| Revision as of 01:41, 26 February 2009 edit173.89.168.152 (talk) →Reproductive effects← Previous edit | Revision as of 05:45, 26 February 2009 edit undo218.186.12.208 (talk) (edit summary removed)Next edit → | ||
| Line 143: | Line 143: | ||
| * longer decision times, leading to slower responses to driving situations; and | * longer decision times, leading to slower responses to driving situations; and | ||
| * a more cautious driving style, including slower average speed and greater following distance. | * a more cautious driving style, including slower average speed and greater following distance. | ||
| bob marley says cannabis is good | |||
| Whereas these results indicate a 'change' from normal conditions, they do not necessarily reflect 'impairment' in terms of performance effectiveness, since few studies report increased accident risk. However, the results do suggest 'impairment' in terms of performance efficiency given that some of these behaviors may limit the available resources to cope with any additional, unexpected or high demand, events. Indeed, compensatory effort may be invoked to offset impairment in the driving task. Subjects under cannabis treatment may perceive that they are impaired and may strategically compensate, for example, by not overtaking, by slowing down and by focusing their attention when they know a response will be required. This compensatory effort may be one reason for the failure to implicate cannabis consumption as an accident ], particularly at lower doses or with more than about one hour after consumption. According to the TRL study, the same compensatory behavior could also be an unconscious adaptation, similar to reduced driving speeds used by a sleepy driver. | Whereas these results indicate a 'change' from normal conditions, they do not necessarily reflect 'impairment' in terms of performance effectiveness, since few studies report increased accident risk. However, the results do suggest 'impairment' in terms of performance efficiency given that some of these behaviors may limit the available resources to cope with any additional, unexpected or high demand, events. Indeed, compensatory effort may be invoked to offset impairment in the driving task. Subjects under cannabis treatment may perceive that they are impaired and may strategically compensate, for example, by not overtaking, by slowing down and by focusing their attention when they know a response will be required. This compensatory effort may be one reason for the failure to implicate cannabis consumption as an accident ], particularly at lower doses or with more than about one hour after consumption. According to the TRL study, the same compensatory behavior could also be an unconscious adaptation, similar to reduced driving speeds used by a sleepy driver. | ||
| Line 184: | Line 184: | ||
| Cannabis also has been shown to have a synergistic cytotoxic effect on lung cancer cell cultures in vitro with the food additive ] (BHA) and possibly the related compound ] (BHT). The study concluded, "Exposure to marijuana smoke in conjunction with BHA, a common food additive, may promote deleterious health effects in the lung." BHA & BHT are human-made fat preservatives, and are found in many packaged foods including: plastics in boxed Cereal, Jello, Slim Jims, and more.<ref>{{cite journal |author=Sarafian TA, Kouyoumjian S, Tashkin D, Roth MD |title=Synergistic cytotoxicity of Delta(9)-tetrahydrocannabinol and butylated hydroxyanisole |journal=Toxicol. Lett. |volume=133 |issue=2-3 |pages=171–9 |year=2002 |month=July |pmid=12119125 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0378427402001340}} | Cannabis also has been shown to have a synergistic cytotoxic effect on lung cancer cell cultures in vitro with the food additive ] (BHA) and possibly the related compound ] (BHT). The study concluded, "Exposure to marijuana smoke in conjunction with BHA, a common food additive, may promote deleterious health effects in the lung." BHA & BHT are human-made fat preservatives, and are found in many packaged foods including: plastics in boxed Cereal, Jello, Slim Jims, and more.<ref>{{cite journal |author=Sarafian TA, Kouyoumjian S, Tashkin D, Roth MD |title=Synergistic cytotoxicity of Delta(9)-tetrahydrocannabinol and butylated hydroxyanisole |journal=Toxicol. Lett. |volume=133 |issue=2-3 |pages=171–9 |year=2002 |month=July |pmid=12119125 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0378427402001340}} | ||
| </ref> | </ref> | ||
| ===Memory=== | |||
| Studies on cannabis and memory are hindered by small sample sizes, confounding drug abuse, and other factors.<ref name=memoryhindered>{{cite journal |author=Riedel G, Davies SN |title=Cannabinoid function in learning, memory and plasticity |journal=Handb Exp Pharmacol |volume= |issue=168 |pages=445–77 |year=2005 |pmid=16596784 |doi= |url=http://www.springerlink.comopenurl.asp?genre=chapter&issn=0171-2004&volume=&page=445}}</ref> The strongest evidence regarding cannabis and memory focuses on its short-term negative effects on short-term and working memory.<ref name=memoryhindered/> | |||
| A 2008 review of the evidence surrounding the acute impact on memory concluded that cannabinoids impair all aspects of short-term memory, especially short-term episodic and working memory.<ref name=acutememory>{{cite journal |author=Ranganathan M, D'Souza DC |title=The acute effects of cannabinoids on memory in humans: a review |journal=Psychopharmacology (Berl.) |volume=188 |issue=4 |pages=425–44 |year=2006 |month=November |pmid=17019571 |doi=10.1007/s00213-006-0508-y |url=}}</ref> One small study found that no learning occurred during the 2 hour period in which the subjects were "stoned".<ref>{{cite journal |author=Curran HV, Brignell C, Fletcher S, Middleton P, Henry J |title=Cognitive and subjective dose-response effects of acute oral Delta 9-tetrahydrocannabinol (THC) in infrequent cannabis users |journal=Psychopharmacology (Berl.) |volume=164 |issue=1 |pages=61–70 |year=2002 |month=October |pmid=12373420 |doi=10.1007/s00213-002-1169-0 |url=}}</ref> Long-term effects on memory may be balanced by ] effects of THC against ].<ref>{{cite journal |author=van der Stelt M, Veldhuis WB, Bär PR, Veldink GA, Vliegenthart JF, Nicolay K |title=Neuroprotection by Delta9-tetrahydrocannabinol, the main active compound in marijuana, against ouabain-induced in vivo excitotoxicity |journal=J. Neurosci. |volume=21 |issue=17 |pages=6475–9 |year=2001 |month=September |pmid=11517236 |doi= |url=http://www.jneurosci.org/cgi/pmidlookup?view=long&pmid=11517236}}</ref> | |||
| ===Appetite=== | |||
| ⚫ | Clinical studies and survey data have found that cannabis increases food enjoyment and interest in food.<ref>Ad Hoc Group of Experts. "" (Workshop on the Medical Utility of Marijauana). ].</ref><ref name=Bonsor>Bonsor, Kevin. "". ]. Retrieved on 2007-11-03</ref> | ||
| ⚫ | Scientists have claimed to be able to explain what causes the increase in appetite, concluding that "]s in the hypothalamus activate cannabinoid receptors that are responsible for maintaining food intake".<ref name=Bonsor/> | ||
| ==Long-term effects== | ==Long-term effects== | ||
| Line 200: | Line 191: | ||
| Research has demonstrated that human ] contains receptors which are stimulated by substances like THC and other cannabis-related chemicals. Tests have implied that smoking of marijuana could impact the sperm's functions, though this impact is unknown.<ref>{{cite journal | title=Evidence that anandamide-signaling regulates human sperm functions required for fertilization | author=H. Schuel ''et al.'' | journal=Molecular Reproduction and Development | month=September | year=2002 | volume=63 | issue=3 | pages=376–387 | url=http://www3.interscience.wiley.com/cgi-bin/fulltext/98517201/PDFSTART | doi=10.1002/mrd.90021}}</ref> | Research has demonstrated that human ] contains receptors which are stimulated by substances like THC and other cannabis-related chemicals. Tests have implied that smoking of marijuana could impact the sperm's functions, though this impact is unknown.<ref>{{cite journal | title=Evidence that anandamide-signaling regulates human sperm functions required for fertilization | author=H. Schuel ''et al.'' | journal=Molecular Reproduction and Development | month=September | year=2002 | volume=63 | issue=3 | pages=376–387 | url=http://www3.interscience.wiley.com/cgi-bin/fulltext/98517201/PDFSTART | doi=10.1002/mrd.90021}}</ref> | ||
| In recent studies, marijuana has been shown to increase testosterone levels in females, resulting in unwanted facial hair; and decrease testosterone levels in males, hindering the maturation process. | |||
| ====Pregnancy==== | ====Pregnancy==== | ||
| One study by Zuckerman and colleagues{{Who|date=October 2008}} included a large sample of women with a substantial prevalence of marijuana use that was verified by ] and no increased ] of ] was found in the ] group. Compared to ], similar types of facial features and related symptoms are not associated with prenatal marijuana exposure.<ref>{{cite journal | title=Analysis of facial shape in children gestationally exposed to marijuana, alcohol, and/or cocaine | author=S.J. Astley, S.K. Clarren, R.E. Little, P.D. Sampson, J.R. Daling | journal=Pediatrics | month=January | year=1992 | volume=89|issue=1 |pages=67–77}}</ref> THC passes into the ] and may affect a breastfed ].<ref>{{cite book | title=The Merck Manual of Medical Information (Home Edition) | author=R. Berkow MD ''et al.'' | year=1997 | pages=449}}</ref> Many studies about drug use during pregnancy are self-administered by the applicants and not always ]. The ] of using illicit drugs while pregnant discourages honest reporting and can invalidate the results. Studies show that women who consume cannabis while they are pregnant may also be likely to consume ], ], ], or other ], which makes it difficult to deduce scientific facts about just marijuana use from statistical results. Very few large, well-controlled ] studies have taken place to understand the connection of marijuana use and pregnancy.{{Fact|date=October 2008}} | One study by Zuckerman and colleagues{{Who|date=October 2008}} included a large sample of women with a substantial prevalence of marijuana use that was verified by ] and no increased ] of ] was found in the ] group. Compared to ], similar types of facial features and related symptoms are not associated with prenatal marijuana exposure.<ref>{{cite journal | title=Analysis of facial shape in children gestationally exposed to marijuana, alcohol, and/or cocaine | author=S.J. Astley, S.K. Clarren, R.E. Little, P.D. Sampson, J.R. Daling | journal=Pediatrics | month=January | year=1992 | volume=89|issue=1 |pages=67–77}}</ref> THC passes into the ] and may affect a breastfed ].<ref>{{cite book | title=The Merck Manual of Medical Information (Home Edition) | author=R. Berkow MD ''et al.'' | year=1997 | pages=449}}</ref> Many studies about drug use during pregnancy are self-administered by the applicants and not always ]. The ] of using illicit drugs while pregnant discourages honest reporting and can invalidate the results. Studies show that women who consume cannabis while they are pregnant may also be likely to consume ], ], ], or other ], which makes it difficult to deduce scientific facts about just marijuana use from statistical results. Very few large, well-controlled ] studies have taken place to understand the connection of marijuana use and pregnancy.{{Fact|date=October 2008}} | ||
| Line 227: | Line 217: | ||
| The direction of causation was more directly examined in a study by Dr. Mikkel Arendt of Aarhus University in Risskov, Denmark, and colleagues, which found that individuals treated for psychotic episodes following cannabis use had the same likelihood of having a mother, sister or other "first-degree" relative with schizophrenia as did the individuals who had actually been treated for schizophrenia themselves. This suggests that the psychosis blamed on cannabis use is in fact the result of a genetic predisposition towards schizophrenia. "These people would have developed schizophrenia whether or not they used cannabis <ref></ref> | The direction of causation was more directly examined in a study by Dr. Mikkel Arendt of Aarhus University in Risskov, Denmark, and colleagues, which found that individuals treated for psychotic episodes following cannabis use had the same likelihood of having a mother, sister or other "first-degree" relative with schizophrenia as did the individuals who had actually been treated for schizophrenia themselves. This suggests that the psychosis blamed on cannabis use is in fact the result of a genetic predisposition towards schizophrenia. "These people would have developed schizophrenia whether or not they used cannabis <ref></ref> | ||
| ===Behavioral effects=== | |||
| ⚫ | |||
| ⚫ | Government studies often point to statistical data accumulated by methods like the ] (NHSDA), the ] study (MTF), and the ] (ADAM) program, which claim lower ] and higher ] rates among users than nonusers. However, the major contributor to a lack of credibility in these studies, is that in many cases, like with NHSDA and MTF, these surveys are usually self-administered and may be anonymous. The likeliness of over or under representing data definitely undermines the effectiveness of these instruments.<ref name="abadinsky" /> The ADAM study is conducted anonymously, but only seeks information from a sample of people who have been arrested for drug-related offenses. Socially deviant behavior may be found more frequently in individuals of the criminal justice system compared to those in the general population, including non users. In response, independent studies of college students have shown that there was no difference in grade point average, and achievement, between marijuana users and nonusers, but the users had a little more difficulty deciding on career goals, and a smaller number were seeking advanced professional degrees.<ref>{{cite journal | title=Marihuana and Psychosocial Adjustment | author=N.Q. Brill, R.L. Christie | journal=Archives of General Psychiatry | year=1974 | volume= 31 | pages= 713–719}}</ref> Laboratory studies of the relationship between motivation and marijuana outside of the classroom, where volunteers worked on operant tasks for a wage representing a working world model, also fail to distinguish a noticeable difference between users and non users.<ref>{{cite book | chapter=The Effects of Marihuana Use on Human Operant Behavior: Individual Data…| author=H.H. Mendelson, J.C. Kuehnle, I. Greenberg; N.K. Mello | title=Pharmacology of Marihuana | location= New York | publisher=Academic Press | year=1976 | volume= 2 | pages= 643–653}}</ref> | ||
| A 2005 meta analysis of available data which evaluated several hypotheses regarding the correlation of cannabis and psychosis found that there is no support for the hypothesis that cannabis can be cause cases of psychosis which would not have occurred otherwise, however further study is needed to explore the correlation between cannabis and other types of psychosis patients.<ref>{{cite journal | |||
| |author=Degenhardt L, Hall W, Lynskey M | |||
| |title=Comorbidity between cannabis use and psychosis: Modelling some possible relationships. Technical Report No. 121 | |||
| |publisher=Sydney: National Drug and Alcohol Research Centre | |||
| |year=2001 | |||
| |url=http://ndarc.med.unsw.edu.au/NDARCWeb.nsf/resources/TR_18/$file/TR.121.PDF | |||
| |accessdate=19.18.2006 | |||
| ⚫ | |||
| ⚫ | At least one study has shown a decrease in depression in cannabis users.<ref name=autogenerated2>{{cite journal | title=Decreased depression in marijuana users | author=T.F. Denson, M. Earleywine | journal=Addictive Behaviors | date= June 20, 2005|url=http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6VC9-4GFCR48-5&_user=10&_coverDate=06%2F20%2F2005&_rdoc=1&_fmt=summary&_orig=browse&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=7dac506ad701a12cddfe8dd713f77138}}</ref> | ||
| ⚫ | |||
| ⚫ | ====Gateway drug hypothesis==== | ||
| ⚫ | {{Main|Gateway drug theory#Cannabis}} | ||
| ⚫ | The ] hypothesis asserts that the use of cannabis may ultimately lead to the use of ]. For the most part, it was commonly thought that cannabis gateways to other drugs because of ] factors. For example, the ] of cannabis in many countries associates its users with ] promoting the ]. | ||
| ⚫ | A July 2006 study by Ellgren ''et al.''<ref>{{cite journal|title=Adolescent Cannabis Exposure Alters Opiate Intake and Opioid Limbic Neuronal Populations in Adult Rats| author=Maria Ellgren, Sabrina M Spano & Yasmin L Hurd|journal=Neuropsychopharmacology|location=advance online| date=July 5, 2006|url=http://www.nature.com/npp/journal/vaop/ncurrent/full/1301127a.html|format={{Dead link|date=June 2008}} – <sup></sup>}}</ref> strictly tested ]s for the biological mechanism of the gateway drug effect. The study administered 6 "]" (28 and 49 days old) rats delta-9-tetrahydrocannabinol, and 6 were the ]. One week after the first part was completed, ] were inserted in the ] of all of the adult rats and they were able to self-administer themselves ] by pushing a lever. The study found that initially both groups behaved the same and began to self-administer heroin frequently, but then stabilized at different levels. The rats that had previously been administered THC consumed about 1.5 times more heroin than those that had not. Because many THC receptors interact with the opioid system, the study surmised that adolescent cannabis use overstimulates and alters the pleasure and reward structures of the brain, thus increasing the already high risk of addiction for people who start to use heroin. However, the rats took up self-administration at the same rate regardless of adolescent THC exposure, and observed levels of "drug-seeking behavior" were also the same. <ref>{{cite journal|title=Adolescent Cannabis Exposure Alters Opiate Intake and Opioid Limbic Neuronal Populations in Adult Rats| author=Maria Ellgren, Sabrina M Spano & Yasmin L Hurd|journal=Neuropsychopharmacology|location=advance online| date=July 5, 2006|url=http://www.nature.com/npp/journal/vaop/ncurrent/full/1301127a.html|format={{Dead link|date=June 2008}} – <sup></sup>}}</ref> Other studies have shown that the dopamine system is independent of the THC receptor glands thus negating these negative effects. {{Fact|date=February 2008}} ] Ian Stolerman, from ], finds the biological cannabis gateway drug effect "somewhat preliminary", and states "it's too early to say there's a consensus, but a small number of studies like this suggest that there is a physiological basis for this effect." Other drugs, he notes, such as cocaine and ] are involved in another brain pathway called the ]. Cells in that system also interact with THC receptors and could be modified by cannabis exposure.<ref>{{cite news|author=Michael Hopkin|title=Rats taking cannabis get taste for heroin|work=]|date=July 5, 2006|url=http://www.nature.com/news/2006/060703/full/060703-9.html}}</ref> Cannabinoid receptors are 10 times more prevalent in the brain than ]. According to Dr. Hurd, one of the study leaders, two other drugs that also stimulate opioid cells, and could therefore also feasibly cause a gateway effect, are ] and alcohol. | ||
| ⚫ | However, a December 2006 study by the ]<ref></ref><ref></ref> challenges these findings. A 12 year study on 214 boys from ages 10-12 showed that adolescents who used marijuana prior to using other drugs, including alcohol and tobacco, were no more likely to develop a substance abuse disorder than other subjects in the study. "This evidence supports what's known as the common liability model ... states the likelihood that someone will transition to the use of illegal drugs is determined not by the preceding use of a particular drug, but instead by the user's individual tendencies and environmental circumstances," investigators stated in a press release. They added, "The emphasis on the drugs themselves, rather than other, more important factors that shape a person's behavior, has been detrimental to drug policy and prevention programs." | ||
| ⚫ | Models used in a 2002 study<ref></ref> by ] cast doubt on the gateway effect and show "that the marijuana gateway effect is not the best explanation for the link between marijuana use and the use of harder drugs," as noted by Andrew Morral, associate director of RAND's Public Safety and Justice unit and lead author of the study. | ||
| ⚫ | ===Co-occurrence of mental illness=== | ||
| ⚫ | Studies have shown that a risk does exist in some individuals with a predisposition to mental illness to develop symptoms of ].<ref>{{cite journal | title=Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people | author=Cécile Henquet, Lydia Krabbendam, Janneke Spauwen, Charles Kaplan, Roselind Lieb, Hans-Ulrich Wittchen and Jim van Os | journal=British Medical Journal | month= December | year= 2004 | volume= 330 | issue= 11 | doi=10.1136/bmj.38267.664086.63 | pages=11 | pmid=15574485}}</ref> The risk was found to be directly related to high dosage and frequency of use, early age of introduction to the drug, and was especially pronounced for those with a predisposition for mental illness. These results have been questioned as being biased by failing to account for medicinal versus recreational usage<ref name=autogenerated2 /> — critics contend it could be a causal relationship, or it could be that people who are susceptible to mental problems tend to smoke cannabis, or it could be connected to the criminalization of cannabis. Another important question is whether the observed symptoms of mental illness are actually connected to development of a permanent ]; cannabis may trigger latent conditions, or be part of a complex coordination of causes of mental illness, referred to in ] as the ]. People with developed psychological disorders are known to ] their symptoms with cannabis as well, although one study has claimed that those with a predisposition for psychosis did not show a statistically significant increase in likelihood of cannabis use four years later.<ref>{{cite journal | title=Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people | author=Cécile Henquet, Lydia Krabbendam, Janneke Spauwen, Charles Kaplan, Roselind Lieb, Hans-Ulrich Wittchen and Jim van Os | journal=British Medical Journal | month= December | year= 2004 | volume= 330 | issue= 11 | doi=10.1136/bmj.38267.664086.63 | pages=11 | pmid=15574485}}</ref> | ||
| ⚫ | ====Correlation versus causality==== | ||
| Some studies conclude that there is a ''correlation'' of cannabis use and some symptoms of psychosis, but don't necessarily support the notion that cannabis use is a sufficient or necessary ''cause'' for psychosis. It might be a component cause, part of a complex constellation of factors leading to psychosis, or it might be a correlation without forward causality at all. | Some studies conclude that there is a ''correlation'' of cannabis use and some symptoms of psychosis, but don't necessarily support the notion that cannabis use is a sufficient or necessary ''cause'' for psychosis. It might be a component cause, part of a complex constellation of factors leading to psychosis, or it might be a correlation without forward causality at all. | ||
| Line 251: | Line 248: | ||
| A study that inversely correlated cerebrospinal anandamide (an endogenous cannabinoid) levels with severity of schizophrenia (i.e., that anandamide was released in order to suppress psychosis) suggests that cannabis use may be an effect of schizophrenia or its predisposition, as opposed to a cause.<ref name="anps">{{cite journal |author=Giuffrida A, Leweke FM, Gerth CW, ''et al'' |title=Cerebrospinal anandamide levels are elevated in acute schizophrenia and are inversely correlated with psychotic symptoms |journal=Neuropsychopharmacology |volume=29 |issue=11 |pages=2108–14 |year=2004 |month=November |pmid=15354183 |doi=10.1038/sj.npp.1300558 |url=}}, </ref> | A study that inversely correlated cerebrospinal anandamide (an endogenous cannabinoid) levels with severity of schizophrenia (i.e., that anandamide was released in order to suppress psychosis) suggests that cannabis use may be an effect of schizophrenia or its predisposition, as opposed to a cause.<ref name="anps">{{cite journal |author=Giuffrida A, Leweke FM, Gerth CW, ''et al'' |title=Cerebrospinal anandamide levels are elevated in acute schizophrenia and are inversely correlated with psychotic symptoms |journal=Neuropsychopharmacology |volume=29 |issue=11 |pages=2108–14 |year=2004 |month=November |pmid=15354183 |doi=10.1038/sj.npp.1300558 |url=}}, </ref> | ||
| The fact that the prevalence of cannabis use has increased substantially during the last decades whereas the prevalence of psychotic illness has not suggests no causal relationship.<ref>{{ |
The fact that the prevalence of cannabis use has increased substantially during the last decades whereas the prevalence of psychotic illness has not suggests no causal relationship.<ref>Degenhardt L, Hall W, Lynskey M ,Comorbidity between cannabis use and psychosis: Modelling some possible relationships. Technical Report No. 121. Sydney: National Drug and Alcohol Research Centre. 2001, Retrieved on 19.18.2006</ref> However, this observation is contradicted by that improved methods for treatment with ] has helped to keep down the number of people with long periods of psychosis.{{cn}} | ||
| |author=Degenhardt L, Hall W, Lynskey M | |||
| |title=Comorbidity between cannabis use and psychosis: Modelling some possible relationships. Technical Report No. 121 | |||
| |publisher=Sydney: National Drug and Alcohol Research Centre | |||
| |year=2001 | |||
| |url=http://ndarc.med.unsw.edu.au/NDARCWeb.nsf/resources/TR_18/$file/TR.121.PDF | |||
| |accessdate=19.18.2006 | |||
| }}</ref> | |||
| === |
===Appetite=== | ||
| ⚫ | Clinical studies and survey data have found that cannabis increases food enjoyment and interest in food.<ref>Ad Hoc Group of Experts. "" (Workshop on the Medical Utility of Marijauana). ].</ref><ref name=Bonsor>Bonsor, Kevin. "". ]. Retrieved on 2007-11-03</ref> | ||
| ⚫ | Government studies often point to statistical data accumulated by methods like the ] (NHSDA), the ] study (MTF), and the ] (ADAM) program, which claim lower ] and higher ] rates among users than nonusers. However, the major contributor to a lack of credibility in these studies, is that in many cases, like with NHSDA and MTF, these surveys are usually self-administered and may be anonymous. The likeliness of over or under representing data definitely undermines the effectiveness of these instruments.<ref name="abadinsky" /> The ADAM study is conducted anonymously, but only seeks information from a sample of people who have been arrested for drug-related offenses. Socially deviant behavior may be found more frequently in individuals of the criminal justice system compared to those in the general population, including non users. In response, independent studies of college students have shown that there was no difference in grade point average, and achievement, between marijuana users and nonusers, but the users had a little more difficulty deciding on career goals, and a smaller number were seeking advanced professional degrees.<ref>{{cite journal | title=Marihuana and Psychosocial Adjustment | author=N.Q. Brill, R.L. Christie | journal=Archives of General Psychiatry | year=1974 | volume= 31 | pages= 713–719}}</ref> Laboratory studies of the relationship between motivation and marijuana outside of the classroom, where volunteers worked on operant tasks for a wage representing a working world model, also fail to distinguish a noticeable difference between users and non users.<ref>{{cite book | chapter=The Effects of Marihuana Use on Human Operant Behavior: Individual Data…| author=H.H. Mendelson, J.C. Kuehnle, I. Greenberg; N.K. Mello | title=Pharmacology of Marihuana | location= New York | publisher=Academic Press | year=1976 | volume= 2 | pages= 643–653}}</ref> | ||
| ⚫ | Scientists have claimed to be able to explain what causes the increase in appetite, concluding that "]s in the hypothalamus activate cannabinoid receptors that are responsible for maintaining food intake".<ref name=Bonsor/> | ||
| ⚫ | At least one study has shown a decrease in depression in cannabis users.<ref name=autogenerated2>{{cite journal | title=Decreased depression in marijuana users | author=T.F. Denson, M. Earleywine | journal=Addictive Behaviors | date= June 20, 2005|url=http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6VC9-4GFCR48-5&_user=10&_coverDate=06%2F20%2F2005&_rdoc=1&_fmt=summary&_orig=browse&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=7dac506ad701a12cddfe8dd713f77138}}</ref> | ||
| ⚫ | ====Gateway drug hypothesis==== | ||
| ⚫ | {{Main|Gateway drug theory#Cannabis}} | ||
| ⚫ | The ] hypothesis asserts that the use of cannabis may ultimately lead to the use of ]. For the most part, it was commonly thought that cannabis gateways to other drugs because of ] factors. For example, the ] of cannabis in many countries associates its users with ] promoting the ]. | ||
| ⚫ | A July 2006 study by Ellgren ''et al.''<ref>{{cite journal|title=Adolescent Cannabis Exposure Alters Opiate Intake and Opioid Limbic Neuronal Populations in Adult Rats| author=Maria Ellgren, Sabrina M Spano & Yasmin L Hurd|journal=Neuropsychopharmacology|location=advance online| date=July 5, 2006|url=http://www.nature.com/npp/journal/vaop/ncurrent/full/1301127a.html|format={{Dead link|date=June 2008}} – <sup></sup>}}</ref> strictly tested ]s for the biological mechanism of the gateway drug effect. The study administered 6 "]" (28 and 49 days old) rats delta-9-tetrahydrocannabinol, and 6 were the ]. One week after the first part was completed, ] were inserted in the ] of all of the adult rats and they were able to self-administer themselves ] by pushing a lever. The study found that initially both groups behaved the same and began to self-administer heroin frequently, but then stabilized at different levels. The rats that had previously been administered THC consumed about 1.5 times more heroin than those that had not. Because many THC receptors interact with the opioid system, the study surmised that adolescent cannabis use overstimulates and alters the pleasure and reward structures of the brain, thus increasing the already high risk of addiction for people who start to use heroin. However, the rats took up self-administration at the same rate regardless of adolescent THC exposure, and observed levels of "drug-seeking behavior" were also the same. <ref>{{cite journal|title=Adolescent Cannabis Exposure Alters Opiate Intake and Opioid Limbic Neuronal Populations in Adult Rats| author=Maria Ellgren, Sabrina M Spano & Yasmin L Hurd|journal=Neuropsychopharmacology|location=advance online| date=July 5, 2006|url=http://www.nature.com/npp/journal/vaop/ncurrent/full/1301127a.html|format={{Dead link|date=June 2008}} – <sup></sup>}}</ref> Other studies have shown that the dopamine system is independent of the THC receptor glands thus negating these negative effects. {{Fact|date=February 2008}} ] Ian Stolerman, from ], finds the biological cannabis gateway drug effect "somewhat preliminary", and states "it's too early to say there's a consensus, but a small number of studies like this suggest that there is a physiological basis for this effect." Other drugs, he notes, such as cocaine and ] are involved in another brain pathway called the ]. Cells in that system also interact with THC receptors and could be modified by cannabis exposure.<ref>{{cite news|author=Michael Hopkin|title=Rats taking cannabis get taste for heroin|work=]|date=July 5, 2006|url=http://www.nature.com/news/2006/060703/full/060703-9.html}}</ref> Cannabinoid receptors are 10 times more prevalent in the brain than ]. According to Dr. Hurd, one of the study leaders, two other drugs that also stimulate opioid cells, and could therefore also feasibly cause a gateway effect, are ] and alcohol. | ||
| ⚫ | However, a December 2006 study by the ]<ref></ref><ref></ref> challenges these findings. A 12 year study on 214 boys from ages 10-12 showed that adolescents who used marijuana prior to using other drugs, including alcohol and tobacco, were no more likely to develop a substance abuse disorder than other subjects in the study. "This evidence supports what's known as the common liability model ... states the likelihood that someone will transition to the use of illegal drugs is determined not by the preceding use of a particular drug, but instead by the user's individual tendencies and environmental circumstances," investigators stated in a press release. They added, "The emphasis on the drugs themselves, rather than other, more important factors that shape a person's behavior, has been detrimental to drug policy and prevention programs." | ||
| ⚫ | Models used in a 2002 study<ref></ref> by ] cast doubt on the gateway effect and show "that the marijuana gateway effect is not the best explanation for the link between marijuana use and the use of harder drugs," as noted by Andrew Morral, associate director of RAND's Public Safety and Justice unit and lead author of the study. | ||
| ===Memory=== | ===Memory=== | ||
| Studies on cannabis and memory are hindered by small sample sizes, confounding drug abuse, and other factors.<ref name=memoryhindered>{{cite journal |author=Riedel G, Davies SN |title=Cannabinoid function in learning, memory and plasticity |journal=Handb Exp Pharmacol |volume= |issue=168 |pages=445–77 |year=2005 |pmid=16596784 |doi= |url=http://www.springerlink.comopenurl.asp?genre=chapter&issn=0171-2004&volume=&page=445}}</ref> The strongest evidence regarding cannabis and memory focuses on its short-term negative effects on short-term and working memory.<ref name=memoryhindered/> Evidence also suggests that long-term effects exist, but these appear to be reversible except |
Studies on cannabis and memory are hindered by small sample sizes, confounding drug abuse, and other factors.<ref name=memoryhindered>{{cite journal |author=Riedel G, Davies SN |title=Cannabinoid function in learning, memory and plasticity |journal=Handb Exp Pharmacol |volume= |issue=168 |pages=445–77 |year=2005 |pmid=16596784 |doi= |url=http://www.springerlink.comopenurl.asp?genre=chapter&issn=0171-2004&volume=&page=445}}</ref> The strongest evidence regarding cannabis and memory focuses on its short-term negative effects on short-term and working memory.<ref name=memoryhindered/> Evidence also suggests that long-term effects exist, but these appear to be reversible except in very heavy users.<ref name=memorylongterm>{{cite journal |author=Grotenhermen F |title=The toxicology of cannabis and cannabis prohibition |journal=Chem. Biodivers. |volume=4 |issue=8 |pages=1744–69 |year=2007 |month=August |pmid=17712818 |doi=10.1002/cbdv.200790151 |url=}}</ref> | ||
| A 2008 study suggests that long-term, heavy cannabis use ( |
A 2008 review of the evidence surrounding the acute impact on memory concluded that cannabinoids impair all aspects of short-term memory, especially short-term episodic and working memory.<ref name=acutememory>{{cite journal |author=Ranganathan M, D'Souza DC |title=The acute effects of cannabinoids on memory in humans: a review |journal=Psychopharmacology (Berl.) |volume=188 |issue=4 |pages=425–44 |year=2006 |month=November |pmid=17019571 |doi=10.1007/s00213-006-0508-y |url=}}</ref> One small study found that no learning occurred during the 2 hour period in which the subjects were "stoned".<ref>{{cite journal |author=Curran HV, Brignell C, Fletcher S, Middleton P, Henry J |title=Cognitive and subjective dose-response effects of acute oral Delta 9-tetrahydrocannabinol (THC) in infrequent cannabis users |journal=Psychopharmacology (Berl.) |volume=164 |issue=1 |pages=61–70 |year=2002 |month=October |pmid=12373420 |doi=10.1007/s00213-002-1169-0 |url=}}</ref> Long-term effects on memory may be balanced by ] effects of THC against ].<ref>{{cite journal |author=van der Stelt M, Veldhuis WB, Bär PR, Veldink GA, Vliegenthart JF, Nicolay K |title=Neuroprotection by Delta9-tetrahydrocannabinol, the main active compound in marijuana, against ouabain-induced in vivo excitotoxicity |journal=J. Neurosci. |volume=21 |issue=17 |pages=6475–9 |year=2001 |month=September |pmid=11517236 |doi= |url=http://www.jneurosci.org/cgi/pmidlookup?view=long&pmid=11517236}}</ref> A 2008 study suggests that long-term, heavy cannabis use (>five joints daily for >ten years) are associated with structural abnormalities in the hippocampus and amygdala areas of the brain. The hippocampus, thought to regulate emotion and memory, and the amygdala, involved with fear and aggression, tended to be smaller in heavy and long term cannabis users than in controls (volume was reduced by an average of 12 percent in the hippocampus and 7.1 percent in the amygdala).<ref>{{cite journal |author=Yücel M, Solowij N, Respondek C, ''et al'' |title=Regional brain abnormalities associated with long-term heavy cannabis use |journal=Arch. Gen. Psychiatry |volume=65 |issue=6 |pages=694–701 |year=2008 |month=June |pmid=18519827 |doi=10.1001/archpsyc.65.6.694 |url=}}</ref> | ||
| A 1998 ''Journal of Neuroscience'' ] research, which was carried out on hippocampal cells excised from decapitated rats, using THC carried in ethanol to saturate the neurons, suggests that THC is toxic for cultured hippocampal neurons.<ref></ref> | A 1998 ''Journal of Neuroscience'' ] research, which was carried out on hippocampal cells excised from decapitated rats, using THC carried in ethanol to saturate the neurons, suggests that THC is toxic for cultured hippocampal neurons.<ref></ref> | ||
Revision as of 05:45, 26 February 2009
This section compares the health issues and the effects of cannabis and tobacco. For the main article on the health issues and the effects of tobacco, see Health effects of tobacco smoking.This article focuses upon the effects of cannabis on the human body. Cannabis is considered a semi-psychoactive drug, and its effects on the brain are mediated through cannabinoids, most notably tetrahydrocannabinol (THC). In some areas of the world, medical cannabis is prescribed for nausea, pain, and alleviation of symptoms surrounding chronic illness, but its use remains controversial.
Acute effects while under the influence can include euphoria, increased appetite, anxiety, short-term memory loss, and circulation effects which may increase risks of heart attacks. However, chronic use is not associated with cardiovascular risk factors such as blood triglyceride levels and blood pressure in the longitudinal CARDIA study.
| This article may be too technical for most readers to understand. Please help improve it to make it understandable to non-experts, without removing the technical details. (Learn how and when to remove this message) |
The evidence of long-term effects on memory is preliminary and hindered by confounding factors. Concerns have been raised about the potential for long-term cannabis consumption to increase risk for schizophrenia, bipolar disorders, and major depression, but the ultimate conclusions on these factors are disputed.
Methods of consumption
Main article: Cannabis consumptionThere are various methods of cannabis consumption and each has various costs and benefits related to the health issues and effects of cannabis. Some methods are smoking, vaporization, and ingestion.
Smoking


Cannabis smoking is the most common method of consumption, either by manually rolling cannabis, sometimes mixed with tobacco or other herbs, into a cigarette (called a "joint" or "spliff"), or by directly burning pre-sifted cannabis, at far lower temperatures, in a narrow-crater pipe or bong. As cigarette smoking is credited with causing most of the 5.4 million premature deaths per year attributed to tobacco , similarly the practice of "rolling a joint" may cause pathologies in "heavy users" of cannabis that are widely attributed to the cannabis. At least one source has suggested that the practice of mixing tobacco with cannabis can lead to nicotine dependence.
Vaporization
Main article: vaporizer
28. Insert moderate (25 mg) serving of cannabis, other herbs or essential oils
36. Flame filter made of a stack of metal screens (5+) or a heat resistant porous material
Vaporization is a much less harmful alternative to smoking and seems well suited for medical use. Rather than burning the herb, which produces numerous harmful by-products, a vaporizer heats the material, ideally to 180 °C (356 °F), so that the active compounds contained in the cannabis boil off, converting them into a gas to be inhaled. This gas is not smoke from combustion but instead a vapor, which has the appearance of smoke but ideally contains virtually zero particulate matter (tar) and reduced noxious gases such as carbon monoxide.

Studies have shown that vaporizers can dramatically reduce or even eliminate the release of irritants and toxic compounds.
The onset of effects from the inhalation of cannabis vapor is very rapid, similar to smoking. In comparison, the effects of ingestion of cannabis may take about one or two hours, depending on form and stomach contents.
Biochemical effects of cannabis constituents
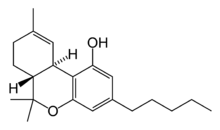
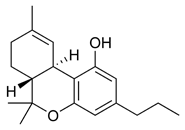



The most prevalent group of psychoactive substances in cannabis is cannabinoids, including delta-9-tetrahydrocannabinol (Δ-THC, commonly called simply THC). In the past two decades, the average content of THC in marijuana sold in North America has increased from about 1% to 3–4% or more. Some varieties, having undergone careful selection and growing techniques, can yield as much as 29% THC. Another psychoactive cannabinoid present in Cannabis sativa is tetrahydrocannabivarin (THCV), but it is only found in small amounts.
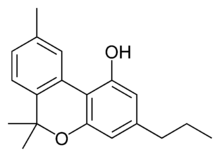
In addition, there are also similar compounds contained in cannabis that do not exhibit any psychoactive response but are obligatory for functionality: cannabidiol (CBD), an isomer of THC; cannabinol (CBN), an oxidation product of THC; cannabivarin (CBV), an analog of CBN with a different sidechain, cannabidivarin (CBDV), an analog of CBD with a different side chain, and cannabinolic acid. How these other compounds interact with THC is not fully understood. Some clinical studies have proposed that CBD acts as a balancing force to regulate the strength of the psychoactive agent THC. Anecdotal and inconclusive reports claim that marijuana with relatively high ratios of THC:CBD is less likely to induce anxiety than marijuana with low THC:CBD ratios. CBD is also believed to regulate the body’s metabolism of THC by inactivating cytochrome P450, an important class of enzymes that metabolize drugs. Experiments in which mice were treated with CBD followed by THC showed that CBD treatment was associated with a substantial increase in brain concentrations of THC and its major metabolites, most likely because it decreased the rate of clearance of THC from the body. Cannabis cofactor compounds have also been linked to lowering body temperature, modulating immune functioning, and cell protection. The essential oil of cannabis contains many fragrant terpenoids which may synergize with the cannabinoids to produce their unique effects. THC is converted rapidly to 11-hydroxy-THC, which is also pharmacologically active, so the drug effect outlasts measurable THC levels in blood.
THC and cannabidiol are also neuroprotective antioxidants. Research in rats has indicated that THC prevented hydroperoxide-induced oxidative damage as well as or better than other antioxidants in a chemical (Fenton reaction) system and neuronal cultures. Cannabidiol was significantly more protective than either vitamin E or vitamin C.
In 1990, the discovery of cannabinoid receptors located throughout the brain and body, along with endogenous cannabinoid neurotransmitters like anandamide (a lipid material derived ligand from arachidonic acid), suggested that the use of cannabis affects the brain in the same manner as a naturally occurring brain chemical. Cannabinoids usually contain a 1,1'-di-methyl-pyrane ring, a variedly derivatized aromatic ring and a variedly unsaturated cyclohexyl ring and their immediate chemical precursors, constituting a family of about 60 bi-cyclic and tri-cyclic compounds. Like most other neurological processes, the effects of cannabis on the brain follow the standard protocol of signal transduction, the electrochemical system of sending signals through neurons for a biological response. It is now understood that cannabinoid receptors appear in similar forms in most vertebrates and invertebrates and have a long evolutionary history of 500 million years. Cannabinoid receptors decrease adenylyl cyclase activity, inhibit calcium N channels, and disinhibit KA channels. There are two types of cannabinoid receptors (CB1 and CB2).
The CB1 receptor is found primarily in the brain and mediates the psychological effects of THC. The CB2 receptor is most abundantly found on cells of the immune system. Cannabinoids act as immunomodulators at CB2 receptors, meaning they increase some immune responses and decrease others. For example, nonpsychotropic cannabinoids can be used as a very effective anti-inflammatory. The affinity of cannabinoids to bind to either receptor is about the same, with only a slight increase observed with the plant-derived compound CBD binding to CB2 receptors more frequently. Cannabinoids likely have a role in the brain’s control of movement and memory, as well as natural pain modulation. It is clear that cannabinoids can affect pain transmission and, specifically, that cannabinoids interact with the brain's endogenous opioid system and may affect dopamine transmission. This is an important physiological pathway for the medical treatment of pain.
The cannabinoid receptor is a typical member of the largest known family of receptors called a G protein-coupled receptor. A signature of this type of receptor is the distinct pattern of how the receptor molecule spans the cell membrane seven times. The location of cannabinoid receptors exists on the cell membrane, and both outside (extracellularly) and inside (intracellularly) the cell membrane. CB1 receptors, the bigger of the two, are extraordinarily abundant in the brain: 10 times more plentiful than μ-opioid receptors, the receptors responsible for the effects of morphine. CB2 receptors are structurally different (the homology between the two subtypes of receptors is 44%), found only on cells of the immune system, and seems to function similarly to its CB1 counterpart. CB2 receptors are most commonly prevalent on B-cells, natural killer cells, and monocytes, but can also be found on polymorphonuclear neurtrophil cells, T8 cells, and T4 cells. In the tonsils the CB2 receptors appear to be restricted to B-lymphocyte-enriched areas.
THC and endogenous anandamide additionally interact with glycine receptors.
Cannabis also contains a related class of compound: the cannaflavins. These compounds have been suggested to contribute certain effects of cannabis, such as analgesia and anti-inflammatory properties, and are considerably more effective than aspirin. Cannaflavins usually contain a 1,4-pyrone ring fused to a variedly derivatized aromatic ring and linked to a second variedly derivatized aromatic ring and include for example the non-psychoactive cannflavin A and B.
Sustainability in the body
The nature of cannabis, its lipophilic (fat soluble) properties, yields a long elimination half-life relative to other recreational drugs. The THC molecule, and related compounds, are usually detectable in drug tests from 3 days up to 10 days according to Redwood Laboratories, after using cannabis depending on frequency of use (see drug test). This detection is possible because non-psychoactive THC metabolites are stored for long periods of time in fat cells, and THC has an extremely low water solubility. The rate of elimination of metabolites is slightly greater for more frequent users due to tolerance.
Toxicity
The LD50 of THC (the dose which causes the death of 50% of individuals) is 1270 mg/kg for male rats and 730 mg/kg for female rats from oral assumption in sesame oil, and 42 mg/kg for rats from inhalation. There have been no human fatalities from cannabis overdose.
Short-term effects
Psychoactive effects
The psychoactive effects of cannabis, known as a "high", are subjective and can vary based on the individual. Some effects may include an altered state of consciousness, euphoria, feelings of well-being, relaxation or stress reduction, lethargy (seen more towards higher CBD:THC ratio plants, such as C. indica dominant strains), increased appreciation of humor, music or art, joviality, metacognition and introspection, enhanced recollection (episodic memory), increased sensuality, increased awareness of sensation, increased libido, creative or philosophical thinking, disruption of linear memory, paranoia, agitation or anxiety, experiential augmentation of other psychedelics and increased awareness of patterns and color.
Cannabis also produces many subjective effects, such as greater enjoyment of food taste and aroma, an enhanced enjoyment of music and comedy, and marked distortions in the perception of time and space (where experiencing an up rush of ideas from the bank of long-term memory can create the subjective impression of long elapsed time, while the clock reveals that only a short time has passed). At higher doses, effects can include altered body image, auditory and/or visual illusions, and ataxia from selective impairment of polysynaptic reflexes. In extremely high doses, marijuana can lead to depersonalisation.
Since cannabis has a very low toxicity, there are virtually no limits to how affected a person can be from cannabis. In case of very large doses as 10 gram, cannabis is strongly hallucinogenic, and a high may last for more than one day.
Somatic effects
Some of the short-term physical effects of cannabis use include increased heart rate, dryness of the mouth, reddening of the eyes (congestion of the conjunctival blood vessels), a reduction in intra-ocular pressure, muscle relaxation and a sensation of cold or hot hands and feet.
Electroencephalography or EEG shows somewhat more persistent alpha waves of slightly lower frequency than usual. Cannabinoids produce a "marked depression of motor activity" via activation of neuronal cannabinoid receptors belonging to the CB1 subtype.
Duration of the effects
The total short-term duration of cannabis intoxication when smoked is about three to six hours depending on how much THC/CBD is consumed.
A study of ten healthy, robust, male volunteers who resided in a residential research facility sought to examine both acute and residual subjective, physiologic, and performance effects of smoking marijuana cigarettes. On three separate days, subjects smoked one NIDA marijuana cigarette containing either 0%, 1.8%, or 3.6% THC, documenting subjective, physiologic, and performance measures prior to smoking, five times following smoking on that day, and three times on the following morning. Subjects reported robust subjective effects following both active doses of marijuana, which returned to baseline levels within 3.5 hours. Heart rate increased and the puplilary light reflex decreased following active dose administration with return to baseline on that day. Additionally, marijuana smoking acutely produced decrements in smooth pursuit eye tracking. Although robust acute effects of marijuana were found on subjective and physiological measures, no effects were evident the day following administration, indicating that the residual effects of smoking a single marijuana cigarette are minimal.
Other effects and studies
A Dutch double blind, randomized, placebo-controlled, cross-over study examining male volunteers aged 18–45 years with a self-reported history of regular cannabis use concluded that smoking of cannabis with very high THC levels (marijuana with 9–23% THC), as currently sold in coffee shops in the Netherlands, may lead to higher THC blood-serum concentrations. This is reflected by an increase of the occurrence of impaired psychomotor skills, particularly among younger or inexperienced cannabis smokers, who do not adapt their smoking-style to the higher THC content. High THC concentrations in cannabis were associated with a dose-related increase of physical effects (such as increase of heart rate, and decrease of blood pressure) and psychomotor effects (such as reacting more slowly, being less concentrated, making more mistakes during performance testing, having less motor control, and experiencing drowsiness). It was also observed during the study that the effects from a single joint lasted for more than eight hours. Reaction times remained impaired five hours after smoking, when the THC serum concentrations were significantly reduced, but still present. When subjects smoke on several occasions per day, accumulation of THC in blood-serum may occur.
Another study showed that consumption of 15 mg of Delta(9)-THC resulted in no learning whatsoever occurring over a three-trial selective reminding task after two hours. In several tasks, delta(9)-THC increased both speed and error rates, reflecting “riskier” speed–accuracy trade-offs.
Neurological effects
The areas of the brain where cannabinoid receptors are most prevalently located are consistent with the behavioral effects produced by cannabinoids. Brain regions in which cannabinoid receptors are very abundant are the basal ganglia, associated with movement control; the cerebellum, associated with body movement coordination; the hippocampus, associated with learning, memory, and stress control; the cerebral cortex, associated with higher cognitive functions; and the nucleus accumbens, regarded as the reward center of the brain. Other regions where cannabinoid receptors are moderately concentrated are the hypothalamus, which regulates homeostatic functions; the amygdala, associated with emotional responses and fears; the spinal cord, associated with peripheral sensations like pain; the brain stem, associated with sleep, arousal, and motor control; and the nucleus of the solitary tract, associated with visceral sensations like nausea and vomiting.
Most notably, the two areas of motor control and memory are where the effects of cannabis are directly and irrefutably evident. Cannabinoids, depending on the dose, inhibit the transmission of neural signals through the basal ganglia and cerebellum. At lower doses, cannabinoids seem to stimulate locomotion while greater doses inhibit it, most commonly manifested by lack of steadiness (body sway and hand steadiness) in motor tasks that require a lot of attention. Other brain regions, like the cortex, the cerebellum, and the neural pathway from cortex to striatum, are also involved in the control of movement and contain abundant cannabinoid receptors, indicating their possible involvement as well.
Experiments on animal and human tissue have shown the potential for the disruption of short-term memory, which is consistent with the abundance of CB1 receptors on the hippocampus, the region of the brain most closely associated with memory. Cannabinoids inhibit the release of several neurotransmitters in the hippocampus, like acetylcholine, norepinephrine, and glutamate, resulting in a major decrease in neuronal activity in that region. This decrease in activity resembles a "temporary hippocampal lesion." In the end, this procedure could lead to the blocking of cellular processes that are associated with memory formation. As the drug is metabolized, normal neurological activity is eventually restored.
In in-vitro experiments THC at extremely high concentrations, which could not be reached with commonly consumed doses, caused competitive inhibition of the AChE enzyme and inhibition of β-amyloid peptide aggregation, the cause of Alzheimer's disease. Compared to currently approved drugs prescribed for the treatment of Alzheimer's disease, THC is a considerably superior inhibitor of A aggregation, and this study provides a previously unrecognized molecular mechanism through which cannabinoid molecules may directly impact the progression of this debilitating disease.
Effects of cannabis on driving
| This section needs additional citations for verification. Please help improve this article by adding citations to reliable sources in this section. Unsourced material may be challenged and removed. (October 2008) (Learn how and when to remove this message) |
It is known that cannabis consumption affects motor skills, reflexes, attention and perception, therefore affecting driving ability.
A 2001 study by the United Kingdom Transit Research Laboratory (TRL) specifically focuses on the effects of cannabis use on driving (see report here: ), and is one of the most recent and commonly quoted studies on the subject. The report summarizes current knowledge about the effects of cannabis on driving and accident risk based on a review of available literature published since 1994 and the effects of cannabis on laboratory based tasks.
The study identified young males, amongst whom cannabis consumption is frequent and increasing, and in whom alcohol consumption is also common, as a risk group for traffic accidents. This is due to driving inexperience and factors associated with youth relating to risk taking, delinquency and motivation. These demographic and psychosocial variables may relate to both drug use and accident risk, thereby presenting an artificial relationship between use of drugs and accident involvement.
The effects of cannabis on laboratory-based tasks show clear impairment with respect to tracking ability, attention, and other tasks depending on the dose administered. These effects however, are not as pronounced on real world tasks, like driving or simulator tasks. Both simulation and road trials generally find that driving behavior shortly after consumption of larger doses of cannabis results in:
- increased variability in lane position (such as taking a curve too tightly or too loosely).
- longer decision times, leading to slower responses to driving situations; and
- a more cautious driving style, including slower average speed and greater following distance.
bob marley says cannabis is good Whereas these results indicate a 'change' from normal conditions, they do not necessarily reflect 'impairment' in terms of performance effectiveness, since few studies report increased accident risk. However, the results do suggest 'impairment' in terms of performance efficiency given that some of these behaviors may limit the available resources to cope with any additional, unexpected or high demand, events. Indeed, compensatory effort may be invoked to offset impairment in the driving task. Subjects under cannabis treatment may perceive that they are impaired and may strategically compensate, for example, by not overtaking, by slowing down and by focusing their attention when they know a response will be required. This compensatory effort may be one reason for the failure to implicate cannabis consumption as an accident risk factor, particularly at lower doses or with more than about one hour after consumption. According to the TRL study, the same compensatory behavior could also be an unconscious adaptation, similar to reduced driving speeds used by a sleepy driver.
Specifically, 4-12% of accident fatalities have detected levels of cannabis. However, most studies report that the majority of fatal cases with detected levels of cannabis are compounded by alcohol.
The study estimates 11 ng/ml THC as the equivalent dose to the legal limit of alcohol (0.08% BAC in the UK). Complicating this assessment is the fact that cannabis effects on driving fade after a short period of time, while some THC may be present in the body for weeks.
Similar conclusions have been reached by studies maintained by the federal governments of Australia, United Kingdom, New Zealand and the United States (see here for a list of studies). Those studies that have concluded that cannabis has a significant negative effect on driving ability generally involve the use of roadside sobriety tests as an indicator of reduced ability (for example, see this NIDA report). However, studies that employ this methodology show that a majority of subjects who tested positive for THC also tested positive for alcohol, already described as a limiting factor of validity.
Toxicity
THC has an extremely low toxicity and the amount that can enter the body through the consumption of cannabis plants poses no threat of death. In lab animal tests, scientists have had much difficulty administering a dosage of THC that is high enough to be lethal. It also appears that humans cannot die from ingesting too much THC, unless it were introduced into the body intravenously (See also: Intravenous Marijuana Syndrome). Indeed, a 1988 ruling from the United States Department of Justice concluded that "In practical terms, marijuana cannot induce a lethal response as a result of drug-related toxicity."
According to the Merck Index, the LD50 (dosage lethal to 50% of rats tested) of Δ-THC by inhalation is 42 mg/kg of body weight. For oral consumption, the LD50 for male rats is 1270 mg/kg, and 730 mg/kg for females—equivalent to the THC in about a pound of 15% THC marijuana.
The ratio of cannabis material required to produce a fatal overdose to the amount required to saturate cannabinoid receptors and cause intoxication is 40,000:1 ; consumption of such a large dose is virtually impossible. There have been no reported deaths or permanent injuries sustained as a result of a marijuana overdose . It is, for all practical purposes, impossible to overdose on marijuana, as the user would certainly either fall asleep or otherwise become incapacitated from the effects of the drug before being able to consume enough THC to be mortally toxic. According to a 2006 United Kingdom government report, using cannabis is much less dangerous than tobacco, prescription drugs, and alcohol in social harms, physical harm, and addiction. It was found in 2007 that while tobacco and cannabis smoke are quite similar, cannabis smoke contained higher amounts of ammonia, hydrogen cyanide, and nitrogen oxides, but lower levels of carcinogenic polycyclic aromatic hydrocarbons (PAHs).
Vascular effects
Cannabis arteritis is a very rare but serious peripheral vascular disease that usually affects younger smokers of cannabis, which can lead to amputation if not diagnosed and treated early.
A 2008 study by the National Institutes of Health suggested a link between heavy long-term marijuana smoking (138 joints per week over 6 years) and increased risk of heart attack or stroke.
Adulterated cannabis
Contaminants may be found in hashish obtained from "soap bar"-type sources. The dried flowers of the plant may be contaminated by the plant taking up heavy metals and other toxins from its growing environment, or by the addition of lead or glass beads, used to increase the weight or to make the cannabis appear as if it has more crystal-looking trichomes indicating a higher THC content . Users who burn hot or mix cannabis with tobacco are at risk of failing to detect deviations from appropriate cannabis taste.
Combination with other drugs
The most obvious confounding factor in cannabis research is the prevalent usage of other recreational drugs, especially alcohol and tobacco. Such complications demonstrate the need for studies on cannabis that have stronger controls, and investigations into alleged symptoms of cannabis use that may also be caused by tobacco. Some critics question whether agencies doing the research make an honest effort to present an accurate, unbiased summary of the evidence, or whether they "cherry-pick" their data to please funding sources which may include the tobacco industry or governments dependent on cigarette tax revenue; others caution that the raw data, and not the final conclusions, are what should be examined.
Cannabis also has been shown to have a synergistic cytotoxic effect on lung cancer cell cultures in vitro with the food additive butylated hydroxyanisole (BHA) and possibly the related compound butylated hydroxytoluene (BHT). The study concluded, "Exposure to marijuana smoke in conjunction with BHA, a common food additive, may promote deleterious health effects in the lung." BHA & BHT are human-made fat preservatives, and are found in many packaged foods including: plastics in boxed Cereal, Jello, Slim Jims, and more.
Long-term effects
Reproductive effects
Marijuana has been reported both to enhance and lessen the subjective enjoyment of sex. It has been shown that administration of high doses of THC to animals lowers serum testosterone levels, impairs sperm production, motility, and viability, disrupts the ovulation cycle, and decreases output of gonadotropic hormones. According to the 1997 Merck Manual of Diagnosis and Therapy, fertility effects related to cannabis use are uncertain.
Research has demonstrated that human sperm contains receptors which are stimulated by substances like THC and other cannabis-related chemicals. Tests have implied that smoking of marijuana could impact the sperm's functions, though this impact is unknown.
Pregnancy
One study by Zuckerman and colleagues included a large sample of women with a substantial prevalence of marijuana use that was verified by urine analysis and no increased probability of birth defects was found in the sample group. Compared to fetal alcohol syndrome, similar types of facial features and related symptoms are not associated with prenatal marijuana exposure. THC passes into the breast milk and may affect a breastfed infant. Many studies about drug use during pregnancy are self-administered by the applicants and not always anonymous. The stigma of using illicit drugs while pregnant discourages honest reporting and can invalidate the results. Studies show that women who consume cannabis while they are pregnant may also be likely to consume alcohol, tobacco, caffeine, or other illicit drugs, which makes it difficult to deduce scientific facts about just marijuana use from statistical results. Very few large, well-controlled epidemiological studies have taken place to understand the connection of marijuana use and pregnancy.
A study of the development of 59 Jamaican children was conducted with the children being monitored from child birth to age 5 years. One-half of the sample's mothers used marijuana during pregnancy; they were paired with non-using mothers who matched age, parity, and socioeconomic status. Testing was done at 1, 3, and 30 days of age with the Brazelton Neonatal Behavioral Assessment Scales, and at ages 4 and 5 years with the McCarthy Scales of Children's Abilities test. Data was also collected from the child's home environment and temperament, as well as standardized tests. The results over the entire research period showed no significant differences in development testing outcomes between using and non-using mothers. At 30 days of age, however, the children of marijuana-using mothers had higher scores on autonomic stability and reflexes. The absence of any differences between the exposed and non-exposed groups in the early neonatal period suggest that the better scores of exposed neonates at 1 month are traceable to the cultural positioning and social and economic characteristics of mothers using marijuana that select for the use of marijuana but also promote neonatal development.
Some studies have found that children of tobacco and marijuana-smoking mothers more frequently suffer from permanent cognitive deficits, concentration disorders, hyperactivity, and impaired social interactions than non-exposed children of the same age and social background. A recent study, with participation of scientists from Europe and the United States, has now identified that naturally occurring endocannabinoid molecules play a role in establishing how certain nerve cells connect to each other in the fetal brain. Another study examining cannabinoid receptor proteins (CBRs) expressed in brain cells of mice determined that endogenous endocannabinoids assist in directing brain cell directional development while in the womb. The researchers suggest that elevated blood THC levels due to cannabis consumption would affect brain development of human fetuses. In contrast, other studies in Jamaica have suggested that cannabis use by expectant mothers does not appear to cause birth defects or developmental delays in their newborn children.
Addiction potential
Research has shown that the overall addiction potential for cannabis to be much less than heroin, cocaine, tobacco and alcohol. There is some evidence that dependence on cannabis can exist in some heavy users. One study with 500 heavy users of cannabis showed that when trying to cease consumption, some experience one or more symptoms such as insomnia, restlessness, loss of appetite, depression, irritability, and anger. Prolonged marijuana use produces both pharmacokinetic changes (how the drug is absorbed, distributed, metabolized, and excreted) and pharmacodynamic changes (how the drug interacts with target cells) to the body. These changes require the user to consume higher doses of the drug to achieve a common desirable effect (known as a higher tolerance), and reinforce the body’s metabolic systems for synthesizing and eliminating the drug more efficiently.
Preliminary research, published in the April 2006 issue of the Journal of Consulting and Clinical Psychology, indicates that cannabis addiction can be offset by a combination of cognitive-behavioral therapy and motivational incentives. Participants in the study (previously diagnosed with marijuana dependence) received either vouchers as incentives to stay drug free, cognitive-behavioral therapy, or both over a 14-week period. At the end of 3 months, 43 percent of those who received both treatments were no longer using marijuana, compared with 40 percent of the voucher group, and 30 percent of the therapy group. At the end of a 12-month follow-up, 37 percent of those who got both treatments remained abstinent, compared with 17 percent of the voucher group, and 23 percent of the therapy group.
A 1998 French governmental report commissioned by Health Secretary of State Bernard Kouchner, and directed by Dr. Pierre-Bernard Roques, classed drugs according to addictiveness and neurotoxicity. It placed heroin, cocaine and alcohol in the most addictive and lethal categories; benzodiazepine, hallucinogens and tobacco in the medium category, and cannabis in the last category. The report stated that "Addiction to cannabis does not involve neurotoxicity such as it was defined in chapter 3 by neuroanatomical, neurochemical and behavioral criteria. Thus, former results suggesting anatomic changes in the brain of chronic cannabis users, measured by tomography, were not confirmed by the accurate modern neuro-imaging techniques. Moreover, morphological impairment of the hippocampus of rat after administration of very high doses of THC (Langfield et al., 1988) was not shown (Slikker et al., 1992)." Health Secretary Bernard Kouchner concluded that : "Scientific facts show that, for cannabis, no neurotoxicity is demonstrated, to the contrary of alcohol and cocaine."
Mental health
Cannabis use has been assessed by several studies to be correlated with the development of anxiety, psychosis and depression. Some studies assess that the causality is more likely to involve a path from cannabis use to psychotic symptoms rather than a path from psychotic symptoms to cannabis use, while others assess the opposite direction of the causality, or hold cannabis to only form parts of "causal constellation", while not inflicting mental health problems that would not have occurred in the absence of the cannabis use. In some cases cannabis can trigger depersonalization disorder, occasionally after the first usage. A common interpretation of the correlation and theorized direction of the causality is the self-medication hypothesis, which is based on partially or fully attributing the correlation between psychiatric diseases and cannabis to the extensive substance abuse among sufferers of certain mental disorders, before diagnosis in many cases, which increases the likeliness of cannabis use among the mentally ill and the undiagnosed, thus accounting for correlation and debunking some claims of causality with the opposite direction. As much as 60% of the mentally ill are suspected to be substance abusers, and many seem to prefer cannabis and alcohol. Dr Stanley Zammit of Bristol and Cardiff universities (in the Daily express newspaper of the 27th of July 2007) reported "Even if cannabis did increase the risk of psychosis, most people using the drug would not get ill" But he added: "Nevertheless, we would still advise people to avoid or limit their use of this drug, especially if they start to develop any mental health symptoms or if they have relatives with psychotic illnesses." A 2007 study of studies published in the Lancet concluded that cannabis users are 40% more likely to be sufferers of a psychotic illness than non-users.
In comparison, alcohol, as the only intoxicating drug with similar levels of popularity, has been linked to more than 65% of all suicides in a UK study, and linked to general psychiatric mental health problems including depression, anxiety, schizophrenia, psychosis, psychoneurosis, Post Traumatic Stress Disorder, physical brain damage and more. The long term effects of alcohol misuse include psychosis as well as Korsakoff's syndrome which is often irreversible. Chronic alcohol misuse can cause psychotic type symptoms to develop, more so than with other drugs of abuse. A study found that there is an 8 fold (or 800%) increased risk of psychotic disorders in alcohol misusing men and 3 fold (or 300%) increased risk in alcohol misusing women.
A large unselected, population-based study, published in British Journal of Psychiatry (2008), examined cannabis use and prodromal symptoms of psychosis at age 15–16 years and conclude that cannabis use is associated with prodromal symptoms of psychosis in adolescence.
The direction of causation was more directly examined in a study by Dr. Mikkel Arendt of Aarhus University in Risskov, Denmark, and colleagues, which found that individuals treated for psychotic episodes following cannabis use had the same likelihood of having a mother, sister or other "first-degree" relative with schizophrenia as did the individuals who had actually been treated for schizophrenia themselves. This suggests that the psychosis blamed on cannabis use is in fact the result of a genetic predisposition towards schizophrenia. "These people would have developed schizophrenia whether or not they used cannabis
Behavioral effects
Government studies often point to statistical data accumulated by methods like the National Household Survey on Drug Abuse (NHSDA), the Monitoring the Future study (MTF), and the Arrestee Drug Abuse Monitoring (ADAM) program, which claim lower school averages and higher dropout rates among users than nonusers. However, the major contributor to a lack of credibility in these studies, is that in many cases, like with NHSDA and MTF, these surveys are usually self-administered and may be anonymous. The likeliness of over or under representing data definitely undermines the effectiveness of these instruments. The ADAM study is conducted anonymously, but only seeks information from a sample of people who have been arrested for drug-related offenses. Socially deviant behavior may be found more frequently in individuals of the criminal justice system compared to those in the general population, including non users. In response, independent studies of college students have shown that there was no difference in grade point average, and achievement, between marijuana users and nonusers, but the users had a little more difficulty deciding on career goals, and a smaller number were seeking advanced professional degrees. Laboratory studies of the relationship between motivation and marijuana outside of the classroom, where volunteers worked on operant tasks for a wage representing a working world model, also fail to distinguish a noticeable difference between users and non users.
At least one study has shown a decrease in depression in cannabis users.
Gateway drug hypothesis
Main article: Gateway drug theory § CannabisThe gateway drug hypothesis asserts that the use of cannabis may ultimately lead to the use of harder drugs. For the most part, it was commonly thought that cannabis gateways to other drugs because of social factors. For example, the criminalization of cannabis in many countries associates its users with organized crime promoting the illegal drug trade.
A July 2006 study by Ellgren et al. strictly tested lab rats for the biological mechanism of the gateway drug effect. The study administered 6 "teenage" (28 and 49 days old) rats delta-9-tetrahydrocannabinol, and 6 were the control. One week after the first part was completed, catheters were inserted in the jugular vein of all of the adult rats and they were able to self-administer themselves heroin by pushing a lever. The study found that initially both groups behaved the same and began to self-administer heroin frequently, but then stabilized at different levels. The rats that had previously been administered THC consumed about 1.5 times more heroin than those that had not. Because many THC receptors interact with the opioid system, the study surmised that adolescent cannabis use overstimulates and alters the pleasure and reward structures of the brain, thus increasing the already high risk of addiction for people who start to use heroin. However, the rats took up self-administration at the same rate regardless of adolescent THC exposure, and observed levels of "drug-seeking behavior" were also the same. Other studies have shown that the dopamine system is independent of the THC receptor glands thus negating these negative effects. Psychopharmacologist Ian Stolerman, from King's College London, finds the biological cannabis gateway drug effect "somewhat preliminary", and states "it's too early to say there's a consensus, but a small number of studies like this suggest that there is a physiological basis for this effect." Other drugs, he notes, such as cocaine and amphetamines are involved in another brain pathway called the dopaminergic system. Cells in that system also interact with THC receptors and could be modified by cannabis exposure. Cannabinoid receptors are 10 times more prevalent in the brain than opioid receptors. According to Dr. Hurd, one of the study leaders, two other drugs that also stimulate opioid cells, and could therefore also feasibly cause a gateway effect, are nicotine and alcohol.
However, a December 2006 study by the American Psychiatric Association challenges these findings. A 12 year study on 214 boys from ages 10-12 showed that adolescents who used marijuana prior to using other drugs, including alcohol and tobacco, were no more likely to develop a substance abuse disorder than other subjects in the study. "This evidence supports what's known as the common liability model ... states the likelihood that someone will transition to the use of illegal drugs is determined not by the preceding use of a particular drug, but instead by the user's individual tendencies and environmental circumstances," investigators stated in a press release. They added, "The emphasis on the drugs themselves, rather than other, more important factors that shape a person's behavior, has been detrimental to drug policy and prevention programs."
Models used in a 2002 study by RAND cast doubt on the gateway effect and show "that the marijuana gateway effect is not the best explanation for the link between marijuana use and the use of harder drugs," as noted by Andrew Morral, associate director of RAND's Public Safety and Justice unit and lead author of the study.
Co-occurrence of mental illness
Studies have shown that a risk does exist in some individuals with a predisposition to mental illness to develop symptoms of psychosis. The risk was found to be directly related to high dosage and frequency of use, early age of introduction to the drug, and was especially pronounced for those with a predisposition for mental illness. These results have been questioned as being biased by failing to account for medicinal versus recreational usage — critics contend it could be a causal relationship, or it could be that people who are susceptible to mental problems tend to smoke cannabis, or it could be connected to the criminalization of cannabis. Another important question is whether the observed symptoms of mental illness are actually connected to development of a permanent mental disorder; cannabis may trigger latent conditions, or be part of a complex coordination of causes of mental illness, referred to in psychology as the diathesis-stress model. People with developed psychological disorders are known to self-medicate their symptoms with cannabis as well, although one study has claimed that those with a predisposition for psychosis did not show a statistically significant increase in likelihood of cannabis use four years later.
Correlation versus causality
Some studies conclude that there is a correlation of cannabis use and some symptoms of psychosis, but don't necessarily support the notion that cannabis use is a sufficient or necessary cause for psychosis. It might be a component cause, part of a complex constellation of factors leading to psychosis, or it might be a correlation without forward causality at all.
For example, a review of the evidence by Louise Arsenault, et al., in 2004 reports that on an individual level, cannabis use confers an overall twofold increase in the relative risk of later schizophrenia, assuming a causal relationship. This same research also states that "There is little dispute that cannabis intoxication can lead to acute transient psychotic episodes in some individuals". The study synthesizes the results of several studies into a statistical model. The study does not correct for the use of other illicit drugs, and relies on self-reporting of cannabis dosage. The study also does not determine if the cannabis use preceded or followed the mental health problem.
Similarly, a landmark study, in 1987, of 50,000 Swedish Army conscripts, found that those who admitted at age 18 to having taken cannabis on more than 50 occasions, were six times more likely to develop schizophrenia in the following 15 years. In fact, psychosis cases were restricted to patients requiring a hospital admission. These findings have not been replicated in another population based sample. As the study did not control for symptoms preexisting onset of cannabis use, the use of other illicit drugs, the study does not resolve the correlation versus causality question but has fueled a major debate within the scientific community. This study also used self reporting for cannabis dosage.
A 2005 study found that "the onset of schizotypal symptoms generally precedes the onset of cannabis use. The findings do not support a causal link between cannabis use and schizotypal traits". It should be noted that a schizotypal personality disorder is a personality disorder different from schizophrenia. A 2007 British study concluded, "We found few appreciable differences in symptomatology between schizophrenic patients who were or were not cannabis users. There were no differences in the proportion of people with a positive family history of schizophrenia between cannabis users and non-users. This argues against a distinct schizophrenia-like psychosis caused by cannabis."
Research based on the Dunedin Multidisciplinary Health and Development Study has found that those who begin regular use of cannabis in early adolescence (from age 15, median 25 days per year by age 18) and also fit a certain genetic profile (specifically, the Val/Val variant of the COMT gene) are five times more likely to develop psychotic illnesses than individuals with differing genotypes, or those who do not use cannabis. The study was noted for having controlled for preexisting symptoms, but is open to the criticism that it cannot control for late adolescent onset of psychotic illness. Also, the study was on a cohort population, so there is no way to correlate a change in the rate of adolescent use with a change in the rate of incidence of schizophrenia in the study population. These points undermine its value in resolving the correlation versus causality question.
A study that inversely correlated cerebrospinal anandamide (an endogenous cannabinoid) levels with severity of schizophrenia (i.e., that anandamide was released in order to suppress psychosis) suggests that cannabis use may be an effect of schizophrenia or its predisposition, as opposed to a cause.
The fact that the prevalence of cannabis use has increased substantially during the last decades whereas the prevalence of psychotic illness has not suggests no causal relationship. However, this observation is contradicted by that improved methods for treatment with early intervention in psychosis has helped to keep down the number of people with long periods of psychosis.
Appetite
Clinical studies and survey data have found that cannabis increases food enjoyment and interest in food. Scientists have claimed to be able to explain what causes the increase in appetite, concluding that "endocannabinoids in the hypothalamus activate cannabinoid receptors that are responsible for maintaining food intake".
Memory
Studies on cannabis and memory are hindered by small sample sizes, confounding drug abuse, and other factors. The strongest evidence regarding cannabis and memory focuses on its short-term negative effects on short-term and working memory. Evidence also suggests that long-term effects exist, but these appear to be reversible except in very heavy users.
A 2008 review of the evidence surrounding the acute impact on memory concluded that cannabinoids impair all aspects of short-term memory, especially short-term episodic and working memory. One small study found that no learning occurred during the 2 hour period in which the subjects were "stoned". Long-term effects on memory may be balanced by neuroprotective effects of THC against excitotoxicity. A 2008 study suggests that long-term, heavy cannabis use (>five joints daily for >ten years) are associated with structural abnormalities in the hippocampus and amygdala areas of the brain. The hippocampus, thought to regulate emotion and memory, and the amygdala, involved with fear and aggression, tended to be smaller in heavy and long term cannabis users than in controls (volume was reduced by an average of 12 percent in the hippocampus and 7.1 percent in the amygdala).
A 1998 Journal of Neuroscience in vitro research, which was carried out on hippocampal cells excised from decapitated rats, using THC carried in ethanol to saturate the neurons, suggests that THC is toxic for cultured hippocampal neurons.
A 1998 report by INSERM and CNRS, which was directed by Dr. Pierre-Bernard Roques, determined that, "former results suggesting anatomic changes in the brain of chronic cannabis users, measured by tomography, were not confirmed by the accurate modern neuro-imaging techniques (such as MRI) ... Moreover, morphological impairment of the hippocampus of rat after administration of very high doses of THC was not shown." He concluded that cannabis does not have any neurotoxicity as defined in the report, unlike alcohol and cocaine.
Legal and political constraints on open research
| The examples and perspective in this article may not represent a worldwide view of the subject. You may improve this article, discuss the issue on the talk page, or create a new article, as appropriate. (November 2007) (Learn how and when to remove this message) |

In many countries, experimental science regarding cannabis is restricted due to its illegality. Thus, cannabis as a drug is often hard to fit into the structural confines of medical research because appropriate, research-grade samples are difficult to obtain for research purposes, unless granted under authority of national governments.
United States
This issue was recently highlighted in the United States by the clash between Multidisciplinary Association for Psychedelic Studies (MAPS), an independent research group, and the National Institute on Drug Abuse (NIDA), a federal agency charged with the application of science to the study of drug abuse. The NIDA largely operates under the general control of the Office of National Drug Control Policy (ONDCP), a White House office responsible for the direct coordination of all legal, legislative, scientific, social and political aspects of federal drug control policy.
The cannabis that is available for research studies in the United States is grown at the University of Mississippi and solely controlled by the NIDA, which has veto power over the Food and Drug Administration (FDA) to define accepted protocols. Since 1942, when cannabis was removed from the U.S. Pharmacopoeia and its medical use was prohibited, there have been no legal (under federal law) privately funded cannabis production projects. This has resulted in a limited amount of research being done and possibly in NIDA producing cannabis which has been alleged to be of very low potency and inferior quality.
MAPS, in conjunction with Professor Lyle Craker, PhD, the director of the Medicinal Plant Program of the University of Massachusetts at Amherst, sought to provide independently grown cannabis of more appropriate research quality for FDA-approved research studies, and encountered opposition by NIDA, the ONDCP, and the U.S. Drug Enforcement Administration (DEA).
United Kingdom
In countries such as the United Kingdom a license for growing cannabis is required if it is to be used for botanical or scientific reasons. It is referred to as a "controlled drug". In such countries a greater depth and variety of scientific research has been performed. Recently several habitual smokers were invited to partake in various tests by British medical companies in order for the UK government to ascertain the influence of cannabis on operating a motor vehicle.
Smoking
The process most popularly used to ingest cannabis is smoking, and for this reason most research has evaluated health effects from this method of ingestion. Other methods of ingestion may have lower or higher health risks. See section on harm reduction below for more information on other methods of ingestion.
Risks compared to tobacco
Tobacco smoking has well-established risks such as bronchitis, coughing, overproduction of mucus, wheezing and addiction. Similar risks for smoking cannabis related to airway inflammation have been suggested in a study of healthy cannabis users who exhibited similar early characteristics to tobacco smoking.
The effects of tobacco and cannabis smoking differ, however, as they affect different parts of the respiratory tract: whereas tobacco tends to penetrate to the smaller, peripheral passageways of the lungs, cannabis tends to concentrate on the larger, central passageways. One consequence of this is that cannabis, unlike tobacco, does not appear to cause emphysema, though this claim is disputed. A 2002 report by the British Lung Foundation estimated that three to four cannabis cigarettes a day were associated with the same amount of damage to the lungs as 20 or more tobacco cigarettes a day. Unlike tobacco, regular cannabis use does not appear to cause chronic obstructive pulmonary disease.
It is important to note that, in some cases, cannabis users mix commercial tobacco in joints, called "Spliff" (popular in Europe), tobacco mixed with hash in a chillum (India), or cannabis rolled in tobacco leaves (Blunt), which would expose the user to the additional risks of tobacco, such as rapid physical addiction to nicotine.
Cancer risk
Cannabis smoke contains numerous carcinogens. However, an extensive study published in 2006 by Donald Tashkin of the University of California, Los Angeles found that there is no significant link between smoking cannabis and lung cancer. The study, which involved a large population sample (1,200 people with lung, neck, or head cancer, and a matching group of 1,040 without cancer) found no correlation between marijuana smoking and increased lung cancer risk. The results indicated no correlation between long and short-term cannabis use and cancer, indicating a possible therapeutic effect. Extensive cellular studies and even some studies in animal models suggest that THC has antitumor properties, either by encouraging programmed cell death of genetically damaged cells that can become cancerous, or by restricting the development of the blood supply that feeds tumors, or both.
In 2008 a smaller study was released by the Medical Research Institute of New Zealand suggested that smoking cannabis increased the risk of lung cancer by 5.7 times over non-smokers. The small 79 person study noted that "In the near future we may see an 'epidemic' of lung cancers connected with this new carcinogen. And the future risk probably applies to many other countries, where increasing use of cannabis among young adults and adolescents is becoming a major public health problem."
Prior, a 1997 study examining the records of 64,855 Kaiser patients (14,033 of whom identified themselves as current smokers), also found no positive correlation between cannabis use and cancer.
A Research Triangle Institute study concluded that THC, a dilative agent, may help cleanse the lungs by dilating the bronchi, and could actively reduce the instance of tumors. Additionally, a study by Rosenblatt et al. found no association between marijuana use and the development of head and neck squamous cell carcinoma. However, a contrasting 2000 study linked the smoking of cannabis to the growth of cancerous tumors through the impairment of anti-tumor defenses.
A 2009 study found that cannabis use may increase the risk of testicular cancer. In particular, the risk of developing nonseminoma testicular cancer, a more aggressive form of the disease, was increased in current cannabis users and even greater in long-term chronic users. This study has prompted the rapid propagation of the slang phrase "ball cancered," as a euphemism for smoking marijuana.
UCLA study
On 23 May 2006, Donald Tashkin, M.D., Professor of Medicine at the David Geffen School of Medicine at UCLA in Los Angeles announced that the use of cannabis does not appear to increase the risk of developing lung cancer, or increase the risk of head and neck cancers, such as cancer of the tongue, mouth, throat, or esophagus.The study involved 2252 participants, with some of the most chronic marijuana smokers having smoked over 22,000 marijuana cigarettes. The finding of Donald Tashkin, M.D., and his team of researchers in 2006 refines their earlier studies published in a Dec. 17th 2000 edition of the peer-reviewed journal Cancer Epidemiology Biomarker and Prevention. Many opponents of marijuana incorrectly cite the original finding of UCLA Medical Center from 2000 as "proof" that marijuana leaves the users at higher risk for cancer of the lung, and cancerous tumors, even though the researchers at the UCLA Medical Center have revised their finding with a more in-depth study on the effects of the use of marijuana. This seemed to contradict assumptions made after some studies, like those from Dale Geirringer et al., which found that 118 carcinogens were produced when marijuana underwent combustion, and two carcinogens {2-Methyl-2, 4(2H-1-benzopyran-5-ol) & 5-azulene-3,8-dione} formed when marijuana underwent vaporization with the Volcano Vaporizer. To help explain this seemingly chemical proof of carcinogenity inherent in the process of combustion, Tashkin noted that "one possible explanation for the new findings, he said, is that THC, a chemical in marijuana smoke, may encourage aging cells to die earlier and therefore be less likely to undergo cancerous transformation."
Reducing Health Risks

The health consequences of cannabis use may vary depending on method of use. Proposed alternatives include:
- filtered cigarettes (see below)
- vaporizers (see above)--devices for inhaling THC without burning the cannabis; top temperature 210°C (410°F) compared to 815°C (1500°F) in a burning cigarette
- electronic cigarette--contains rechargeable battery and a heating element which vaporizes, in most brands, liquid nicotine from a cartridge; cannabinol could be loaded into the cartridge instead of nicotine
- one-hitters or single-toke utensils--1/4"/6-mm. diameter screened crater; suck slow for minimum burning temperature, or as close as possible to 210C(410F); minimizes THC loss; minimizes carbon monoxide dosage; eliminates side-stream smoke (see illustration, above). (More research needed about burning temperature compared to that of cigarettes or "joints").
- eating Cannabis brownies or other foods containing cannabutter or budder
- bongs-specialized pipes filtering, often cooling and sometimes diffusing smoke through water
- high potency cannabis and cannabis extracts, such as hashish or honey oil, allowing the absorption of the same amount of cannabinoids while inhaling less smoke
- bleach and glue free papers such as Aleda and RAW
Like tobacco smoke, cannabis smoke contains tars which, unlike cannabinoids themselves, are rich in carcinogenic polycyclic aromatic hydrocarbons, a prime culprit in smoking-related cancers. An obvious way to protect smokers' health is therefore to minimize the content of smoke tars relative to cannabinoids.
The most obvious way to do this is to bypass smoking completely, simply eating the cannabis by extracting the THC and other cannabinoids to a fat (like butter) or alcoholic drink, such as Green Dragon, or by vaporization.
Another way is to increase the THC potency of the cannabis (see also section on potency above). This can be done with hashish, honey oil, or high-quality cannabis. Assuming smokers adjust their smoke intake to the cannabinoid dosage by using a miniature utensil, the higher the concentration of cannabinoids, the lower the amount of tars—- and carbon monoxide—- they are likely to consume to achieve their desired effect.
Vaporizers, by heating the cannabis active constituents and aromatic substances to be inhaled without combustion of the preparation, almost exclude the risk altogether. A 2000 study conducted by NORML and MAPS found that the two tested vaporizers delivered significantly fewer carcinogens than a cigarette.
A lower temperature combustion method like burning a cooler fuel, or focusing a magnifying glass in respect to the sun, are other ways to selectively burn substances without a vaporizer or water pipe.
Pathogens and microtoxins
Most microorganisms found in cannabis only affect plants and not humans, but some microorganisms, especially those that proliferate when the herb is not correctly dried and stored, can be harmful to humans.
Fungi
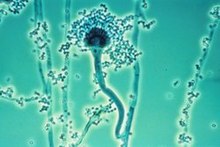
The fungi Aspergillus flavus, Aspergillus fumigatus, Aspergillus niger, Aspergillus parasiticus, Aspergillus tamarii, Aspergillus sulphureus, Aspergillus repens, Mucor hiemalis (not a human pathogen), Penicillin chrysogenum, Penicillin italicum and Rhizopus nigrans have been found in moldy cannabis. Aspergillus mold species can infect the lungs via smoking or handling of infected cannabis and cause opportunistic and sometimes deadly Aspergillosis. Some of the microorganisms found create aflatoxins, which are toxic and carcinogenic. Researchers suggest that moldy cannabis thus be discarded.
Mold is also found in smoke from mold infected cannabis, and the lungs and nasal passages are a major means of contracting fungal infections. "Levitz and Diamond (1991) suggested baking marijuana in home ovens at 150 °C , for five minutes before smoking. Oven treatment killed conidia of A. fumigatus, A. flavus and A. niger, and did not degrade the active component of marijuana, tetrahydrocannabinol (THC)."
Bacteria
Cannabis contaminated with Salmonella muenchen was positively correlated with dozens of cases of salmonellosis in 1981. "Thermophilic actinomycetes" were also found in cannabis.
See also
- Harm reduction
- Medical cannabis
- Psychoactive drug
- Responsible drug use
- Tradable smoking pollution permits
- National Cannabis Prevention and Information Centre
- Contact high
References
- ^ Ranganathan M, D'Souza DC (2006). "The acute effects of cannabinoids on memory in humans: a review". Psychopharmacology (Berl.). 188 (4): 425–44. doi:10.1007/s00213-006-0508-y. PMID 17019571.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Grotenhermen F (2007). "The toxicology of cannabis and cannabis prohibition". Chem. Biodivers. 4 (8): 1744–69. doi:10.1002/cbdv.200790151. PMID 17712818.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Riedel G, Davies SN (2005). "Cannabinoid function in learning, memory and plasticity". Handb Exp Pharmacol (168): 445–77. PMID 16596784.
- Leweke FM, Koethe D (2008). "Cannabis and psychiatric disorders: it is not only addiction". Addict Biol. 13 (2): 264–75. doi:10.1111/j.1369-1600.2008.00106.x. PMID 18482435.
{{cite journal}}: Unknown parameter|month=ignored (help) - Rubino T, Parolaro D (2008). "Long lasting consequences of cannabis exposure in adolescence". Mol. Cell. Endocrinol. 286 (1-2 Suppl 1): S108–13. doi:10.1016/j.mce.2008.02.003. PMID 18358595.
{{cite journal}}: Unknown parameter|month=ignored (help) - DeLisi LE (2008). "The effect of cannabis on the brain: can it cause brain anomalies that lead to increased risk for schizophrenia?". Curr Opin Psychiatry. 21 (2): 140–50. doi:10.1097/YCO.0b013e3282f51266. PMID 18332661.
{{cite journal}}: Unknown parameter|month=ignored (help) - Johnson, Pamela J. (2005). "Marijuana and Depression: USC College study finds no link between symptoms of depression and regular marijuana use". University of Southern California. Retrieved 2008-08-10.
{{cite web}}: Unknown parameter|month=ignored (help) - Press Conference On World Health Organization Report On Global Tobacco Epidemic
- ^ Australian Government Department of Health: National Cannabis Strategy Consultation Paper, page 4. "Cannabis has been described as a 'Trojan Horse' for nicotine addiction, given the usual method of mixing cannabis with tobacco when preparing marijuana for administration."
- Cannabis Vaporizer Combines Efficient Delivery of THC with Effective Suppression of Pyrolytic Compounds By D. Gieringer et.al. Journal of Cannabis Therapeutics, Vol. 4(1) 2004,
- Hazekamp A, Ruhaak R, Zuurman L, van Gerven J, Verpoorte R (2006). "Evaluation of a vaporizing device (Volcano) for the pulmonary administration of tetrahydrocannabinol". J Pharm Sci. 95 (6): 1308–17. doi:10.1002/jps.20574. PMID 16637053.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ H.K. Kalant & W.H.E. Roschlau (1998). Principles of Medical Pharmacology (6th edition ed.). pp. 373–375.
{{cite book}}:|edition=has extra text (help) - Turner C, Bouwsma O, Billets S, Elsohly M (1980). "Constituents of Cannabis sativa L. XVIII--Electron voltage selected ion monitoring study of cannabinoids". Biomed. Mass Spectrom. 7 (6): 247–56. doi:10.1002/bms.1200070605. PMID 7426688.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ J.E. Joy, S. J. Watson, Jr., and J.A. Benson, Jr, (1999). Marijuana and Medicine: Assessing The Science Base. Washington D.C: National Academy of Sciences Press.
{{cite book}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - Hampson AJ, Grimaldi M, Axelrod J, Wink D (1998). "Cannabidiol and (-)Δ9-tetrahydrocannabinol are neuroprotective antioxidants". Proc. Natl. Acad. Sci. U.S.A. 95 (14): 8268–73. PMC 20965. PMID 9653176.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ H. Abadinsky (2004). Drugs: An Introduction (5th edition ed.). pp. 62–77, 160–166.
{{cite book}}:|edition=has extra text (help) - "Erowid Cannabis (Marijuana) Vault". Retrieved 18 August 2004.
{{cite web}}: Unknown parameter|dateformat=ignored (help) - "What is the lethal dose of cannabis". Retrieved 18 February 2009.
- Web4Health: Physical effects of cannabis/haschish/marijuana Written by: Wendy Moelker, Psychologist in charge, tutor, Emergis center for mental health care, Goes, the Netherlands. Latest revision: 19 Sep 2008.
- Andersson M, Usiello A, Borgkvist A; et al. (2005). "Cannabinoid action depends on phosphorylation of dopamine- and cAMP-regulated phosphoprotein of 32 kDa at the protein kinase A site in striatal projection neurons". J. Neurosci. 25 (37): 8432–8. doi:10.1523/JNEUROSCI.1289-05.2005. PMID 16162925.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - http://www.erowid.org/plants/cannabis/cannabis_effects.shtml
- Fant R, Heishman S, Bunker E, Pickworth W (1998). "Acute and residual effects of marijuana in humans". Pharmacol. Biochem. Behav. 60 (4): 777–84. doi:10.1016/S0091-3057(97)00386-9. PMID 9700958.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Tj. T. Mensinga; et al., A double-blind, randomized, placebo-controlled, cross-over study on the pharmacokinetics and effects of cannabis (PDF), RIVM, retrieved 2007-09-21
{{citation}}: Explicit use of et al. in:|author=(help) - Curran HV, Brignell C, Fletcher S, Middleton P, Henry J (2002). "Cognitive and subjective dose-response effects of acute oral Delta 9-tetrahydrocannabinol (THC) in infrequent cannabis users". Psychopharmacology (Berl.). 164 (1): 61–70. doi:10.1007/s00213-002-1169-0. PMID 12373420.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Pertwee R (1997). "Pharmacology of cannabinoid CB1 and CB2 receptors". Pharmacol. Ther. 74 (2): 129–80. doi:10.1016/S0163-7258(97)82001-3. PMID 9336020.
- Eubanks L, Rogers C, Beuscher A, Koob G, Olson A, Dickerson T, Janda K (2006). "A molecular link between the active component of marijuana and Alzheimer's disease pathology". Mol. Pharm. 3 (6): 773–7. doi:10.1021/mp060066m. PMID 17140265.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Judge Young - Part 4
- 1996. The Merck Index, 12th ed., Merck & Co., Rahway, New Jersey
- Erowid. "Cannabis Chemistry". Retrieved 2006-03-20.
- "UK government report" (PDF). House of Commons Science and Technology Committee. 2006-07-18. Retrieved 2006-08-29.]
- Moir D, Rickert WS, Levasseur G, Larose Y, Maertens R, White P, Desjardins S. (2007). "A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions". Chem. Res. Toxicol. 21: 494. doi:10.1021/tx700275p. PMID 18062674.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Department of Dermatology, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland Bernard Noël, MD, Isabelle Ruf, MD, Renato G. Panizzon, MD
- "Heavy pot smoking could raise risk of heart attack, stroke". CBC.
- Soapbar - Just Say No to polluted hash
- Flin Flon Mine Area Marijuana Contamination
- BBC NEWS | England | Devon | Warnings over glass in cannabis
- Zhang, Z.-F., Morgenstern, H., Spitz, M. R., Tashkin, D. P., Yu, G.-P., Marshall, J. R., Hsu, T. C., and Schantz, S. P. 1999.
- Public opinion on drugs and drug policy. Transform Drug Policy Foundation: Fact Research Guide. "Data is notoriously easy to cherry pick or spin to support a particular agenda or position. Often the raw data will conceal all sorts of interesting facts that the headlines have missed." Transform Drug Policy Foundation, Easton Business Centre, Felix Rd., Bristol, UK. Retrieved on 24 March 2007.
- Sarafian TA, Kouyoumjian S, Tashkin D, Roth MD (2002). "Synergistic cytotoxicity of Delta(9)-tetrahydrocannabinol and butylated hydroxyanisole". Toxicol. Lett. 133 (2–3): 171–9. PMID 12119125.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - UCSB's SexInfo - Sex Under the Influence
- W. Hall, N. Solowij (1998). "Adverse Effects of Cannabis". The Lancet. 352: 1611–6. doi:10.1016/S0140-6736(98)05021-1.
{{cite journal}}: Unknown parameter|month=ignored (help) - H. Schuel; et al. (2002). "Evidence that anandamide-signaling regulates human sperm functions required for fertilization". Molecular Reproduction and Development. 63 (3): 376–387. doi:10.1002/mrd.90021.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - S.J. Astley, S.K. Clarren, R.E. Little, P.D. Sampson, J.R. Daling (1992). "Analysis of facial shape in children gestationally exposed to marijuana, alcohol, and/or cocaine". Pediatrics. 89 (1): 67–77.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - R. Berkow MD; et al. (1997). The Merck Manual of Medical Information (Home Edition). p. 449.
{{cite book}}: Explicit use of et al. in:|author=(help) - J.S. Hayes, R. Lampart, M.C. Dreher, L. Morgan (1991). "Five-year follow-up of rural Jamaican children whose mothers used marijuana during pregnancy". West Indian Medical Journal. 40 (3): 120–3. doi:10.1590/S1516-31802004000300007.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - M.C. Dreher, K. Nugent, R. Hudgins (1994). "Prenatal Marijuana Exposure and Neonatal Outcomes in Jamaica: An Ethnographic Study". Pediatrics. 93 (3): 254–260. doi:10.1590/S1516-31802004000300007.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Huizink AC, Mulder EJ (2006). "Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring". Neurosci Biobehav Rev. 30 (1): 24–41. doi:10.1016/j.neubiorev.2005.04.005. PMID 16095697.
- Fried PA, Watkinson B, Gray R (2003). "Differential effects on cognitive functioning in 13- to 16-year-olds prenatally exposed to cigarettes and marihuana". Neurotoxicol Teratol. 25 (4): 427–36. PMID 12798960.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hardwiring the Brain: Endocannabinoids Shape Neuronal Connectivity Science, May 25, 2007
- Paul Berghuis,...:Endocannabinoids regulate interneuron migration and morphogenesis... 2007
- Harkany et al: The emerging functions of endocannabinoid signaling during CNS development
- JR Minkel: Marijuana-Like Chemicals Guide Fetal Brain Cells, Scientific American, May24, 2007
- J.S. Hayes, R. Lampart, M.C. Dreher, L. Morgan (1991). "Five-year follow-up of rural Jamaican children whose mothers used marijuana during pregnancy". West Indian Medical Journal. 40 (3): 120–3. doi:10.1590/S1516-31802004000300007.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Dreher, M. C., Nugent, K., Hudgins, R. 1994. Prenatal marijuana exposure and neonatal outcomes in Jamaica: an ethnographic study. Pediatrics 93(2): 254-260. Retrieved on 5 March 2007
- Withdrawal Symptoms From Smoking Pot?
- "Combination of Cognitive-Behavioral Therapy and Motivational Incentives Enhance Treatment for Marijuana Addiction" (Press release). National Institutes of Health. April 1, 2006.
- 1998 INSERM-CNRS report, directed by Pr. Bernard Roques and commissioned by Health Secretary of State Bernard Kouchner
- Henquet, C., Krabbendam, L., Spauwen, J., Kaplan, C., Lieb, R., Wittchen, H.-U., and van Os, J. 2005. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 330(7481): 11. Retrieved on 4 March 2007
- Patton, G. C., Coffey, C., Carlin, J. B., Degenhardt, L., Lynskey, M., and Hall, W. 2002. Cannabis use and mental health in young people: cohort study. BMJ 325(7374): 1195-1198. Retrieved 45 March 2007
- Fergusson, David M.; Horwood, John L.; Ridder, Elizabeth M. "Research Report: Tests of causal linkages between cannabis use and psychotic symptoms. University of Otago Christchurch School of Medicine published in the Society for the Study of Addiction (2004-11-05). Retrieved on 2007-11-03.
- Hall, Wayne; Degenhardt, Lousia; Teesson, Maree. "Cannabis use and psychotic disorders: an update". Office of Public Policy and Ethics, Institute for Molecular Bioscience University of Queensland Australia, and National Drug and Alcohol Research Centre University of New South Wales Australia published in Drug and Alcohol Review (December 2004). Vol 23 Issue 4. Pg 433-443
- Arseneault, Louise; Cannon, Mary; Wiitton, John; Murray, Robin M. "Causal association between cannabis and psychosis:Causal association between cannabis and psychosis: examination of the evidence". Institute of Psychiatry published in British Journal of Psychiatry (2004). #184, Pg. 110-117
- Earth Erowid (2005). "Cannabis & Psychosis - A guide to current research about cannabis and mental health".
- Robert E. Drake M.D.,Ph.D. and Michael A. Wallach Ph.D. Substance Abuse Among the Chronic Mentally Ill
- "Cannabis 'raises psychosis risk'". BBC News (2007-07-27). Retrieved on 2007-11-03.
- ^ 'Cheers', U.K study of alcohol and its role in mental health
- eMedicine - Alcohol-Related Psychosis : Article by Michael Larson
- http://www.alzheimers.org.uk/site/scripts/documents_info.php?categoryID=200171&documentID=98
- Tien AY (1990). "Epidemiological analysis of alcohol and drug use as risk factors for psychotic experiences". J Nerv Ment Dis. 178 (8): 473–80. doi:10.1097/00005053-199017880-00001. PMID 2380692.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - Jouko Miettunen, PhD ... Association of cannabis use with prodromal symptoms of psychosis in adolescence, The British Journal of Psychiatry (2008) 192: 470-471.
- N.Q. Brill, R.L. Christie (1974). "Marihuana and Psychosocial Adjustment". Archives of General Psychiatry. 31: 713–719.
- H.H. Mendelson, J.C. Kuehnle, I. Greenberg; N.K. Mello (1976). "The Effects of Marihuana Use on Human Operant Behavior: Individual Data…". Pharmacology of Marihuana. Vol. 2. New York: Academic Press. pp. 643–653.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ T.F. Denson, M. Earleywine (June 20, 2005). "Decreased depression in marijuana users". Addictive Behaviors.
- Maria Ellgren, Sabrina M Spano & Yasmin L Hurd (July 5, 2006). "Adolescent Cannabis Exposure Alters Opiate Intake and Opioid Limbic Neuronal Populations in Adult Rats" ( – ). Neuropsychopharmacology. advance online.
{{cite journal}}: External link in|format= - Maria Ellgren, Sabrina M Spano & Yasmin L Hurd (July 5, 2006). "Adolescent Cannabis Exposure Alters Opiate Intake and Opioid Limbic Neuronal Populations in Adult Rats" ( – ). Neuropsychopharmacology. advance online.
{{cite journal}}: External link in|format= - Michael Hopkin (July 5, 2006). "Rats taking cannabis get taste for heroin". Nature.
- Marijuana Use Per Se Not a 'Gateway' To Illicit Drug Use, Study Says - NORML
- Predictors of Marijuana Use in Adolescents Before and After Licit Drug Use: Examination of the Gateway Hypothesis - Tarter et al. 163 (12): 2134 - Am J Psychiatry
- RAND | News Release | RAND Study Casts Doubt on Claims That Marijuana Acts as "Gateway" to the Use of Cocaine and Heroin
- Cécile Henquet, Lydia Krabbendam, Janneke Spauwen, Charles Kaplan, Roselind Lieb, Hans-Ulrich Wittchen and Jim van Os (2004). "Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people". British Medical Journal. 330 (11): 11. doi:10.1136/bmj.38267.664086.63. PMID 15574485.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Cécile Henquet, Lydia Krabbendam, Janneke Spauwen, Charles Kaplan, Roselind Lieb, Hans-Ulrich Wittchen and Jim van Os (2004). "Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people". British Medical Journal. 330 (11): 11. doi:10.1136/bmj.38267.664086.63. PMID 15574485.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - L. Arseneault; et al. (2004). "Causal association between cannabis and psychosis: examination of the evidence". The British Journal of Psychiatry. 184: 110–117. doi:10.1192/bjp.184.2.110. PMID 14754822.
{{cite journal}}: Explicit use of et al. in:|author=(help) - S. Andreasson; et al. (1987). "Cannabis and Schizophrenia: A Longitudinal Study of Swedish Conscripts". The Lancet. 2: 1483–1486. doi:10.1016/S0140-6736(87)92620-1.
{{cite journal}}: Explicit use of et al. in:|author=(help) - J. Schiffman; et al. (30 March 2005). "Symptoms of schizotypy precede cannabis use". Psychiatry Research. 134 (1): 37–42. doi:10.1016/j.psychres.2005.01.004.
{{cite journal}}: Explicit use of et al. in:|author=(help) - Boydell J, Dean K, Dutta R, Giouroukou E, Fearon P, Murray R (2007). "A comparison of symptoms and family history in schizophrenia with and without prior cannabis use: implications for the concept of cannabis psychosis". Schizophr. Res. 93 (1–3): 203–10. doi:10.1016/j.schres.2007.03.014. PMID 17462864.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Louise Arseneault, Mary Cannon, Richie Poulton, Robin Murray, Avshalom Caspi, Terrie E Moffitt (23 November 2002). "Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study" (PDF). British Medical Journal.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Avshalom Caspi, Terrie E. Moffitt, Mary Cannon, Joseph McClay, Robin Murray, HonaLee Harrington, Alan Taylor, Louise Arseneault, Ben Williams, Antony Braithwaite, Richie Poulton, and Ian W. Craig (18 January 2005). "Moderation of the Effect of Adolescent-Onset Cannabis Use on Adult Psychosis by a Functional Polymorphism in the catechol-O-Methyltransferase Gene: Longitudinal Evidence of a Gene X Environment Interaction" (PDF). Society of Biological Psychiatry. 122. doi:10.1590/S1516-31802004000300007.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Giuffrida A, Leweke FM, Gerth CW; et al. (2004). "Cerebrospinal anandamide levels are elevated in acute schizophrenia and are inversely correlated with psychotic symptoms". Neuropsychopharmacology. 29 (11): 2108–14. doi:10.1038/sj.npp.1300558. PMID 15354183.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link), New Scientist - Degenhardt L, Hall W, Lynskey M ,Comorbidity between cannabis use and psychosis: Modelling some possible relationships. Technical Report No. 121. Sydney: National Drug and Alcohol Research Centre. 2001, Retrieved on 19.18.2006
- Ad Hoc Group of Experts. "Report to the Director, National Institutes of Health" (Workshop on the Medical Utility of Marijauana). Institute of Medicine.
- ^ Bonsor, Kevin. "How Marijauan Works: Other Physiological Effects". HowStuffWorks. Retrieved on 2007-11-03
- Curran HV, Brignell C, Fletcher S, Middleton P, Henry J (2002). "Cognitive and subjective dose-response effects of acute oral Delta 9-tetrahydrocannabinol (THC) in infrequent cannabis users". Psychopharmacology (Berl.). 164 (1): 61–70. doi:10.1007/s00213-002-1169-0. PMID 12373420.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - van der Stelt M, Veldhuis WB, Bär PR, Veldink GA, Vliegenthart JF, Nicolay K (2001). "Neuroprotection by Delta9-tetrahydrocannabinol, the main active compound in marijuana, against ouabain-induced in vivo excitotoxicity". J. Neurosci. 21 (17): 6475–9. PMID 11517236.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Yücel M, Solowij N, Respondek C; et al. (2008). "Regional brain abnormalities associated with long-term heavy cannabis use". Arch. Gen. Psychiatry. 65 (6): 694–701. doi:10.1001/archpsyc.65.6.694. PMID 18519827.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hippocampal Neurotoxicity of Delta 9-Tetrahydrocannabinol - Chan et al. 18 (14): 5322 - Journal of Neuroscience
- INSERM-CNRS. Released June 1998. Excerpts from the Roques report. Hemp Info. Retrieved 5 March 2007
- Rapport Roques sur la dangerosité des drogues. (in French). Retrieved on 5 March 2007
- L'alcool aussi dangereux que l'héroïne. (in French) Retrieved on 5 March 2007
- Lyle E. Craker, Ph. D. v. U.S. Drug Enforcement Administration, Docket No. 05-16, May 8 2006, 8-27 PDF
- M.D. Roth; et al. (1998). "Airway Inflammation in Young Marijuana and Tobacco Smokers". American Journal of Respiratory and Critical Care Medicine. 157 (3): 928–937. PMID 9517614.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - http://www.lunguk.org/downloads/A_Smoking_Gun.pdf
- D.P. Tashkin; et al. (1997). "Heavy habitual marijuana smoking does not cause an accelerated decline in FEV1 with age". Am. J. Respir. Crit. Care Med. 155 (1): 141–148. doi:10.1136/thx.2006.077081.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - Hashibe M, Straif K, Tashkin D, Morgenstern H, Greenland S, Zhang Z (2005). "Epidemiologic review of marijuana use and cancer risk". Alcohol. 35 (3): 265–75. doi:10.1016/j.alcohol.2005.04.008. PMID 16054989.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Novotny M, Lee M, Bartle K (1976). "A possible chemical basis for the higher mutagenicity of marijuana smoke as compared to tobacco smoke". Experientia. 32 (3): 280–2. doi:10.1007/BF01940790. PMID 1253890.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - http://www.norml.org/pdf_files/NORML_Cannabis_Smoke_Cancer.pdf
- "Study Finds No Cancer-Marijuana Connection". Washington Post. 2006-05-26. Retrieved 2007-02-23.
{{cite news}}: External link in|publisher= - WebMD (23 May 2006). "Pot Smoking Not Linked to Lung Cancer". ScienceNOW, Abstract
- Cannabis bigger cancer risk than cigarettes: study | Health | Reuters
- S. Sidney (1997). "Marijuana use and cancer incidence (California, United States)". Cancer Causes and Control. 8 (5): 722–728. doi:10.1023/A:1018427320658.
{{cite journal}}: Unknown parameter|month=ignored (help) - J. Huff & P. Chan (2000). "Antitumor Effects of THC". Environmental Health Perspectives. 108 (10): A442–3. doi:10.2307/3435034.
{{cite journal}}: Unknown parameter|month=ignored (help) - K.A. Rosenblatt; et al. (1 June 2004). "Marijuana Use and Risk of Oral Squamous Cell Carcinoma". Cancer Research. 64: 4049–4054. doi:10.1158/0008-5472.CAN-03-3425. PMID 15173020.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Dr. Steven M. Dubinett (2006-07). "Study Finds Marijuana Ingredient Promotes Tumor Growth, Impairs Anti-Tumor Defenses".
{{cite news}}: Check date values in:|date=(help); Unknown parameter|org=ignored (help) - "Marijuana may raise testicular cancer risk", MSNBC, Reuters, 9 February 2009
- ^ "Study Finds No Link Between Marijuana Use And Lung Cancer". 26 May 2006.
{{cite news}}: Unknown parameter|org=ignored (help) Cite error: The named reference "Study Finds No Link Between Marijuana Use And Lung Cancer" was defined multiple times with different content (see the help page). - Fred Gardner (2006-07-06). "Marijuana Smoking Does Not Cause Lung Cancer".
{{cite news}}: Unknown parameter|org=ignored (help) - Tashkin, D. P., Simmons, M. S., Sherrill, D. L., and Coulson, A. H. 1997. Heavy habitual marijuana smoking does not cause an accelerated decline in FEV1 with age. American Journal of Respiratory and Critical Care Medicine 155(1): 141-148. Retrieved on 5 March 2007
- "Study finds no marijuana-lung cancer link". Washington Post. 2006-05-26. Retrieved 2006-07-13.
- Sarafian TA, Kouyoumjian S, Tashkin D, Roth MD (2002). "Synergistic cytotoxicity of Delta(9)-tetrahydrocannabinol and butylated hydroxyanisole". Toxicol. Lett. 133 (2–3): 171–9. PMID 12119125.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - B. Mirken (17 September 1999). "Vaporizers for Medical Marijuana". AIDS Treatment News. 327.
- ^ "Microbiological contaminants of marijuana". www.hempfood.com. Retrieved 2008-06-22.
- ^ Kagen SL, Kurup VP, Sohnle PG, Fink JN (1983). "Marijuana smoking and fungal sensitization". J. Allergy Clin. Immunol. 71 (4): 389–93. PMID 6833678.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - lib.bioinfo.pl
External links
- How marijuana works from HowStuffWorks
- Microbiological contaminants of marijuana
- Cannabis Use and Psychosis from National Drug and Alcohol Research Centre, Australia
- The key research on cannabis use and mental illness at BBC News
- Provision of Marijuana and Other Compounds For Scientific Research recommendations of The National Institute on Drug Abuse National Advisory Council
- Scientific American Magazine (December 2004 Issue) The Brain's Own Marijuana
- Ramström, J. (2003), Adverse Health Consequences of Cannabis Use, A Survey of Scientific Studies Published up to and including the Autumn of 2003, National institute of public health, Sweden, Stockholm.
- Hall, W., Solowij, N., Lemon, J., The Health and Psychological Consequences of Cannabis Use. Canberra: Australian Government Publishing Service; 1994.
- Deaths from Marijuana v. 17 FDA-Approved Drugs
- Benefits and risks of marijuana use in treating various diseases & conditions Analysis includes AIDS, Alzheimer's, Crohn's, glaucoma, depression, arthritis, etc.
- World Health Organisation, PROGRAMME ON SUBSTANCE ABUSE, Cannabis: a health perspective and research agenda;1997.
- ProCon's Marijuana Health Facts
- Bibliography of scholarly histories on cannabis and hashish. (Updated to include article abstracts.)
- Marijuana and Immunity
- The National Cannabis Prevention and Information Centre (Australia)
- EU Research paper on the potency of Cannabis (2004)(.pdf)
| Cannabis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| General | |||||||||
| Usage |
| ||||||||
| Variants | |||||||||
| Effects |
| ||||||||
| Culture | |||||||||
| Organizations |
| ||||||||
| Demographics | |||||||||
| Politics |
| ||||||||
| Related | |||||||||