| Revision as of 05:27, 10 July 2015 editVaccinationist (talk | contribs)Extended confirmed users4,734 editsNo edit summary← Previous edit | Revision as of 04:25, 15 July 2015 edit undoDavidruben (talk | contribs)Extended confirmed users18,994 edits →Mechanism of action: almost never used now in UK for trimethoprim alone as effective & less side effects. Pneumocystis carnii its only common indicationNext edit → | ||
| Line 146: | Line 146: | ||
| ==Mechanism of action== | ==Mechanism of action== | ||
| ] synthesis pathway]] | ] synthesis pathway]] | ||
| Trimethoprim binds to dihydrofolate reductase and inhibits the reduction of ] (DHF) to ] (THF).<ref name = drugs82/> THF is an essential precursor in the thymidine synthesis pathway and interference with this pathway inhibits bacterial DNA synthesis.<ref name = drugs82/> Trimethoprim's affinity for bacterial dihydrofolate reductase is several thousand times greater than its affinity for human dihydrofolate reductase.<ref name = drugs82/> ] inhibits dihydropteroate synthetase, an enzyme involved further upstream in the same pathway.<ref name = drugs82/> ] |
Trimethoprim binds to dihydrofolate reductase and inhibits the reduction of ] (DHF) to ] (THF).<ref name = drugs82/> THF is an essential precursor in the thymidine synthesis pathway and interference with this pathway inhibits bacterial DNA synthesis.<ref name = drugs82/> Trimethoprim's affinity for bacterial dihydrofolate reductase is several thousand times greater than its affinity for human dihydrofolate reductase.<ref name = drugs82/> ] inhibits dihydropteroate synthetase, an enzyme involved further upstream in the same pathway.<ref name = drugs82/> ] was commonly used in combination due to claimed synergistic effects,<ref name = drugs82/> and reduced development of resistance,<ref name = drugs82>{{cite journal|last=Brogden|first=RN|author2=Carmine, AA |author3=Heel, RC |author4=Speight, TM |author5= Avery, GS |title=Trimethoprim: a review of its antibacterial activity, pharmacokinetics and therapeutic use in urinary tract infections.|journal=Drugs|date=June 1982|volume=23|issue=6|pages=405–30|doi=10.2165/00003495-198223060-00001|pmid=7049657}}</ref> but now has a limited clinical role.<ref>{{cite journal |author=Brumfitt, W; Hamilton-Miller, JM |title=Reassessment of the rationale for the combinations of sulphonamides with diaminopyrimidines | journal=Journal of Chemotherapy |date=December 1993|volume=5|issue=6|pages=465–9|pmid=8195839}}</ref> | ||
| ] | ] | ||
Revision as of 04:25, 15 July 2015
Pharmaceutical compound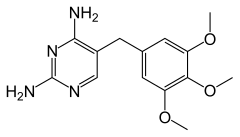 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684025 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 90–100% |
| Protein binding | 44% |
| Metabolism | hepatic |
| Elimination half-life | 8-12 hours |
| Excretion | Urine (50–60%), faeces (4%) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.010.915 |
| Chemical and physical data | |
| Formula | C14H18N4O3 |
| Molar mass | 290.32 g/mol g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Trimethoprim (INN) /traɪˈmɛθəprɪm/ is a bacteriostatic antibiotic used mainly in the prevention and treatment of urinary tract infections.
It belongs to the class of chemotherapeutic agents known as dihydrofolate reductase inhibitors. Trimethoprim was formerly marketed by GlaxoSmithKline under trade names including Proloprim, Monotrim, and Triprim, but these trade names have been licensed to various generic pharmaceutical manufacturers.
Trimethoprim is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.
Trimethoprim and sulfamethoxazole are commonly used in combination.
The abbreviations TRI and TMP (in clinical use) or W (in laboratory use) are common for referring to trimethoprim, but abbreviating drug names is not best practice in medicine.
Medical uses
It is primarily used in the treatment of urinary tract infections, although it may be used against any susceptible aerobic bacterial species. It may also be used to treat and prevent Pneumocystis jiroveci pneumonia. It is generally not recommended for the treatment of anaerobic infections such as pseudomembranous colitis (the leading cause for antibiotic-induced diarrhoea).
| Micro-organism name | Susceptible to trimethoprim? |
|---|---|
| Aerobic bacteria | |
| Acinetobacter sp. | No |
| Aeromonas sp. | Yes |
| Burkholderia cepacia | Yes |
| Burkholderia pseudomallei | No |
| Campylobacter coli | No |
| Campylobacter jejuni | No |
| Citrobacter freundii | Yes |
| Corynebacterium jeikeium | No |
| Enterobacter sp. | Yes |
| Enterococcus sp. | No |
| Escherichia coli sp. | Yes |
| Haemophilus influenzae | Yes |
| Klebsiella sp. | Yes |
| Moraxella catarrhalis | No |
| Morganella sp. | Yes |
| Neisseria meningitidis | No |
| Proteus mirabilis | Yes |
| Proteus vulgaris | Yes |
| Providencia sp. | Yes |
| Pseudomonas aeruginosa | No |
| Salmonella sp. | Yes |
| Serratia sp. | Yes |
| Shigella sp. | No |
| Staphylococcus aureus | Yes |
| Staphylococcus saprophyticus | Yes |
| Stenotrophomonas maltophilia | No |
| Streptococcus - groups A, B, C, G | Yes |
| Streptococcus pneumoniae | No |
| Streptococcus viridans group | No |
| Yersinia sp. | Yes |
Mechanism of action

Trimethoprim binds to dihydrofolate reductase and inhibits the reduction of dihydrofolic acid (DHF) to tetrahydrofolic acid (THF). THF is an essential precursor in the thymidine synthesis pathway and interference with this pathway inhibits bacterial DNA synthesis. Trimethoprim's affinity for bacterial dihydrofolate reductase is several thousand times greater than its affinity for human dihydrofolate reductase. Sulfamethoxazole inhibits dihydropteroate synthetase, an enzyme involved further upstream in the same pathway. Trimethoprim and sulfamethoxazole was commonly used in combination due to claimed synergistic effects, and reduced development of resistance, but now has a limited clinical role.

Co-trimoxazole
Trimethoprim was commonly (from 1969 to 1980 in the UK) used in a 1:5 combination with sulfamethoxazole, a sulfonamide antibiotic, which inhibits an earlier step in the folate synthesis pathway. This combination, also known as co-trimoxazole, TMP-sulfa, or TMP-SMX, results in an in vitro synergistic antibacterial effect by inhibiting successive steps in folate synthesis. This claimed benefit was not seen in general clinical use.
The combination's use has been declining due to reports of sulfamethoxazole having bone marrow toxicity, resistance and lack of greater efficacy in treating common urinary and chest infections, and side effects of antibacterial sulfonamides. As a consequence, the use of co-trimoxazole was restricted in 1995 following the availability of trimethoprim (not in combination) in 1980.
With its greater efficacy against a limited number of bacteria, co-trimoxazole remains indicated for some infections; for example, it is used as prophylaxis in patients at risk for Pneumocystis jirovecii pneumonia (e.g. AIDS patients and those with some hematological malignancies) and as therapy in Whipple's disease. Gram-positive bacteria are generally or moderately susceptible.
Contraindications and reactions
Trimethoprim can cause thrombocytopenia (low levels of platelets) by lowering folic acid levels; this may also cause megaloblastic anemia. Trimethoprim antagonises the epithelial sodium channel in the distal tubule, thus acting like amiloride. This can cause hyperkalemia. Trimethoprim also competes with creatinine for secretion into the renal tubule. This can cause an artefactual rise in the serum creatinine. Use in EHEC infections may lead to an increase in expression of Shiga toxin. Because it crosses the placenta and can affect folate metabolism, trimethoprim is relatively contraindicated during pregnancy, especially the first trimester. It may be involved in a reaction similar to disulfiram when alcohol is consumed after it is used, in particular when used in combination with sulfamethoxazole. The trophoblasts in the early fetus are sensitive to changes in the folate cycle. A recent study has found a doubling in the risk of miscarriage in women exposed to trimethoprim in the early pregnancy.
See also
References
- "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ^ Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ^ Brogden, RN; Carmine, AA; Heel, RC; Speight, TM; Avery, GS (June 1982). "Trimethoprim: a review of its antibacterial activity, pharmacokinetics and therapeutic use in urinary tract infections". Drugs. 23 (6): 405–30. doi:10.2165/00003495-198223060-00001. PMID 7049657.
- Brumfitt, W; Hamilton-Miller, JM (December 1993). "Reassessment of the rationale for the combinations of sulphonamides with diaminopyrimidines". Journal of Chemotherapy. 5 (6): 465–9. PMID 8195839.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19280600, please use {{cite journal}} with
|pmid=19280600instead. - Brumfitt W, Hamilton-Miller JM (December 1993). "Reassessment of the rationale for the combinations of sulphonamides with diaminopyrimidines". J Chemother. 5 (6): 465–9. PMID 8195839.
- Brumfitt W, Hamilton-Miller JM (February 1993). "Limitations of and indications for the use of co-trimoxazole". J Chemother. 6 (1): 3–11. PMID 8071675.
- Bean DC, Livermore DM, Papa I, Hall LM (November 2005). "Resistance among Escherichia coli to sulphonamides and other antimicrobials now little used in man". J Antimicrob Chemother. 56 (5): 962–4. doi:10.1093/jac/dki332. PMID 16150859.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Felmingham D, Reinert RR, Hirakata Y, Rodloff A (September 2002). "Increasing prevalence of antimicrobial resistance among isolates of Streptococcus pneumoniae from the PROTEKT surveillance study, and compatative in vitro activity of the ketolide, telithromycin". J Antimicrob Chemother. 50 (Suppl S1): 25–37. doi:10.1093/jac/dkf808. PMID 12239226.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Johnson JR, Manges AR, O'Bryan TT, Riley LW (June 29, 2002). "A disseminated multidrug-resistant clonal group of uropathogenic Escherichia coli in pyelonephritis". Lancet. 359 (9325): 2249–51. doi:10.1016/S0140-6736(02)09264-4. PMID 12103291.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lawrenson RA, Logie JW (December 2001). "Antibiotic failure in the treatment of urinary tract infections in young women". J Antimicrob Chemother. 48 (6): 895–901. doi:10.1093/jac/48.6.895. PMID 11733475. - suggest some small advantage in UTIs
- "Co-trimoxazole use restricted". Drug Ther Bull. 33 (12): 92–3. December 1995. doi:10.1136/dtb.1995.331292. PMID 8777892.
- Kimmitt PT, Harwood CR, Barer MR (2000). "Toxin Gene Expression by Shiga Toxin-producing Escherichia coli: The Role of Antibiotics and the Bacterial SOS Response" (pdf). Emerg Infect Dis. 6 (5): 458–465. doi:10.3201/eid0605.000503. PMC 2627954. PMID 10998375.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Use extra precautions when taking the contraceptive pill". netdoctor.co.uk.
- Edwards DL, Fink PC, van Dyke PO (1986). "Disulfiram-like reaction associated with intravenous trimethoprim-sulfamethoxazole and metronidazole". J Clinical pharmacy. 5 (12): 999–1000. PMID 3492326.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Heelon MW; White M (1998). "Disulfiram cotrimoxazole reaction". J Pharmacotherapy. 18 (4): 869–870. PMID 9692665.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Andersen JT, Petersen M, Jimenez-Solem E, Broedbaek K, Andersen EW, Andersen NL, Afzal S, Torp-Pedersen C, Keiding N, Poulsen HE (2013). "Trimethoprim use in early pregnancy and the risk of miscarriage: a register-based nationwide cohort study". Epidemiology and Infection. 141 (8): 1749–1755. doi:10.1017/S0950268812002178. PMID 23010291.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
External links
- Nucleic acid inhibitors (PDF file).
| Antibacterials that inhibit nucleic acid (J01E, J01M) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antifolates (inhibit bacterial purine metabolism, thereby inhibiting DNA and RNA synthesis) |
| ||||||||||||||||
| Quinolones (inhibit bacterial topoisomerase and/or DNA gyrase, thereby inhibiting DNA replication) |
| ||||||||||||||||
| Anaerobic DNA inhibitors |
| ||||||||||||||||
| RNA synthesis |
| ||||||||||||||||
| |||||||||||||||||