclone. When the dose is reduced or the drug is stopped these adaptions which have occurred when a person's body has become addicted to a drug are revealed. The result is rebound withdrawal symptoms that can include a range of withdrawal symptoms seen in benzodiazepine withdrawal. | |||
| In the United States, zopiclone is not commercially available,<ref>{{cite web|url=https://www.drugs.com/cons/zopiclone.html |title=Zopiclone consumer information from |publisher=Drugs.com |access-date=2013-06-06}}</ref> although its active ], ], is. Zopiclone is a controlled substance in the United States, Japan, Brazil, New Zealand and some European countries, and may be illegal to possess without a prescription. {{citation needed|date=August 2021}} | |||
| ==History== | |||
| Zopiclone was first developed and introduced in 1986 by ] S.A., now part of ], the main worldwide manufacturer of the drug. Initially it was promoted as being an improvement on ]. A recent ] found that zopiclone had no superiority over benzodiazepines in any of the aspects assessed.<ref>{{cite journal |author=Holbrook AM, Crowther R, Lotter A, Cheng C, King D |title=Meta-analysis of benzodiazepine use in the treatment of insomnia |journal=CMAJ |volume=162 |issue=2 |pages=225–33 |year=2000 |month=January |pmid=10674059 |pmc=1232276 |doi= }}</ref> On April 4, 2005, the United States ] listed zopiclone under ], due to evidence that the drug has ] properties similar to benzodiazepines. | |||
| Zopiclone is known colloquially as a "]". Other Z-drugs include ] and ] and were initially thought to be less addictive than benzodiazepines. However, this appraisal has shifted somewhat in the last few years as cases of addiction and habituation have been presented. Zopiclone is recommended to be taken at the lowest effective dose, with a duration of 2–3 weeks for short-term insomnia.<ref>{{citation| title=Clinical need and practice - Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia|chapter=Chapter 3 - The technologies, section 3.4|id=Technology appraisal guidance |publisher=] (NICE)| date=28 April 2004 | url=https://www.nice.org.uk/guidance/ta77/chapter/3-The-technologies|quote=This guidance will be reviewed if there is new evidence.}} Current as of 8 June 2023</ref> Daily or continuous use of the drug is not usually advised, and caution must be taken when the compound is used in conjunction with benzodiazepines, sedatives or other drugs affecting the central nervous system.<ref>{{cite journal |pmid=2744064 |year=1989 | vauthors = Van Der Kleijn E |title=Effects of zopiclone and temazepam on sleep, behaviour and mood during the day |volume=36 |issue=3 |pages=247–251 |issn=0031-6970 |journal=European Journal of Clinical Pharmacology |doi=10.1007/BF00558155 }}</ref> | |||
| Zopiclone, as traditionally sold worldwide, is a ] mixture of two ]s, only one of which is active.<ref>{{cite journal |pmid=8398600 |url= |format= |year=1993 |month= |author=Blaschke, G; Hempel, G; Müller, We |title=Preparative and analytical separation of the zopiclone enantiomers and determination of their affinity to the benzodiazepine receptor binding site. |volume=5 |issue=6 |pages=419–21 |issn=0899-0042 |doi=10.1002/chir.530050605 |journal=Chirality }}</ref><ref>{{cite journal |pmid=7905394 |url= |format= |year=1993 |month=Nov |author=Fernandez, C; Maradeix, V; Gimenez, F; Thuillier, A; Farinotti, R |title=Pharmacokinetics of zopiclone and its enantiomers in Caucasian young healthy volunteers. |volume=21 |issue=6 |pages=1125–8 |issn=0090-9556 |journal=Drug metabolism and disposition: the biological fate of chemicals }}</ref> In 2005, the pharmaceutical company ] of ] began marketing the active stereoisomer ] under the name ''']''' in the United States. This had the consequence of placing what is a ] in most of the world under patent control in the United States. Although it was expected to be available in generic form by 2010, no generic has become available there at present. <ref>http://insomnia.emedtv.com/lunesta/generic-lunesta.html</ref>{{Update after|2013|01|31}} However, Zopiclone is currently available off-patent in a number of European countries, as well as ] and ]. The eszopiclone/zopiclone difference is in the dosage—the strongest eszopiclone derivative dosage contains 3 mg of the therapeutic stereoisomer, whereas, the highest zopiclone dosage (7.5 mg) contains 3.75 mg of the active stereoisomer. The two agents have not yet been studied in head-to-head clinical trials to determine the existence of any potential clinical differences (efficacy, side effects, developing dependence on the drug, safety, etc.); the significant possibility that the two drugs have identical effects and only differ in dosing and the simple fact that investing in clinical trials is a very expensive undertaking may be responsible for this line of inquiry thus far remaining unpursued.{{citation needed|date=April 2011}} | |||
| {{TOC limit}} | |||
| ==Indications== | |||
| Zopiclone is indicated for the short term treatment of ] where sleep initiation or sleep maintenance are prominent symptoms. Long term use is not recommended as ], dependence, addiction can occur with prolonged use.<ref>{{cite journal |author= |title=What's wrong with prescribing hypnotics? |journal=Drug Ther Bull |volume=42 |issue=12 |pages=89–93 |year=2004 |month=December |pmid=15587763 |doi= 10.1136/dtb.2004.421289|url=}}</ref><ref>{{cite journal |author=Touitou Y |title= |language=French |journal=Ann Pharm Fr |volume=65 |issue=4 |pages=230–8 |year=2007 |month=July |pmid=17652991 |doi= |url=}}</ref> | |||
| == |
==Medical uses== | ||
| ] | ] | ||
| Zopiclone is used for the short-term treatment of insomnia where sleep initiation or sleep maintenance are prominent symptoms. Long-term use is not recommended, as ], dependence, and addiction can occur.<ref>{{cite journal | vauthors = | title = What's wrong with prescribing hypnotics? | journal = Drug and Therapeutics Bulletin | volume = 42 | issue = 12 | pages = 89–93 | date = December 2004 | pmid = 15587763 | doi = 10.1136/dtb.2004.421289 | s2cid = 40188442 }}</ref><ref>{{cite journal | vauthors = Touitou Y | title = | language = fr | journal = Annales Pharmaceutiques Françaises | volume = 65 | issue = 4 | pages = 230–238 | date = July 2007 | pmid = 17652991 | doi = 10.1016/s0003-4509(07)90041-3 }}</ref> One low-quality study found that zopiclone is ineffective in improving sleep quality or increasing sleep time in ]ers, and more research in this area has been recommended.<ref>{{cite journal | vauthors = Liira J, Verbeek JH, Costa G, Driscoll TR, Sallinen M, Isotalo LK, Ruotsalainen JH | title = Pharmacological interventions for sleepiness and sleep disturbances caused by shift work | journal = The Cochrane Database of Systematic Reviews | volume = 2014 | issue = 8 | pages = CD009776 | date = August 2014 | pmid = 25113164 | doi = 10.1002/14651858.CD009776.pub2 | pmc = 10025070 }}</ref> | |||
| ] has been found to be superior to zopiclone in the treatment of insomnia and has been found to have lasting effects on sleep quality for at least a year after therapy.<ref>{{cite journal | vauthors = | title = Cognitive therapy superior to zopiclone for insomnia | journal = The Journal of Family Practice | volume = 55 | issue = 10 | pages = 845 | date = October 2006 | pmid = 17089469 }}</ref><ref>{{cite journal | vauthors = Baillargeon L, Landreville P, Verreault R, Beauchemin JP, Grégoire JP, Morin CM | title = Discontinuation of benzodiazepines among older insomniac adults treated with cognitive-behavioural therapy combined with gradual tapering: a randomized trial | journal = CMAJ | volume = 169 | issue = 10 | pages = 1015–1020 | date = November 2003 | pmid = 14609970 | pmc = 236226 | url = http://www.cmaj.ca/cgi/content/full/169/10/1015 }}</ref><ref>{{cite journal | vauthors = Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik OE, Kvale G, Nielsen GH, Nordhus IH | title = Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial | journal = JAMA | volume = 295 | issue = 24 | pages = 2851–2858 | date = June 2006 | pmid = 16804151 | doi = 10.1001/jama.295.24.2851 | doi-access = }}</ref><ref>{{cite journal | vauthors = Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M | title = Psychological treatment for insomnia in the regulation of long-term hypnotic drug use | journal = Health Technology Assessment | volume = 8 | issue = 8 | pages = iii–iv, 1–68 | date = February 2004 | pmid = 14960254 | doi = 10.3310/hta8080 | doi-access = free }}</ref> | |||
| Zopiclone is sold under a wide variety of brand names world wide.<ref>{{cite web |url= http://www.non-benzodiazepines.org.uk/benzodiazepine-names.html#Zopiclone |title= Benzodiazepine Names |accessdate= 26 July 2008 }}</ref> | |||
| *'''Zalepla''' - Costa Rica, Ecuador, Guatemala, Panama | |||
| *'''Zimovane''' - United Kingdom | |||
| *'''Zimovane, Zileze, Zimoclone, Zopitan, Zorclone''' - Ireland | |||
| *'''Imovane, Apo-Zopiclone, pms-Zopiclone, Ran-Zopiclone, Rhovane, Pro Zopiclone''' - Canada | |||
| *'''Imovane or Imrest''' - Australia, New Zealand, Iceland, Italy, Poland, Finland, Sweden, Norway and Brazil. | |||
| *'''Nocturno''' and '''Imovane''' - Israel | |||
| *'''Imovane (Имован); Relaxon (Релаксон); Somnol (Сомнол)''' - Russia | |||
| *'''Alchera, Imovane, Z-Dorm, Zopimed, Zopivane''' - South Africa | |||
| *'''Imoclone, Imozop or Imovane''' - Denmark | |||
| *'''Somnols; Imovane; Zopitin''' - Lithuania | |||
| *'''Limovan''' - Spain | |||
| *'''Ximovan''' - Germany | |||
| *'''Zopicon''' - India (by Intas Pharma) | |||
| *'''Zopiclon''' - Netherlands, Bulgaria | |||
| *'''Zopiclona''' - Argentina | |||
| *'''Zetix''' - Bolivia, Chile, Ecuador | |||
| *'''Hypnor''' - Egypt | |||
| *'''Amoban''' - Japan | |||
| *'''Zopilcone Actavis''' Norway | |||
| ===Specific populations=== | |||
| ==Adverse reactions== | |||
| ====Elderly==== | |||
| The side effect most commonly seen in clinical trials is taste alteration or ] (bitter, metallic taste, which is usually fleeting in most users but can persist until the drug's ] has expired). ] may occur in the daytime following withdrawal from the drug after prolonged periods of use (especially when taken for more than two weeks).{{fact|date=August 2012}} | |||
| Zopiclone, similar to other benzodiazepines and ] ] drugs, causes impairments in body balance and standing steadiness in individuals who wake up at night or the next morning. Falls and hip fractures are frequently reported. The combination with ] consumption increases these impairments. Partial, but incomplete tolerance develops to these impairments.<ref name="Mets-2010">{{cite journal | vauthors = Mets MA, Volkerts ER, Olivier B, Verster JC | title = Effect of hypnotic drugs on body balance and standing steadiness | journal = Sleep Medicine Reviews | volume = 14 | issue = 4 | pages = 259–267 | date = August 2010 | pmid = 20171127 | doi = 10.1016/j.smrv.2009.10.008 }}</ref> | |||
| Zopiclone increases ] and increases the number of falls in older people, as well as cognitive side effects. Falls are a significant cause of death in older people.<ref>{{cite journal | vauthors = Tada K, Sato Y, Sakai T, Ueda N, Kasamo K, Kojima T | title = Effects of zopiclone, triazolam, and nitrazepam on standing steadiness | journal = Neuropsychobiology | volume = 29 | issue = 1 | pages = 17–22 | year = 1994 | pmid = 8127419 | doi = 10.1159/000119057 }}</ref><ref>{{cite journal | vauthors = Allain H, Bentué-Ferrer D, Tarral A, Gandon JM | title = Effects on postural oscillation and memory functions of a single dose of zolpidem 5 mg, zopiclone 3.75 mg and lormetazepam 1 mg in elderly healthy subjects. A randomized, cross-over, double-blind study versus placebo | journal = European Journal of Clinical Pharmacology | volume = 59 | issue = 3 | pages = 179–188 | date = July 2003 | pmid = 12756510 | doi = 10.1007/s00228-003-0591-5 | s2cid = 13440208 }}</ref><ref>{{cite journal | vauthors = Antai-Otong D | title = The art of prescribing. Risks and benefits of non-benzodiazepine receptor agonists in the treatment of acute primary insomnia in older adults | journal = Perspectives in Psychiatric Care | volume = 42 | issue = 3 | pages = 196–200 | date = August 2006 | pmid = 16916422 | doi = 10.1111/j.1744-6163.2006.00070.x | doi-access = }}</ref> | |||
| An extensive review of the medical literature regarding the management of insomnia and the elderly found that considerable evidence of the effectiveness and lasting benefits of nondrug treatments for insomnia exist. Compared with the benzodiazepines, the nonbenzodiazepine sedative-hypnotics, such as zopiclone, offer few if any advantages in efficacy or tolerability in elderly persons. Newer agents such as the ]s may be more suitable and effective for the management of chronic insomnia in elderly people. Long-term use of sedative-hypnotics for insomnia lacks an evidence base and is discouraged for reasons that include concerns about such potential adverse drug effects as ] (]), daytime sedation, motor incoordination, and increased risk of motor vehicle accidents and falls. In addition, the effectiveness and safety of long-term use of nonbenzodiazepine hypnotic drugs remains to be determined.<ref>{{cite journal | vauthors = Bain KT | title = Management of chronic insomnia in elderly persons | journal = The American Journal of Geriatric Pharmacotherapy | volume = 4 | issue = 2 | pages = 168–192 | date = June 2006 | pmid = 16860264 | doi = 10.1016/j.amjopharm.2006.06.006 }}</ref> | |||
| Zopiclone induces amnesia type memory impairments similar to ]<ref>{{cite journal |author=Gorenstein C, Tavares SM, Gentil V, Peres C, Moreno RA, Dreyfus JF |title=Psychophysiological effects and dose equivalence of zopiclone and triazolam administered to healthy volunteers. Methodological considerations |journal=Braz. J. Med. Biol. Res. |volume=23 |issue=10 |pages=941–51 |year=1990 |pmid=2101059 |doi= |url=}}</ref> and ]. Impairment of driving skills with a resultant increased risk of ] is probably the most important side effect. This side effect is not unique to zopiclone but also occurs with other ] drugs.<ref>{{cite journal |author=Gustavsen I, Bramness JG, Skurtveit S, Engeland A, Neutel I, Mørland J |title=Road traffic accident risk related to prescriptions of the hypnotics zopiclone, zolpidem, flunitrazepam and nitrazepam |journal=Sleep Med. |volume=9 |issue=8 |pages=818–22 |year=2008 |month=December |pmid=18226959 |doi=10.1016/j.sleep.2007.11.011 |url=http://linkinghub.elsevier.com/retrieve/pii/S1389-9457(07)00424-8}}</ref><ref>{{cite journal |author=Verster JC, Veldhuijzen DS, Patat A, Olivier B, Volkerts ER |title=Hypnotics and driving safety: meta-analyses of randomized controlled trials applying the on-the-road driving test |journal=Curr Drug Saf |volume=1 |issue=1 |pages=63–71 |year=2006 |month=January |pmid=18690916 |doi= 10.2174/157488606775252674}}</ref> A study assessing the impact of zopiclone on driving skills the next day found that the impairments on driving skills are double that of a social dose of ]. ] had no detrimental effects on driving skills the next day.<ref>{{cite journal |author=Vermeeren A, Riedel WJ, van Boxtel MP, Darwish M, Paty I, Patat A |title=Differential residual effects of zaleplon and zopiclone on actual driving: a comparison with a low dose of alcohol |journal=Sleep |volume=25 |issue=2 |pages=224–31 |year=2002 |month=March |pmid=11905433 }}</ref> | |||
| === |
====Liver disease==== | ||
| Patients with liver disease eliminate zopiclone much more slowly than normal patients and in addition experience exaggerated pharmacological effects of the drug.<ref>{{cite journal | vauthors = Parker G, Roberts CJ | title = Plasma concentrations and central nervous system effects of the new hypnotic agent zopiclone in patients with chronic liver disease | journal = British Journal of Clinical Pharmacology | volume = 16 | issue = 3 | pages = 259–265 | date = September 1983 | pmid = 6626417 | pmc = 1428012 | doi = 10.1111/j.1365-2125.1983.tb02159.x }}</ref> | |||
| Gastrointestinal: taste disturbances including bitter metallic taste, ].<ref>{{cite journal |pmid=6996815 |url= |year=1980 |month= |author=Giercksky, Ke; Wickstrom, E |title=A dose-response study in situational insomnia with zopiclone, a new tranquilizer |volume=3 |issue=1 |pages=21–7 |issn=0149-2918 |journal=Clinical therapeutics }}</ref><ref>{{cite journal |author=Ratrema M, Guy C, Nelva A, ''et al.'' |title= |language=French |journal=Therapie |volume=56 |issue=1 |pages=41–50 |year=2001 |pmid=11322016 |doi= |url=}}</ref> | |||
| Nervous system: disruption of ], ], drowsiness, memory impairments, visuospatial impairments, ], ]s, and ].<ref>{{cite journal |pmid=7188378 |year=1982 |month= |author=Nicholson, An; Stone, Bm |title=Zopiclone: sleep and performance studies in healthy man. |volume=17 Suppl 2 |issue= |pages=92–7 |issn=0020-8272 |journal=International pharmacopsychiatry }}</ref><ref>{{cite journal |pmid=6152563 |year=1984 |month= |author=Subhan, Z; Hindmarch, I |title=Effects of zopiclone and benzodiazepine hypnotics on search in short-term memory. |volume=12 |issue=4 |pages=244–8 |issn=0302-282X |journal=Neuropsychobiology |url= |format= |doi=10.1159/000118146 }}</ref><ref>{{cite journal |pmid=6529528 |year=1984 |month=Dec |author=Channer, Ks; Dent, M; Roberts, Cj |title=The effect of posture at the time of administration on the central depressant effects of the new hypnotic zopiclone. |volume=18 |issue=6 |pages=879–86 |issn=0306-5251 |pmc=1463687 |journal=British Journal of Clinical Pharmacology }}</ref><ref>{{cite journal |pmid=3521857 |url= |format= |year=1986 |month= |author=Monchesky, Tc; Billings, Bj; Phillips, R |title=Zopiclone: a new nonbenzodiazepine hypnotic used in general practice. |volume=8 |issue=3 |pages=283–91 |issn=0149-2918 |journal=Clinical therapeutics }}</ref><ref>{{cite journal |author=Bocca ML, Denise P |title=Residual effects of hypnotics on disengagement of spatial attention |journal=J. Psychopharmacol. (Oxford) |volume=14 |issue=4 |pages=401–5 |year=2000 |pmid=11198059 |doi= 10.1177/026988110001400409|url=http://jop.sagepub.com/cgi/pmidlookup?view=long&pmid=11198059}}</ref> Unexpected ] have been noted, which if experienced should lead to the drug being withdrawn from the patient. | |||
| == |
==Adverse reactions== | ||
| Sleeping pills, including zopiclone, have been associated with an increased risk of death.<ref>{{cite journal | vauthors = Kripke DF | title = Mortality Risk of Hypnotics: Strengths and Limits of Evidence | journal = Drug Safety | volume = 39 | issue = 2 | pages = 93–107 | date = February 2016 | pmid = 26563222 | doi = 10.1007/s40264-015-0362-0 | s2cid = 7946506 | doi-access = free | url = https://escholarship.org/content/qt08d9f3d5/qt08d9f3d5.pdf?t=nz1gjv }}</ref> The ] states adverse reactions as follows: "taste disturbance (some report a metallic taste); less commonly nausea, vomiting, dizziness, drowsiness, dry mouth, headache; rarely amnesia, confusion, depression, hallucinations, nightmares; very rarely light headedness, incoordination, paradoxical effects and sleep-walking also reported".<ref name=bnf>{{citation |publisher=National Institute for Health and Care Excellence |date=19 September 2016 |url=https://www.evidence.nhs.uk/document?ci=https%3a%2f%2fwww.evidence.nhs.uk%2fformulary%2fbnf%2fcurrent%2f4-central-nervous-system%2f41-hypnotics-and-anxiolytics%2f411-hypnotics%2fzaleplon-zolpidem-and-zopiclone%2fzopiclone&returnUrl=Search%3fq%3dzopiclone&q=zopiclone |title=Zopiclone |work=British National Formulary |access-date=2 October 2016 |archive-url=https://web.archive.org/web/20161009182953/https://www.evidence.nhs.uk/document?ci=https%3a%2f%2fwww.evidence.nhs.uk%2fformulary%2fbnf%2fcurrent%2f4-central-nervous-system%2f41-hypnotics-and-anxiolytics%2f411-hypnotics%2fzaleplon-zolpidem-and-zopiclone%2fzopiclone&returnUrl=Search%3fq%3dzopiclone&q=zopiclone |archive-date=9 October 2016 |url-status=dead }}</ref> | |||
| * '''Gastrointestinal''': ], ], ], ], coated tongue, ], ] or increased ], ], ] pains, ], ], ]. | |||
| * '''Cardiovascular''': ]s in ] patients. | |||
| * '''Skin''': ], ] in the arms and legs. | |||
| * '''Miscellaneous''': blurred vision, frequent ], ], mild to moderate increases in ] ]s and/or ] ] and ] have been reported very rarely.<ref>{{cite journal |author=Hussain N, MacKinnon M, Akbari A |title=Zopiclone-induced acute interstitial nephritis |journal=Am. J. Kidney Dis. |volume=41 |issue=5 |pages=E17 |year=2003 |month=May |pmid=12778435 |doi= 10.1016/S0272-6386(03)00382-2|url=http://linkinghub.elsevier.com/retrieve/pii/S0272638603002130}}</ref> | |||
| * '''Reproductive''': ], ], ] in both women and men.{{Citation needed|date=January 2008}} | |||
| * '''Nervous system''': ],<ref>{{cite journal |author=Moloney I, Breen EG, El Hassan H, Kelly BD |title=Extreme agitation occurring with zopiclone |journal=Ir Med J |volume=100 |issue=6 |pages=511 |year=2007 |month=June |pmid=17668690 |doi= |url=}}</ref> ], ] including ] and ], ], ], ], ], ], ] and/or ], feeling of drunkenness, ], ],<ref>{{cite journal |author=Ferentinos P, Paparrigopoulos T |title=Zopiclone and sleepwalking |journal=Int. J. Neuropsychopharmacol. |volume=12 |issue=1 |pages=141–2 |year=2009 |month=February |pmid=18925983 |doi=10.1017/S1461145708009541 |url=http://journals.cambridge.org/abstract_S1461145708009541}}</ref> coordination abnormality, ], ], ]s of various strengths, usually auditory and visual, behavioural disorders, ], ], ], ]s, ].<ref>{{cite journal |pmid=3679064 |url= |year=1987 |month= |author=Warot, D; Bensimon, G; Danjou, P; Puech, Aj |title=Comparative effects of zopiclone, triazolam and placebo on memory and psychomotor performance in healthy volunteers. |volume=1 |issue=2 |pages=145–52 |issn=0767-3981 |journal=Fundamental & clinical pharmacology |format= |doi=10.1111/j.1472-8206.1987.tb00553.x }}</ref><ref>{{cite journal |author=Fava GA |title=Amnestic syndrome induced by zoplclone |journal=Eur. J. Clin. Pharmacol. |volume=50 |issue=6 |pages=509 |year=1996 |pmid=8858280 |doi= 10.1007/s002280050149|url=}}</ref><ref>{{cite journal |author=Silva A, Collao A, Orellana M, Meléndez J, Caviedes P, Cárdenas AM |title=Zopiclone, but not brotizolam, impairs memory storage during sleep |journal=Neurosci. Res. |volume=47 |issue=2 |pages=241–3 |year=2003 |month=October |pmid=14512149 |doi= 10.1016/S0168-0102(03)00170-6|url=http://linkinghub.elsevier.com/retrieve/pii/S0168010203001706}}</ref> ] can also occur but is a side effect mainly seen in the elderly.<ref>{{cite journal |author=David M, Breton JL, Guy I, Vandel S |title= |language=French |journal=Therapie |volume=53 |issue=1 |pages=78–80 |year=1998 |pmid=9773104 |doi= |url=}}</ref> | |||
| ==Contraindications== | |||
| ==Tolerance, dependence and withdrawal== | |||
| Zopiclone causes ] skills similar to those of benzodiazepines. Long-term users of hypnotic drugs for ]s develop only partial tolerance to adverse effects on driving, with users of hypnotic drugs even after one year of use still showing an increased motor vehicle accident rate.<ref>{{cite journal | vauthors = Staner L, Ertlé S, Boeijinga P, Rinaudo G, Arnal MA, Muzet A, Luthringer R | title = Next-day residual effects of hypnotics in DSM-IV primary insomnia: a driving simulator study with simultaneous electroencephalogram monitoring | journal = Psychopharmacology | volume = 181 | issue = 4 | pages = 790–798 | date = October 2005 | pmid = 16025317 | doi = 10.1007/s00213-005-0082-8 | s2cid = 26351598 }}</ref> Patients who drive motor vehicles should not take zopiclone as there is a significantly increased risk of accidents in zopiclone users.<ref>{{cite journal | vauthors = Barbone F, McMahon AD, Davey PG, Morris AD, Reid IC, McDevitt DG, MacDonald TM | title = Association of road-traffic accidents with benzodiazepine use | journal = Lancet | volume = 352 | issue = 9137 | pages = 1331–1336 | date = October 1998 | pmid = 9802269 | doi = 10.1016/S0140-6736(98)04087-2 | s2cid = 40825194 }}</ref> Zopiclone induces impairment of psychomotor function.<ref>{{cite journal | vauthors = Yasui M, Kato A, Kanemasa T, Murata S, Nishitomi K, Koike K, Tai N, Shinohara S, Tokomura M, Horiuchi M, Abe K | title = | journal = Nihon Shinkei Seishin Yakurigaku Zasshi = Japanese Journal of Psychopharmacology | volume = 25 | issue = 3 | pages = 143–151 | date = June 2005 | pmid = 16045197 }}</ref><ref>{{cite journal | vauthors = Rettig HC, de Haan P, Zuurmond WW, von Leeuwen L | title = Effects of hypnotics on sleep and psychomotor performance. A double-blind randomised study of lormetazepam, midazolam and zopiclone | journal = Anaesthesia | volume = 45 | issue = 12 | pages = 1079–1082 | date = December 1990 | pmid = 2278337 | doi = 10.1111/j.1365-2044.1990.tb14896.x | s2cid = 36841164 | doi-access = free }}</ref> Driving or operating machinery should be avoided after taking zopiclone as effects can carry over to the next day, including impaired hand-eye coordination.<ref>{{cite journal | vauthors = Lader M, Denney SC | title = A double-blind study to establish the residual effects of zopiclone on performance in healthy volunteers | journal = International Pharmacopsychiatry | volume = 17 | issue = Suppl 2 | pages = 98–108 | year = 1982 | pmid = 7188379 }}</ref><ref>{{cite journal | vauthors = Billiard M, Besset A, de Lustrac C, Brissaud L | title = Dose-response effects of zopiclone on night sleep and on nighttime and daytime functioning | journal = Sleep | volume = 10 | issue = Suppl 1 | pages = 27–34 | year = 1987 | pmid = 3326113 | doi = 10.1093/sleep/10.suppl_1.27 | doi-access = free }}</ref> | |||
| Zopiclone, a benzodiazepine-like drug was introduced and initially promoted as having less dependence and withdrawal than traditional ] drugs. However, zopiclone may have an even greater addictive potential than benzodiazepines and has been described as a "benzodiazepine in disguise".<ref>{{cite journal | author = Bramness JG | coauthors = Olsen H. | year = 1998 | title = | journal = Tidsskrift for den Norske laegeforening. | volume = 118 | issue = 13 | pages = 2029–32 | pmid = 9656789 }}</ref><ref>{{cite journal |author=Luty S, Sellman D |title=Imovane—a benzodiazepine in disguise |journal=N. Z. Med. J. |volume=106 | issue=959 |pages=293 |year=1993 |month=July |pmid=8321452 |doi= |url=}}</ref><ref>{{cite journal |author=Deveaux M, Chèze M, Pépin G |title= The role of liquid chromatography-tandem mass spectrometry (LC-MS/MS) to test blood and urine samples for the toxicological investigation of drug-facilitated crimes |journal=Ther Drug Monit |volume=30 |issue=2 |pages=225–8 |year=2008 |month=April |pmid=18367985 |doi= 10.1097/FTD.0b013e3181676186 |url = http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?an=00007691-200804000-00015}}</ref> Tolerance to the effects of zopiclone can develop after a few weeks. Long term use should be avoided. Abrupt withdrawal particularly with prolonged and high doses can in severe cases cause ] and ].<ref>{{cite journal |author= | title = Hypnotic dependence: zolpidem and zopiclone too |journal=Prescrire Int |volume=10 |issue=51 |pages=15 |year=2001 |month= February | pmid = 11503851 | doi= |url=}}</ref><ref>{{cite journal |author=Wong CP, Chiu PK, Chu LW |title=Zopiclone withdrawal: an unusual cause of delirium in the elderly |journal=Age Ageing |volume=34 |issue=5 |pages=526–7 |year=2005 |month=September |pmid=16107464 |doi= 10.1093/ageing/afi132 |url = http://ageing.oxfordjournals.org/cgi/reprint/34/5/526 |format=PDF}}</ref> | |||
| A ] study on the effect on performance of several hypnotic medications, relevant to military personnel who may have to be awakened to carry out duties, found that drugs listed in increasing order of performance impact duration were melatonin (with no impact), zaleplon, temazepam, and zopiclone. The effects on serial reaction time (SRT), logical reasoning (LRT), serial subtraction (SST), and multitask (MT) were measured. For zaleplon (10 mg), zopiclone (7.5 mg) and temazepam (15 mg) respectively the times to recover normal performance for SRT were 3.25, {{Em|6.25}}, and 5.25 hours; for LRT 3.25, {{Em|>6.25}}, and 4.25 hours; for SST 2.25, {{Em|>6.25}}, and 4.25 hours; and for MT 2.25, {{Em|4.25}}, and 3.25 hours. The study did not consider the effectiveness of the drugs on sleep.<ref>{{cite journal | vauthors = Paul MA, Gray G, Kenny G, Pigeau RA | title = Impact of melatonin, zaleplon, zopiclone, and temazepam on psychomotor performance | journal = Aviation, Space, and Environmental Medicine | volume = 74 | issue = 12 | pages = 1263–1270 | date = December 2003 | pmid = 14692469 | url = https://www.researchgate.net/publication/8945690 | publisher = Aerospace Medical Association }}</ref> | |||
| Publications in the '']'' do not give any evidence to the claim that zopiclone has a low dependence potential. In fact, physical dependence and recreational abuse and withdrawal syndromes similar to those seen in ] are frequently encountered. Withdrawal symptoms included ], ], ], sweats, flushes, ], ], and further insomnia.<ref>{{cite journal |author=Jones IR, Sullivan G |title=Physical dependence on zopiclone: case reports |journal=BMJ |volume= 316 |issue=7125 |pages=117 |year=1998 |month=January |pmid=9462317 |doi= |url=http://bmj.com/cgi/pmidlookup?view=long&pmid=9462317 |pmc= 2665371}}</ref> Suspected withdrawal convulsions during detoxification from zopiclone has been reported, however the individual was a high dose zopiclone misuser.<ref>{{cite journal |pmid=1754610 |url= |format= |year=1991 |month=Jul |author=Aranko, K; Henriksson, M; Hublin, C; Seppäläinen, Am |title=Misuse of zopiclone and convulsions during withdrawal. |volume=24 |issue=4 |pages=138–40 |issn=0176-3679 |journal= Pharmacopsychiatry |doi=10.1055/s-2007-1014457 }}</ref> | |||
| ==EEG and sleep== | |||
| The risk of dependency on zopiclone when used for less than 2 weeks or only used occasionally is low.<ref>{{cite journal | pmid = 3326116 | url = | year=1987 |month= |author=Anderson, Aa |title=Zopiclone and nitrazepam: a multicenter placebo controlled comparative study of efficacy and tolerance in insomniac patients in general practice. |volume=10 Suppl 1 |issue= |pages=54–62 |issn=0161-8105 |journal=Sleep }}</ref> However, this is disputed by one study of low dose zopiclone taken for only 7 nights. It found that discontinuation of zopiclone caused significant ]. Furthermore when ] taken for 7 nights was discontinued no rebound insomnia occurred suggesting that zopiclone may have even more significant problems of tolerance and dependence than the ].<ref>{{cite journal |pmid=1297939 | url= | format = |year=1992 |month=Oct |author=Begg, Ej; Robson, Ra; Frampton, Cm; Campbell, Je |title= A comparison of efficacy and tolerance of the short acting sedatives midazolam and zopiclone. |volume=105 |issue=944 |pages=428–9 |issn=0028-8446 |journal=The New Zealand medical journal}}</ref> After 3 weeks of use mild to moderate rebound withdrawal symptoms appear upon discontinuation of zopiclone.<ref>{{cite journal |pmid=6669632 |url= |year=1983 |month= |author=Dorian, P; Sellers, Em; Kaplan, H; Hamilton, C |title=Evaluation of zopiclone physical dependence liability in normal volunteers. |volume=27 Suppl 2 |issue= |pages=228–34 |issn=0031-7012 |journal=Pharmacology |format= |doi= 10.1159/000137931}}</ref> Due to the risk of ] and ], zopiclone is only recommended for short term (1–4 weeks max) relief of insomnia, or alternatively, long term infrequent use.<ref>{{cite journal |author=Mendelson WB, Jain B |title = An assessment of short-acting hypnotics |journal=Drug Saf |volume=13 |issue=4 |pages=257–70 |year=1995 |month=October |pmid=8573298 |doi= 10.2165/00002018-199513040-00005|url=}}</ref> Long-term zopiclone users who have become physically dependent should not discontinue their medication abruptly as severe withdrawal symptoms may occur such as ].<ref>{{cite journal |author=Harter C, Piffl-Boniolo E, Rave-Schwank M |title= |language=German |journal = Psychiatr Prax |volume=26 |issue=6 |pages=309 |year=1999 |month=November |pmid=10627964 |doi= |url=}}</ref> If zopiclone has been taken for more than a few weeks then the medication should be gradually reduced or preferably to cross over to an ] of ] (Valium), which has a much longer half-life which makes withdrawal easier and then gradually taper their dosage over a period of several months in order to avoid extremely severe and unpleasant withdrawal symptoms (e.g., inner restlessness, ], ], hypertension, hallucinations, seizures, anxiety, depression, psychosis, etc.) which can last up to two years after withdraw if the withdrawal is done too abruptly.<ref>{{cite web |url=http://www.sanofi-aventis.ca/products/en/imovane.pdf |title=IMOVANE (zopiclone) Tablets, 5.0 mg and 7.5 mg |author=sanofi-aventis Canada Inc |authorlink=sanofi-aventis| date=October 30, 2008 | format=PDF}}</ref><ref>{{cite journal | author=Kahlert I | coauthors=Brüne M | year=2001 |month=June | title= | journal=Dtsch Med Wochenschr | volume=126 | issue=22 | pages=653–4 | pmid=11450624 | doi=10.1055/s-2001-14488 }}</ref><ref>{{cite web |url=http://www.benzo.org.uk/manual/ |title=BENZODIAZEPINES: HOW THEY WORK AND HOW TO WITHDRAW |author=Professor Heather Ashton}}</ref> | |||
| It causes similar alterations on EEG readings and ] as benzodiazepines and causes disturbances in sleep architecture on withdrawal as part of its ].<ref>{{cite journal |vauthors=Trachsel L, Dijk DJ, Brunner DP, Klene C, Borbély AA |title=Effect of zopiclone and midazolam on sleep and EEG spectra in a phase-advanced sleep schedule |journal=Neuropsychopharmacology |volume=3 |issue=1 |pages=11–18 |date=February 1990 |pmid=2306331 }}</ref><ref>{{cite journal |vauthors=Mann K, Bauer H, Hiemke C, Röschke J, Wetzel H, Benkert O |title=Acute, subchronic and discontinuation effects of zopiclone on sleep EEG and nocturnal melatonin secretion |journal=Eur Neuropsychopharmacol |volume=6 |issue=3 |pages=163–168 |date=August 1996 |pmid=8880074 |doi= 10.1016/0924-977X(96)00014-4|s2cid=25259646 }}</ref> Zopiclone reduces both delta waves and the number of high-amplitude delta waves whilst increasing low-amplitude waves.<ref>{{cite journal |vauthors=Wright NA, Belyavin A, Borland RG, Nicholson AN |title=Modulation of delta activity by hypnotics in middle-aged subjects: studies with a benzodiazepine (flurazepam) and a cyclopyrrolone (zopiclone) |journal=Sleep |volume=9 |issue=2 |pages=348–352 |date=June 1986 |pmid=3505734 |doi= 10.1093/sleep/9.2.348|doi-access=free }}</ref> Zopiclone reduces the total amount of time spent in ] as well as delaying its onset.<ref>{{cite journal |vauthors=Kim YD, Zhuang HY, Tsutsumi M, Okabe A, Kurachi M, Kamikawa Y |title=Comparison of the effect of zopiclone and brotizolam on sleep EEG by quantitative evaluation in healthy young women |journal=Sleep |volume=16 |issue=7 |pages=655–661 |date=October 1993 |pmid=8290860 |doi= 10.1093/sleep/16.7.655|doi-access=free }}</ref><ref>{{cite journal |vauthors=Kanno O, Watanabe H, Kazamatsuri H |title=Effects of zopiclone, flunitrazepam, triazolam and levomepromazine on the transient change in sleep-wake schedule: polygraphic study, and the evaluation of sleep and daytime condition |journal=Prog. Neuropsychopharmacol. Biol. Psychiatry |volume=17 |issue=2 |pages=229–239 |date=March 1993 |pmid=8430216 |doi= 10.1016/0278-5846(93)90044-S|s2cid=54285586 }}</ref> In ] studies, zopiclone significantly increases the energy of the beta frequency band, increasing stage 2. Zopiclone is less selective to the α1 site and has higher affinity to the α2 site than zaleplon. Zopiclone is therefore very similar pharmacologically to benzodiazepines.<ref>{{cite journal | vauthors = Noguchi H, Kitazumi K, Mori M, Shiba T | title = Electroencephalographic properties of zaleplon, a non-benzodiazepine sedative/hypnotic, in rats | journal = Journal of Pharmacological Sciences | volume = 94 | issue = 3 | pages = 246–251 | date = March 2004 | pmid = 15037809 | doi = 10.1254/jphs.94.246 | doi-access = free }}</ref> | |||
| After 4 weeks of nightly use of zopiclone day time withdrawal related ] begin to emerge in some users. However, the day time withdrawal anxiety does not appear to be as intense as that seen with the much shorter acting ] which provokes even more profound day time withdrawal anxiety symptoms in long term users.<ref>{{cite journal |pmid=2230061 |url= |format=PDF |year=1990 |month=Jul |author=Fontaine, R; Beaudry, P; Le, Morvan, P; Beauclair, L; Chouinard, G |title=Zopiclone and triazolam in insomnia associated with generalized anxiety disorder: a placebo-controlled evaluation of efficacy and daytime anxiety. |volume=5 |issue=3 |pages=173–83 |issn=0268-1315 |journal=International clinical psychopharmacology |doi=10.1097/00004850-199007000-00002 }}</ref> | |||
| ==Overdose== | |||
| According to the ], zopiclone, although molecularly is not a ], binds unselectively with high affinity to the same benzodiazepine sites that the benzodiazepine class of drugs do. The World Health Organisation also stated that zopiclone is cross tolerant with ] and one can substitute one for the other. In the review of zopiclone by the ] they found that the appearance of ] usually occurred either when the drug was misused in excessive doses or when use of zopiclone was prolonged. The ] from zopiclone reported included ], ], ], ], rebound ], ], ], ] and flushes.<ref name=whoaoz>{{Cite web | url = http://www.who.int/medicines/areas/quality_safety/4.6ZopicloneCritReview.pdf | title = World Health Organisation - Assessment of Zopiclone | author = WHO | authorlink = World Health Organisation | year = 2006 | format = PDF | publisher = who.int }}</ref> | |||
| Zopiclone is sometimes used as a method of suicide.<ref>{{cite journal | vauthors = Mannaert E, Tytgat J, Daenens P | title = Detection and quantification of the hypnotic zopiclone, connected with an uncommon case of drowning | journal = Forensic Science International | volume = 83 | issue = 1 | pages = 67–72 | date = November 1996 | pmid = 8939015 | doi = 10.1016/0379-0738(96)02018-X }}</ref> It has a similar fatality index to that of benzodiazepine drugs, apart from ], which is particularly toxic in overdose.<ref>Buckley NA, Dawson AH, Whyte IM, McManus P, Ferguson N.Correlations between prescriptions and drugs taken in self-poisoning: Implications for prescribers and drug regulation. Med J Aust (in press)</ref><ref name="pmid12474705">{{cite journal | vauthors = Buckley NA, Dawson AH, Whyte IM, O'Connell DL | title = Relative toxicity of benzodiazepines in overdose | journal = BMJ | volume = 310 | issue = 6974 | pages = 219–221 | date = January 1995 | pmid = 7866122 | pmc = 2548618 | doi = 10.1136/bmj.310.6974.219 }}</ref> Deaths have occurred from zopiclone overdose, alone or in combination with other drugs.<ref>{{cite journal | vauthors = Meatherall RC | title = Zopiclone fatality in a hospitalized patient | journal = Journal of Forensic Sciences | volume = 42 | issue = 2 | pages = 340–343 | date = March 1997 | pmid = 9068198 | doi = 10.1520/JFS14125J }}</ref><ref>{{cite journal | vauthors = Van Bocxlaer J, Meyer E, Clauwaert K, Lambert W, Piette M, De Leenheer A | title = Analysis of zopiclone (Imovane) in postmortem specimens by GC-MS and HPLC with diode-array detection | journal = Journal of Analytical Toxicology | volume = 20 | issue = 1 | pages = 52–54 | year = 1996 | pmid = 8837952 | doi = 10.1093/jat/20.1.52 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Yamazaki M, Terada M, Mitsukuni Y, Yoshimura M | title = | language = ja | journal = Nihon Hoigaku Zasshi = the Japanese Journal of Legal Medicine | volume = 52 | issue = 4 | pages = 245–252 | date = August 1998 | pmid = 9893443 }}</ref> Overdose of zopiclone may present with excessive sedation and depressed respiratory function that may progress to coma and possibly death.<ref>{{cite journal | vauthors = Boniface PJ, Russell SG | title = Two cases of fatal zopiclone overdose | journal = Journal of Analytical Toxicology | volume = 20 | issue = 2 | pages = 131–133 | year = 1996 | pmid = 8868406 | doi = 10.1093/jat/20.2.131 | doi-access = }}</ref> Zopiclone combined with ], ], or other central nervous system depressants may be even more likely to lead to fatal overdoses. Zopiclone overdosage can be treated with the GABA<sub>A</sub> receptor benzodiazepine site antagonist ], which displaces zopiclone from its binding site, thereby rapidly reversing its effects.<ref>{{cite journal | vauthors = Cienki JJ, Burkhart KK, Donovan JW | title = Zopiclone overdose responsive to flumazenil | journal = Clinical Toxicology | volume = 43 | issue = 5 | pages = 385–386 | year = 2005 | pmid = 16235515 | doi = 10.1081/clt-200058944 | s2cid = 41701825 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Pounder DJ, Davies JI | title = Zopiclone poisoning: tissue distribution and potential for postmortem diffusion | journal = Forensic Science International | volume = 65 | issue = 3 | pages = 177–183 | date = May 1994 | pmid = 8039775 | doi = 10.1016/0379-0738(94)90273-9 }}</ref> Serious effects on the heart may also occur from a zopiclone overdose<ref>{{cite journal | vauthors = Regouby Y, Delomez G, Tisserant A | title = | language = fr | journal = Therapie | volume = 45 | issue = 2 | pages = 162 | year = 1990 | pmid = 2353332 }}</ref><ref>{{cite journal | vauthors = Regouby Y, Delomez G, Tisserant A | title = | language = fr | journal = Therapie | volume = 44 | issue = 5 | pages = 379–380 | year = 1989 | pmid = 2814922 }}</ref> when combined with ].<ref>{{cite book |title= Medical Toxicology| vauthors = Dart RC |year= 2003|isbn= 978-0-7817-2845-4|page= 889| publisher = Lippincott Williams & Wilkins }}</ref> | |||
| Death certificates show the number of zopiclone-related deaths is on the rise.<ref>{{cite journal | vauthors = Carlsten A, Waern M, Holmgren P, Allebeck P | title = The role of benzodiazepines in elderly suicides | journal = Scandinavian Journal of Public Health | volume = 31 | issue = 3 | pages = 224–228 | year = 2003 | pmid = 12850977 | doi = 10.1080/14034940210167966 | s2cid = 24102880 }}</ref> When taken alone, it usually is not fatal, but when mixed with alcohol or other drugs such as ], or in patients with respiratory, or hepatic disorders, the risk of a serious and fatal overdose increases.<ref>{{cite journal | vauthors = Harry P | title = | journal = La Revue du Praticien | volume = 47 | issue = 7 | pages = 731–735 | date = April 1997 | pmid = 9183949 }}</ref><ref>{{cite journal | vauthors = Bramness JG, Arnestad M, Karinen R, Hilberg T | title = Fatal overdose of zopiclone in an elderly woman with bronchogenic carcinoma | journal = Journal of Forensic Sciences | volume = 46 | issue = 5 | pages = 1247–1249 | date = September 2001 | pmid = 11569575 | doi = 10.1520/JFS15131J }}</ref> | |||
| Zopiclone is ] with ].<ref>{{cite journal |pmid=7862917 |url= |format= |year=1994 |month=Jun |author=Cohen, C; Sanger, Dj |title=Tolerance, cross-tolerance and dependence measured by operant responding in rats treated with triazolam via osmotic pumps. |volume=115 |issue=1-2 |pages=86–94 |issn=0033-3158 |journal=Psychopharmacology |doi=10.1007/BF02244756 }}</ref> Alcohol has cross tolerance with GABA<sub>A</sub> receptor positive modulators such as the ] and the ] drugs. For this reason alcoholics or recovering alcoholics may be at increased risk of ] on zopiclone. Also, alcoholics and drug abusers may be at increased risk of abusing and or becoming psychologically dependent on zopiclone. Zopiclone should be avoided in those with a history of ], ] (illicit or prescription misuse), or in those with history of ] or ] on ]-hypnotic drugs. | |||
| ==Interactions== | |||
| Withdrawing from Zopiclone sleeping tablets has been recommended to be done via a cross over to an equivalent dose of diazepam. This is because diazepam is available in low potency tablets, is cross-tolerant with zopiclone and is longer acting than zopiclone, which allows for a smoother withdrawal and for the body to adjust to a constant dose.<ref>http://www.cks.nhs.uk/benzodiazepine_and_z_drug_withdrawal/management/scenario_benzodiazepine_and_z_drug_withdrawal/view_full_scenario</ref><ref>http://www.benzo.org.uk/manual/</ref><ref></ref> While zopiclone acts on the same benzodiazepine receptors as the benzodiazepine family of drugs it is not classed as a ] (with which it shares a number of characteristics and effects) due to its differing molecular structure. Zopiclone is classed as a ] derivative.<ref>{{cite journal |pmid=7188374 |year=1982 |month= |author=Elie, R; Deschenes, Jp |title=Efficacy and tolerance of zopiclone in insomniac geriatric patients |volume=17 Suppl 2 |issue= |pages=179–87 |issn=0020-8272 |journal=International pharmacopsychiatry |url= |format= }}</ref> | |||
| Zopiclone also interacts with ] and ].<ref>{{cite journal | vauthors = Caille G, du Souich P, Spenard J, Lacasse Y, Vezina M | title = Pharmacokinetic and clinical parameters of zopiclone and trimipramine when administered simultaneously to volunteers | journal = Biopharmaceutics & Drug Disposition | volume = 5 | issue = 2 | pages = 117–125 | date = April 1984 | pmid = 6743780 | doi = 10.1002/bdd.2510050205 | doi-access = }}</ref><ref>{{cite journal | vauthors = Mattila ME, Mattila MJ, Nuotto E | title = Caffeine moderately antagonizes the effects of triazolam and zopiclone on the psychomotor performance of healthy subjects | journal = Pharmacology & Toxicology | volume = 70 | issue = 4 | pages = 286–289 | date = April 1992 | pmid = 1351673 | doi = 10.1111/j.1600-0773.1992.tb00473.x }}</ref> | |||
| Alcohol has an additive effect when combined with zopiclone, enhancing the adverse effects including the overdose potential of zopiclone significantly.<ref name="pmid2201724" /><ref>{{cite journal | vauthors = Koski A, Ojanperä I, Vuori E | title = Interaction of alcohol and drugs in fatal poisonings | journal = Human & Experimental Toxicology | volume = 22 | issue = 5 | pages = 281–287 | date = May 2003 | pmid = 12774892 | doi = 10.1191/0960327103ht324oa | bibcode = 2003HETox..22..281K | s2cid = 37777007 }}</ref> Due to these risks and the increased risk for dependence, alcohol should be avoided when using zopiclone.<ref name="pmid2201724">{{cite journal | vauthors = Kuitunen T, Mattila MJ, Seppala T | title = Actions and interactions of hypnotics on human performance: single doses of zopiclone, triazolam and alcohol | journal = International Clinical Psychopharmacology | volume = 5 | issue = Suppl 2 | pages = 115–130 | date = April 1990 | pmid = 2201724 }}</ref> | |||
| ==Carcinogenicity== | |||
| Zopiclone may be ] and ] according to rat, mice and hamster studies. At 100 mg per kg of bodyweight per day, the experimental dosage was considerably higher than the therapeutic dose for humans. The authors of an uncontrolled study of zopiclone said that it may take decades in ] people before carcinogenic effects from past zopiclone use develops. It was suggested that further research and monitoring was required into the potential for zopiclone to cause ] in immunocompetent patients.<ref>{{cite journal | journal = J Clin Oncol | date = November 1, 2005 | volume = 23 | issue = 31 | pages = 8134–6 | title = Incidence of cancer in individuals receiving chronic zopiclone or eszopiclone requires prospective study | doi = 10.1200/JCO.2005.03.5881 | author = Stebbing J | coauthors = Waters L, Davies L, Mandalia S, Nelson M, Gazzard B, Bower M | pmid = 16258120}}</ref> | |||
| ] appears to increase the absorption rate of zopiclone and prolong its ], leading to increased plasma levels and more pronounced effects. ] has a similar effect on zopiclone pharmacokinetics as erythromycin. The elderly may be particularly sensitive to the erythromycin and itraconazole ] with zopiclone. Temporary dosage reduction during combined therapy may be required, especially in the elderly.<ref>{{cite journal | vauthors = Aranko K, Luurila H, Backman JT, Neuvonen PJ, Olkkola KT | title = The effect of erythromycin on the pharmacokinetics and pharmacodynamics of zopiclone | journal = British Journal of Clinical Pharmacology | volume = 38 | issue = 4 | pages = 363–367 | date = October 1994 | pmid = 7833227 | pmc = 1364781 | doi = 10.1111/j.1365-2125.1994.tb04367.x }}</ref><ref>{{cite journal | vauthors = Jalava KM, Olkkola KT, Neuvonen PJ | title = Effect of itraconazole on the pharmacokinetics and pharmacodynamics of zopiclone | journal = European Journal of Clinical Pharmacology | volume = 51 | issue = 3–4 | pages = 331–334 | year = 1996 | pmid = 9010708 | doi = 10.1007/s002280050207 | s2cid = 20916689 }}</ref> | |||
| A recent analysis of both ] (FDA) data and clinical trial data shows that ] at prescribed doses cause an increased risk of developing ] in humans. There have been 15 ] which have shown that hypnotic drugs cause increased mortality, mainly due to increased cancer deaths. The cancers included those of the brain, lung, bowel, breast, and bladder. One possible explanation for the increased cancer deaths is that the Z-drugs have an adverse effect on the immune system. The fact that clinical trial subjects taking other Z-drugs (], ] and ]) had an increased rate of infections seems to support this theory. Benzodiazepine hypnotic agents are also associated with an increased risk of cancer in humans, namely ]. Development of ] has been associated with zolpidem usage, but the ] of neoplasm in zolpidem users is as yet unknown.<ref name="etnhcc2008"/> | |||
| ] causes a very notable reduction in half-life of zopiclone and peak plasma levels, which results in a large reduction in the hypnotic effect of zopiclone. ] and ] may also provoke similar interactions.<ref>{{cite journal | vauthors = Villikka K, Kivistö KT, Lamberg TS, Kantola T, Neuvonen PJ | title = Concentrations and effects of zopiclone are greatly reduced by rifampicin | journal = British Journal of Clinical Pharmacology | volume = 43 | issue = 5 | pages = 471–474 | date = May 1997 | pmid = 9159561 | pmc = 2042775 | doi = 10.1046/j.1365-2125.1997.00579.x }}</ref> ] and ] interfere with the metabolism of zopiclone.<ref>{{cite journal | vauthors = Becquemont L, Mouajjah S, Escaffre O, Beaune P, Funck-Brentano C, Jaillon P | title = Cytochrome P-450 3A4 and 2C8 are involved in zopiclone metabolism | journal = Drug Metabolism and Disposition | volume = 27 | issue = 9 | pages = 1068–1073 | date = September 1999 | pmid = 10460808 | url = http://dmd.aspetjournals.org/cgi/content/full/27/9/1068 | access-date = 2008-12-16 | archive-date = 2005-04-17 | archive-url = https://web.archive.org/web/20050417094458/http://dmd.aspetjournals.org/cgi/content/full/27/9/1068 | url-status = dead }}</ref> ] impairs the metabolism of zopiclone leading to increased zopiclone levels and marked next-day sedation.<ref>{{cite journal | vauthors = Alderman CP, Gebauer MG, Gilbert AL, Condon JT | title = Possible interaction of zopiclone and nefazodone | journal = The Annals of Pharmacotherapy | volume = 35 | issue = 11 | pages = 1378–1380 | date = November 2001 | pmid = 11724087 | doi = 10.1345/aph.1A074 | s2cid = 38894701 }}{{Dead link|date=February 2020 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> | |||
| ], another ] drug has also shown an increased rate of cancers in clinical trials. The review author concluded by saying: "The likelihood of cancer causation is sufficiently strong now that physicians and patients should be warned that hypnotics possibly place patients at higher risk for cancer".<ref name="etnhcc2008">{{cite journal | last = Kripke | first = Daniel F | year = 2008 | title = Evidence That New Hypnotics Cause Cancer | journal = Department of Psychiatry, UCSD | publisher = University of California | url = http://repositories.cdlib.org/cgi/viewcontent.cgi?article=1002&context=ucsdpsych | format = PDF | quote = the likelihood of cancer causation is sufficiently strong now that physicians and patients should be warned that hypnotics possibly place patients at higher risk for cancer. }}</ref> | |||
| ==Contraindications== | |||
| Zopiclone causes ] skills which are similar to benzodiazepines. Long term users of hypnotic drugs for ]s only develop partial tolerance to adverse effects on driving with users of hypnotic drugs even after 1 years use still showing an increased motor vehicle accident rate.<ref>{{cite journal |author=Staner L, Ertlé S, Boeijinga P, ''et al.'' |title=Next-day residual effects of hypnotics in DSM-IV primary insomnia: a driving simulator study with simultaneous electroencephalogram monitoring |journal=Psychopharmacology (Berl.) |volume=181 |issue=4 |pages=790–8 |year=2005 |month=October |pmid=16025317 |doi=10.1007/s00213-005-0082-8 |url=http://www.springerlink.com/content/q3742117g8140426/fulltext.pdf |format=PDF}}</ref> Patients who drive ] should not take zopiclone unless they stop driving due to a significant increased risk of ] in zopiclone users.<ref>{{cite journal |author=Barbone F, McMahon AD, Davey PG, ''et al.'' |title=Association of road-traffic accidents with benzodiazepine use |journal=Lancet |volume=352 |issue=9137 |pages=1331–6 |year=1998 |month=October |pmid=9802269 |doi= 10.1016/S0140-6736(98)04087-2|url=http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(98)04087-2/fulltext}}</ref> Zopiclone induces impairment of psychomotor function.<ref>{{cite journal |author=Yasui M |coauthors=Kato A, Kanemasa T, Murata S, Nishitomi K, Koike K, Tai N, Shinohara S, Tokomura M, Horiuchi M, Abe K |title= |volume=25 |issue=3 |pages=143–51 |month=June |year=2005 |pmid=16045197 |journal=Nihon Shinkei Seishin Yakurigaku Zasshi }}</ref><ref>{{cite journal |pmid=2278337 |url= |format= |year=1990 |month=Dec |author=Rettig, Hc; De, Haan, P; Zuurmond, Ww; Von, Leeuwen, L |title=Effects of hypnotics on sleep and psychomotor performance. A double-blind randomised study of lormetazepam, midazolam and zopiclone. |volume=45 |issue=12 |pages=1079–82 |issn=0003-2409 |journal=Anaesthesia |doi=10.1111/j.1365-2044.1990.tb14896.x }}</ref> Driving or operating machinery should be avoided after taking zopiclone as effects can carry over to the next day including impaired hand eye coordination.<ref>{{cite journal |pmid=7188379 |year=1982 |month= |author=Lader, M; Denney, Sc |title=A double-blind study to establish the residual effects of zopiclone on performance in healthy volunteers. |volume=17 Suppl 2 |issue= |pages=98–108 |issn=0020-8272 |journal=International pharmacopsychiatry }}</ref><ref>{{cite journal |pmid=3326113 |url= |year=1987 |month= |author=Billiard, M; Besset, A; De, Lustrac, C; Brissaud, L |title=Dose-response effects of zopiclone on night sleep and on nighttime and daytime functioning. |volume=10 Suppl 1 |issue= |pages=27–34 |issn=0161-8105 |journal=Sleep }}</ref> Patients with a history of substance abuse should not be prescribed zopiclone, as it has a very high potential for problematic drug misuse.<ref>{{cite journal |author=Bannan N, Rooney S, O'connor J |title=Zopiclone misuse: an update from Dublin |journal=Drug Alcohol Rev |volume=26 |issue=1 |pages=83–5 |year=2007 |month=January |pmid=17364840 |doi=10.1080/09595230601052777 |url=http://www.informaworld.com/smpp/content~db=all?content=10.1080/09595230601052777}}</ref> Zopiclone is known to, in some case, induce a state of amnesia, which is largely related (and not too dissimilar to 'sleep-walking'). This can extend to sleep-eating, sleep-talking (quite naturally), to dangerously 'sleep driving'. It is therefore usually not used as an anti-anxiety drug (such as ]), as the patient may be liable to make very poor judgment decisions (as they are essentially mentally 'asleep') and attempt dangerous activities. - With absolutely no recollection at all of the events.{{Citation needed|date=July 2011}} | |||
| ==Special precautions== | |||
| Alcohol should be avoided when using zopiclone as alcohol and zopiclone enhance the effects of each other and the risk of dependence could increase.<ref>{{cite journal |author=Kuitunen T |coauthors=Mattila MJ, Seppala T |title=Actions and interactions of hypnotics on human performance: single doses of zopiclone, triazolam and alcohol |volume=5 |issue=Suppl 2 |pages=115–30 |month=April |year=1990 |pmid=2201724 |journal=Int Clin Psychopharmacol }}</ref> | |||
| Patients with ] eliminate zopiclone much slower than normal patients and in addition experience exaggerated pharmacological effects of the drug.<ref>{{cite journal |pmid=6626417 |year=1983 |month=Sep |author=Parker, G; Roberts, Cj |title=Plasma concentrations and central nervous system effects of the new hypnotic agent zopiclone in patients with chronic liver disease. |volume=16 |issue=3 |pages=259–65 |issn=0306-5251 |pmc=1428012 |journal=British Journal of Clinical Pharmacology }}</ref> | |||
| Zopiclone increases sway and increases the number of falls in older people as well as cognitive side effects. Falls are a significant cause of death in older people.<ref>{{cite journal |pmid=8127419 |url= |format= |year=1994 |month= |author=Tada, K; Sato, Y; Sakai, T; Ueda, N; Kasamo, K; Kojima, T |title=Effects of zopiclone, triazolam, and nitrazepam on standing steadiness. |volume=29 |issue=1 |pages=17–22 |issn=0302-282X |journal=Neuropsychobiology |doi=10.1159/000119057 }}</ref><ref>{{cite journal |author=Allain H, Bentué-Ferrer D, Tarral A, Gandon JM |title=Effects on postural oscillation and memory functions of a single dose of zolpidem 5 mg, zopiclone 3.75 mg and lormetazepam 1 mg in elderly healthy subjects. A randomized, cross-over, double-blind study versus placebo |journal=Eur. J. Clin. Pharmacol. |volume=59 |issue=3 |pages=179–88 |year=2003 |month=July |pmid=12756510 |doi=10.1007/s00228-003-0591-5 |url=http://www.springerlink.com/content/kun2pr7nyfv8ua00/fulltext.pdf |format=PDF}}</ref><ref>{{cite journal |author=Antai-Otong D |title=The art of prescribing. Risks and benefits of non-benzodiazepine receptor agonists in the treatment of acute primary insomnia in older adults |journal=Perspect Psychiatr Care |volume=42 |issue=3 |pages=196–200 |year=2006 |month=August |pmid=16916422 |doi=10.1111/j.1744-6163.2006.00070.x |url=http://www3.interscience.wiley.com/journal/118727940/abstract}}</ref> | |||
| Patients who suffer from muscle weakness due to ] or have poor respiratory reserves due to severe ], ] or other lung disease, or have ] cannot safely take zopiclone, nor can a patient with any untreated abnormality of the ].<ref>{{cite book |last1=Upfal |first1=Jonathan |title=The Australian Drug Guide |edition=5 |year=2000 |origyear=1991 |publisher=Bookman Press Pty Ltd |location=Melbourne |isbn=1-86395-170-9 |page=743}}</ref> | |||
| ==Elderly== | |||
| Zopiclone, similar to other benzodiazepines and ] ] drugs causes impairments in body balance and standing steadiness in individuals who wake up at night or the next morning. Falls and hip fractures are frequently reported. The combination with alcohol increases these impairments. Partial, but incomplete tolerance develops to these impairments.<ref name="Mets-2010">{{Cite journal | last1 = Mets | first1 = MA. | last2 = Volkerts | first2 = ER. | last3 = Olivier | first3 = B. | last4 = Verster | first4 = JC. | title = Effect of hypnotic drugs on body balance and standing steadiness. | journal = Sleep Med Rev | volume = 14 | month = Feb | issue = 4 | pages = 259–67 | year = 2010 | doi = 10.1016/j.smrv.2009.10.008 | pmid = 20171127 }}</ref> | |||
| An extensive review of the medical literature regarding the management of insomnia and the elderly found that there is considerable evidence of the effectiveness and lasting benefits of non-drug treatments for insomnia. Compared with the benzodiazepines, the nonbenzodiazepine sedative-hypnotics, such as zopiclone, offer little if any advantages in efficacy or tolerability in elderly persons. It was found that newer agents such as the melatonin agonists may be more suitable and effective for the management of chronic insomnia in elderly people. Long-term use of sedative-hypnotics for insomnia lacks an evidence base and is discouraged for reasons that include concerns about such potential adverse drug effects as ] (]), daytime sedation, motor incoordination, and increased risk of motor vehicle accidents and falls. In addition, the effectiveness and safety of long-term use of ] ] remains to be determined. It was concluded that further research is needed to evaluate the long-term effects of treatment and the most appropriate management strategy for elderly persons with chronic insomnia.<ref>{{cite journal | journal = Am J Geriatr Pharmacother | year = 2006 | month = June | volume = 4 | issue = 2 | pages = 168–92 | title = Management of chronic insomnia in elderly persons | author = Bain KT | pmid = 16860264 | doi = 10.1016/j.amjopharm.2006.06.006}}</ref> | |||
| ==Pharmacology== | ==Pharmacology== | ||
| The therapeutic pharmacological properties of zopiclone include ], ], ] and ] properties.<ref>{{cite journal | |
The therapeutic pharmacological properties of zopiclone include ], ], ], and ] properties.<ref>{{cite journal | vauthors = Röschke J, Mann K, Aldenhoff JB, Benkert O | title = Functional properties of the brain during sleep under subchronic zopiclone administration in man | journal = European Neuropsychopharmacology | volume = 4 | issue = 1 | pages = 21–30 | date = March 1994 | pmid = 8204993 | doi = 10.1016/0924-977X(94)90311-5 | s2cid = 40503805 }}</ref> Zopiclone and benzodiazepines bind to the same sites on GABA<sub>A</sub> receptors, causing an enhancement of the actions of ] to produce the therapeutic and adverse effects of zopiclone. The metabolite of zopiclone ] is also pharmacologically active, although it has predominately anxiolytic properties. One study found some slight selectivity for zopiclone on α1 and α5 subunits,<ref>{{cite journal | vauthors = Petroski RE, Pomeroy JE, Das R, Bowman H, Yang W, Chen AP, Foster AC | title = Indiplon is a high-affinity positive allosteric modulator with selectivity for alpha1 subunit-containing GABAA receptors | journal = The Journal of Pharmacology and Experimental Therapeutics | volume = 317 | issue = 1 | pages = 369–377 | date = April 2006 | pmid = 16399882 | doi = 10.1124/jpet.105.096701 | s2cid = 46510829 }}</ref> although it is regarded as being unselective in its binding to GABA<sub>A</sub> receptors containing α1, α2, α3, and α5 subunits. Desmethylzopiclone has been found to have ] properties, unlike the parent drug zopiclone, which is a full agonist.<ref>{{cite journal | vauthors = Atack JR | title = Anxioselective compounds acting at the GABA(A) receptor benzodiazepine binding site | journal = Current Drug Targets. CNS and Neurological Disorders | volume = 2 | issue = 4 | pages = 213–232 | date = August 2003 | pmid = 12871032 | doi = 10.2174/1568007033482841 }}</ref> The ] of zopiclone is similar to benzodiazepines, with similar effects on ] and on ] and ] turnover.<ref>{{cite journal | vauthors = Liu HJ, Sato K, Shih HC, Shibuya T, Kawamoto H, Kitagawa H | title = Pharmacologic studies of the central action of zopiclone: effects on locomotor activity and brain monoamines in rats | journal = International Journal of Clinical Pharmacology, Therapy, and Toxicology | volume = 23 | issue = 3 | pages = 121–128 | date = March 1985 | pmid = 2581904 }}</ref><ref>{{cite journal | vauthors = Sato K, Hong YL, Yang MS, Shibuya T, Kawamoto H, Kitagawa H | title = Pharmacologic studies of central actions of zopiclone: influence on brain monoamines in rats under stressful condition | journal = International Journal of Clinical Pharmacology, Therapy, and Toxicology | volume = 23 | issue = 4 | pages = 204–210 | date = April 1985 | pmid = 2860074 }}</ref> | ||
| A ] of randomised controlled ] |
A ] of randomised controlled ] that compared benzodiazepines to zopiclone or other Z drugs such as zolpidem and zaleplon has found few clear and consistent differences between zopiclone and the benzodiazepines in ], total sleep duration, number of awakenings, quality of sleep, adverse events, tolerance, rebound insomnia, and daytime alertness.<ref>{{cite journal | vauthors = Dündar Y, Dodd S, Strobl J, Boland A, Dickson R, Walley T | title = Comparative efficacy of newer hypnotic drugs for the short-term management of insomnia: a systematic review and meta-analysis | journal = Human Psychopharmacology | volume = 19 | issue = 5 | pages = 305–322 | date = July 2004 | pmid = 15252823 | doi = 10.1002/hup.594 | s2cid = 10888200 }}</ref> | ||
| Zopiclone is in the ] family of drugs. Other cyclopyrrolone drugs include ]. Zopiclone although molecularly different from benzodiazepines, shares an almost identical pharmacological profile as benzodiazepines including anxiolytic properties. Its mechanism of action is |
Zopiclone is in the ] family of drugs. Other cyclopyrrolone drugs include ]. Zopiclone, although molecularly different from benzodiazepines, shares an almost identical pharmacological profile as benzodiazepines, including anxiolytic properties. Its mechanism of action is by binding to the benzodiazepine site and acting as a ], which in turn positively modulates benzodiazepine-sensitive GABA<sub>A</sub> receptors and enhances GABA binding at the GABA<sub>A</sub> receptors to produce zopiclone's pharmacological properties.<ref>{{cite journal | vauthors = Blanchard JC, Julou L | title = Suriclone: a new cyclopyrrolone derivative recognizing receptors labeled by benzodiazepines in rat hippocampus and cerebellum | journal = Journal of Neurochemistry | volume = 40 | issue = 3 | pages = 601–607 | date = March 1983 | pmid = 6298365 | doi = 10.1111/j.1471-4159.1983.tb08023.x | s2cid = 35732735 }}</ref><ref>{{cite journal | vauthors = Skerritt JH, Johnston GA | title = Enhancement of GABA binding by benzodiazepines and related anxiolytics | journal = European Journal of Pharmacology | volume = 89 | issue = 3–4 | pages = 193–198 | date = May 1983 | pmid = 6135616 | doi = 10.1016/0014-2999(83)90494-6 }}</ref><ref>{{cite journal | vauthors = De Deyn PP, Macdonald RL | title = Effects of non-sedative anxiolytic drugs on responses to GABA and on diazepam-induced enhancement of these responses on mouse neurones in cell culture | journal = British Journal of Pharmacology | volume = 95 | issue = 1 | pages = 109–120 | date = September 1988 | pmid = 2905900 | pmc = 1854132 | doi = 10.1111/j.1476-5381.1988.tb16554.x }}</ref> In addition to zopiclone's benzodiazepine pharmacological properties, it also has some ]-like properties.<ref>{{cite journal | vauthors = Julou L, Bardone MC, Blanchard JC, Garret C, Stutzmann JM | title = Pharmacological studies on zopiclone | journal = Pharmacology | volume = 27 | issue = Suppl 2 | pages = 46–58 | year = 1983 | pmid = 6142468 | doi = 10.1159/000137911 }}</ref><ref>{{cite journal | vauthors = Blanchard JC, Boireau A, Julou L | title = Brain receptors and zopiclone | journal = Pharmacology | volume = 27 | issue = Suppl 2 | pages = 59–69 | year = 1983 | pmid = 6322210 | doi = 10.1159/000137912 }}</ref> | ||
| ===Pharmacokinetics=== | |||
| In ] studies, zopiclone significantly increases the energy of the beta frequency band and shows characteristics of high-voltage slow waves, desynchronization of hippocampal theta waves and an increase in the energy of the delta frequency band. Zopiclone increases both stage 2 and slow wave sleep (SWS), while ], an α1-selective compound, increases only SWS and causes no effect on stage 2 sleep. Zopiclone is less selective to the α1 site and has higher affinity to the α2 site than ]. Zopiclone is therefore very similar pharmacologically to benzodiazepines.<ref>{{cite journal | author = Noguchi H | coauthors = Kitazumi K, Mori M, Shiba T. | year = 2004 | month = March | title = Electroencephalographic properties of zaleplon, a non-benzodiazepine sedative/hypnotic, in rats | journal = J Pharmacol Sci. | volume = 94 | issue = 3 |pages = 246–51 | pmid = 15037809 | url = http://www.jstage.jst.go.jp/article/jphs/94/3/246/_pdf | format = pdf | doi = 10.1254/jphs.94.246 }}</ref> | |||
| ]{{clear left}} | |||
| After oral administration, zopiclone is rapidly absorbed, with a ] around 75–80%. Time to peak plasma concentration is 1–2 hours. A high-fat meal preceding zopiclone administration does not change absorption (as measured by ]), but reduces peak plasma levels and delays its occurrence, thus may delay the onset of therapeutic effects. | |||
| The plasma protein-binding of zopiclone has been reported to be weak, between 45 and 80% (mean 52–59%). It is rapidly and widely distributed to body tissues, including the brain, and is excreted in urine, saliva, and ]. Zopiclone is partly extensively metabolized in the liver to form an active ''N''-demethylated derivative (''N''-desmethylzopiclone) and an inactive zopiclone-''N''-oxide. Hepatic enzymes playing the most significant role in zopiclone metabolism are ] and ]. In addition, about 50% of the administered dose is decarboxylated and excreted via the lungs. In urine, the ''N''-demethyl and ''N''-oxide metabolites account for 30% of the initial dose. Between 7 and 10% of zopiclone is recovered from the urine, indicating extensive metabolism of the drug before excretion. The terminal elimination half-life of zopiclone ranges from 3.5 to 6.5 hours (5 hours on average).<ref name = "Assessment" /> | |||
| ==EEG and sleep== | |||
| Similar to other sedative hypnotic drugs zopiclone causes a decrease in the core ] and is effective in decreasing ].<ref>{{cite journal |author=Holmes AL, Gilbert SS, Dawson D |title=Melatonin and zopiclone: the relationship between sleep propensity and body temperature |journal=Sleep |volume=25 |issue=3 |pages=301–6 |year=2002 |month=May |pmid=12003160 |doi= |url=}}</ref> Zopiclone causes similar alterations on EEG readings and ] as benzodiazepines and causes disturbances in sleep architecture on withdrawal as part of its ].<ref>{{cite journal |author=Trachsel L, Dijk DJ, Brunner DP, Klene C, Borbély AA |title=Effect of zopiclone and midazolam on sleep and EEG spectra in a phase-advanced sleep schedule |journal=Neuropsychopharmacology |volume=3 |issue=1 |pages=11–8 |year=1990 |month=February |pmid=2306331 |doi= |url=}}</ref><ref>{{cite journal |author=Mann K, Bauer H, Hiemke C, Röschke J, Wetzel H, Benkert O |title=Acute, subchronic and discontinuation effects of zopiclone on sleep EEG and nocturnal melatonin secretion |journal=Eur Neuropsychopharmacol |volume=6 |issue=3 |pages=163–8 |year=1996 |month=August |pmid=8880074 |doi= 10.1016/0924-977X(96)00014-4|url=http://linkinghub.elsevier.com/retrieve/pii/0924-977X(96)00014-4}}</ref> Zopiclone reduces both delta waves and the number of high-amplitude delta waves whilst increasing low-amplitude waves.<ref>{{cite journal |author=Wright NA, Belyavin A, Borland RG, Nicholson AN |title=Modulation of delta activity by hypnotics in middle-aged subjects: studies with a benzodiazepine (flurazepam) and a cyclopyrrolone (zopiclone) |journal=Sleep |volume=9 |issue=2 |pages=348–52 |year=1986 |month=June |pmid=3505734 |doi= |url=}}</ref> Zopiclone reduces the total amount of time spent in ] as well as delaying its onset.<ref>{{cite journal |author=Kim YD, Zhuang HY, Tsutsumi M, Okabe A, Kurachi M, Kamikawa Y |title=Comparison of the effect of zopiclone and brotizolam on sleep EEG by quantitative evaluation in healthy young women |journal=Sleep |volume=16 |issue=7 |pages=655–61 |year=1993 |month=October |pmid=8290860 |doi= |url=}}</ref><ref>{{cite journal |author=Kanno O, Watanabe H, Kazamatsuri H |title=Effects of zopiclone, flunitrazepam, triazolam and levomepromazine on the transient change in sleep-wake schedule: polygraphic study, and the evaluation of sleep and daytime condition |journal=Prog. Neuropsychopharmacol. Biol. Psychiatry |volume=17 |issue=2 |pages=229–39 |year=1993 |month=March |pmid=8430216 |doi= 10.1016/0278-5846(93)90044-S|url=}}</ref> ] has been found to be superior to zopiclone in the treatment of insomnia and has been found to have lasting effects on sleep quality for at least a year after therapy.<ref>{{cite journal |author= |title=Cognitive therapy superior to zopiclone for insomnia |journal=J Fam Pract |volume=55 |issue=10 |pages=845 |year=2006 |month=October |pmid=17089469 |doi= |url=}}</ref><ref>{{cite journal |author=Baillargeon L, Landreville P, Verreault R, Beauchemin JP, Grégoire JP, Morin CM |title=Discontinuation of benzodiazepines among older insomniac adults treated with cognitive-behavioural therapy combined with gradual tapering: a randomized trial |journal=CMAJ |volume=169 |issue=10 |pages=1015–20 |year=2003 |month=November |pmc=236226 |doi= |url=http://www.cmaj.ca/cgi/content/full/169/10/1015 |pmid=14609970}}</ref><ref>{{cite journal |author=Sivertsen B, Omvik S, Pallesen S, ''et al.'' |title=Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial |journal=JAMA |volume=295 |issue=24 |pages=2851–8 |year=2006 |month=June |pmid=16804151 |doi=10.1001/jama.295.24.2851 |url=http://jama.ama-assn.org/cgi/content/full/295/24/2851}}</ref><ref>{{cite journal |author=Morgan K |coauthors=Dixon S, Mathers N, Thompson J, Tomeny M |year=2004 |month=Feb |title=Psychological treatment for insomnia in the regulation of long-term hypnotic drug use |journal=Health Technol Assess |volume=8 |issue=8 |pages=1–68 |publisher=National Institute for Health Research |pmid=14960254 |url=http://www.hta.ac.uk/fullmono/mon808.pdf |format=PDF}}</ref> | |||
| The ] of zopiclone in humans are ]. After oral administration of the ], C<sub>max</sub> (time to maximum plasma concentration), area under the plasma time-concentration curve (]) and ] values are higher for the ] ]s, owing to the slower total clearance and smaller ] (corrected by the bioavailability), compared with the levorotatory enantiomer. In urine, the concentrations of the dextrorotatory enantiomers of the ''N''-demethyl and ''N''-oxide metabolites are higher than those of the respective ]. | |||
| ==Pharmacokinetics== | |||
| After oral administration, zopiclone is rapidly absorbed, with a bioavailability of approximately 80%. The plasma protein binding of zopiclone has been reported to be between 45 and 80%. Zopiclone is rapidly and widely distributed to body tissues including the brain, and is excreted in urine, saliva and ]. Zopiclone is partly metabolised in the liver to form an inactive N-demethylated derivative and an active N-oxide metabolite. In addition, approximately 50% of the administered dose is decarboxylated and excreted via the lungs. In urine, the N-demethyl and N-oxide metabolites account for 30% of the initial dose. Between 7 and 10% of zopiclone is recovered from the urine indicating extensive ] of the drug before excretion. The terminal elimination half-life (t1/2z) of zopiclone ranges from 3.5 to 6.5 hours. The ] of zopiclone in humans are stereoselective. After oral administration of the racemic mixture, Cmax (time to maximum plasma concentration), AUC (area under the plasma time-concentration curve) and t1/2z values are higher for the dextrorotatory enantiomer owing to the slower total clearance and smaller ] (corrected by the bioavailability), compared with the levorotatory enantiomer. In urine, the concentrations of the dextrorotatory enantiomers of the N-demethyl and N-oxide metabolites are higher than those of the respective antipodes. The pharmacokinetics of zopiclone are altered by aging and are influenced by renal and hepatic functions.<ref>{{cite journal |pmid=7188377 |year=1982 |month= |author=Gaillot, J; Heusse, D; Hougton, Gw; Marc, Aurele, J; Dreyfus, Jf |title=Pharmacokinetics and metabolism of zopiclone. |volume=17 Suppl 2 |issue= |pages=76–91 |issn=0020-8272 |journal=International pharmacopsychiatry }}</ref> | |||
| The pharmacokinetics of zopiclone are altered by aging and are influenced by renal and hepatic functions.<ref>{{cite journal | vauthors = Gaillot J, Heusse D, Hougton GW, Marc Aurele J, Dreyfus JF | title = Pharmacokinetics and metabolism of zopiclone | journal = International Pharmacopsychiatry | volume = 17 | issue = Suppl 2 | pages = 76–91 | year = 1982 | pmid = 7188377 }}</ref> In severe chronic ], the area under the curve value for zopiclone was larger and the half-life associated with the elimination rate constant longer, but these changes were not considered to be clinically significant.<ref>{{cite journal | vauthors = Viron B, De Meyer M, Le Liboux A, Frydman A, Maillard F, Mignon F, Gaillot J | title = Steady state pharmacokinetics of zopiclone during multiple oral dosing (7.5 mg nocte) in patients with severe chronic renal failure | journal = International Clinical Psychopharmacology | volume = 5 | issue = Suppl 2 | pages = 95–104 | date = April 1990 | pmid = 2387982 }}</ref> Sex and race have not been found to interact with pharmacokinetics of zopiclone.<ref name = "Assessment" /> | |||
| ==Interactions== | |||
| Zopiclone also interacts with ] and ].<ref>{{cite journal |pmid=6743780 |year=1984 |month=Apr |author=Caille, G; Du, Souich, P; Spenard, J; Lacasse, Y; Vezina, M |title=Pharmacokinetic and clinical parameters of zopiclone and trimipramine when administered simultaneously to volunteers. |volume=5 |issue=2 |pages=117–25 |issn=0142-2782 |journal=Biopharmaceutics & drug disposition |doi=10.1002/bdd.2510050205 }}</ref><ref>{{cite journal |pmid=1351673 |url= |format= |year=1992 |month=Apr |author=Mattila, Me; Mattila, Mj; Nuotto, E |title=Caffeine moderately antagonizes the effects of triazolam and zopiclone on the psychomotor performance of healthy subjects. |volume=70 |issue=4 |pages=286–9 |issn=0901-9928 |journal=Pharmacology & toxicology |doi=10.1111/j.1600-0773.1992.tb00473.x }}</ref> | |||
| Alcohol has an additive effect when combined with zopiclone, enhancing the adverse effects including the overdose potential of zopiclone significantly.<ref>{{cite journal |pmid=2201724 |url= | format= |year=1990 |month=Apr |author=Kuitunen, T; Mattila, Mj; Seppala, T |title=Actions and interactions of hypnotics on human performance: single doses of zopiclone, triazolam and alcohol. |volume=5 Suppl 2 |issue= |pages=115–30 |issn=0268-1315 |journal=International clinical psychopharmacology }}</ref><ref>{{cite journal |author=Koski A, Ojanperä I, Vuori E |title=Interaction of alcohol and drugs in fatal poisonings |journal=Hum Exp Toxicol |volume=22 |issue=5 |pages=281–7 |year=2003 |month=May |pmid=12774892 |doi= 10.1191/0960327103ht324oa|url=}}</ref> ] appears to increase the absorption rate of zopiclone and prolong the ] of zopiclone leading to increased plasma levels and more pronounced effects. ] has a similar effect on zopiclone pharmacokinetics as erythromycin. The elderly may be particularly sensitive to the erythromycin and itraconazole ] with zopiclone. Temporary dosage reduction during combined therapy may be required especially in the elderly.<ref>{{cite journal |pmid=7833227 |year=1994 |month=Oct |author=Aranko, K; Luurila, H; Backman, Jt; Neuvonen, Pj; Olkkola, Kt |title=The effect of erythromycin on the pharmacokinetics and pharmacodynamics of zopiclone. |volume=38 |issue=4 |pages=363–7 |issn=0306-5251 |pmc=1364781 |journal=British Journal of Clinical Pharmacology }}</ref><ref>{{cite journal |author=Jalava KM, Olkkola KT, Neuvonen PJ |title=Effect of itraconazole on the pharmacokinetics and pharmacodynamics of zopiclone |journal=Eur. J. Clin. Pharmacol. |volume=51 |issue=3-4 |pages=331–4 |year=1996 |pmid=9010708 |doi= 10.1007/s002280050207|url=}}</ref> | |||
| ] causes a very notable reduction in half-life of zopiclone and peak plasma levels which results in a large reduction in the ] effect of zopiclone. ] and ] may also provoke similar interactions.<ref>{{cite journal |author=Villikka K, Kivistö KT, Lamberg TS, Kantola T, Neuvonen PJ |title=Concentrations and effects of zopiclone are greatly reduced by rifampicin |journal=Br J Clin Pharmacol |volume=43 |issue=5 |pages=471–4 |year=1997 |month=May |pmid=9159561 |pmc=2042775 |doi= 10.1046/j.1365-2125.1997.00579.x|url=}}</ref> ] and ] interfere with the metabolism of zopiclone.<ref>{{cite journal |author=Becquemont L, Mouajjah S, Escaffre O, Beaune P, Funck-Brentano C, Jaillon P |title=Cytochrome P-450 3A4 and 2C8 are involved in zopiclone metabolism |journal=Drug Metab. Dispos. |volume=27 |issue=9 |pages=1068–73 |year=1999 |month=September |pmid=10460808 |doi= |url=http://dmd.aspetjournals.org/cgi/content/full/27/9/1068}}</ref> ] impairs the metabolism of zopiclone leading to increased zopiclone levels and marked next day sedation.<ref>{{cite journal |author=Alderman CP, Gebauer MG, Gilbert AL, Condon JT |title=Possible interaction of zopiclone and nefazodone |journal=Ann Pharmacother |volume=35 |issue=11 |pages=1378–80 |year=2001 |month=November |pmid=11724087 |doi= 10.1345/aph.1A074|url=http://www.theannals.com/cgi/pmidlookup?view=long&pmid=11724087}}</ref> | |||
| == |
==Chemistry== | ||
| The ] of zopiclone is 178 °C.<ref name="Pubchem Zopiclone">{{cite web |title=Zopiclone |url=https://pubchem.ncbi.nlm.nih.gov/compound/5735 |website=pubchem.ncbi.nlm.nih.gov |publisher=U.S. National Library of Medicine |access-date=11 June 2018 |language=en}}</ref> Zopiclone's solubility in water, at room temperature (25 °C) are 0.151 mg/mL.<ref name="Pubchem Zopiclone" /> The ] value of zopiclone is 0.8.<ref name="Pubchem Zopiclone" /> | |||
| Zopiclone is a drug with the potential for misuse with the potential for causing dosage escalation, ] and ]. Zopiclone is well known amongst drug addicts as a drug of abuse and they commonly seek it from their doctors. {{citation needed|date=September 2012}} It is abused orally and sometimes intravenously and often combined with alcohol to achieve a combined sedative hypnotic - alcohol euphoria. Patients who do abuse the drug are also at risk of ]. Withdrawal symptoms can be seen after long term use of normal doses even after a gradual reduction regime. The Compendium of Pharmaceuticals and Specialties recommends that zopiclone prescriptions do not exceed 7 – 10 days due to concerns of ], ] and ].<ref>{{cite journal |author=Cimolai N |title=Zopiclone: is it a pharmacologic agent for abuse? |journal=Can Fam Physician |volume=53 |issue=12 |pages=2124–9 |year=2007 |month=December |pmid=18077750 |pmc=2231551 |doi= }}</ref> Two types of drug misuse can occur; either recreational misuse, where the drug is taken to achieve a high, or when the drug is continued long term against medical advice.<ref>{{cite journal |author=Griffiths RR, Johnson MW |title=Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds |journal=J Clin Psychiatry |volume=66 Suppl 9 |issue= |pages=31–41 |year=2005 |pmid=16336040 |doi= |url=}}</ref><ref>{{cite journal |author=Hoffmann F, Pfannkuche M, Glaeske G |title= |language=German |journal=Nervenarzt |volume=79 |issue=1 |pages=67–72 |year=2008 |month=January |pmid=17457554 |doi=10.1007/s00115-007-2280-6}}</ref> Zopiclone may be more addictive than ].<ref>{{cite journal |author=Bramness JG, Olsen H |title= |language=Norwegian |journal=Tidsskr. Nor. Laegeforen. |volume=118 |issue=13 |pages=2029–32 |year=1998 |month=May |pmid=9656789 |doi= |url=}}</ref> Those with a history of ] or ] may be at an increased risk of high dose zopiclone misuse.<ref>{{cite journal |author=Ströhle A, Antonijevic IA, Steiger A, Sonntag A |title= |language=German |journal=Nervenarzt |volume=70 |issue=1 |pages=72–5 |year=1999 |month=January |pmid=10087521 |doi= 10.1007/s001150050403|url= }}</ref> High dose misuse of zopiclone and increasing popularity amongst drug abusers who have been prescribed with zopiclone<ref>{{cite journal |author=Sikdar S |title=Physical dependence on zopiclone. Prescribing this drug to addicts may give rise to iatrogenic drug misuse |journal=BMJ |volume=317 |issue=7151 |pages=146 |year=1998 |month=July |pmid=9657802 |pmc=1113504 |doi= |url=http://bmj.com/cgi/pmidlookup?view=long&pmid=9657802}}</ref> The symptoms of zopiclone ] can include ], ], ], slow thoughts, ], ], ] and ].<ref>{{cite journal |author=Kuntze MF, Bullinger AH, Mueller-Spahn F |title=Excessive use of zopiclone: a case report |journal=Swiss Med Wkly |volume=132 |issue=35-36 |pages=523 |year=2002 |month=September |pmid=12506335 |url=http://www.smw.ch/docs/pdf200x/2002/35/smw-10074.pdf |format=PDF}}</ref> | |||
| ===Detection in biological fluids=== | |||
| Zopiclone and other sedative hypnotic drugs are detected frequently in cases of people suspected of driving under the influence of drugs. Other drugs including the ] and ] are also found in high numbers of suspected drugged drivers. Many drivers have blood levels far exceeding the therapeutic dose range and often in combination with other alcohol, illegal or ]s of abuse suggesting a high degree of abuse potential for ], ] and zopiclone.<ref>{{cite journal | author = Jones AW | coauthors = Holmgren A, Kugelberg FC. | year = 2007 | month = April | title = Concentrations of scheduled prescription drugs in blood of impaired drivers: considerations for interpreting the results | volume = 29 | issue = 2 | pages = 248–60 | pmid = 17417081 | journal = Ther Drug Monit. | doi = 10.1097/FTD.0b013e31803d3c04}}</ref><ref>{{cite journal |author=Bramness JG, Skurtveit S, Mørland J |title= |language=Norwegian |journal=Tidsskr. Nor. Laegeforen. |volume=119 |issue=19 |pages=2820–1 |year=1999 |month=August |pmid=10494203 |doi= |url=}}</ref> Zopiclone which at prescribed doses causes moderate impairment the next day has been estimated to increase the risk of vehicle accidents by 50%, causing an increase of 503 excess accidents per 100,000 persons. It was recommended that ] or other non-impairing sleep aids are used instead of zopiclone to reduce ].<ref>{{cite journal |author=Menzin J, Lang KM, Levy P, Levy E |title=A general model of the effects of sleep medications on the risk and cost of motor vehicle accidents and its application to France |journal=PharmacoEconomics |volume=19 |issue=1 |pages=69–78 |year=2001 |month=January |pmid=11252547 |doi= 10.2165/00019053-200119010-00005|url=}}</ref> Zopiclone as with other ] drugs is sometimes abused to carry out criminal acts such as ].<ref>{{cite journal |author=Kintz P, Villain M, Ludes B |title=Testing for the undetectable in drug-facilitated sexual assault using hair analyzed by tandem mass spectrometry as evidence |journal=Ther Drug Monit |volume=26 |issue=2 |pages=211–4 |year=2004 |month=April |pmid=15228167 |doi= 10.1097/00007691-200404000-00022|url=}}</ref> | |||
| Zopiclone may be measured in blood, plasma, or urine by chromatographic methods. Plasma concentrations are typically less than 100 μg/L during therapeutic use, but frequently exceed 100 μg/L in automotive vehicle operators arrested for impaired driving ability and may exceed 1000 μg/L in acutely poisoned patients. ''Post mortem'' blood concentrations are usually in a range of 400 to 3900 μg/L in victims of fatal acute overdose.<ref name="pmid15329838">{{cite journal | vauthors = Kratzsch C, Tenberken O, Peters FT, Weber AA, Kraemer T, Maurer HH | title = Screening, library-assisted identification and validated quantification of 23 benzodiazepines, flumazenil, zaleplone, zolpidem and zopiclone in plasma by liquid chromatography/mass spectrometry with atmospheric pressure chemical ionization | journal = Journal of Mass Spectrometry | volume = 39 | issue = 8 | pages = 856–72 | date = August 2004 | pmid = 15329838 | doi = 10.1002/jms.599 | bibcode = 2004JMSp...39..856K }}</ref><ref name="pmid19393793">{{cite journal | vauthors = Gustavsen I, Al-Sammurraie M, Mørland J, Bramness JG | title = Impairment related to blood drug concentrations of zopiclone and zolpidem compared to alcohol in apprehended drivers | journal = Accident Analysis and Prevention | volume = 41 | issue = 3 | pages = 462–6 | date = May 2009 | pmid = 19393793 | doi = 10.1016/j.aap.2009.01.011 }}</ref><ref>{{cite book | vauthors = Baselt R | title = Disposition of Toxic Drugs and Chemicals in Man | edition = 8th | publisher = Biomedical Publications | location = Foster City, CA | date = 2008 | pages = 1677–1679 }}</ref> | |||
| ==History== | |||
| Zopiclone has cross tolerance with barbiturates and is able to suppress barbiturate withdrawal signs. Zopiclone is frequently self administered intravenously in studies on monkeys suggesting a high risk of abuse potential.<ref>{{cite journal | author = Yanagita T. | coauthors = | year = 1982 | month = | title = Dependence potential of zopiclone studied in monkeys | journal = International pharmacopsychiatry. | volume = 17 | issue = 2 | pages = 216–27 | pmid = 6892368 }}</ref> | |||
| Zopiclone was developed and first introduced in 1986 by ] S.A., now part of ], the main worldwide manufacturer. Initially, it was promoted as an improvement on benzodiazepines, but a recent meta-analysis found it was no better than benzodiazepines in any of the aspects assessed.<ref>{{cite journal |vauthors=Holbrook AM, Crowther R, Lotter A, Cheng C, King D |title=Meta-analysis of benzodiazepine use in the treatment of insomnia |journal=CMAJ |volume=162 |issue=2 |pages=225–233 |date=January 2000 |pmid=10674059 |pmc=1232276 }}</ref> On April 4, 2005, the U.S. ] listed zopiclone under ], due to evidence that the drug has ] properties similar to benzodiazepines. | |||
| Zopiclone, as traditionally sold worldwide, is a ] mixture of two ]s, only one of which is active.<ref>{{cite journal | vauthors = Blaschke G, Hempel G, Müller WE | title = Preparative and analytical separation of the zopiclone enantiomers and determination of their affinity to the benzodiazepine receptor binding site | journal = Chirality | volume = 5 | issue = 6 | pages = 419–421 | year = 1993 | pmid = 8398600 | doi = 10.1002/chir.530050605 }}</ref><ref>{{cite journal | vauthors = Fernandez C, Maradeix V, Gimenez F, Thuillier A, Farinotti R | title = Pharmacokinetics of zopiclone and its enantiomers in Caucasian young healthy volunteers | journal = Drug Metabolism and Disposition | volume = 21 | issue = 6 | pages = 1125–1128 | date = November 1993 | pmid = 7905394 }}</ref> In 2005, the pharmaceutical company ] of ], began marketing the active stereoisomer ] under the name Lunesta in the United States. This had the consequence of placing what is a ] in most of the world under patent control in the United States. Generic forms of Lunesta have since become available in the United States. Zopiclone is currently available off-patent in a number of European countries, Brazil, Canada, Hong Kong, and New Zealand. The eszopiclone/zopiclone difference is in the dosage—the strongest eszopiclone dosage contains 3 mg of the therapeutic stereoisomer, whereas the highest zopiclone dosage (10 mg) contains 5 mg of the active stereoisomer{{Citation needed|date=June 2020}}. The two agents have not yet{{When||date=June 2023}} been studied in head-to-head clinical trials to determine the existence of any potential clinical differences (efficacy, side effects, developing dependence on the drug, safety, etc.). | |||
| Zopiclone is in the top ten medications obtained using false prescription in France.<ref name=whoaoz/> | |||
| ==Society and culture== | |||
| However, due to its distinctly bitter taste it is unlikely to be covertly administered to facilitate drug-related crime such as robbery, sexual assault etc. The tablets are coated with a film to mask the taste when swallowed, but crushing destroys this film. Also, a common side-effect is a bitter, metallic taste following ingestion, so a person who has administered zopiclone is likely to be aware that they are under the influence of this drug. | |||
| ===Recreational use=== | |||
| Zopiclone has the potential for non-medical use, dosage escalation, and drug dependence. It is taken orally and sometimes intravenously when used non-medically, and often combined with alcohol to achieve euphoria. Patients abusing the drug are also at risk of dependence. Withdrawal symptoms can be seen after long-term use of normal doses even after a gradual reduction regimen. The Compendium of Pharmaceuticals and Specialties recommends zopiclone prescriptions not exceed 7 to 10 days, owing to concerns of addiction, tolerance, and physical dependence.<ref>{{cite journal | vauthors = Cimolai N | title = Zopiclone: is it a pharmacologic agent for abuse? | journal = Canadian Family Physician | volume = 53 | issue = 12 | pages = 2124–2129 | date = December 2007 | pmid = 18077750 | pmc = 2231551 }}</ref> Two types of drug misuse can occur: either recreational misuse, wherein the drug is taken to achieve a high, or when the drug is continued long-term against medical advice.<ref>{{cite journal | vauthors = Griffiths RR, Johnson MW | title = Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds | journal = The Journal of Clinical Psychiatry | volume = 66 | issue = Suppl 9 | pages = 31–41 | year = 2005 | pmid = 16336040 }}</ref><ref>{{cite journal | vauthors = Hoffmann F, Pfannkuche M, Glaeske G | title = | language = de | journal = Der Nervenarzt | volume = 79 | issue = 1 | pages = 67–72 | date = January 2008 | pmid = 17457554 | doi = 10.1007/s00115-007-2280-6 | s2cid = 31103719 }}</ref> Zopiclone may be more addictive than ].<ref>{{cite journal | vauthors = Bramness JG, Olsen H | title = | language = no | journal = Tidsskrift for den Norske Laegeforening | volume = 118 | issue = 13 | pages = 2029–2032 | date = May 1998 | pmid = 9656789 }}</ref> Those with a history of ] or ] may be at an increased risk of high-dose zopiclone misuse.<ref>{{cite journal | vauthors = Ströhle A, Antonijevic IA, Steiger A, Sonntag A | title = | language = de | journal = Der Nervenarzt | volume = 70 | issue = 1 | pages = 72–75 | date = January 1999 | pmid = 10087521 | doi = 10.1007/s001150050403 | s2cid = 42630879 }}</ref> High dose misuse of zopiclone and increasing popularity amongst people who use substances who have been prescribed with zopiclone<ref>{{cite journal | vauthors = Sikdar S | title = Physical dependence on zopiclone. Prescribing this drug to addicts may give rise to iatrogenic drug misuse | journal = BMJ | volume = 317 | issue = 7151 | pages = 146 | date = July 1998 | pmid = 9657802 | pmc = 1113504 | doi = 10.1136/bmj.317.7151.146 }}</ref>{{clarification needed|date=December 2022}} The symptoms of zopiclone addiction can include depression, ], ], slow thoughts, ], ], ], and ].<ref>{{cite journal | vauthors = Kuntze MF, Bullinger AH, Mueller-Spahn F | title = Excessive use of zopiclone: a case report | journal = ] | volume = 132 | issue = 35–36 | pages = 523 | date = September 2002 | doi = 10.4414/smw.2002.10074 | pmid = 12506335 | s2cid = 33400840 | url = http://www.smw.ch/docs/pdf200x/2002/35/smw-10074.pdf | access-date = 2008-12-18 | archive-date = 2016-03-03 | archive-url = https://web.archive.org/web/20160303165243/http://www.smw.ch/docs/pdf200x/2002/35/smw-10074.pdf | url-status = dead }}</ref> | |||
| Zopiclone and other sedative hypnotic drugs are detected frequently in cases of people suspected of driving under the influence of drugs. Other sedating drugs, including benzodiazepines and zolpidem, are also found in high numbers of suspected drugged drivers. Many drivers have blood levels far exceeding the therapeutic dose range and often in combination with alcohol, illegal, or addictive ]s, suggesting a high degree of potential for non-medical use of benzodiazepines, zolpidem, and zopiclone.<ref>{{cite journal | vauthors = Jones AW, Holmgren A, Kugelberg FC | title = Concentrations of scheduled prescription drugs in blood of impaired drivers: considerations for interpreting the results | journal = Therapeutic Drug Monitoring | volume = 29 | issue = 2 | pages = 248–260 | date = April 2007 | pmid = 17417081 | doi = 10.1097/FTD.0b013e31803d3c04 | s2cid = 25511804 }}</ref><ref>{{cite journal | vauthors = Bramness JG, Skurtveit S, Mørland J | title = | language = no | journal = Tidsskrift for den Norske Laegeforening | volume = 119 | issue = 19 | pages = 2820–2821 | date = August 1999 | pmid = 10494203 }}</ref> Zopiclone, which at prescribed doses causes moderate impairment the next day, has been estimated to increase the risk of vehicle accidents by 50%, causing an increase of 503 excess accidents per 100,000 persons. ] or other nonimpairing sleep aids were recommended be used instead of zopiclone to reduce traffic accidents.<ref>{{cite journal | vauthors = Menzin J, Lang KM, Levy P, Levy E | title = A general model of the effects of sleep medications on the risk and cost of motor vehicle accidents and its application to France | journal = PharmacoEconomics | volume = 19 | issue = 1 | pages = 69–78 | date = January 2001 | pmid = 11252547 | doi = 10.2165/00019053-200119010-00005 | s2cid = 45013069 }}</ref> Zopiclone, as with other hypnotic drugs, is sometimes used to carry out criminal acts such as ].<ref>{{cite journal | vauthors = Kintz P, Villain M, Ludes B | title = Testing for the undetectable in drug-facilitated sexual assault using hair analyzed by tandem mass spectrometry as evidence | journal = Therapeutic Drug Monitoring | volume = 26 | issue = 2 | pages = 211–214 | date = April 2004 | pmid = 15228167 | doi = 10.1097/00007691-200404000-00022 | s2cid = 46445345 }}</ref> | |||
| ==Overdose== | |||
| Zopiclone is sometimes used as a method of suicide.<ref>{{cite journal |author=Mannaert E, Tytgat J, Daenens P |title=Detection and quantification of the hypnotic zopiclone, connected with an uncommon case of drowning |journal=Forensic Sci. Int. |volume=83 |issue=1 |pages=67–72 |year=1996 |month=November |pmid=8939015 |doi= 10.1016/0379-0738(96)02018-X|url=http://linkinghub.elsevier.com/retrieve/pii/0379-0738(96)02018-X}}</ref> Zopiclone has a similar fatality index as benzodiazepine drugs, apart from ] which is particularly toxic in overdosage.<ref></ref><ref>Buckley NA, Dawson AH, Whyte IM, McManus P, Ferguson N.Correlations between prescriptions and drugs taken in self-poisoning: Implications for prescribers and drug regulation.Med J Aust (in press)</ref><ref name="pmid12474705">{{cite journal |author=Buckley NA, Dawson AH, Whyte IM, O'Connell DL. |title= |journal=BMJ |volume=310 |issue= 6974|pages=219–21 |year=1995 |pmid=7866122 |doi= 10.1136/bmj.310.6974.219|url=http://www.bmj.com/cgi/content/full/310/6974/219 |pmc=2548618}}</ref> Deaths have occurred from zopiclone ], alone or in combination with other drugs.<ref>{{cite journal |author=Meatherall RC |title=Zopiclone fatality in a hospitalized patient |journal=J. Forensic Sci. |volume=42 |issue=2 |pages=340–3 |year=1997 |month=March |pmid=9068198 |doi= |url=}}</ref><ref>{{cite journal |author=Van Bocxlaer J, Meyer E, Clauwaert K, Lambert W, Piette M, De Leenheer A |title=Analysis of zopiclone (Imovane) in postmortem specimens by GC-MS and HPLC with diode-array detection |journal=J Anal Toxicol |volume=20 |issue=1 |pages=52–4 |year=1996 |pmid=8837952 |doi= |url=}}</ref><ref>{{cite journal |author=Yamazaki M, Terada M, Mitsukuni Y, Yoshimura M |title= |language=Japanese |journal=Nihon Hoigaku Zasshi |volume=52 |issue=4 |pages=245–52 |year=1998 |month=August |pmid=9893443 |doi= |url=}}</ref> Overdose of zopiclone may present with excessive sedation, depressed respiratory function which may progress to coma and possibly death.<ref>{{cite journal |author=Boniface PJ, Russell SG |title=Two cases of fatal zopiclone overdose |journal=J Anal Toxicol |volume=20 |issue=2 |pages=131–3 |year=1996 |pmid=8868406 |doi= |url=}}</ref> Zopiclone combined with ], ] or other ] depressants may be even more likely to lead to fatal overdoses. Zopiclone overdosage can be treated with the benzodiazepine receptor antagonist ] which displaces zopiclone from its binding site on the benzodiazepine receptor thereby rapidly reversing the effects of zopiclone.<ref>{{cite journal | last = Cienki | first = JJ | coauthors = Burkhart KK, Donovan JW. | year = 2005 | month = | title = Zopiclone overdose responsive to flumazenil | journal = Clin Toxicol (Phila). | volume = 43 | issue = 5 | pages = 385–6 | pmid = 16235515 }}</ref><ref>{{cite journal |pmid=8039775 |url= |format= |year=1994 |month=May |author=Pounder, Dj; Davies, Ji |title=Zopiclone poisoning: tissue distribution and potential for postmortem diffusion. |volume=65 |issue=3 |pages=177–83 |issn=0379-0738 |journal=Forensic Science International |doi=10.1016/0379-0738(94)90273-9 }}</ref> Serious effects on the heart may also occur from a zopiclone overdose<ref>{{cite journal |author=Regouby Y, Delomez G, Tisserant A |title= |language=French |journal=Therapie |volume=45 |issue=2 |pages=162 |year=1990 |pmid=2353332 |doi= |url=}}</ref><ref>{{cite journal |author=Regouby Y, Delomez G, Tisserant A |title= |language=French |journal=Therapie |volume=44 |issue=5 |pages=379–80 |year=1989 |pmid=2814922 |doi= |url=}}</ref> when combined with piperazine.<ref>{{cite book |title= Medical Toxicology|last= Dart|first= Richard C.|authorlink= |coauthors= |year= 2003|publisher= |location= |isbn= 978-0-7817-2845-4|oclc= |page= 889|pages= |url= |accessdate=}}</ref> | |||
| Death certificates show the number of zopiclone related deaths is on the rise.<ref>{{cite journal | last = Carlsten | first = A | coauthors = Waern M, Holmgren P, Allebeck P. | year = 2003 | month = | title = The role of benzodiazepines in elderly suicides | journal = Scand J Public Health. | volume = 31 | issue = 3 | pages = 224–8 | pmid = 12850977| doi = 10.1080/14034940210167966 }}</ref> Zopiclone when taken alone usually is not fatal, however, when mixed with alcohol or other drugs such as ], or in patients with respiratory, or hepatic disorders, the risk of a serious and fatal overdose increases.<ref>{{cite journal | author=Harry P | year= 1997| month=April | title= | journal=Rev Prat | volume=47 | issue=7 | pages=731–5 | pmid=9183949 }}</ref><ref>{{cite journal |author=Bramness JG, Arnestad M, Karinen R, Hilberg T |title=Fatal overdose of zopiclone in an elderly woman with bronchogenic carcinoma |journal=J. Forensic Sci. |volume=46 |issue=5 |pages=1247–9 |year=2001 |month=September |pmid=11569575 |doi= |url=}}</ref> | |||
| Zopiclone has crosstolerance with barbiturates and is able to suppress barbiturate withdrawal symptoms. It is frequently self-administered intravenously in studies on monkeys, suggesting a high risk of addictive potential.<ref>{{cite journal | vauthors = Yanagita T | title = Dependence potential of zopiclone studied in monkeys | journal = International Pharmacopsychiatry | volume = 17 | issue = 2 | pages = 216–227 | year = 1982 | pmid = 6892368 }}</ref> | |||
| ==Detection in biological fluids== | |||
| Zopiclone may be measured in blood, plasma or urine by chromatographic methods. Plasma zopiclone concentrations are typically less than 100 μg/L during therapeutic usage, but frequently exceed 100 μg/L in automotive vehicle operators arrested for impaired driving ability and may exceed 1000 μg/L in acutely poisoned patients. Postmortem blood concentrations are usually in a range of 0.4-3.9 mg/L in victims of fatal acute overdosage.<ref>Kratzsch C, Tenberken O, Peters FT et al. Screening, library-assisted identification and validated quantification of 23 benzodiazepines, flumazenil, zaleplone, zolpidem and zopiclone in plasma by liquid chromatography/mass spectrometry with atmospheric pressure chemical ionization. J. Mass Spec. 39: 856-872, 2004.</ref><ref>Gustavsen I, Al-Sammurraie M, Mørland J, Bramness JG. Impairment related to blood drug concentrations of zopiclone and zolpidem compared to alcohol in apprehended drivers. Accid. Anal. Prev. 41: 462-466, 2009.</ref><ref>R. Baselt, ''Disposition of Toxic Drugs and Chemicals in Man'', 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 1677-1679.</ref> | |||
| Zopiclone is in the top ten medications obtained using a false prescription in France.<ref name = "Assessment" /> | |||
| ==See also== | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| *] | |||
| ==References== | ==References== | ||
| {{Reflist |
{{Reflist}} | ||
| ==External links== | ==External links== | ||
| * | * {{Webarchive|url=https://web.archive.org/web/20060404232506/http://www.mentalhealth.com/drug/p30-i01.html |date=2006-04-04 }} | ||
| * (] file) | * (] file) | ||
| * | * | ||
| * | * | ||
| * | * {{Webarchive|url=https://web.archive.org/web/20150402104653/http://www.non-benzodiazepines.org.uk/ |date=2015-04-02 }} | ||
| {{Hypnotics and sedatives}} | {{Hypnotics and sedatives}} | ||
| {{Insomnia pharmacotherapies}} | |||
| {{GABAAR PAMs}} | |||
| ] | |||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | ] | ||
| ] | ] | ||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 01:25, 10 December 2024
Hypnotic medicationPharmaceutical compound
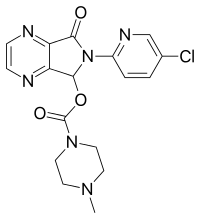 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Imovane, Zimovane, Dopareel, others |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Routes of administration | Oral tablets, 3.75 mg or 7.5mg (UK), 5 mg, 7.5 mg, or 10 mg (JP) |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 75–80% |
| Protein binding | 52–59% |
| Metabolism | Hepatic through CYP3A4 and CYP2E1 |
| Elimination half-life | ~5 hours (3.5–6.5 hours) ~7–9 hours for 65+ years old |
| Excretion | Urine (80%) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.051.018 |
| Chemical and physical data | |
| Formula | C17H17ClN6O3 |
| Molar mass | 388.81 g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Zopiclone, sold under the brand name Imovane among others, is a nonbenzodiazepine, specifically a cyclopyrrolone, used to treat difficulty sleeping. Zopiclone is molecularly distinct from benzodiazepine drugs and is classed as a cyclopyrrolone. However, zopiclone increases the normal transmission of the neurotransmitter gamma-aminobutyric acid (GABA) in the central nervous system, via modulating GABAA receptors similarly to the way benzodiazepine drugs do inducing sedation but not with the anti-anxiety properties of the benzodiazepines.
Zopiclone is a sedative. It works by causing a depression or tranquilization of the central nervous system. After prolonged use, the body can become accustomed to the effects of zopiclone. When the dose is then reduced or the drug is abruptly stopped, withdrawal symptoms may result. These can include a range of symptoms similar to those of benzodiazepine withdrawal. Although withdrawal symptoms from therapeutic doses of zopiclone and its isomers (i.e., eszopiclone) do not typically present with convulsions and are therefore not considered life-threatening, patients may experience such significant agitation or anxiety that they seek emergency medical attention.
In the United States, zopiclone is not commercially available, although its active stereoisomer, eszopiclone, is. Zopiclone is a controlled substance in the United States, Japan, Brazil, New Zealand and some European countries, and may be illegal to possess without a prescription.
Zopiclone is known colloquially as a "Z-drug". Other Z-drugs include zaleplon and zolpidem and were initially thought to be less addictive than benzodiazepines. However, this appraisal has shifted somewhat in the last few years as cases of addiction and habituation have been presented. Zopiclone is recommended to be taken at the lowest effective dose, with a duration of 2–3 weeks for short-term insomnia. Daily or continuous use of the drug is not usually advised, and caution must be taken when the compound is used in conjunction with benzodiazepines, sedatives or other drugs affecting the central nervous system.
Medical uses

Zopiclone is used for the short-term treatment of insomnia where sleep initiation or sleep maintenance are prominent symptoms. Long-term use is not recommended, as tolerance, dependence, and addiction can occur. One low-quality study found that zopiclone is ineffective in improving sleep quality or increasing sleep time in shift workers, and more research in this area has been recommended.
Cognitive behavioral therapy has been found to be superior to zopiclone in the treatment of insomnia and has been found to have lasting effects on sleep quality for at least a year after therapy.
Specific populations
Elderly
Zopiclone, similar to other benzodiazepines and nonbenzodiazepine hypnotic drugs, causes impairments in body balance and standing steadiness in individuals who wake up at night or the next morning. Falls and hip fractures are frequently reported. The combination with alcohol consumption increases these impairments. Partial, but incomplete tolerance develops to these impairments. Zopiclone increases postural sway and increases the number of falls in older people, as well as cognitive side effects. Falls are a significant cause of death in older people.
An extensive review of the medical literature regarding the management of insomnia and the elderly found that considerable evidence of the effectiveness and lasting benefits of nondrug treatments for insomnia exist. Compared with the benzodiazepines, the nonbenzodiazepine sedative-hypnotics, such as zopiclone, offer few if any advantages in efficacy or tolerability in elderly persons. Newer agents such as the melatonin receptor agonists may be more suitable and effective for the management of chronic insomnia in elderly people. Long-term use of sedative-hypnotics for insomnia lacks an evidence base and is discouraged for reasons that include concerns about such potential adverse drug effects as cognitive impairment (anterograde amnesia), daytime sedation, motor incoordination, and increased risk of motor vehicle accidents and falls. In addition, the effectiveness and safety of long-term use of nonbenzodiazepine hypnotic drugs remains to be determined.
Liver disease
Patients with liver disease eliminate zopiclone much more slowly than normal patients and in addition experience exaggerated pharmacological effects of the drug.
Adverse reactions
Sleeping pills, including zopiclone, have been associated with an increased risk of death. The British National Formulary states adverse reactions as follows: "taste disturbance (some report a metallic taste); less commonly nausea, vomiting, dizziness, drowsiness, dry mouth, headache; rarely amnesia, confusion, depression, hallucinations, nightmares; very rarely light headedness, incoordination, paradoxical effects and sleep-walking also reported".
Contraindications
Zopiclone causes impaired driving skills similar to those of benzodiazepines. Long-term users of hypnotic drugs for sleep disorders develop only partial tolerance to adverse effects on driving, with users of hypnotic drugs even after one year of use still showing an increased motor vehicle accident rate. Patients who drive motor vehicles should not take zopiclone as there is a significantly increased risk of accidents in zopiclone users. Zopiclone induces impairment of psychomotor function. Driving or operating machinery should be avoided after taking zopiclone as effects can carry over to the next day, including impaired hand-eye coordination.
A double-blind study on the effect on performance of several hypnotic medications, relevant to military personnel who may have to be awakened to carry out duties, found that drugs listed in increasing order of performance impact duration were melatonin (with no impact), zaleplon, temazepam, and zopiclone. The effects on serial reaction time (SRT), logical reasoning (LRT), serial subtraction (SST), and multitask (MT) were measured. For zaleplon (10 mg), zopiclone (7.5 mg) and temazepam (15 mg) respectively the times to recover normal performance for SRT were 3.25, 6.25, and 5.25 hours; for LRT 3.25, >6.25, and 4.25 hours; for SST 2.25, >6.25, and 4.25 hours; and for MT 2.25, 4.25, and 3.25 hours. The study did not consider the effectiveness of the drugs on sleep.
EEG and sleep
It causes similar alterations on EEG readings and sleep architecture as benzodiazepines and causes disturbances in sleep architecture on withdrawal as part of its rebound effect. Zopiclone reduces both delta waves and the number of high-amplitude delta waves whilst increasing low-amplitude waves. Zopiclone reduces the total amount of time spent in REM sleep as well as delaying its onset. In EEG studies, zopiclone significantly increases the energy of the beta frequency band, increasing stage 2. Zopiclone is less selective to the α1 site and has higher affinity to the α2 site than zaleplon. Zopiclone is therefore very similar pharmacologically to benzodiazepines.
Overdose
Zopiclone is sometimes used as a method of suicide. It has a similar fatality index to that of benzodiazepine drugs, apart from temazepam, which is particularly toxic in overdose. Deaths have occurred from zopiclone overdose, alone or in combination with other drugs. Overdose of zopiclone may present with excessive sedation and depressed respiratory function that may progress to coma and possibly death. Zopiclone combined with alcohol, opiates, or other central nervous system depressants may be even more likely to lead to fatal overdoses. Zopiclone overdosage can be treated with the GABAA receptor benzodiazepine site antagonist flumazenil, which displaces zopiclone from its binding site, thereby rapidly reversing its effects. Serious effects on the heart may also occur from a zopiclone overdose when combined with piperazine.
Death certificates show the number of zopiclone-related deaths is on the rise. When taken alone, it usually is not fatal, but when mixed with alcohol or other drugs such as opioids, or in patients with respiratory, or hepatic disorders, the risk of a serious and fatal overdose increases.
Interactions
Zopiclone also interacts with trimipramine and caffeine.
Alcohol has an additive effect when combined with zopiclone, enhancing the adverse effects including the overdose potential of zopiclone significantly. Due to these risks and the increased risk for dependence, alcohol should be avoided when using zopiclone.
Erythromycin appears to increase the absorption rate of zopiclone and prolong its elimination half-life, leading to increased plasma levels and more pronounced effects. Itraconazole has a similar effect on zopiclone pharmacokinetics as erythromycin. The elderly may be particularly sensitive to the erythromycin and itraconazole drug interaction with zopiclone. Temporary dosage reduction during combined therapy may be required, especially in the elderly. Rifampicin causes a very notable reduction in half-life of zopiclone and peak plasma levels, which results in a large reduction in the hypnotic effect of zopiclone. Phenytoin and carbamazepine may also provoke similar interactions. Ketoconazole and sulfaphenazole interfere with the metabolism of zopiclone. Nefazodone impairs the metabolism of zopiclone leading to increased zopiclone levels and marked next-day sedation.
Pharmacology
The therapeutic pharmacological properties of zopiclone include hypnotic, anxiolytic, anticonvulsant, and myorelaxant properties. Zopiclone and benzodiazepines bind to the same sites on GABAA receptors, causing an enhancement of the actions of GABA to produce the therapeutic and adverse effects of zopiclone. The metabolite of zopiclone desmethylzopiclone is also pharmacologically active, although it has predominately anxiolytic properties. One study found some slight selectivity for zopiclone on α1 and α5 subunits, although it is regarded as being unselective in its binding to GABAA receptors containing α1, α2, α3, and α5 subunits. Desmethylzopiclone has been found to have partial agonist properties, unlike the parent drug zopiclone, which is a full agonist. The mechanism of action of zopiclone is similar to benzodiazepines, with similar effects on locomotor activity and on dopamine and serotonin turnover. A meta-analysis of randomised controlled clinical trials that compared benzodiazepines to zopiclone or other Z drugs such as zolpidem and zaleplon has found few clear and consistent differences between zopiclone and the benzodiazepines in sleep onset latency, total sleep duration, number of awakenings, quality of sleep, adverse events, tolerance, rebound insomnia, and daytime alertness. Zopiclone is in the cyclopyrrolone family of drugs. Other cyclopyrrolone drugs include suriclone. Zopiclone, although molecularly different from benzodiazepines, shares an almost identical pharmacological profile as benzodiazepines, including anxiolytic properties. Its mechanism of action is by binding to the benzodiazepine site and acting as a full agonist, which in turn positively modulates benzodiazepine-sensitive GABAA receptors and enhances GABA binding at the GABAA receptors to produce zopiclone's pharmacological properties. In addition to zopiclone's benzodiazepine pharmacological properties, it also has some barbiturate-like properties.
Pharmacokinetics
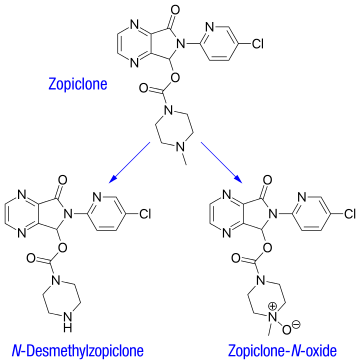
After oral administration, zopiclone is rapidly absorbed, with a bioavailability around 75–80%. Time to peak plasma concentration is 1–2 hours. A high-fat meal preceding zopiclone administration does not change absorption (as measured by AUC), but reduces peak plasma levels and delays its occurrence, thus may delay the onset of therapeutic effects.
The plasma protein-binding of zopiclone has been reported to be weak, between 45 and 80% (mean 52–59%). It is rapidly and widely distributed to body tissues, including the brain, and is excreted in urine, saliva, and breast milk. Zopiclone is partly extensively metabolized in the liver to form an active N-demethylated derivative (N-desmethylzopiclone) and an inactive zopiclone-N-oxide. Hepatic enzymes playing the most significant role in zopiclone metabolism are CYP3A4 and CYP2E1. In addition, about 50% of the administered dose is decarboxylated and excreted via the lungs. In urine, the N-demethyl and N-oxide metabolites account for 30% of the initial dose. Between 7 and 10% of zopiclone is recovered from the urine, indicating extensive metabolism of the drug before excretion. The terminal elimination half-life of zopiclone ranges from 3.5 to 6.5 hours (5 hours on average).
The pharmacokinetics of zopiclone in humans are stereoselective. After oral administration of the racemic mixture, Cmax (time to maximum plasma concentration), area under the plasma time-concentration curve (AUC) and terminal elimination half-life values are higher for the dextrorotatory enantiomers, owing to the slower total clearance and smaller volume of distribution (corrected by the bioavailability), compared with the levorotatory enantiomer. In urine, the concentrations of the dextrorotatory enantiomers of the N-demethyl and N-oxide metabolites are higher than those of the respective antipodes.
The pharmacokinetics of zopiclone are altered by aging and are influenced by renal and hepatic functions. In severe chronic kidney failure, the area under the curve value for zopiclone was larger and the half-life associated with the elimination rate constant longer, but these changes were not considered to be clinically significant. Sex and race have not been found to interact with pharmacokinetics of zopiclone.
Chemistry
The melting point of zopiclone is 178 °C. Zopiclone's solubility in water, at room temperature (25 °C) are 0.151 mg/mL. The logP value of zopiclone is 0.8.
Detection in biological fluids
Zopiclone may be measured in blood, plasma, or urine by chromatographic methods. Plasma concentrations are typically less than 100 μg/L during therapeutic use, but frequently exceed 100 μg/L in automotive vehicle operators arrested for impaired driving ability and may exceed 1000 μg/L in acutely poisoned patients. Post mortem blood concentrations are usually in a range of 400 to 3900 μg/L in victims of fatal acute overdose.
History
Zopiclone was developed and first introduced in 1986 by Rhône-Poulenc S.A., now part of Sanofi, the main worldwide manufacturer. Initially, it was promoted as an improvement on benzodiazepines, but a recent meta-analysis found it was no better than benzodiazepines in any of the aspects assessed. On April 4, 2005, the U.S. Drug Enforcement Administration listed zopiclone under schedule IV, due to evidence that the drug has addictive properties similar to benzodiazepines.
Zopiclone, as traditionally sold worldwide, is a racemic mixture of two stereoisomers, only one of which is active. In 2005, the pharmaceutical company Sepracor of Marlborough, Massachusetts, began marketing the active stereoisomer eszopiclone under the name Lunesta in the United States. This had the consequence of placing what is a generic drug in most of the world under patent control in the United States. Generic forms of Lunesta have since become available in the United States. Zopiclone is currently available off-patent in a number of European countries, Brazil, Canada, Hong Kong, and New Zealand. The eszopiclone/zopiclone difference is in the dosage—the strongest eszopiclone dosage contains 3 mg of the therapeutic stereoisomer, whereas the highest zopiclone dosage (10 mg) contains 5 mg of the active stereoisomer. The two agents have not yet been studied in head-to-head clinical trials to determine the existence of any potential clinical differences (efficacy, side effects, developing dependence on the drug, safety, etc.).
Society and culture
Recreational use
Zopiclone has the potential for non-medical use, dosage escalation, and drug dependence. It is taken orally and sometimes intravenously when used non-medically, and often combined with alcohol to achieve euphoria. Patients abusing the drug are also at risk of dependence. Withdrawal symptoms can be seen after long-term use of normal doses even after a gradual reduction regimen. The Compendium of Pharmaceuticals and Specialties recommends zopiclone prescriptions not exceed 7 to 10 days, owing to concerns of addiction, tolerance, and physical dependence. Two types of drug misuse can occur: either recreational misuse, wherein the drug is taken to achieve a high, or when the drug is continued long-term against medical advice. Zopiclone may be more addictive than benzodiazepines. Those with a history of substance misuse or mental health disorders may be at an increased risk of high-dose zopiclone misuse. High dose misuse of zopiclone and increasing popularity amongst people who use substances who have been prescribed with zopiclone The symptoms of zopiclone addiction can include depression, dysphoria, hopelessness, slow thoughts, social isolation, worrying, sexual anhedonia, and nervousness.
Zopiclone and other sedative hypnotic drugs are detected frequently in cases of people suspected of driving under the influence of drugs. Other sedating drugs, including benzodiazepines and zolpidem, are also found in high numbers of suspected drugged drivers. Many drivers have blood levels far exceeding the therapeutic dose range and often in combination with alcohol, illegal, or addictive prescription drugs, suggesting a high degree of potential for non-medical use of benzodiazepines, zolpidem, and zopiclone. Zopiclone, which at prescribed doses causes moderate impairment the next day, has been estimated to increase the risk of vehicle accidents by 50%, causing an increase of 503 excess accidents per 100,000 persons. Zaleplon or other nonimpairing sleep aids were recommended be used instead of zopiclone to reduce traffic accidents. Zopiclone, as with other hypnotic drugs, is sometimes used to carry out criminal acts such as sexual assaults.
Zopiclone has crosstolerance with barbiturates and is able to suppress barbiturate withdrawal symptoms. It is frequently self-administered intravenously in studies on monkeys, suggesting a high risk of addictive potential.
Zopiclone is in the top ten medications obtained using a false prescription in France.
References
- Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- ^ "Assessment of Zopiclone" (PDF). World Health Organization. Essential Medicines and Health Products. World Health Organization. 2006. p. 9 (Section 5. Pharmacokinetics). Retrieved 5 December 2015.
- "Zopiclone consumer information from". Drugs.com. Retrieved 2013-06-06.
- "Chapter 3 - The technologies, section 3.4", Clinical need and practice - Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia, National Institute for Health and Care Excellence (NICE), 28 April 2004, Technology appraisal guidance ,
This guidance will be reviewed if there is new evidence.
Current as of 8 June 2023 - Van Der Kleijn E (1989). "Effects of zopiclone and temazepam on sleep, behaviour and mood during the day". European Journal of Clinical Pharmacology. 36 (3): 247–251. doi:10.1007/BF00558155. ISSN 0031-6970. PMID 2744064.
- "What's wrong with prescribing hypnotics?". Drug and Therapeutics Bulletin. 42 (12): 89–93. December 2004. doi:10.1136/dtb.2004.421289. PMID 15587763. S2CID 40188442.
- Touitou Y (July 2007). "". Annales Pharmaceutiques Françaises (in French). 65 (4): 230–238. doi:10.1016/s0003-4509(07)90041-3. PMID 17652991.
- Liira J, Verbeek JH, Costa G, Driscoll TR, Sallinen M, Isotalo LK, et al. (August 2014). "Pharmacological interventions for sleepiness and sleep disturbances caused by shift work". The Cochrane Database of Systematic Reviews. 2014 (8): CD009776. doi:10.1002/14651858.CD009776.pub2. PMC 10025070. PMID 25113164.
- "Cognitive therapy superior to zopiclone for insomnia". The Journal of Family Practice. 55 (10): 845. October 2006. PMID 17089469.
- Baillargeon L, Landreville P, Verreault R, Beauchemin JP, Grégoire JP, Morin CM (November 2003). "Discontinuation of benzodiazepines among older insomniac adults treated with cognitive-behavioural therapy combined with gradual tapering: a randomized trial". CMAJ. 169 (10): 1015–1020. PMC 236226. PMID 14609970.
- Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik OE, Kvale G, et al. (June 2006). "Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial". JAMA. 295 (24): 2851–2858. doi:10.1001/jama.295.24.2851. PMID 16804151.
- Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M (February 2004). "Psychological treatment for insomnia in the regulation of long-term hypnotic drug use". Health Technology Assessment. 8 (8): iii–iv, 1–68. doi:10.3310/hta8080. PMID 14960254.
- Mets MA, Volkerts ER, Olivier B, Verster JC (August 2010). "Effect of hypnotic drugs on body balance and standing steadiness". Sleep Medicine Reviews. 14 (4): 259–267. doi:10.1016/j.smrv.2009.10.008. PMID 20171127.
- Tada K, Sato Y, Sakai T, Ueda N, Kasamo K, Kojima T (1994). "Effects of zopiclone, triazolam, and nitrazepam on standing steadiness". Neuropsychobiology. 29 (1): 17–22. doi:10.1159/000119057. PMID 8127419.
- Allain H, Bentué-Ferrer D, Tarral A, Gandon JM (July 2003). "Effects on postural oscillation and memory functions of a single dose of zolpidem 5 mg, zopiclone 3.75 mg and lormetazepam 1 mg in elderly healthy subjects. A randomized, cross-over, double-blind study versus placebo". European Journal of Clinical Pharmacology. 59 (3): 179–188. doi:10.1007/s00228-003-0591-5. PMID 12756510. S2CID 13440208.
- Antai-Otong D (August 2006). "The art of prescribing. Risks and benefits of non-benzodiazepine receptor agonists in the treatment of acute primary insomnia in older adults". Perspectives in Psychiatric Care. 42 (3): 196–200. doi:10.1111/j.1744-6163.2006.00070.x. PMID 16916422.
- Bain KT (June 2006). "Management of chronic insomnia in elderly persons". The American Journal of Geriatric Pharmacotherapy. 4 (2): 168–192. doi:10.1016/j.amjopharm.2006.06.006. PMID 16860264.
- Parker G, Roberts CJ (September 1983). "Plasma concentrations and central nervous system effects of the new hypnotic agent zopiclone in patients with chronic liver disease". British Journal of Clinical Pharmacology. 16 (3): 259–265. doi:10.1111/j.1365-2125.1983.tb02159.x. PMC 1428012. PMID 6626417.
- Kripke DF (February 2016). "Mortality Risk of Hypnotics: Strengths and Limits of Evidence" (PDF). Drug Safety. 39 (2): 93–107. doi:10.1007/s40264-015-0362-0. PMID 26563222. S2CID 7946506.
- "Zopiclone", British National Formulary, National Institute for Health and Care Excellence, 19 September 2016, archived from the original on 9 October 2016, retrieved 2 October 2016
- Staner L, Ertlé S, Boeijinga P, Rinaudo G, Arnal MA, Muzet A, et al. (October 2005). "Next-day residual effects of hypnotics in DSM-IV primary insomnia: a driving simulator study with simultaneous electroencephalogram monitoring". Psychopharmacology. 181 (4): 790–798. doi:10.1007/s00213-005-0082-8. PMID 16025317. S2CID 26351598.
- Barbone F, McMahon AD, Davey PG, Morris AD, Reid IC, McDevitt DG, et al. (October 1998). "Association of road-traffic accidents with benzodiazepine use". Lancet. 352 (9137): 1331–1336. doi:10.1016/S0140-6736(98)04087-2. PMID 9802269. S2CID 40825194.
- Yasui M, Kato A, Kanemasa T, Murata S, Nishitomi K, Koike K, et al. (June 2005). "". Nihon Shinkei Seishin Yakurigaku Zasshi = Japanese Journal of Psychopharmacology. 25 (3): 143–151. PMID 16045197.
- Rettig HC, de Haan P, Zuurmond WW, von Leeuwen L (December 1990). "Effects of hypnotics on sleep and psychomotor performance. A double-blind randomised study of lormetazepam, midazolam and zopiclone". Anaesthesia. 45 (12): 1079–1082. doi:10.1111/j.1365-2044.1990.tb14896.x. PMID 2278337. S2CID 36841164.
- Lader M, Denney SC (1982). "A double-blind study to establish the residual effects of zopiclone on performance in healthy volunteers". International Pharmacopsychiatry. 17 (Suppl 2): 98–108. PMID 7188379.
- Billiard M, Besset A, de Lustrac C, Brissaud L (1987). "Dose-response effects of zopiclone on night sleep and on nighttime and daytime functioning". Sleep. 10 (Suppl 1): 27–34. doi:10.1093/sleep/10.suppl_1.27. PMID 3326113.
- Paul MA, Gray G, Kenny G, Pigeau RA (December 2003). "Impact of melatonin, zaleplon, zopiclone, and temazepam on psychomotor performance". Aviation, Space, and Environmental Medicine. 74 (12). Aerospace Medical Association: 1263–1270. PMID 14692469.
- Trachsel L, Dijk DJ, Brunner DP, Klene C, Borbély AA (February 1990). "Effect of zopiclone and midazolam on sleep and EEG spectra in a phase-advanced sleep schedule". Neuropsychopharmacology. 3 (1): 11–18. PMID 2306331.
- Mann K, Bauer H, Hiemke C, Röschke J, Wetzel H, Benkert O (August 1996). "Acute, subchronic and discontinuation effects of zopiclone on sleep EEG and nocturnal melatonin secretion". Eur Neuropsychopharmacol. 6 (3): 163–168. doi:10.1016/0924-977X(96)00014-4. PMID 8880074. S2CID 25259646.
- Wright NA, Belyavin A, Borland RG, Nicholson AN (June 1986). "Modulation of delta activity by hypnotics in middle-aged subjects: studies with a benzodiazepine (flurazepam) and a cyclopyrrolone (zopiclone)". Sleep. 9 (2): 348–352. doi:10.1093/sleep/9.2.348. PMID 3505734.
- Kim YD, Zhuang HY, Tsutsumi M, Okabe A, Kurachi M, Kamikawa Y (October 1993). "Comparison of the effect of zopiclone and brotizolam on sleep EEG by quantitative evaluation in healthy young women". Sleep. 16 (7): 655–661. doi:10.1093/sleep/16.7.655. PMID 8290860.
- Kanno O, Watanabe H, Kazamatsuri H (March 1993). "Effects of zopiclone, flunitrazepam, triazolam and levomepromazine on the transient change in sleep-wake schedule: polygraphic study, and the evaluation of sleep and daytime condition". Prog. Neuropsychopharmacol. Biol. Psychiatry. 17 (2): 229–239. doi:10.1016/0278-5846(93)90044-S. PMID 8430216. S2CID 54285586.
- Noguchi H, Kitazumi K, Mori M, Shiba T (March 2004). "Electroencephalographic properties of zaleplon, a non-benzodiazepine sedative/hypnotic, in rats". Journal of Pharmacological Sciences. 94 (3): 246–251. doi:10.1254/jphs.94.246. PMID 15037809.
- Mannaert E, Tytgat J, Daenens P (November 1996). "Detection and quantification of the hypnotic zopiclone, connected with an uncommon case of drowning". Forensic Science International. 83 (1): 67–72. doi:10.1016/0379-0738(96)02018-X. PMID 8939015.
- Buckley NA, Dawson AH, Whyte IM, McManus P, Ferguson N.Correlations between prescriptions and drugs taken in self-poisoning: Implications for prescribers and drug regulation. Med J Aust (in press)
- Buckley NA, Dawson AH, Whyte IM, O'Connell DL (January 1995). "Relative toxicity of benzodiazepines in overdose". BMJ. 310 (6974): 219–221. doi:10.1136/bmj.310.6974.219. PMC 2548618. PMID 7866122.
- Meatherall RC (March 1997). "Zopiclone fatality in a hospitalized patient". Journal of Forensic Sciences. 42 (2): 340–343. doi:10.1520/JFS14125J. PMID 9068198.
- Van Bocxlaer J, Meyer E, Clauwaert K, Lambert W, Piette M, De Leenheer A (1996). "Analysis of zopiclone (Imovane) in postmortem specimens by GC-MS and HPLC with diode-array detection". Journal of Analytical Toxicology. 20 (1): 52–54. doi:10.1093/jat/20.1.52. PMID 8837952.
- Yamazaki M, Terada M, Mitsukuni Y, Yoshimura M (August 1998). "". Nihon Hoigaku Zasshi = the Japanese Journal of Legal Medicine (in Japanese). 52 (4): 245–252. PMID 9893443.
- Boniface PJ, Russell SG (1996). "Two cases of fatal zopiclone overdose". Journal of Analytical Toxicology. 20 (2): 131–133. doi:10.1093/jat/20.2.131. PMID 8868406.
- Cienki JJ, Burkhart KK, Donovan JW (2005). "Zopiclone overdose responsive to flumazenil". Clinical Toxicology. 43 (5): 385–386. doi:10.1081/clt-200058944. PMID 16235515. S2CID 41701825.
- Pounder DJ, Davies JI (May 1994). "Zopiclone poisoning: tissue distribution and potential for postmortem diffusion". Forensic Science International. 65 (3): 177–183. doi:10.1016/0379-0738(94)90273-9. PMID 8039775.
- Regouby Y, Delomez G, Tisserant A (1990). "". Therapie (in French). 45 (2): 162. PMID 2353332.
- Regouby Y, Delomez G, Tisserant A (1989). "". Therapie (in French). 44 (5): 379–380. PMID 2814922.
- Dart RC (2003). Medical Toxicology. Lippincott Williams & Wilkins. p. 889. ISBN 978-0-7817-2845-4.
- Carlsten A, Waern M, Holmgren P, Allebeck P (2003). "The role of benzodiazepines in elderly suicides". Scandinavian Journal of Public Health. 31 (3): 224–228. doi:10.1080/14034940210167966. PMID 12850977. S2CID 24102880.
- Harry P (April 1997). "". La Revue du Praticien. 47 (7): 731–735. PMID 9183949.
- Bramness JG, Arnestad M, Karinen R, Hilberg T (September 2001). "Fatal overdose of zopiclone in an elderly woman with bronchogenic carcinoma". Journal of Forensic Sciences. 46 (5): 1247–1249. doi:10.1520/JFS15131J. PMID 11569575.
- Caille G, du Souich P, Spenard J, Lacasse Y, Vezina M (April 1984). "Pharmacokinetic and clinical parameters of zopiclone and trimipramine when administered simultaneously to volunteers". Biopharmaceutics & Drug Disposition. 5 (2): 117–125. doi:10.1002/bdd.2510050205. PMID 6743780.
- Mattila ME, Mattila MJ, Nuotto E (April 1992). "Caffeine moderately antagonizes the effects of triazolam and zopiclone on the psychomotor performance of healthy subjects". Pharmacology & Toxicology. 70 (4): 286–289. doi:10.1111/j.1600-0773.1992.tb00473.x. PMID 1351673.
- ^ Kuitunen T, Mattila MJ, Seppala T (April 1990). "Actions and interactions of hypnotics on human performance: single doses of zopiclone, triazolam and alcohol". International Clinical Psychopharmacology. 5 (Suppl 2): 115–130. PMID 2201724.
- Koski A, Ojanperä I, Vuori E (May 2003). "Interaction of alcohol and drugs in fatal poisonings". Human & Experimental Toxicology. 22 (5): 281–287. Bibcode:2003HETox..22..281K. doi:10.1191/0960327103ht324oa. PMID 12774892. S2CID 37777007.
- Aranko K, Luurila H, Backman JT, Neuvonen PJ, Olkkola KT (October 1994). "The effect of erythromycin on the pharmacokinetics and pharmacodynamics of zopiclone". British Journal of Clinical Pharmacology. 38 (4): 363–367. doi:10.1111/j.1365-2125.1994.tb04367.x. PMC 1364781. PMID 7833227.
- Jalava KM, Olkkola KT, Neuvonen PJ (1996). "Effect of itraconazole on the pharmacokinetics and pharmacodynamics of zopiclone". European Journal of Clinical Pharmacology. 51 (3–4): 331–334. doi:10.1007/s002280050207. PMID 9010708. S2CID 20916689.
- Villikka K, Kivistö KT, Lamberg TS, Kantola T, Neuvonen PJ (May 1997). "Concentrations and effects of zopiclone are greatly reduced by rifampicin". British Journal of Clinical Pharmacology. 43 (5): 471–474. doi:10.1046/j.1365-2125.1997.00579.x. PMC 2042775. PMID 9159561.
- Becquemont L, Mouajjah S, Escaffre O, Beaune P, Funck-Brentano C, Jaillon P (September 1999). "Cytochrome P-450 3A4 and 2C8 are involved in zopiclone metabolism". Drug Metabolism and Disposition. 27 (9): 1068–1073. PMID 10460808. Archived from the original on 2005-04-17. Retrieved 2008-12-16.
- Alderman CP, Gebauer MG, Gilbert AL, Condon JT (November 2001). "Possible interaction of zopiclone and nefazodone". The Annals of Pharmacotherapy. 35 (11): 1378–1380. doi:10.1345/aph.1A074. PMID 11724087. S2CID 38894701.
- Röschke J, Mann K, Aldenhoff JB, Benkert O (March 1994). "Functional properties of the brain during sleep under subchronic zopiclone administration in man". European Neuropsychopharmacology. 4 (1): 21–30. doi:10.1016/0924-977X(94)90311-5. PMID 8204993. S2CID 40503805.
- Petroski RE, Pomeroy JE, Das R, Bowman H, Yang W, Chen AP, et al. (April 2006). "Indiplon is a high-affinity positive allosteric modulator with selectivity for alpha1 subunit-containing GABAA receptors". The Journal of Pharmacology and Experimental Therapeutics. 317 (1): 369–377. doi:10.1124/jpet.105.096701. PMID 16399882. S2CID 46510829.
- Atack JR (August 2003). "Anxioselective compounds acting at the GABA(A) receptor benzodiazepine binding site". Current Drug Targets. CNS and Neurological Disorders. 2 (4): 213–232. doi:10.2174/1568007033482841. PMID 12871032.
- Liu HJ, Sato K, Shih HC, Shibuya T, Kawamoto H, Kitagawa H (March 1985). "Pharmacologic studies of the central action of zopiclone: effects on locomotor activity and brain monoamines in rats". International Journal of Clinical Pharmacology, Therapy, and Toxicology. 23 (3): 121–128. PMID 2581904.
- Sato K, Hong YL, Yang MS, Shibuya T, Kawamoto H, Kitagawa H (April 1985). "Pharmacologic studies of central actions of zopiclone: influence on brain monoamines in rats under stressful condition". International Journal of Clinical Pharmacology, Therapy, and Toxicology. 23 (4): 204–210. PMID 2860074.
- Dündar Y, Dodd S, Strobl J, Boland A, Dickson R, Walley T (July 2004). "Comparative efficacy of newer hypnotic drugs for the short-term management of insomnia: a systematic review and meta-analysis". Human Psychopharmacology. 19 (5): 305–322. doi:10.1002/hup.594. PMID 15252823. S2CID 10888200.
- Blanchard JC, Julou L (March 1983). "Suriclone: a new cyclopyrrolone derivative recognizing receptors labeled by benzodiazepines in rat hippocampus and cerebellum". Journal of Neurochemistry. 40 (3): 601–607. doi:10.1111/j.1471-4159.1983.tb08023.x. PMID 6298365. S2CID 35732735.
- Skerritt JH, Johnston GA (May 1983). "Enhancement of GABA binding by benzodiazepines and related anxiolytics". European Journal of Pharmacology. 89 (3–4): 193–198. doi:10.1016/0014-2999(83)90494-6. PMID 6135616.
- De Deyn PP, Macdonald RL (September 1988). "Effects of non-sedative anxiolytic drugs on responses to GABA and on diazepam-induced enhancement of these responses on mouse neurones in cell culture". British Journal of Pharmacology. 95 (1): 109–120. doi:10.1111/j.1476-5381.1988.tb16554.x. PMC 1854132. PMID 2905900.
- Julou L, Bardone MC, Blanchard JC, Garret C, Stutzmann JM (1983). "Pharmacological studies on zopiclone". Pharmacology. 27 (Suppl 2): 46–58. doi:10.1159/000137911. PMID 6142468.
- Blanchard JC, Boireau A, Julou L (1983). "Brain receptors and zopiclone". Pharmacology. 27 (Suppl 2): 59–69. doi:10.1159/000137912. PMID 6322210.
- Gaillot J, Heusse D, Hougton GW, Marc Aurele J, Dreyfus JF (1982). "Pharmacokinetics and metabolism of zopiclone". International Pharmacopsychiatry. 17 (Suppl 2): 76–91. PMID 7188377.
- Viron B, De Meyer M, Le Liboux A, Frydman A, Maillard F, Mignon F, et al. (April 1990). "Steady state pharmacokinetics of zopiclone during multiple oral dosing (7.5 mg nocte) in patients with severe chronic renal failure". International Clinical Psychopharmacology. 5 (Suppl 2): 95–104. PMID 2387982.
- ^ "Zopiclone". pubchem.ncbi.nlm.nih.gov. U.S. National Library of Medicine. Retrieved 11 June 2018.
- Kratzsch C, Tenberken O, Peters FT, Weber AA, Kraemer T, Maurer HH (August 2004). "Screening, library-assisted identification and validated quantification of 23 benzodiazepines, flumazenil, zaleplone, zolpidem and zopiclone in plasma by liquid chromatography/mass spectrometry with atmospheric pressure chemical ionization". Journal of Mass Spectrometry. 39 (8): 856–72. Bibcode:2004JMSp...39..856K. doi:10.1002/jms.599. PMID 15329838.
- Gustavsen I, Al-Sammurraie M, Mørland J, Bramness JG (May 2009). "Impairment related to blood drug concentrations of zopiclone and zolpidem compared to alcohol in apprehended drivers". Accident Analysis and Prevention. 41 (3): 462–6. doi:10.1016/j.aap.2009.01.011. PMID 19393793.
- Baselt R (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 1677–1679.
- Holbrook AM, Crowther R, Lotter A, Cheng C, King D (January 2000). "Meta-analysis of benzodiazepine use in the treatment of insomnia". CMAJ. 162 (2): 225–233. PMC 1232276. PMID 10674059.
- Blaschke G, Hempel G, Müller WE (1993). "Preparative and analytical separation of the zopiclone enantiomers and determination of their affinity to the benzodiazepine receptor binding site". Chirality. 5 (6): 419–421. doi:10.1002/chir.530050605. PMID 8398600.
- Fernandez C, Maradeix V, Gimenez F, Thuillier A, Farinotti R (November 1993). "Pharmacokinetics of zopiclone and its enantiomers in Caucasian young healthy volunteers". Drug Metabolism and Disposition. 21 (6): 1125–1128. PMID 7905394.
- Cimolai N (December 2007). "Zopiclone: is it a pharmacologic agent for abuse?". Canadian Family Physician. 53 (12): 2124–2129. PMC 2231551. PMID 18077750.
- Griffiths RR, Johnson MW (2005). "Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds". The Journal of Clinical Psychiatry. 66 (Suppl 9): 31–41. PMID 16336040.
- Hoffmann F, Pfannkuche M, Glaeske G (January 2008). "". Der Nervenarzt (in German). 79 (1): 67–72. doi:10.1007/s00115-007-2280-6. PMID 17457554. S2CID 31103719.
- Bramness JG, Olsen H (May 1998). "". Tidsskrift for den Norske Laegeforening (in Norwegian). 118 (13): 2029–2032. PMID 9656789.
- Ströhle A, Antonijevic IA, Steiger A, Sonntag A (January 1999). "". Der Nervenarzt (in German). 70 (1): 72–75. doi:10.1007/s001150050403. PMID 10087521. S2CID 42630879.
- Sikdar S (July 1998). "Physical dependence on zopiclone. Prescribing this drug to addicts may give rise to iatrogenic drug misuse". BMJ. 317 (7151): 146. doi:10.1136/bmj.317.7151.146. PMC 1113504. PMID 9657802.
- Kuntze MF, Bullinger AH, Mueller-Spahn F (September 2002). "Excessive use of zopiclone: a case report" (PDF). Swiss Medical Weekly. 132 (35–36): 523. doi:10.4414/smw.2002.10074. PMID 12506335. S2CID 33400840. Archived from the original (PDF) on 2016-03-03. Retrieved 2008-12-18.
- Jones AW, Holmgren A, Kugelberg FC (April 2007). "Concentrations of scheduled prescription drugs in blood of impaired drivers: considerations for interpreting the results". Therapeutic Drug Monitoring. 29 (2): 248–260. doi:10.1097/FTD.0b013e31803d3c04. PMID 17417081. S2CID 25511804.
- Bramness JG, Skurtveit S, Mørland J (August 1999). "". Tidsskrift for den Norske Laegeforening (in Norwegian). 119 (19): 2820–2821. PMID 10494203.
- Menzin J, Lang KM, Levy P, Levy E (January 2001). "A general model of the effects of sleep medications on the risk and cost of motor vehicle accidents and its application to France". PharmacoEconomics. 19 (1): 69–78. doi:10.2165/00019053-200119010-00005. PMID 11252547. S2CID 45013069.
- Kintz P, Villain M, Ludes B (April 2004). "Testing for the undetectable in drug-facilitated sexual assault using hair analyzed by tandem mass spectrometry as evidence". Therapeutic Drug Monitoring. 26 (2): 211–214. doi:10.1097/00007691-200404000-00022. PMID 15228167. S2CID 46445345.
- Yanagita T (1982). "Dependence potential of zopiclone studied in monkeys". International Pharmacopsychiatry. 17 (2): 216–227. PMID 6892368.
External links
- Detailed pharmacological information Archived 2006-04-04 at the Wayback Machine
- Scheduling recommendation (PDF file)
- Details on scheduling
- Erowid zopiclone vault
- Support for zopiclone dependency/addiction Archived 2015-04-02 at the Wayback Machine
| Insomnia medications | |
|---|---|
| GABAA receptor positive modulators |
|
| Antihistamines (H1 receptor inverse agonists) |
|
| Orexin receptor antagonists | |
| Melatonin receptor agonists | |
| Miscellaneous |
|
| |
| GABAA receptor positive modulators | |
|---|---|
| Alcohols | |
| Barbiturates |
|
| Benzodiazepines |
|
| Carbamates | |
| Flavonoids |
|
| Imidazoles | |
| Kava constituents | |
| Monoureides | |
| Neuroactive steroids |
|
| Nonbenzodiazepines | |
| Phenols | |
| Piperidinediones | |
| Pyrazolopyridines | |
| Quinazolinones | |
| Volatiles/gases |
|
| Others/unsorted |
|
| See also: Receptor/signaling modulators • GABA receptor modulators • GABA metabolism/transport modulators | |