| Revision as of 08:29, 16 November 2011 editJfdwolff (talk | contribs)Administrators81,547 edits rv, this is a case report (see WP:MEDRS) - discuss on talk← Previous edit | Latest revision as of 17:15, 5 January 2025 edit undo188.83.49.79 (talk) →HistoryTags: Mobile edit Mobile web edit | ||
| (853 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
| {{Short description|Anticoagulant medication}} | |||
| {{About|the drug with the brandname Coumadin|the anticoagulant rodenticide poisons often called "coumarins" or "coumadins"|4-hydroxycoumarins}} | |||
| {{Redirect|Coumadin|the class of compounds known as "coumadins"|Coumadins|the natural compound|Coumarin}} | |||
| {{Redirect|Waran|the Polish Armored Personnel Carrier|Waran (armored personnel carrier)}} | |||
| {{Use dmy dates|date=October 2010}} | |||
| {{Good article}} | |||
| {{drugbox | Verifiedfields = changed | |||
| {{Use dmy dates|date=January 2024}} | |||
| | verifiedrevid = 413746125 | |||
| {{Use American English|date=June 2018}} | |||
| | IUPAC_name = (''RS'')-4-hydroxy- 3-(3- oxo- 1-phenylbutyl)- 2''H''- chromen- 2-one | |||
| {{cs1 config|name-list-style=vanc|display-authors=6}} | |||
| {{Infobox drug | |||
| | Verifiedfields = changed | |||
| | Watchedfields = changed | |||
| | verifiedrevid = 460939157 | |||
| | image = Warfarin.svg | | image = Warfarin.svg | ||
| | width = 200 | |||
| | image2 = Warfarin-from-xtal-3D-balls.png | |||
| | alt = | |||
| | image2 = Warfarin ball-and-stick model.png | |||
| | width2 = 200 | |||
| | alt2 = | |||
| | caption = | |||
| <!--Clinical data--> | <!-- Clinical data --> | ||
| | pronounce = {{IPAc-en|ˈ|w|ɔːr|f|ər|ɪ|n}} | |||
| | tradename = Coumadin | |||
| | tradename = Coumadin, others<ref name=brands /><ref name=brands2/><ref name=brands3/> | |||
| | Drugs.com = {{drugs.com|monograph|coumadin}} | |||
| | Drugs.com = {{drugs.com|monograph|warfarin-sodium}} | |||
| | MedlinePlus = a682277 | | MedlinePlus = a682277 | ||
| | DailyMedID = Warfarin | |||
| | pregnancy_AU = D | | pregnancy_AU = D | ||
| | pregnancy_AU_comment = <ref name="Drugs.com pregnancy">{{cite web | title=Warfarin Use During Pregnancy | website=Drugs.com | date=4 September 2019 | url=https://www.drugs.com/pregnancy/warfarin.html | access-date=7 February 2020 | archive-date=9 February 2018 | archive-url=https://web.archive.org/web/20180209025743/https://www.drugs.com/pregnancy/warfarin.html | url-status=live }}</ref> | |||
| | pregnancy_US = X | |||
| | pregnancy_category = | |||
| | routes_of_administration = ], ] | |||
| | class = | |||
| | ATC_prefix = B01 | |||
| | ATC_suffix = AA03 | |||
| | ATC_supplemental = {{ATCvet|B01|AA03}} | |||
| <!-- Legal status --> | |||
| | legal_AU = S4 | | legal_AU = S4 | ||
| | legal_AU_comment = | |||
| | legal_BR = <!-- OTC, A1, A2, A3, B1, B2, C1, C2, C3, C4, C5, D1, D2, E, F --> | |||
| | legal_BR_comment = | |||
| | legal_CA = Rx-only | |||
| | legal_CA_comment = <ref>{{cite web | title=Product information | website=] | date=3 August 2000 | url=https://health-products.canada.ca/dpd-bdpp/info?lang=eng&code=163 | access-date=23 September 2024 | archive-date=23 September 2024 | archive-url=https://web.archive.org/web/20240923050123/https://health-products.canada.ca/dpd-bdpp/info?lang=eng&code=163 | url-status=live }}</ref><ref>{{cite web | title=Product information | website=] | date=30 June 2020 | url=https://health-products.canada.ca/dpd-bdpp/info?lang=eng&code=12818 | access-date=23 September 2024 | archive-date=23 September 2024 | archive-url=https://web.archive.org/web/20240923050024/https://health-products.canada.ca/dpd-bdpp/info?lang=eng&code=12818 | url-status=live }}</ref> | |||
| | legal_DE = <!-- Anlage I, II, III or Unscheduled --> | |||
| | legal_DE_comment = | |||
| | legal_NZ = <!-- Class A, B, C --> | |||
| | legal_NZ_comment = | |||
| | legal_UK = POM | | legal_UK = POM | ||
| | legal_UK_comment = <ref>{{cite web | title=Summary of Product Characteristics (SmPC) | website=(emc) | date=7 November 2023 | url=https://www.medicines.org.uk/emc/product/2803/smpc | access-date=23 September 2024 | archive-date=18 August 2022 | archive-url=https://web.archive.org/web/20220818112658/https://www.medicines.org.uk/emc/product/2803/smpc | url-status=live }}</ref> | |||
| | legal_US = Rx-only | | legal_US = Rx-only | ||
| | legal_US_comment = <ref name="Coumadin FDA label">{{cite web | title=Coumadin- warfarin sodium tablet | website=DailyMed | url=https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3ebcb71e-9a7e-4969-abb9-7c7d3e3aae3c | access-date=25 December 2021 | archive-date=26 December 2021 | archive-url=https://web.archive.org/web/20211226074624/https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3ebcb71e-9a7e-4969-abb9-7c7d3e3aae3c | url-status=live }}</ref> | |||
| | routes_of_administration = Oral or ] | |||
| | legal_EU = | |||
| | legal_EU_comment = | |||
| | legal_UN = <!-- N I, II, III, IV / P I, II, III, IV --> | |||
| | legal_UN_comment = | |||
| | legal_status = <!-- For countries not listed above --> | |||
| <!--Pharmacokinetic data--> | <!-- Pharmacokinetic data --> | ||
| | bioavailability = 79–100% (by mouth)<ref name = PCK>{{cite journal | vauthors = Holford NH | title = Clinical pharmacokinetics and pharmacodynamics of warfarin. Understanding the dose-effect relationship | journal = Clinical Pharmacokinetics | volume = 11 | issue = 6 | pages = 483–504 | date = December 1986 | pmid = 3542339 | doi = 10.2165/00003088-198611060-00005 | s2cid = 92210077 }}</ref> | |||
| | bioavailability = 100% | |||
| | protein_bound = 99 |
| protein_bound = 99%<ref name=TGA/> | ||
| | metabolism = |
| metabolism = ]: ], ], 2C8, 2C18, ] and ]<ref name = TGA /> | ||
| | metabolites = | |||
| | elimination_half-life = 40 hours | |||
| | onset = | |||
| | excretion = ] (92%) | |||
| | elimination_half-life = 1 week (active half-life is 20-60 hours)<ref name = TGA /> | |||
| | duration_of_action = | |||
| | excretion = ] (92%)<ref name = TGA /> | |||
| <!--Identifiers--> | <!-- Identifiers --> | ||
| | index2_label = as salt | |||
| | CASNo_Ref = {{cascite|correct|CAS}} | |||
| | CAS_number_Ref = {{cascite|correct|??}} | | CAS_number_Ref = {{cascite|correct|??}} | ||
| | CAS_number = 81-81-2 | | CAS_number = 81-81-2 | ||
| | |
| CAS_number2 = 129-06-6 | ||
| | CAS_supplemental = | |||
| | ATC_suffix = AA03 | |||
| | PubChem = |
| PubChem = 54678486 | ||
| | PubChem2 = 16204922 | |||
| | IUPHAR_ligand = 6853 | |||
| | DrugBank_Ref = {{drugbankcite|changed|drugbank}} | | DrugBank_Ref = {{drugbankcite|changed|drugbank}} | ||
| | DrugBank = DB00682 | | DrugBank = DB00682 | ||
| | DrugBank2 = DBSALT000278 | |||
| | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | | ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | ||
| | ChemSpiderID = 10442445 | | ChemSpiderID = 10442445 | ||
| | ChemSpiderID2 = 17333193 | |||
| | UNII_Ref = {{fdacite|correct|FDA}} | | UNII_Ref = {{fdacite|correct|FDA}} | ||
| | UNII = 5Q7ZVV76EI | | UNII = 5Q7ZVV76EI | ||
| | UNII2 = 6153CWM0CL | |||
| | KEGG_Ref = {{keggcite|correct|kegg}} | | KEGG_Ref = {{keggcite|correct|kegg}} | ||
| | KEGG = D08682 | | KEGG = D08682 | ||
| | KEGG2 = D00564 | |||
| | ChEBI_Ref = {{ebicite|changed|EBI}} | |||
| | ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| | ChEBI = 10033 | | ChEBI = 10033 | ||
| | ChEBI2 = 10034 | |||
| | ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| | ChEMBL_Ref = {{ebicite|changed|EBI}} | |||
| | ChEMBL = 1464 | | ChEMBL = 1464 | ||
| | ChEMBL2 = 1200879 | |||
| | NIAID_ChemDB = | |||
| | PDB_ligand = RWF | |||
| | PDB_ligand2 = SWF<!-- this is broken; PDB is R,S enantiomer but that won’t fit into chembox --> | |||
| | synonyms = | |||
| <!--Chemical data--> | <!-- Chemical and physical data --> | ||
| | IUPAC_name = (''RS'')-4-Hydroxy-3-(3-oxo-1-phenylbutyl)- 2''H''-chromen-2-one | |||
| | C=19 | H=16 | O=4 | |||
| | C = 19 | |||
| | molecular_weight = 308.33 g/mol | |||
| | H = 16 | |||
| | smiles = CC(=O)CC(C\1=C(/O)c2ccccc2OC/1=O)c3ccccc3 | |||
| | O = 4 | |||
| | InChI = 1/C19H16O4/c1-12(20)11-15(13-7-3-2-4-8-13)17-18(21)14-9-5-6-10-16(14)23-19(17)22/h2-10,15,21H,11H2,1H3 | |||
| | SMILES = CC(=O)CC(C\1=C(/O)c2ccccc2OC/1=O)c3ccccc3 | |||
| | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | | StdInChI_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChI = 1S/C19H16O4/c1-12(20)11-15(13-7-3-2-4-8-13)17-18(21)14-9-5-6-10-16(14)23-19(17)22/h2-10,15,21H,11H2,1H3 | | StdInChI = 1S/C19H16O4/c1-12(20)11-15(13-7-3-2-4-8-13)17-18(21)14-9-5-6-10-16(14)23-19(17)22/h2-10,15,21H,11H2,1H3 | ||
| | StdInChI_comment = | |||
| | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | | StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | ||
| | StdInChIKey = PJVWKTKQMONHTI-UHFFFAOYSA-N | | StdInChIKey = PJVWKTKQMONHTI-UHFFFAOYSA-N | ||
| | density = | |||
| | density_notes = | |||
| | melting_point = | |||
| | melting_high = | |||
| | melting_notes = | |||
| | boiling_point = | |||
| | boiling_notes = | |||
| | solubility = | |||
| | sol_units = | |||
| | specific_rotation = | |||
| }} | }} | ||
| '''Warfarin''' (also known under the ] names '''Coumadin''', '''Jantoven''', '''Marevan''', '''Lawarin''', '''Waran''', and '''Warfant''') is an ]. It is most likely to be the drug popularly referred to as a "blood thinner," yet this is a misnomer, since it does not affect the thickness or viscosity of blood. Instead, it acts on the liver to decrease the quantity of a few key proteins in blood that allow blood to clot. | |||
| <!-- Definition and medical uses --> | |||
| It was initially marketed as a ] against ]s and ] and is still popular for this purpose, although more potent poisons such as ] have since been developed. A few years after its introduction, warfarin was found to be effective and relatively safe for ] ] and ] (abnormal formation and migration of blood clots) in many disorders. It was approved for use as a medication in the early 1950s and has remained popular ever since; warfarin is the most widely prescribed oral anticoagulant drug in North America.<ref name=Holbrook/> | |||
| '''Warfarin''', sold under the brand name '''Coumadin''' among others, is an ] ].<ref name="AHFS2017" /> While the drug is described as a "blood thinner", it does not reduce viscosity but rather prevents blood clots (]) from forming (]). Accordingly, it is commonly used to prevent ] and ], and to protect against ] in people who have ], ], or ].<ref name=AHFS2017 /> Warfarin may sometimes be prescribed following ] (STEMI) and ].<ref name=AHFS2017 /> It is usually taken by mouth, but may also be administered ]ly.<ref name=AHFS2017>{{cite web |title = Warfarin sodium |url = https://www.drugs.com/monograph/warfarin-sodium.html |publisher = The American Society of Health-System Pharmacists |date = 13 October 2022 |access-date = 16 February 2023 |archive-date = 12 June 2018 |archive-url = https://web.archive.org/web/20180612143838/https://www.drugs.com/monograph/warfarin-sodium.html |url-status = live }}</ref> It is a vitamin K antagonist.<ref name="Coumadin FDA label" /> | |||
| <!-- Side effects --> | |||
| Despite its effectiveness, treatment with warfarin has several shortcomings. Many commonly used medications ] with warfarin, as do some foods (particularly fresh plant-based foods containing ]), and its activity has to be monitored by ]ing for the ] (INR) to ensure an adequate yet safe dose is taken.<ref name=Ansell2004>{{cite journal |author=Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E |title=The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy |journal=Chest |volume=126 |issue=3 Suppl |pages=204S–233S |year=2004 |pmid=15383473 |doi=10.1378/chest.126.3_suppl.204S|url=http://www.chestjournal.org/cgi/content/full/126/3_suppl/204S}} ()</ref> | |||
| The common ], a natural consequence of reduced clotting, is ].<ref name=AHFS2017 /> Less common side effects may include areas of ], and ].<ref name=AHFS2017 /> Use is not recommended during ].<ref name=AHFS2017 /> The effects of warfarin are typically monitored by checking ] (INR) every one to four weeks.<ref name=AHFS2017 /> Many other medications and ] can interact with warfarin, either increasing or decreasing its effectiveness.<ref name=AHFS2017 /><ref name=Ag2012>{{cite journal | vauthors = Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G | title = Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines | journal = Chest | volume = 141 | issue = 2 Suppl | pages = e44S–e88S | date = February 2012 | pmid = 22315269 | pmc = 3278051 | doi = 10.1378/chest.11-2292 }}</ref> The effects of warfarin may be reversed with ] (vitamin K<sub>1</sub>), ], or ].<ref name=Ag2012 /> | |||
| <!-- Mechanism --> | |||
| Warfarin and related ]-containing molecules decrease blood ] by inhibiting ], an ] that recycles ] vitamin K to its reduced form after it has participated in the ] of several blood coagulation proteins, mainly ] and ]. For this reason, drugs in this class are also referred to as ].<ref name=Ansell2004/> When administered, these drugs do not anticoagulate blood immediately. Instead, onset of their effect requires about a day before clotting factors being normally made by the liver have time to naturally disappear in metabolism, and the duration of action of a single dose of racemic warfarin is 2 to 5 days. Under normal pharmacological therapy the drugs are administered to decrease the action of the clotting factors they affect by 30 to 50%.<ref></ref> | |||
| Warfarin decreases blood clotting by blocking ], an ] that reactivates ].<ref name=Ag2012 /> Without sufficient active vitamin K<sub>1</sub>, the plasma concentrations of ] II, VII, IX, and X are reduced and thus have decreased clotting ability.<ref name=Ag2012 /> The anticlotting ] and ] are also inhibited, but to a lesser degree.<ref name=Ag2012 /> | |||
| Despite being labeled a vitamin K antagonist, warfarin does not antagonize the action of vitamin K1, but rather antagonizes vitamin K1 recycling, depleting active vitamin K1. | |||
| A few days are required for full effect to occur, and these effects can last for up to five days.<ref name=AHFS2017 /><ref>{{cite book | vauthors = Arcangelo VP, Peterson AM |title = Pharmacotherapeutics for Advanced Practice: A Practical Approach |date = 2006 |publisher = Lippincott Williams & Wilkins |isbn = 978-0-7817-5784-3 |page = 774 |url = https://books.google.com/books?id=EaP1yJz4fkEC&pg=PA774 |url-status = live |archive-url = https://web.archive.org/web/20170918185711/https://books.google.com/books?id=EaP1yJz4fkEC&pg=PA774 |archive-date = 18 September 2017 }}</ref> Because the mechanism involves enzymes such as '']'', patients on warfarin with ] may require adjustments in therapy if the genetic variant that they have is more readily inhibited by warfarin, thus requiring lower doses.<ref>{{cite book | vauthors = Dasgupta A, Wahed A | chapter = Pharmacogenomics | title = Clinical Chemistry, Immunology and Laboratory Quality Control |date=2014 |pages=353–362 |doi=10.1016/B978-0-12-407821-5.00020-6| isbn = 978-0-12-407821-5 }}</ref> | |||
| <!-- History and culture --> | |||
| Warfarin is a synthetic derivative of ], a 4-hydroxycoumarin-derived ] anticoagulant originally discovered in spoiled ]-based animal feeds. ], in turn, is derived from ], a sweet-smelling but coagulation-inactive chemical found naturally in "sweet" clover (to which it gives its odor and name) and many other plants. The name ''warfarin'' stems from its discovery at the ], incorporating the acronym for the organization which funded the key research (''WARF'', for '']'') and the ending ''-arin,'' indicating its link with coumarin. | |||
| Warfarin first came into large-scale commercial use in 1948 as a ].<ref>{{cite book | vauthors = Ravina E |title = The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs |date = 2011 |publisher = John Wiley & Sons |isbn = 978-3-527-32669-3 |page = 148 |url = https://books.google.com/books?id=iDNy0XxGqT8C&pg=PA148 |url-status = live |archive-url = https://web.archive.org/web/20170918185711/https://books.google.com/books?id=iDNy0XxGqT8C&pg=PA148 |archive-date = 18 September 2017 }}</ref><ref name=poison/> It was formally approved as a medication to treat blood clots in humans by the U.S. ] in 1954.<ref name=AHFS2017 /> In 1955, warfarin's reputation as a safe and acceptable treatment for ], ], and ] was bolstered when President ] was treated with warfarin following a highly publicized heart attack.<ref>{{cite journal | vauthors = Lim GB | title = Milestone 2: Warfarin: from rat poison to clinical use | journal = Nature Reviews. Cardiology | date = December 2017 | pmid = 29238065 | doi = 10.1038/nrcardio.2017.172 | doi-access = free | title-link=doi }}</ref> It is on the ].<ref name="WHO23rd">{{cite book | vauthors = ((World Health Organization)) | title = The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023) | year = 2023 | hdl = 10665/371090 | author-link = World Health Organization | publisher = World Health Organization | location = Geneva | id = WHO/MHP/HPS/EML/2023.02 | hdl-access=free }}</ref> Warfarin is available as a ]<ref name=BNF69>{{cite book |title = British national formulary |date = 2015 |publisher = British Medical Association |isbn = 978-0-85711-156-2 |pages = 154–155 |edition = 69 }}</ref> and is sold under many brand names.<ref name=brands/> In 2022, it was the 85th most commonly prescribed medication in the United States, with more than 8{{nbsp}}million prescriptions.<ref>{{cite web | title=The Top 300 of 2022 | url=https://clincalc.com/DrugStats/Top300Drugs.aspx | website=ClinCalc | access-date=30 August 2024 | archive-date=30 August 2024 | archive-url=https://web.archive.org/web/20240830202410/https://clincalc.com/DrugStats/Top300Drugs.aspx | url-status=live }}</ref><ref>{{cite web | title = Warfarin Drug Usage Statistics, United States, 2013 - 2022 | website = ClinCalc | url = https://clincalc.com/DrugStats/Drugs/Warfarin | access-date = 30 August 2024 | archive-date = 13 April 2020 | archive-url = https://web.archive.org/web/20200413034226/https://clincalc.com/DrugStats/Drugs/Warfarin | url-status = live }}</ref> | |||
| {{TOC limit|3}} | |||
| {{TOC limit}} | |||
| ==Medical uses== | |||
| == Medical uses == | |||
| Warfarin is used to decrease the tendency for ] or as secondary prophylaxis (prevention of further episodes) in those individuals that have already formed a blood clot (]). Warfarin treatment can help prevent formation of future blood clots and help reduce the risk of ] (migration of a thrombus to a spot where it blocks blood supply to a vital organ).<ref name=AHFS>{{cite web|title=coumadin|url=http://www.drugs.com/monograph/coumadin.html|work=The American Society of Health-System Pharmacists|accessdate=3 April 2011}}</ref> | |||
| Warfarin is ] for the prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism;<ref name="Coumadin FDA label" /> prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation and/or cardiac valve replacement;<ref name="Coumadin FDA label" /> and reduction in the risk of death, recurrent myocardial infarction, and thromboembolic events such as stroke or systemic embolization after myocardial infarction.<ref name="Coumadin FDA label" /> | |||
| Warfarin is used to decrease the tendency for ], or as secondary ] (prevention of further episodes) in those individuals who have already formed a blood clot (]). Warfarin treatment can help prevent formation of future blood clots and help reduce the risk of ] (migration of a thrombus to a spot where it blocks ] to a ]).<ref name=AHFS>{{cite web |title = Coumadin |url = https://www.drugs.com/monograph/coumadin.html |publisher = The American Society of Health-System Pharmacists |access-date = 3 April 2011 |url-status = live |archive-url = https://web.archive.org/web/20110203081242/http://www.drugs.com/monograph/coumadin.html |archive-date = 3 February 2011 }}</ref><ref>{{cite book | vauthors = Sanders GD, Lowenstern A, Borre E, Chatterjee R, Goode A, Sharan L, Lapointe NA, Raitz G, Shah B, Yapa R, Davis JK |title=Stroke Prevention in Patients With Atrial Fibrillation: A Systematic Review Update |series=AHRQ Comparative Effectiveness Reviews |date=2018 |publisher=Agency for Healthcare Research and Quality (US) |url=https://www.ncbi.nlm.nih.gov/books/NBK534141/ |pmid=30480925 }}</ref> | |||
| The type of anticoagulation (clot formation inhibition) for which warfarin is best suited, is that in areas of slowly-running blood, such as in veins and the pooled blood behind artificial and natural valves, and pooled in dysfunctional cardiac atria. Thus, common clinical indications for warfarin use are ], the presence of ]s, ], and ] (where the embolized clots first form in veins). Warfarin is also used in ]. It has been used occasionally after heart attacks (]s), but is far less effective at preventing new thromboses in coronary arteries. Prevention of clotting in arteries is usually undertaken with ]s, which act by a different mechanism from warfarin (which normally has no effect on platelet function).<ref name=Hirsh>{{cite journal |author=Hirsh J, ], Ansell J, ] |title=American Heart Association/American College of Cardiology Foundation guide to warfarin therapy |journal=J. Am. Coll. Cardiol. |volume=41 |issue=9 |pages=1633–52 |year=2003 |pmid=12742309 |url=http://content.onlinejacc.org/cgi/content/full/41/9/1633| doi=10.1016/S0735-1097(03)00416-9}}</ref> | |||
| Warfarin is best suited for anticoagulation (clot formation inhibition) in areas of slowly running blood (such as in veins and the pooled blood behind artificial and natural valves), and in blood pooled in dysfunctional ]. Thus, common clinical indications for warfarin use are ], the presence of ]s, ], and ] (where the embolized clots first form in veins). Warfarin is also used in ]. It has been used occasionally after heart attacks (]s), but is far less effective at preventing new thromboses in ]. Prevention of clotting in arteries is usually undertaken with ]s, which act by a different mechanism from warfarin (which normally has no effect on platelet function).<ref name="Hirsh_2003">{{cite journal | vauthors = Hirsh J, Fuster V, Ansell J, Halperin JL | title = American Heart Association/American College of Cardiology Foundation guide to warfarin therapy | journal = Journal of the American College of Cardiology | volume = 41 | issue = 9 | pages = 1633–1652 | date = May 2003 | pmid = 12742309 | doi = 10.1016/S0735-1097(03)00416-9 | author-link2 = Valentín Fuster | doi-access = free | title-link=doi | author-link4 = Jonathan L. Halperin }}</ref> It can be used to treat people following ]s due to ], though ]s (DOACs) may offer greater benefits.<ref>{{cite journal | vauthors = Kim IS, Kim HJ, Kim TH, Uhm JS, Joung B, Lee MH, Pak HN | title = Appropriate doses of non-vitamin K antagonist oral anticoagulants in high-risk subgroups with atrial fibrillation: Systematic review and meta-analysis | journal = Journal of Cardiology | volume = 72 | issue = 4 | pages = 284–291 | date = October 2018 | pmid = 29706404 | doi = 10.1016/j.jjcc.2018.03.009 | doi-access = free | title-link=doi }}</ref> | |||
| In some countries, other coumarins are used instead of warfarin, such as ] and ]. These have a shorter (acenocoumarol) or longer (phenprocoumon) ], and are not completely interchangeable with warfarin. The oral anticoagulant ] (trade name Exanta) was expected to replace warfarin to a large degree when introduced; however, reports of ] (liver damage) prompted its manufacturer to withdraw it from further development. Other drugs offering the efficacy of warfarin without a need for monitoring, such as ] and ], are under development.<ref>{{cite journal |author=Hirsh J, O'Donnell M, Eikelboom JW |title=Beyond unfractionated heparin and warfarin: current and future advances |journal=Circulation |volume=116 |issue=5 |pages=552–60 |year=2007 |month=July |pmid=17664384 |doi=10.1161/CIRCULATIONAHA.106.685974 |url=http://circ.ahajournals.org/cgi/content/full/116/5/552}}</ref> | |||
| ===Dosing=== | === Dosing === | ||
| Dosing of warfarin is complicated |
Dosing of warfarin is complicated because it is known to interact with many commonly used medications and ].<ref name=Holbrook2005>{{cite journal | vauthors = Holbrook AM, Pereira JA, Labiris R, McDonald H, Douketis JD, Crowther M, Wells PS | title = Systematic overview of warfarin and its drug and food interactions | journal = Archives of Internal Medicine | volume = 165 | issue = 10 | pages = 1095–1106 | date = May 2005 | pmid = 15911722 | doi = 10.1001/archinte.165.10.1095 | doi-access = | title-link=doi }}</ref> These interactions may enhance or reduce warfarin's anticoagulation effect. To optimize the therapeutic effect without risking dangerous ]s such as bleeding, close monitoring of the degree of anticoagulation is required by a ] measuring an ] (INR). During the initial stage of treatment, INR is checked daily; intervals between tests can be lengthened if the patient manages stable therapeutic INR levels on an unchanged warfarin dose.<ref name="Hirsh_2003" /> Newer ] is available and has increased the ease of INR testing in the outpatient setting. Instead of a ], the point-of-care test involves a simple finger prick.<ref name="Perry 2010">{{cite journal | vauthors = Perry DJ, Fitzmaurice DA, Kitchen S, Mackie IJ, Mallett S | title = Point-of-care testing in haemostasis | journal = British Journal of Haematology | volume = 150 | issue = 5 | pages = 501–514 | date = September 2010 | pmid = 20618331 | doi = 10.1111/j.1365-2141.2010.08223.x | s2cid = 32069018 | doi-access = free }}</ref> | ||
| ==== Maintenance dose ==== | |||
| When initiating warfarin therapy ("warfarinization"), the doctor will decide how strong the anticoagulant therapy needs to be. The target INR level will vary from case to case depending on the clinical indicators, but tends to be 2–3 in most conditions. In particular, target INR may be 2.5–3.5 (or even 3.0–4.5) in patients with one or more ]s.<ref>{{cite journal |author=Baglin TP, Keeling DM, Watson HG |title=Guidelines on oral anticoagulation (warfarin): third edition—2005 update |journal=Br. J. Haematol. |volume=132 |issue=3 |pages=277–85 |year=2006 |month=February |pmid=16409292 |doi=10.1111/j.1365-2141.2005.05856.x |url=http://www.blackwell-synergy.com/doi/pdf/10.1111/j.1365-2141.2006.06379.x}}</ref> | |||
| ]-warfarin interaction effect: When warfarin levels are high, people have more risk of bleeding. Conversely, lower levels of warfarin lead to increased risk of blood clots. A narrow range exists where the benefits of warfarin are greater than the risks, its ]. Certain drugs, herbal medicines, and foods can interact with warfarin, increasing or decreasing a previously stable warfarin level.<ref>{{cite web | work = U.S. National Institutes of Health |title = important information to know when you are taking : Coumadine and vitamine K |url = http://ods.od.nih.gov/pubs/factsheets/coumadin1.pdf |access-date = 27 March 2014 |url-status = dead |archive-url = https://web.archive.org/web/20131020203725/http://ods.od.nih.gov/pubs/factsheets/coumadin1.pdf |archive-date = 20 October 2013 }}</ref>]] | |||
| Recommendations by many national bodies, including the ],<ref name=Holbrook2012>{{cite journal | vauthors = Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, Svensson PJ, Veenstra DL, Crowther M, Guyatt GH | title = Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines | journal = Chest | volume = 141 | issue = 2 Suppl | pages = e152S–e184S | date = February 2012 | pmid = 22315259 | pmc = 3278055 | doi = 10.1378/chest.11-2295 }}</ref> have been distilled to help manage dose adjustments.<ref name="pmid15926414">{{cite journal | vauthors = Ebell MH | title = Evidence-based adjustment of warfarin (Coumadin) doses | journal = American Family Physician | volume = 71 | issue = 10 | pages = 1979–1982 | date = May 2005 | pmid = 15926414 | url = https://www.aafp.org/afp/2005/0515/p1979.html | url-status = live | archive-url = https://web.archive.org/web/20180201075216/https://www.aafp.org/afp/2005/0515/p1979.html | archive-date = 1 February 2018 }}</ref> | |||
| The ] of warfarin can fluctuate significantly depending on the amount of vitamin K<sub>1</sub> in the diet. Keeping vitamin K<sub>1</sub> intake at a stable level can prevent these fluctuations. ]s tend to contain higher amounts of vitamin K<sub>1</sub>. Green parts of members of the family ], such as ], ], and ] are extremely rich sources of vitamin K; ] such as ] and ], as well as the darker varieties of ]s and other ]s, are also relatively high in vitamin K<sub>1</sub>. Green vegetables such as ] and ] do not have such high amounts of vitamin K<sub>1</sub> as leafy greens. Certain ]s have high amounts of vitamin K<sub>1</sub>. Foods low in vitamin K<sub>1</sub> include roots, bulbs, tubers, and most fruits and fruit juices. Cereals, grains, and other milled products are also low in vitamin K<sub>1</sub>.<ref>{{cite web |url = https://www.mayoclinic.org/diseases-conditions/thrombophlebitis/expert-answers/warfarin/faq-20058443 |title = Warfarin diet: What foods should I avoid? |publisher = Mayo Foundation |access-date = 9 August 2011 |url-status = live |archive-url = https://web.archive.org/web/20110824075323/http://www.mayoclinic.com/health/warfarin/AN00455 |archive-date = 24 August 2011 }}</ref> | |||
| ====Loading dose==== | |||
| Several researchers have proposed algorithms for commencing warfarin treatment: | |||
| * The Kovacs 10 mg algorithm was better than a 5 mg algorithm.<ref name="pmid12729425">{{cite journal |author=Kovacs MJ, Rodger M, Anderson DR, ''et al.'' |title=Comparison of 10-mg and 5-mg warfarin initiation nomograms together with low-molecular-weight heparin for outpatient treatment of acute venous thromboembolism. A randomized, double-blind, controlled trial |journal=Ann. Intern. Med. |volume=138 |issue=9 |pages=714–9 |year=2003 |pmid=12729425 |doi=|url=http://annals.org/cgi/content/full/138/9/714}} ()</ref> | |||
| * The Fennerty 10 mg regimen is for urgent anticoagulation<ref name="pmid3144365">{{cite journal |author=Fennerty A, Campbell IA, Routledge PA |title=Anticoagulants in venous thromboembolism |journal=BMJ |volume=297 |issue=6659 |pages=1285–8 |year=1988 |pmid=3144365 |doi=10.1136/bmj.297.6659.1285 |pmc=1834928}} {{PMC|1834928}}</ref> | |||
| * The Tait 5 mg regimen is for "routine" (low-risk) anticoagulation<ref name="pmid9633885">{{cite journal |author=Tait RC, Sefcick A |title=A warfarin induction regimen for out-patient anticoagulation in patients with atrial fibrillation |journal=Br. J. Haematol. |volume=101 |issue=3 |pages=450–4 |year=1998 |pmid=9633885 |doi=10.1046/j.1365-2141.1998.00716.x}} </ref> | |||
| * Lenzini ''et al.'' derived and prospectively validated a model including ''CYP2C9'' and ''VKORC1'' genotypes. This model could predict 70% of the variation in warfarin doses in a validation cohort (versus 48% without genotype). The pharmacogenetic protocol lead to a reduction in out of range INR values as compared to a historic control.<ref>{{cite journal |author=Lenzini PA, Grice GR, Milligan PE, ''et al.'' |title=Laboratory and clinical outcomes of pharmacogenetic vs. clinical protocols for warfarin initiation in orthopedic patients|journal= Journal of Thrombosis and Haemostasis|volume=6 |pages=1–8 |year=2008 |doi=10.1111/j.1538-7836.2008.03095x |doi_brokendate=2010-03-20}} .</ref> | |||
| * www.WarfarinDosing.org is a non-profit website programmed with dosing calculators and other decision support tools for clinicians' use when initiating warfarin therapy.<ref>.</ref> | |||
| Several studies reported that the maintenance dose can be predicted based on various clinical data.<ref>{{cite journal | vauthors = Hu YH, Wu F, Lo CL, Tai CT | title = Predicting warfarin dosage from clinical data: a supervised learning approach | journal = Artificial Intelligence in Medicine | volume = 56 | issue = 1 | pages = 27–34 | date = September 2012 | pmid = 22537823 | doi = 10.1016/j.artmed.2012.04.001 }}</ref><ref>{{cite journal | vauthors = Solomon I, Maharshak N, Chechik G, Leibovici L, Lubetsky A, Halkin H, Ezra D, Ash N | title = Applying an artificial neural network to warfarin maintenance dose prediction | journal = The Israel Medical Association Journal | volume = 6 | issue = 12 | pages = 732–735 | date = December 2004 | pmid = 15609884 }}</ref> | |||
| ====Maintenance dose==== | |||
| Recommendations by many national bodies including the ]<ref name="Ansell2004"/> have been distilled to help manage dose adjustments.<ref>{{cite web |url=http://www.aafp.org/afp/20050515/pocform.html |title=Point-of-Care Guides: May 15, 2005. American Family Physician |accessdate=20 August 2007 |work= |archiveurl = http://web.archive.org/web/20070929083239/http://www.aafp.org/afp/20050515/pocform.html |archivedate = 29 September 2007}}</ref> | |||
| ==== Self-testing ==== | |||
| The maintenance dose of warfarin can fluctuate significantly depending on the amount of vitamin K in the diet. Keeping vitamin K intake at a stable level can prevent these fluctuations. Leafy green vegetables tend to contain higher amounts of vitamin K and typically green vegetables, cabbages, and lettuces are high in vitamin K. Certain vegetable oils have high amounts of vitamin K. Foods that are low in vitamin K include roots, bulbs, tubers, some fruits and fruit juices. Cereals, grains and other milled products are also low in vitamin K. <ref>{{cite web|url=http://www.mayoclinic.com/health/warfarin/AN00455|title=Warfarin diet: What foods should I avoid?|publisher=Mayoclinic.com|accessdate=2011-08-09}}</ref> | |||
| ====Self-testing==== | |||
| {{Main|INR self-monitoring}} | {{Main|INR self-monitoring}} | ||
| ] | |||
| Patients are making increasing use of self-testing and home monitoring of oral anticoagulation. International guidelines on home testing were published in 2005.<ref name="Ansell2005">{{cite journal |author=Ansell J, Jacobson A, Levy J, Völler H, Hasenkam JM |title=Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation |journal=Int. J. Cardiol. |volume=99 |issue=1 |pages=37–45 |year=2005 |month=March |pmid=15721497 |doi=10.1016/j.ijcard.2003.11.008|url = http://patientselftesting.com/uploads/Int_Cardio_Journal_-_Patient_Self_Management.pdf}}</ref> The guidelines stated: "The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently available self-testing/self-management devices give INR results which are comparable with those obtained in laboratory testing."<ref name=Ansell2005/> A 2006 ] and ] of 14 randomized trials showed that home testing led to a reduced incidence of complications (thrombosis and major bleeding) and improved the time in the therapeutic range.<ref>{{cite journal |author=Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P |title=Self-monitoring of oral anticoagulation: a systematic review and meta-analysis |journal=Lancet |volume=367 |issue=9508 |pages=404–11 |year=2006 |month=February |pmid=16458764 |doi=10.1016/S0140-6736(06)68139-7|url = http://www.hadassah.org.il/NR/rdonlyres/7DD940DC-E6B5-43FA-8869-288CAE8FF831/7797/Selfmonitoringoforalanticoagulationasystematicrevi.pdf}}</ref> | |||
| Anticoagulation with warfarin can also be monitored by patients at home. International guidelines on home testing were published in 2005.<ref name="Ansell2005">{{cite journal | vauthors = Ansell J, Jacobson A, Levy J, Völler H, Hasenkam JM | title = Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation | journal = International Journal of Cardiology | volume = 99 | issue = 1 | pages = 37–45 | date = March 2005 | pmid = 15721497 | doi = 10.1016/j.ijcard.2003.11.008 | url = http://patientselftesting.com/uploads/Int_Cardio_Journal_-_Patient_Self_Management.pdf | url-status = dead | archive-url = https://web.archive.org/web/20160303221536/http://patientselftesting.com/uploads/Int_Cardio_Journal_-_Patient_Self_Management.pdf | archive-date = 3 March 2016 }}</ref> The guidelines stated:<ref name="Ansell2005" /> | |||
| {{blockquote|The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently available self-testing/self-management devices give INR results that are comparable with those obtained in laboratory testing.}} | |||
| ==Contraindications== | |||
| ===Pregnancy=== | |||
| {{further|]}} | |||
| Warfarin is ] in pregnancy, as it passes through the ]l barrier and may cause bleeding in the fetus; warfarin use during pregnancy is commonly associated with ], ], ], and ].<ref name=HDT>{{cite book |author=Macina, Orest T.; Schardein, James L. |title=Human Developmental Toxicants |publisher=CRC Taylor & Francis |chapter=Warfarin |location=Boca Raton |year=2007 |pages=193–4 |isbn=0-8493-7229-1 |url=http://books.google.com/?id=8_Lc58cGZj0C}} Retrieved on 15 December 2008 through ].</ref> Coumarins (such as warfarin) are also ]s, that is, they cause ]s; the incidence of birth defects in infants exposed to warfarin '']'' appears to be around 5%, although higher figures (up to 30%) have been reported in some studies.<ref name=Loftus>{{cite book |author=Loftus, Christopher M. |title=Neurosurgical Aspects of Pregnancy |chapter=Fetal toxicity of common neurosurgical drugs |publisher=American Association of Neurological Surgeons |location=Park Ridge, Ill |year=1995 |pages=11–3 |isbn=1-879284-36-7 |url=http://books.google.com/?id=X58R5BqtHmEC}}</ref> Depending on when exposure occurs during pregnancy, two distinct combinations of congenital abnormalities can arise.<ref name=HDT/> | |||
| A 2006 ] and ] of 14 ]s showed home testing led to a reduced incidence of complications (] and ]), and improved the time in the ].<ref>{{cite journal | vauthors = Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P | title = Self-monitoring of oral anticoagulation: a systematic review and meta-analysis | journal = Lancet | volume = 367 | issue = 9508 | pages = 404–411 | date = February 2006 | pmid = 16458764 | doi = 10.1016/S0140-6736(06)68139-7 | url = http://www.hadassah.org.il/NR/rdonlyres/7DD940DC-E6B5-43FA-8869-288CAE8FF831/7797/Selfmonitoringoforalanticoagulationasystematicrevi.pdf | url-status = dead | s2cid = 1494933 | archive-url = https://web.archive.org/web/20120319160502/http://www.hadassah.org.il/NR/rdonlyres/7DD940DC-E6B5-43FA-8869-288CAE8FF831/7797/Selfmonitoringoforalanticoagulationasystematicrevi.pdf | archive-date = 19 March 2012 }}</ref> | |||
| When warfarin (or another 4-hydroxycoumarin derivative) is given during the first trimester—particularly between the sixth and ninth weeks of pregnancy—a constellation of birth defects known variously as ] (FWS), ''warfarin embryopathy'', or ''coumarin embryopathy'' can occur. FWS is characterized mainly by ] abnormalities, which include nasal hypoplasia, a depressed or narrowed nasal bridge, ], and ]s in the ], ], and ] which show a peculiar stippled appearance on ]. ], such as ] (unusually short fingers and toes) or underdeveloped extremities, can also occur.<ref name=HDT/><ref name=Loftus/> Common non-skeletal features of FWS include ] and ].<ref name=HDT/><ref name=Loftus/> | |||
| === Alternative anticoagulants === | |||
| Warfarin administration in the second and third trimesters is much less commonly associated with birth defects, and when they do occur, are considerably different from fetal warfarin syndrome. The most common congenital abnormalities associated with warfarin use in late pregnancy are ] disorders, including ] and ]s, and eye defects.<ref name=HDT/><ref name=Loftus/> Because of such later pregnancy birth defects, anticoagulation with warfarin poses a problem in pregnant women requiring warfarin for vital indications, such as stroke prevention in those with ]s. | |||
| In some countries, other ]s are used instead of warfarin, such as ] and ]. These have a shorter (acenocoumarol) or longer (phenprocoumon) ], and are not completely interchangeable with warfarin. Several types of anticoagulant drugs offering the efficacy of warfarin without a need for monitoring, such as ], ], ], and ], have been approved in a number of countries for classical warfarin uses. Complementing these drugs are ]s available for dabigatran (]), and for apixaban, and rivaroxaban (]).<ref>{{cite journal | vauthors = Cuker A, Burnett A, Triller D, Crowther M, Ansell J, Van Cott EM, Wirth D, Kaatz S | title = Reversal of direct oral anticoagulants: Guidance from the Anticoagulation Forum | journal = American Journal of Hematology | volume = 94 | issue = 6 | pages = 697–709 | date = June 2019 | pmid = 30916798 | doi = 10.1002/ajh.25475 | doi-access = free | title-link=doi }}</ref> Andexanet alfa is suggested for edoxaban, but use of it is considered off label due to limited evidence. A reversal agent for dabigatran, apixaban, edoxaban, and rivaroxaban is in development (]).<ref>{{cite journal | vauthors = Levy JH, Ageno W, Chan NC, Crowther M, Verhamme P, Weitz JI | title = When and how to use antidotes for the reversal of direct oral anticoagulants: guidance from the SSC of the ISTH | journal = Journal of Thrombosis and Haemostasis | volume = 14 | issue = 3 | pages = 623–627 | date = March 2016 | pmid = 26911798 | doi = 10.1111/jth.13227 | doi-access = | title-link=doi | s2cid = 27269191 }}</ref><!-- An initial failure was ] (trade name Exanta), however, reports of ] (liver damage) prompted its manufacturer to withdraw it from further development. A similar and later drug dabigatran has since been more successful --> | |||
| == Contraindications == | |||
| Usually, warfarin is avoided in the first trimester, and a ] such as ] is substituted. With heparin, risk of maternal hemorrhage and other complications is still increased, but heparins do not cross the placental barrier and therefore do not cause birth defects.<ref name=Loftus/> Various solutions exist for the time around delivery. | |||
| All anticoagulants are generally contraindicated in situations in which the reduction in clotting that they cause might lead to serious and potentially life-threatening bleeds. This includes people with active bleeding conditions (such as ]s), or disease states with increased risk of bleeding (e.g., low platelets, severe liver disease, uncontrolled hypertension). For patients undergoing surgery, treatment with anticoagulants is generally suspended. Similarly, spinal and ] (e.g., spinal injections, ]s, etc.) carry increased risk, so treatment is suspended prior to these procedures.<ref name="martindale">Brayfield A (ed), Martindale: The Complete Drug Reference London: Pharmaceutical Press </ref><ref name=FDA2015>{{cite web |title = Coumadin |url = https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/009218s115lbl.pdf |website = U.S. ] (FDA) |access-date = 24 April 2017 |date = October 2015 |url-status = live |archive-url = https://web.archive.org/web/20170623024610/https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/009218s115lbl.pdf |archive-date = 23 June 2017 }}</ref> | |||
| Warfarin should not be given to people with ] until ] has improved or normalised.<ref name="martindale" /> Warfarin is usually best avoided in people with protein C or protein S deficiency, as these ] conditions increase the risk of skin ], which is a rare but serious side effect associated with warfarin.<ref name="rapini">{{cite book | vauthors = Bolognia JL, Jorizzo JL, Rapini RP |title = Dermatology |url = https://archive.org/details/dermatologyvolum00mdje |url-access = limited |date = 2008 |publisher = Mosby/Elsevier |location = St. Louis, Mo. |isbn = 978-1-4160-2999-1 |pages = , 340 |edition = 2nd }}</ref> | |||
| ==Adverse effects== | |||
| ===Hemorrhage=== | |||
| The only common ] of warfarin is ] (bleeding). The risk of severe bleeding is small but definite (a median annual rate of 0.9 to 2.7% has been reported<ref name=Horton>{{cite journal |author=Horton JD, Bushwick BM |title=Warfarin therapy: evolving strategies in anticoagulation |journal=Am Fam Physician |volume=59 |issue=3 |pages=635–46 |year=1999 |month=February |pmid=10029789 |url=http://www.aafp.org/afp/990201ap/635.html}}</ref>) and any benefit needs to outweigh this risk when warfarin is considered as a therapeutic measure. Risk of bleeding is augmented if the ] is out of range (due to accidental or deliberate overdose or due to interactions), and may cause ] (coughing up blood), excessive bruising, bleeding from nose or gums, or blood in ] or ]. | |||
| === Pregnancy === | |||
| The risks of bleeding is increased when warfarin is combined with ]s such as ], ], or other ]s.<ref name="pmid17698822">{{cite journal |author=Delaney JA, Opatrny L, Brophy JM, Suissa S |title=Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding |journal=CMAJ |volume=177 |issue=4 |pages=347–51 |year=2007 |pmid=17698822 |doi=10.1503/cmaj.070186|url=http://www.cmaj.ca/cgi/content/full/177/4/347 |pmc=1942107}} {{PMC|1942107}}</ref> The risk may also be increased in elderly patients<ref name="pmid17515465">{{cite journal |author=Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S |title=Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation |journal=Circulation |volume=115 |issue=21 |pages=2689–96 |year=2007 |pmid=17515465 |doi=10.1161/CIRCULATIONAHA.106.653048}}</ref> and in patients on ].<ref name="pmid17720522">{{cite journal |author=Elliott MJ, Zimmerman D, Holden RM |title=Warfarin anticoagulation in hemodialysis patients: a systematic review of bleeding rates |journal=Am. J. Kidney Dis. |volume=50 |issue=3 |pages=433–40 |year=2007 |pmid=17720522 |doi=10.1053/j.ajkd.2007.06.017}}</ref> | |||
| {{further|Fetal warfarin syndrome|Anticoagulation in pregnancy}} | |||
| Warfarin is ] in pregnancy, as it passes through the ]l barrier and may cause bleeding in the fetus; warfarin use during pregnancy is commonly associated with ], ], ], and ].<ref name=HDT>{{cite book |vauthors = Macina OT, Schardein JL |title = Human Developmental Toxicants |publisher = CRC Taylor & Francis |chapter = Warfarin |location = Boca Raton |year = 2007 |pages = 193–4 |isbn = 978-0-8493-7229-2 |chapter-url = https://books.google.com/books?id=8_Lc58cGZj0C |access-date = 26 August 2020 |archive-date = 5 March 2024 |archive-url = https://web.archive.org/web/20240305112952/https://books.google.com/books?id=8_Lc58cGZj0C |url-status = live }} Retrieved on 15 December 2008 through ].</ref> Coumarins (such as warfarin) are also ]s, that is, they cause ]s; the incidence of birth defects in infants exposed to warfarin '']'' appears to be around 5%, although higher figures (up to 30%) have been reported in some studies.<ref name=Loftus>{{cite book |vauthors = Loftus CM |title = Neurosurgical Aspects of Pregnancy |chapter = Fetal toxicity of common neurosurgical drugs |publisher = American Association of Neurological Surgeons |location = Park Ridge, Ill |year = 1995 |pages = 11–3 |isbn = 978-1-879284-36-4 |chapter-url = https://books.google.com/books?id=X58R5BqtHmEC |access-date = 26 August 2020 |archive-date = 5 March 2024 |archive-url = https://web.archive.org/web/20240305112942/https://books.google.com/books?id=X58R5BqtHmEC |url-status = live }}</ref> Depending on when exposure occurs during pregnancy, two distinct combinations of ] abnormalities can arise.<ref name=HDT /> | |||
| ==== First trimester of pregnancy ==== | |||
| ===Warfarin necrosis=== | |||
| Usually, warfarin is avoided in the ], and a ] such as ] is substituted. With heparin, risks of ] and other complications are still increased, but heparins do not cross the placental barrier, so do not cause birth defects.<ref name=Loftus /> Various solutions exist for the time around delivery. | |||
| {{Main|warfarin necrosis}} | |||
| A rare but serious complication resulting from treatment with warfarin is ], which occurs more frequently shortly after commencing treatment in patients with a deficiency of ]. Protein C is an innate anticoagulant that, like the procoagulant factors that warfarin inhibits, requires vitamin K-dependent carboxylation for its activity. Since warfarin initially decreases protein C levels faster than the coagulation factors, it can paradoxically increase the blood's tendency to coagulate when treatment is first begun (many patients when starting on warfarin are given ] in parallel to combat this), leading to massive thrombosis with skin ] and ] of limbs. Its natural counterpart, ], occurs in children who are ] for certain protein C mutations.<ref name="pmid10718793">{{cite journal |author=Chan YC, Valenti D, Mansfield AO, Stansby G |title=Warfarin induced skin necrosis |journal=Br J Surg |volume=87 |issue=3 |pages=266–72 |year=2000 |pmid=10718793 |doi=10.1046/j.1365-2168.2000.01352.x}}</ref> | |||
| Protein S deficiency can be affected in the same way as protein C deficiency is affected. | |||
| When warfarin (or another 4-hydroxycoumarin derivative) is given during the first trimester—particularly between the sixth and ninth weeks of pregnancy—a constellation of birth defects known variously as ] (FWS), warfarin embryopathy, or coumarin embryopathy can occur. FWS is characterized mainly by ] abnormalities, which include nasal ], a depressed or narrowed ], ], and ]s in the ], ], and ], which show a peculiar ]d appearance on ]. ], such as ] (unusually short fingers and toes) or underdeveloped extremities, can also occur.<ref name=HDT /><ref name=Loftus /> Common nonskeletal features of FWS include ] and ].<ref name=HDT /><ref name=Loftus /> | |||
| ===Osteoporosis=== | |||
| After initial reports that warfarin could reduce ], several studies have demonstrated a link between warfarin use and ]-related ]. A 1999 study in 572 women taking warfarin for deep venous thrombosis, risk of vertebral fracture and rib fracture was increased; other fracture types did not occur more commonly.<ref>{{cite journal |author=Caraballo PJ, Heit JA, Atkinson EJ, ''et al.'' |title=Long-term use of oral anticoagulants and the risk of fracture |journal=Arch. Intern. Med. |volume=159 |issue=15 |pages=1750–6 |year=1999 |pmid=10448778|doi=10.1001/archinte.159.15.1750}}</ref> A 2002 study looking at a randomly selected selection of 1523 patients with osteoporotic fracture found no increased exposure to anticoagulants compared to controls, and neither did stratification of the duration of anticoagulation reveal a trend towards fracture.<ref>{{cite journal |author=Pilon D, Castilloux AM, Dorais M, LeLorier J |title=Oral anticoagulants and the risk of osteoporotic fractures among elderly |journal=Pharmacoepidemiol Drug Saf |volume=13 |issue=5 |pages=289–94 |year=2004 |pmid=15133779 |doi=10.1002/pds.888}}</ref> | |||
| ==== Second trimester and later ==== | |||
| A 2006 retrospective study of 14,564 Medicare recipients showed that warfarin use for more than one year was linked with a 60% increased risk of osteoporosis-related fracture in men; there was no association in women. The mechanism was thought to be a combination of reduced intake of vitamin K, which is necessary for bone health, and inhibition by warfarin of vitamin K-mediated carboxylation of certain bone proteins, rendering them nonfunctional.<ref>{{cite journal |author=Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF |title=Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2 |journal=Arch. Intern. Med. |volume=166 |issue=2 |pages=241–6 |year=2006 |pmid=16432096 |doi=10.1001/archinte.166.2.241| url=http://archinte.ama-assn.org/cgi/content/full/166/2/241}}</ref> | |||
| Warfarin administration in the second and third trimesters is much less commonly associated with birth defects, and when they do occur, are considerably different from FWS. The most common congenital abnormalities associated with warfarin use in late pregnancy are ] disorders, including ] and ]s, and eye defects.<ref name=HDT /><ref name=Loftus /> Because of such later pregnancy birth defects, anticoagulation with warfarin poses a problem in pregnant women requiring warfarin for vital indications, such as stroke prevention in those with artificial heart valves. | |||
| Warfarin may be used in ] women who wish to breastfeed their infants.<ref name="Bates 2012">{{cite journal | vauthors = Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO | title = VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines | journal = Chest | volume = 141 | issue = 2 Suppl | pages = e691S–e736S | date = February 2012 | pmid = 22315276 | pmc = 3278054 | doi = 10.1378/chest.11-2300 }}</ref> Available data does not suggest that warfarin crosses into the breast milk. Similarly, INR levels should be checked to avoid adverse effects.<ref name="Bates 2012" /> | |||
| ===Purple toe syndrome=== | |||
| Another rare complication that may occur early during warfarin treatment (usually within 3 to 8 weeks of commencement) is '']''. This condition is thought to result from small deposits of ] breaking loose and flowing into the blood vessels in the skin of the feet, which causes a blueish purple color and may be painful. | |||
| == Adverse effects == | |||
| It is typically thought to affect the big toe, but it affects other parts of the feet as well, including the bottom of the foot (plantar surface). The occurrence of purple toe syndrome may require discontinuation of warfarin.<ref>{{cite journal |author=Talmadge DB, Spyropoulos AC |title=Purple toes syndrome associated with warfarin therapy in a patient with antiphospholipid syndrome |journal=Pharmacotherapy |volume=23 |issue=5 |pages=674–7 |year=2003 |pmid=12741443 |doi=10.1592/phco.23.5.674.32200}}</ref> | |||
| === |
=== Bleeding === | ||
| The only common side effect of warfarin is hemorrhage. The risk of severe bleeding is small but definite (a typical yearly rate of 1–3% has been reported),<ref name=Holbrook2012 /> and any benefit needs to outweigh this risk when warfarin is considered. All types of bleeding occur more commonly, but the most severe ones are those involving the brain (]/]) and the ].<ref name=Holbrook2012 /> Risk of bleeding is increased if the INR is out of range (due to accidental or deliberate overdose or due to interactions).<ref name=Garcia2010>{{cite journal | vauthors = Garcia D, Crowther MA, Ageno W | title = Practical management of coagulopathy associated with warfarin | journal = BMJ | volume = 340 | pages = c1813 | date = April 2010 | pmid = 20404060 | doi = 10.1136/bmj.c1813 | s2cid = 37076001 }}</ref> This risk increases greatly once the INR exceeds 4.5.<ref name=Brown2015>{{cite journal | vauthors = Brown DG, Wilkerson EC, Love WE | title = A review of traditional and novel oral anticoagulant and antiplatelet therapy for dermatologists and dermatologic surgeons | journal = Journal of the American Academy of Dermatology | volume = 72 | issue = 3 | pages = 524–534 | date = March 2015 | pmid = 25486915 | doi = 10.1016/j.jaad.2014.10.027 }}</ref> | |||
| Warfarin ]s with many commonly-used drugs, and the ] of warfarin varies greatly between patients. Some foods have also been reported to interact with warfarin.<ref name=Holbrook>{{cite journal |author=Holbrook AM, Pereira JA, Labiris R, ''et al.'' |title=Systematic overview of warfarin and its drug and food interactions |journal=Arch. Intern. Med. |volume=165 |issue=10 |pages=1095–106 |year=2005 |pmid=15911722 |doi=10.1001/archinte.165.10.1095 | url=http://archinte.ama-assn.org/cgi/content/full/165/10/1095}}</ref> Apart from the metabolic interactions, highly protein bound drugs can displace warfarin from ] and cause an increase in the INR.<ref>{{cite journal |author=Gage BF, Fihn SD, White RH |title=Management and dosing of warfarin therapy |journal=Am. J. Med. |volume=109 |issue=6 |pages=481–8 |year=2000 |month=October |pmid=11042238 |doi=10.1016/S0002-9343(00)00545-3}}</ref> This makes finding the correct dosage difficult, and accentuates the need of monitoring; when initiating a medication that is known to interact with warfarin (e.g. ]), ] checks are increased or dosages adjusted until a new ideal dosage is found. | |||
| Several risk scores exist to predict bleeding in people using warfarin and similar anticoagulants. A commonly used score (]) includes known predictors of warfarin-related bleeding: uncontrolled high ] (H), abnormal ] (A), previous stroke (S), known previous bleeding condition (B), previous ] INR when on anticoagulation (L), elderly as defined by age over 65 (E), and drugs associated with bleeding (e.g., aspirin) or alcohol misuse (D). While their use is recommended in clinical practice guidelines,<ref name=Camm2012>{{cite journal | vauthors = Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P | title = 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association | journal = European Heart Journal | volume = 33 | issue = 21 | pages = 2719–2747 | date = November 2012 | pmid = 22922413 | doi = 10.1093/eurheartj/ehs253 | doi-access = free | title-link = doi | url = https://boris.unibe.ch/15016/1/ehs253.pdf | access-date = 5 March 2024 | archive-date = 27 January 2024 | archive-url = https://web.archive.org/web/20240127015717/https://boris.unibe.ch/15016/1/ehs253.pdf | url-status = live }}</ref> they are only moderately effective in predicting bleeding risk and do not perform well in predicting hemorrhagic stroke.<ref>{{cite journal | vauthors = Shoeb M, Fang MC | title = Assessing bleeding risk in patients taking anticoagulants | journal = Journal of Thrombosis and Thrombolysis | volume = 35 | issue = 3 | pages = 312–319 | date = April 2013 | pmid = 23479259 | pmc = 3888359 | doi = 10.1007/s11239-013-0899-7 }}</ref> Bleeding risk may be increased in people on ].<ref name="pmid17720522">{{cite journal | vauthors = Elliott MJ, Zimmerman D, Holden RM | title = Warfarin anticoagulation in hemodialysis patients: a systematic review of bleeding rates | journal = American Journal of Kidney Diseases | volume = 50 | issue = 3 | pages = 433–440 | date = September 2007 | pmid = 17720522 | doi = 10.1053/j.ajkd.2007.06.017 }}</ref> Another score used to assess bleeding risk on anticoagulation, specifically Warfarin or Coumadin, is the ATRIA score, which uses a weighted additive scale of clinical findings to determine bleeding risk stratification.<ref>{{cite journal | vauthors = Fang MC, Go AS, Chang Y, Borowsky LH, Pomernacki NK, Udaltsova N, Singer DE | title = A new risk scheme to predict warfarin-associated hemorrhage: The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study | journal = Journal of the American College of Cardiology | volume = 58 | issue = 4 | pages = 395–401 | date = July 2011 | pmid = 21757117 | pmc = 3175766 | doi = 10.1016/j.jacc.2011.03.031 }}</ref> The risks of bleeding are increased further when warfarin is combined with ]s such as ], ], or ]s.<ref name="pmid17698822">{{cite journal | vauthors = Delaney JA, Opatrny L, Brophy JM, Suissa S | title = Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding | journal = CMAJ | volume = 177 | issue = 4 | pages = 347–351 | date = August 2007 | pmid = 17698822 | pmc = 1942107 | doi = 10.1503/cmaj.070186 }}</ref> | |||
| Many commonly-used antibiotics, such as ] or the ]s, will greatly increase the effect of warfarin by reducing the ] of warfarin in the body. Other ]s can reduce the amount of the normal ], which make significant quantities of vitamin K, thus potentiating the effect of warfarin.<ref name=Juurlink>{{cite journal |author=Juurlink DN |title=Drug interactions with warfarin: what clinicians need to know |journal=CMAJ |volume=177 |issue=4 |pages=369–71 |year=2007 |month=August |pmid=17698826 |pmc=1942100 |doi=10.1503/cmaj.070946 |url=http://www.cmaj.ca/cgi/content/full/177/4/369}}</ref> In addition, food that contains large quantities of vitamin K will reduce the warfarin effect.<ref name=Holbrook/> ] activity also appears to influence warfarin dosing requirements;<ref name=Kurnik>{{cite journal |author=Kurnik D, Loebstein R, Farfel Z, Ezra D, Halkin H, Olchovsky D |title=Complex drug-drug-disease interactions between amiodarone, warfarin, and the thyroid gland |journal=Medicine (Baltimore) |volume=83 |issue=2 |pages=107–13 |year=2004 |month=March |pmid=15028964 |doi= 10.1097/01.md.0000123095.65294.34|url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0025-7974&volume=83&issue=2&spage=107}}</ref> ] (decreased thyroid function) makes people less responsive to warfarin treatment,<ref>{{cite journal |author=Stephens MA, Self TH, Lancaster D, Nash T |title=Hypothyroidism: effect on warfarin anticoagulation |journal=South Med J |volume=82 |issue=12 |pages=1585–6 |year=1989 |month=December |pmid=2595433 |doi= |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0038-4348&volume=82&issue=12&spage=1585}}</ref> while ] (overactive thyroid) boosts the anticoagulant effect.<ref>{{cite journal |author=Chute JP, Ryan CP, Sladek G, Shakir KM |title=Exacerbation of warfarin-induced anticoagulation by hyperthyroidism |journal=Endocr Pract |volume=3 |issue=2 |pages=77–9 |year=1997 |pmid=15251480 |doi= |url=http://aace.metapress.com/openurl.asp?genre=article&issn=1530-891X&volume=3&issue=2&spage=77}}</ref> Several mechanisms have been proposed for this effect, including changes in the rate of breakdown of clotting factors and changes in the metabolism of warfarin.<ref name=Kurnik/><ref>{{cite journal |author=Kellett HA, Sawers JS, Boulton FE, Cholerton S, Park BK, Toft AD |title=Problems of anticoagulation with warfarin in hyperthyroidism |journal=Q J Med |volume=58 |issue=225 |pages=43–51 |year=1986 |month=January |pmid=3704105 |doi= |url=http://qjmed.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=3704105}}</ref> | |||
| === Warfarin necrosis === | |||
| Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR.<ref>{{cite journal |author=Weathermon R, Crabb DW |title=Alcohol and medication interactions |journal=Alcohol Res Health |volume=23 |issue=1 |pages=40–54 |year=1999 |pmid=10890797 |doi=}}</ref> Patients are often cautioned against the excessive use of alcohol while taking warfarin. | |||
| {{Main|Warfarin necrosis}} | |||
| A rare but serious complication resulting from treatment with warfarin is ], which occurs more frequently shortly after commencing treatment in patients with a deficiency of ], an innate anticoagulant that, like the procoagulant factors whose synthesis warfarin inhibits, requires vitamin K-dependent ] for its activity. Since warfarin initially decreases protein C levels faster than the coagulation factors, it can paradoxically increase the blood's tendency to coagulate when treatment is first begun (many patients when starting on warfarin are given ] in parallel to combat this), leading to massive thrombosis with skin ] and ] of limbs. Its natural counterpart, ], occurs in children who are ] for certain protein C mutations.<ref name="pmid10718793">{{cite journal | vauthors = Chan YC, Valenti D, Mansfield AO, Stansby G | title = Warfarin induced skin necrosis | journal = The British Journal of Surgery | volume = 87 | issue = 3 | pages = 266–272 | date = March 2000 | pmid = 10718793 | pmc = 4928566 | doi = 10.1046/j.1365-2168.2000.01352.x }}</ref> | |||
| === Osteoporosis === | |||
| Warfarin also interacts with many herbs and spices,<ref name="drug-herb">{{cite book |author=Austin, Steve and Batz, Forrest|editor=Lininger, Schuyler W.|title=A-Z guide to drug-herb-vitamin interactions: how to improve your health and avoid problems when using common medications and natural supplements together |publisher=Prima Health |location=Roseville, Calif |year=1999 |page=224 |isbn=0-7615-1599-2 |oclc= |doi=}}</ref> some used in food (such as ] and ]) and others used purely for medicinal purposes (such as ] and '']''). All may increase bleeding and bruising in people taking warfarin; similar effects have been reported with ] (]) oil or fish oils.<ref>{{Cite web |url=http://www.rpsgb.org/pdfs/libnewadd0802.pdf|title= Information Pharmacists’ news|accessdate=14 January 2009 |year= 2008|month= February|format= PDF| work = Information Centre Bulletin |publisher=] |location= 1 Lambeth High Street, London SE1 7JN|page= 1}} {{Dead link|date=September 2010|bot=H3llBot}}</ref> ], sometimes recommended to help with mild to moderate depression, interacts with warfarin; it ] the enzymes that break down warfarin in the body, causing a reduced anticoagulant effect.<ref>{{Cite web |url=http://www.rpsgb.org.uk/pdfs/scifactsheetstjwort.pdf |title= Herb-medicine interactions: St John’s Wort (Hypericum perforatum) Useful information for pharmacist |accessdate=14 January 2009 |author=Dr Jo Barnes BPharm MRPharmS |coauthors= Working Group on Complementary Medicine |year= 2002|month= September|format= PDF|publisher=] |location= 1 Lambeth High Street, London SE1 7JN |page= 5}}</ref> | |||
| After initial reports that warfarin could reduce ], several studies demonstrated a link between warfarin use and ]-related ]. A 1999 study in 572 women taking warfarin for ], risk of ] and ] was increased; other fracture types did not occur more commonly.<ref name="pmid10448778">{{cite journal | vauthors = Caraballo PJ, Heit JA, Atkinson EJ, Silverstein MD, O'Fallon WM, Castro MR, Melton LJ | title = Long-term use of oral anticoagulants and the risk of fracture | journal = Archives of Internal Medicine | volume = 159 | issue = 15 | pages = 1750–1756 | year = 1999 | pmid = 10448778 | doi = 10.1001/archinte.159.15.1750 | doi-access = | title-link=doi }}</ref> A 2002 study looking at a randomly selected selection of 1,523 patients with ] fracture found no increased exposure to anticoagulants compared to controls, and neither did stratification of the duration of anticoagulation reveal a trend towards fracture.<ref>{{cite journal | vauthors = Pilon D, Castilloux AM, Dorais M, LeLorier J | title = Oral anticoagulants and the risk of osteoporotic fractures among elderly | journal = Pharmacoepidemiology and Drug Safety | volume = 13 | issue = 5 | pages = 289–294 | date = May 2004 | pmid = 15133779 | doi = 10.1002/pds.888 | s2cid = 45496277 }}</ref> | |||
| A 2006 retrospective study of 14,564 ] recipients showed that warfarin use for more than one year was linked with a 60% increased risk of ]-related fracture in men, but no association in women was seen. The mechanism was thought to be a combination of reduced intake of vitamin K (a vitamin necessary for bone health) and inhibition by warfarin of vitamin K-mediated carboxylation of certain bone proteins, rendering them nonfunctional.<ref>{{cite journal | vauthors = Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF | title = Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2 | journal = Archives of Internal Medicine | volume = 166 | issue = 2 | pages = 241–246 | date = January 2006 | pmid = 16432096 | doi = 10.1001/archinte.166.2.241 | doi-access = | title-link=doi }}</ref> | |||
| Between 2003 and 2004, the UK ] received several reports of increased INR and risk of hemorrhage in people taking warfarin and ].<ref>{{cite web |url=http://news.bbc.co.uk/1/hi/health/3120206.stm |title=Cranberry juice clot drug warning |work=BBC news |date=18 September 2003 |accessdate=18 May 2008}}</ref><ref name=Suvarna>{{cite journal |author=Suvarna R, Pirmohamed M, Henderson L |title=Possible interaction between warfarin and cranberry juice |journal=BMJ |volume=327 |issue=7429 |page=1454 |year=2003 |month=December |pmid=14684645 |pmc=300803 |doi=10.1136/bmj.327.7429.1454 |url=}}</ref><ref name=Aston>{{cite journal |author=Aston JL, Lodolce AE, Shapiro NL |title=Interaction between warfarin and cranberry juice |journal=Pharmacotherapy |volume=26 |issue=9 |pages=1314–9 |year=2006 |month=September |pmid=16945054 |doi=10.1592/phco.26.9.1314 |url=}} </ref> Data establishing a causal relationship is still lacking, and a 2006 review found no cases of this interaction reported to the FDA;<ref name=Aston/> nevertheless, several authors have recommended that both doctors and patients be made aware of its possibility.<ref name=Pham>{{cite journal |author=Pham DQ, Pham AQ |title=Interaction potential between cranberry juice and warfarin |journal=Am J Health Syst Pharm |volume=64 |issue=5 |pages=490–4 |year=2007 |month=March |pmid=17322161 |doi=10.2146/ajhp060370 |url=}}</ref> The mechanism behind the interaction is still unclear.<ref name=Aston/> | |||
| === |
=== Purple toe syndrome === | ||
| {{see also|Blue toe syndrome}} | |||
| The effects of warfarin can be reversed with vitamin K, or, when rapid reversal is needed (such as in case of severe bleeding), with ]—which contains only the factors inhibited by warfarin—or ] (depending upon the clinical indication) in addition to ] vitamin K. | |||
| Another rare complication that may occur early during warfarin treatment (usually within 3 to 8 weeks of commencement) is ]. This condition is thought to result from small deposits of ] breaking loose and causing embolisms in blood vessels in the skin of the feet, which causes a blueish-purple colour and may be painful.<ref>{{cite journal | vauthors = O'Keeffe ST, Woods BO, Breslin DJ, Tsapatsaris NP | title = Blue toe syndrome. Causes and management | journal = Archives of Internal Medicine | volume = 152 | issue = 11 | pages = 2197–2202 | date = November 1992 | pmid = 1444678 | doi = 10.1001/archinte.1992.00400230023004 }}</ref> | |||
| It is typically thought to affect the ], but it affects other parts of the feet, as well, including the bottom of the foot (] surface). The occurrence of purple toe syndrome may require discontinuation of warfarin.<ref>{{cite journal | vauthors = Talmadge DB, Spyropoulos AC | title = Purple toes syndrome associated with warfarin therapy in a patient with antiphospholipid syndrome | journal = Pharmacotherapy | volume = 23 | issue = 5 | pages = 674–677 | date = May 2003 | pmid = 12741443 | doi = 10.1592/phco.23.5.674.32200 | s2cid = 28632135 }}</ref> | |||
| Details on reversing warfarin are provided in ] from the ].<ref name="Ansell2004"/> For patients with an ] (INR) between 4.5 and 10.0, a small dose of oral vitamin K is sufficient.<ref name="pmid12186515">{{cite journal |author=Crowther MA, Douketis JD, Schnurr T, ''et al.'' |title=Oral vitamin K lowers the international normalized ratio more rapidly than subcutaneous vitamin K in the treatment of warfarin-associated coagulopathy. A randomized, controlled trial |journal=Ann. Intern. Med. |volume=137 |issue=4 |pages=251–4 |year=2002 |pmid=12186515 |url=http://www.annals.org/cgi/reprint/137/4/251| format=PDF}}</ref> | |||
| === Calcification === | |||
| ==Pharmacology== | |||
| Several studies have also implicated warfarin use in valvular and vascular ]. No specific treatment is available, but some modalities are under investigation.<ref>{{cite journal | vauthors = Palaniswamy C, Sekhri A, Aronow WS, Kalra A, Peterson SJ | title = Association of warfarin use with valvular and vascular calcification: a review | journal = Clinical Cardiology | volume = 34 | issue = 2 | pages = 74–81 | date = February 2011 | pmid = 21298649 | pmc = 6652734 | doi = 10.1002/clc.20865 }}</ref> | |||
| ] | |||
| ===Pharmacokinetics=== <!--S-Waran redirects here--> | |||
| Warfarin consists of a ] mixture of two active ]s—''R''- and ''S''- forms—each of which is cleared by different pathways. S-warfarin has five times the potency of the R-isomer with respect to vitamin K antagonism.<ref name=Hirsh/> | |||
| == Overdose <span class="anchor" id="Reversal"></span>== | |||
| Warfarin is slower-acting than the common anticoagulant ], though it has a number of advantages. Heparin must be given by injection, whereas warfarin is available orally. Warfarin has a long half-life and need only be given once a day. Heparin can also cause a prothrombotic condition, ] (an antibody-mediated decrease in ] levels), which increases the risk for ]. It takes several days for warfarin to reach the therapeutic effect since the circulating coagulation factors are not affected by the drug (thrombin has a half-life time of days). Warfarin's long half-life means that it remains effective for several days after it was stopped. Furthermore, if given initially without additional anticoagulant cover, it can increase thrombosis risk (see below). For these main reasons, ]ised patients are usually given heparin with warfarin initially, the heparin covering the 3–5 day lag period and being withdrawn after a few days. | |||
| The major side effect of warfarin use is bleeding. Risk of bleeding is increased if the INR is out of range (due to accidental or deliberate overdose or due to interactions).<ref name=Garcia2010 /> Many drug interactions can increase the effect of warfarin, also causing an overdose.<ref name=Holbrook2005 /> | |||
| In patients with supratherapeutic INR but INR less than 10 and no bleeding, it is enough to lower the dose or omit a dose, monitor the INR and resume warfarin at an adjusted lower dose when the target INR is reached.<ref name=Farinde2019>{{cite journal|url=https://emedicine.medscape.com/article/2172018-overview|title=Warfarin Overanticoagulation|website=Medscape|date=18 April 2019|author=Abimbola Farinde|access-date=19 August 2022|archive-date=19 August 2022|archive-url=https://web.archive.org/web/20220819155343/https://emedicine.medscape.com/article/2172018-overview|url-status=live}}</ref> For people who need rapid reversal of warfarin – such as due to serious bleeding – or who need emergency surgery, the effects of warfarin can be reversed with vitamin K, ] (PCC), or ] (FFP).<ref name=Ag2012 /> Generally, four-factor PCC can be given more quickly than FFP, the amount needed is a smaller volume of fluid than FFP, and does not require ABO ]. Administration of PCCs results in rapid hemostasis, similar to that of FFP, namely, with comparable rates of thromboembolic events, but with reduced rates of volume overload. Blood products should not be routinely used to reverse warfarin overdose, when vitamin K could work alone.<ref name=Ag2012 /> While PCC has been found in lab tests to be better than FFP, when rapid reversal is needed,<ref name=Chai2016>{{cite journal | vauthors = Chai-Adisaksopha C, Hillis C, Siegal DM, Movilla R, Heddle N, Iorio A, Crowther M | title = Prothrombin complex concentrates versus fresh frozen plasma for warfarin reversal. A systematic review and meta-analysis | journal = Thrombosis and Haemostasis | volume = 116 | issue = 5 | pages = 879–890 | date = October 2016 | pmid = 27488143 | doi = 10.1160/TH16-04-0266 | s2cid = 4733615 }}</ref> as of 2018, whether a difference in outcomes such as death or disability exists is unclear.<ref>{{cite journal | vauthors = Tornkvist M, Smith JG, Labaf A | title = Current evidence of oral anticoagulant reversal: A systematic review | journal = Thrombosis Research | volume = 162 | pages = 22–31 | date = February 2018 | pmid = 29258056 | doi = 10.1016/j.thromres.2017.12.003 }}</ref> | |||
| ===Mechanism of action=== | |||
| Warfarin inhibits the ]-dependent synthesis of biologically active forms of the ]-dependent ] factors ], ], ] and ], as well as the regulatory factors ], ], and ].<ref name=Ansell2004/><ref>{{cite journal |author=Freedman MD |title=Oral anticoagulants: pharmacodynamics, clinical indications and adverse effects |journal=J Clin Pharmacol |volume=32 |issue=3 |pages=196–209 |year=1992 |month=March |pmid=1564123}}</ref> Other proteins not involved in blood clotting, such as ], or ], may also be affected. | |||
| When warfarin is being given and INR is in therapeutic range, simple discontinuation of the drug for five days is usually enough to reverse the effect and cause INR to drop below 1.5.<ref name="pmid12186515">{{cite journal | vauthors = Crowther MA, Douketis JD, Schnurr T, Steidl L, Mera V, Ultori C, Venco A, Ageno W | title = Oral vitamin K lowers the international normalized ratio more rapidly than subcutaneous vitamin K in the treatment of warfarin-associated coagulopathy. A randomized, controlled trial | journal = Annals of Internal Medicine | volume = 137 | issue = 4 | pages = 251–254 | date = August 2002 | pmid = 12186515 | doi = 10.7326/0003-4819-137-4-200208200-00009 | s2cid = 10450603 }}</ref> | |||
| The precursors of these factors require ] of their ] residues to allow the coagulation factors to bind to ] surfaces inside blood vessels, on the vascular ]. The enzyme that carries out the carboxylation of glutamic acid is ]. The carboxylation reaction will proceed only if the carboxylase enzyme is able to convert a ] form of vitamin K (vitamin K hydroquinone) to vitamin K epoxide at the same time. The vitamin K epoxide is in turn recycled back to vitamin K and vitamin K hydroquinone by another enzyme, the ] (VKOR). Warfarin inhibits epoxide reductase<ref name=Whitlon>{{cite journal |author=Whitlon DS, Sadowski JA, Suttie JW |title=Mechanism of coumarin action: significance of vitamin K epoxide reductase inhibition |journal=Biochemistry |volume=17 |issue=8 |pages=1371–7 |year=1978 |pmid=646989|doi=10.1021/bi00601a003}}</ref> (specifically the VKORC1 subunit<ref>{{cite journal |author=Li T, Chang CY, Jin DY, Lin PJ, Khvorova A, Stafford DW |title=Identification of the gene for vitamin K epoxide reductase |journal=Nature |volume=427 |issue=6974 |pages=541–4 |year=2004 |pmid=14765195 |doi=10.1038/nature02254}}</ref><ref name="pmid14765194">{{cite journal |author=Rost S, Fregin A, Ivaskevicius V, ''et al.'' |title=Mutations in VKORC1 cause warfarin resistance and multiple coagulation factor deficiency type 2 |journal=Nature |volume=427 |issue=6974 |pages=537–41 |year=2004 |pmid=14765194 |doi=10.1038/nature02214}}</ref>), thereby diminishing available vitamin K and vitamin K hydroquinone in the tissues, which inhibits the carboxylation activity of the glutamyl carboxylase. When this occurs, the coagulation factors are no longer carboxylated at certain ] residues, and are incapable of binding to the ] surface of blood vessels, and are thus biologically inactive. As the body's stores of previously-produced active factors degrade (over several days) and are replaced by inactive factors, the anticoagulation effect becomes apparent. The coagulation factors are produced, but have decreased functionality due to undercarboxylation; they are collectively referred to as PIVKAs (proteins induced vitamin K absence/antagonism), and individual coagulation factors as PIVKA-''number'' (e.g. ]). The end result of warfarin use, therefore, is to diminish blood clotting in the patient. | |||
| {|class=wikitable | |||
| When warfarin is newly started, it may ''promote'' clot formation temporarily. This is because the level of ] and ] are also dependent on vitamin K activity. Warfarin causes decline in protein C levels in first 36 hours. In addition, reduced levels of protein S lead to a reduction in activity of ] (for which it is the co-factor) and therefore reduced degradation of ]a and ]a. Although loading doses of warfarin over 5 mg also produce a precipitous decline in ], resulting in an initial prolongation of the INR, full antithrombotic effect does not take place until significant reduction in factor II occurs days later. The hemostasis system becomes temporarily biased towards thrombus formation, leading to a prothrombotic state. Thus, when warfarin is loaded rapidly at greater than 5 mg per day, it is beneficial to co-administer ], an anticoagulant that acts upon ] and helps reduce the risk of thrombosis, with warfarin therapy for four to five days, in order to have the benefit of anticoagulation from heparin until the full effect of warfarin has been achieved.<ref>{{cite journal |author=Litin SC, Gastineau DA |title=Current concepts in anticoagulant therapy |journal=Mayo Clin. Proc. |volume=70 |issue=3 |pages=266–72 |year=1995 |month=March |pmid=7861815 |doi=10.4065/70.3.266}}</ref><ref>{{cite journal |author=Wittkowsky AK |title=Why warfarin and heparin need to overlap when treating acute venous thromboembolism |journal=Dis Mon |volume=51 |issue=2–3 |pages=112–5 |year=2005 |pmid=15900262 |doi=10.1016/j.disamonth.2005.03.005}}</ref> | |||
| |+Warfarin overdose recommendations<ref name=Farinde2019/> | |||
| |- | |||
| ! Supratherapeutic INR but INR < 4.5, no bleeding | |||
| | | |||
| *Lowering the dose or omit a dose | |||
| *Monitoring daily | |||
| *Resuming at an adjusted lower dose when the target INR is reached. | |||
| |- | |||
| ! INR 4.5-10, no bleeding | |||
| | | |||
| *Omitting 1-2 doses | |||
| *Monitoring INR | |||
| *Readjusting dose | |||
| |- | |||
| ! INR >10.0, no bleeding | |||
| | | |||
| *Holding warfarin, monitoring INR, and readjusting dose | |||
| *Vitamin K1 (phytonadione) 2-2.5 mg PO or 0.5–1 mg IV | |||
| |- | |||
| ! Minor bleeding, any elevated INR: | |||
| | | |||
| *Holding warfarin, monitoring INR, and readjusting dose | |||
| *Considering vitamin K1 (phytonadione) 2.5–5 mg PO once, and may repeat if needed after 24 h | |||
| |- | |||
| ! Major bleeding, any elevated INR | |||
| | | |||
| *Holding warfarin, monitoring INR, and readjusting dose | |||
| *Prothrombin complex concentrate plus vitamin K1 (phytonadione) 5–10 mg IV | |||
| May also consider supplementation with fresh frozen plasma (FFP) or recombinant factor VIIa | |||
| |- | |||
| ! Life-threatening bleeding and elevated INR: | |||
| | | |||
| *Holding warfarin therapy | |||
| *] and vitamin K 10 mg by slow IV infusion | |||
| |} | |||
| == Interactions == | |||
| ===Chemical synthesis=== | |||
| The succinct synthesis of warfarin starts with condensation of ortho-hydroxyacetophenone | |||
| (1–2) with ethyl carbonate to give the b-ketoester as the intermediate shown in the ] form. Attack of the ] on the ester grouping leads to cyclization and formation of the ]. ] of the ] from that product to methyl styryl ketone gives the corresponding ] and thus warfarin.<ref>{{Cite journal|doi=10.1021/ja01319a042|year=1934|last1=Blicke|first1=F. F.|last2=Swisher|first2=R. D.|journal=Journal of the American Chemical Society|volume=56|pages=902|issue=4}}</ref> | |||
| Warfarin ] with many commonly used drugs, and the ] of warfarin varies greatly between patients.<ref name=Holbrook2005 /> Some foods have also been reported to interact with warfarin.<ref name=Holbrook2005 /> Apart from the metabolic interactions, highly protein bound drugs can displace warfarin from ] and cause an increase in the INR.<ref>{{cite journal | vauthors = Gage BF, Fihn SD, White RH | title = Management and dosing of warfarin therapy | journal = The American Journal of Medicine | volume = 109 | issue = 6 | pages = 481–488 | date = October 2000 | pmid = 11042238 | doi = 10.1016/S0002-9343(00)00545-3 }}</ref> This makes finding the correct dosage difficult, and accentuates the need of monitoring; when initiating a medication that is known to interact with warfarin (e.g., ]), ] checks are increased or dosages adjusted until a new ideal dosage is found. | |||
| ] | |||
| When taken with ]s (NSAIDs), warfarin increases the risk for ]. This increased risk is due to the antiplatelet effect of NSAIDs and possible damage to the gastrointestinal ].<ref>{{cite journal | vauthors = Ament PW, Bertolino JG, Liszewski JL | title = Clinically significant drug interactions | journal = American Family Physician | volume = 61 | issue = 6 | pages = 1745–1754 | date = March 2000 | pmid = 10750880 | url = https://www.aafp.org/pubs/afp/issues/2000/0315/p1745.html | access-date = 22 August 2023 | url-status = live | archive-url = https://web.archive.org/web/20160507065339/http://www.aafp.org/afp/2000/0315/p1745.html | archive-date = 7 May 2016 }}</ref><ref>{{cite journal | vauthors = Carpenter M, Berry H, Pelletier AL | title = Clinically Relevant Drug-Drug Interactions in Primary Care | journal = American Family Physician | volume = 99 | issue = 9 | pages = 558–564 | date = May 2019 | pmid = 31038898 | url = https://www.aafp.org/pubs/afp/issues/2019/0501/p558.html | access-date = 22 August 2023 | archive-date = 23 August 2023 | archive-url = https://web.archive.org/web/20230823020207/https://www.aafp.org/pubs/afp/issues/2019/0501/p558.html | url-status = live }}</ref> | |||
| ===Molecular structure=== | |||
| X-ray crystallographic studies of warfarin show that it exists in ]ic form, as the cyclic ], which is formed from the 4-hydroxycoumadin and the ketone in the 3-position substituent.<ref>{{ cite journal | journal = ] | year = 1975 | volume = 31 | pages = 954–960 | title = The crystal and molecular structure and absolute configuration of (−)-(''S'')-warfarin | first1 = E. J. | last1 = Valente | first2 = W. F. | last2 = Trager | first3 = L. H. | last3 = Jensen | doi = 10.1107/S056774087500427X | issue = 4 }}</ref> However, the existence of many 4-hydroxycoumadin anticoagulants (for example ]) that possess no ketone group in the 3-substituent to form such a structure, suggests that the hemiketal must hydrolyze to the 4-hydroxy form in order for warfarin to be active.<ref>{{cite journal | doi = 10.1021/jp072505i | title = The Spectrophysics of Warfarin: Implications for Protein Binding | year = 2007 | last1 = Karlsson | first1 = Björn C. G. | last2 = Rosengren | first2 = Annika M. | last3 = Andersson | first3 = Per Ola | last4 = Nicholls | first4 = Ian A. | journal = The Journal of Physical Chemistry B | volume = 111 | issue = 35 | pages = 10520–10528 | pmid = 17691835}}</ref> | |||
| :]{{clear-left}} | |||
| Many commonly used ]s, such as ] or the ]s, greatly increase the effect of warfarin by reducing the metabolism of warfarin in the body. Other ]s can reduce the amount of the normal ], which make significant quantities of vitamin K<sub>1</sub>, thus potentiating the effect of warfarin.<ref name=Juurlink>{{cite journal | vauthors = Juurlink DN | title = Drug interactions with warfarin: what clinicians need to know | journal = CMAJ | volume = 177 | issue = 4 | pages = 369–371 | date = August 2007 | pmid = 17698826 | pmc = 1942100 | doi = 10.1503/cmaj.070946 }}</ref> In addition, food that contains large quantities of vitamin K<sub>1</sub> will reduce the warfarin effect.<ref name=Holbrook2005 /><ref name=Holbrook2012 /> ] activity also appears to influence warfarin dosing requirements;<ref name=Kurnik>{{cite journal | vauthors = Kurnik D, Loebstein R, Farfel Z, Ezra D, Halkin H, Olchovsky D | title = Complex drug-drug-disease interactions between amiodarone, warfarin, and the thyroid gland | journal = Medicine | volume = 83 | issue = 2 | pages = 107–113 | date = March 2004 | pmid = 15028964 | doi = 10.1097/01.md.0000123095.65294.34 | s2cid = 43173080 | doi-access = free }}</ref> ] (decreased thyroid function) makes people less responsive to warfarin treatment,<ref>{{cite journal | vauthors = Stephens MA, Self TH, Lancaster D, Nash T | title = Hypothyroidism: effect on warfarin anticoagulation | journal = Southern Medical Journal | volume = 82 | issue = 12 | pages = 1585–1586 | date = December 1989 | pmid = 2595433 | doi = 10.1097/00007611-198912000-00035 }}</ref> while ] (overactive thyroid) boosts the anticoagulant effect.<ref>{{cite journal | vauthors = Chute JP, Ryan CP, Sladek G, Shakir KM | title = Exacerbation of warfarin-induced anticoagulation by hyperthyroidism | journal = Endocrine Practice | volume = 3 | issue = 2 | pages = 77–79 | year = 1997 | pmid = 15251480 | doi = 10.4158/EP.3.2.77 }}</ref> Several mechanisms have been proposed for this effect, including changes in the rate of breakdown of clotting factors and changes in the metabolism of warfarin.<ref name=Kurnik /><ref>{{cite journal | vauthors = Kellett HA, Sawers JS, Boulton FE, Cholerton S, Park BK, Toft AD | title = Problems of anticoagulation with warfarin in hyperthyroidism | journal = The Quarterly Journal of Medicine | volume = 58 | issue = 225 | pages = 43–51 | date = January 1986 | pmid = 3704105 }}</ref> | |||
| ===Pharmacogenomics=== | |||
| Warfarin activity is determined partially by genetic factors. The American ] "highlights the opportunity for healthcare providers to use genetic tests to improve their initial estimate of what is a reasonable warfarin dose for individual patients".<ref>{{cite web |url=http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108967.htm |title=FDA Approves Updated Warfarin (Coumadin) Prescribing Information |accessdate=4 August 2009 |work=}}</ref> ]s in two genes (VKORC1 and CYP2C9) are particularly important. | |||
| Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR, and thus increase the risk of bleeding.<ref>{{cite journal | vauthors = Weathermon R, Crabb DW | title = Alcohol and medication interactions | journal = Alcohol Research & Health | volume = 23 | issue = 1 | pages = 40–54 | year = 1999 | pmid = 10890797 | pmc = 6761694 }}</ref> The U.S. ] (FDA) product insert on warfarin states that alcohol should be avoided.<ref name=TGA >{{cite web |title = PRODUCT INFORMATION COUMADIN |work = TGA eBusiness Services |publisher = Aspen Pharma Pty Ltd |date = 19 January 2010 |access-date = 11 December 2013 |url = https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-02588-3 |format = PDF |url-status = live |archive-url = https://web.archive.org/web/20151017135417/https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-02588-3 |archive-date = 17 October 2015 }}</ref> The ] suggests that when taking warfarin one should not drink more than "one beer, 6 oz of wine, or one shot of alcohol per day".<ref>{{cite web|url=https://my.clevelandclinic.org/health/drugs/16182-warfarin-a-blood-thinning-drug-what-you-need-to-know-|title=Warfarin Anticoagulant Medication|access-date=30 June 2020|archive-date=1 July 2020|archive-url=https://web.archive.org/web/20200701125620/https://my.clevelandclinic.org/health/drugs/16182-warfarin-a-blood-thinning-drug-what-you-need-to-know-|url-status=live}}</ref> | |||
| * ] polymorphisms explain 30% of the dose variation between patients:<ref name="pmid15883587">{{cite journal |author=Wadelius M, Chen LY, Downes K, ''et al.'' |title=Common VKORC1 and GGCX polymorphisms associated with warfarin dose |journal=Pharmacogenomics J. |volume=5 |issue=4 |pages=262–70 |year=2005 |pmid=15883587 |doi=10.1038/sj.tpj.6500313}}</ref> particular mutations make VKORC1 less susceptible to suppression by warfarin.<ref name="pmid14765194"/> There are two main haplotypes that explain 25% of variation: low-dose haplotype group (A) and a high-dose haplotype group (B).<ref name="pmid15930419">{{cite journal |author=Rieder MJ, Reiner AP, Gage BF, ''et al.'' |title=Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose |journal=N. Engl. J. Med. |volume=352 |issue=22 |pages=2285–93 |year=2005 |doi=10.1056/NEJMoa044503 | pmid=15930419}}</ref> ''VKORC1'' polymorphisms explain why African Americans are on average relatively resistant to warfarin (higher proportion of group B haplotypes), while ]s are generally more sensitive (higher proportion of group A haplotypes).<ref name="pmid15930419"/> Group A ''VKORC1'' polymorphisms lead to a more rapid achievement of a therapeutic INR, but also a shorter time to reach an INR over 4, which is associated with bleeding.<ref name="pmid18322281">{{cite journal |author=Schwarz UI, Ritchie MD, Bradford Y, ''et al.'' |title=Genetic determinants of response to warfarin during initial anticoagulation |journal=N. Engl. J. Med. |volume=358 |issue=10 |pages=999–1008 |year=2008 |pmid=18322281 |doi=10.1056/NEJMoa0708078}}</ref> | |||
| Warfarin also interacts with many herbs and spices,<ref name="drug-herb">{{cite book | vauthors = Austin S, Batz F | veditors = Lininger SW |title = A-Z guide to drug-herb-vitamin interactions: how to improve your health and avoid problems when using common medications and natural supplements together |publisher = Prima Health |location = Roseville, Calif |year = 1999 |page = |isbn = 978-0-7615-1599-9 |url-access = registration |url = https://archive.org/details/azguidetodrugher0000unse/page/224 }}</ref> some used in food (such as ] and ]) and others used purely for medicinal purposes (such as ] and '']''). All may increase bleeding and bruising in people taking warfarin; similar effects have been reported with ] (]) oil.<ref>{{cite journal | vauthors = Heck AM, DeWitt BA, Lukes AL | title = Potential interactions between alternative therapies and warfarin | journal = American Journal of Health-System Pharmacy | volume = 57 | issue = 13 | pages = 1221–1227; quiz 1228–1230 | date = July 2000 | pmid = 10902065 | doi = 10.1093/ajhp/57.13.1221 | doi-access = free }}</ref> ], sometimes recommended to help with mild to moderate depression, reduces the effectiveness of a given dose of warfarin; it ] the enzymes that break down warfarin in the body, causing a reduced anticoagulant effect.<ref>{{cite web |url = http://www.rpsgb.org.uk/pdfs/scifactsheetstjwort.pdf |title = Herb-medicine interactions: St John's Wort (Hypericum perforatum) Useful information for pharmacist |access-date = 14 January 2009 |vauthors = Barnes J, ((Working Group on Complementary Medicine)) |date = September 2002 |publisher = ] |location = London |page = 5 |url-status = dead |archive-url = https://web.archive.org/web/20060924184428/http://www.rpsgb.org.uk/pdfs/scifactsheetstjwort.pdf |archive-date = 24 September 2006 }}</ref> | |||
| * '']'' polymorphisms explain 10% of the dose variation between patients,<ref name="pmid15883587"/> mainly among Caucasian patients as these variants are rare in African American and most Asian populations.<ref name="pmid15714076">{{cite journal |author=Sanderson S, Emery J, Higgins J |title=CYP2C9 gene variants, drug dose, and bleeding risk in warfarin-treated patients: a HuGEnet systematic review and meta-analysis |journal=Genet. Med. |volume=7 |issue=2 |pages=97–104 |year=2005 |pmid=15714076 |doi=10.1002/ajmg.a.30391}}</ref> These ''CYP2C9'' polymorphisms do not influence time to effective INR as opposed to ''VKORC1'', but does shorten the time to ] >4.<ref name="pmid18322281"/> | |||
| Between 2003 and 2004, the UK ] received several reports of increased INR and risk of haemorrhage in people taking warfarin and ].<ref>{{cite web |url = http://news.bbc.co.uk/1/hi/health/3120206.stm |title = Cranberry juice clot drug warning |work = BBC News |date = 18 September 2003 |access-date = 18 May 2008 |url-status = live |archive-url = https://web.archive.org/web/20080209212613/http://news.bbc.co.uk/1/hi/health/3120206.stm |archive-date = 9 February 2008 }}</ref><ref name=Suvarna>{{cite journal | vauthors = Suvarna R, Pirmohamed M, Henderson L | title = Possible interaction between warfarin and cranberry juice | journal = BMJ | volume = 327 | issue = 7429 | pages = 1454 | date = December 2003 | pmid = 14684645 | pmc = 300803 | doi = 10.1136/bmj.327.7429.1454 }}</ref><ref name=Aston>{{cite journal | vauthors = Aston JL, Lodolce AE, Shapiro NL | title = Interaction between warfarin and cranberry juice | journal = Pharmacotherapy | volume = 26 | issue = 9 | pages = 1314–1319 | date = September 2006 | pmid = 16945054 | doi = 10.1592/phco.26.9.1314 | s2cid = 28468365 }} {{webarchive|url=https://web.archive.org/web/20101109014448/http://www.medscape.com/viewarticle/545631 |date=9 November 2010 }}</ref> Data establishing a causal relationship are still lacking, and a 2006 review found no cases of this interaction reported to the USFDA;<ref name=Aston /> nevertheless, several authors have recommended that both doctors and patients be made aware of its possibility.<ref name=Pham>{{cite journal | vauthors = Pham DQ, Pham AQ | title = Interaction potential between cranberry juice and warfarin | journal = American Journal of Health-System Pharmacy | volume = 64 | issue = 5 | pages = 490–494 | date = March 2007 | pmid = 17322161 | doi = 10.2146/ajhp060370 }}</ref> The mechanism behind the interaction is still unclear.<ref name=Aston /> | |||
| Despite the promise of pharmacogenomic testing in warfarin dosing, its use in clinical practice is controversial. In August 2009 the ] concluded that "the available evidence does not demonstrate that pharmacogenomic testing of CYP2C9 or VKORC1 alleles to predict warfarin responsiveness improves health outcomes in ] beneficiaries."<ref>{{cite web |url=http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=224&ver=15&NcaName=Pharmacogenomic+Testing+for+Warfarin+Response&NCDId=333&ncdver=1&IsPopup=y&bc=AAAAAAAAEAAA& |title=Decision Memo for Pharmacogenomic Testing for Warfarin Response (CAG-00400N) |author=Jensen TS, Jacques LB, Ciccanti M, Long K, Eggleston L, Roche J |date=August 3, 2009 |publisher=Centers for Medicare and Medicaid Services |accessdate=March 27, 2011}}</ref> Two ] have found that even though genetic testing may predict stable doses of warfarin, the testing does not increase time in therapeutic range (i.e., time in the desired level of anticoagulation).<ref>{{Cite journal | author = Anderson JL, Horne BD, Stevens SM, Grove AS, Barton S, Nicholas ZP, Kahn SF, May HT, Samuelson KM, Muhlestein JB, Carlquist JF; Couma-Gen Investigators | title = Randomized trial of genotype-guided versus standard warfarin dosing in patients initiating oral anticoagulation | journal = Circulation | volume = 116 | pages = 2563–70 | year = 2007 | doi = 10.1161/CIRCULATIONAHA.107.737312 | pmid = 17989110 | url = http://circ.ahajournals.org/cgi/content/full/CIRCULATIONAHA.107.737312/ | issue = 22}}</ref><ref>{{Cite journal | author = Burmester JK, Berg RL, Yale SH, Rottscheit CM, Glurich IE, Schmelzer JR, Caldwell MD | title = A randomized controlled trial of genotype-based Coumadin initiation | journal = Genet Med | volume = 13 | pages = 509–518 | year = 2011 | doi = 10.1097/GIM.0b013e31820ad77d | pmid = 21423021 | issue = 6 }}</ref> A recent study found that prospective warfarin genotyping reduced hospitalization rates for patients just starting warfarin therapy<ref>{{Cite journal | author = Epstein RS, Moyer TP, Aubert RE, O'Kane DJ, Xia F Verbrugge RR, Gage BF, Teagarden JR | title = Warfarin genotyping reduces hospitalization rates, results from the MM-WES (Medco-Mayo Warfarin Effectiveness study). | journal = Journal of the American College of Cardiology | volume = 55 | pages = 2804–2812 | year = 2010 | doi = doi:10.1016/j.jacc.2010.03.009 | pmid = 20381283}}</ref>. | |||
| == |
== Chemistry == | ||
| ] | |||
| In the early 1920s, there was an outbreak of a previously unrecognised ] disease in the northern United States and Canada. Cattle were ] after minor procedures, and on some occasions, spontaneously. For example, 21 out of 22 cows died after dehorning, and 12 out of 25 bulls died after castration. All of these animals had bled to death.<ref name="Laurence 1973 23.4-23.5">{{cite book|title=Clinical Pharmacology |last=Laurence |first=D.R. |others=Peter Kneebone |year=1973 |publisher=Churchill Livingstone|location=Edinburgh, London and New York |pages=23.4–23.5 |isbn=0443049904}}</ref> | |||
| X-ray ] studies of warfarin show that it exists in ]ic form, as the cyclic ], which is formed from the 4-hydroxycoumarin and the ] in the 3-position substituent.<ref>{{cite journal |journal = ] |year = 1975 |volume = 31 |issue = 4 |pages = 954–960 |title = The crystal and molecular structure and absolute configuration of (−)-(''S'')-warfarin | vauthors = Valente EJ, Trager, Jensen LH |doi = 10.1107/S056774087500427X |bibcode = 1975AcCrB..31..954V |url = http://pilotscholars.up.edu/cgi/viewcontent.cgi?article=1004&context=chm_facpubs |url-status = dead |archive-url = https://web.archive.org/web/20151020103015/http://pilotscholars.up.edu/cgi/viewcontent.cgi?article=1004&context=chm_facpubs |archive-date = 20 October 2015 |url-access = subscription }}</ref> However, the existence of many 4-hydroxycoumadin anticoagulants (for example ]) that possess no ketone group in the 3-substituent to form such a structure, suggests that the hemiketal must tautomerise to the 4-hydroxy form in order for warfarin to be active.<ref name="pmid17691835">{{cite journal | vauthors = Karlsson BC, Rosengren AM, Andersson PO, Nicholls IA | title = The spectrophysics of warfarin: implications for protein binding | journal = The Journal of Physical Chemistry B | volume = 111 | issue = 35 | pages = 10520–10528 | date = September 2007 | pmid = 17691835 | doi = 10.1021/jp072505i | author-link4 = Ian A. Nicholls }}</ref> | |||
| === Stereochemistry === | |||
| In 1921, Frank Schofield, a Canadian ] ], determined that the cattle were ingesting mouldy ] made from ] that functioned as a potent anticoagulant. Only spoiled hay made from sweet clover (grown in northern states of the USA and in Canada since the turn of the century) produced the disease.<ref>{{cite journal|author=Schofield FW|title=Damaged sweet clover; the cause of a new disease in cattle simulating haemorrhagic septicemia and blackleg|journal=J Am Vet Med Assoc|year=1924|volume=64|pages=553–6}}</ref> Schofield separated good clover stalks and damaged clover stalks from the same hay mow, and fed each to a different rabbit. The rabbit that had ingested the good stalks remained well, but the rabbit that had ingested the damaged stalks died from a haemorrhagic illness. A duplicate experiment with a different sample of clover hay produced the same result.<ref name="Laurence 1973 23.4-23.5"/> In 1929, North Dakota veterinarian Dr L.M. Roderick demonstrated that the condition was due to a lack of functioning ].<ref>{{cite journal|author=Roderick LM|year=1931|title=A problem in the coagulation of the blood; "sweet clover disease of the cattle"|journal=Am J Physiol |volume=96|pages=413–6}}.</ref> | |||
| Warfarin contains a ] and consists of two ]s. This is a ], i.e., a 1: 1 mixture of ('' R '') – and the ('' S '') – form:<ref name="Rote Liste">{{cite book |publisher = Rote Liste Service GmbH |title = Rote Liste 2017 – Arzneimittelverzeichnis für Deutschland (einschließlich EU-Zulassungen und bestimmter Medizinprodukte) |location = Frankfurt/Main |year = 2017 |isbn = 978-3-946057-10-9 |page = 226 }}</ref> | |||
| {| class="wikitable" style="text-align:center" | |||
| The identity of the anticoagulant substance in spoiled sweet clover remained a mystery until 1940. In 1933 ] and his lab of chemists working at the ] set out to isolate and characterize the hemorrhagic agent from the spoiled hay. It took five years for Link's student Harold A. Campbell to recover 6 mg of crystalline anticoagulant. Next, Link's student Mark A. Stahmann took over the project and initiated a large-scale extraction, isolating 1.8 g of recrystallized anticoagulant in about 4 months. This was enough material for Stahmann and Charles F. Huebner to check their results against Campbell's and to thoroughly characterize the compound. Through degradation experiments they established that the anticoagulant was 3,3'-methylenebis-(4-hydroxycoumarin), which they later named ]. They confirmed their results by synthesizing dicoumarol and proving in 1940 that it was identical to the naturally occurring agent.<ref>{{cite journal|author=Stahmann MA, Huebner CF, Link KP|date=1 April 1941|title=Studies on the hemorrhagic sweet clover disease. V. Identification and synthesis of the hemorrhagic agent|journal=J Biol Chem|volume=138|pages=513–27|url=http://www.jbc.org/cgi/reprint/138/2/513|issue=2}}</ref> | |||
| |- class="hintergrundfarbe6" | |||
| ! colspan="2"| Enantiomers of warfarin | |||
| |- | |||
| | ]<br /><small> CAS Number: 5543-58-8</small> | |||
| | ]<br /><small> CAS Number: 5543-57-7</small> | |||
| |} | |||
| == Pharmacology == | |||
| Dicoumarol was a product of the plant molecule ] (not to be confused with Couma'''d'''in, a later tradename for warfarin). Coumarin is now known to be present in many plants, and produces the notably sweet smell of freshly cut grass or hay and plants like ]; in fact, the plant's high content of coumarin is responsible for the original common name of "sweet clover", which is named for its sweet smell, not its bitter taste.<ref name="Laurence 1973 23.4-23.5"/> They are present notably in ] (''Galium odoratum'', ]), and at lower levels in ], ], and various other species. However, coumarins themselves do not influence clotting or warfarin-like action, but must first be metabolized by various fungi into compounds such as ], then further (in the presence of naturally occurring ]) into ], in order to have any anticoagulant properties. Fungal attack of the damaged and dying clover stalks explained the presence of the anticoagulant only in spoiled clover silages; dicoumarol is considered to be a fermentation product and ].<ref>Bye, A., King, H. K., 1970. The biosynthesis of 4-hydroxycoumarin and dicoumarol by Aspergillus fumigatus Fresenius. Biochemical Journal 117, 237–245.</ref> | |||
| ] | |||
| === Pharmacokinetics === | |||
| Over the next few years, numerous similar chemicals (specifically 4-hydroxycoumarins with a large ] substitutent at the '''3'''' position) were found to have the same anticoagulant properties. The first drug in the class to be widely commercialized was ] itself, patented in 1941 and later used as a pharmaceutical. Karl Link continued working on developing more potent coumarin-based anticoagulants for use as ], resulting in warfarin in 1948. The name "warfarin" stems from the acronym ''WARF'', for '']'' + the ending ''-arin'' indicating its link with coumarin. Warfarin was first registered for use as a rodenticide in the US in 1948, and was immediately popular. Although warfarin was developed by Link, the WARF financially supported the research and was assigned the patent.<ref name="pmid13619027">{{cite journal |author=Link KP |title=The discovery of dicumarol and its sequels |journal=Circulation |volume=19 |issue=1 |pages=97–107 |date=1 January 1959|pmid=13619027|url=http://circ.ahajournals.org/cgi/reprint/19/1/97}}</ref> | |||
| <!-- S-Waran redirects here --> | |||
| Warfarin consists of a ] mixture of two active ]s—''R''- and ''S''- forms—each of which is cleared by different pathways. S-warfarin is two to five times more potent than the R-isomer in producing an anticoagulant response.<ref name="Hirsh_2003" /> Both the enantiomers of warfarin undergo CYP-mediated metabolism by many different CYPs to form 3',4',6,7,8 and 10-hydroxy warfarin metabolites, major being 7-OH warfarin formed from S-warfarin by CYP2C9 and 10-OH warfarin from R-warfarin by CYP3A4.<ref>{{cite journal | vauthors = Shaik AN, Grater R, Lulla M, Williams DA, Gan LL, Bohnert T, LeDuc BW | title = Comparison of enzyme kinetics of warfarin analyzed by LC-MS/MS QTrap and differential mobility spectrometry | journal = Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences | volume = 1008 | issue = 1 | pages = 164–173 | date = January 2016 | pmid = 26655108 | doi = 10.1016/j.jchromb.2015.11.036 }}</ref> | |||
| Warfarin is slower-acting than the common anticoagulant ], though it has a number of advantages. Heparin must be given by injection, whereas warfarin is available orally. Warfarin has a long half-life and need only be given once a day. Heparin can also cause a prothrombotic condition, ] (an ]-mediated decrease in ] levels), which increases the risk for thrombosis. It takes several days for warfarin to reach the therapeutic effect, since the circulating coagulation factors are not affected by the drug (thrombin has a half-life time of days). Warfarin's long half-life means that it remains effective for several days after it is stopped. Furthermore, if given initially without additional anticoagulant cover, it can increase thrombosis risk (see below). | |||
| After an incident in 1951, where a ] inductee unsuccessfully attempted ] with multiple doses of warfarin in rodenticide and recovered fully after presenting to a hospital, and being treated with vitamin K (by then known as a specific antidote),<ref name="pmid13619027"/> studies began in the use of warfarin as a therapeutic anticoagulant. It was found to be generally superior to dicoumarol, and in 1954 was approved for medical use in humans. An early recipient of warfarin was US president ], who was prescribed the drug after having a heart attack in 1955.<ref name="pmid13619027"/> | |||
| === Mechanism of action === | |||
| The exact ] remained unknown until it was demonstrated, in 1978, that warfarin ] the enzyme ] and hence interferes with vitamin K metabolism.<ref name=Whitlon /> | |||
| Warfarin is one of several drugs often referred to as a "blood thinner"; this is not technically correct, as these drugs reduce coagulation of blood, increasing the ], without affecting the ] ("thickness") as such of blood.<ref>{{cite book|url=https://books.google.com/books?id=UtA8BAAAQBAJ&pg=PA138|isbn=978-0-19-997624-9|title=X-Ray Vision: The Evolution of Medical Imaging and Its Human Significance|date=28 November 2012|publisher=Oxford University Press|access-date=20 March 2023|archive-date=30 June 2023|archive-url=https://web.archive.org/web/20230630155034/https://books.google.com/books?id=UtA8BAAAQBAJ&pg=PA138|url-status=live}}</ref> | |||
| Warfarin inhibits the vitamin K-dependent synthesis of biologically active forms of the ] factors ], ], ] and ], as well as the regulatory factors protein C, protein S, and ].<ref name="Ansell">{{cite journal | vauthors = Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G | title = Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) | journal = Chest | volume = 133 | issue = 6 Suppl | pages = 160S–198S | date = June 2008 | pmid = 18574265 | doi = 10.1378/chest.08-0670 | s2cid = 12305488 }}</ref><ref>{{cite journal | vauthors = Freedman MD | title = Oral anticoagulants: pharmacodynamics, clinical indications and adverse effects | journal = Journal of Clinical Pharmacology | volume = 32 | issue = 3 | pages = 196–209 | date = March 1992 | pmid = 1564123 | doi = 10.1002/j.1552-4604.1992.tb03827.x | s2cid = 38963632 }}</ref> Other proteins not involved in blood clotting, such as ], or ], may also be affected. | |||
| A theory published in 2003 posits that ], ] and others conspired to use warfarin to poison the Soviet leader ]. Warfarin is tasteless and colorless, and produces symptoms similar to those that Stalin exhibited.<!--when? Before his death?--><ref>{{cite book |author=Naumov, Vladimir Pavlovich; Brent, Jonathan |title=Stalin's last crime: the plot against the Jewish doctors, 1948–1953 |publisher=HarperCollins |location=London |year=2003 |pages= |isbn=0-06-019524-X}}</ref> | |||
| The precursors of these factors require ] carboxylation of their ] residues to allow the coagulation factors to bind to ] surfaces inside blood vessels, on the vascular ]. The ] that carries out the carboxylation of glutamic acid is ]. The carboxylation reaction proceeds only if the carboxylase enzyme is able to convert a ] form of vitamin K (vitamin K hydroquinone) to vitamin K ] at the same time. The vitamin K epoxide is, in turn, recycled back to vitamin K and vitamin K ] by another enzyme, the ] (''VKOR''). Warfarin inhibits ''VKOR''<ref name=Whitlon>{{cite journal | vauthors = Whitlon DS, Sadowski JA, Suttie JW | title = Mechanism of coumarin action: significance of vitamin K epoxide reductase inhibition | journal = Biochemistry | volume = 17 | issue = 8 | pages = 1371–1377 | date = April 1978 | pmid = 646989 | doi = 10.1021/bi00601a003 }}</ref> (specifically the VKORC1 subunit<ref>{{cite journal | vauthors = Li T, Chang CY, Jin DY, Lin PJ, Khvorova A, Stafford DW | title = Identification of the gene for vitamin K epoxide reductase | journal = Nature | volume = 427 | issue = 6974 | pages = 541–544 | date = February 2004 | pmid = 14765195 | doi = 10.1038/nature02254 | s2cid = 4424554 | bibcode = 2004Natur.427..541L }}</ref><ref name="pmid14765194">{{cite journal | vauthors = Rost S, Fregin A, Ivaskevicius V, Conzelmann E, Hörtnagel K, Pelz HJ, Lappegard K, Seifried E, Scharrer I, Tuddenham EG, Müller CR, Strom TM, Oldenburg J | title = Mutations in VKORC1 cause warfarin resistance and multiple coagulation factor deficiency type 2 | journal = Nature | volume = 427 | issue = 6974 | pages = 537–541 | date = February 2004 | pmid = 14765194 | doi = 10.1038/nature02214 | s2cid = 4424197 | bibcode = 2004Natur.427..537R }}</ref>), thereby diminishing available vitamin K and vitamin K hydroquinone in the tissues, which decreases the carboxylation activity of the glutamyl carboxylase. When this occurs, the coagulation factors are no longer carboxylated at certain ] residues, and are incapable of binding to the endothelial surface of blood vessels, and are thus biologically inactive. As the body's stores of previously produced active factors degrade (over several days) and are replaced by inactive factors, the anticoagulation effect becomes apparent. The coagulation factors are produced, but have decreased functionality due to undercarboxylation; they are collectively referred to as PIVKAs (proteins induced vitamin K absence), and individual coagulation factors as PIVKA-''number'' (e.g., ]). | |||
| When warfarin is newly started, it may ''promote'' clot formation temporarily, because the level of proteins C and S are also dependent on vitamin K activity. Warfarin causes decline in protein C levels in first 36 hours. In addition, reduced levels of protein S lead to a reduction in activity of protein C (for which it is the co-factor), so reduces degradation of factor Va and factor VIIIa. Although loading doses of warfarin over 5 mg also produce a precipitous decline in factor VII, resulting in an initial prolongation of the INR, full antithrombotic effect does not take place until significant reduction in factor II occurs days later. The haemostasis system becomes temporarily biased towards thrombus formation, leading to a prothrombotic state. Thus, when warfarin is loaded rapidly at greater than 5 mg per day, to co-administering ], an anticoagulant that acts upon ] and helps reduce the risk of thrombosis, is beneficial, with warfarin therapy for four to five days, to have the benefit of anticoagulation from heparin until the full effect of warfarin has been achieved.<ref>{{cite journal | vauthors = Litin SC, Gastineau DA | title = Current concepts in anticoagulant therapy | journal = Mayo Clinic Proceedings | volume = 70 | issue = 3 | pages = 266–272 | date = March 1995 | pmid = 7861815 | doi = 10.4065/70.3.266 | doi-access = free | title-link=doi }}</ref><ref>{{cite journal | vauthors = Wittkowsky AK | title = Why warfarin and heparin need to overlap when treating acute venous thromboembolism | journal = Disease-a-Month | volume = 51 | issue = 2–3 | pages = 112–115 | year = 2005 | pmid = 15900262 | doi = 10.1016/j.disamonth.2005.03.005 }}</ref> | |||
| ==Use as a pesticide== | |||
| {{main|4-hydroxycoumarins}} | |||
| ] river in Steendorp, Belgium. The tube contains ], a second-generation ("super-warfarin") anticoagulant.]] | |||
| To this day, the so-called "coumarins" (4-hydroxycoumarin derivatives) are used as ]s for controlling ]s and ] in residential, industrial, and agricultural areas. Warfarin is both odorless and tasteless, and is effective when mixed with food ], because the ]s will return to the bait and continue to feed over a period of days until a lethal dose is accumulated (considered to be 1 mg/kg/day over about six days). It may also be mixed with ] and used as a ''tracking powder'', which accumulates on the animal's skin and fur, and is subsequently consumed during grooming. The {{LD50}} is 50–500 mg/kg. The ] value is 100 mg/m³ (warfarin; various species).<ref>{{cite web |url=http://www.cdc.gov/Niosh/idlh/81812.html |title=Documentation for Immediately Dangerous To Life or Health Concentrations (IDLHs): Warfarin |author=United States ] (OSHA) |date=16 August 1996 |publisher=] |accessdate=7 July 2008}}</ref> | |||
| === Pharmacogenomics === | |||
| The use of warfarin itself as a rat poison is now declining, because many rat populations have developed resistance to it, and poisons of considerably greater potency are now available. Other 4-hydroxycoumarins used as rodenticides include ] and ], which is sometimes referred to as "super-warfarin", because it is more potent, longer-acting, and effective even in rat and mouse populations that are resistant to warfarin. Unlike warfarin, which is readily excreted, newer anticoagulant poisons also ] in the liver and kidneys after ingestion.<ref name=NZToxins>{{cite book |title=Vertebrate pesticide toxicology manual (poisons) |author=Charles T. Eason |coauthors=Mark Wickstrom |year=2001 |publisher=] |chapter=2. Anticoagulant poisons |chapterurl=http://www.doc.govt.nz/upload/documents/science-and-technical/docts23b.pdf |pages=41–74 |isbn=0-478-22035-9 |accessdate=7 July 2008}}</ref> | |||
| Warfarin activity is determined partially by genetic factors. ] in two genes (''VKORC1'' and ''CYP2C9'') play a particularly large role in response to warfarin. | |||
| '']'' polymorphisms explain 30% of the dose variation between patients:<ref name="pmid15883587">{{cite journal | vauthors = Wadelius M, Chen LY, Downes K, Ghori J, Hunt S, Eriksson N, Wallerman O, Melhus H, Wadelius C, Bentley D, Deloukas P | title = Common VKORC1 and GGCX polymorphisms associated with warfarin dose | journal = The Pharmacogenomics Journal | volume = 5 | issue = 4 | pages = 262–270 | year = 2005 | pmid = 15883587 | doi = 10.1038/sj.tpj.6500313 | doi-access = | title-link=doi }}</ref> particular ]s make VKORC1 less susceptible to suppression by warfarin.<ref name="pmid14765194" /> There are two main haplotypes that explain 25% of variation: low-dose haplotype group (A) and a high-dose haplotype group (B).<ref name="pmid15930419">{{cite journal | vauthors = Rieder MJ, Reiner AP, Gage BF, Nickerson DA, Eby CS, McLeod HL, Blough DK, Thummel KE, Veenstra DL, Rettie AE | title = Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose | journal = The New England Journal of Medicine | volume = 352 | issue = 22 | pages = 2285–2293 | date = June 2005 | pmid = 15930419 | doi = 10.1056/NEJMoa044503 | doi-access = free | title-link=doi }}</ref> ''VKORC1'' polymorphisms explain why African Americans are on average relatively resistant to warfarin (higher proportion of group B ]s), while Asian Americans are generally more sensitive (higher proportion of group A haplotypes).<ref name="pmid15930419" /> Group A ''VKORC1'' polymorphisms lead to a more rapid achievement of a therapeutic INR, but also a shorter time to reach an INR over 4, which is associated with bleeding.<ref name="pmid18322281">{{cite journal | vauthors = Schwarz UI, Ritchie MD, Bradford Y, Li C, Dudek SM, Frye-Anderson A, Kim RB, Roden DM, Stein CM | title = Genetic determinants of response to warfarin during initial anticoagulation | journal = The New England Journal of Medicine | volume = 358 | issue = 10 | pages = 999–1008 | date = March 2008 | pmid = 18322281 | pmc = 3894627 | doi = 10.1056/NEJMoa0708078 | doi-access = free | title-link=doi }}</ref> | |||
| {{clear}} | |||
| '']'' polymorphisms explain 10% of the dose variation between patients,<ref name="pmid15883587" /> mainly among ] patients as these variants are rare in African American and most Asian populations.<ref name="pmid15714076">{{cite journal | vauthors = Sanderson S, Emery J, Higgins J | title = CYP2C9 gene variants, drug dose, and bleeding risk in warfarin-treated patients: a HuGEnet systematic review and meta-analysis | journal = Genetics in Medicine | volume = 7 | issue = 2 | pages = 97–104 | date = February 2005 | pmid = 15714076 | doi = 10.1097/01.GIM.0000153664.65759.CF | doi-access = | title-link=doi }}</ref> These ''CYP2C9'' polymorphisms do not influence time to effective INR as opposed to ''VKORC1'', but do shorten the time to ] > 4.<ref name="pmid18322281" /> | |||
| ==References== | |||
| {{Reflist|2}} | |||
| Despite the promise of ] testing in warfarin dosing, its use in clinical practice is controversial. In August 2009, the ] concluded, "the available evidence does not demonstrate that pharmacogenomic testing of ''CYP2C9'' or ''VKORC1'' ]s to predict warfarin responsiveness improves health outcomes in ] beneficiaries."<ref>{{cite web |url = https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=224&ver=15 <!-- http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=224&ver=15&NcaName=Pharmacogenomic+Testing+for+Warfarin+Response&NCDId=333&ncdver=1&IsPopup=y&bc=AAAAAAAAEAAA& --> |title = Decision Memo for Pharmacogenomic Testing for Warfarin Response (CAG-00400N) |vauthors = Jensen TS, Jacques LB, Ciccanti M, Long K, Eggleston L, Roche J |date = 3 August 2009 |publisher = Centers for Medicare and Medicaid Services |access-date = 14 April 2018 |url-status = live |archive-url = https://web.archive.org/web/20180414233940/https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=224&ver=15 |archive-date = 14 April 2018 }}</ref> A 2014 ] showed that using genotype-based dosing did not confer benefit in terms of time within therapeutic range, excessive anticoagulation (as defined by INR greater than 4), or a reduction in either major bleeding or thromboembolic events.<ref name=Stergiopoulos>{{cite journal | vauthors = Stergiopoulos K, Brown DL | title = Genotype-guided vs clinical dosing of warfarin and its analogues: meta-analysis of randomized clinical trials | journal = JAMA Internal Medicine | volume = 174 | issue = 8 | pages = 1330–1338 | date = August 2014 | pmid = 24935087 | doi = 10.1001/jamainternmed.2014.2368 | doi-access = | title-link=doi }}</ref> | |||
| ==External links== | |||
| * from the ] | |||
| * | |||
| == History == | |||
| {{Antithrombotics}} | |||
| In the early 1920s, an outbreak occurred of a previously unrecognized cattle disease in the ] and Canada. Cattle were ] after minor procedures, and on some occasions spontaneously.<ref name="Distillations"/> For example, 21 of 22 cows died after dehorning, and 12 of 25 bulls died after ]. All of these animals had bled to death.<ref name="Laurence 1973 23.4-23.5">{{cite book |title = Clinical Pharmacology |vauthors = Laurence DR, Kneebone P |year = 1973 |publisher = Churchill Livingstone |location = Edinburgh, London and New York |pages = 23.4–23.5 |isbn = 978-0-443-04990-3 |url = https://archive.org/details/clinicalpharmaco0000laur |url-access = registration }}</ref> | |||
| In 1921, ], a Canadian ] ], determined that the cattle were ingesting moldy ] made from ], and that this was functioning as a potent anticoagulant.<ref name="Distillations"/> Only spoiled hay made from sweet clover (grown in northern states of the US and in Canada since the turn of the century) produced the disease.<ref>{{cite journal |author = Schofield FW |title = Damaged sweet clover; the cause of a new disease in cattle simulating haemorrhagic septicemia and blackleg |journal = J Am Vet Med Assoc |year = 1924 |volume = 64 |pages = 553–6 }}</ref> Schofield separated good clover stalks and damaged clover stalks from the same hay mow, and fed each to a different rabbit. The rabbit that had ingested the good stalks remained well, but the rabbit that had ingested the damaged stalks died from a haemorrhagic illness. A duplicate experiment with a different sample of clover hay produced the same result.<ref name="Laurence 1973 23.4-23.5" /> In 1929, ] veterinarian Lee M. Roderick demonstrated that the condition was due to a lack of functioning prothrombin.<ref>{{cite journal |author = Roderick LM |year = 1931 |title = A problem in the coagulation of the blood; "sweet clover disease of the cattle" |journal = Am J Physiol |volume = 96 |issue = 2 |pages = 413–425 |doi = 10.1152/ajplegacy.1931.96.2.413 }}</ref> | |||
| {{good article}} | |||
| The identity of the anticoagulant substance in spoiled sweet clover remained a mystery until 1940. In 1933, ] and his laboratory of chemists working at the ] set out to isolate and characterize the haemorrhagic agent from the spoiled hay.<ref name="Distillations"/> Five years were needed before Link's student, Harold A. Campbell, recovered 6 mg of crystalline anticoagulant. Next, Link's student, Mark A. Stahmann, took over the project and initiated a large-scale extraction, isolating 1.8 g of recrystallized anticoagulant in about 4 months. This was enough material for Stahmann and Charles F. Huebner to check their results against Campbell's, and to thoroughly characterize the compound. Through degradation experiments, they established that the anticoagulant was 3,3'-methylenebis-(4-hydroxycoumarin), which they later named ]. They confirmed their results by synthesizing dicoumarol and proving in 1940 that it was identical to the naturally occurring agent.<ref>{{cite journal |vauthors = Stahmann MA, Huebner CF, Link KP |date = 1 April 1941 |title = Studies on the hemorrhagic sweet clover disease. V. Identification and synthesis of the hemorrhagic agent |journal = J Biol Chem |volume = 138 |pages = 513–27 |issue = 2 |doi = 10.1016/S0021-9258(18)51377-6 |doi-access = free | title-link = doi }}</ref> | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| Dicoumarol was a product of the plant molecule ] (not to be confused with Couma'''d'''in, a later tradename for warfarin). Coumarin is now known to be present in many plants, and produces the notably sweet smell of ] or hay and plants such as ]; in fact, the plant's high content of coumarin is responsible for the original common name of "sweet clover", which is named for its sweet smell, not its bitter taste.<ref name="Laurence 1973 23.4-23.5" /> They are present notably in ] (''Galium odoratum'', ]), and at lower levels in ], ], and various other species. The name coumarin comes via the French ''coumarou'' from ''kumarú'', the ] name for the tree of the ], which notably contains a high concentration of coumarin.<ref>{{cite web |title=Warfarin, Molecule of the Month for February 2011, by John Maher |url=https://www.chm.bris.ac.uk/motm/warfarin/ |access-date=20 December 2023 |website=www.chm.bris.ac.uk |archive-date=27 September 2023 |archive-url=https://web.archive.org/web/20230927151716/https://www.chm.bris.ac.uk/motm/warfarin/ |url-status=live }}</ref> However, coumarins themselves do not influence clotting or warfarin-like action, but must first be metabolized by various fungi into compounds such as ], then further (in the presence of naturally occurring ]) into dicoumarol, to have any anticoagulant properties. | |||
| ] | |||
| ] | |||
| Over the next few years, numerous similar chemicals (specifically 4-hydroxycoumarins with a large ] substituent at the '''3''' position) were found to have the same anticoagulant properties. The first drug in the class to be widely commercialized was dicoumarol itself, patented in 1941 and later used as a ]. Karl Link continued working on developing more potent coumarin-based anticoagulants for use as ], resulting in warfarin in 1948. The name "warfarin" stems from the acronym WARF, for ] + the ending "-arin" indicating its link with coumarin. Warfarin was first registered for use as a ] in the US in 1948, and was immediately popular. Although warfarin was developed by Link, the Wisconsin Alumni Research Foundation financially supported the research and was assigned the patent.<ref name="pmid13619027">{{cite journal | vauthors = Link KP | title = The discovery of dicumarol and its sequels | journal = Circulation | volume = 19 | issue = 1 | pages = 97–107 | date = January 1959 | pmid = 13619027 | doi = 10.1161/01.CIR.19.1.97 | doi-access = free | title-link=doi }}</ref> | |||
| ] | |||
| ] | |||
| After an incident in 1951, in which an army inductee attempted suicide with multiple doses of warfarin in rodenticide, but recovered fully after presenting to a naval hospital and being treated with vitamin K (by then known as a specific ]),<ref name="pmid13619027" /> studies began in the use of warfarin as a therapeutic anticoagulant.<ref name="Distillations">{{cite journal |vauthors=Rajagopalan R |title=A Study in Scarlet |url=https://www.sciencehistory.org/distillations/magazine/a-study-in-scarlet |journal=Distillations |date=2018 |volume=4 |issue=1 |pages=26–35 |access-date=27 June 2018 |archive-date=23 June 2019 |archive-url=https://web.archive.org/web/20190623094350/https://www.sciencehistory.org/distillations/magazine/a-study-in-scarlet |url-status=live }}</ref> It was found to be generally superior to dicoumarol, and in 1954, was approved for medical use in humans. An early recipient of warfarin was US President ], who was prescribed the drug after having a heart attack in 1955.<ref name="pmid13619027" /> | |||
| ] | |||
| ] | |||
| The exact ] remained unknown until it was demonstrated, in 1978, that warfarin ] the enzyme vitamin K epoxide reductase, and hence interferes with vitamin K metabolism.<ref name=Whitlon /> | |||
| ] | |||
| ] | |||
| ] and I. V. Khrustalyov are thought to have conspired to use warfarin to poison Soviet leader ]. Warfarin is tasteless and colourless, and produces symptoms similar to those that Stalin exhibited.<!-- when? Before his death? --><ref>{{cite book | vauthors = Naumov VP, Brent J |title = Stalin's last crime: the plot against the Jewish doctors, 1948–1953 |publisher = HarperCollins |location = London |year = 2003 |isbn = 978-0-06-019524-3 }}</ref> | |||
| ] | |||
| ] | |||
| ===Occupational safety=== | |||
| ] | |||
| Warfarin used for pest control is a hazardous substance harmful to health. People can be exposed to warfarin in the workplace by breathing it in, swallowing it, skin absorption, and eye contact. The ] has set the legal limit (]) for warfarin exposure in the workplace as 0.1 mg/m<sup>3</sup> over an 8-hour workday. The ] has set a ] of 0.1 mg/m<sup>3</sup> over an 8-hour workday. At levels of 100 mg/m<sup>3</sup>, warfarin is ].<ref>{{cite web |title = CDC – NIOSH Pocket Guide to Chemical Hazards – Warfarin |url = https://www.cdc.gov/niosh/npg/npgd0665.html |website = www.cdc.gov |access-date = 27 November 2015 |url-status = live |archive-url = https://web.archive.org/web/20151208093728/http://www.cdc.gov/niosh/npg/npgd0665.html |archive-date = 8 December 2015 }}</ref> | |||
| ] | |||
| ] | |||
| It is classified as an ] in the United States as defined in Section 302 of the U.S. ] (42 U.S.C. 11002), and is subject to strict reporting requirements by facilities which produce, store, or use it in significant quantities.<ref name="gov-right-know">{{cite web |publisher = ] |title = 40 C.F.R.: Appendix A to Part 355—The List of Extremely Hazardous Substances and Their Threshold Planning Quantities |url = https://www.ecfr.gov/current/title-40/chapter-I/subchapter-J/part-355/appendix-Appendix%20A%20to%20Part%20355 |edition = 21 August 2023 |access-date = 22 August 2023 |archive-date = 9 January 2023 |archive-url = https://web.archive.org/web/20230109114558/https://www.ecfr.gov/current/title-40/chapter-I/subchapter-J/part-355/appendix-Appendix%20A%20to%20Part%20355 |url-status = live }}</ref> | |||
| ] | |||
| ] | |||
| == Society and culture == | |||
| ] | |||
| The name "warfarin" is derived from the acronym for "Wisconsin Alumni Research Foundation", plus "-arin", indicating its link with coumarin. Warfarin is a derivative of dicoumarol, an anticoagulant originally discovered in spoiled sweet clover. Dicoumarol, in turn, is from coumarin, a sweet-smelling but coagulation-inactive chemical found in "sweet" clover and ] (also known as ''cumaru'' from which coumarin's name derives). | |||
| ] | |||
| ] | |||
| === Brand names === | |||
| ] | |||
| Warfarin as a drug is marketed under many brand and generic names, including Aldocumar, Anasmol, Anticoag, Befarin, Cavamed, Cicoxil, Circuvit, Cofarin, Coumadin, Coumadine, Cumar, Farin, Foley, Haemofarin, Jantoven, Kovar, Lawarin, Maforan, Marevan, Marfarin, Marivanil, Martefarin, Morfarin, Orfarin, Panwarfin, Scheme, Simarc, Varfarin, Varfarins, Varfine, Waran, Warcok, Warf, Warfareks, Warfarin, Warfarina, Warfarine, Warfarinum, Warfen, Warfin, Warik, Warin, Warlin, and Zyfarin.<ref name=brands>{{cite web |title = Warfarin international brands |url = https://www.drugs.com/international/warfarin.html |publisher = Drugs.com |url-status = live|archive-url = https://web.archive.org/web/20170405172058/https://www.drugs.com/international/warfarin.html|archive-date=5 April 2017|date =12 February 2023}}</ref> | |||
| ] | |||
| ] | |||
| == Veterinary use == | |||
| ] | |||
| Warfarin is used as a ] and other pests.<ref name=poison>{{cite journal | vauthors = Lim GB | title = Milestone 2: Warfarin: from rat poison to clinical use | journal = Nature Reviews. Cardiology | date = December 2017 | pmid = 29238065 | doi = 10.1038/nrcardio.2017.172 | doi-access = free }}</ref><ref name=NZToxins/> | |||
| ] | |||
| === Pest control === | |||
| Warfarin was introduced as a ], only later finding medical uses; in both cases it was used as an anticoagulant.<ref name=poison/> The use of warfarin itself as a rat poison is declining, because many rat populations have developed resistance to it,<ref name="RRAC-anticoags"/> and poisons of considerably greater potency have become available. However, {{As of|2023|lc=y}} warfarin continued to be considered a valuable tool for rodent control which minimised risk to other species.<ref>{{cite web| title=Warfarin - A valuable tool for successful rodent control whilst minimising risk to non-target species| publisher=National Pest Technicians Association| date=21 October 2019| url=https://www.npta.org.uk/warfarin-a-valuable-tool-for-successful-rodent-control-whilst-minimising-risk-to-non-target-species/| access-date=18 February 2023| archive-date=17 February 2023| archive-url=https://web.archive.org/web/20230217044318/https://www.npta.org.uk/warfarin-a-valuable-tool-for-successful-rodent-control-whilst-minimising-risk-to-non-target-species/| url-status=live}}</ref> | |||
| ====Rodents==== | |||
| {{Main|4-hydroxycoumarins}} | |||
| ] River in ]: The tube contains ], a second-generation ("super-warfarin") anticoagulant.]] | |||
| Coumarins (4-hydroxycoumarin derivatives) are used as ]s for controlling ]s and ] in residential, industrial, and agricultural areas. Warfarin is both odorless and tasteless, and is effective when mixed with food ], because the ]s will return to the bait and continue to feed over a period of days until a lethal dose is accumulated (considered to be 1 mg/kg/day over about six days). It may also be mixed with ] and used as a tracking powder, which accumulates on the animal's skin and fur, and is subsequently consumed during grooming. The {{LD50}} for warfarin is 50–100{{nbsp}}mg/kg for a single dose, after 5–7 days.<ref name="RRAC-anticoags">{{cite web |url=http://croplife.org/wp-content/uploads/2015/10/Rodenticide-Resistance-Strategy_Sept2015v3.pdf |publisher=] |website=] |vauthors=Endepols S, Buckle A, Eason C, Pelz HJ, Meyer A, Berny P, Baert K, Prescott C |place=] |date=September 2015 |pages=1–29 |title=RRAC guidelines on Anticoagulant Rodenticide Resistance Management |access-date=23 October 2021 |archive-date=4 November 2021 |archive-url=https://web.archive.org/web/20211104132536/https://croplife.org/wp-content/uploads/2015/10/Rodenticide-Resistance-Strategy_Sept2015v3.pdf |url-status=live }}</ref> {{LD50}} 1{{nbsp}}mg/kg for repeated daily doses for 5 days, after 5–8 days.<ref name="RRAC-anticoags" /> The ] value is 100 mg/m<sup>3</sup> (warfarin; various species).<ref>{{cite web |url = https://www.cdc.gov/niosh/idlh/81812.html |title = Documentation for Immediately Dangerous To Life or Health Concentrations (IDLHs): Warfarin |author = United States ] (OSHA) |date = 16 August 1996 |publisher = ] |access-date = 7 July 2008 |url-status = live |archive-url = https://web.archive.org/web/20080726031247/http://www.cdc.gov/niosh/idlh/81812.html |archive-date = 26 July 2008 }}</ref> | |||
| Resistance to warfarin as a poison has developed in many rat populations due to an ] ] on chromosome 1 in ]s.<ref name="RRAC-anticoags" /> This has ] several times around the world.<ref name="RRAC-anticoags" /> Other 4-hydroxycoumarins used as rodenticides include ] and ], which is sometimes referred to as "super-warfarin", because it is more potent, longer-acting, and effective even in rat and mouse populations that are resistant to warfarin. Unlike warfarin, which is readily excreted, newer anticoagulant poisons also ] in the ] and ]s after ingestion.<ref name=NZToxins>{{cite book |title = Vertebrate pesticide toxicology manual (poisons) |vauthors = Eason CT, Wickstrom M |year = 2001 |publisher = ] |chapter = 2. Anticoagulant poisons |chapter-url=http://www.doc.govt.nz/upload/documents/science-and-technical/docts23b.pdf |pages = 41–74 |isbn = 978-0-478-22035-3 |url-status = live |archive-url = https://web.archive.org/web/20081017022833/http://www.doc.govt.nz/upload/documents/science-and-technical/docts23b.pdf |archive-date = 17 October 2008 }}</ref> However, such rodenticides may also accumulate in ] and other animals that eat the poisoned rodents or baits.<ref>{{cite news |title = Killing rats is killing birds |vauthors = Lovett RA |date = 14 November 2012 |access-date = 5 April 2015 |url = http://www.nature.com/news/killing-rats-is-killing-birds-1.11824 |journal = ] |doi = 10.1038/nature.2012.11824 |url-status = live |archive-url = https://web.archive.org/web/20150426133605/http://www.nature.com/news/killing-rats-is-killing-birds-1.11824 |archive-date = 26 April 2015 }}</ref> | |||
| ==== Vampire bats ==== | |||
| Warfarin is used to cull populations of ]s, in which ] is often prevalent, in areas where ] is a concern.<ref name="Johnson 2014">{{cite journal | vauthors = Johnson N, Aréchiga-Ceballos N, Aguilar-Setien A | title = Vampire bat rabies: ecology, epidemiology and control | journal = Viruses | volume = 6 | issue = 5 | pages = 1911–1928 | date = April 2014 | pmid = 24784570 | pmc = 4036541 | doi = 10.3390/v6051911 | doi-access = free | title-link=doi }}</ref> Vampire bats are captured with ]s and coated with a combination of ] and warfarin. The bat returns to its roost and other members of the roost become poisoned as well by ingesting the warfarin after ].<ref name="Johnson 2014" /> Suspected vampire bat roosts may also be coated in the warfarin solution, though this kills other bat species and remains in the environment for years.<ref name="Johnson 2014" /> The efficacy of killing vampire bats to reduce rabies transmission is questionable; a study in ] showed that culling programs did not lead to lower transmission rates of ] to livestock and humans.<ref name="Streicker 2012">{{cite journal | vauthors = Streicker DG, Recuenco S, Valderrama W, Gomez Benavides J, Vargas I, Pacheco V, Condori Condori RE, Montgomery J, Rupprecht CE, Rohani P, Altizer S | title = Ecological and anthropogenic drivers of rabies exposure in vampire bats: implications for transmission and control | journal = Proceedings. Biological Sciences | volume = 279 | issue = 1742 | pages = 3384–3392 | date = September 2012 | pmid = 22696521 | pmc = 3396893 | doi = 10.1098/rspb.2012.0538 }}</ref> | |||
| === Brand names === | |||
| Warfarin as a pest control poison is marketed under many brand and generic names, including Cov-R-Tox, Co-Rax, d-Con, Dethmor, Killgerm Sewercide, Mar-Fin, Rattunal, Rax, Rodex, Rodex Blox, Rosex, Sakarat, Sewarin, Solfarin, Sorex Warfarin, Tox-Hid, Warf, warfarin, and Warfarat. Warfarin is called coumafene in France, zoocoumarin in the Netherlands and Russia, and coumarin in Japan.<ref name=brands2>{{cite web | title=Pesticide Information Profiles: WARFARIN | website=EXTOXNET Extension Toxicology Network | url=http://extoxnet.orst.edu/pips/warfarin.htm | date=September 1995 | access-date=18 February 2023 | archive-date=10 June 2023 | archive-url=https://web.archive.org/web/20230610174038/http://extoxnet.orst.edu/pips/warfarin.htm | url-status=live }}</ref><ref name=brands3>{{cite web | title=Rat poison product list | website=The Barn Owl Trust | date=22 September 2021 | url=https://www.barnowltrust.org.uk/hazards-solutions/rodenticides/rat-poison-product-list/ | access-date=18 February 2023 | archive-date=18 February 2023 | archive-url=https://web.archive.org/web/20230218154554/https://www.barnowltrust.org.uk/hazards-solutions/rodenticides/rat-poison-product-list/ | url-status=live }}</ref> | |||
| == References == | |||
| {{Reflist}} | |||
| == Further reading == | |||
| * {{cite book | title=Medical Genetics Summaries | chapter=Warfarin Therapy and VKORC1 and CYP Genotype | chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK84174/ | veditors=Pratt VM, McLeod HL, Rubinstein WS, Scott SA, Dean LC, Kattman BL, Malheiro AJ | display-editors=6 | publisher=] (NCBI) | year=2012 | pmid=28520347 | id=Bookshelf ID: NBK84174 | vauthors=Dean L | url=https://www.ncbi.nlm.nih.gov/books/NBK61999/ }} | |||
| == External links == | |||
| * {{PPDB|681}} | |||
| {{clear}} | |||
| {{Antithrombotics}} | |||
| {{rodenticides}} | |||
| {{Portal bar | Medicine}} | |||
| {{Authority control}} | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
| ] | |||
Latest revision as of 17:15, 5 January 2025
Anticoagulant medication "Coumadin" redirects here. For the class of compounds known as "coumadins", see Coumadins. For the natural compound, see Coumarin. "Waran" redirects here. For the Polish Armored Personnel Carrier, see Waran (armored personnel carrier).Pharmaceutical compound
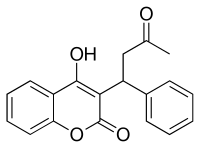 | |
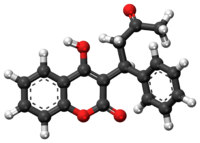 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈwɔːrfərɪn/ |
| Trade names | Coumadin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682277 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 79–100% (by mouth) |
| Protein binding | 99% |
| Metabolism | Liver: CYP2C9, 2C19, 2C8, 2C18, 1A2 and 3A4 |
| Elimination half-life | 1 week (active half-life is 20-60 hours) |
| Excretion | Kidney (92%) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank |
|
| ChemSpider | |
| UNII |
|
| KEGG | |
| ChEBI |
|
| ChEMBL |
|
| PDB ligand | |
| ECHA InfoCard | 100.001.253 |
| Chemical and physical data | |
| Formula | C19H16O4 |
| Molar mass | 308.333 g·mol |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (what is this?) (verify) | |
Warfarin, sold under the brand name Coumadin among others, is an anticoagulant medication. While the drug is described as a "blood thinner", it does not reduce viscosity but rather prevents blood clots (thrombus) from forming (coagulating). Accordingly, it is commonly used to prevent deep vein thrombosis and pulmonary embolism, and to protect against stroke in people who have atrial fibrillation, valvular heart disease, or artificial heart valves. Warfarin may sometimes be prescribed following ST-segment elevation myocardial infarctions (STEMI) and orthopedic surgery. It is usually taken by mouth, but may also be administered intravenously. It is a vitamin K antagonist.
The common side effect, a natural consequence of reduced clotting, is bleeding. Less common side effects may include areas of tissue damage, and purple toes syndrome. Use is not recommended during pregnancy. The effects of warfarin are typically monitored by checking prothrombin time (INR) every one to four weeks. Many other medications and dietary factors can interact with warfarin, either increasing or decreasing its effectiveness. The effects of warfarin may be reversed with phytomenadione (vitamin K1), fresh frozen plasma, or prothrombin complex concentrate.
Warfarin decreases blood clotting by blocking vitamin K epoxide reductase, an enzyme that reactivates vitamin K1. Without sufficient active vitamin K1, the plasma concentrations of clotting factors II, VII, IX, and X are reduced and thus have decreased clotting ability. The anticlotting protein C and protein S are also inhibited, but to a lesser degree. Despite being labeled a vitamin K antagonist, warfarin does not antagonize the action of vitamin K1, but rather antagonizes vitamin K1 recycling, depleting active vitamin K1. A few days are required for full effect to occur, and these effects can last for up to five days. Because the mechanism involves enzymes such as VKORC1, patients on warfarin with polymorphisms of the enzymes may require adjustments in therapy if the genetic variant that they have is more readily inhibited by warfarin, thus requiring lower doses.
Warfarin first came into large-scale commercial use in 1948 as a rat poison. It was formally approved as a medication to treat blood clots in humans by the U.S. Food and Drug Administration in 1954. In 1955, warfarin's reputation as a safe and acceptable treatment for coronary artery disease, arterial plaques, and ischemic strokes was bolstered when President Dwight D. Eisenhower was treated with warfarin following a highly publicized heart attack. It is on the World Health Organization's List of Essential Medicines. Warfarin is available as a generic medication and is sold under many brand names. In 2022, it was the 85th most commonly prescribed medication in the United States, with more than 8 million prescriptions.
Medical uses
Warfarin is indicated for the prophylaxis and treatment of venous thrombosis and its extension, pulmonary embolism; prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation and/or cardiac valve replacement; and reduction in the risk of death, recurrent myocardial infarction, and thromboembolic events such as stroke or systemic embolization after myocardial infarction.
Warfarin is used to decrease the tendency for thrombosis, or as secondary prophylaxis (prevention of further episodes) in those individuals who have already formed a blood clot (thrombus). Warfarin treatment can help prevent formation of future blood clots and help reduce the risk of embolism (migration of a thrombus to a spot where it blocks blood supply to a vital organ).
Warfarin is best suited for anticoagulation (clot formation inhibition) in areas of slowly running blood (such as in veins and the pooled blood behind artificial and natural valves), and in blood pooled in dysfunctional cardiac atria. Thus, common clinical indications for warfarin use are atrial fibrillation, the presence of artificial heart valves, deep venous thrombosis, and pulmonary embolism (where the embolized clots first form in veins). Warfarin is also used in antiphospholipid syndrome. It has been used occasionally after heart attacks (myocardial infarctions), but is far less effective at preventing new thromboses in coronary arteries. Prevention of clotting in arteries is usually undertaken with antiplatelet drugs, which act by a different mechanism from warfarin (which normally has no effect on platelet function). It can be used to treat people following ischemic strokes due to atrial fibrillation, though direct oral anticoagulants (DOACs) may offer greater benefits.
Dosing
Dosing of warfarin is complicated because it is known to interact with many commonly used medications and certain foods. These interactions may enhance or reduce warfarin's anticoagulation effect. To optimize the therapeutic effect without risking dangerous side effects such as bleeding, close monitoring of the degree of anticoagulation is required by a blood test measuring an prothrombin time (INR). During the initial stage of treatment, INR is checked daily; intervals between tests can be lengthened if the patient manages stable therapeutic INR levels on an unchanged warfarin dose. Newer point-of-care testing is available and has increased the ease of INR testing in the outpatient setting. Instead of a blood draw, the point-of-care test involves a simple finger prick.
Maintenance dose

Recommendations by many national bodies, including the American College of Chest Physicians, have been distilled to help manage dose adjustments.
The maintenance dose of warfarin can fluctuate significantly depending on the amount of vitamin K1 in the diet. Keeping vitamin K1 intake at a stable level can prevent these fluctuations. Leafy green vegetables tend to contain higher amounts of vitamin K1. Green parts of members of the family Apiaceae, such as parsley, cilantro, and dill are extremely rich sources of vitamin K; cruciferous vegetables such as cabbage and broccoli, as well as the darker varieties of lettuces and other leafy greens, are also relatively high in vitamin K1. Green vegetables such as peas and green beans do not have such high amounts of vitamin K1 as leafy greens. Certain vegetable oils have high amounts of vitamin K1. Foods low in vitamin K1 include roots, bulbs, tubers, and most fruits and fruit juices. Cereals, grains, and other milled products are also low in vitamin K1.
Several studies reported that the maintenance dose can be predicted based on various clinical data.
Self-testing
Main article: INR self-monitoring
Anticoagulation with warfarin can also be monitored by patients at home. International guidelines on home testing were published in 2005. The guidelines stated:
The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently available self-testing/self-management devices give INR results that are comparable with those obtained in laboratory testing.
A 2006 systematic review and meta-analysis of 14 randomized trials showed home testing led to a reduced incidence of complications (thrombosis and major bleeding), and improved the time in the therapeutic range.
Alternative anticoagulants
In some countries, other coumarins are used instead of warfarin, such as acenocoumarol and phenprocoumon. These have a shorter (acenocoumarol) or longer (phenprocoumon) half-life, and are not completely interchangeable with warfarin. Several types of anticoagulant drugs offering the efficacy of warfarin without a need for monitoring, such as dabigatran, apixaban, edoxaban, and rivaroxaban, have been approved in a number of countries for classical warfarin uses. Complementing these drugs are reversal agents available for dabigatran (idarucizumab), and for apixaban, and rivaroxaban (andexanet alfa). Andexanet alfa is suggested for edoxaban, but use of it is considered off label due to limited evidence. A reversal agent for dabigatran, apixaban, edoxaban, and rivaroxaban is in development (ciraparantag).
Contraindications
All anticoagulants are generally contraindicated in situations in which the reduction in clotting that they cause might lead to serious and potentially life-threatening bleeds. This includes people with active bleeding conditions (such as gastrointestinal ulcers), or disease states with increased risk of bleeding (e.g., low platelets, severe liver disease, uncontrolled hypertension). For patients undergoing surgery, treatment with anticoagulants is generally suspended. Similarly, spinal and lumbar puncture (e.g., spinal injections, epidurals, etc.) carry increased risk, so treatment is suspended prior to these procedures.
Warfarin should not be given to people with heparin-induced thrombocytopenia until platelet count has improved or normalised. Warfarin is usually best avoided in people with protein C or protein S deficiency, as these thrombophilic conditions increase the risk of skin necrosis, which is a rare but serious side effect associated with warfarin.
Pregnancy
Further information: Fetal warfarin syndrome and Anticoagulation in pregnancyWarfarin is contraindicated in pregnancy, as it passes through the placental barrier and may cause bleeding in the fetus; warfarin use during pregnancy is commonly associated with spontaneous abortion, stillbirth, neonatal death, and preterm birth. Coumarins (such as warfarin) are also teratogens, that is, they cause birth defects; the incidence of birth defects in infants exposed to warfarin in utero appears to be around 5%, although higher figures (up to 30%) have been reported in some studies. Depending on when exposure occurs during pregnancy, two distinct combinations of congenital abnormalities can arise.
First trimester of pregnancy
Usually, warfarin is avoided in the first trimester, and a low-molecular-weight heparin such as enoxaparin is substituted. With heparin, risks of maternal haemorrhage and other complications are still increased, but heparins do not cross the placental barrier, so do not cause birth defects. Various solutions exist for the time around delivery.
When warfarin (or another 4-hydroxycoumarin derivative) is given during the first trimester—particularly between the sixth and ninth weeks of pregnancy—a constellation of birth defects known variously as fetal warfarin syndrome (FWS), warfarin embryopathy, or coumarin embryopathy can occur. FWS is characterized mainly by skeletal abnormalities, which include nasal hypoplasia, a depressed or narrowed nasal bridge, scoliosis, and calcifications in the vertebral column, femur, and heel bone, which show a peculiar stippled appearance on X-rays. Limb abnormalities, such as brachydactyly (unusually short fingers and toes) or underdeveloped extremities, can also occur. Common nonskeletal features of FWS include low birth weight and developmental disabilities.
Second trimester and later
Warfarin administration in the second and third trimesters is much less commonly associated with birth defects, and when they do occur, are considerably different from FWS. The most common congenital abnormalities associated with warfarin use in late pregnancy are central nervous system disorders, including spasticity and seizures, and eye defects. Because of such later pregnancy birth defects, anticoagulation with warfarin poses a problem in pregnant women requiring warfarin for vital indications, such as stroke prevention in those with artificial heart valves.
Warfarin may be used in lactating women who wish to breastfeed their infants. Available data does not suggest that warfarin crosses into the breast milk. Similarly, INR levels should be checked to avoid adverse effects.
Adverse effects
Bleeding
The only common side effect of warfarin is hemorrhage. The risk of severe bleeding is small but definite (a typical yearly rate of 1–3% has been reported), and any benefit needs to outweigh this risk when warfarin is considered. All types of bleeding occur more commonly, but the most severe ones are those involving the brain (intracerebral hemorrhage/hemorrhagic stroke) and the spinal cord. Risk of bleeding is increased if the INR is out of range (due to accidental or deliberate overdose or due to interactions). This risk increases greatly once the INR exceeds 4.5.
Several risk scores exist to predict bleeding in people using warfarin and similar anticoagulants. A commonly used score (HAS-BLED) includes known predictors of warfarin-related bleeding: uncontrolled high blood pressure (H), abnormal kidney function (A), previous stroke (S), known previous bleeding condition (B), previous labile INR when on anticoagulation (L), elderly as defined by age over 65 (E), and drugs associated with bleeding (e.g., aspirin) or alcohol misuse (D). While their use is recommended in clinical practice guidelines, they are only moderately effective in predicting bleeding risk and do not perform well in predicting hemorrhagic stroke. Bleeding risk may be increased in people on hemodialysis. Another score used to assess bleeding risk on anticoagulation, specifically Warfarin or Coumadin, is the ATRIA score, which uses a weighted additive scale of clinical findings to determine bleeding risk stratification. The risks of bleeding are increased further when warfarin is combined with antiplatelet drugs such as clopidogrel, aspirin, or nonsteroidal anti-inflammatory drugs.
Warfarin necrosis
Main article: Warfarin necrosisA rare but serious complication resulting from treatment with warfarin is warfarin necrosis, which occurs more frequently shortly after commencing treatment in patients with a deficiency of protein C, an innate anticoagulant that, like the procoagulant factors whose synthesis warfarin inhibits, requires vitamin K-dependent carboxylation for its activity. Since warfarin initially decreases protein C levels faster than the coagulation factors, it can paradoxically increase the blood's tendency to coagulate when treatment is first begun (many patients when starting on warfarin are given heparin in parallel to combat this), leading to massive thrombosis with skin necrosis and gangrene of limbs. Its natural counterpart, purpura fulminans, occurs in children who are homozygous for certain protein C mutations.
Osteoporosis
After initial reports that warfarin could reduce bone mineral density, several studies demonstrated a link between warfarin use and osteoporosis-related fracture. A 1999 study in 572 women taking warfarin for deep venous thrombosis, risk of vertebral fracture and rib fracture was increased; other fracture types did not occur more commonly. A 2002 study looking at a randomly selected selection of 1,523 patients with osteoporotic fracture found no increased exposure to anticoagulants compared to controls, and neither did stratification of the duration of anticoagulation reveal a trend towards fracture.
A 2006 retrospective study of 14,564 Medicare recipients showed that warfarin use for more than one year was linked with a 60% increased risk of osteoporosis-related fracture in men, but no association in women was seen. The mechanism was thought to be a combination of reduced intake of vitamin K (a vitamin necessary for bone health) and inhibition by warfarin of vitamin K-mediated carboxylation of certain bone proteins, rendering them nonfunctional.
Purple toe syndrome
See also: Blue toe syndromeAnother rare complication that may occur early during warfarin treatment (usually within 3 to 8 weeks of commencement) is purple toe syndrome. This condition is thought to result from small deposits of cholesterol breaking loose and causing embolisms in blood vessels in the skin of the feet, which causes a blueish-purple colour and may be painful.
It is typically thought to affect the big toe, but it affects other parts of the feet, as well, including the bottom of the foot (plantar surface). The occurrence of purple toe syndrome may require discontinuation of warfarin.
Calcification
Several studies have also implicated warfarin use in valvular and vascular calcification. No specific treatment is available, but some modalities are under investigation.
Overdose
The major side effect of warfarin use is bleeding. Risk of bleeding is increased if the INR is out of range (due to accidental or deliberate overdose or due to interactions). Many drug interactions can increase the effect of warfarin, also causing an overdose.
In patients with supratherapeutic INR but INR less than 10 and no bleeding, it is enough to lower the dose or omit a dose, monitor the INR and resume warfarin at an adjusted lower dose when the target INR is reached. For people who need rapid reversal of warfarin – such as due to serious bleeding – or who need emergency surgery, the effects of warfarin can be reversed with vitamin K, prothrombin complex concentrate (PCC), or fresh frozen plasma (FFP). Generally, four-factor PCC can be given more quickly than FFP, the amount needed is a smaller volume of fluid than FFP, and does not require ABO blood typing. Administration of PCCs results in rapid hemostasis, similar to that of FFP, namely, with comparable rates of thromboembolic events, but with reduced rates of volume overload. Blood products should not be routinely used to reverse warfarin overdose, when vitamin K could work alone. While PCC has been found in lab tests to be better than FFP, when rapid reversal is needed, as of 2018, whether a difference in outcomes such as death or disability exists is unclear.
When warfarin is being given and INR is in therapeutic range, simple discontinuation of the drug for five days is usually enough to reverse the effect and cause INR to drop below 1.5.
| Supratherapeutic INR but INR < 4.5, no bleeding |
|
|---|---|
| INR 4.5-10, no bleeding |
|
| INR >10.0, no bleeding |
|
| Minor bleeding, any elevated INR: |
|
| Major bleeding, any elevated INR |
May also consider supplementation with fresh frozen plasma (FFP) or recombinant factor VIIa |
| Life-threatening bleeding and elevated INR: |
|
Interactions
Warfarin interacts with many commonly used drugs, and the metabolism of warfarin varies greatly between patients. Some foods have also been reported to interact with warfarin. Apart from the metabolic interactions, highly protein bound drugs can displace warfarin from serum albumin and cause an increase in the INR. This makes finding the correct dosage difficult, and accentuates the need of monitoring; when initiating a medication that is known to interact with warfarin (e.g., simvastatin), INR checks are increased or dosages adjusted until a new ideal dosage is found.
When taken with nonsteroidal anti-inflammatory drugs (NSAIDs), warfarin increases the risk for gastrointestinal bleeding. This increased risk is due to the antiplatelet effect of NSAIDs and possible damage to the gastrointestinal mucosa.
Many commonly used antibiotics, such as metronidazole or the macrolides, greatly increase the effect of warfarin by reducing the metabolism of warfarin in the body. Other broad-spectrum antibiotics can reduce the amount of the normal bacterial flora in the bowel, which make significant quantities of vitamin K1, thus potentiating the effect of warfarin. In addition, food that contains large quantities of vitamin K1 will reduce the warfarin effect. Thyroid activity also appears to influence warfarin dosing requirements; hypothyroidism (decreased thyroid function) makes people less responsive to warfarin treatment, while hyperthyroidism (overactive thyroid) boosts the anticoagulant effect. Several mechanisms have been proposed for this effect, including changes in the rate of breakdown of clotting factors and changes in the metabolism of warfarin.
Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR, and thus increase the risk of bleeding. The U.S. Food and Drug Administration (FDA) product insert on warfarin states that alcohol should be avoided. The Cleveland Clinic suggests that when taking warfarin one should not drink more than "one beer, 6 oz of wine, or one shot of alcohol per day".
Warfarin also interacts with many herbs and spices, some used in food (such as ginger and garlic) and others used purely for medicinal purposes (such as ginseng and Ginkgo biloba). All may increase bleeding and bruising in people taking warfarin; similar effects have been reported with borage (starflower) oil. St. John's wort, sometimes recommended to help with mild to moderate depression, reduces the effectiveness of a given dose of warfarin; it induces the enzymes that break down warfarin in the body, causing a reduced anticoagulant effect.
Between 2003 and 2004, the UK Committee on Safety of Medicines received several reports of increased INR and risk of haemorrhage in people taking warfarin and cranberry juice. Data establishing a causal relationship are still lacking, and a 2006 review found no cases of this interaction reported to the USFDA; nevertheless, several authors have recommended that both doctors and patients be made aware of its possibility. The mechanism behind the interaction is still unclear.
Chemistry

X-ray crystallographic studies of warfarin show that it exists in tautomeric form, as the cyclic hemiketal, which is formed from the 4-hydroxycoumarin and the ketone in the 3-position substituent. However, the existence of many 4-hydroxycoumadin anticoagulants (for example phenprocoumon) that possess no ketone group in the 3-substituent to form such a structure, suggests that the hemiketal must tautomerise to the 4-hydroxy form in order for warfarin to be active.
Stereochemistry
Warfarin contains a stereocenter and consists of two enantiomers. This is a racemate, i.e., a 1: 1 mixture of ( R ) – and the ( S ) – form:
| Enantiomers of warfarin | |
|---|---|
 CAS Number: 5543-58-8 |
 CAS Number: 5543-57-7 |
Pharmacology

Pharmacokinetics
Warfarin consists of a racemic mixture of two active enantiomers—R- and S- forms—each of which is cleared by different pathways. S-warfarin is two to five times more potent than the R-isomer in producing an anticoagulant response. Both the enantiomers of warfarin undergo CYP-mediated metabolism by many different CYPs to form 3',4',6,7,8 and 10-hydroxy warfarin metabolites, major being 7-OH warfarin formed from S-warfarin by CYP2C9 and 10-OH warfarin from R-warfarin by CYP3A4.
Warfarin is slower-acting than the common anticoagulant heparin, though it has a number of advantages. Heparin must be given by injection, whereas warfarin is available orally. Warfarin has a long half-life and need only be given once a day. Heparin can also cause a prothrombotic condition, heparin-induced thrombocytopenia (an antibody-mediated decrease in platelet levels), which increases the risk for thrombosis. It takes several days for warfarin to reach the therapeutic effect, since the circulating coagulation factors are not affected by the drug (thrombin has a half-life time of days). Warfarin's long half-life means that it remains effective for several days after it is stopped. Furthermore, if given initially without additional anticoagulant cover, it can increase thrombosis risk (see below).
Mechanism of action
Warfarin is one of several drugs often referred to as a "blood thinner"; this is not technically correct, as these drugs reduce coagulation of blood, increasing the clotting time, without affecting the viscosity ("thickness") as such of blood.
Warfarin inhibits the vitamin K-dependent synthesis of biologically active forms of the clotting factors II, VII, IX and X, as well as the regulatory factors protein C, protein S, and protein Z. Other proteins not involved in blood clotting, such as osteocalcin, or matrix Gla protein, may also be affected. The precursors of these factors require gamma carboxylation of their glutamic acid residues to allow the coagulation factors to bind to phospholipid surfaces inside blood vessels, on the vascular endothelium. The enzyme that carries out the carboxylation of glutamic acid is gamma-glutamyl carboxylase. The carboxylation reaction proceeds only if the carboxylase enzyme is able to convert a reduced form of vitamin K (vitamin K hydroquinone) to vitamin K epoxide at the same time. The vitamin K epoxide is, in turn, recycled back to vitamin K and vitamin K hydroquinone by another enzyme, the vitamin K epoxide reductase (VKOR). Warfarin inhibits VKOR (specifically the VKORC1 subunit), thereby diminishing available vitamin K and vitamin K hydroquinone in the tissues, which decreases the carboxylation activity of the glutamyl carboxylase. When this occurs, the coagulation factors are no longer carboxylated at certain glutamic acid residues, and are incapable of binding to the endothelial surface of blood vessels, and are thus biologically inactive. As the body's stores of previously produced active factors degrade (over several days) and are replaced by inactive factors, the anticoagulation effect becomes apparent. The coagulation factors are produced, but have decreased functionality due to undercarboxylation; they are collectively referred to as PIVKAs (proteins induced vitamin K absence), and individual coagulation factors as PIVKA-number (e.g., PIVKA-II).
When warfarin is newly started, it may promote clot formation temporarily, because the level of proteins C and S are also dependent on vitamin K activity. Warfarin causes decline in protein C levels in first 36 hours. In addition, reduced levels of protein S lead to a reduction in activity of protein C (for which it is the co-factor), so reduces degradation of factor Va and factor VIIIa. Although loading doses of warfarin over 5 mg also produce a precipitous decline in factor VII, resulting in an initial prolongation of the INR, full antithrombotic effect does not take place until significant reduction in factor II occurs days later. The haemostasis system becomes temporarily biased towards thrombus formation, leading to a prothrombotic state. Thus, when warfarin is loaded rapidly at greater than 5 mg per day, to co-administering heparin, an anticoagulant that acts upon antithrombin and helps reduce the risk of thrombosis, is beneficial, with warfarin therapy for four to five days, to have the benefit of anticoagulation from heparin until the full effect of warfarin has been achieved.
Pharmacogenomics
Warfarin activity is determined partially by genetic factors. Polymorphisms in two genes (VKORC1 and CYP2C9) play a particularly large role in response to warfarin.
VKORC1 polymorphisms explain 30% of the dose variation between patients: particular mutations make VKORC1 less susceptible to suppression by warfarin. There are two main haplotypes that explain 25% of variation: low-dose haplotype group (A) and a high-dose haplotype group (B). VKORC1 polymorphisms explain why African Americans are on average relatively resistant to warfarin (higher proportion of group B haplotypes), while Asian Americans are generally more sensitive (higher proportion of group A haplotypes). Group A VKORC1 polymorphisms lead to a more rapid achievement of a therapeutic INR, but also a shorter time to reach an INR over 4, which is associated with bleeding.
CYP2C9 polymorphisms explain 10% of the dose variation between patients, mainly among Caucasian patients as these variants are rare in African American and most Asian populations. These CYP2C9 polymorphisms do not influence time to effective INR as opposed to VKORC1, but do shorten the time to INR > 4.
Despite the promise of pharmacogenomic testing in warfarin dosing, its use in clinical practice is controversial. In August 2009, the Centers for Medicare and Medicaid Services concluded, "the available evidence does not demonstrate that pharmacogenomic testing of CYP2C9 or VKORC1 alleles to predict warfarin responsiveness improves health outcomes in Medicare beneficiaries." A 2014 meta-analysis showed that using genotype-based dosing did not confer benefit in terms of time within therapeutic range, excessive anticoagulation (as defined by INR greater than 4), or a reduction in either major bleeding or thromboembolic events.
History
In the early 1920s, an outbreak occurred of a previously unrecognized cattle disease in the northern United States and Canada. Cattle were haemorrhaging after minor procedures, and on some occasions spontaneously. For example, 21 of 22 cows died after dehorning, and 12 of 25 bulls died after castration. All of these animals had bled to death.
In 1921, Frank Schofield, a Canadian veterinary pathologist, determined that the cattle were ingesting moldy silage made from sweet clover, and that this was functioning as a potent anticoagulant. Only spoiled hay made from sweet clover (grown in northern states of the US and in Canada since the turn of the century) produced the disease. Schofield separated good clover stalks and damaged clover stalks from the same hay mow, and fed each to a different rabbit. The rabbit that had ingested the good stalks remained well, but the rabbit that had ingested the damaged stalks died from a haemorrhagic illness. A duplicate experiment with a different sample of clover hay produced the same result. In 1929, North Dakota veterinarian Lee M. Roderick demonstrated that the condition was due to a lack of functioning prothrombin.
The identity of the anticoagulant substance in spoiled sweet clover remained a mystery until 1940. In 1933, Karl Paul Link and his laboratory of chemists working at the University of Wisconsin set out to isolate and characterize the haemorrhagic agent from the spoiled hay. Five years were needed before Link's student, Harold A. Campbell, recovered 6 mg of crystalline anticoagulant. Next, Link's student, Mark A. Stahmann, took over the project and initiated a large-scale extraction, isolating 1.8 g of recrystallized anticoagulant in about 4 months. This was enough material for Stahmann and Charles F. Huebner to check their results against Campbell's, and to thoroughly characterize the compound. Through degradation experiments, they established that the anticoagulant was 3,3'-methylenebis-(4-hydroxycoumarin), which they later named dicoumarol. They confirmed their results by synthesizing dicoumarol and proving in 1940 that it was identical to the naturally occurring agent.
Dicoumarol was a product of the plant molecule coumarin (not to be confused with Coumadin, a later tradename for warfarin). Coumarin is now known to be present in many plants, and produces the notably sweet smell of freshly cut grass or hay and plants such as sweet grass; in fact, the plant's high content of coumarin is responsible for the original common name of "sweet clover", which is named for its sweet smell, not its bitter taste. They are present notably in woodruff (Galium odoratum, Rubiaceae), and at lower levels in licorice, lavender, and various other species. The name coumarin comes via the French coumarou from kumarú, the Tupi name for the tree of the tonka bean, which notably contains a high concentration of coumarin. However, coumarins themselves do not influence clotting or warfarin-like action, but must first be metabolized by various fungi into compounds such as 4-hydroxycoumarin, then further (in the presence of naturally occurring formaldehyde) into dicoumarol, to have any anticoagulant properties.
Over the next few years, numerous similar chemicals (specifically 4-hydroxycoumarins with a large aromatic substituent at the 3 position) were found to have the same anticoagulant properties. The first drug in the class to be widely commercialized was dicoumarol itself, patented in 1941 and later used as a pharmaceutical. Karl Link continued working on developing more potent coumarin-based anticoagulants for use as rodent poisons, resulting in warfarin in 1948. The name "warfarin" stems from the acronym WARF, for Wisconsin Alumni Research Foundation + the ending "-arin" indicating its link with coumarin. Warfarin was first registered for use as a rodenticide in the US in 1948, and was immediately popular. Although warfarin was developed by Link, the Wisconsin Alumni Research Foundation financially supported the research and was assigned the patent.
After an incident in 1951, in which an army inductee attempted suicide with multiple doses of warfarin in rodenticide, but recovered fully after presenting to a naval hospital and being treated with vitamin K (by then known as a specific antidote), studies began in the use of warfarin as a therapeutic anticoagulant. It was found to be generally superior to dicoumarol, and in 1954, was approved for medical use in humans. An early recipient of warfarin was US President Dwight Eisenhower, who was prescribed the drug after having a heart attack in 1955.
The exact mechanism of action remained unknown until it was demonstrated, in 1978, that warfarin inhibits the enzyme vitamin K epoxide reductase, and hence interferes with vitamin K metabolism.
Lavrenty Beria and I. V. Khrustalyov are thought to have conspired to use warfarin to poison Soviet leader Joseph Stalin. Warfarin is tasteless and colourless, and produces symptoms similar to those that Stalin exhibited.
Occupational safety
Warfarin used for pest control is a hazardous substance harmful to health. People can be exposed to warfarin in the workplace by breathing it in, swallowing it, skin absorption, and eye contact. The Occupational Safety and Health Administration has set the legal limit (permissible exposure limit) for warfarin exposure in the workplace as 0.1 mg/m over an 8-hour workday. The National Institute for Occupational Safety and Health has set a recommended exposure limit of 0.1 mg/m over an 8-hour workday. At levels of 100 mg/m, warfarin is immediately dangerous to life and health.
It is classified as an extremely hazardous substance in the United States as defined in Section 302 of the U.S. Emergency Planning and Community Right-to-Know Act (42 U.S.C. 11002), and is subject to strict reporting requirements by facilities which produce, store, or use it in significant quantities.
Society and culture
The name "warfarin" is derived from the acronym for "Wisconsin Alumni Research Foundation", plus "-arin", indicating its link with coumarin. Warfarin is a derivative of dicoumarol, an anticoagulant originally discovered in spoiled sweet clover. Dicoumarol, in turn, is from coumarin, a sweet-smelling but coagulation-inactive chemical found in "sweet" clover and tonka beans (also known as cumaru from which coumarin's name derives).
Brand names
Warfarin as a drug is marketed under many brand and generic names, including Aldocumar, Anasmol, Anticoag, Befarin, Cavamed, Cicoxil, Circuvit, Cofarin, Coumadin, Coumadine, Cumar, Farin, Foley, Haemofarin, Jantoven, Kovar, Lawarin, Maforan, Marevan, Marfarin, Marivanil, Martefarin, Morfarin, Orfarin, Panwarfin, Scheme, Simarc, Varfarin, Varfarins, Varfine, Waran, Warcok, Warf, Warfareks, Warfarin, Warfarina, Warfarine, Warfarinum, Warfen, Warfin, Warik, Warin, Warlin, and Zyfarin.
Veterinary use
Warfarin is used as a poison for rats and other pests.
Pest control
Warfarin was introduced as a rodenticide, only later finding medical uses; in both cases it was used as an anticoagulant. The use of warfarin itself as a rat poison is declining, because many rat populations have developed resistance to it, and poisons of considerably greater potency have become available. However, as of 2023 warfarin continued to be considered a valuable tool for rodent control which minimised risk to other species.
Rodents
Main article: 4-hydroxycoumarins
Coumarins (4-hydroxycoumarin derivatives) are used as rodenticides for controlling rats and mice in residential, industrial, and agricultural areas. Warfarin is both odorless and tasteless, and is effective when mixed with food bait, because the rodents will return to the bait and continue to feed over a period of days until a lethal dose is accumulated (considered to be 1 mg/kg/day over about six days). It may also be mixed with talc and used as a tracking powder, which accumulates on the animal's skin and fur, and is subsequently consumed during grooming. The LD50 for warfarin is 50–100 mg/kg for a single dose, after 5–7 days. LD50 1 mg/kg for repeated daily doses for 5 days, after 5–8 days. The IDLH value is 100 mg/m (warfarin; various species).
Resistance to warfarin as a poison has developed in many rat populations due to an autosomal dominant on chromosome 1 in brown rats. This has arisen independently and become fixed several times around the world. Other 4-hydroxycoumarins used as rodenticides include coumatetralyl and brodifacoum, which is sometimes referred to as "super-warfarin", because it is more potent, longer-acting, and effective even in rat and mouse populations that are resistant to warfarin. Unlike warfarin, which is readily excreted, newer anticoagulant poisons also accumulate in the liver and kidneys after ingestion. However, such rodenticides may also accumulate in birds of prey and other animals that eat the poisoned rodents or baits.
Vampire bats
Warfarin is used to cull populations of vampire bats, in which rabies is often prevalent, in areas where human–wildlife conflict is a concern. Vampire bats are captured with mist nets and coated with a combination of petroleum jelly and warfarin. The bat returns to its roost and other members of the roost become poisoned as well by ingesting the warfarin after reciprocal grooming. Suspected vampire bat roosts may also be coated in the warfarin solution, though this kills other bat species and remains in the environment for years. The efficacy of killing vampire bats to reduce rabies transmission is questionable; a study in Peru showed that culling programs did not lead to lower transmission rates of rabies to livestock and humans.
Brand names
Warfarin as a pest control poison is marketed under many brand and generic names, including Cov-R-Tox, Co-Rax, d-Con, Dethmor, Killgerm Sewercide, Mar-Fin, Rattunal, Rax, Rodex, Rodex Blox, Rosex, Sakarat, Sewarin, Solfarin, Sorex Warfarin, Tox-Hid, Warf, warfarin, and Warfarat. Warfarin is called coumafene in France, zoocoumarin in the Netherlands and Russia, and coumarin in Japan.
References
- ^ "Warfarin international brands". Drugs.com. 12 February 2023. Archived from the original on 5 April 2017.
- ^ "Pesticide Information Profiles: WARFARIN". EXTOXNET Extension Toxicology Network. September 1995. Archived from the original on 10 June 2023. Retrieved 18 February 2023.
- ^ "Rat poison product list". The Barn Owl Trust. 22 September 2021. Archived from the original on 18 February 2023. Retrieved 18 February 2023.
- "Warfarin Use During Pregnancy". Drugs.com. 4 September 2019. Archived from the original on 9 February 2018. Retrieved 7 February 2020.
- "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- "Product information". Health Canada. 3 August 2000. Archived from the original on 23 September 2024. Retrieved 23 September 2024.
- "Product information". Health Canada. 30 June 2020. Archived from the original on 23 September 2024. Retrieved 23 September 2024.
- "Summary of Product Characteristics (SmPC)". (emc). 7 November 2023. Archived from the original on 18 August 2022. Retrieved 23 September 2024.
- ^ "Coumadin- warfarin sodium tablet". DailyMed. Archived from the original on 26 December 2021. Retrieved 25 December 2021.
- Holford NH (December 1986). "Clinical pharmacokinetics and pharmacodynamics of warfarin. Understanding the dose-effect relationship". Clinical Pharmacokinetics. 11 (6): 483–504. doi:10.2165/00003088-198611060-00005. PMID 3542339. S2CID 92210077.
- ^ "PRODUCT INFORMATION COUMADIN" (PDF). TGA eBusiness Services. Aspen Pharma Pty Ltd. 19 January 2010. Archived from the original on 17 October 2015. Retrieved 11 December 2013.
- ^ "Warfarin sodium". The American Society of Health-System Pharmacists. 13 October 2022. Archived from the original on 12 June 2018. Retrieved 16 February 2023.
- ^ Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G (February 2012). "Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e44S–e88S. doi:10.1378/chest.11-2292. PMC 3278051. PMID 22315269.
- Arcangelo VP, Peterson AM (2006). Pharmacotherapeutics for Advanced Practice: A Practical Approach. Lippincott Williams & Wilkins. p. 774. ISBN 978-0-7817-5784-3. Archived from the original on 18 September 2017.
- Dasgupta A, Wahed A (2014). "Pharmacogenomics". Clinical Chemistry, Immunology and Laboratory Quality Control. pp. 353–362. doi:10.1016/B978-0-12-407821-5.00020-6. ISBN 978-0-12-407821-5.
- Ravina E (2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. p. 148. ISBN 978-3-527-32669-3. Archived from the original on 18 September 2017.
- ^ Lim GB (December 2017). "Milestone 2: Warfarin: from rat poison to clinical use". Nature Reviews. Cardiology. doi:10.1038/nrcardio.2017.172. PMID 29238065.
- Lim GB (December 2017). "Milestone 2: Warfarin: from rat poison to clinical use". Nature Reviews. Cardiology. doi:10.1038/nrcardio.2017.172. PMID 29238065.
- World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- British national formulary (69 ed.). British Medical Association. 2015. pp. 154–155. ISBN 978-0-85711-156-2.
- "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- "Warfarin Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Archived from the original on 13 April 2020. Retrieved 30 August 2024.
- "Coumadin". The American Society of Health-System Pharmacists. Archived from the original on 3 February 2011. Retrieved 3 April 2011.
- Sanders GD, Lowenstern A, Borre E, Chatterjee R, Goode A, Sharan L, et al. (2018). Stroke Prevention in Patients With Atrial Fibrillation: A Systematic Review Update. AHRQ Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality (US). PMID 30480925.
- ^ Hirsh J, Fuster V, Ansell J, Halperin JL (May 2003). "American Heart Association/American College of Cardiology Foundation guide to warfarin therapy". Journal of the American College of Cardiology. 41 (9): 1633–1652. doi:10.1016/S0735-1097(03)00416-9. PMID 12742309.
- Kim IS, Kim HJ, Kim TH, Uhm JS, Joung B, Lee MH, et al. (October 2018). "Appropriate doses of non-vitamin K antagonist oral anticoagulants in high-risk subgroups with atrial fibrillation: Systematic review and meta-analysis". Journal of Cardiology. 72 (4): 284–291. doi:10.1016/j.jjcc.2018.03.009. PMID 29706404.
- ^ Holbrook AM, Pereira JA, Labiris R, McDonald H, Douketis JD, Crowther M, et al. (May 2005). "Systematic overview of warfarin and its drug and food interactions". Archives of Internal Medicine. 165 (10): 1095–1106. doi:10.1001/archinte.165.10.1095. PMID 15911722.
- Perry DJ, Fitzmaurice DA, Kitchen S, Mackie IJ, Mallett S (September 2010). "Point-of-care testing in haemostasis". British Journal of Haematology. 150 (5): 501–514. doi:10.1111/j.1365-2141.2010.08223.x. PMID 20618331. S2CID 32069018.
- "important information to know when you are taking : Coumadine and vitamine K" (PDF). U.S. National Institutes of Health. Archived from the original (PDF) on 20 October 2013. Retrieved 27 March 2014.
- ^ Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, et al. (February 2012). "Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e152S–e184S. doi:10.1378/chest.11-2295. PMC 3278055. PMID 22315259.
- Ebell MH (May 2005). "Evidence-based adjustment of warfarin (Coumadin) doses". American Family Physician. 71 (10): 1979–1982. PMID 15926414. Archived from the original on 1 February 2018.
- "Warfarin diet: What foods should I avoid?". Mayo Foundation. Archived from the original on 24 August 2011. Retrieved 9 August 2011.
- Hu YH, Wu F, Lo CL, Tai CT (September 2012). "Predicting warfarin dosage from clinical data: a supervised learning approach". Artificial Intelligence in Medicine. 56 (1): 27–34. doi:10.1016/j.artmed.2012.04.001. PMID 22537823.
- Solomon I, Maharshak N, Chechik G, Leibovici L, Lubetsky A, Halkin H, et al. (December 2004). "Applying an artificial neural network to warfarin maintenance dose prediction". The Israel Medical Association Journal. 6 (12): 732–735. PMID 15609884.
- ^ Ansell J, Jacobson A, Levy J, Völler H, Hasenkam JM (March 2005). "Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation" (PDF). International Journal of Cardiology. 99 (1): 37–45. doi:10.1016/j.ijcard.2003.11.008. PMID 15721497. Archived from the original (PDF) on 3 March 2016.
- Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P (February 2006). "Self-monitoring of oral anticoagulation: a systematic review and meta-analysis" (PDF). Lancet. 367 (9508): 404–411. doi:10.1016/S0140-6736(06)68139-7. PMID 16458764. S2CID 1494933. Archived from the original (PDF) on 19 March 2012.
- Cuker A, Burnett A, Triller D, Crowther M, Ansell J, Van Cott EM, et al. (June 2019). "Reversal of direct oral anticoagulants: Guidance from the Anticoagulation Forum". American Journal of Hematology. 94 (6): 697–709. doi:10.1002/ajh.25475. PMID 30916798.
- Levy JH, Ageno W, Chan NC, Crowther M, Verhamme P, Weitz JI (March 2016). "When and how to use antidotes for the reversal of direct oral anticoagulants: guidance from the SSC of the ISTH". Journal of Thrombosis and Haemostasis. 14 (3): 623–627. doi:10.1111/jth.13227. PMID 26911798. S2CID 27269191.
- ^ Brayfield A (ed), Martindale: The Complete Drug Reference London: Pharmaceutical Press
- "Coumadin" (PDF). U.S. Food and Drug Administration (FDA). October 2015. Archived (PDF) from the original on 23 June 2017. Retrieved 24 April 2017.
- Bolognia JL, Jorizzo JL, Rapini RP (2008). Dermatology (2nd ed.). St. Louis, Mo.: Mosby/Elsevier. pp. 331, 340. ISBN 978-1-4160-2999-1.
- ^ Macina OT, Schardein JL (2007). "Warfarin". Human Developmental Toxicants. Boca Raton: CRC Taylor & Francis. pp. 193–4. ISBN 978-0-8493-7229-2. Archived from the original on 5 March 2024. Retrieved 26 August 2020. Retrieved on 15 December 2008 through Google Book Search.
- ^ Loftus CM (1995). "Fetal toxicity of common neurosurgical drugs". Neurosurgical Aspects of Pregnancy. Park Ridge, Ill: American Association of Neurological Surgeons. pp. 11–3. ISBN 978-1-879284-36-4. Archived from the original on 5 March 2024. Retrieved 26 August 2020.
- ^ Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO (February 2012). "VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e691S–e736S. doi:10.1378/chest.11-2300. PMC 3278054. PMID 22315276.
- ^ Garcia D, Crowther MA, Ageno W (April 2010). "Practical management of coagulopathy associated with warfarin". BMJ. 340: c1813. doi:10.1136/bmj.c1813. PMID 20404060. S2CID 37076001.
- Brown DG, Wilkerson EC, Love WE (March 2015). "A review of traditional and novel oral anticoagulant and antiplatelet therapy for dermatologists and dermatologic surgeons". Journal of the American Academy of Dermatology. 72 (3): 524–534. doi:10.1016/j.jaad.2014.10.027. PMID 25486915.
- Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. (November 2012). "2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association" (PDF). European Heart Journal. 33 (21): 2719–2747. doi:10.1093/eurheartj/ehs253. PMID 22922413. Archived (PDF) from the original on 27 January 2024. Retrieved 5 March 2024.
- Shoeb M, Fang MC (April 2013). "Assessing bleeding risk in patients taking anticoagulants". Journal of Thrombosis and Thrombolysis. 35 (3): 312–319. doi:10.1007/s11239-013-0899-7. PMC 3888359. PMID 23479259.
- Elliott MJ, Zimmerman D, Holden RM (September 2007). "Warfarin anticoagulation in hemodialysis patients: a systematic review of bleeding rates". American Journal of Kidney Diseases. 50 (3): 433–440. doi:10.1053/j.ajkd.2007.06.017. PMID 17720522.
- Fang MC, Go AS, Chang Y, Borowsky LH, Pomernacki NK, Udaltsova N, et al. (July 2011). "A new risk scheme to predict warfarin-associated hemorrhage: The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study". Journal of the American College of Cardiology. 58 (4): 395–401. doi:10.1016/j.jacc.2011.03.031. PMC 3175766. PMID 21757117.
- Delaney JA, Opatrny L, Brophy JM, Suissa S (August 2007). "Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding". CMAJ. 177 (4): 347–351. doi:10.1503/cmaj.070186. PMC 1942107. PMID 17698822.
- Chan YC, Valenti D, Mansfield AO, Stansby G (March 2000). "Warfarin induced skin necrosis". The British Journal of Surgery. 87 (3): 266–272. doi:10.1046/j.1365-2168.2000.01352.x. PMC 4928566. PMID 10718793.
- Caraballo PJ, Heit JA, Atkinson EJ, Silverstein MD, O'Fallon WM, Castro MR, et al. (1999). "Long-term use of oral anticoagulants and the risk of fracture". Archives of Internal Medicine. 159 (15): 1750–1756. doi:10.1001/archinte.159.15.1750. PMID 10448778.
- Pilon D, Castilloux AM, Dorais M, LeLorier J (May 2004). "Oral anticoagulants and the risk of osteoporotic fractures among elderly". Pharmacoepidemiology and Drug Safety. 13 (5): 289–294. doi:10.1002/pds.888. PMID 15133779. S2CID 45496277.
- Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF (January 2006). "Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2". Archives of Internal Medicine. 166 (2): 241–246. doi:10.1001/archinte.166.2.241. PMID 16432096.
- O'Keeffe ST, Woods BO, Breslin DJ, Tsapatsaris NP (November 1992). "Blue toe syndrome. Causes and management". Archives of Internal Medicine. 152 (11): 2197–2202. doi:10.1001/archinte.1992.00400230023004. PMID 1444678.
- Talmadge DB, Spyropoulos AC (May 2003). "Purple toes syndrome associated with warfarin therapy in a patient with antiphospholipid syndrome". Pharmacotherapy. 23 (5): 674–677. doi:10.1592/phco.23.5.674.32200. PMID 12741443. S2CID 28632135.
- Palaniswamy C, Sekhri A, Aronow WS, Kalra A, Peterson SJ (February 2011). "Association of warfarin use with valvular and vascular calcification: a review". Clinical Cardiology. 34 (2): 74–81. doi:10.1002/clc.20865. PMC 6652734. PMID 21298649.
- ^ Abimbola Farinde (18 April 2019). "Warfarin Overanticoagulation". Medscape. Archived from the original on 19 August 2022. Retrieved 19 August 2022.
- Chai-Adisaksopha C, Hillis C, Siegal DM, Movilla R, Heddle N, Iorio A, et al. (October 2016). "Prothrombin complex concentrates versus fresh frozen plasma for warfarin reversal. A systematic review and meta-analysis". Thrombosis and Haemostasis. 116 (5): 879–890. doi:10.1160/TH16-04-0266. PMID 27488143. S2CID 4733615.
- Tornkvist M, Smith JG, Labaf A (February 2018). "Current evidence of oral anticoagulant reversal: A systematic review". Thrombosis Research. 162: 22–31. doi:10.1016/j.thromres.2017.12.003. PMID 29258056.
- Crowther MA, Douketis JD, Schnurr T, Steidl L, Mera V, Ultori C, et al. (August 2002). "Oral vitamin K lowers the international normalized ratio more rapidly than subcutaneous vitamin K in the treatment of warfarin-associated coagulopathy. A randomized, controlled trial". Annals of Internal Medicine. 137 (4): 251–254. doi:10.7326/0003-4819-137-4-200208200-00009. PMID 12186515. S2CID 10450603.
- Gage BF, Fihn SD, White RH (October 2000). "Management and dosing of warfarin therapy". The American Journal of Medicine. 109 (6): 481–488. doi:10.1016/S0002-9343(00)00545-3. PMID 11042238.
- Ament PW, Bertolino JG, Liszewski JL (March 2000). "Clinically significant drug interactions". American Family Physician. 61 (6): 1745–1754. PMID 10750880. Archived from the original on 7 May 2016. Retrieved 22 August 2023.
- Carpenter M, Berry H, Pelletier AL (May 2019). "Clinically Relevant Drug-Drug Interactions in Primary Care". American Family Physician. 99 (9): 558–564. PMID 31038898. Archived from the original on 23 August 2023. Retrieved 22 August 2023.
- Juurlink DN (August 2007). "Drug interactions with warfarin: what clinicians need to know". CMAJ. 177 (4): 369–371. doi:10.1503/cmaj.070946. PMC 1942100. PMID 17698826.
- ^ Kurnik D, Loebstein R, Farfel Z, Ezra D, Halkin H, Olchovsky D (March 2004). "Complex drug-drug-disease interactions between amiodarone, warfarin, and the thyroid gland". Medicine. 83 (2): 107–113. doi:10.1097/01.md.0000123095.65294.34. PMID 15028964. S2CID 43173080.
- Stephens MA, Self TH, Lancaster D, Nash T (December 1989). "Hypothyroidism: effect on warfarin anticoagulation". Southern Medical Journal. 82 (12): 1585–1586. doi:10.1097/00007611-198912000-00035. PMID 2595433.
- Chute JP, Ryan CP, Sladek G, Shakir KM (1997). "Exacerbation of warfarin-induced anticoagulation by hyperthyroidism". Endocrine Practice. 3 (2): 77–79. doi:10.4158/EP.3.2.77. PMID 15251480.
- Kellett HA, Sawers JS, Boulton FE, Cholerton S, Park BK, Toft AD (January 1986). "Problems of anticoagulation with warfarin in hyperthyroidism". The Quarterly Journal of Medicine. 58 (225): 43–51. PMID 3704105.
- Weathermon R, Crabb DW (1999). "Alcohol and medication interactions". Alcohol Research & Health. 23 (1): 40–54. PMC 6761694. PMID 10890797.
- "Warfarin Anticoagulant Medication". Archived from the original on 1 July 2020. Retrieved 30 June 2020.
- Austin S, Batz F (1999). Lininger SW (ed.). A-Z guide to drug-herb-vitamin interactions: how to improve your health and avoid problems when using common medications and natural supplements together. Roseville, Calif: Prima Health. p. 224. ISBN 978-0-7615-1599-9.
- Heck AM, DeWitt BA, Lukes AL (July 2000). "Potential interactions between alternative therapies and warfarin". American Journal of Health-System Pharmacy. 57 (13): 1221–1227, quiz 1228–1230. doi:10.1093/ajhp/57.13.1221. PMID 10902065.
- Barnes J, Working Group on Complementary Medicine (September 2002). "Herb-medicine interactions: St John's Wort (Hypericum perforatum) Useful information for pharmacist" (PDF). London: Royal Pharmaceutical Society of Great Britain. p. 5. Archived from the original (PDF) on 24 September 2006. Retrieved 14 January 2009.
- "Cranberry juice clot drug warning". BBC News. 18 September 2003. Archived from the original on 9 February 2008. Retrieved 18 May 2008.
- Suvarna R, Pirmohamed M, Henderson L (December 2003). "Possible interaction between warfarin and cranberry juice". BMJ. 327 (7429): 1454. doi:10.1136/bmj.327.7429.1454. PMC 300803. PMID 14684645.
- ^ Aston JL, Lodolce AE, Shapiro NL (September 2006). "Interaction between warfarin and cranberry juice". Pharmacotherapy. 26 (9): 1314–1319. doi:10.1592/phco.26.9.1314. PMID 16945054. S2CID 28468365.Free full text with registration at Medscape Archived 9 November 2010 at the Wayback Machine
- Pham DQ, Pham AQ (March 2007). "Interaction potential between cranberry juice and warfarin". American Journal of Health-System Pharmacy. 64 (5): 490–494. doi:10.2146/ajhp060370. PMID 17322161.
- Valente EJ, Trager, Jensen LH (1975). "The crystal and molecular structure and absolute configuration of (−)-(S)-warfarin". Acta Crystallographica Section B. 31 (4): 954–960. Bibcode:1975AcCrB..31..954V. doi:10.1107/S056774087500427X. Archived from the original on 20 October 2015.
- Karlsson BC, Rosengren AM, Andersson PO, Nicholls IA (September 2007). "The spectrophysics of warfarin: implications for protein binding". The Journal of Physical Chemistry B. 111 (35): 10520–10528. doi:10.1021/jp072505i. PMID 17691835.
- Rote Liste 2017 – Arzneimittelverzeichnis für Deutschland (einschließlich EU-Zulassungen und bestimmter Medizinprodukte). Frankfurt/Main: Rote Liste Service GmbH. 2017. p. 226. ISBN 978-3-946057-10-9.
- Shaik AN, Grater R, Lulla M, Williams DA, Gan LL, Bohnert T, et al. (January 2016). "Comparison of enzyme kinetics of warfarin analyzed by LC-MS/MS QTrap and differential mobility spectrometry". Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences. 1008 (1): 164–173. doi:10.1016/j.jchromb.2015.11.036. PMID 26655108.
- X-Ray Vision: The Evolution of Medical Imaging and Its Human Significance. Oxford University Press. 28 November 2012. ISBN 978-0-19-997624-9. Archived from the original on 30 June 2023. Retrieved 20 March 2023.
- Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G (June 2008). "Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition)". Chest. 133 (6 Suppl): 160S – 198S. doi:10.1378/chest.08-0670. PMID 18574265. S2CID 12305488.
- Freedman MD (March 1992). "Oral anticoagulants: pharmacodynamics, clinical indications and adverse effects". Journal of Clinical Pharmacology. 32 (3): 196–209. doi:10.1002/j.1552-4604.1992.tb03827.x. PMID 1564123. S2CID 38963632.
- ^ Whitlon DS, Sadowski JA, Suttie JW (April 1978). "Mechanism of coumarin action: significance of vitamin K epoxide reductase inhibition". Biochemistry. 17 (8): 1371–1377. doi:10.1021/bi00601a003. PMID 646989.
- Li T, Chang CY, Jin DY, Lin PJ, Khvorova A, Stafford DW (February 2004). "Identification of the gene for vitamin K epoxide reductase". Nature. 427 (6974): 541–544. Bibcode:2004Natur.427..541L. doi:10.1038/nature02254. PMID 14765195. S2CID 4424554.
- ^ Rost S, Fregin A, Ivaskevicius V, Conzelmann E, Hörtnagel K, Pelz HJ, et al. (February 2004). "Mutations in VKORC1 cause warfarin resistance and multiple coagulation factor deficiency type 2". Nature. 427 (6974): 537–541. Bibcode:2004Natur.427..537R. doi:10.1038/nature02214. PMID 14765194. S2CID 4424197.
- Litin SC, Gastineau DA (March 1995). "Current concepts in anticoagulant therapy". Mayo Clinic Proceedings. 70 (3): 266–272. doi:10.4065/70.3.266. PMID 7861815.
- Wittkowsky AK (2005). "Why warfarin and heparin need to overlap when treating acute venous thromboembolism". Disease-a-Month. 51 (2–3): 112–115. doi:10.1016/j.disamonth.2005.03.005. PMID 15900262.
- ^ Wadelius M, Chen LY, Downes K, Ghori J, Hunt S, Eriksson N, et al. (2005). "Common VKORC1 and GGCX polymorphisms associated with warfarin dose". The Pharmacogenomics Journal. 5 (4): 262–270. doi:10.1038/sj.tpj.6500313. PMID 15883587.
- ^ Rieder MJ, Reiner AP, Gage BF, Nickerson DA, Eby CS, McLeod HL, et al. (June 2005). "Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose". The New England Journal of Medicine. 352 (22): 2285–2293. doi:10.1056/NEJMoa044503. PMID 15930419.
- ^ Schwarz UI, Ritchie MD, Bradford Y, Li C, Dudek SM, Frye-Anderson A, et al. (March 2008). "Genetic determinants of response to warfarin during initial anticoagulation". The New England Journal of Medicine. 358 (10): 999–1008. doi:10.1056/NEJMoa0708078. PMC 3894627. PMID 18322281.
- Sanderson S, Emery J, Higgins J (February 2005). "CYP2C9 gene variants, drug dose, and bleeding risk in warfarin-treated patients: a HuGEnet systematic review and meta-analysis". Genetics in Medicine. 7 (2): 97–104. doi:10.1097/01.GIM.0000153664.65759.CF. PMID 15714076.
- Jensen TS, Jacques LB, Ciccanti M, Long K, Eggleston L, Roche J (3 August 2009). "Decision Memo for Pharmacogenomic Testing for Warfarin Response (CAG-00400N)". Centers for Medicare and Medicaid Services. Archived from the original on 14 April 2018. Retrieved 14 April 2018.
- Stergiopoulos K, Brown DL (August 2014). "Genotype-guided vs clinical dosing of warfarin and its analogues: meta-analysis of randomized clinical trials". JAMA Internal Medicine. 174 (8): 1330–1338. doi:10.1001/jamainternmed.2014.2368. PMID 24935087.
- ^ Rajagopalan R (2018). "A Study in Scarlet". Distillations. 4 (1): 26–35. Archived from the original on 23 June 2019. Retrieved 27 June 2018.
- ^ Laurence DR, Kneebone P (1973). Clinical Pharmacology. Edinburgh, London and New York: Churchill Livingstone. pp. 23.4 – 23.5. ISBN 978-0-443-04990-3.
- Schofield FW (1924). "Damaged sweet clover; the cause of a new disease in cattle simulating haemorrhagic septicemia and blackleg". J Am Vet Med Assoc. 64: 553–6.
- Roderick LM (1931). "A problem in the coagulation of the blood; "sweet clover disease of the cattle"". Am J Physiol. 96 (2): 413–425. doi:10.1152/ajplegacy.1931.96.2.413.
- Stahmann MA, Huebner CF, Link KP (1 April 1941). "Studies on the hemorrhagic sweet clover disease. V. Identification and synthesis of the hemorrhagic agent". J Biol Chem. 138 (2): 513–27. doi:10.1016/S0021-9258(18)51377-6.
- "Warfarin, Molecule of the Month for February 2011, by John Maher". www.chm.bris.ac.uk. Archived from the original on 27 September 2023. Retrieved 20 December 2023.
- ^ Link KP (January 1959). "The discovery of dicumarol and its sequels". Circulation. 19 (1): 97–107. doi:10.1161/01.CIR.19.1.97. PMID 13619027.
- Naumov VP, Brent J (2003). Stalin's last crime: the plot against the Jewish doctors, 1948–1953. London: HarperCollins. ISBN 978-0-06-019524-3.
- "CDC – NIOSH Pocket Guide to Chemical Hazards – Warfarin". www.cdc.gov. Archived from the original on 8 December 2015. Retrieved 27 November 2015.
- "40 C.F.R.: Appendix A to Part 355—The List of Extremely Hazardous Substances and Their Threshold Planning Quantities" (21 August 2023 ed.). Government Printing Office. Archived from the original on 9 January 2023. Retrieved 22 August 2023.
- ^ Eason CT, Wickstrom M (2001). "2. Anticoagulant poisons" (PDF). Vertebrate pesticide toxicology manual (poisons). New Zealand Department of Conservation. pp. 41–74. ISBN 978-0-478-22035-3. Archived (PDF) from the original on 17 October 2008.
- ^ Endepols S, Buckle A, Eason C, Pelz HJ, Meyer A, Berny P, et al. (September 2015). "RRAC guidelines on Anticoagulant Rodenticide Resistance Management" (PDF). RRAC. Brussels: CropLife. pp. 1–29. Archived (PDF) from the original on 4 November 2021. Retrieved 23 October 2021.
- "Warfarin - A valuable tool for successful rodent control whilst minimising risk to non-target species". National Pest Technicians Association. 21 October 2019. Archived from the original on 17 February 2023. Retrieved 18 February 2023.
- United States Occupational Safety and Health Administration (OSHA) (16 August 1996). "Documentation for Immediately Dangerous To Life or Health Concentrations (IDLHs): Warfarin". Centers for Disease Control and Prevention. Archived from the original on 26 July 2008. Retrieved 7 July 2008.
- Lovett RA (14 November 2012). "Killing rats is killing birds". Nature. doi:10.1038/nature.2012.11824. Archived from the original on 26 April 2015. Retrieved 5 April 2015.
- ^ Johnson N, Aréchiga-Ceballos N, Aguilar-Setien A (April 2014). "Vampire bat rabies: ecology, epidemiology and control". Viruses. 6 (5): 1911–1928. doi:10.3390/v6051911. PMC 4036541. PMID 24784570.
- Streicker DG, Recuenco S, Valderrama W, Gomez Benavides J, Vargas I, Pacheco V, et al. (September 2012). "Ecological and anthropogenic drivers of rabies exposure in vampire bats: implications for transmission and control". Proceedings. Biological Sciences. 279 (1742): 3384–3392. doi:10.1098/rspb.2012.0538. PMC 3396893. PMID 22696521.
Further reading
- Dean L (2012). "Warfarin Therapy and VKORC1 and CYP Genotype". In Pratt VM, McLeod HL, Rubinstein WS, Scott SA, Dean LC, Kattman BL, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520347. Bookshelf ID: NBK84174.
External links
- Warfarin in the Pesticide Properties DataBase (PPDB)
| Antithrombotics (thrombolytics, anticoagulants and antiplatelet drugs) (B01) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antiplatelet drugs |
| ||||||||||||||
| Anticoagulants |
| ||||||||||||||
| Thrombolytic drugs/ fibrinolytics | |||||||||||||||
| Non-medicinal | |||||||||||||||
| |||||||||||||||
| Pest control: Rodenticides | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Anticoagulants / Vitamin K antagonists |
| ||||||||
| Convulsants | |||||||||
| Calciferols | |||||||||
| Inorganic compounds | |||||||||
| Organochlorine | |||||||||
| Organophosphorus | |||||||||
| Carbamates | |||||||||
| Others | |||||||||