This is an old revision of this page, as edited by Nono64 (talk | contribs) at 20:30, 18 January 2011 (Low-density lipoprotein). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 20:30, 18 January 2011 by Nono64 (talk | contribs) (Low-density lipoprotein)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff) Pharmaceutical compound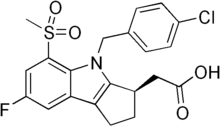 | |
| Clinical data | |
|---|---|
| Other names | MK-0524A |
| License data | |
| Routes of administration | Oral |
| ATC code | |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| KEGG | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.207.712 |
| Chemical and physical data | |
| Formula | C21H19ClFNO4S |
| Molar mass | 435.90 g/mol g·mol |
Laropiprant (INN) is used in combination with niacin to reduce blood cholesterol (LDL and VLDL). Merck & Co. planned to market this combination under the trade names Cordaptive and Tredaptive. On April 28, 2008, the U.S. Food and Drug Administration (FDA) issued a "not approved" letter for Cordaptive. Tredaptive was approved by the European Medicines Agency (EMA) on July 3, 2008.
Laropiprant itself has no cholesterol lowering effect, but it reduces facial flushes induced by niacin. In a trial with 1613 patients, 10.2% patients stopped taking the medication in the Cordaptive group versus 22.2% under niacin monotherapy.
Tredaptive contains 1000 mg of niacin and 20 mg of laropiprant in each tablet.
Mechanism of action
Niacin in cholesterol lowering doses (500–2000 mg per day) causes facial flushes by stimulating biosynthesis of prostaglandin D2, especially in the skin. PG D2 acts as a vasodilator via DP1 receptors, increasing blood flow and thus leading to flushes.
Laropiprant acts as a DP1 antagonist, reducing the vasodilation.
Taking 650 mg of aspirin 20–30 minutes prior to taking niacin has also been proven to prevent flushing in 90% of patients, presumably by suppressing prostaglandin synthesis, but this medication also increases the risk of gastrointestinal bleeding, though the increased risk is less than 1 percent.
References
- Carey, John (April 29, 2008). "FDA Rejects Merck's Cordaptive". BusinessWeek. Retrieved 2009-11-13.
- "Tredaptive European Public Assessment Report". European Medicines Agency. Retrieved November 13, 2009.
-
Lai E, De Lepeleire I, Crumley TM; et al. (2007). "Suppression of niacin-induced vasodilation with an antagonist to prostaglandin D2 receptor subtype 1". Clin. Pharmacol. Ther. 81 (6): 849–57. doi:10.1038/sj.clpt.6100180. PMID 17392721.
{{cite journal}}:|access-date=requires|url=(help); Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Tredaptive Prescribing Information" (PDF). Merck & Co. Retrieved 2009-11-14.
- PMID 19878384
- Richard A. Kunin (1976). "The Action of Aspirin in Preventing the Niacin Flush and its Relevance to the Antischizophrenic Action of Megadose Niacin" (PDF). Orthomolecular Psychiatry. 5 (2): 89–100. Retrieved 2009-11-14.
-
Sørensen HT, Mellemkjaer L, Blot WJ; et al. (2000). "Risk of upper gastrointestinal bleeding associated with use of low-dose aspirin". Am. J. Gastroenterol. 95 (9): 2218–24. doi:10.1111/j.1572-0241.2000.02248.x. PMID 11007221.
{{cite journal}}:|access-date=requires|url=(help); Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
| Lipid-lowering agents (C10) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GI tract |
| ||||||||||||
| Liver |
| ||||||||||||
| Blood vessels |
| ||||||||||||
| Combinations | |||||||||||||
| Other | |||||||||||||
| |||||||||||||