| Revision as of 14:53, 3 January 2025 edit109.241.162.167 (talk) →Synthesis and breakdown: fix journal name← Previous edit |
Latest revision as of 18:19, 3 January 2025 edit undo109.241.162.167 (talk) change to subscript in refs |
| Line 47: |
Line 47: |
|
}} |
|
}} |
|
|
|
|
|
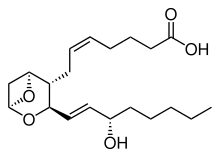
'''Thromboxane A<sub>2</sub>''' ('''TXA<sub>2</sub>''') is a type of ] that is produced by activated ] during ] and has prothrombotic properties: it stimulates activation of new platelets as well as increases platelet aggregation. This is achieved by activating the ], which results in platelet-shape change, inside-out activation of ]s, and ].<ref>{{Cite journal|last=Offermanns|first=Stefan|date=2006-12-08|title=Activation of Platelet Function Through G Protein–Coupled Receptors|journal=Circulation Research|language=EN|volume=99|issue=12|pages=1293–1304|doi=10.1161/01.res.0000251742.71301.16|pmid=17158345|issn=0009-7330|doi-access=free}}</ref> Circulating ] binds these receptors on adjacent platelets, further strengthening the ]. TXA<sub>2</sub> is also a known ]<ref>{{Cite journal|last1=Ding|first1=Xueqin|last2=Murray|first2=Paul A.|date=November 2005|title=Cellular mechanisms of thromboxane A2-mediated contraction in pulmonary veins|journal=American Journal of Physiology. Lung Cellular and Molecular Physiology|volume=289|issue=5|pages=L825–833|doi=10.1152/ajplung.00177.2005|issn=1040-0605|pmid=15964897|s2cid=3171857 }}</ref><ref>{{Cite journal|last1=Yamamoto|first1=K.|last2=Ebina|first2=S.|last3=Nakanishi|first3=H.|last4=Nakahata|first4=N.|date=November 1995|title=Thromboxane A2 receptor-mediated signal transduction in rabbit aortic smooth muscle cells|journal=General Pharmacology|volume=26|issue=7|pages=1489–1498|issn=0306-3623|pmid=8690235|doi=10.1016/0306-3623(95)00025-9}}</ref><ref>{{Cite journal|last=Smyth|first=Emer M|date=2010-04-01|title=Thromboxane and the thromboxane receptor in cardiovascular disease|journal=Clinical Lipidology|volume=5|issue=2|pages=209–219|doi=10.2217/CLP.10.11|issn=1758-4299|pmc=2882156|pmid=20543887}}</ref><ref>{{Cite journal|last1=Winn|first1=R|last2=Harlan|first2=J|last3=Nadir|first3=B|last4=Harker|first4=L|last5=Hildebrandt|first5=J|date=September 1983|title=Thromboxane A2 mediates lung vasoconstriction but not permeability after endotoxin.|journal=Journal of Clinical Investigation|volume=72|issue=3|pages=911–918|issn=0021-9738|pmc=1129256|pmid=6886010|doi=10.1172/jci111062}}</ref> and is especially important during tissue injury and inflammation. It is also regarded as responsible for ]. |
|
'''Thromboxane A<sub>2</sub>''' ('''TXA<sub>2</sub>''') is a type of ] that is produced by activated ] during ] and has prothrombotic properties: it stimulates activation of new platelets as well as increases platelet aggregation. This is achieved by activating the ], which results in platelet-shape change, inside-out activation of ]s, and ].<ref>{{Cite journal|last=Offermanns|first=Stefan|date=2006-12-08|title=Activation of Platelet Function Through G Protein–Coupled Receptors|journal=Circulation Research|language=EN|volume=99|issue=12|pages=1293–1304|doi=10.1161/01.res.0000251742.71301.16|pmid=17158345|issn=0009-7330|doi-access=free}}</ref> Circulating ] binds these receptors on adjacent platelets, further strengthening the ]. TXA<sub>2</sub> is also a known ]<ref>{{Cite journal|last1=Ding|first1=Xueqin|last2=Murray|first2=Paul A.|date=November 2005|title=Cellular mechanisms of thromboxane A<sub>2</sub>-mediated contraction in pulmonary veins|journal=American Journal of Physiology. Lung Cellular and Molecular Physiology|volume=289|issue=5|pages=L825–833|doi=10.1152/ajplung.00177.2005|issn=1040-0605|pmid=15964897|s2cid=3171857 }}</ref><ref>{{Cite journal|last1=Yamamoto|first1=K.|last2=Ebina|first2=S.|last3=Nakanishi|first3=H.|last4=Nakahata|first4=N.|date=November 1995|title=Thromboxane A<sub>2</sub> receptor-mediated signal transduction in rabbit aortic smooth muscle cells|journal=General Pharmacology|volume=26|issue=7|pages=1489–1498|issn=0306-3623|pmid=8690235|doi=10.1016/0306-3623(95)00025-9}}</ref><ref>{{Cite journal|last=Smyth|first=Emer M|date=2010-04-01|title=Thromboxane and the thromboxane receptor in cardiovascular disease|journal=Clinical Lipidology|volume=5|issue=2|pages=209–219|doi=10.2217/CLP.10.11|issn=1758-4299|pmc=2882156|pmid=20543887}}</ref><ref>{{Cite journal|last1=Winn|first1=R|last2=Harlan|first2=J|last3=Nadir|first3=B|last4=Harker|first4=L|last5=Hildebrandt|first5=J|date=September 1983|title=Thromboxane A<sub>2</sub> mediates lung vasoconstriction but not permeability after endotoxin.|journal=Journal of Clinical Investigation|volume=72|issue=3|pages=911–918|issn=0021-9738|pmc=1129256|pmid=6886010|doi=10.1172/jci111062}}</ref> and is especially important during tissue injury and inflammation. It is also regarded as responsible for ]. |
|
|
|
|
|
Receptors that mediate TXA<sub>2</sub> actions are ]. The human TXA<sub>2</sub> receptor (TP) is a typical G protein-coupled receptor (GPCR) with seven transmembrane segments. In humans, two TP receptor splice variants – TPα and TPβ – have so far been cloned. |
|
Receptors that mediate TXA<sub>2</sub> actions are ]. The human TXA<sub>2</sub> receptor (TP) is a typical G protein-coupled receptor (GPCR) with seven transmembrane segments. In humans, two TP receptor splice variants – TPα and TPβ – have so far been cloned. |
| Line 54: |
Line 54: |
|
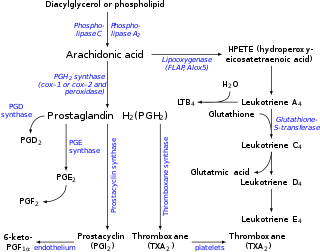
Thromboxane A<sub>2</sub> (TXA<sub>2</sub>) is generated from ] by ] in a metabolic reaction which generates approximately equal amounts of ] (12-HHT). ] irreversibly inhibits platelet ] preventing the formation of prostaglandin H<sub>2</sub>, and therefore TXA<sub>2</sub>. Contrastly, TXA<sub>2</sub> vascular tissue synthesis is stimulated by angiotensin II which promotes cyclooxygenase I's metabolism of arachidonic acid. An angiotensin II dependent pathway also induces hypertension and interacts with TXA<sub>2</sub> receptors.<ref>{{Cite journal |last1=Francois |first1=Helene |last2=Athirakul |first2=Krairerk |last3=Mao |first3=Lan |last4=Rockman |first4=Howard |last5=Coffman |first5=Thomas M. |date=February 2004 |title=Role for Thromboxane Receptors in Angiotensin-II–Induced Hypertension |journal=Hypertension |language=en |volume=43 |issue=2 |pages=364–369 |doi=10.1161/01.HYP.0000112225.27560.24 |issn=0194-911X|doi-access=free |pmid=14718360 }}</ref> |
|
Thromboxane A<sub>2</sub> (TXA<sub>2</sub>) is generated from ] by ] in a metabolic reaction which generates approximately equal amounts of ] (12-HHT). ] irreversibly inhibits platelet ] preventing the formation of prostaglandin H<sub>2</sub>, and therefore TXA<sub>2</sub>. Contrastly, TXA<sub>2</sub> vascular tissue synthesis is stimulated by angiotensin II which promotes cyclooxygenase I's metabolism of arachidonic acid. An angiotensin II dependent pathway also induces hypertension and interacts with TXA<sub>2</sub> receptors.<ref>{{Cite journal |last1=Francois |first1=Helene |last2=Athirakul |first2=Krairerk |last3=Mao |first3=Lan |last4=Rockman |first4=Howard |last5=Coffman |first5=Thomas M. |date=February 2004 |title=Role for Thromboxane Receptors in Angiotensin-II–Induced Hypertension |journal=Hypertension |language=en |volume=43 |issue=2 |pages=364–369 |doi=10.1161/01.HYP.0000112225.27560.24 |issn=0194-911X|doi-access=free |pmid=14718360 }}</ref> |
|
|
|
|
|
TXA<sub>2</sub> is very unstable in aqueous solution, since it is hydrated within about 30 seconds to the biologically inactive ]. 12-HHT, while once thought to be an inactive byproduct of TXA<sub>2</sub> synthesis, has recently been shown to have a range of potentially important actions, some of which relate to the actions of TXA<sub>2</sub> (see ]).<ref>{{cite journal | doi = 10.1093/jb/mvu078 | volume=157 | title=Two distinct leukotriene B4 receptors, BLT1 and BLT2 | year=2014 | journal=Journal of Biochemistry | pages=65–71 | last1 = Yokomizo | first1 = T. | issue=2 | pmid=25480980| doi-access= }}</ref> Due to its very short half life, TXA<sub>2</sub> primarily functions as an autocrine or paracrine mediator in the nearby tissues surrounding its site of production. Most work in the field of TXA<sub>2</sub> is done instead with synthetic analogs such as ] and ].<ref name= Wilson >{{cite journal |vauthors=Wilson DP, Susnjar M, Kiss E, Sutherland C, Walsh MP |date=April 2005 |title=Thromboxane A<sub>2</sub>-induced contraction of rat caudal arterial smooth muscle involves activation of Ca<sup>2+</sup> entry and Ca<sup>2+</sup> sensitization: Rho-associated kinase-mediated phosphorylation of MYPT1 at Thr-855 but not Thr-697 |journal=Biochemical Journal |volume=389(Pt 3) |pages=763-774 |publisher= Portland Press |doi=10.1042/BJ20050237 |pmc=1180727 |pmid=15823093 }}</ref> In human studies, ] levels are used to indirectly measure TXA<sub>2</sub> production.<ref>{{cite journal|title=11-Dehydrothromboxane B2: a quantitative index of thromboxane A2 formation in the human circulation|vauthors=Catella F, Healy D, Lawson JA, FitzGerald GA|journal=PNAS|year=1986|volume=83|issue=16|pages=5861–5865|pmid=3461463|doi=10.1073/pnas.83.16.5861|pmc=386396|bibcode=1986PNAS...83.5861C|doi-access=free}}</ref><ref>{{cite journal|vauthors=Lordkipanidzé M, Pharand C, Schampaert E, Turgeon J, Palisaitis DA, Diodati JG|title=A comparison of six major platelet function tests to determine the prevalence of aspirin resistance in patients with stable coronary artery disease|journal=Eur Heart J|year=2007|volume=28|issue=14|pages=1702–1708|doi=10.1093/eurheartj/ehm226|pmid=17569678|doi-access=free}}</ref> |
|
TXA<sub>2</sub> is very unstable in aqueous solution, since it is hydrated within about 30 seconds to the biologically inactive ]. 12-HHT, while once thought to be an inactive byproduct of TXA<sub>2</sub> synthesis, has recently been shown to have a range of potentially important actions, some of which relate to the actions of TXA<sub>2</sub> (see ]).<ref>{{cite journal | doi = 10.1093/jb/mvu078 | volume=157 | title=Two distinct leukotriene B<sub>4</sub> receptors, BLT1 and BLT2 | year=2014 | journal=Journal of Biochemistry | pages=65–71 | last1 = Yokomizo | first1 = T. | issue=2 | pmid=25480980| doi-access= }}</ref> Due to its very short half life, TXA<sub>2</sub> primarily functions as an autocrine or paracrine mediator in the nearby tissues surrounding its site of production. Most work in the field of TXA<sub>2</sub> is done instead with synthetic analogs such as ] and ].<ref name= Wilson >{{cite journal |vauthors=Wilson DP, Susnjar M, Kiss E, Sutherland C, Walsh MP |date=April 2005 |title=Thromboxane A<sub>2</sub>-induced contraction of rat caudal arterial smooth muscle involves activation of Ca<sup>2+</sup> entry and Ca<sup>2+</sup> sensitization: Rho-associated kinase-mediated phosphorylation of MYPT1 at Thr-855, but not Thr-697 |journal=Biochemical Journal |volume=389(Pt 3) |pages=763-774 |publisher= Portland Press |doi=10.1042/BJ20050237 |pmc=1180727 |pmid=15823093 }}</ref> In human studies, ] levels are used to indirectly measure TXA<sub>2</sub> production.<ref>{{cite journal|title=11-Dehydrothromboxane B<sub>2</sub>: a quantitative index of thromboxane A<sub>2</sub> formation in the human circulation|vauthors=Catella F, Healy D, Lawson JA, FitzGerald GA|journal=PNAS|year=1986|volume=83|issue=16|pages=5861–5865|pmid=3461463|doi=10.1073/pnas.83.16.5861|pmc=386396|bibcode=1986PNAS...83.5861C|doi-access=free}}</ref><ref>{{cite journal|vauthors=Lordkipanidzé M, Pharand C, Schampaert E, Turgeon J, Palisaitis DA, Diodati JG|title=A comparison of six major platelet function tests to determine the prevalence of aspirin resistance in patients with stable coronary artery disease|journal=Eur Heart J|year=2007|volume=28|issue=14|pages=1702–1708|doi=10.1093/eurheartj/ehm226|pmid=17569678|doi-access=free}}</ref> |
|
|
|
|
|
] |
|
] |